Large airway disease
Onno Mets and Hans Daniels
Radiology and Pulmonology department University Medical Center Amsterdam
Publicationdate
Pathology of the
trachea and central bronchi is infrequently encountered, and therefore most
radiologists find it challenging.
Although there is a relatively limited differential diagnosis, pathology
nevertheless varies between congenital, benign, primary malignant and
metastatic disease.
This article summarizes the typical imaging features of the differential diagnostic considerations of large airway diseases and hopefully serves as a reference for those that need it every now and then.
Introduction
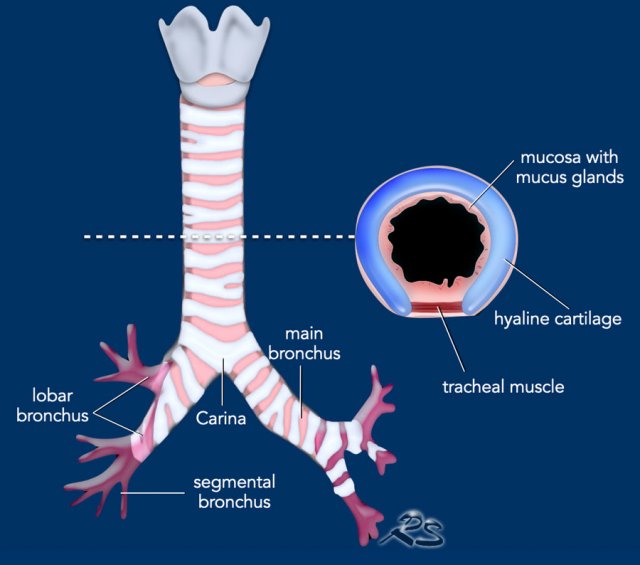
The central airways consist of the
trachea and main bronchi, before the airways branch towards the periphery into
the lobar, segmental and subsegmental airways on both sides.
The trachea has a length of about 10-15 cm and has an extrathoracic and
intrathoracic component. It contains about 15-20 horseshoe shaped cartilaginous
rings.
The posterior wall of the trachea and main bronchi is membranous and
does not contain cartilage, which is important for the imaging differential
diagnosis, as will be discussed later.
The inner lining of the airways consists
of respiratory ciliated epithelium interspersed with goblet cells, minor
salivary glands and neuro-endocrine cells.
Furthermore, the airways contain
muscle tissue, cartilage, nerves, etc.
All of which may give rise to pathology.
Differential diagnosis
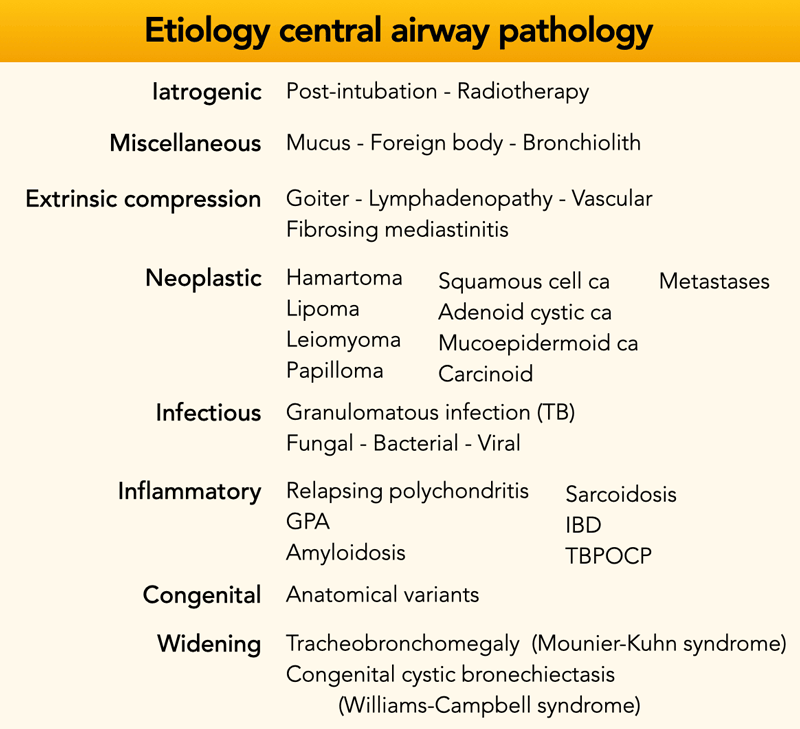
Central airway pathology can be divided into subgroups, either by etiology (ie. inflammatory, neoplastic, etc.) or by imaging appearance (ie. nodular, single/multifocal, diffuse infiltration, etc.).
In the table an overview based on disease etiology subgroups to provide a comprehensive overview.
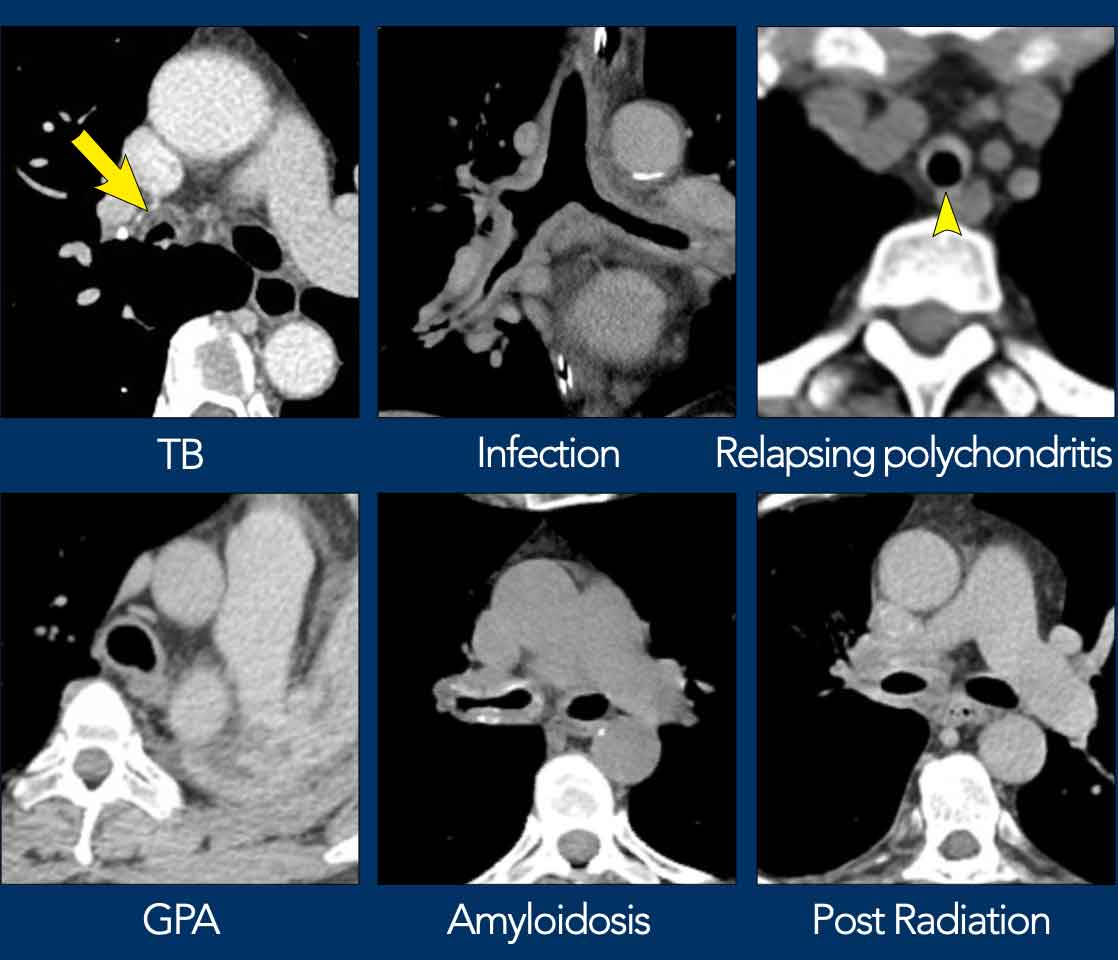
- TB = tuberculosis
- GPA = granulomatosis with polyangiitis
- IBD = inflammatory bowel disease
- TBP-OCP = tracheobronchopathia osteochondroplastica
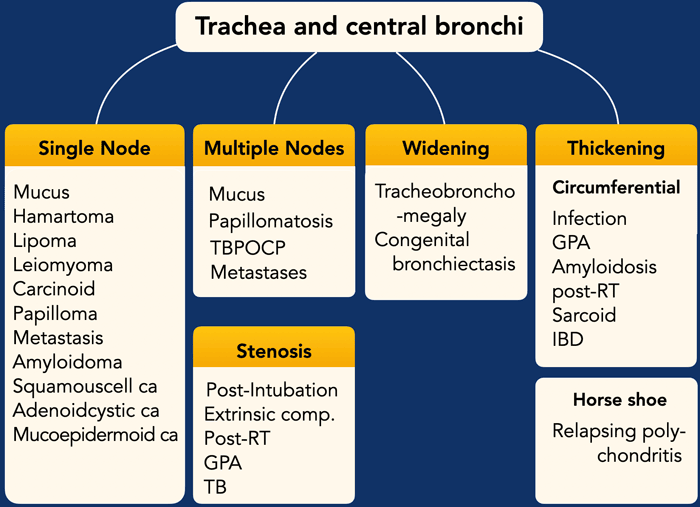
This is a flow-chart that is based on imaging appearances, which can be used to narrow down the differential diagnosis.
Nodular - differential
Nodular
lesions protrude into the lumen and distort the smooth inner contour of the
airway.
Only a minority of these lesions will have specific morphologic
features.
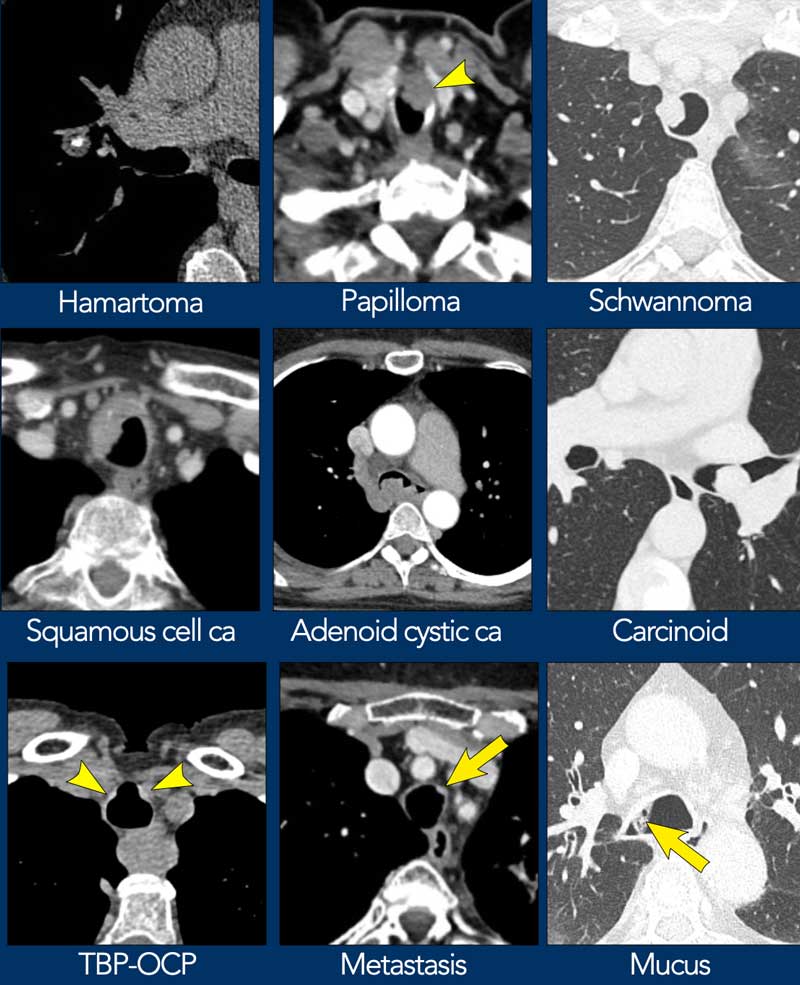
Here some examples of nodular or mass lesions in the trachea and
bronchi.
- Squamous cell carcinoma usually has a destructive pattern with invasion of surrounding structures.
- Carcinoid is a well circumscribed endobronchial lesion, that rarely involves the trachea.
- Macroscopic fat may be seen in either hamartoma or lipoma.
- Mucus has low density and is usually only seen in lung window settings.
Wall thickening - differential
At the site
of involvement there is loss of the normal smooth and thin contour of the
tracheal and bronchial wall.
Only a few diseases have specific morphologic
features.
Here some examples of both focal and diffuse central airway wall
thickening.
- Relapsing polychondritis has a characteristic horseshoe shaped appearance.
- Amyloidosis shows a strikingly irregular pattern with calcification, virtually pathognomonic.
- Radiotherapy effect is limited to the radiation field.
Iatrogenic
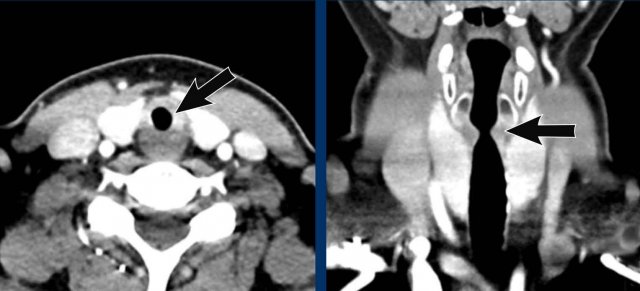
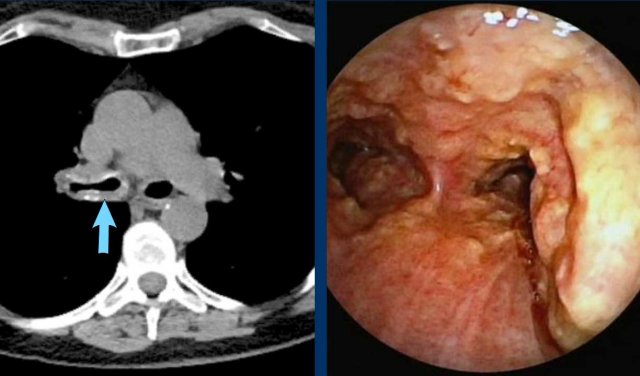
Post-intubation
The most common iatrogenic central airway pathology is focal stenosis after endotracheal intubation or tracheostomy. Focal fibrosis may occur in reaction to necrosis caused by cuff pressure or due to direct iatrogenic damage of the tracheal wall.
Typically, a subglottic stenosis near the thoracic inlet is seen with an hourglass shape in the coronal plane, due to a short segment of focal scarring in the trachea (figure).
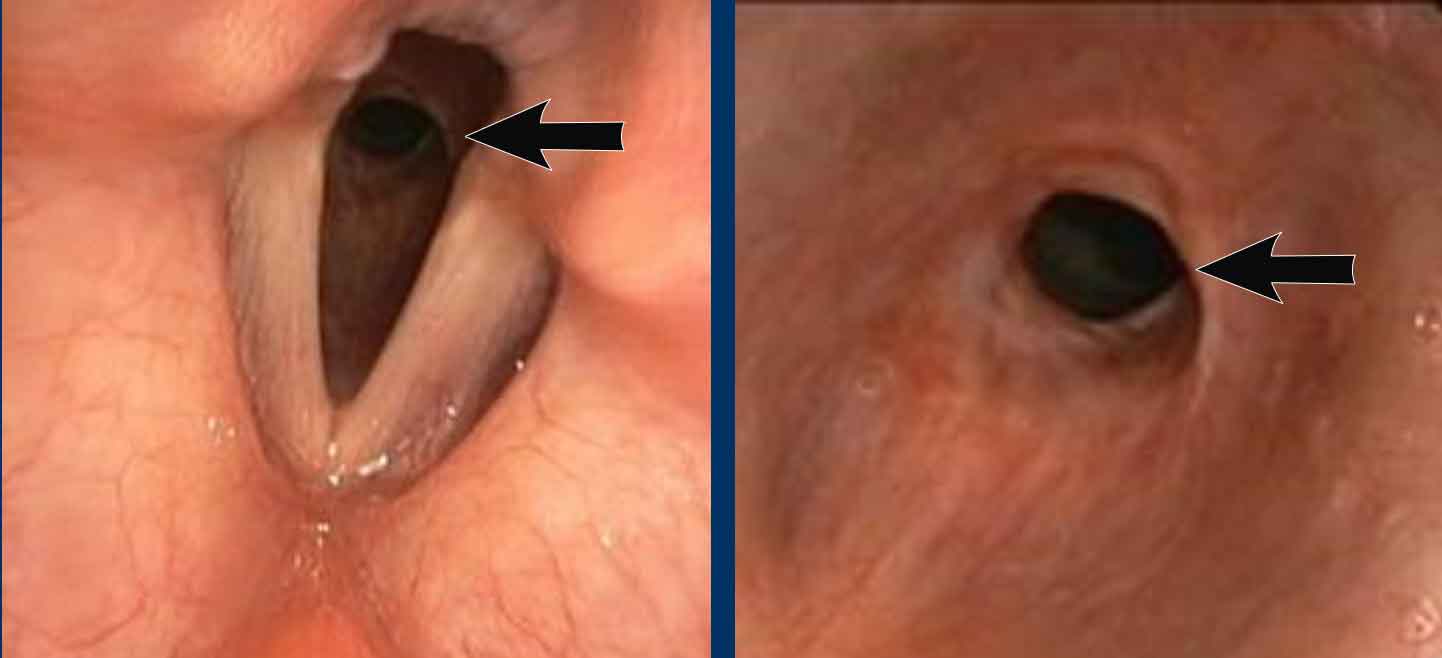
Bronchoscopy images from above and below the level of the vocal cords, show a significant subglottic narrowing of the trachea.
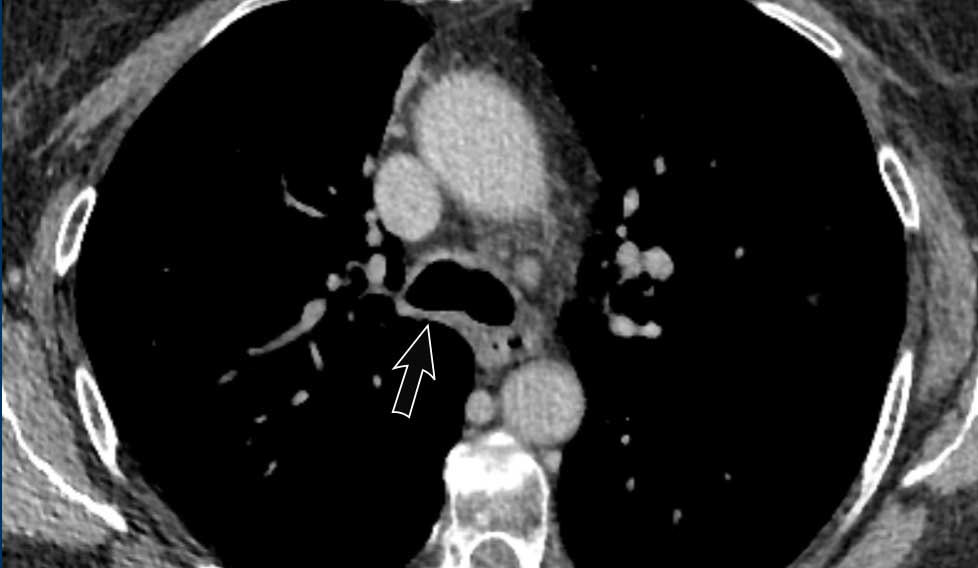
Radiotherapy
When applied to tumors in proximity to
the central airways radiotherapy can cause airway narrowing, fistula, necrosis and sometimes massive hemoptysis.
In addition mediastinal fatty
infiltration and esophageal wall thickening may be present in the acute phase.
Image
Wall thickening of the trachea bifurcation post-radiotherapy.
Foreign body
Aspiration of a foreign body is rare in adults, and most often encountered in children.
Among adults aspiration of dental parts is relatively common, especially in the trauma population. Conventional imaging after aspiration may not show a radiopaque foreign body, depending on material composition.
Indirect signs might be present though, for example unilateral hyperinflation or lung atelectasis due to check valve mechanism and obstruction, respectively.
Image
Aspiration of device during dental surgery, visible in the right lower lobe bronchus.
Bronchiolith
Endobronchial calcification which may be caused by
calcification of aspirated foreign material, or migration or erosion and
extrusion of adjacent calcified material from for example a lymph node or
ossified bronchial cartilage.
Mucus
The most encountered focal abnormality in the trachea is mucus.
In large quantities it can cause bronchial obstruction and atelectasis, especially in the ICU setting.
In most cases it represents an irrelevant finding, but small quantities sticking to the airway wall may create a diagnostic dilemma.
In general mucus may show an associated mucus thread and is often not dense enough to be seen on the soft tissue reconstruction windows.
When in doubt whether focal airway wall pathology is present, follow-up imaging or bronchoscopy might be considered.
Mucus will resolve or change position on follow-up CT imaging, whereas a solid lesion persists.
Extrinsic compression
Enlarged goiter
Intrinsic versus extrinsic pathology is one of the first differentiations that has to be made when interpreting CT imaging.
The most common cause of extrinsic compression is intrathoracic extension of an enlarged thyroid, causing displacement of the trachea more than narrowing.
Other mediastinal causes are:
- Thoracic aorta aneurysm.
- Anatomical variant of the great vessels (eg. double aortic arch), usually in young patients.
- Bulky lymphadenopathy or mass.
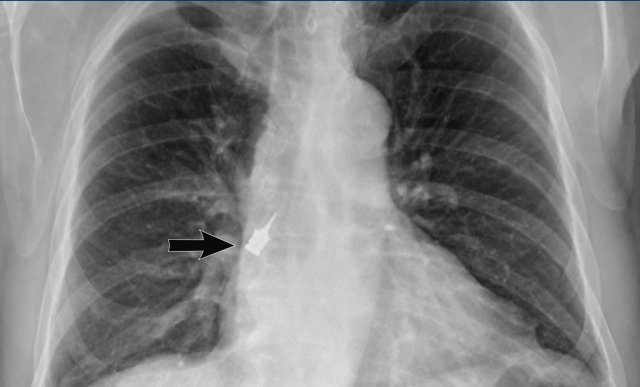
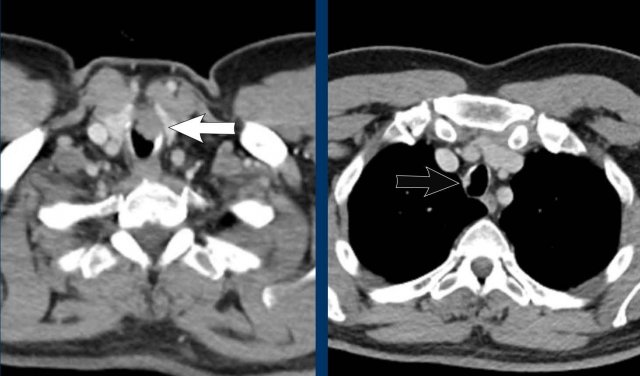
Lymph nodes
Compression of the right main bronchus by enlarged lymph nodes.
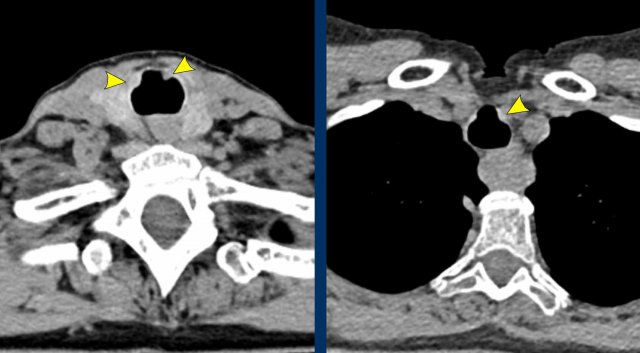
Double aortic arch
This patient has a double aortic arch which compresses the trachea.
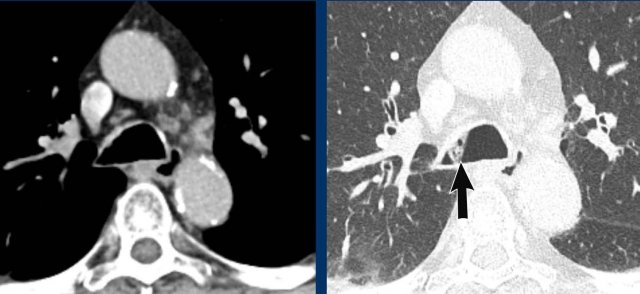
Fibrosing mediastinitis
Fibrosing mediastinitis is a more tricky
cause of extrinsic compression and displacement as it is often hard to diagnose
with certainty.
On CT imaging it can show considerable overlap with findings of
airway involvement due to a central lung malignancy.
Repetitive negative tissue
sampling and follow-up will often seal the case eventually.
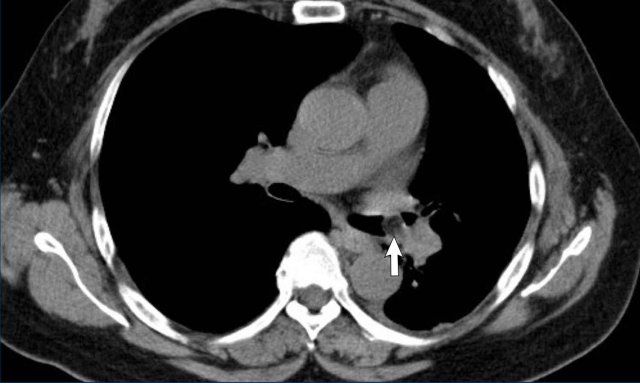
Image
Right-sided fibrosing mediastinitis in a 51 year old male, showing soft tissue density around the right main bronchus (arrow).
Same patient.
There are secondary signs of central airway and vessel
compression, with localized lung volume loss and interstitial thickening due to
edema.
Benign neoplasm
Hamartoma
Hamartoma is a benign lesion that is composed
of various mesenchymal tissues such as chondroid cartilage, fat and fibrous
tissue.
It is the most common benign lung tumor and most often located more
peripherally in the lung parenchyma, but sometimes arises in the airways.
Image
Endobronchial
hamartoma as an incidental finding in the middle lobe of a 73 y.o male.
CT characteristics of a hamartoma are independent of its location:
- Hypodense lesion
- Fat attenuation
- Popcorn calcification (may
be present)
Image
Fat containing hamartoma obstructing the left lower lobe bronchus in a 58 y.o female.
Lipoma
Typically seen as an endoluminal lesion without soft tissue component due to its pure fatty nature. It arises from the submucosal fat tissue of the tracheobronchial tree. The lesion is often pedunculated, although this is not always evident on CT.
Leiomyoma
Leiomyoma arise from the smooth muscle cells of the trachea. Typically it is seen as an endoluminal mass in relation to the posterior wall. The lesion may show heterogeneous density due to cystic degeneration as a result of poor vascularity.
Papilloma
A squamous cell
papilloma is the solitary variant of tracheobronchial papillomatosis, where
papillomatous growth of the epithelium is a response to HPV infection.
Laryngeal involvement is more common than tracheobronchial disease and when
central airway involvement occurs it may be seen on CT as multifocal nodularity not extending beyond the wall, and without calcification.
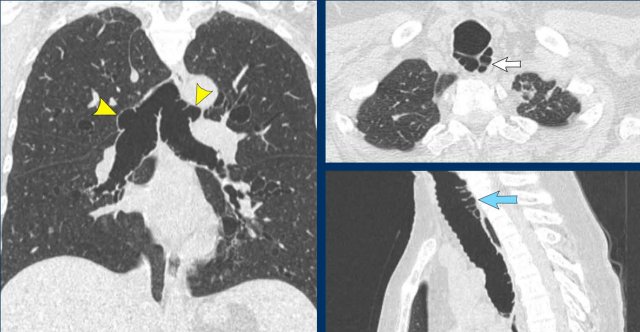
Image
Tracheobronchial
papillomatosis with lung involvement in a 54 y.o male, showing two papillomas
in the trachea.
Continue with the lung window...
The image shows multiple cystic lesions in both lungs (arrowheads).
In rare cases extension into the lung parenchyma can occur, showing cystic nodules most often in the dependent apical segments of the lower lobes. There is a small risk of malignant transformation from squamous cell papilloma into squamous cell carcinoma.
Miscellaneous
Given that any cell type present in the
central airways may give rise to pathology, all kind of rare lesions can develop.
This includes for example neurogenic tumors (figure) and rare lesions such as inflammatory myofibroblastic tumor.
Malignant neoplasm
Several primary malignant lesions arise in
the central airways.
Often they cause respiratory symptoms, and sometimes
hemoptysis.
In line with the benign neoplastic lesions, a specific radiological
diagnosis is challenging.
Patient characteristics such as age, smoking history,
as well as lesion morphology and location may give clues and will influence the
order of differential diagnostic considerations.
Given that any cell type present in the
central airways may give rise to pathology, all kind of rare lesions
develop.
This includes for example malignant lesions such as chondrosarcoma.
Radical surgical resection is
the preferred treatment, but often technically impossible.
Depending on the histology
and stage of the tumour, other modalities such as chemoradiotherapy may be used
with curative intent.
Squamous cell carcinoma
Squamous cell carcinoma is the most common primary
malignancy of the trachea.
Generally, it occurs in older patients with a
substantial smoking history.
Typically, an irregular mass is seen that tends
to invade surrounding tissues outside the airway wall.
Image
Irregular
focal mass that invades the trachea wall and peritracheal tissue in a 66 y.o
male.
PA:
Squamous cell carcinoma.
Adenoid cystic carcinoma
Adenoid cystic carcinoma (ACC) is the next most common
primary malignancy of the central airways.
Contrary to squamous cell carcinoma there is no association
with smoking.
Patients also tend to be younger, mostly middle-aged.
Radiologically adenoid cystic carcinoma can present as either a:
- focal mass
- more diffuse infiltrating morphology with a long segment of submucosal involvement.
Image
Severe luminal narrowing by a focal mass in 48 y.o female.
PA: Tracheal adenoid cystic carcinoma.
The malignancy arises from the submucosal minor salivary glands, as does the less common mucoepidermoid carcinoma (see below).
The tumor is mostly very centrally located.
The most common sites for metastases are the lung parenchyma and the liver.
Image
Irregular
more diffusely infiltrating mass with long segment of wall thickening invading the mediastinum in a 51 y.o female.
PA:
adenoid cystic carcinoma.
Bronchoscopic view of obstructing tracheal adenoid cystic carcinoma.
Mucoepidermoid carcinoma (MEC)
As mentioned above, MEC is a tumour that arises from the submucosal minor salivary glands. It is found in younger patients - often younger than those with ACC - and has no known association with smoking. It has a predilection for the more distal airways, as they are found more often in the segmental/lobar airways and rarely in the trachea. CT imaging features are non-specific; an enhancing focal soft tissue mass, with varying degrees of heterogeneity. Some show internal calcification. Post-obstructive changes may be present.
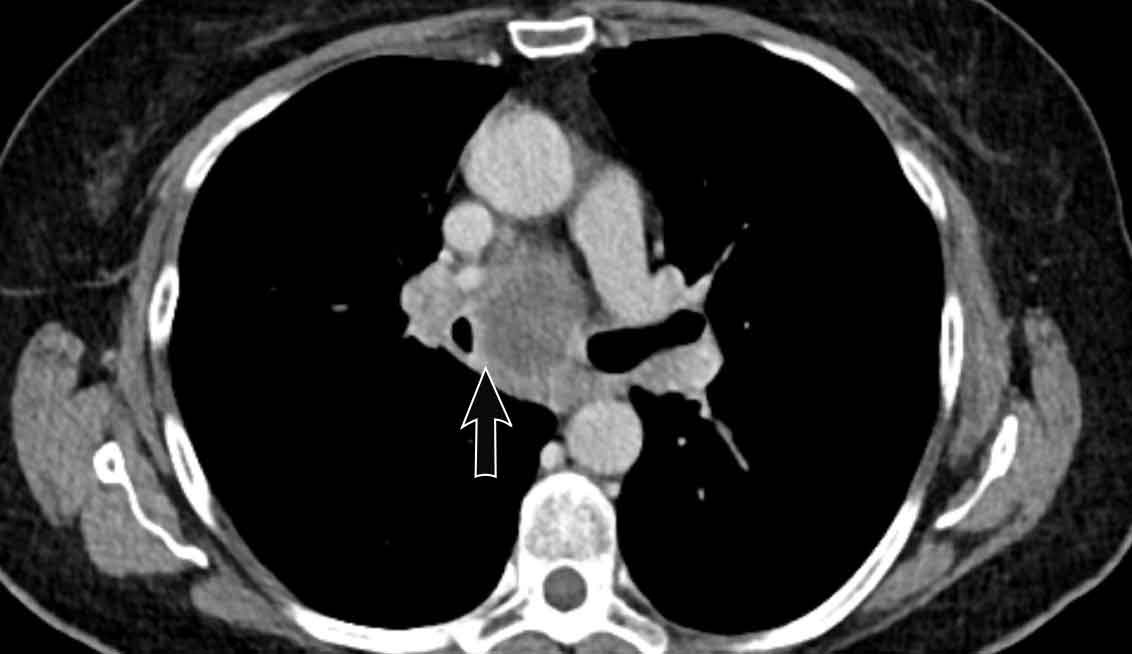
Carcinoid
Carcinoid tumours are low-grade
neuroendocrine tumours (NET) that originate from the neuroendocrine cells in
the airway wall.
Histopathologically, they may be typical or atypical, depending
on the mitotic rate and the presence of focal necrosis.
The majority are
typical carcinoids though, and these behave quite indolent.
They are found in
both younger and older patients, and there is no association with smoking.
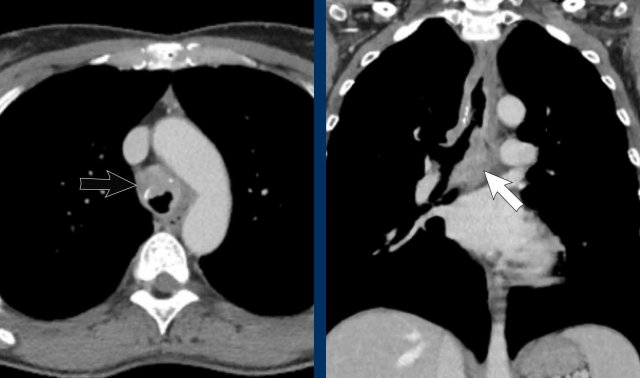
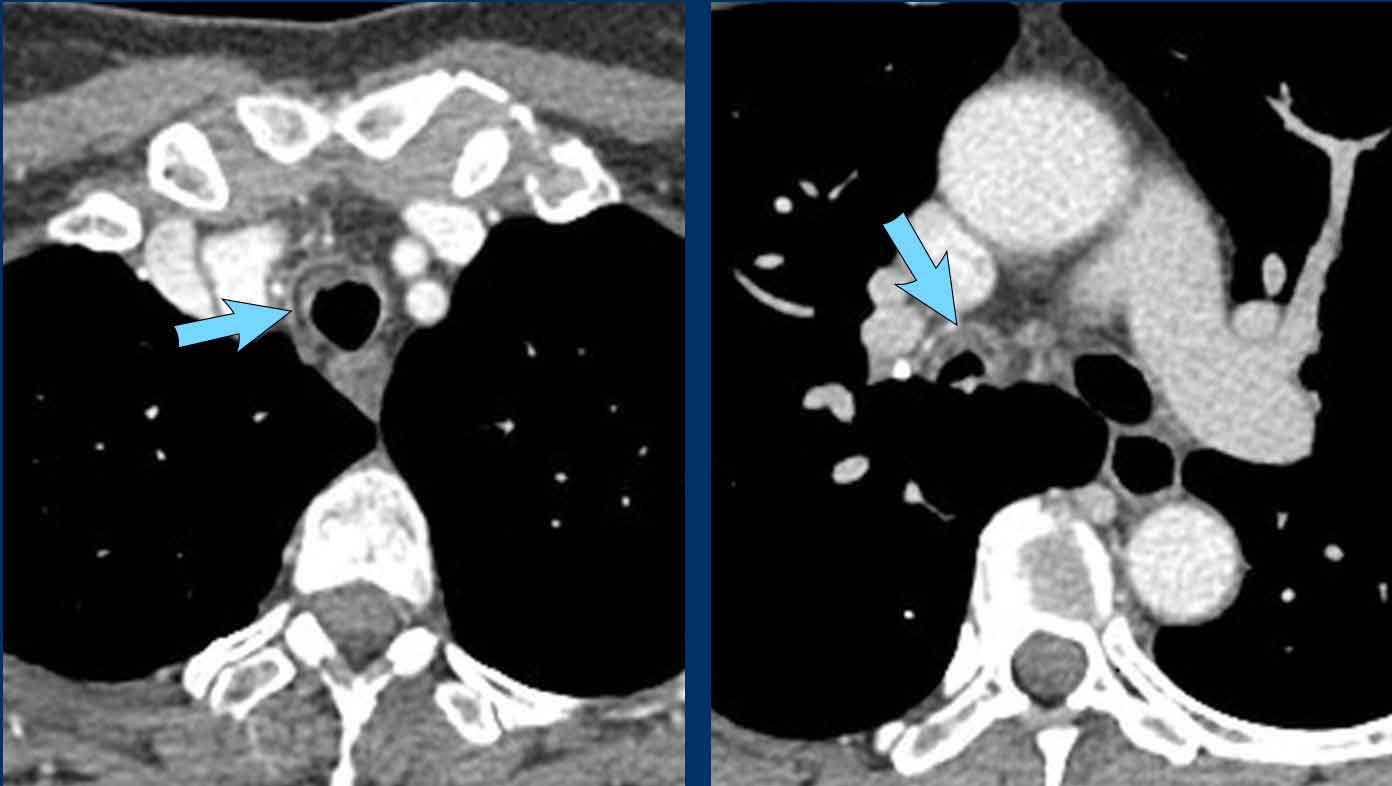
Image
Well-defined mass in the left main
bronchus in a 39 year old male.
Continue with the PET-CT...
The 68Ga-Dotatate PET-CT shows vivid uptake confirming the neuroendocrine cell origin.
Carcinoids arise in the more central airways (although hardly
ever in the trachea) as well as in the more peripheral ones, all the way
towards the outer third of the lung.
On CT carcinoid is a well-defined lesion, often hyperdense on post-contrast CT given their hypervascular nature.
Calcifications may be present in a minority.
Post-obstructive changes are common due to luminal obstruction, and may be the reason it is found.
Some lesions also show an extraluminal component, which excludes the option of complete curation through an endoscopic procedure.
Anatomical surgical resection is needed in these cases.
Continue with the bronchoscopic view...
Bronchoscopic view showing the typical finding of a well-defined and
vascularized lesion obstructing the lower lobe orifice.
PA: Carcinoid.
Metastases
Metastatic disease to the
central airways does occur through distant hematogenous or lymphatic spread.
Although uncommon, it is sometimes seen for instance in breast carcinoma, renal cell cancer and colorectal carcinoma.
Imaging findings are nonspecific and may show single or multiple solid nodules
projecting into the airway lumen.
Larger and more peripheral lesions may cause
airway obstruction.
Usually airway metastatic disease is not an isolated finding, but seen in patients with known metastatic disease.
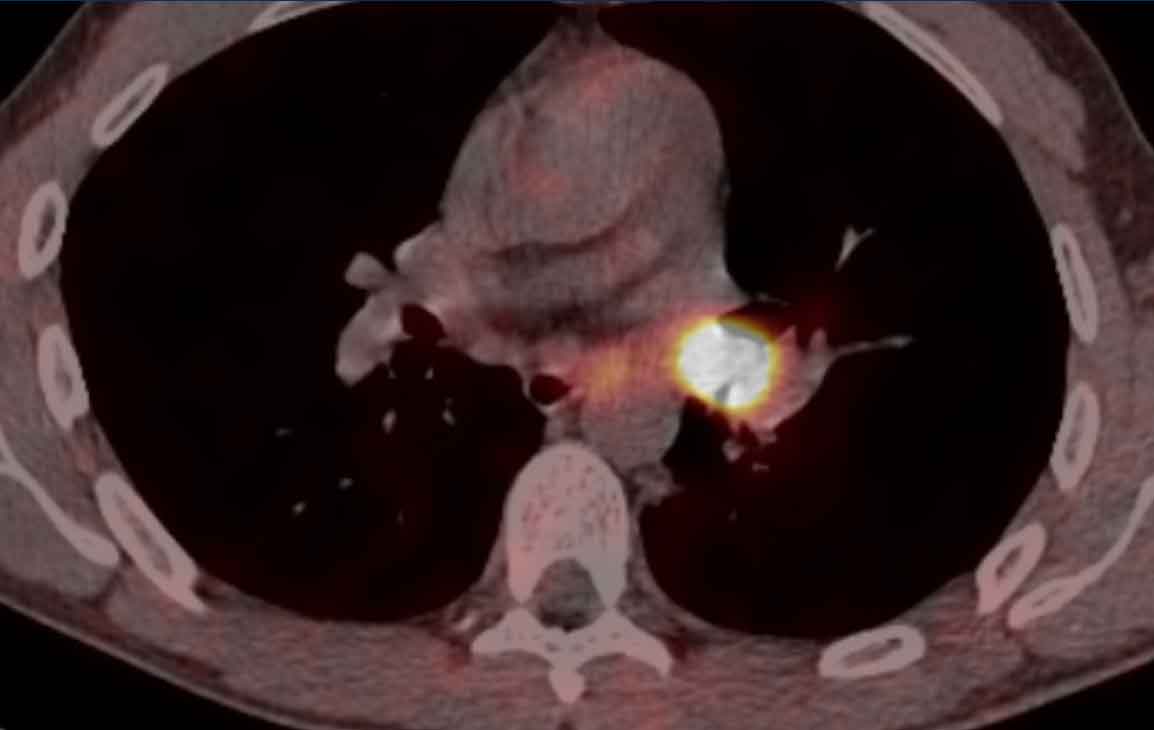
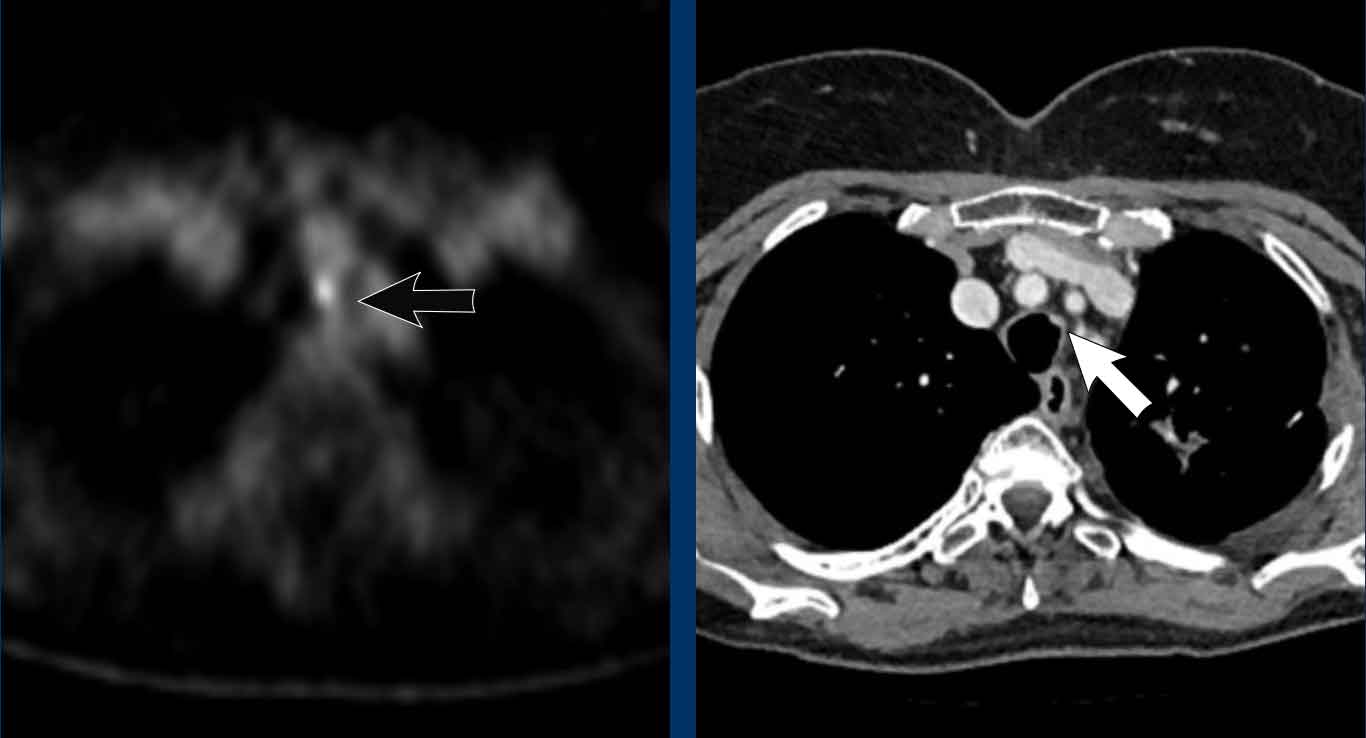
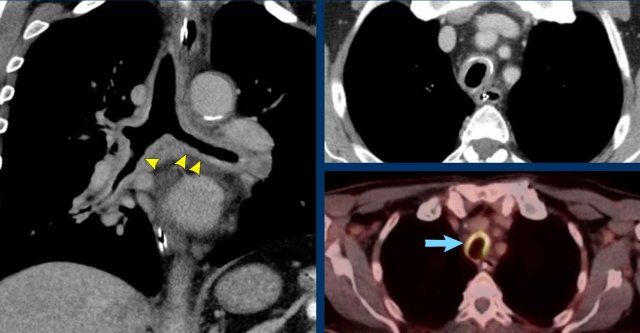
Image
The PET-CT shows high uptake corresponding to a small nodular
lesion in the proximal trachea in a 52 y.o female with prior colorectal
cancer.
PA: metastasis of colorectal cancer.
Infection
TB
As with most other infectious diseases, pathogens causing tracheobronchial infection can be either bacterial, fungal or viral.
Community acquired bronchitis is mostly triggered by a viral infection. Sometimes infection may be associated with procedures such as tracheostomy, as shown on the left.
Although tuberculosis can cause central airway
abnormalities, isolated tracheobronchitis is very rare.
Central airway involvement during more widespread thoracic
disease is more likely, and can reveal itself on CT imaging as irregular focal
or more diffuse wall thickening.
In the chronic phase it may lead to focal
airway stenosis due to airway remodelling and formation of fibrosis in reaction
to ulceration of submucosal tubercles.
Image
Focal wall thickening with luminal narrowing of the trachea and right main bronchus in a 63 y.o female with remote TB infection. Biopsy showed fibroelastic scarring.
Fungal infections causing tracheobronchitis might also be encountered, for example by Aspergillus, Candida or Histoplasmosis.
This occurs primarily in the immunocompromised population.
In line with the above mentioned TB morphology, it may cause non-specific CT findings of focal or more diffuse wall thickening, with residual scarring and stenosis in later stages of the disease.
Image
Diffuse
circumferential wall thickening of the trachea and central bronchi with
uptake on FDG-PET scan (blue arrow) in a 72 y.o male after tracheostomy due to
complicated thyroidectomy.
Clinically labelled as low-grade infectious,
despite the fact that no specific pathogen was cultured.
Inflammatory
Relapsing polychondritis
Relapsing polychondritis is an auto-immune disorder that affects
the cartilage in the central airways with recurrent episodes of inflammation
and possible destruction and fibrosis.
As cartilage in other parts of the body
may also be affected, clinically one may see ear and nose involvement as well
(eg. saddle-nose deformity). Cardiovascular disease such as cardiac valve
disease and aortic aneurysm can occur.
On CT imaging of the chest central airway wall
thickening with soft tissue density is seen.
Abnormalities typically spare the
posterior wall which lacks cartilage.
Beyond the acute phase calcification and stenosis may form, as well as
excessive airway collapse in expiration (ie. tracheobronchomalacia) due to
cartilage destruction.
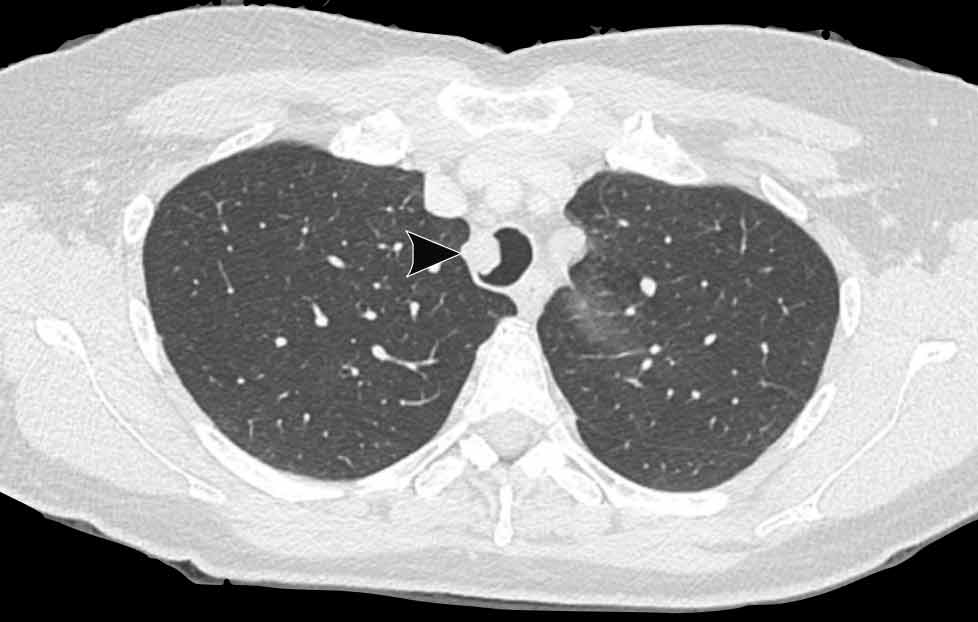
Image
Relapsing polychondritis in a 55 y.o female, showing inflammatory central airway wall thickening with the characteristic horseshoe shaped appearance (arrowhead). No thickening of posterior wall (yellow arrow).
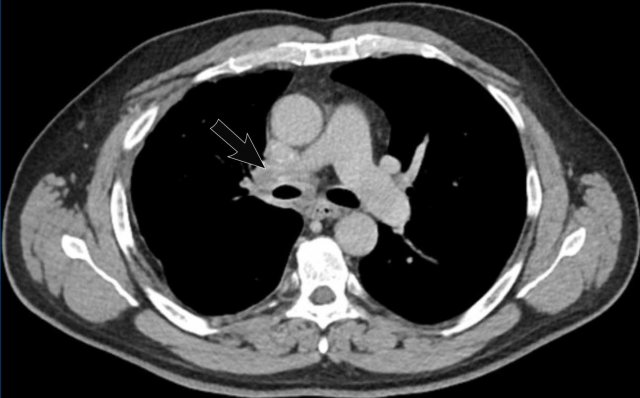
Granulomatosis with polyangiitis
Granulomatosis with polyangiitis (GPA), previously known as Wegener's granulomatosis, is a
multisystem necrotizing vasculitis that affects the medium and small size vessels with involvement of paranasal sinuses, lungs and kidneys.
Clinically
it is associated with elevated c-ANCA titers.
GPA can cause irregular
circumferential wall thickening of the central airways, which can lead to
stenosis in later stages of the disease.
This is typically seen in the
subglottic trachea but also occurs in the main stem and lobar bronchi.
Synchronous pulmonary findings of cavitating consolidations and ground glass caused by the vasculitis – due to necrosis and alveolar hemorrhage, respectively – are helpful to sort the differential diagnostic considerations.
Image
Central airway involvement in GPA showing circumferential tracheal wall thickening at the level of the carina in a 43 y.o male. There is left lung collapse due to chronic involvement of the left main bronchus with stenosis.
Amyloidosis
Tracheobronchial amyloidosis is characterized by submucosal
deposition of abnormal amyloid protein.
It is a very rare disease, which is
usually isolated but can be associated with systemic amyloid disease.
The protein deposition can either be focal (ie. mass-like;
amyloidoma) or more diffuse and infiltrative.
Amyloid in the airway walls leads
to dense and calcified, strikingly irregular soft tissue thickening on CT
imaging.
There is no cure, and therapeutic options such as external beam
radiation and bronchoscopic debulking are focussed on limiting luminal
obstruction to relieve respiratory symptoms.
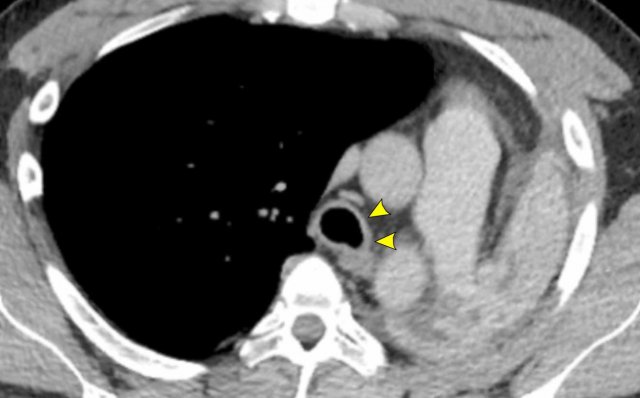
Image
Tracheobronchial amyloidosis in a 61 y.o
female, showing irregular airway wall thickening with dense and calcified foci causing
significant luminal narrowing of the right main bronchus.
Bronchoscopy
shows typical yellowish irregular lesions.
Sarcoidosis
The most common manifestations of sarcoidosis in the chest
are symmetrical hilar and mediastinal lymphadenopathy and pulmonary parenchymal
involvement with lymphatic distribution of small nodules.
This imaging
morphology is classic, but the disease is known for its wide range of
appearances and may be considered in the differential diagnosis for a lot of
imaging findings.
Although histopathologically granulomatous involvement of the
airways is relatively common, CT signs of central airway involvement in
sarcoidosis are relatively rare.
Of course, architectural distortion and airway
obstruction may be caused by extrinsic compression due to peribronchial fibrosis, which is often seen in the
hilar regions.
In addition, direct airway remodelling due to granulomatous involvement
of the central airways may lead to circumferential airway wall thickening.
If
present, it is almost always part of more extensive thoracic disease and not an
isolated finding.
Inflammatory bowel disease (IBD)
Both
ulcerative colitis (UC) and Crohn's disease (CD) may show airway involvement.
More common than central airway disease is peripheral bronchial wall thickening
and bronchiectasis, as well as signs of involvement of the smaller airways (ie.
bronchiolitis and air trapping).
When
the trachea and main bronchi are involved, CT imaging may show nonspecific
circumferential wall thickening, luminal narrowing and postobstructive
findings.
Tracheobronchopathia osteochondroplastica
The etiology of this disease is not well known.
It is
characterized by submucosal osteocartilaginous nodules that on CT imaging
present as multiple small calcified nodules that only involve the cartilaginous
portion of the central airways, and thus spares the posterior wall of the
trachea.
This disease may be an incidental finding, but may also
cause mild respiratory symptoms.
The prognosis is generally good and in
asymptomatic cases no interventions are needed.
If needed, therapeutic options may be focussed on limiting luminal obstruction caused
by the osteocartilaginous nodules.
Image
Tracheobronchopathia
osteochondroplastica in a 67 y.o female with non-specific airway symptoms,
showing multiple small nodules along the cartilaginous part of the trachea
Congenital
Tracheal bronchus
Airway branching variation is very common, especially at
the segmental level.
Several anatomical variants are encountered on a more
regular basis and might be worth mentioning, although patients are mostly asymptomatic.
If
they do lead to symptoms, this is mostly due to recurrent infections caused by abnormal
drainage.
In case of a tracheal bronchus (also called pig bronchus) the right upper lobe parenchyma is partially aerated through a separate bronchus that originates directly from the supracarinal portion of the trachea.
Image
Incidental tracheal
bronchus in a 28 y.o male scanned for oncology follow-up (axial image) and in a 77 y.o male scanned in trauma setting (coronal image).
Cardiac bronchus
This truly supernumerary bronchus
originates on the medial side of the bronchus intermedius, opposite to the
right upper lobe orifice.
This might be a blind ending structure, or an airway
that aerates a small amount of lung parenchyma.
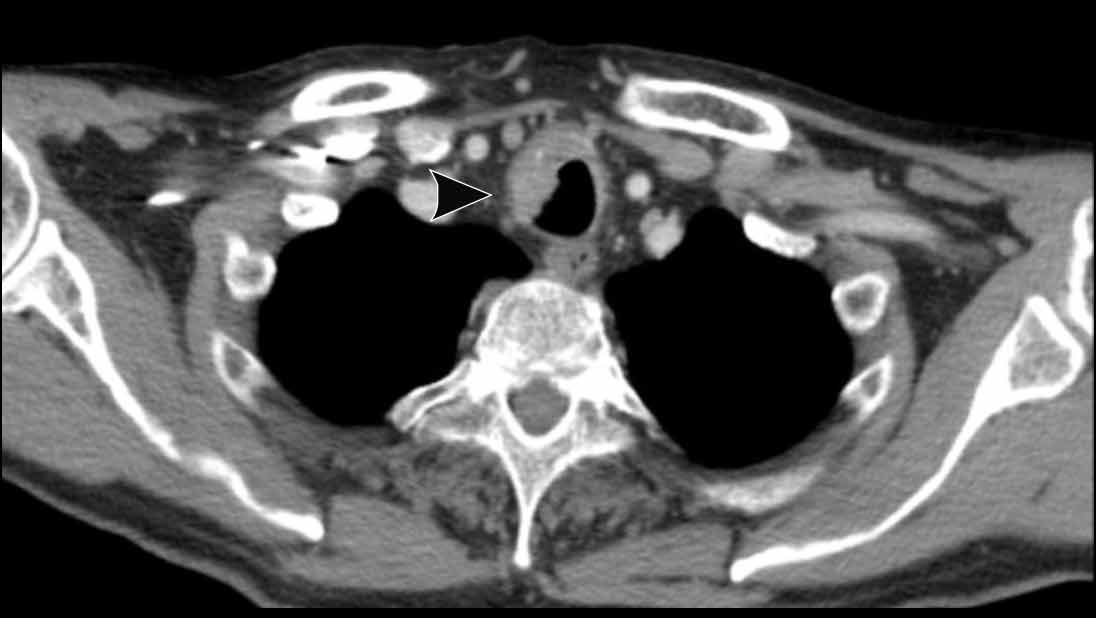
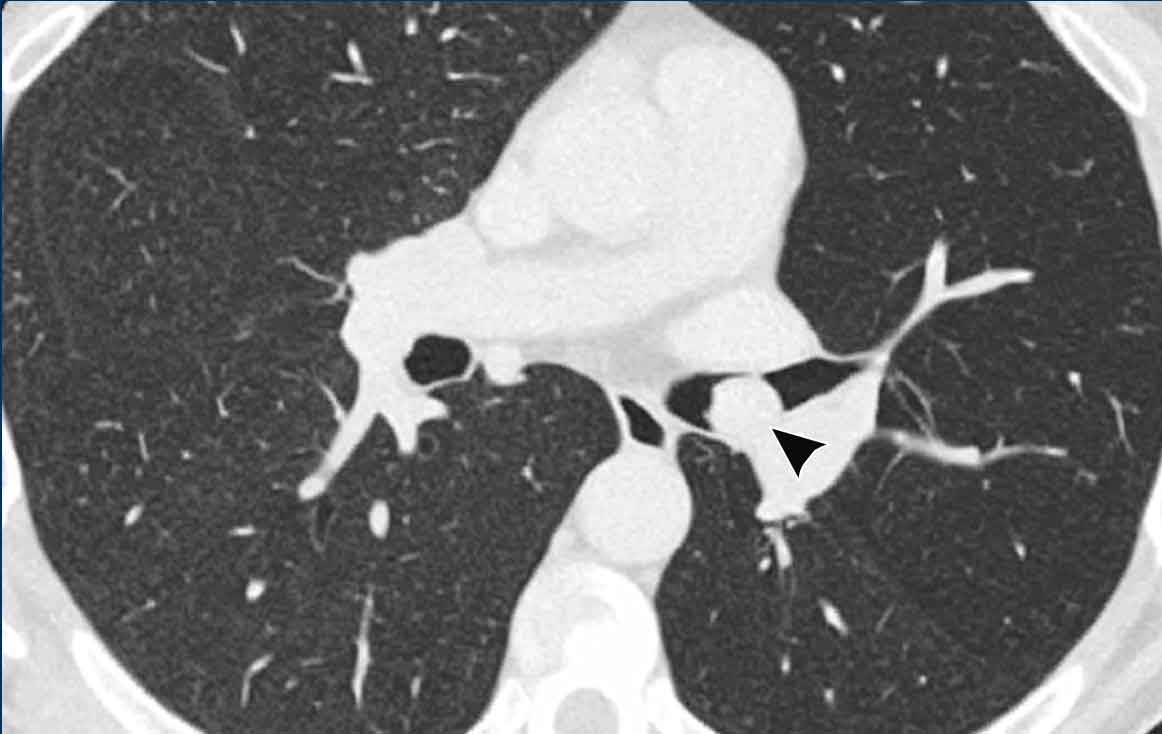
Image
Cardiac
bronchus (arrowhead) in a 57 y.o female in follow-up for interstitial lung disease.
 Tracheobronchomegaly in a 59 y.o female, showing a severely dilated trachea and mainstem bronchi, with evident posterior diverticulosis.
Tracheobronchomegaly in a 59 y.o female, showing a severely dilated trachea and mainstem bronchi, with evident posterior diverticulosis.
Tracheobronchomegaly
Tracheobronchomegaly (also called Mounier-Kuhn syndrome) is caused by
abnormal elastic fibres and smooth muscle cells in the central airways.
Typically, it is seen in middle aged men who present with
chronic cough and/or recurrent infections.
CT findings:
- Enlargement of central airways in inspiration (trachea > 3 cm)
- Due to the flaccidity of the airways, marked collapse in expiration.
- Posterior tracheal diverticulosis
- Central bronchiectasis
Williams-Campbell syndrome
This
disease is characterized by congenital cystic bronchiectasis, and typically
presents with recurrent infections.
It is thought to be caused by cartilage
deficiency in the subsegmental bronchi (ie. 4th to 6th order).
It therefore shows bilateral diffuse
bronchiectasis on CT imaging, with typical sparing of the lower order bronchi
and trachea.
This in contrast to
tracheobronchomegaly that typically involves the 1st to 4th order bronchi.
Image
Localized perihilar bronchiectasis but normal dimensions of the trachea, main bronchi as well as peripheral airways.
This was a 46 y.o male with the
diagnosis of Williams-Campbell syndrome, presenting with recurrent infections,
mild hemoptysis and longstanding airway symptoms.