Cervical Cancer - MR staging
Stephanie Nougaret¹, Doenja Lambregts² and Annemarie Bruining²
¹ Dept. of Radiology, Montpellier Cancer Centre, France and ² the Netherlands Cancer Institute, Amsterdam
Publicationdate
In
this article we describe the role of MRI for the local staging of cervical
cancer.
In
addition to clinical and pathological examination, MRI has an important role in
identifying patients with advanced disease and thereby to guide treatment
planning.
It also aids in selecting patients eligible for fertility-preserving
strategies.
MRI is also important to monitor treatment response and to detect
recurrent disease during post-treatment follow up.
We will discuss:
- MR reporting checklist for cervical cancer staging
- Interpretation and reporting pitfalls
- MR anatomy relevant for cervical cancer staging and treatment planning
- MR protocol including the role of functional imaging sequences
- Overview
of current FIGO staging
Introduction
Cervical cancer represents the fifth most common cancer type
in women and - together with endometrium cancer - accounts for 0,7% of all
cancer related deaths in the world (1,2).
Persistent human papilloma virus infection is the key risk
factor responsible for nearly all cervical cancers.
HIV infection is a second
known risk factor, which increases the risk for cervical cancer by
approximately six-fold.
Most common types of cervical cancer are squamous cell
carcinoma followed by adenocarcinoma and some rare other types such as
neuroendocrine tumors.
Cervical cancer can be effectively prevented by vaccination
against HPV.
Secondary prevention includes HPV DNA testing to screen for
active infection and prompt treatment of cervical pre-cancer.
The primary
treatment for advanced cervical cancer (stage ≥ IB) is chemoradiotherapy (CRT)
followed by brachytherapy.
In the vast majority of cases, this results in a complete
local tumor response and no further surgical intervention is needed.
In the
minority of cases with persistent tumor after completion of CRT, addition surgical
resection is required. Early cases are treated with conservative surgery.
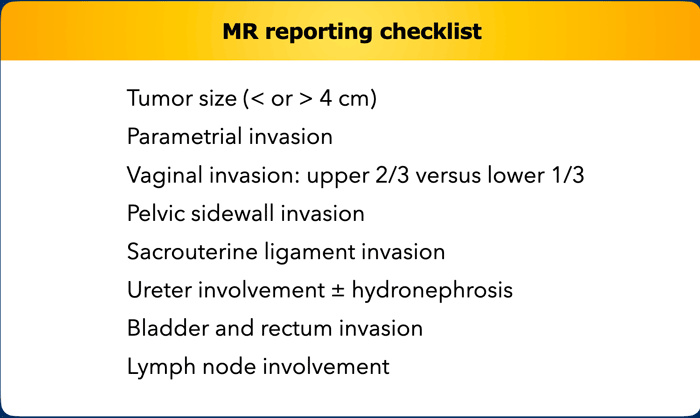
The key risk factors in cervical cancer to assess on imaging are tumor size, invasion into parametrium, pelvic side wall, vagina, bladder or rectum, and lymph node involvement.
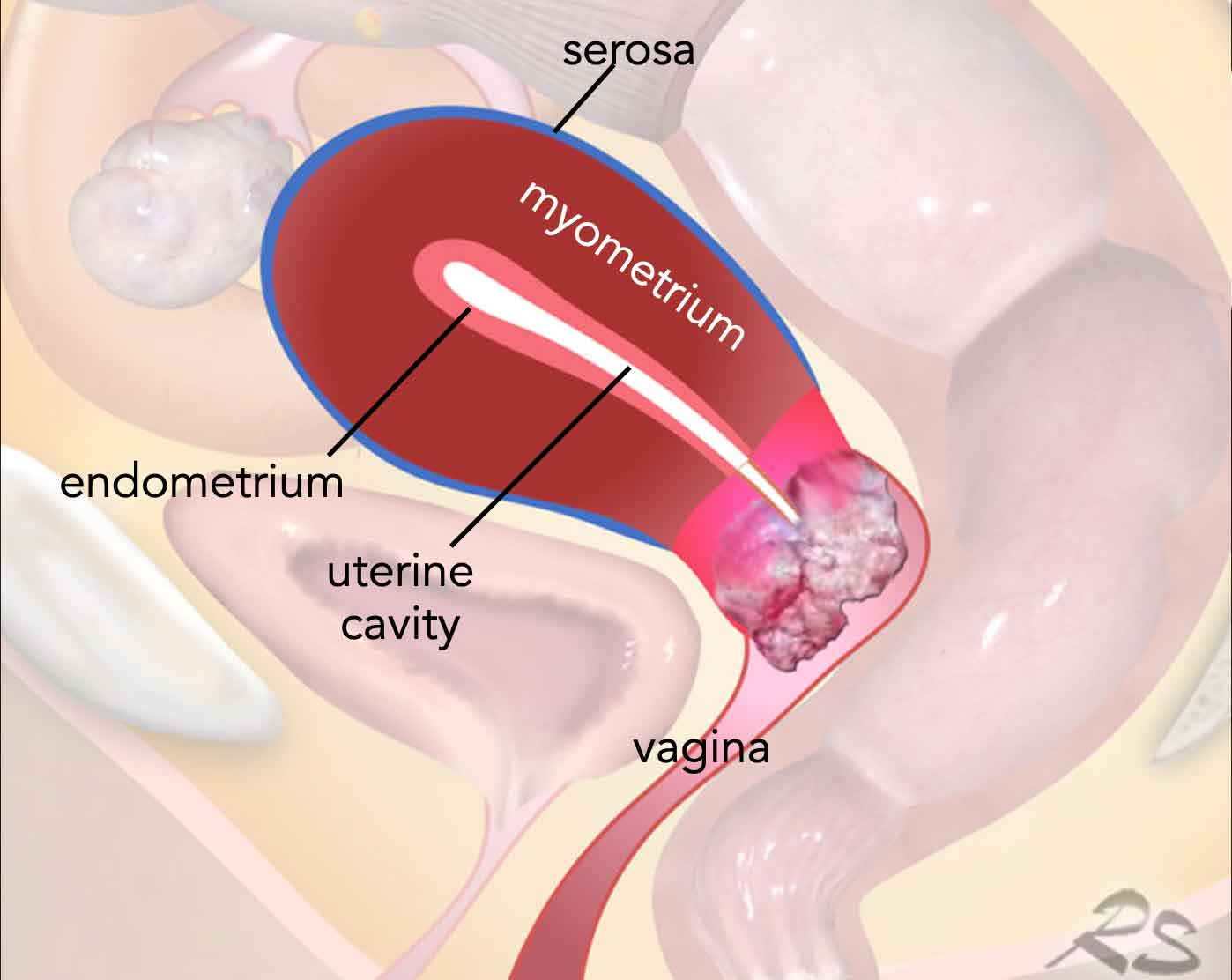
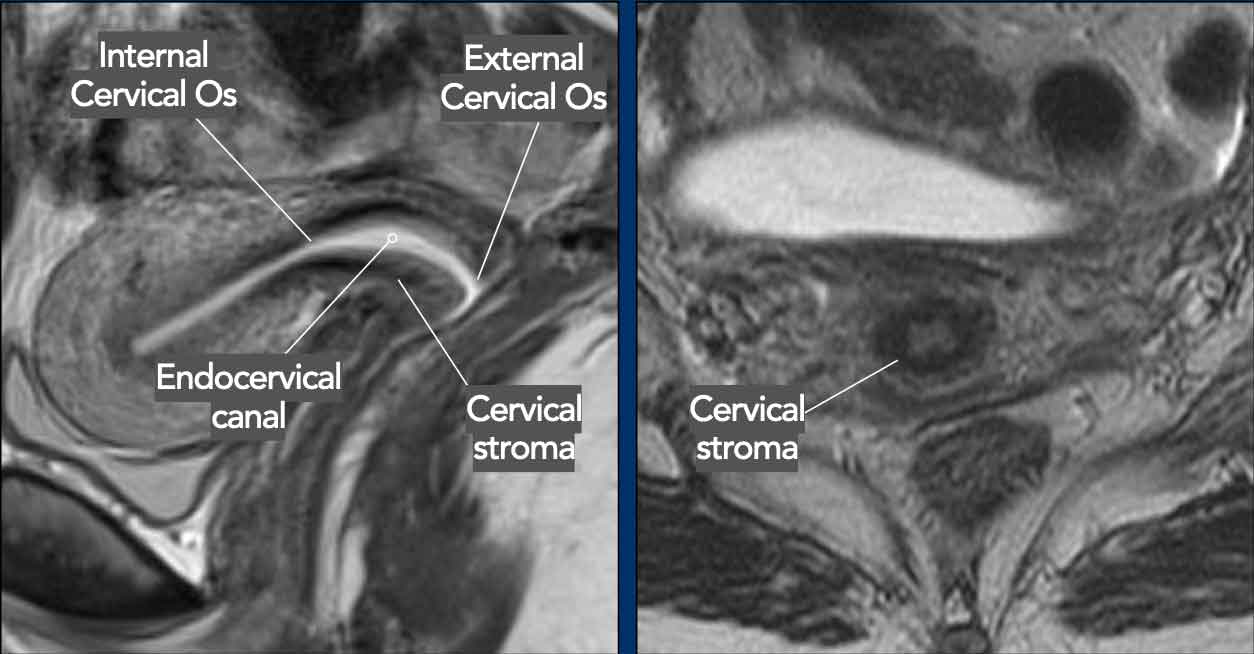
Like the uterus, the cervix shows distinct layers on T2W MRI.
The cervical mucosa has a high signal intensity.
The normal cervical stroma
has a low signal with an intact outer border.
The external cervical os is
the opening between the cervix and vagina.
The internal cervical os is the opening
between the cervix and the uterine cavity.
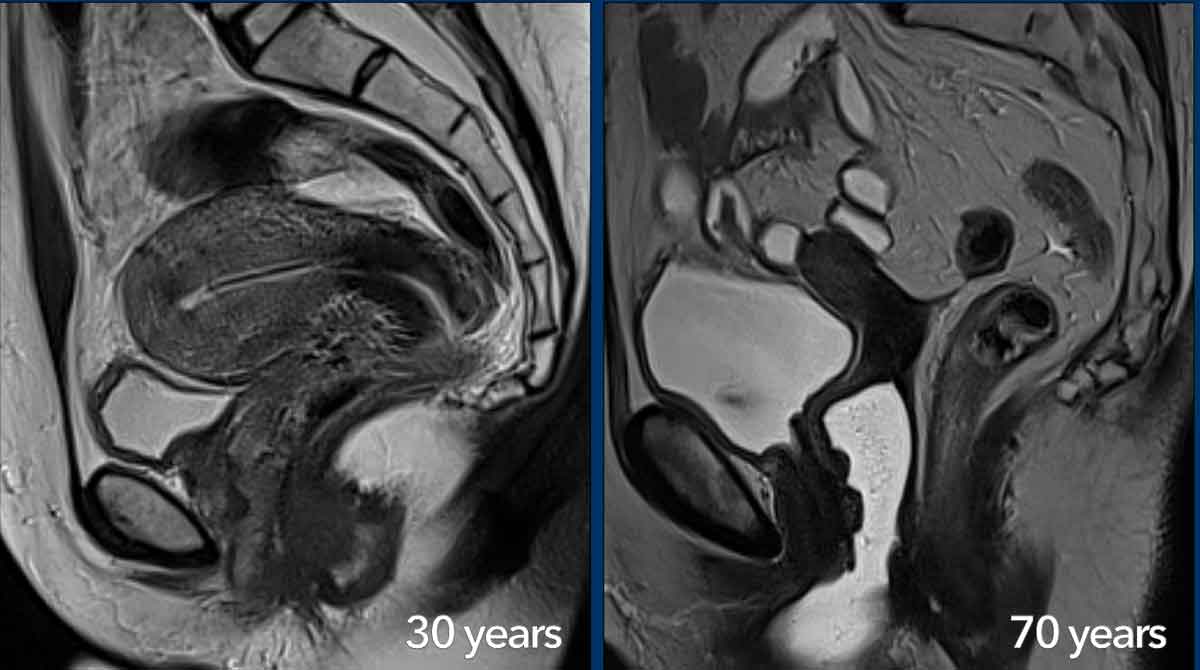
The zonal MRI anatomy of the uterus and cervix varies with age.
During the reproductive age the different layers of the uterus and cervix are well recognizable and the muscular part of the uterine wall can be highly vascularized like in this 30-year-old woman (left image).
There is an IUD in the uterine cavity, which can be recognized as a hypointense linear structure.
In postmenopausal women the zonal anatomy becomes less
visible and the cervical stroma, junctional zone and myometrium appear more
homogeneously hypointense on T2W-images, like in this 70-year-old woman (right
image).
With age, the female reproductive organs gradually become
smaller with a more pronounced loss in volume for the uterus compared to the
cervix.
Staging Cervical Cancer
MR reporting checklist
The MRI report in cervical cancer should address the key risk factors used to stage the patient as listed in the table in order to determine the most appropriate treatment strategy.
Additional factors to report, that are mainly used for surgical treatment planning:
- Distance between tumor and internal cervical os
- to assess feasibility of fertility sparing
- Total uterine size … x… cm, measured in sagittal plane
- to assess feasibility of laparoscopic versus open surgery
- Associated benign conditions like endometriosis and leiomyoma
- Anatomic variants
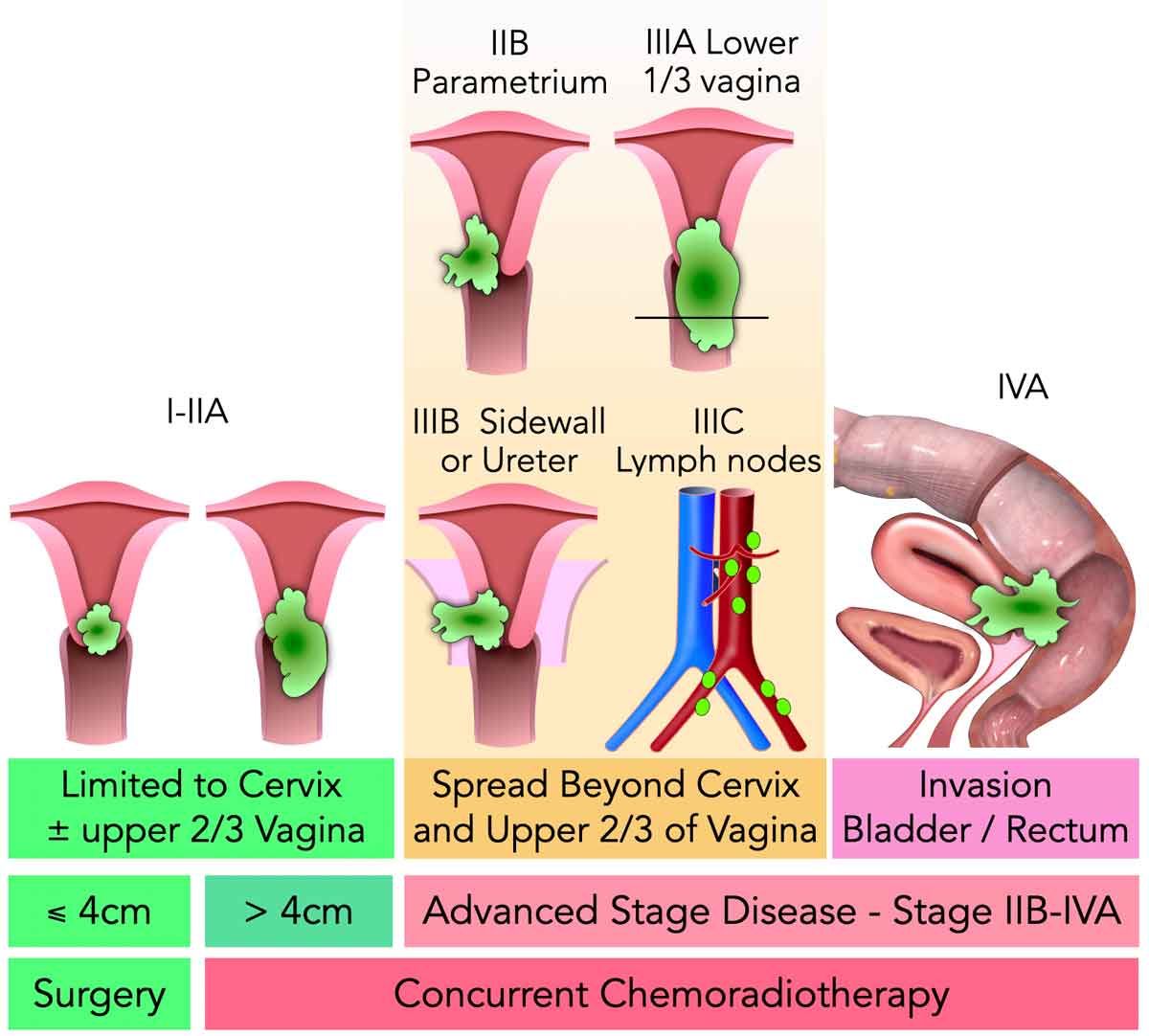
This schematic overview shows how the key risk factors that should be assessed on MRI impact the clinical tumor stage and corresponding treatment planning.
- Only small (<4 cm) early-stage tumors are amendable to upfront surgery (without chemo- or radiotherapy).
- For the remaining stages, concurrent (=combined) chemoradiotherapy (CRT) is the standard treatment.
The CRT scheme typically consists of external beam radiotherapy combined with chemotherapy, followed by brachytherapy. - If the tumor has spread to distant organs, lymph nodes (above the renal veins) or the peritoneum we are dealing with stage IV metastasized disease, in which case patients are typically no longer amendable to local treatment but receive palliative chemotherapy.
Tumor type and size
The tumor size should be measured in the longest possible dimension, which is often best visualized in the sagittal and sometimes in the coronal plane.
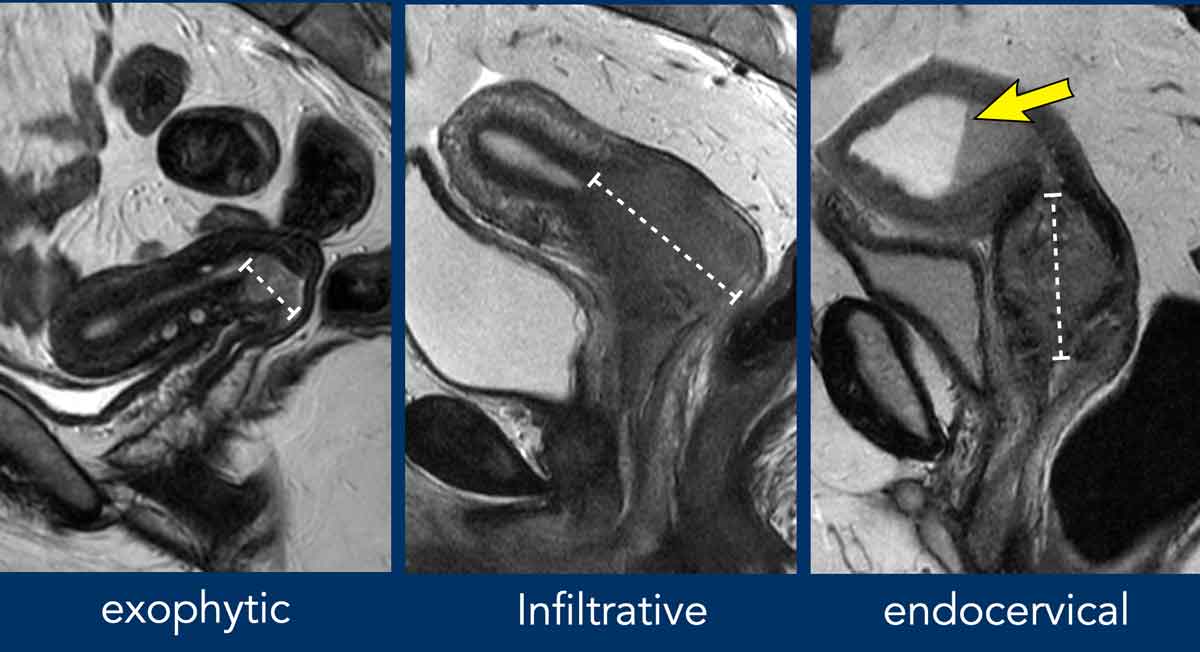
Cervical tumors can show either an exophytic (typically in
younger women), diffuse infiltrative or endocervical (typically in older women
and/or adenocarcinomas) growth pattern.
Note that in the right image where
there is an endocervical mass, this mass causes obstruction of the cervical
canal with widening of the uterine cavity which is filled with high signal
fluid and intermediate signal blood resulting in a blood-fluid line.
Vaginal invasion
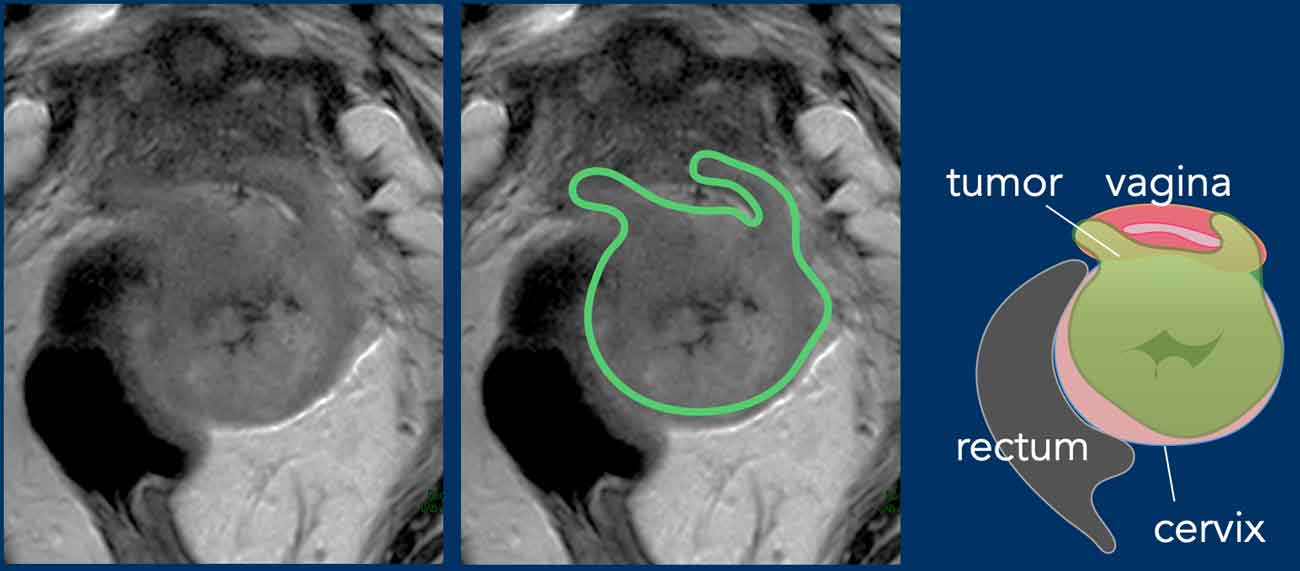
Invasion of the vaginal wall can be recognized on T2-weighted MRI as the extension of relatively hyperintense soft tissue extending into the vaginal wall.
In case of vaginal invasion you need to establish whether
this concerns the upper 2/3 (stage IIA) or lower 1/3 (stage III) of the vagina, as this impact patient management.
Stage IIA1/IIA2 may be eligible for upfront surgery.
In contrast lower vaginal involvement preclude surgery and patients are referred for chemoradiation.
Parametrial invasion
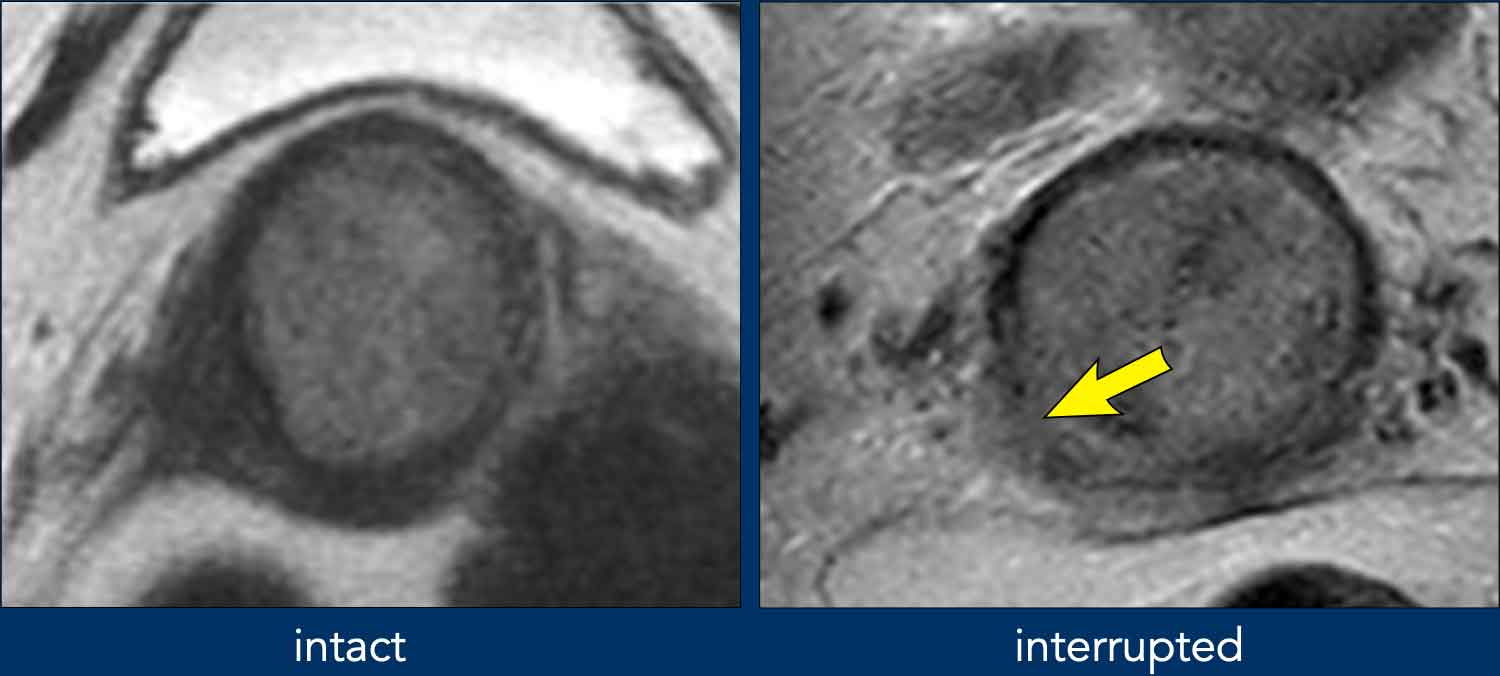
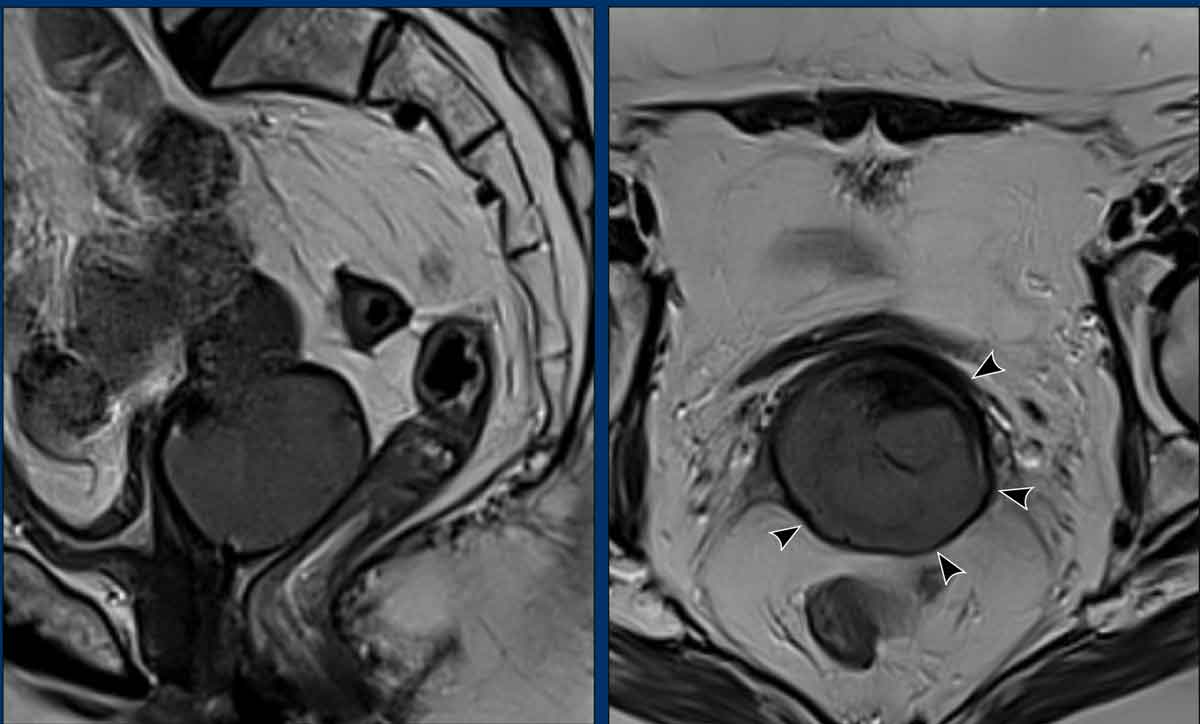
When the hypointense stromal ring of the cervix is intact (left image), MRI can predict the absence of parametrial invasion with a high negative predictive value of more than 90%.
Interruption of the hypointense stromal ring of the cervix (right image) and tumoral signal intensity or soft tissue mass extending into the parametrium are signs indicative of parametrial invasion (FIGO stage IIB).
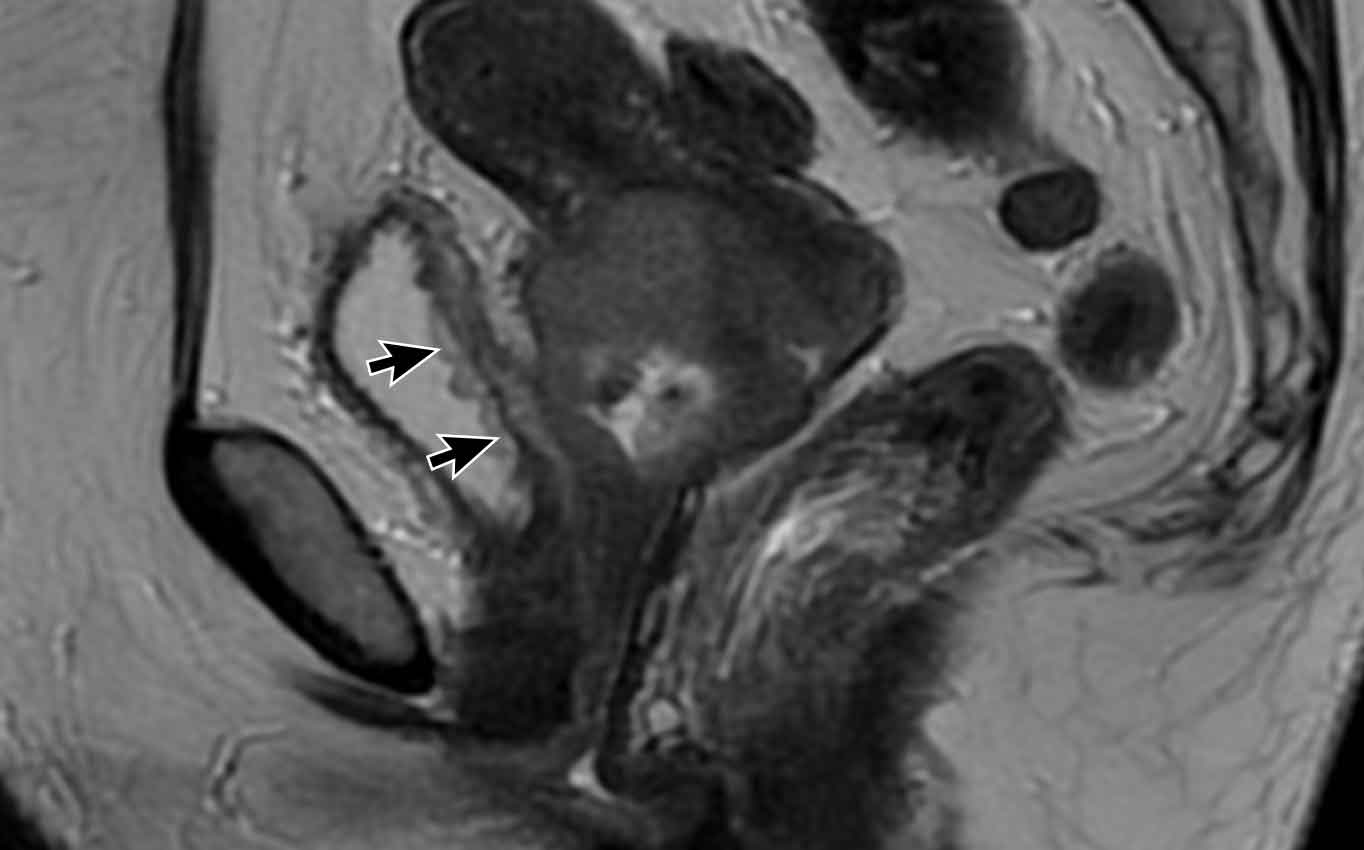
Pitfall - Expansion versus invasion
This example shows a large tumor that expands the cervix.
Note that there is no actual invasion of the parametia as the
hypointense stromal ring of the cervix is completely intact as indicated by the
arrowheads.
Pelvic sidewall invasion
Pelvic sidewall invasion is defined as invasion or tumor abutment within < 3 mm of the internal obturator, levator ani or piriformis muscles, or the iliac vessels, either with or without obstruction of the ureter resulting in hydronephrosis (stage IIIB).
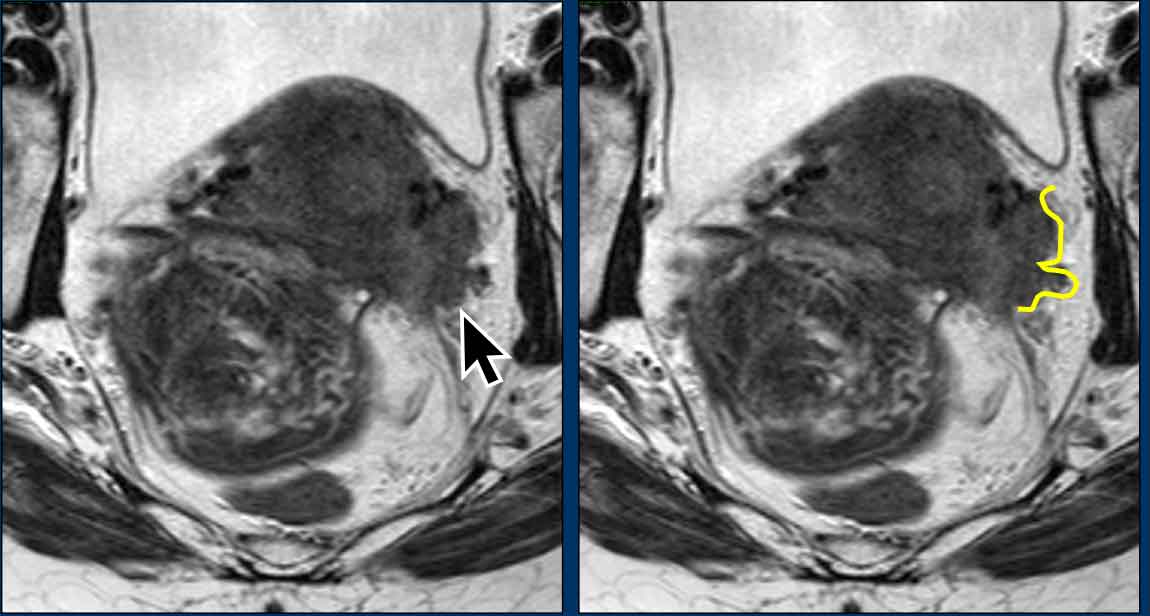
Sacrouterine ligament invasion
This sagittal MRI shows a locally advanced cervical cancer (circle) with extensive invasion along the sacrouterine ligaments (arrows).
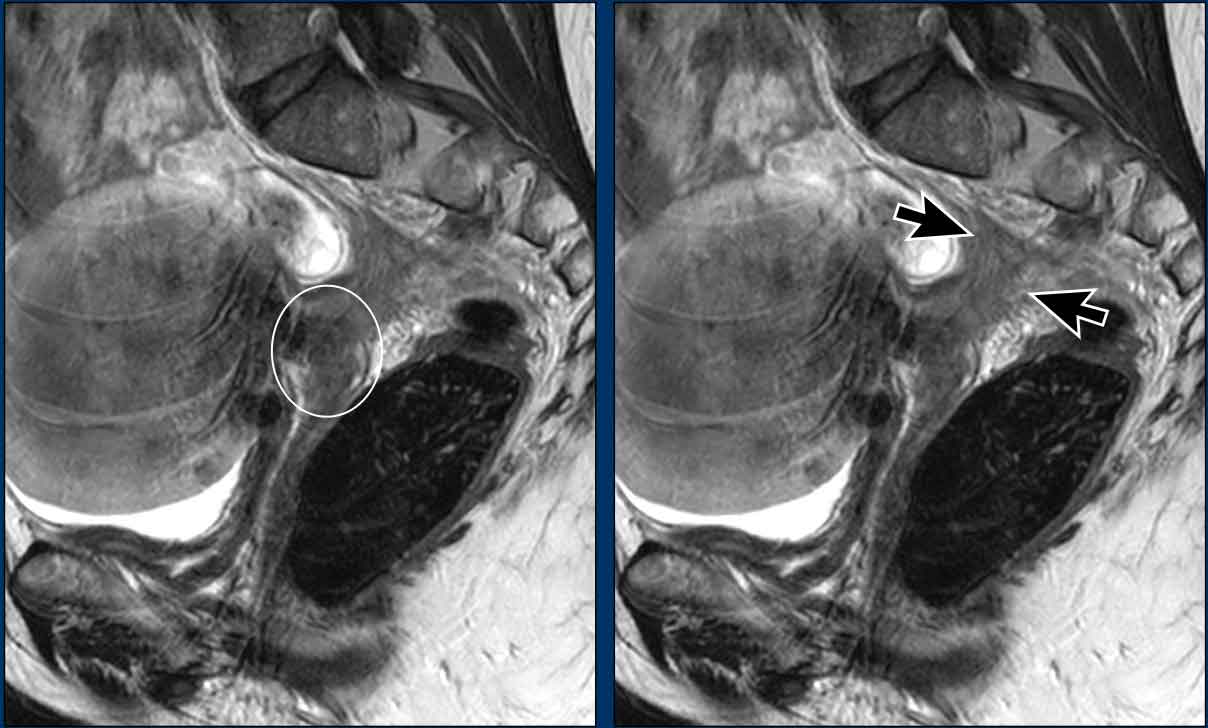
Bladder and rectal invasion
The case on the
left shows a cervical tumor with clear invasion of the dorsal bladder wall
extending into the bladder lumen.
This represents stage IV disease.
Pitfall
- Invasion versus bullous edema
The image shows a cervical tumor invading the upper 1/3 of
the vagina.
There is a hyperintense layered appearance of the bladder
wall (arrows) consistent with bullous edema.
There is no intermediate T2-weighted signal intensity or
nodularity within the bladder, suggesting that there is no actual tumor
invasion into the bladder.
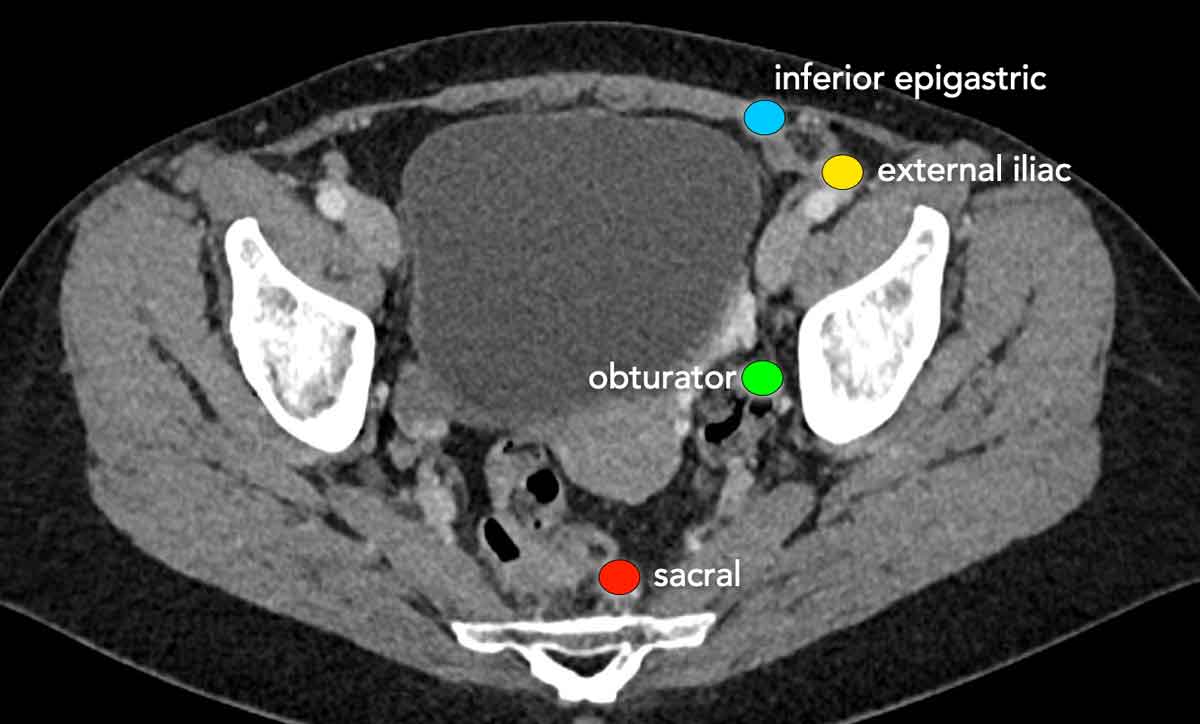
Lymph node staging
The regional lymph nodes in staging cervical cancer include all lymph nodes in the pelvis and para-aortic nodes up to the level of the renal veins.
It is important to detect para-aortic lymph node metastases, as presence of these nodes requires adaptation of the radiotherapy field.
Inguinal lymph nodes and para-aortic nodes above the level of the renal veins are considered distant metastases.
MRI has a
limited diagnostic performance for pelvic lymph node staging.
It mainly
relies on nodal size as a criterion; size cut-offs vary in literature but a
commonly used threshold is 1 cm.
Reported sensitivities (±40-90%) and
specificities (±80-100%) for MRI vary widely.
PET/CT is more accurate than MRI
and is used for pelvic lymph node staging, as well as for the assessment of
para-aortic lymph nodes and distant lymph node metastases above the level
of the renal veins (3).
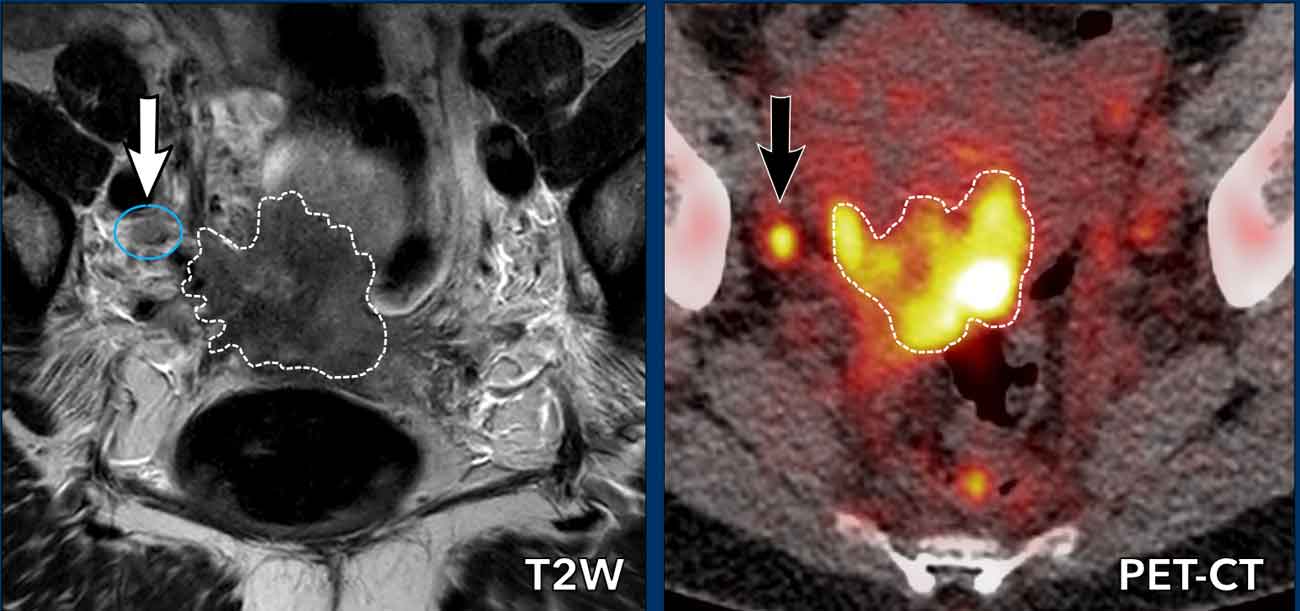
Images
There is a locally
advanced cervical cancer with right-sided parametrial and pelvic sidewall
involvement.
There is a 7 mm node dorsal to the right external iliac
vein (white arrow) which is indeterminate on MRI.
Based on its size it is not
clearly pathologic.
On corresponding
PET/CT the primary tumor is clearly FDG-avid, as is the small para-iliac lymph
node (black arrow), thereby diagnosing it as N+.
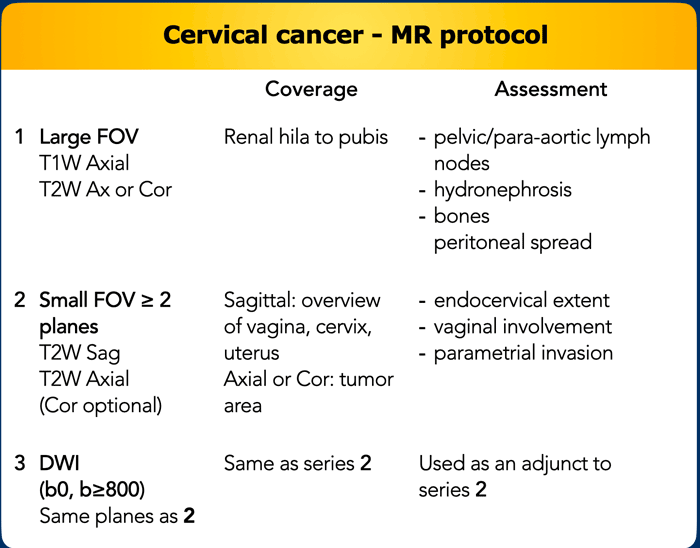
MR protocol
The recommended MRI protocol is summarized in the table.
Addional recommendations are as follows:
- Field strength should be 1.5T or higher, using a pelvic phased-array coil.
- Patient in supine position
- Use of saturation bands on the subcutaneous fat (anterior and posterior) is recommended.
Patient preparation:
- Fasting (4-6 hours), empty bladder
- Use of anti-peristaltic agents (Buscopan or Glucagon)
- Optional: vaginal gel to assess upper vaginal involvement
Note that contrast-enhanced images are not required for
cervical cancer staging.
Scheduling the examination according to the menstrual
cycle is not required.
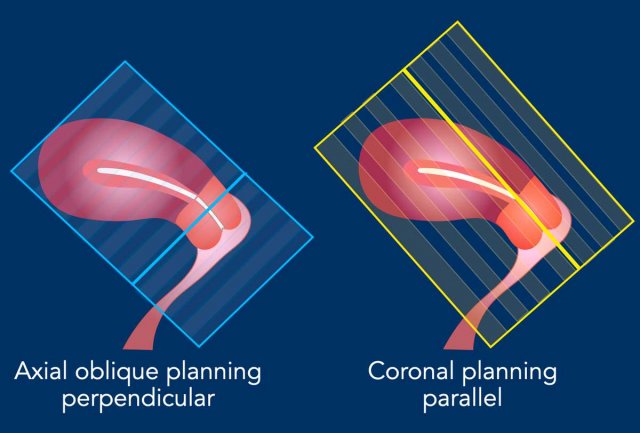
Sequence planning
The MR sequences are planned relative to
the long axis of the cervical canal.
The axial plane is perpendicular to the long axis of the cervical canal.
The coronal plane is parallel to the long axis of the cervical canal.
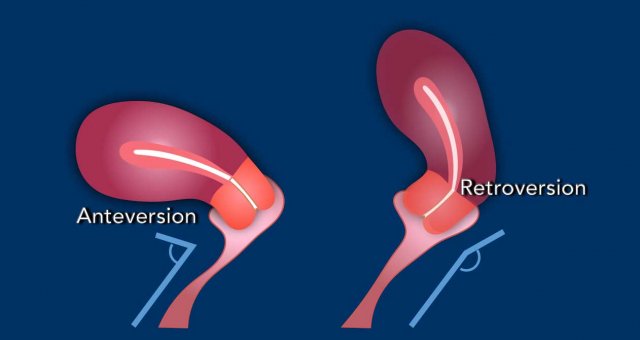
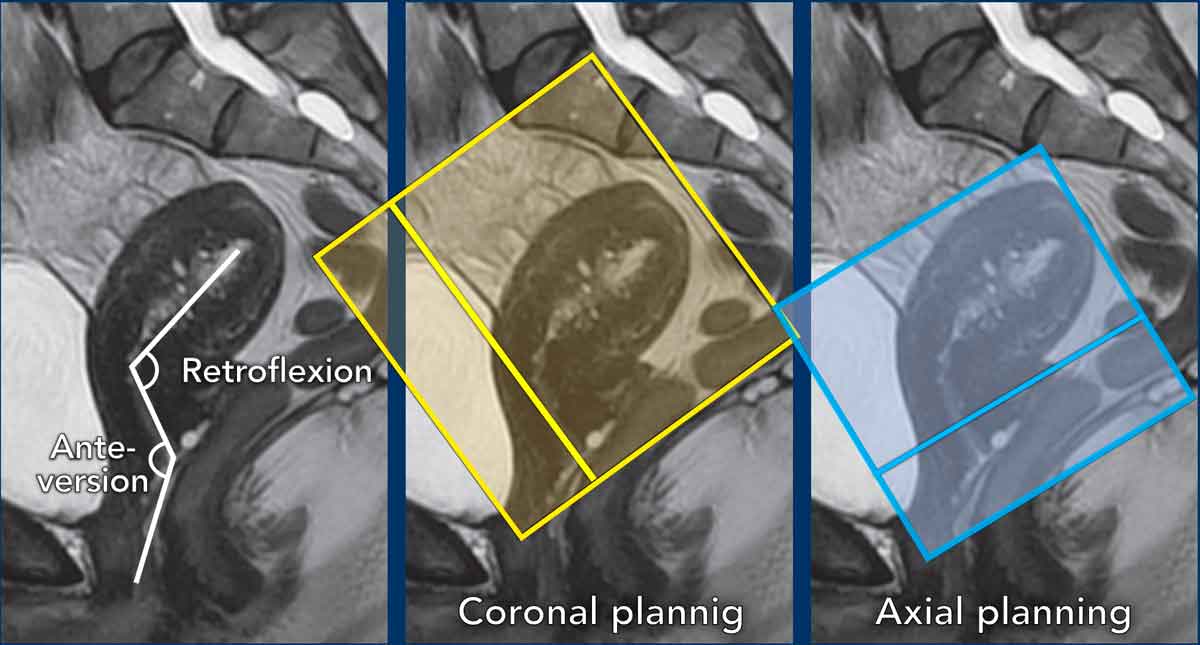
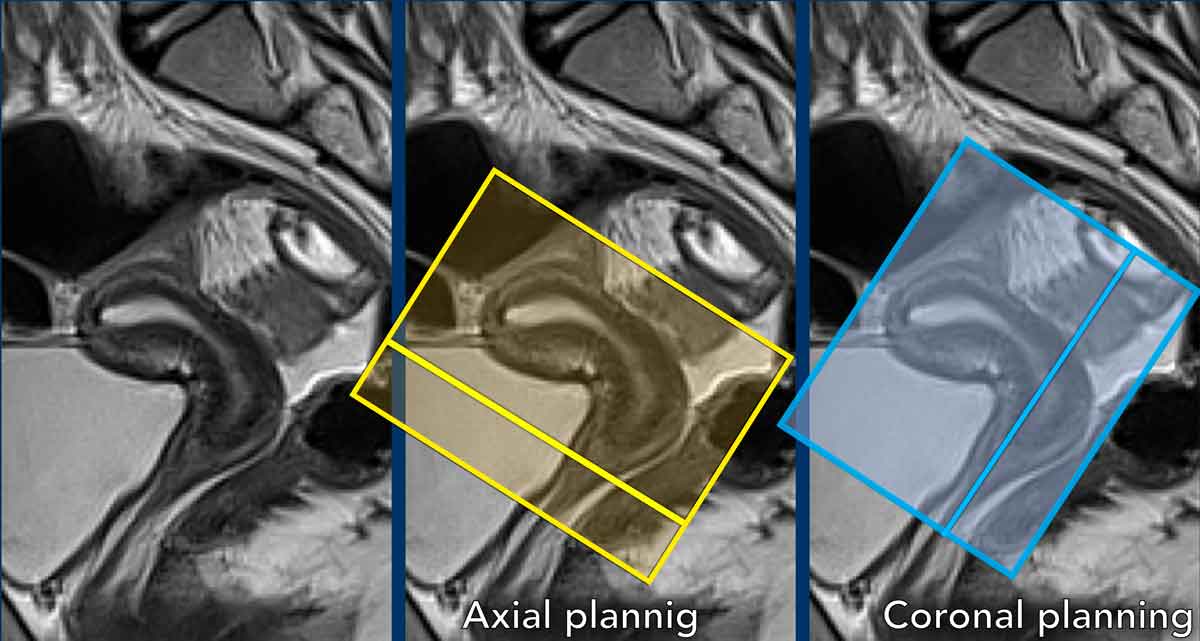
Pitfall: variations in cervical anatomy
The position of the cervical canal needs to be taken into account and the perpendicular and parallel MRI sequences need to be planned accordingly.
Example showing
how flexion, and in particular version impact sequence planning.
In this case
there is anteversion of the cervix and retroflexion of the uterus.
Remember that in
cervical cancer, the axial sequences are planned perpendicular to the cervical
canal.
Another
example showing the cervix in retroversion and the uterus in anteflexion.
See how
this variation in position impacts corresponding sequence planning.
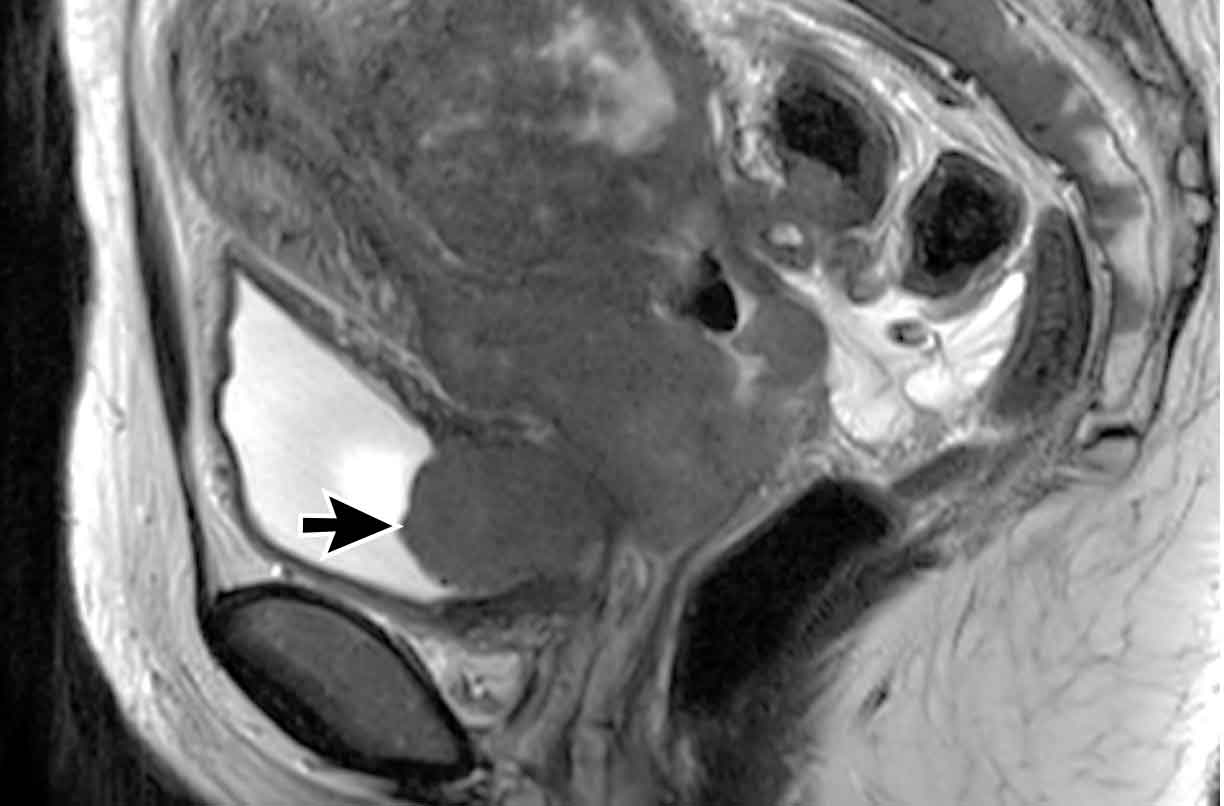
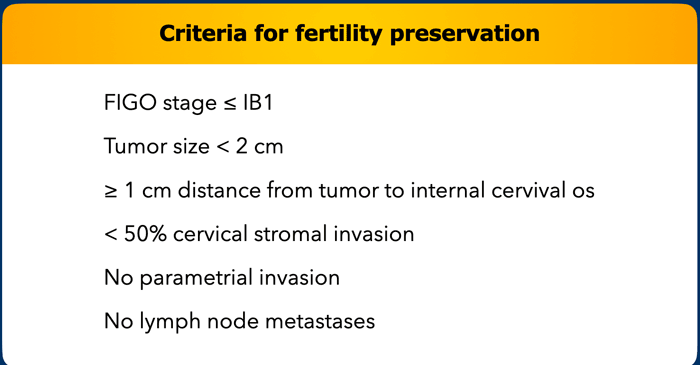
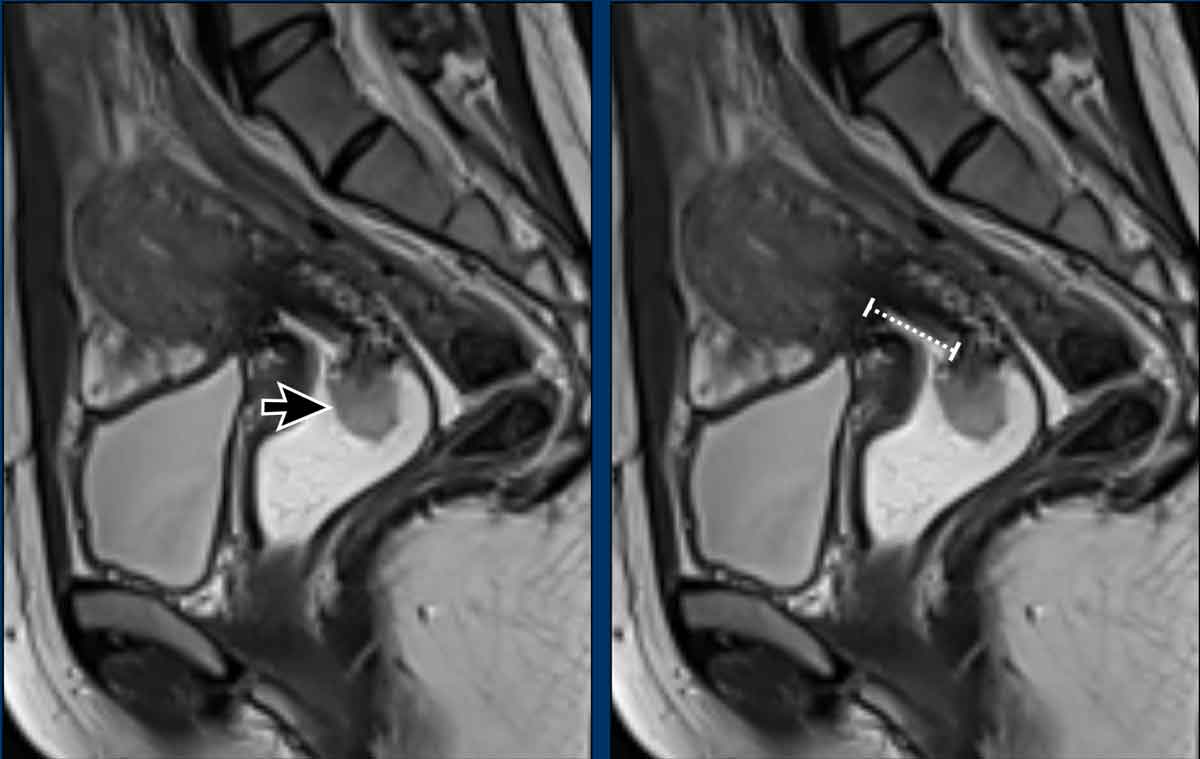
Fertility preservation
Fertility preserving surgery (trachelectomy) can be offered in selected patients with early stage cervical cancer, based on the criteria shown in the Table.
Example showing how to assess the distance to internal
cervical os
The image shows an exophytic cervical tumor.
The distance from the tumor to the internal os measured at
the stalk of the lesion is > 1cm.
The patient was eligible to trachelectomy.
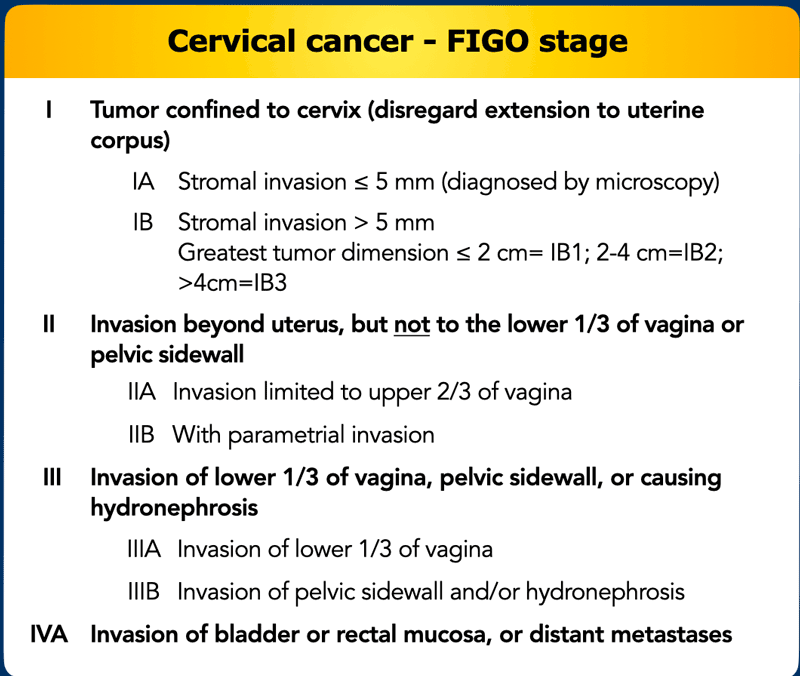
FIGO stage
The International
Federation of Gynaecology and Obstretrics (FIGO) staging system that is most
commonly used to stage cervical cancer was traditionally designed as a clinical surgical staging system.
However, current evidence and clinical guidelines
recommend to include imaging findings (in particular MRI) for staging and
treatment planning as it provides crucial information on tumor size and depth,
extent of invasion into surrounding organs and structures, and lymph node
status, which are essential in choosing the most appropriate treatment
strategy.
An overview of the current 2023 FIGO stages for cervical cancer is
provided in this Table.
We refer readers to the complete FIGO guidelines for more detailed
info (4).
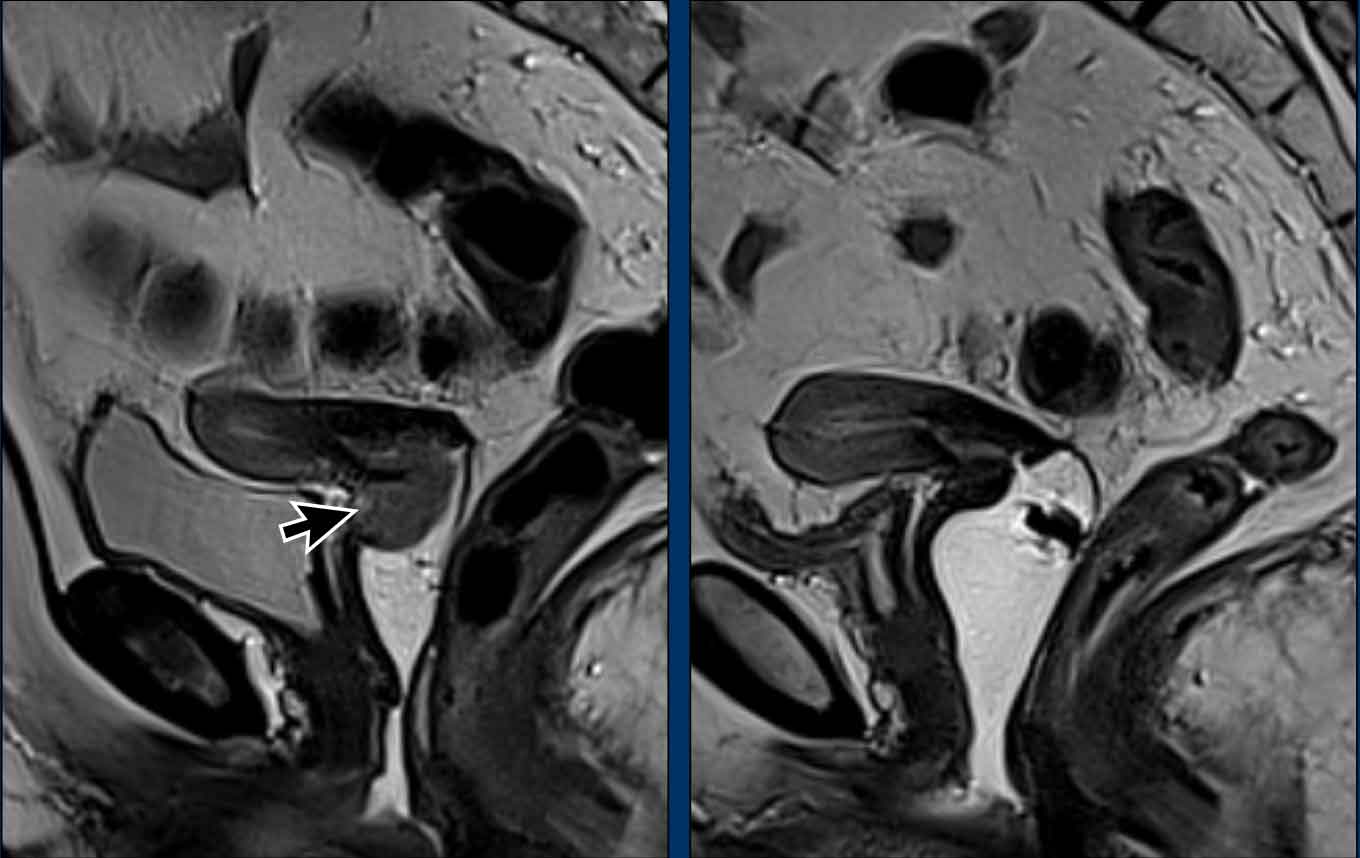
Response assessment
Most cervical cancer patients (stage ≥ IB) undergo CRT followed by
brachytherapy.
In the majority this results in a complete response as shown in
this example.
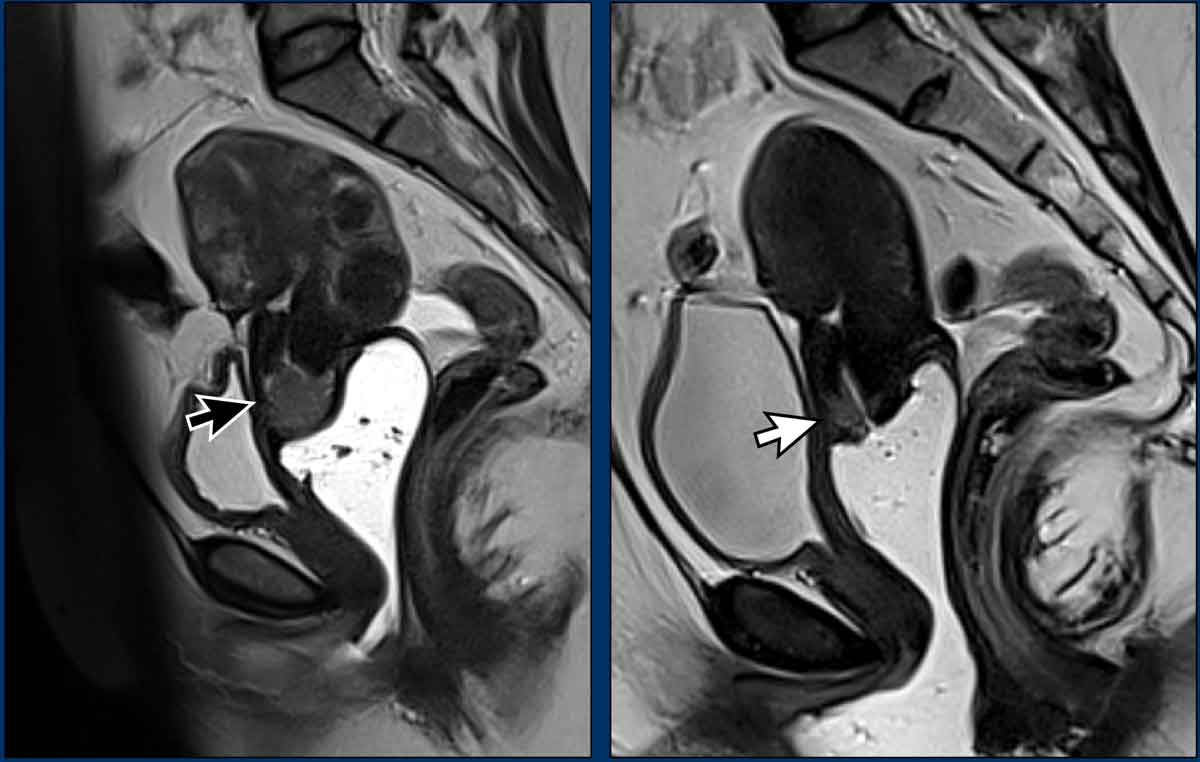
Images
The pre-treatment MRI on the left shows an intermediate signal
exophytic cervical mass.
The post-treatment MRI on the right shows that the tumor is
completely replaced by hypointense fibrosis.
No intermediate tumor signal
remains.
DWI can help in confirming the absence of tumor.
In case of a compete
response, no further surgery is required.
Note that in this case imaging was performed after the
introduction of endovaginal gel.
This is not routinely recommended but can be considered to
help in the assessment of potential upper vaginal invasion.
In a minority of cases the standard treatment of CRT with brachytherapy is not
sufficient and residual disease is suspected, as shown in this example.
Images
The pre-treatment MRI on the left shows an intermediate signal exophytic
cervical mass (black arrow).
The post-treatment MRI on the right shows a small
but clearly visible residual
intermediate T2 signal mass, indicating that the tumor has not been replaced
completely by fibrosis (white arrow).
The patient was referred to surgery,
which is the standard treatment for patients with incomplete response after CRT
+ brachytherapy.
DWI can aid in the detection of residual tumor after CRT.
Note that the recommended timing to evaluate response after CRT is 4 to 6 weeks after completion of treatment.
If the post-treatment MRI findings are inconclusive and there is doubt whether the patient has undergone a complete response or may still have a minor tumor remnant, patients are often further followed and response evaluation including MRI will be repeated (for example after an additional x months follow-up)
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.