Nonvascular Mediastinal Masses
Marilyn J. Siegel and Valerie Niehe
Mallinckrodt Institute of Radiology, St. Louis, MO and the Medical Centre Haaglanden in the Hague, the Netherlands
Publicationdate
This review is based on a presentation by Marilyn Siegel and was adapted for the Radiology Assistant by Valerie Niehe.
Marilyn Siegel is specialized in pediatric and chest radiology.
In this review we will discuss the most common non-vascular mediastinal masses in the chest.
In Pediatric Chest CT part II we will discuss the most common vascular anomalies of the aorta, pulmonary vessels and systemic veins in the chest.
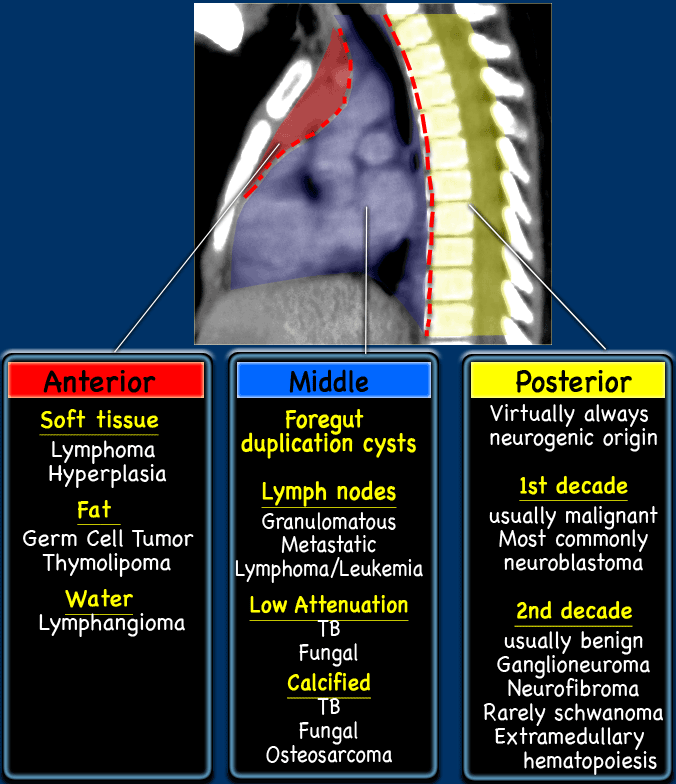
Differential diagnosis
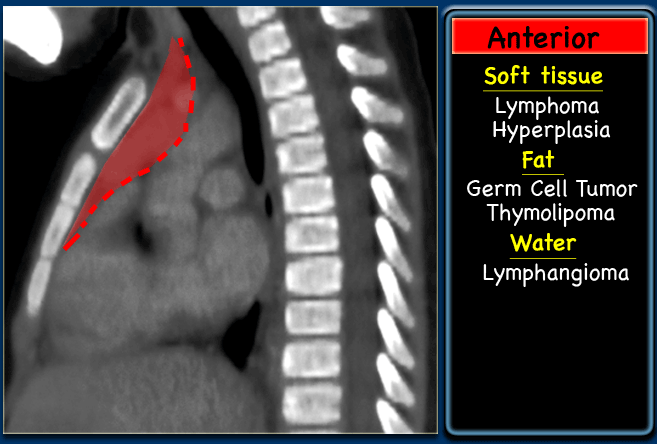
The differential diagnosis of a mediastinal mass is based on identifying its location in anterior, middle or posterior mediastinum and attenuation: soft tissue, fat, fluid and enhancement.
Normal anatomy
Thymus
In infants and young children (
In older children, the thymus gradually assumes a triangular or arrowhead configuration with straight or concave margins.
By 15 years of age it is triangular in nearly all individuals.
Marked lobularity of the thymus is always abnormal.
In prepubertal children, the thymus is homogeneous.
The attenuation value is equal to that of skeletal muscle.
In adolescents it may be heterogeneous, containing areas of fat.
Anatomic variations include extension into the posterior mediastinum or upper neck.
Clues to the diagnosis are:
- No mass effect
- Contiguous with normal thymus
- Extends between superior vena cava and trachea
The figure shows a thymus that extends cranially to the brachiocephalic vessels.
It is contiguous with the normal thymus and extend between the superior vena cava and the trachea.
There is no mass effect.
Normal Lymph nodes
There are no well-established data concerning size of normal lymph nodes in infants and young children.
Mediastinal lymph nodes are generally not seen on CT prior to puberty.
The nodes should then not exceed 1 cm in the widest dimension.
The azygoesophageal recess is dextroconvex in children younger than 6 years of age, straight in children between 5 and 12 years of age, and concave in adolescents and adults.
Recognizing the normal dextroconvex appearance is important so that it is not mistaken for lymphadenopathy.
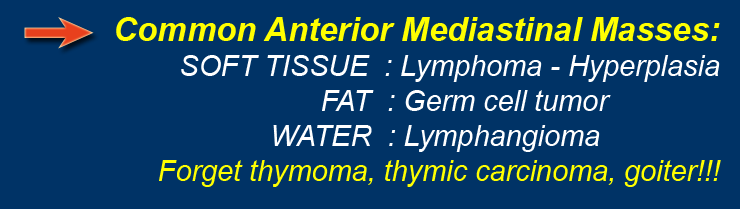
Anterior Mediastinal Masses
Anterior mediastinal masses are usually of thymic origin.
- Soft tissue: Lymphoma and Thymic hyperplasia
- Fat: Germ Cell Tumor.
- Water density: Lymphangioma
Hodgkin lymphoma
Lymphoma is the most common anterior mediastinal mass in children, with Hodgkin lymphoma occurring three to four times more frequently than non-Hodgkin lymphoma.
Calcifications or cystic areas, due to ischemic necrosis consequent to rapid tumor growth, can be seen.
Lymphadenopathy from lymphoma has varied appearances, ranging from mildly enlarged nodes in a single area to large conglomerate soft tissue masses in multiple regions.
Thymic enlargement and lymphadenopathy show minimal if any enhancement after intravenous contrast.
Additional findings include airway narrowing and compression of vascular structures.
Hodgkin lymphoma in children is more common in the second decade of life.
The lymphomatous mass is most common located in the anterior mediastinum and reflects lymphadenopathy or infiltration and enlargement of the thymus.
The enlarged thymus has a quadrilateral shape with convex, lobular lateral borders.
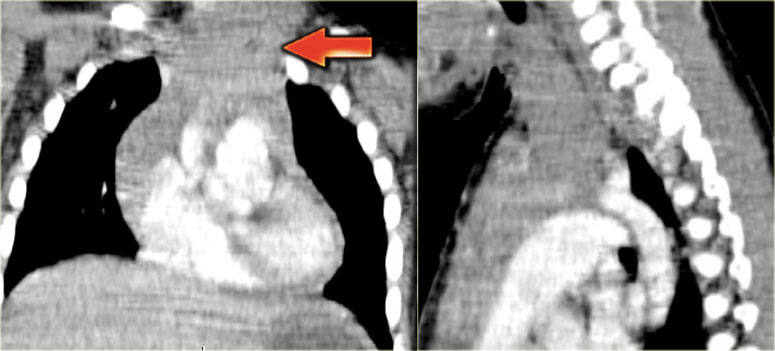
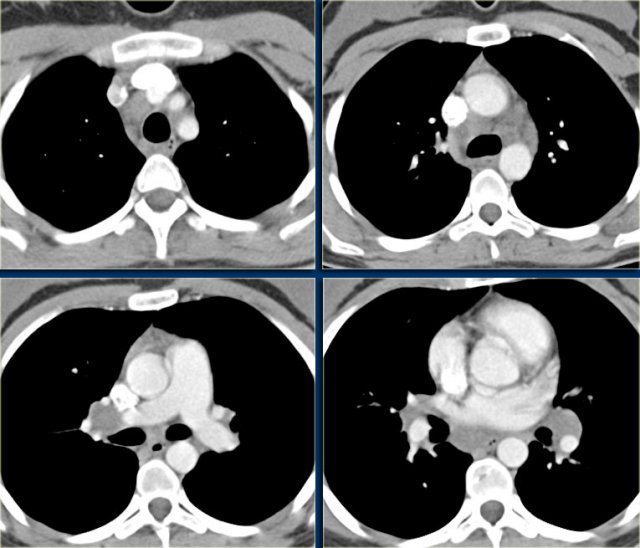
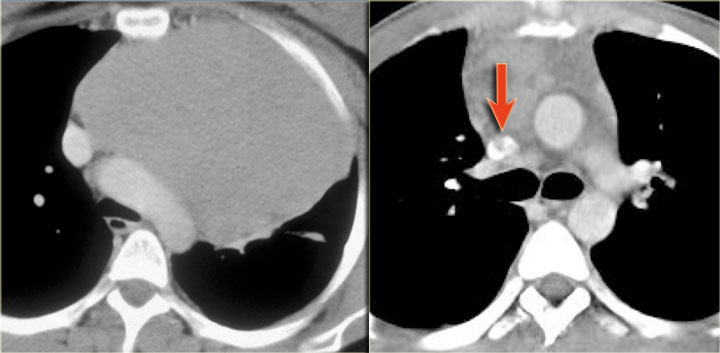
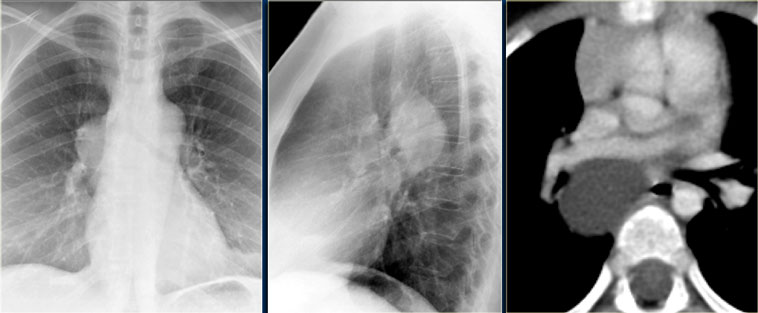
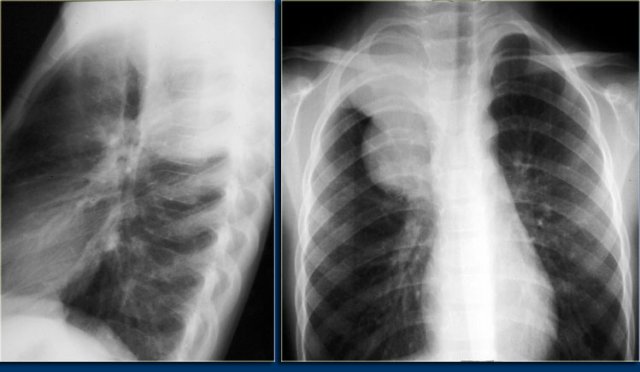
The chest film shows the typical features of Hodgkin lymphoma, e.g., an anterior mediastinal mass.
The CT-images of the same patient show a large soft tissue mass in the anterior mediastinum, which arises in the thymus.
There is associated paratracheal adenopathy (arrow).
Two more cases of Hodgkin lymphoma.
Again these cases show an anterior mediastinal mass and paratracheal adenopathy.
Non-Hodgkin lymphoma
Non-Hodgkin disease in children occurs in the first and second decade of life.
The disease usually involves the nodes in the chest (paratracheal, subcarinal and hilar).
The extension of the disease is not contiguous, it can skip a location.
Non-Hodgkin disease, in contrast to Hodgkin disease, often spares the thymus.
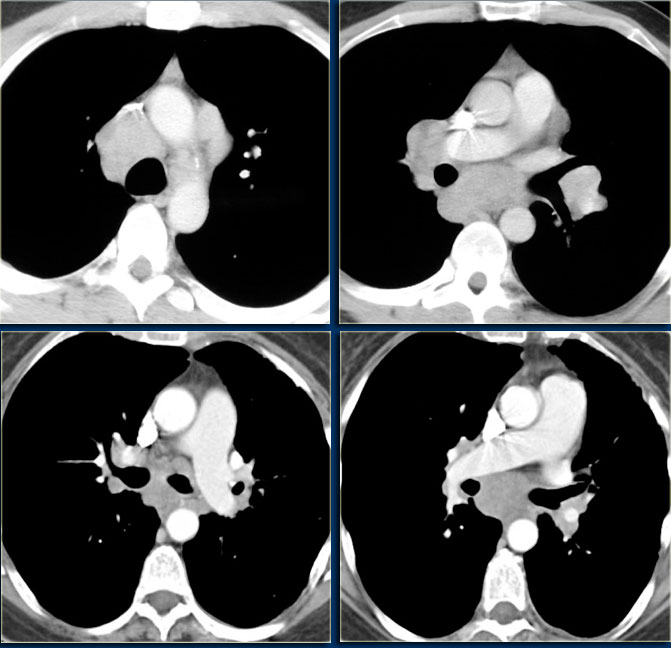
In this case, enlarged lymph nodes are seen in the right paratracheal , hilar and subcarinal areas.
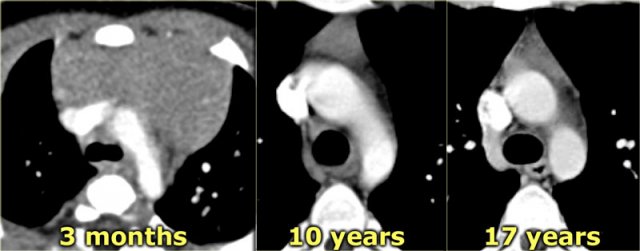
Thymic hyperplasia
Thymic hyperplasia is another cause of thymic enlargement.
In childhood, thymic hyperplasia is most often 'rebound' hyperplasia associated with chemotherapy, particularly therapy with corticosteroids.
Rebound hyperplasia may be observed during the course of chemotherapy or after therapy completion and occurs 3 to 10 months after the start of chemotherapy.
The mechanism of hyperplasia is believed to be initial depletion of lymphocytes from the cortical portion of the gland due to high serum levels of glucocorticoids, followed by repopulation of the cortical lymphocytes when the cortisone levels return to normal.
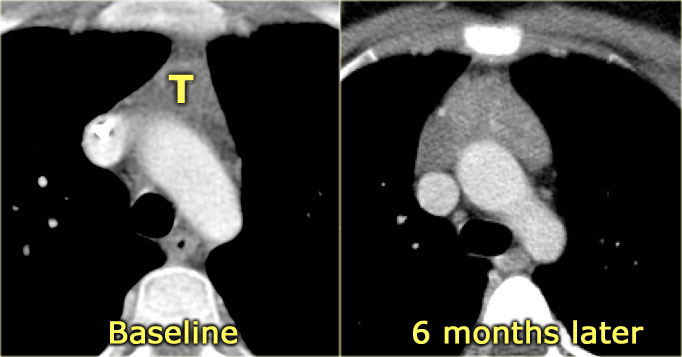
On CT, hyperplasia appears as diffuse enlargement of the thymus, with preservation of the normal triangular shape.
The definition of thymic hyperplasia is a > 50 % increase in volume of the thymus.
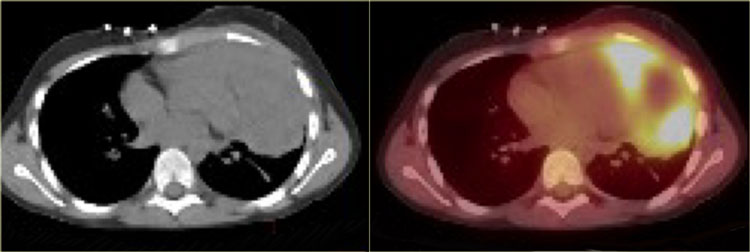
CT, MRI of PET cannot differentiate rebound hyperplasia from infiltration of the thymus by tumor.
The absence of other active disease and a gradual decrease in thymus size on serial CT's supports the diagnosis of rebound hyperplasia.
The thymus usually returns to its normal size in 3 to 6 months.
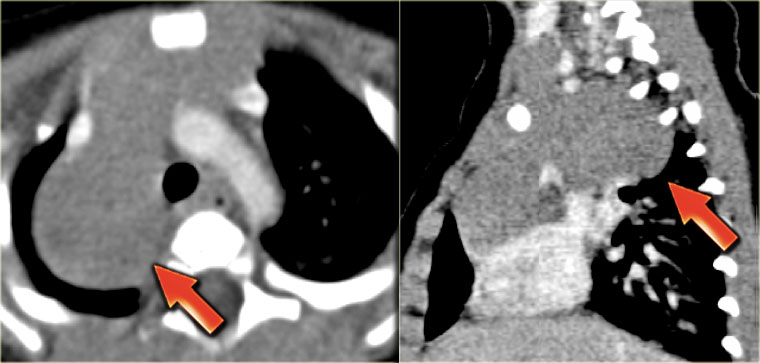
Thymoma
Thymomas are common and account for 20% of mediastinal neoplasms.
Thymic carcinomas are extremely rare and acount for less than 1% of all thymic tumors.
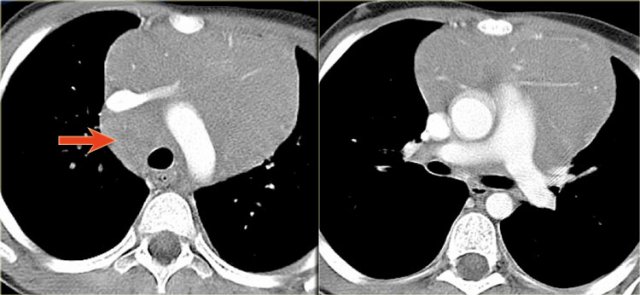
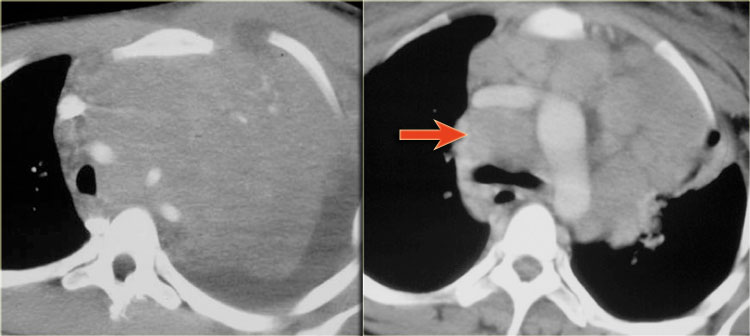
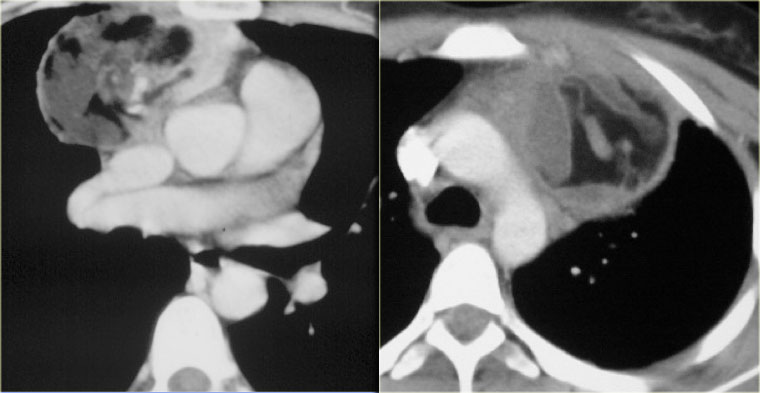
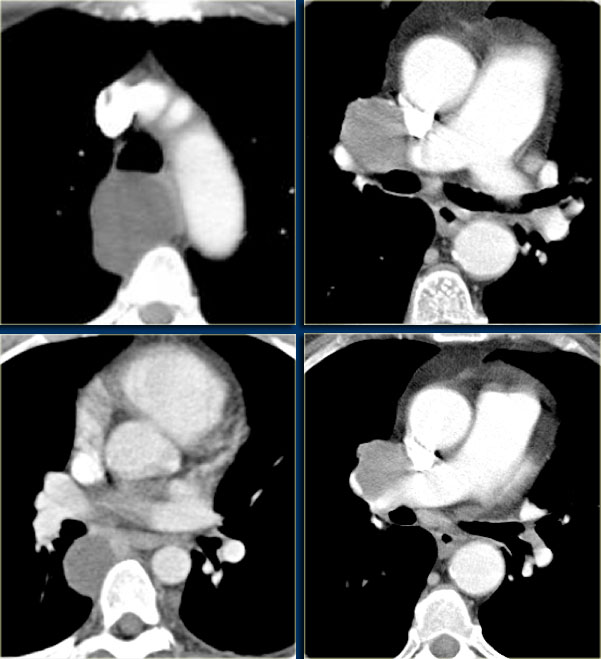
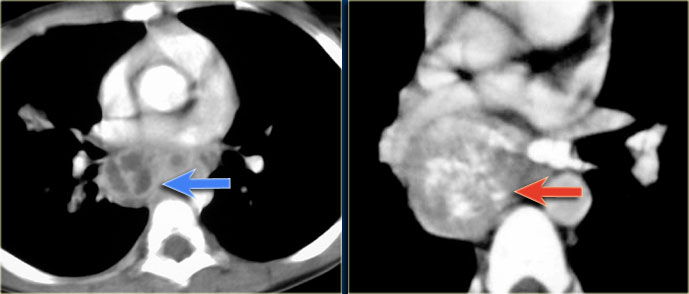
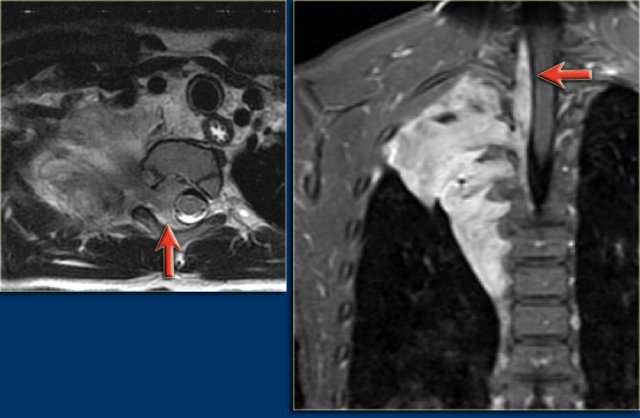
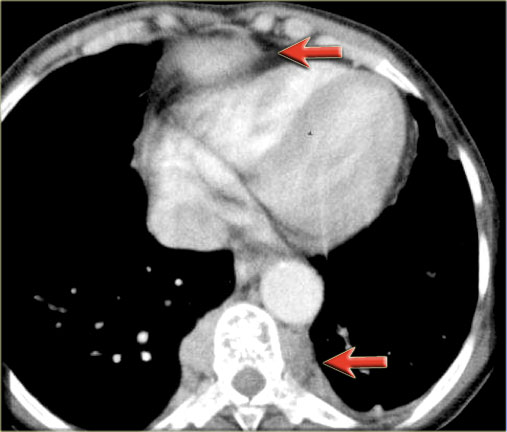
The images show a thymoma on the left and a carcinoma on the right.
The thymic carcinoma has invaded the superior vena cava (arrow).
Germ-cell tumors
Germ-cell tumors are the most common cause of a fat containing lesions in the anterior mediastinum and the second most common cause of an anterior mediastinal mass in children.
Approximately 90 % are benign germ-cell tumors.
Most arise in the thymus.
On CT, a benign teratoma is a well-defined, thick-wall cystic mass containing a variable mixture of water, calcium, fat and soft tissue.
The soft tissue component in benign teratoma is minimal.
Size is not an indicator of malignancy.
Mature teratomas can be very large and still be benign.
Malignant teratomas make up 10 % of all teratomas.
They tend to have irregular or nodular walls and a predominance of soft tissue components.
They also may show pulmonary or liver metastases and chest wall invasion.
The most common nonteratomatous germ-cell tumors in the pediatric population are choriocarcinoma, embryonal cell cancer and yolk-sac cancer.
Thymolipoma
Thymolipoma is an infrequent fat-containing thymic tumor.
At CT, it appears as a heterogeneous mass containing fat and soft tissue elements.
Calcifications are absent.
Thymolipoma does not have a capsule and does not have any mass effect.
Lymphangioma or Cystic hygroma
Lymphangiomas are developmental tumors of the lymphatic system.
In the mediastinum they are almost always an inferior extension of a cervical lymphangioma.
Isolated mediastinal involvement is rare.
Lymphangioma is a benign, but aggressive tumor that shows mass effect and may encase vessels and other structures.
It typically affects infants younger than 6 months of age.
At CT it appears as nonenhancing, thin-walled, multiloculated mass with near water attenuation.
MRI may sometimes be used to better delineate the extension of the lesion.
The MRI in this patient shows a cystic mass in the neck extending into the right axilla and mediastinum.
The tumor encases vessels.
The presence of contrast enhancement of the wall or internal septations suggests superimposed infection or a hemangiomatous component.
Thymic cysts
Thymic cysts are usually congenital lesions resulting from persistence of the thymopharyngeal duct.
They can also occur after thoracotomy.
Typically, they are thinwalled, homogeneous masses of near water attenuation on CT.
The attenuation value may be higher than that of simple cysts when the contents are proteinaceous or hemorrhagic rather than serous.
In children thymoma, thymic carcinoma and goiter are so uncommon, that you should put them very low in your differential diagnosis.
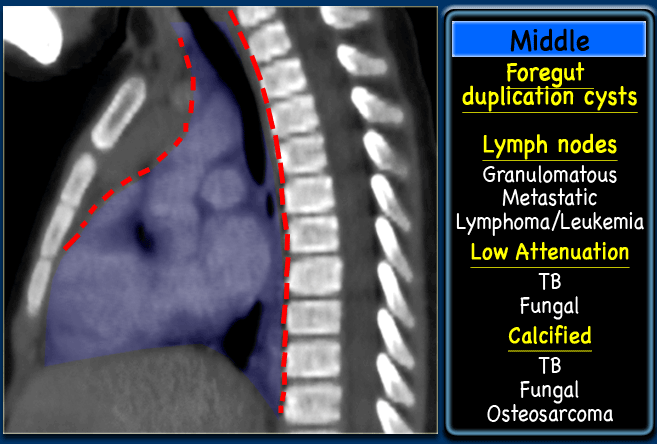
Middle Mediastinal masses
In the middle mediastinum we will find foregut duplication cysts or lymph nodes.
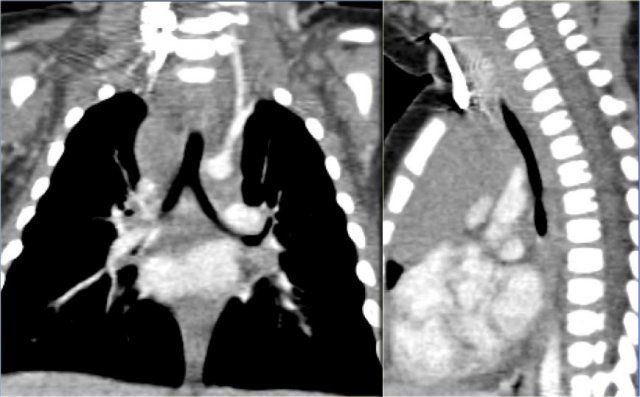
Foregut cysts in the middle mediastinum are classified as bronchogenic or enteric.
Bronchogenic cysts are lined by respiratory epithelium and most are located in the subcarinal or right paratracheal area in close proximity to the trachea or bronchus.
Enteric cysts are lined by gastrointestinal mucosa and are located in a paraspinal position in the middle to posterior mediastinum near the esophagus.
Bronchogenic Cysts
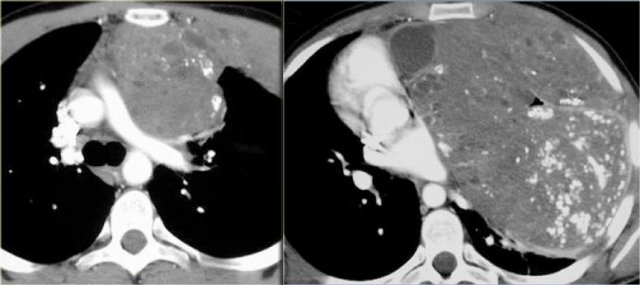
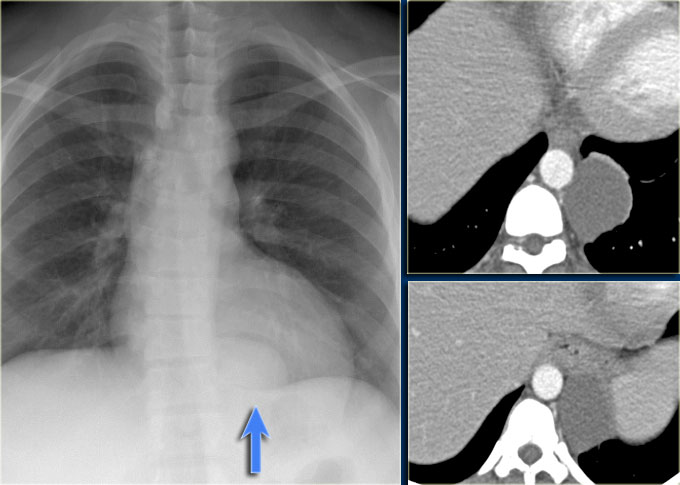
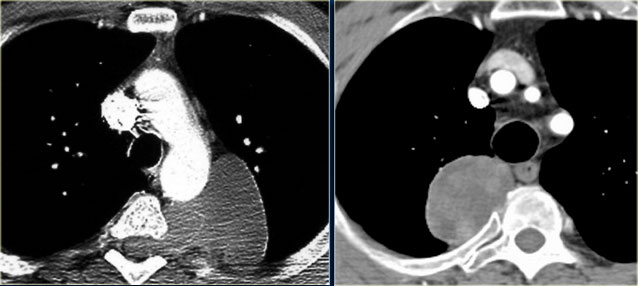
The images show a well defined lesion of water attenuation in close proximity to the trachea or bronchus, which is typical for a bronchogenic foregut cyst.
The images show more examples of bronchogenic cysts and their close proximity to the airway.
Enteric foregut cyst
The images show a well defined lesion of water attenuation in the lower mediastinum in close proximity to the esophagus, which is typical for an enteric foregut cyst.
Mediastinal lymphadenopathy
Mediastinal lymphadenopathy is usually caused by lymphoma or granulomatous disease.
Metastatic disease from rhabdomyosarcoma, osteosarcoma or a Wilms tumor, is also a possibility.
On CT, adenopathy can appear as discrete, round, soft tissue masses or as a single soft tissue mass with poorly defined margins.
Calcification within lymph nodes suggests old healed granulomatous disease, fungal infection or metastatic disease from osteosarcoma.
Areas of low attenuation suggest tuberculosis or fungal infection.
Posterior Mediastinal masses
Posterior mediastinal masses are of neural origin in approximately 95 % of cases and may arise from sympathetic ganglion cells (neuroblastoma, ganglioneuroblastoma or ganglioneuroma) or from nerve sheaths (neurofibroma or schwannoma).
In the first decade of life they are usually malignant, most commonly neuroblastoma.
In the second decade or life they are usually benign (ganglioneuroma, neurofibroma, rarely schwanoma).
Neuroblastoma
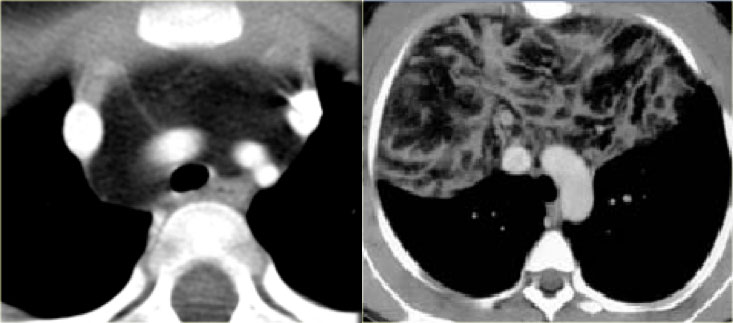
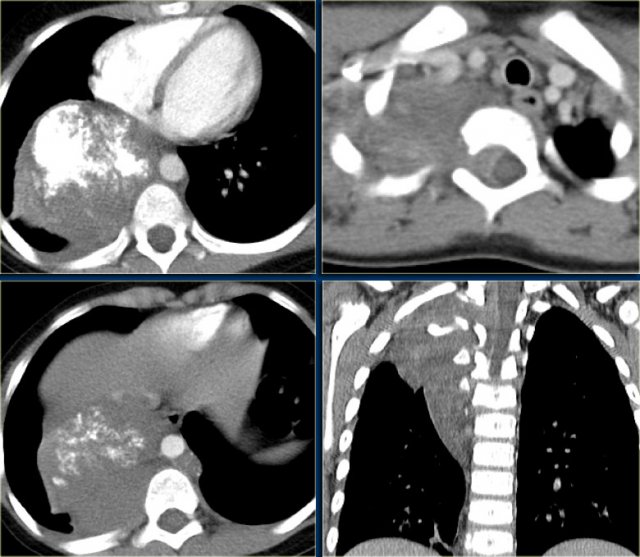
Neuroblastoma typically is fusiform in shape, of soft tissue density; 50% of thoracic tumors have calcifications.
Neuroblastoma grows over several interspaces and frequently invades the vertebral canal.
The CT-images show a calcified mass in the posterior mediastinum extending over several vertebrae, which grows into the vertebral canal.
On the MR-images the invasion of the vetebral canal is better seen (arrows).
Other Neurogenic Tumors
In the 2nd decade other neurogenic tumors are seen like
ganglioneuroma, neurofibroma and rarely schwanoma.
They are round or oval in shape, smaller in size than ganglion cell tumors and usually extend over only one or two vertebrae.
Both types of tumor may cause pressure erosion of a rib and invade the spinal canal.
Neurenteric Cyst
Neurogenic cysts contain neural and gastrointestinal element.
They are commonly associated with vertebral anomalies and scoliosis. The cyst does not communicate with CSF.
The cyst is well demarcated and has a near water attenuation value on CT and water signal intensity on MRI, as shown in the case on the left.
Extramedullary hematopoiesis
Extramedullary hematopoiesis accounts for less than 0.1 % of the lesions in the posterior mediastinum.
It is characterized by formation of blood elements outside of the bone marrow. It occurs with severe anemia.
On CT it is seen as a paravertebral mass and occurs with coarse bone trabeculation in the adjacent vertebra.