Transvaginal Ultrasound for Non-Gynaecological Conditions
including Deep Infiltrating Endometriosis
Julien Puylaert
Amsterdam UMC and Haaglanden MC, The Hague
This is an overview of the use of Transvaginal Ultrasound (TVUS) for the diagnosis of various non-gynaecological conditions as they appear in the pelvic cavity.
This pictorial essay is for gynaecologists who want to look beyond pathology of uterus and ovaries, and diagnose non-gynaecological conditions. Also included here is Deep Infiltrating Endometriosis (DIE). Although the latter is obviously a gynaecological disorder, its diagnosis requires thorough knowledge of TVUS aspect of colon, ileum and bladder.
This pictorial essay is also for radiologists who like to master
the TVUS technique as an adjunct for their transabdominal US examination, diagnosing
both gynaecological and non-gynaecological conditions.
See also ‘US of acute gynaecological conditions'
For critical comments and additional remarks: j.puylaert@gmail.com
Introduction
TVUS is traditionally performed by gynaecologists and obstetric sonographers and their scope is generally focussed on the uterus, ovaries and Fallopian tubes.
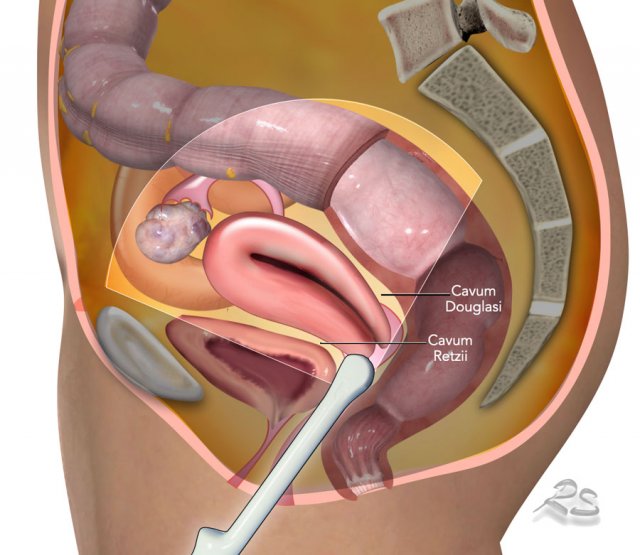
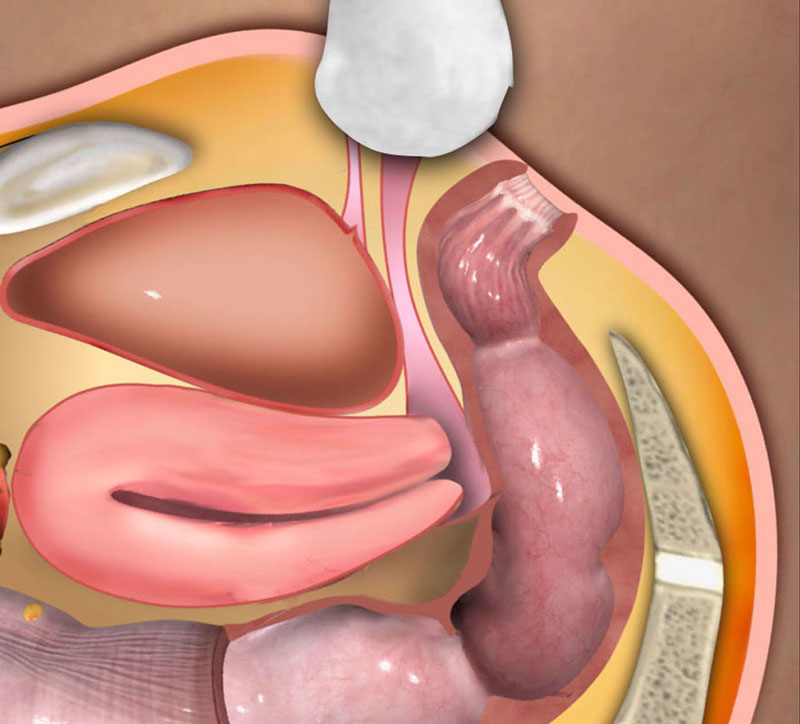
However, there are more organs within the female pelvis
in reach of the transvaginal probe such as the bladder, urethra, distal ureters, sigmoid,
anorectum and the appendix.
Also the virtual spaces of the peritoneal cavity as
cavum Retzii and Douglas pouch can be inspected.
Due to the high mobility of the vaginal top, pathology of these organs and regions can be studied by TVUS with a high frequency probe, resulting in exceptionally detailed images.

Uterus and ovaries are best visualized with a half-full bladder. A very full bladder is unpleasant for the patient, hinders adequate compression and pushes organs away from the ventral abdominal wall, out of reach for transabdominal US.
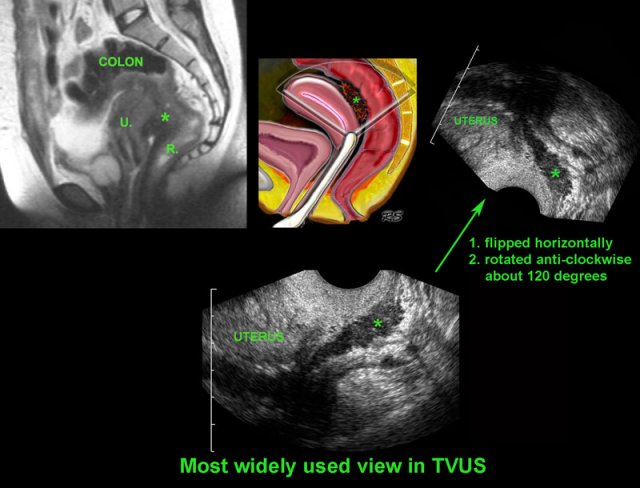
In the sagittal view, uterus, cervix, vagina, anorectum and urethra (u.) can be identified, as well as the collapsed anterior and posterior fornix of the vagina.
Studying the uterus in retroflexion, usually requires more bladder filling.
Sagittal view of the normal uterus with some intravaginal fluid, outlining the portio as well as the anterior (*) and the posterior fornix (*).
It is important to understand also the anatomy outside
the uterus.
A little fluid in Douglas’ pouch and a small Nabothian cyst (n.) may
be easy to identify, but what are the structures marked with a question mark?
Note the full bladder displacing the uterus posteriorly..
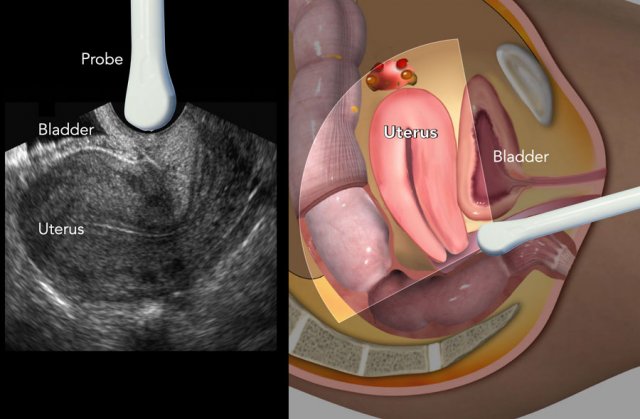
It is important to realize that the orientation of the endovaginal probe is different from that of the abdominal probe. The right panel shows the anteflexed uterus visualized with the endovaginal probe in the anterior fornix of the vagina. This position of the uterus corresponds with the image during transabdominal US.
Most sonographers, however, look at the TVUS image rotated 90 degrees anti-clockwise, as in the right panel.
This is not necessarily a problem, as long as one realizes the different presentation of the anatomy, including gravity effects.
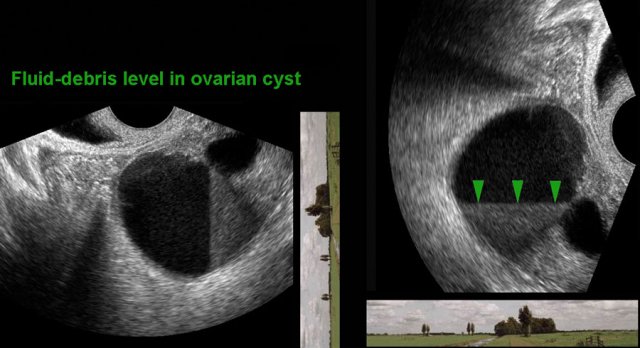
Note the horizon in relation to the TVUS image.
For instance, in this patient with an endometriotic cyst the fluid-debris-level is vertically oriented, and could therefore be misinterpreted.
This could be overcome by clockwise rotating the US image 90 degrees (right image).
However, liberal switching of US image orientation does not favour good pattern recognition. For this reason, it is best to stick to one and the same orientation.
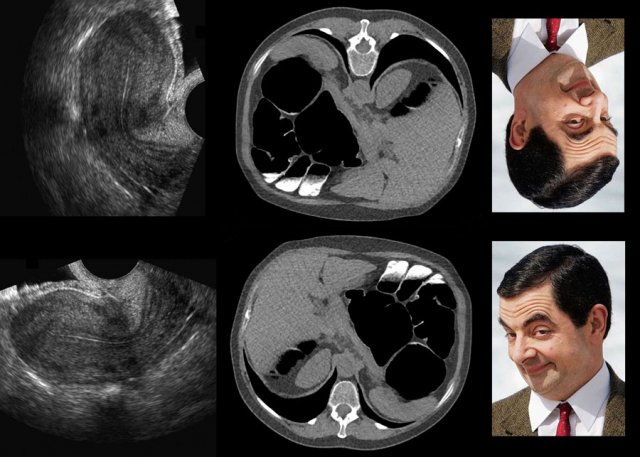
For example, many radiologists reading a CT colonography, made with the patient in prone position, will switch to the familiar CT image in “supine” position, especially when searching for extra-colonic pathology.
Likewise, although the image information of the two Mr. Bean portraits is identical, the comedian is much easier recognized on the picture hanging normal than on the one hanging upside-down.
TVUS for Urological Pathology
Ureteral stones
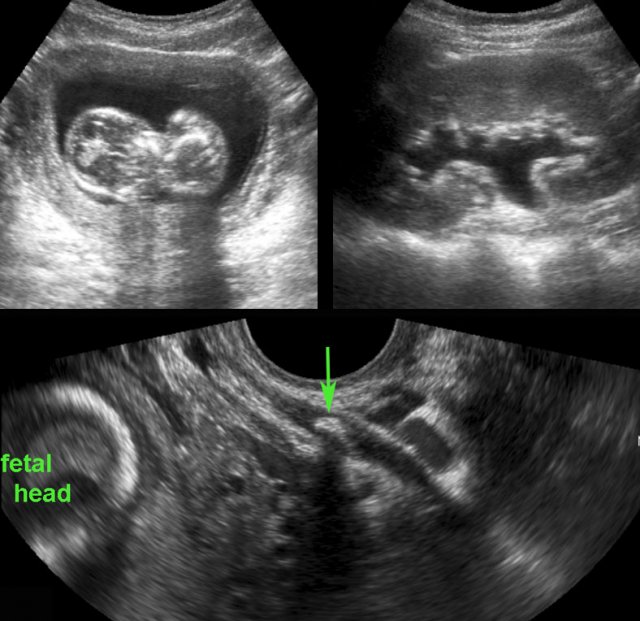
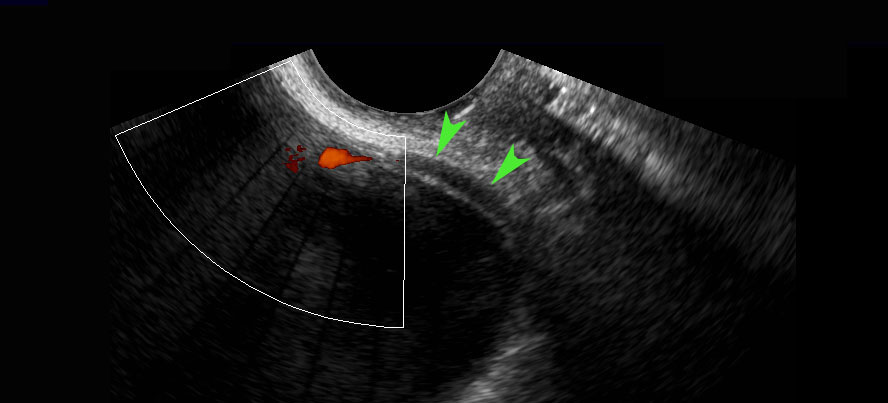
In pregnant patients with suspected ureterolithiasis, CT is contra-indicated. If distal ureteric stones cannot be visualized with transabdominal US, TVUS may be of help.
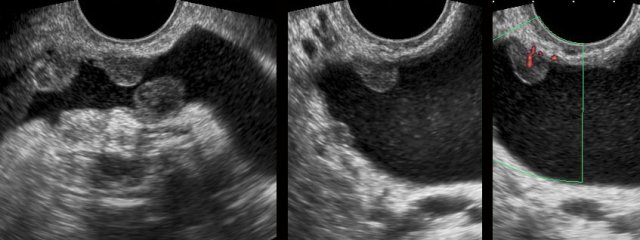
In this woman, the normal distal ureter (arrowheads) was visualized including a ureteric “jet-phenomenon” using Doppler. Note the small distance between vaginal probe and distal ureter.
US confirmed an intact pregnancy and showed a left-sided hydronephrosis.
The bladder was empty and no obstructing stone could be visualized.
Additional TVUS demonstrated a distal stone (arrow) in the left ureter.
A 58 year old woman had a left sided colicky attack, followed by a burning sensation during micturition as well as macroscopic haematuria. She lost some blood clots in the urine, but did not notice any stones. CT showed no stones. The sediment showed atypical urothelial cells.
TVUS showed irregular wall thickening of the distal right ureter (arrowheads). The combination of these findings, raised the possibility of urothelial malignancy.
Seven days later, she was symptom free without any treatment, the urine sediment was normal again and follow up TVUS showed complete normalization of the distal ureter (arrowheads).
The final diagnosis was unnoticed stone passage with confusing secondary effects of transient ureteric wall thickening and of abnormal urothelial cells in the sediment.
Pathology of the urethra, distal vagina and anal sphincter can be studied with the transvaginal probe positioned in the vulva (sagittal plane).
Images
Normal US anatomy with probe in vulvar position
Urethral diverticulum
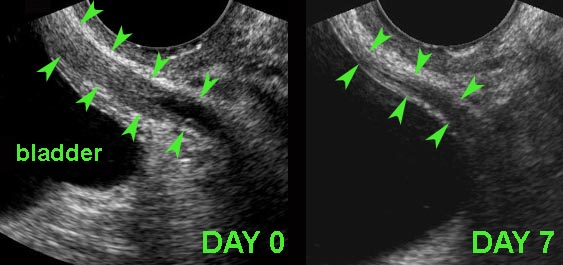
Recurrent lower urinary tract infections may be caused by intermittent obstruction / infection of an urethral diverticulum. In this young woman, TVUS (with the probe in vulvar position) detected a large, inflamed urethral diverticulum (*) right and anterior of the urethra (U.) (V. and S. = vagina and symphysis).
Confirmation by sagittal and coronal MRI.
Bladder carcinoma
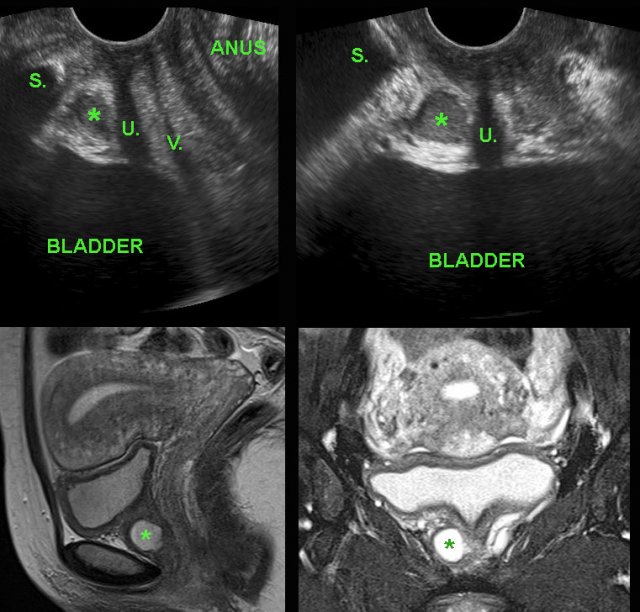
During routine TVUS, the gynaecologist detected a solid, well-vascularized, moderately well-defined mass with a diameter of 2.5 cms, arising from the bladder wall.
There was no history of hematuria or micturition problems.
Cystoscopic surgery revealed a grade 1 transitional cell carcinoma.
TVUS for Intestinal Pathology
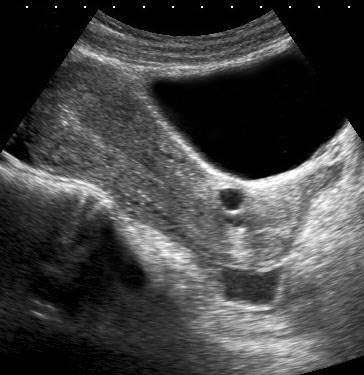
Normal colon: TVUS anatomy
TVUS anatomy of the normal and well-compressible sigmoid in longitudinal and axial view.
At the end, in the transverse view, the sigmoid is easily compressed with the probe (arrowheads) against the sacrum.
Diverticulitis
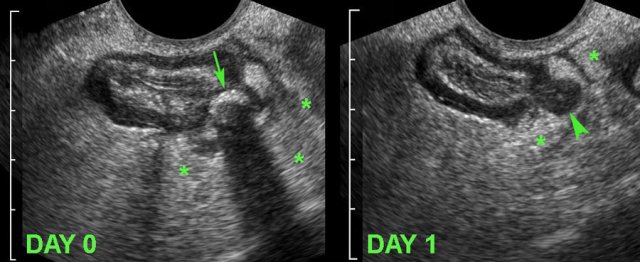
A 34-year old woman, presented with acute LLQ pain.
TVUS demonstrated local wall thickening of the sigmoid and a diverticulum harbouring a fecolith (arrow), which was surrounded by inflamed fat (*), representing mesentery and omentum, effectively walling-off the imminent perforation.
The next day, she felt much better and follow up TVUS showed
a hypoechoic, oedematously thickened, empty diverticulum (arrowhead).
The fecolith
apparently did evacuate to the sigmoid lumen.
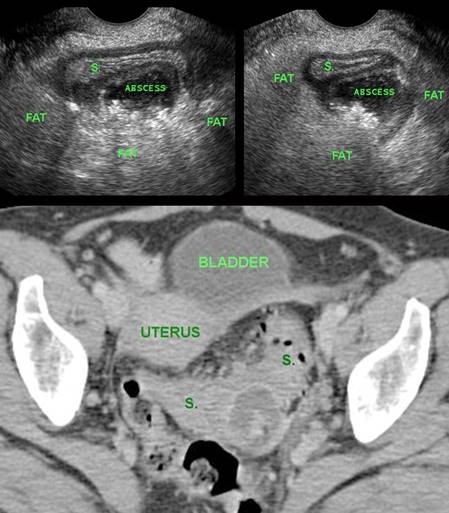
A 37-year old woman, clinically suspected of a tubo-ovarian abscess, underwent TVUS.
The gynaecologist consulted the radiologist, who recognized it as small paracolic abscess, probably of diverticular origin.
Subsequently proven by CT scan (S. = sigmoid).
Sigmoid carcinoma
A 66-year old woman presented with progressive bloating and constipation. CT showed massive colonic dilatation, but pelvic CT (not shown here) was of low quality due to two hip prostheses.
US confirmed multiple, strongly dilated, air-filled large bowel loops, but was otherwise non-diagnostic.
TVUS demonstrated a small, stenosing sigmoid carcinoma with concomitant desmoid reaction (*) in the surrounding fat.
Adenomatous polyp
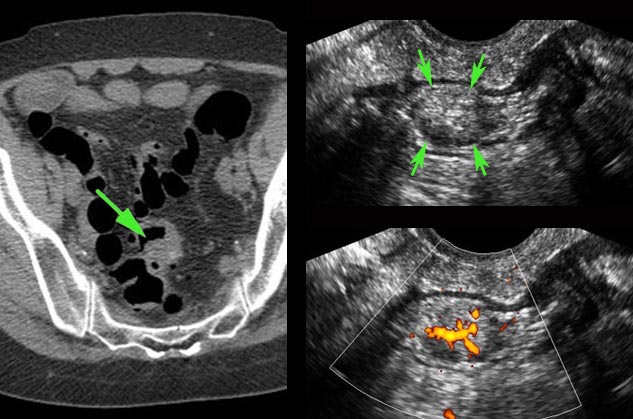
A colonic polyp (arrow) was seen both on CT and at
colonoscopy, however due to adhesion-related kinking, the polyp was out of
reach for biopsy.
Surgeons wanted more proof before proceeding to laparoscopic
resection.
TVUS showed an ovoid, solid, well-defined, inhomogeneous,
hypervascular, intraluminal mass (arrows) with a diameter of 1.5 cm.
Segment
resection was done, histology showed a malignant adenomatous polyp.
Rectal cancer
A 39-year old woman with known ulcerative colitis for 20 years, presents with blood in the stool.
TVUS confirms thickening of the hyperechoic submucosa (arrowheads) compatible with longstanding inactive colitis.
Also a hypoechoic carcinoma (CA) in the ventral rectal wall is detected. Note the focal obliteration of the layer structure and the desmoplastic reaction at the serosal side (*).
Appendicitis
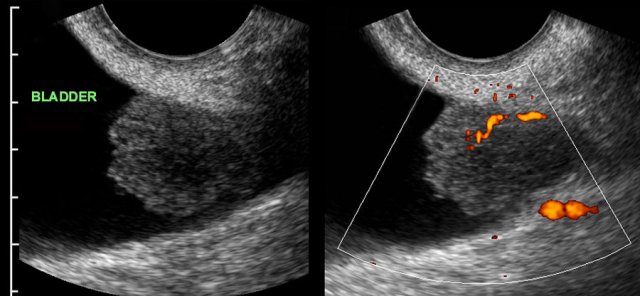
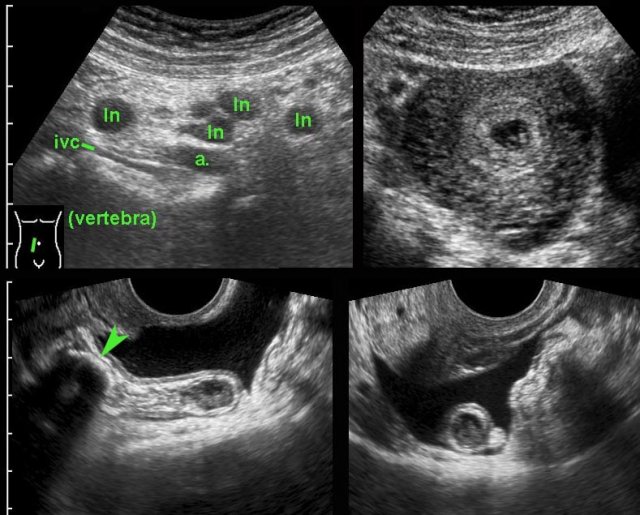
A young, early pregnant woman presented with acute deep pelvic pain.
US demonstrated enlarged mesenteric lymph nodes (ln) and
an intact intra-uterine pregnancy.
The appendix was not visualized. (ivc =
inferior vena cava, a = iliac artery).
TVUS easily demonstrated a 12-mm, inflamed appendix harbouring
a large fecolith (arrowhead).
The appendix was in pelvic position and surrounded
by free fluid.
There was no perforation
at surgery.
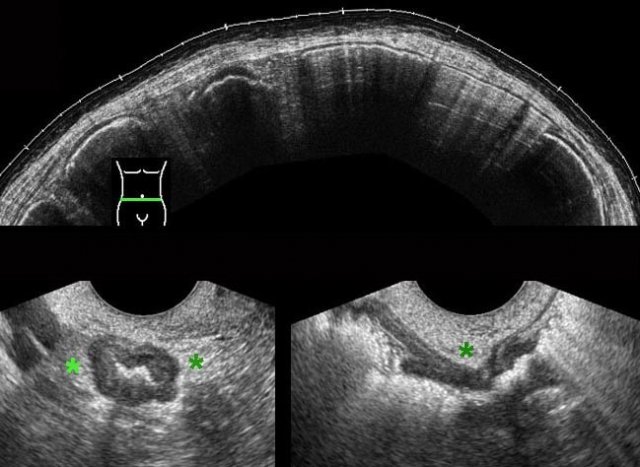
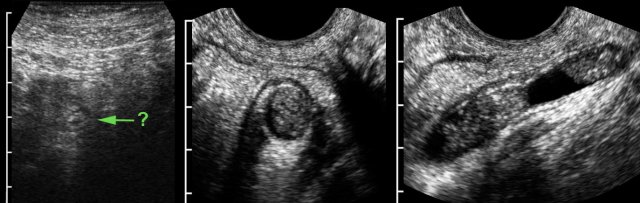
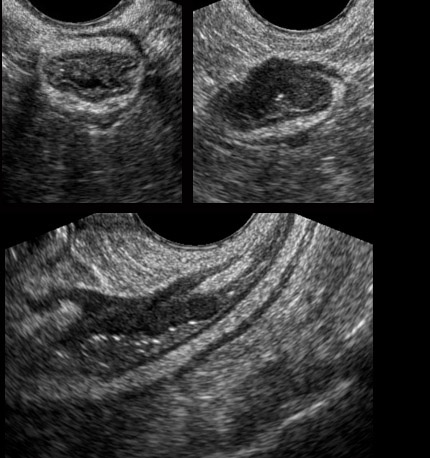
In this obese, 3 weeks pregnant woman, transabdominal US visualized an dubiously abnormal appendix (← ?).
TVUS showed a dilated, pus filled, inflamed appendix in deep pelvic location.
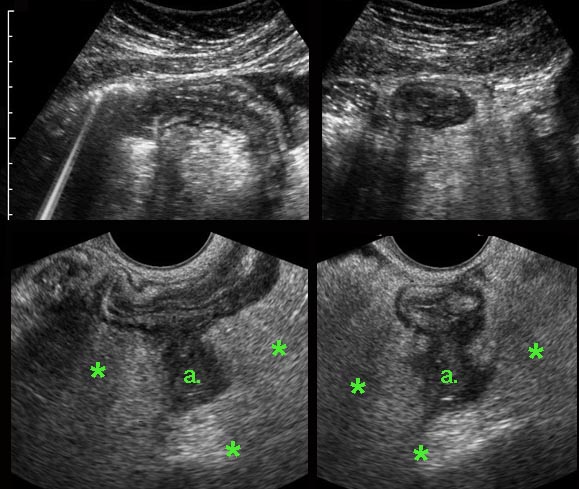
Crohn’s disease
A young, 4 weeks pregnant woman presented with 6 days of RLQ pain and a CRP of 120.
US demonstrated wall thickening of the terminal ileum with echolucent changes in the submucosa, suspect for Crohn’s disease.
Complementary TVUS detected an abscess (a.) walled-off by mesenterial and omental fat (*).
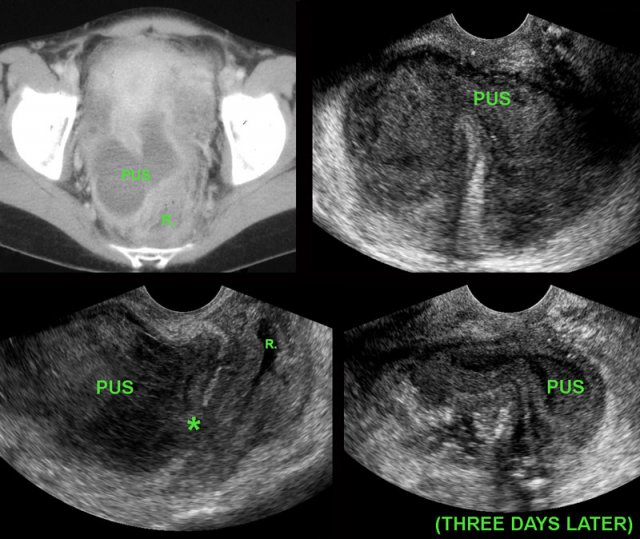
Deep pelvic abscess
Young woman with abdominal pain and fever 10 days after surgery for perforated appendicitis.
CT shows a bilobar puscollection, close to the thick-walled, empty rectum (R.).
TVUS confirms the abscess, and demonstrates an echolucent
tract (*) from the abscess towards the rectal lumen (R.) with focal blurring of the layer structure of
the oedematous rectal wall.
These TVUS findings, in combination with the improving
symptoms of the patient, are signs of impending spontaneous evacuation.
Three days later the thick-walled abscess is almost
empty.
The patient recovered without surgical or radiological drainage.
Malignant peritonitis
Elderly lady with malaise, weightloss and at transabdominal US only some ascites.
TVUS demonstrates slightly hyperechoic ascites and multiple, vascularized tumour deposits on the peritoneum, strongly suspect for malignant peritonitis.
TVUS for Deep Infiltrating Endometriosis
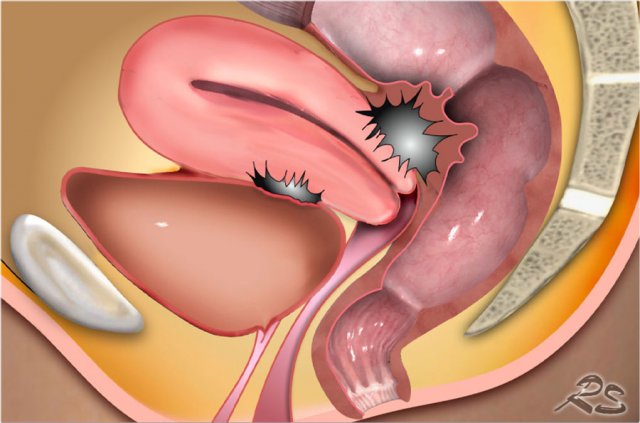
DIE is a potentially devastating, gynaecological
condition.
By repeated episodes of bleeding, resorption and the resulting formation
of scar tissue, the endometriotic implants may cause pain, dyspareunia and subfertility.
DIE, if localized in Douglas pouch and the vesico-uterine recess, may aggressively invade the rectum, bladder and ureters, with all its sequelae, as colonic obstruction, micturition problems and hydronephrosis.
In prominent, longstanding DIE, the resulting bulky scar tissue of DIE (*), may cause narrowing, and eventually total obstruction, of the colonic lumen.
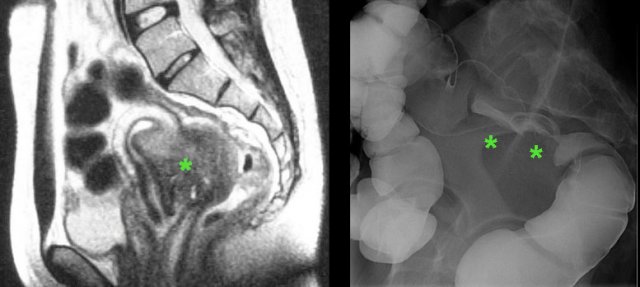
In this young lady with unexplained chronic abdominal symptoms for many years, CT and subsequent MRI demonstrated extensive endometriosis.
In addition there are large, adhesive endometriotic cysts (“kissing ovaries”), bilateral hydronephrosis and complete obstruction of the colon, due to ingrowth of endometriosis in the ureters and the rectum.
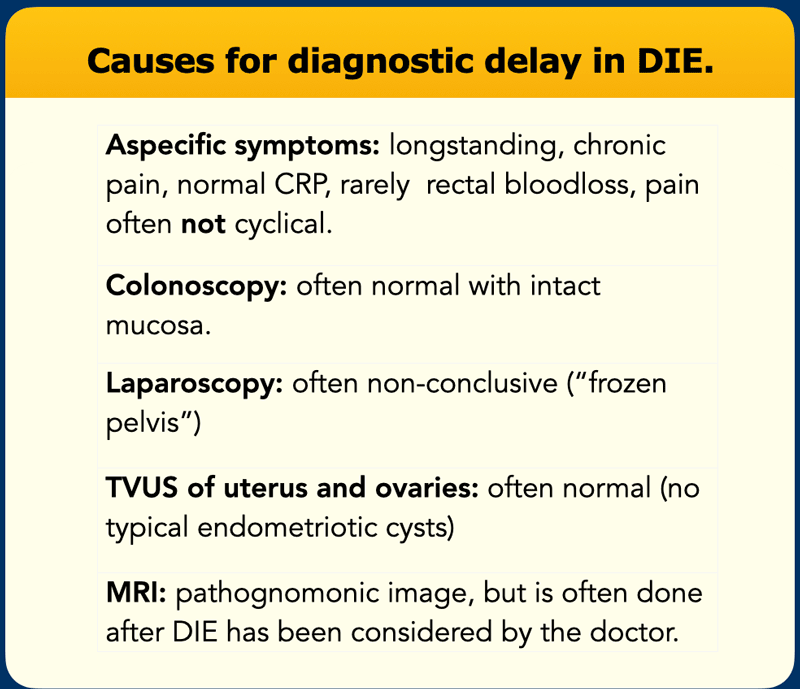
Background
There are many reasons for diagnostic delay in
DIE.
The symptoms of DIE are chronic, atypical and often non-cyclical.
Gynaecological
TVUS often shows a normal uterus and normal ovaries.
The lab findings are usually
normal and colonoscopy in DIE is often inconclusive
Even laparoscopy can be non-diagnostic because DIE may hide under adhesions.
MRI of DIE (*) yields pathognomonic images, but is only performed when there is clinical suspicion of endometriosis.
TVUS provides a unique opportunity to make the diagnosis of DIE in patients who undergo routine examination for aspecific symptoms.
DIE of the rectum
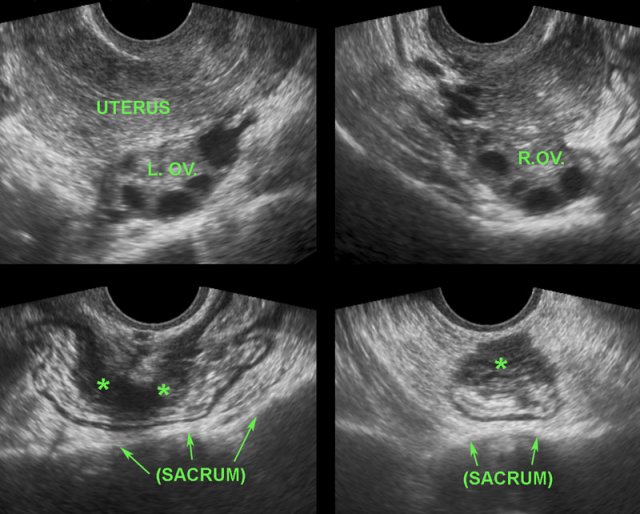
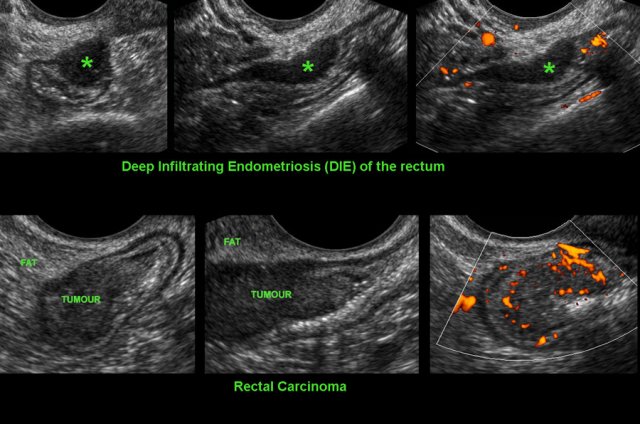
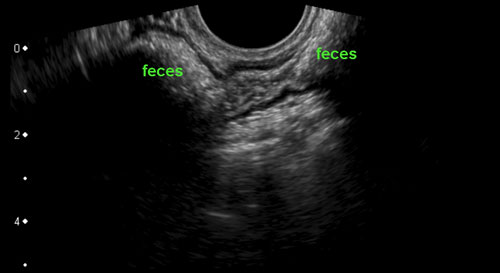
The images are of a patient with DIE and a normal aspect of uterus and ovaries.
DIE has typical, almost pathognomonic TVUS features.
Although
obviously a gynaecological condition, it is not infrequently overlooked by
gynaecologists during TVUS.
The reason is that the majority of patients with DIE (*), lack the typical endometriotic cysts and have, as in the patient here, a normal uterus and ovaries (L. OV. and R. OV.). Furthermore, the TVUS diagnosis of DIE requires thorough knowledge of the US image of normal and pathological bowel and bladder, which knowledge may be absent in gynaecologists.
(See also: “US of the GI tract: normal anatomy”)
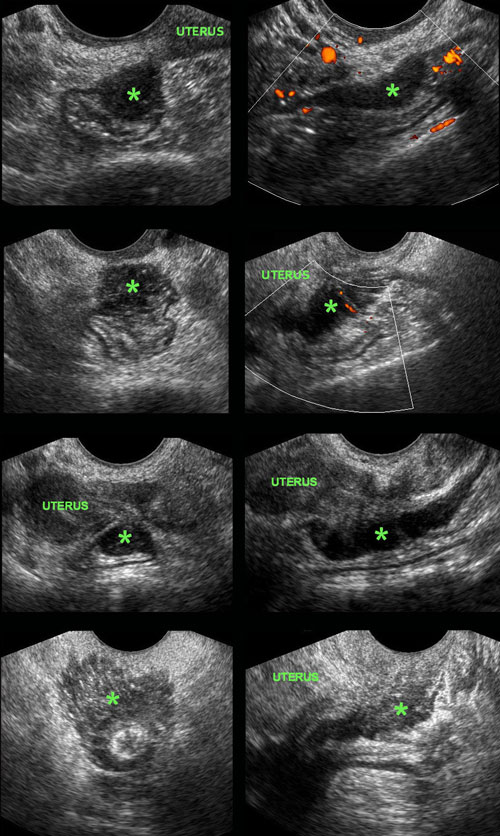
DIE implants on the outer surface of the colon in four different patients.
DIE implants (*) in Douglas pouch, are asymmetrically localized, solid, hypoechoic, poorly vascularized masses, which are continuous with the outer hypoechoic muscularis layer of the colon.
The overlying hyperechoic submucosa, and also the colonic mucosa are generally intact. This explains also why blood in the stool is quite rare in DIE.
The outer contour of these hypoechoic masses is mostly firmly adherent to uterus and/or cervix. Often there is spiculation or “tethering” visible on the outer margins.
Adherence to the uterus and cervix can be demonstrated by gently pushing with the probe to-and-fro.
Whereas the normal sigmoid and rectum can easily be pushed away from the uterus with the probe (“sliding phenomenon”), the adhesions (arrow) belonging to DIE (*) block the entrance of the probe into the posterior fornix.
In this videoclip, the transvaginal probe is gently moved to-and-fro.
The implant (*) has developed firm adhesions between uterus and colon, which prevent entering of the probe deeper in the direction of the sacrum.
In the normal situation, uterus and colon can be easily be pushed aside.
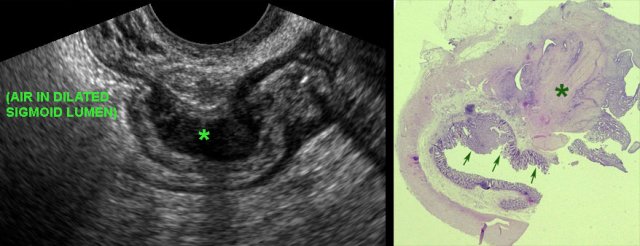
TVUS image of DIE with operative specimen.
In this patient, the hyperechoic submucosa of the ventral sigmoid wall, clearly overlies the large DIE implant (*). Note also the completely normal dorsal sigmoid wall.
The resected specimen shows that the (sub)mucosa (arrows) is intact and overlies the DIE (*). As expected, also this patient had no history of rectal bloodloss.
For a proper understanding of the TVUS image of DIE and especially the correlation with the MRI images, it is important to realize the different orientations used in both image modalities.
In the upper three rows, the “MRI-orientation” prevails, and the upper-right TVUS image is therefore is 1. flipped horizontally (mirror view) and 2. rotated anti-clockwise about 120 degrees.
Although one might argue that this flipped and rotated image corresponds better to the sagittal MRI, pattern recognition benefits from using the “classic” TVUS view, as shown in the bottom image.
Differentiating DIE from carcinoma
Differentiating rectal cancer from DIE of the rectum.
Both conditions appear as solid, moderately defined, rather hypoechoic, asymmetrically localized masses arising from the rectum with a tendency to narrow the lumen. TVUS may be key to discriminate the two.
In DIE the hypoechoic mass is hypovascular, it is localized at the outer contour of the rectum and is continuous with the hypoechoic muscularis. The submucosa and mucosa of the colon are intact.
In rectal CA, the hypoechoic mass is hypervascular and the mass originates from the mucosa, with focal loss of layer structure as a consequence of transmural tumour growth.
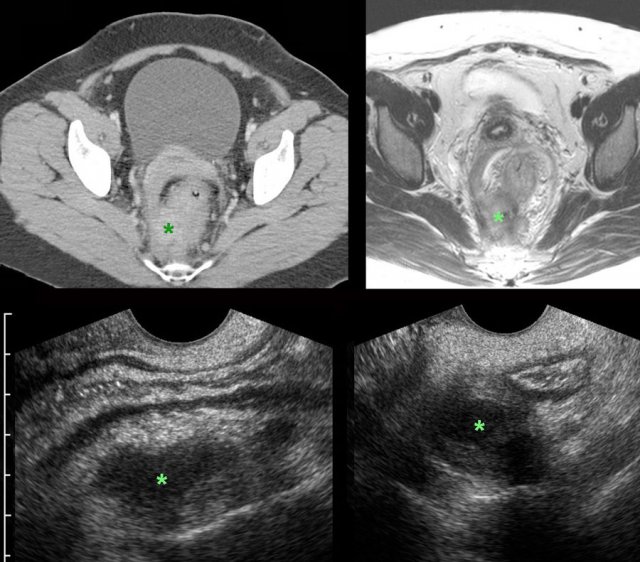
Differentiating DIE from actinomycosis
A 43-year old woman with longstanding lower pelvic pain. During routine US (not shown here) an ill-understood asymmetrical rectal wall thickening with inflammation of the surrounding fat was found. A CT was advised.
Images
CT and subsequent MRI confirmed the US findings and also
showed extension of the abnormalities to the pararectal fascia and cervix.
Within the mass (*) small areas of necrosis or fluid were seen.
CRP was 2.
TVUS showed oedematous. thickening of an otherwise
normal rectum, and an atypical hypoechoic mass (*) right posteriorly,
surrounded by hyperechoic, non-compressible fat.
The mass felt very hard at toucher.
An atypical form of DIE was suggested.
Eventually, deep EUS guided colonoscopic biopsies showed a fibrosing, low-grade infection, and no features of endometriosis or malignancy. The diagnosis of actinomycosis was suggested. After six months of intravenous penicillin (port-a-cath), only minimal residual abnormalities remained. The patient was pain free. Fifteen years earlier an IUD had been removed. The low CRP was compatible with longstanding, low grade infection. No bacteriological proof was obtained.
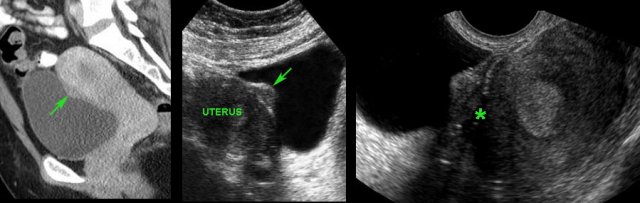
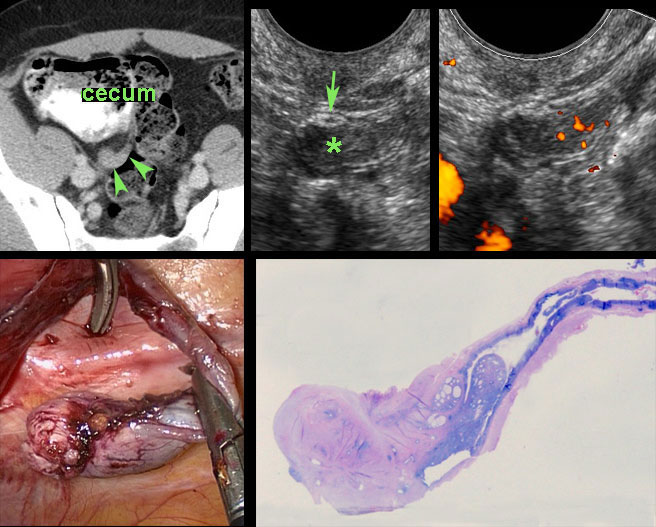
Bladder endometriosis
Coincidental finding of “bladder polyp” (arrow) on CT scan in young female.
Confirmation of a flat polypoid structure (arrow) by abdominal US.
Cystoscopy was completely normal, indicating that the mass is covered by normal bladder mucosa..
TVUS demonstrates
that the mass in fact is an endometriotic implant and shows blurring of the
hyperechoic contour (*) of the uterus, indicating local ingrowth.
TVUS also
demonstrated DIE in Douglas pouch (not shown here).
A 45-year old woman with a long history of painful micturition. Cystoscopy was negative.
CT shows a plaque-like, irregularly defined mass (arrow).
TVUS confirms a large endometriotic implant (arrow) in the prevesical space (cavum Retzii). Note again the ill-defined border with the uterus.

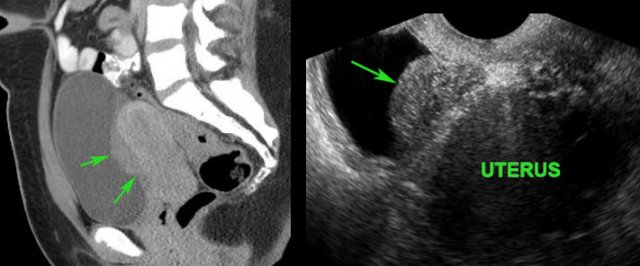
Ileum endometriosis
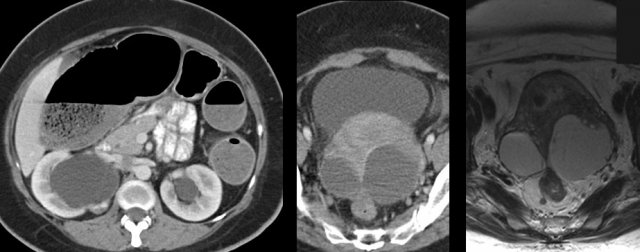
A 32-year old woman with a long history of chronic abdominal pain.
US revealed a poorly vascularized hypoechoic mass between ileum and cecum (DIE). The mass was continuous with the muscularis, and spared the (sub)mucosa of ileum and cecum. Although there was no local pain on pressure, an endometriotic implant was suggested.
Subsequent MRI revealed extensive DIE affecting not only the ileocecal region, but also Douglas pouch and the cavum Retzii.
A 34-year old woman with known extensive pelvic DIE, presented with subacute pain in the RLQ.
A large polylobular mass was found on CT.
The corresponding abdominal US confirmed the mass to be multiple coalescent DIE implants, leaving the hyperechoic submucosa of the ileum intact.
(a and v = iliac artery and vein)
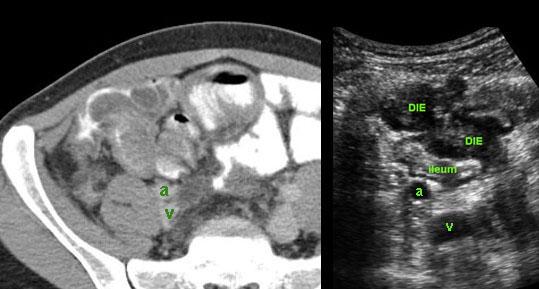
Appendix endometriosis
Enlarged, hyperattenuating tip of the appendix on CT scan in 43-year old woman, with previous extirpation of uterus and adnexa for DIE.
TVUS revealed a solid, moderately vascularized, extrinsic mass (*) in close contact with a thin appendix (arrow), suspect for endometriosis. However malignancy could not be excluded.
Appendectomy revealed a longitudinally oriented endometriotic implant on the appendix tip.
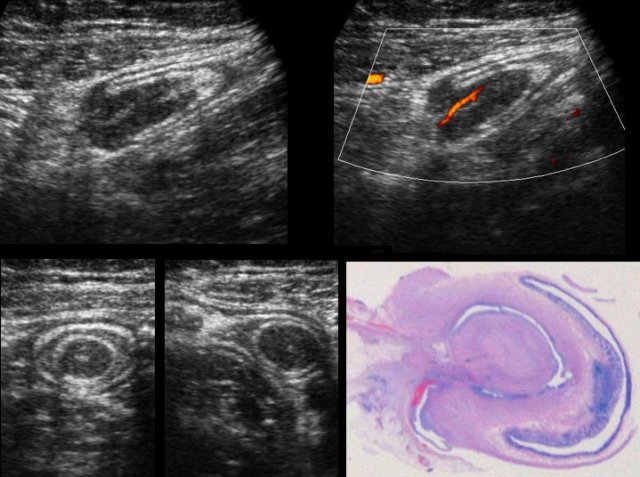
A 26-year old woman presents with recurrent subacute pain RLQ. US shows an -at that time ill-understood- intussusception containing a small, solid, vascularized mass, in the region of the cecum. Malignancy was suggested.
At surgery a “tumour mass” was found originating from the cecal pole, where the appendix was expected. This mass could be stapled-off safely, and turned out to be the appendix, intussuscepted into the cecum due to extensive endometriosis.
Epilogue
The author thanks his fellow radiologists for their valuable help in collecting all the educational material. A special thanks to gynaecologist Jan Lind, for his advice in editing the manuscript.
Finally, for all those interested in DIE, I strongly recommend the excellent youtube-lecture of gynaecologist Sofie Piessens from Melbourne.