White Matter Lesions - Differential diagnosis
Robin Smithuis and Frederik Barkhof
Amsterdam University Medical Center and University College London and Alrijne Hospital Leiderdorp, the Netherlands
Publicationdate
White matter lesions (WMLs) are common findings in MRI examinations of the brain.
They are best seen on T2W- and FLAIR imaging.
WMLs are seen in normal aging and are probably the result of small vessel disease.
It is more frequent in patients with vascular disorders like atherosclerosis, amyloid angiopathy, migraine, CADASIL and vasculitis.
The list of diagnoses is very long and includes besides these vascular disorders also non-vascular disorders like inflammation, infection, toxic and metabolic and also genetic disorders with leukodystrophy.
We will review some of the more common diseases that present with WMLs.
Introduction
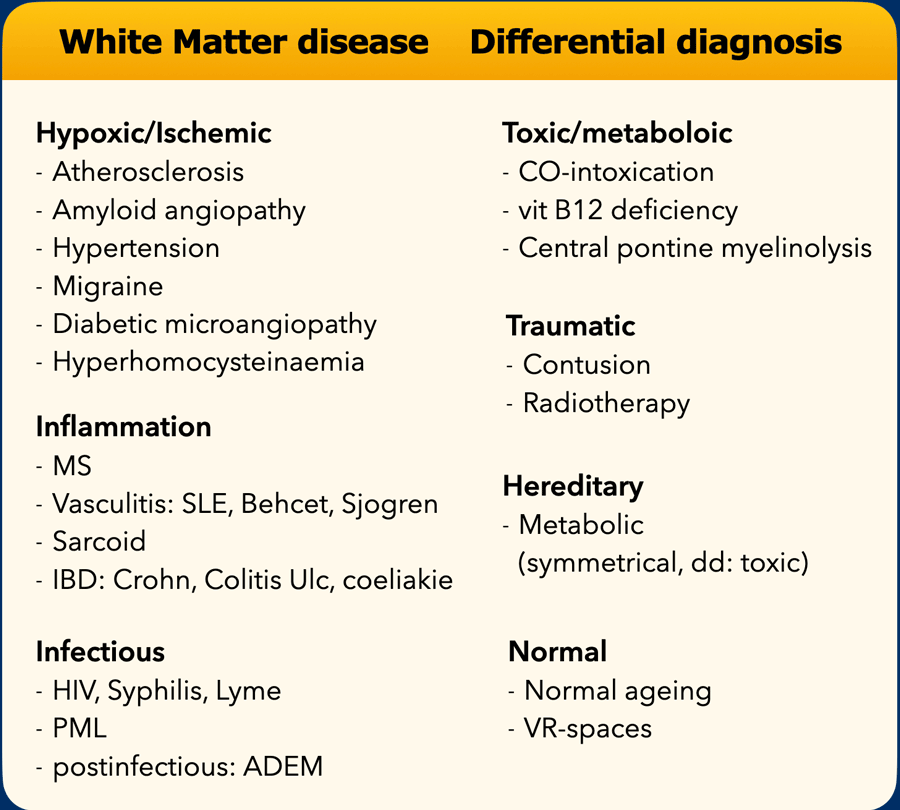
Differential diagnosis
The differential diagnosis of white matter lesions (WMLs) is extremely long (see table).
Here are some statements about WMLs:
- Most WMLs are acquired and of hypoxic-ischemic origin.
- WMLs are seen in normal aging
- The most common inflammatory disease is Multiple Sclerosis.
- The most common viral infections are PML and HIV.
- Inherited diseases usually will have symmetrical abnormalities, so they have to be differentiated from intoxications.
- Only if the clinical findings strongly direct us towards inflammatory, infectious, toxic or other diseases, should we consider these diagnoses.
- Suggesting the diagnosis of MS in a patient with WMLs and with no clinical suspicion for MS would be unwise.
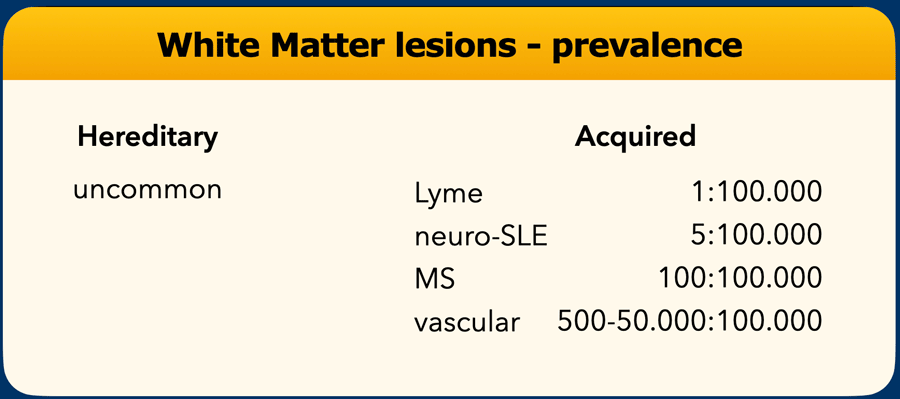
Prevalence
When we look at the prevalence of the white matter diseases, you will notice that there are enormous differences.
When incidental WMLs are found, these are usually the result of small vessel disease, since up to 50% of patients that get an MR examination for whatever reason, will have WMLs of vascular origin.
They are more common in older people and in patients with vascular risk factors like atherosclerosis, high blood pressure, high cholesterol, diabetes, amyloid angiopathy, hyperhomocysteinemia, atrial fibrillation etc.
Hereditary diseases are extremely uncommon as individual diseases, but as a group they are not that uncommon, but still far more uncommon than MS.
If we look at the prevalence of Lyme disease, which is a rather popular disease at the moment, then we will notice that it still is a very uncommon disease despite of all the serological tests that are being performed nowadays.
Imaging findings
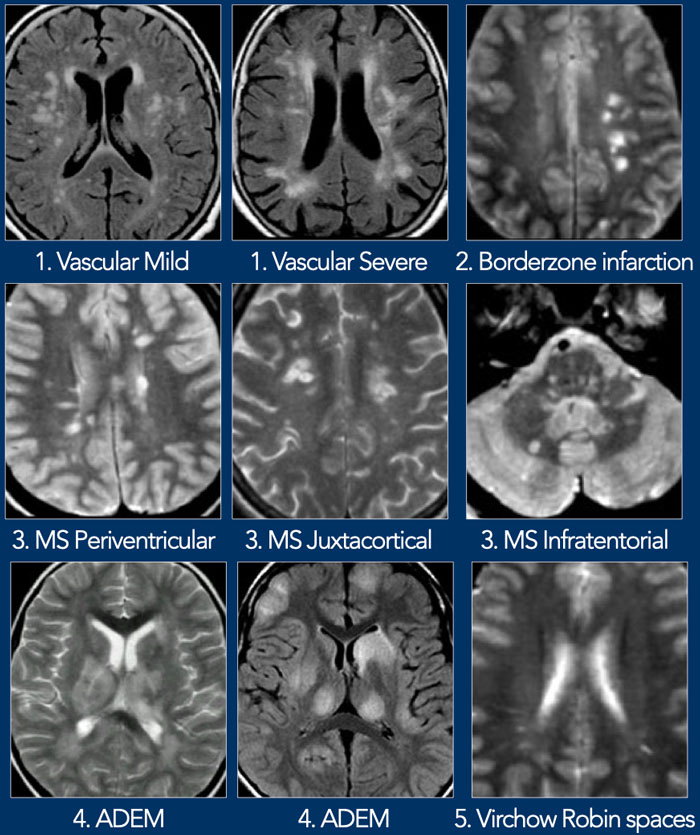
Multiple punctate and patchy lesions
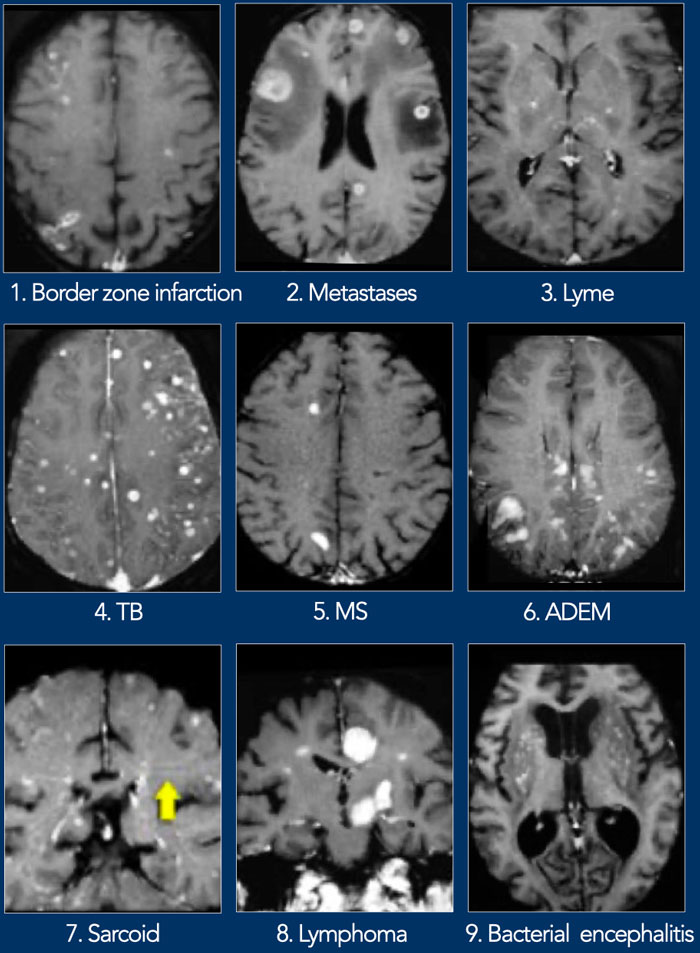
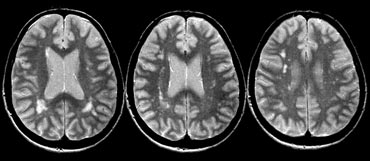
The figure shows a collection of images with multiple punctate and patchy lesions in the WM.
- Small vessel disease
WMLs in the deep white matter. Not located in corpus callosum, juxtaventricular or juxtacortical. - Borderzone infarction
Typically these lesions are located in only one hemisphere, either in a deep or peripheral watershed area. In the case on the left the infarctions are in the deep watershed area. - MS
Typical for MS is involvement of corpus callosum, U-fibers, temporal lobes, brainstem, cerebellum and spinal cord.
This pattern of involvement is uncommon in other diseases.
Periventricular lesions must touch the ventricles. Juxtacortical lesions must touch the cortex. Infratentorial lesions are quite common in MS. - ADEM
Multifocal lesions in WM and basal ganglia 10-14 days following infection or vaccination. As in MS, ADEM can involve the spinal cord, U-fibers and corpus callosum and sometimes show enhancement. Different from MS is that the lesions are often large and in a younger age group. The disease is monophasic. - Virchow Robin spaces
Key finding: Bright on T2WI and dark on FLAIR.
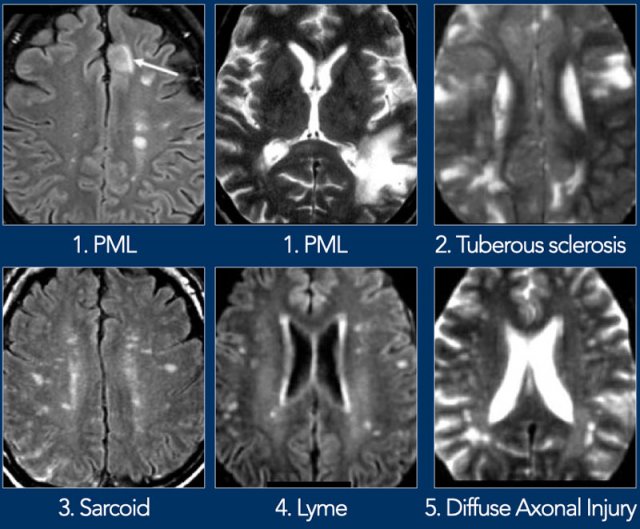
Here some more examples of punctate and patchy white matter lesions.
- PML
Progressive Multifocal Leukoencephalopathy is a demyelinating disease caused by JC virus in immunosuppressed patients.
Key finding: space-occupying, nonenhancing WMLs in the U-fibers (unlike HIV or CMV). PML may be unilateral, but more often it is bilateral and asymmetrical. - Tuberous sclerosis
- Sarcoid
Sarcoid is the great mimicker. The distribution of lesions is quite similar to MS. - Lyme
2-3mm lesions simulating MS in a patient with skin rash and influenza-like illness. Other findings are high signal in spinal cord and enhancement of CN7 (root entry zone). - Diffuse Axonal Injury
Multiple small lesions in the white matter near the cortex as a result of severe traumatic brain injury with rapid deceleration as in high velocity traffic accidents.
Multiple enhancing lesions
Here a collection of images with multiple enhancing lesions in the white matter.
- Borderzone infarction
Peripheral border zone infarctions may enhance in the early phase. - Metastases
Metastases do enhance and are mostly surrounded by edema. - Lyme
- TB
- MS
Enhancement in MS is seen in new lesions and is only present for a couple of weeks. It is an important finding as it is a sign if dissemination in time which is a hallmark in the diagnosis of MS. - ADEM
- Sarcoid
- Lymphoma
- Bacterial encephalitis
Vasculitis
Most diseases with vasculitis are characterized by punctiform enhancement.
Vasculitis in the brain is seen in SLE, PAN, Behcet, syphilis, Wegener, Sjogren and Primary angiitis of CNS
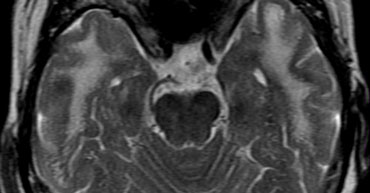
Behcet
Behcet is more commonly seen in Turkish patients.
Typical findings are brainstem lesions with nodular enhancement in the acute phase
Specific diseases with WMLs
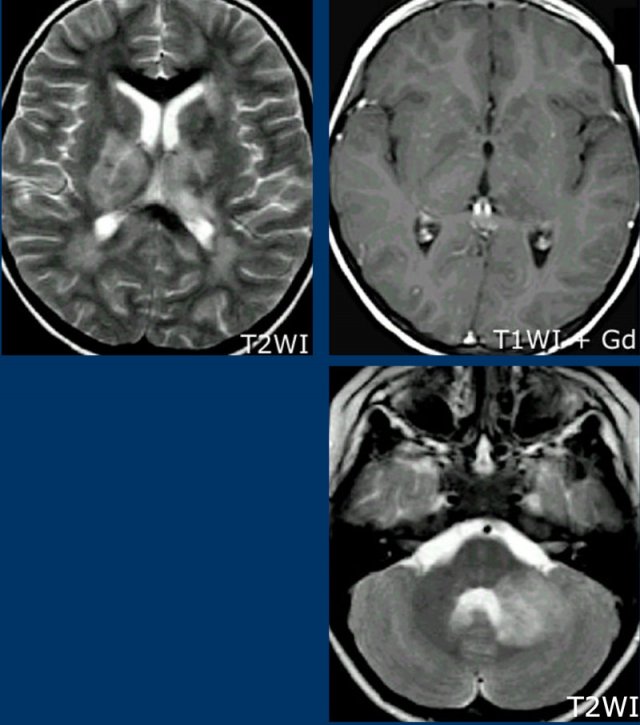
Virchow Robin spaces
Virchow Robin spaces are CSF spaces around penetrating leptomeningeal vessels.
They are typically located in basal ganglia, around atria, near the anterior commissure and in the middle of the brainstem.
On MR they follow the signal intensity of CSF on all sequences.
They are dark on FLAIR and PD unlike other WMLs.
Usually they are small except around the anterior commissure, where perivascular spaces can be larger.
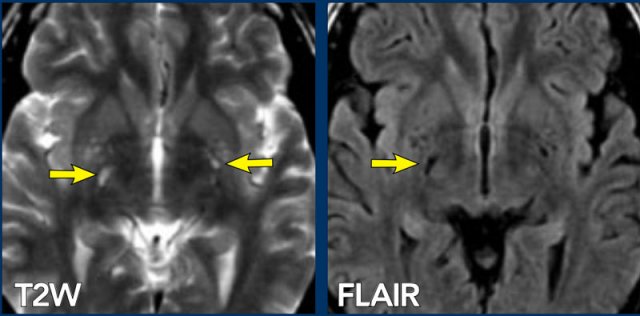
Images
On the T2W image there are some small high intensity lesions in the basal ganglia. On the FLAIR image these lesions are dark, so they follow the intensity of CSF on all sequences. They were hypointense on the T1WI (not shown). This signal intensity in combination with the location is typical for VR spaces.
This case nicely illustrates the difference between VR spaces (white arrowheads: dark on FLAIR) and WMLs (yellow arrows: bright on FLAIR).
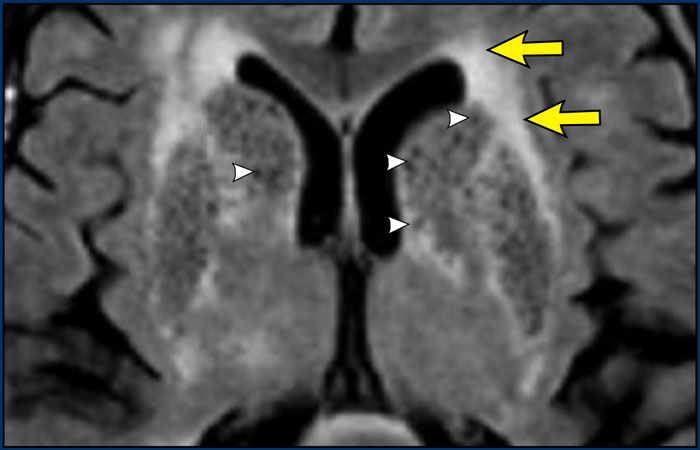
This is an extreme case of wide VR spaces and this condition is known as etat crible.
VR spaces enlarge with age and in patients with hypertension as a result of atrophy of surrounding structures.
Image
There are both very wide VR spaces as well as confluent hyperintense lesions in the WM.
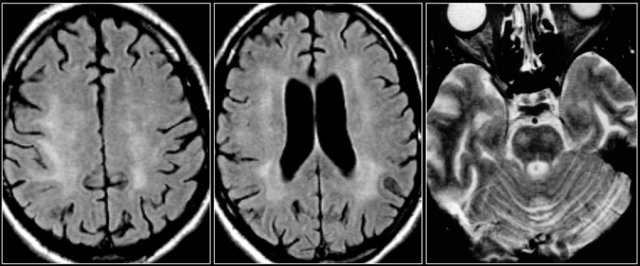
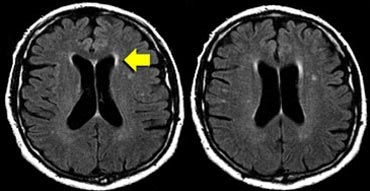 Normal aging: Widening of sulci, periventricular caps (arrow) and bands and some punctate WMLs in the deep white matter.
Normal aging: Widening of sulci, periventricular caps (arrow) and bands and some punctate WMLs in the deep white matter.
Normal Aging
In normal aging common findings are:
- Periventricular caps and bands
- Mild atrophy with widening of sulci and ventricles
- Punctate and sometimes even confluent lesions in the deep white matter (Fazekas I and II).
Periventricular caps are hyperintense regions around the anterior and posterior pole of the lateral ventricles and are associated with myelin pallor and dilated perivascular spaces.
Periventricular bands or 'rims' are thin linear lesions along the body of the lateral ventricles and are associated with subependymal gliosis.
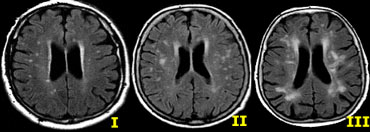
Normal Aging (2)
The clinical significance of white matter changes in aging has not been fully elucidated.
There is a relationship between several cerebrovascular risk factors and the presence of white matter changes.
One of the strongest risk factors however, apart from hypertension, is that of age.
What is still considered normal depends on the age of the patient.
These white matter changes are classified according to Fazekas:
- Mild - punctate WMLs: Fazekas I)
- Moderate - confluent WMLs: Fazekas II - in the deep white matter can be considered normal in aging.
- Severe - extensive confluent WMLs: Fazekas III - always abnormal.
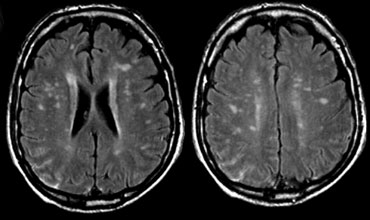
Small Vessel disease
The location of these white matter lesions is in the deep white matter and it is important to notice that these lesions are not directly periventricular, not juxtacortical and not located in the corpus callosum.
Unlike in MS, they do not touch the ventricles or the cortex.
Given the distribution and a priori greater chance of hypoxic-ischemic WM lesions, we must conclude that these WMLs probably have a vascular origin, even in a patient who doesn't smoke, doesn't have hypertension or diabetes and has a normal cholesterol.
Small vessel disease (2)
Ischemic WMLs present as lacunar infarcts, watershed infarcts or diffuse hyperintense lesions within the deep white matter.
Lacunar infarcts are due to arteriolar sclerosis of small penetrating medullary arteries.
Watershed infarctions are the result of atherosclerosis of larger vessels, for instance carotid obstruction or the result of hypoperfusion.
Atherosclerotic brain changes are seen in 50% of patients older than 50 years.
They are found in normotensive patients, but more common in hypertensives.
Image
Widespread WMLs in the deep white matter, but the U-fibers and corpus callosum are not involved.
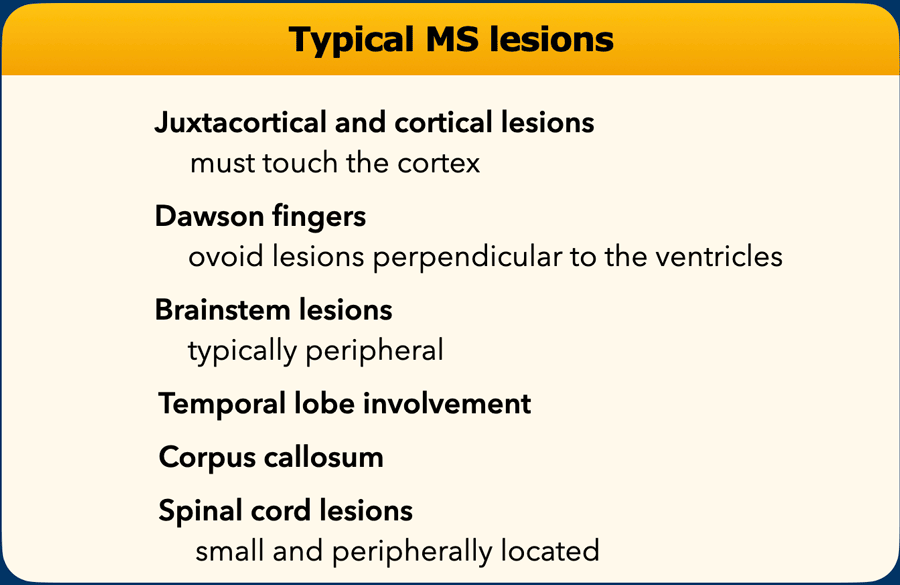
Multiple Sclerosis
Multiple sclerosis (MS) is the most common inflammatory demyelinating disease of the central nervous system in young and middle-age adults, but also may affect older people.
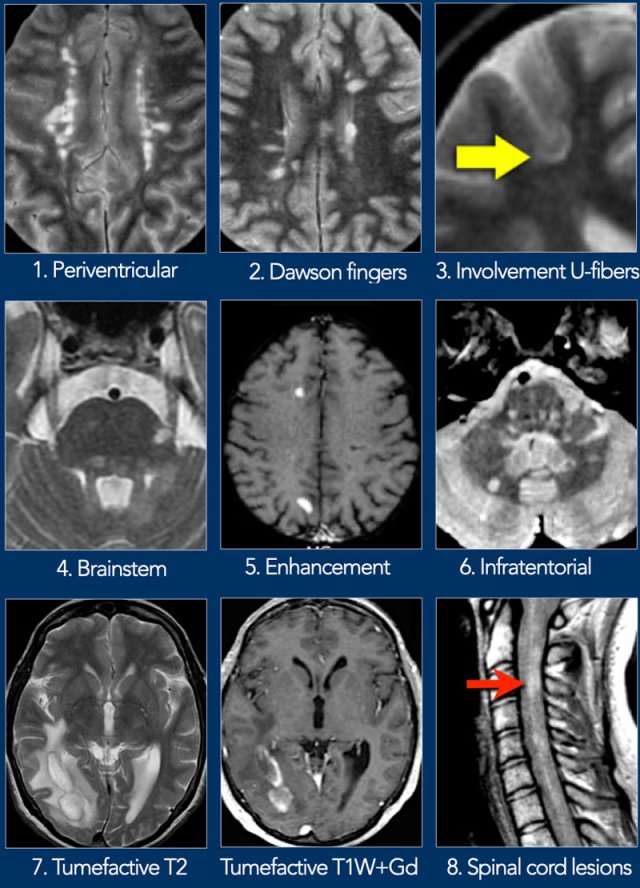
Typical findings are listed in the table.
MS is discussed in more detail here.
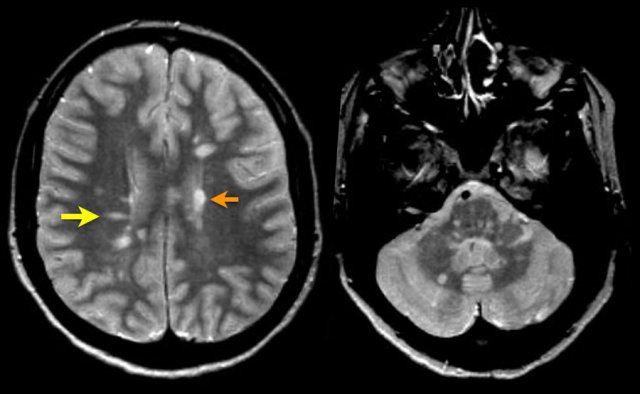
Images
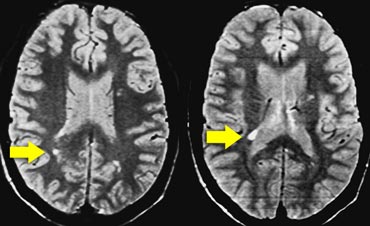
Typical findings for MS as seen in this case are:
- Multiple lesions adjacent to the ventricles (orange arrow).
- Ovoid lesions perpendicular to the ventricles (yellow arrow).
- Multiple infratentorial lesions in brainstem and cerebellum.
These ovoid lesions are also called Dawson fingers.
They represent areas of demyelination along the small cerebral veins that run perpendicular to the ventricles.
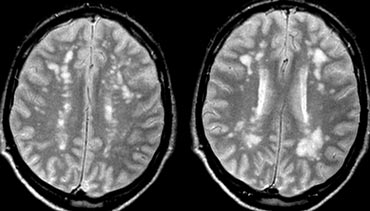
Here more typical examples of MS lesions.
Click image to enlarge.
- Periventricular.
ADEM
Acute Disseminated Encephalomyelitis (ADEM) is a monophasic, autoimmune-mediated white matter
inflammation and subsequent demyelination.
It usually presents 1-3 weeks following exposure to a virus or a vaccine.
ADEM is steroid-responsive, and usually resolves within 1-2 months, although a minority of patients have permanent sequelae.
Many of the patients have MOG antibodies (MOG= Myelin oligodendrocyte glycoprotein).
On MRI there are often diffuse and relatively symmetrical lesions in the supra-and infratentorial white matter which may enhance simultaneously.
There often is preferential involvement of the cortical gray matter and the deep gray matter of the basal ganglia and thalami.
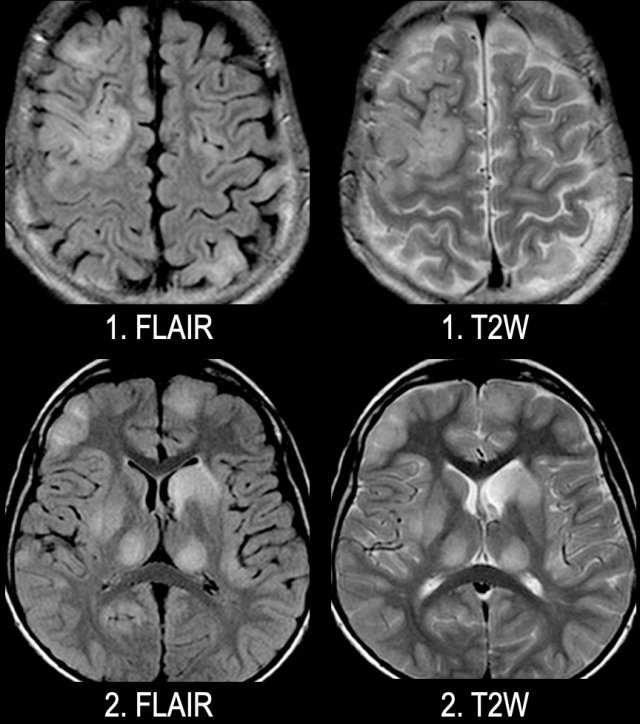
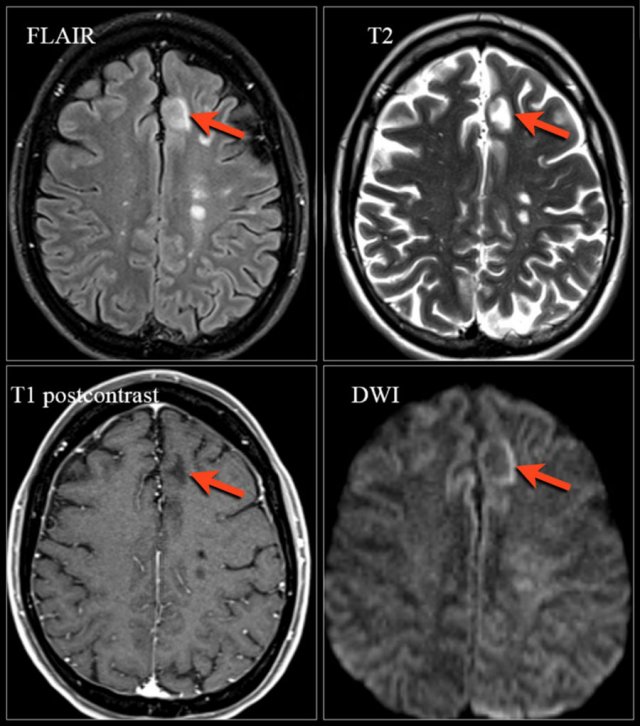
Images
Axial FLAIR and T2W-images of a young patient with ADEM. Notice the extensive involvement of the cortical and gray matter, including the thalamus.
ADEM (2)
Here another case of ADEM.
Notice the involvement of the basal ganglia and the middle cerebral peduncle.
 Natalizumab-associated PML. Images were kindly provided by Bénédicte Quivron CH Jolimont, La Louvière, Belgium
Natalizumab-associated PML. Images were kindly provided by Bénédicte Quivron CH Jolimont, La Louvière, Belgium
PML
Progressive Multifocal Leukoencephalopathy (PML) is a demyelinating disease caused by JC virus in immunosuppressed patients.
PML can also be seen as a relatively rare but serious side effect of immune therapy with Natalizumab in patients with MS.
The diagnosis of PML is based on the clinical presentation, the identification of JCV DNA in the cerebrospinal fluid and imaging findings preferably on MRI.
Sarcoid
The distribution of lesions in Sarcoid is quite similar to MS.
Besides lesions in the deep WM, there are some juxtaventricular lesions and even Dawson finger-like lesions.
The final diagnosis was sarcoid.
Sarcoid has surpassed neurosyphilis as the great mimicker.
Sarcoid (2)
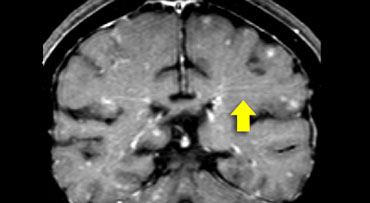
On the left we see the coronal Gd-enhanced T1W images of this patient.
First study these images, than continue.
There is punctate enhancement in the basal nuclei.
This is seen in sarcoid and can also be seen in SLE or other vasculitis.
Typical for sarcoid in this case is the leptomeningeal enhancement (yellow arrow).
This is the result of granulomatous inflammation of the leptomeninges.
Similar findings can be seen in the spinal cord, leading to so-called trident sign on axial post-contrast T1-weighted images
Sarcoid (3)
Another typical finding in this same case is the linear enhancement (yellow arrow).
This is due to inflammation along the Virchow Robin spaces.
This is also a form of leptomeningeal enhancement.
This explains why sarcoid has a similar distribution to MS: the Virchow Robin spaces follow the small penetrating veins, which are involved in MS.
Lyme disease
Lyme disease is caused by a spirochete (borreliaBurgdorferi) that is transmitted by a tick.
It first causes a skin rash.
A few months later the spirochete can infect the CNS and MS-like WMLs are seen.
Clinically Lyme presents with acute CNS symptoms (e.g.cranial nerve palsy) and sometimes transverse myelitis.
Lyme disease (2)
Key finding: 2-3mm lesions simulating MS in a patient with skin rash and influenza-like illness.
Other findings are high signal in spinal cord and enhancement of CN7 (root entry zone).
HIV
HIV encephalitis is a complication of HIV infection, which presents with neurocognitive dysfunction of varying severity.
HIV encephalitis is very uncommon these days due to the administration of antiretroviral therapy
Key finding: Atrophy and symmetric periventricular or more diffuse WMLs in an AIDS patient.
Cadasil
Cadasil is short for cerebral autosomal dominant arteriopathy with subcortical infarcts and leukencephalopathy.
It is an inherited small vessel disease.
Clinical clues: migraine, dementia and family history.
Key finding: subcortical lacunar infarcts with small cystic lesions and leukoencephalopathy in young adults.
Localizations of the WMLs in the anterior temporal pole and external capsule have a high specificity.