Peritoneal Carcinomatosis
Thijs van Oudheusden
Department of Radiology, Catharina Cancer Institute, Eindhoven in the Netherlands
Peritoneal carcinomatosis is metastatic disease, that has spread to the abdominal cavity.
It is characterized by metastatic deposits along the peritoneal surface.
Treatment options dependent on the volume, the
pattern of spread and the presence of other abdominal or extra-abdominal
metastases.
The imaging findings in peritoneal carcinomatosis can be overwhelming, but in some cases be very subtle.
This explains why the disease is sometimes not detected and frequently underestimated.
In this article we describe which areas in the abdomen will need your special attention in order to diagnose peritoneal carcinomatosis and to score the extend.
Introduction
Peritoneal Anatomy
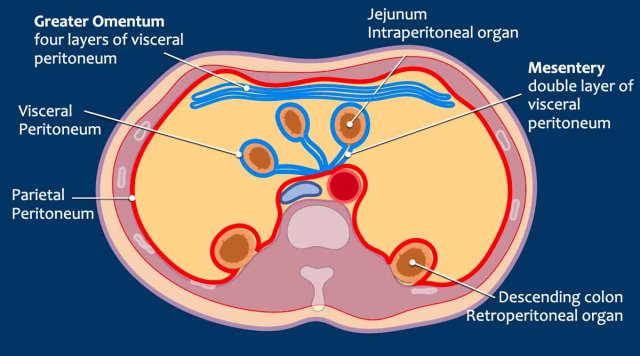
The peritoneum consists of two layers.
The parietal peritoneum is the outer layer which adheres to the anterior and posterior abdominal wall (in red).
The visceral peritoneum is the inner layer which lines the abdominal organs (in blue).
The mesentery has a double layer of peritoneum.
The greater omentum is a large fold of four layers of visceral peritoneum.
It extends as a double layer from the greater curvature of the stomach, passing in front of the small intestines and doubles back to ascend to the transverse colon.
It consists of the gastrocolic ligament, which connects the stomach to the transverse colon, and the gastrosplenic ligament, which connects the stomach to the spleen.
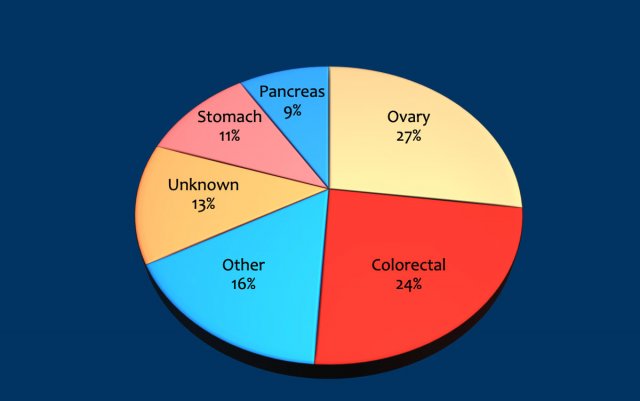
Peritoneal carcinomatosis is most commonly seen in patients with ovary, colorectal, gastric and pancreatic cancer, but almost any primary tumor can present with peritoneal carcinomatosis (tabel).
The synchronous form of peritoneal carcinomatosis - primary cancer and peritoneal spread present at the same time - is rather common and ranks 5th in both male and female cancer.
The metachronous presentation - peritoneal cancer as recurrent disease
after primary curative surgery - is also rather common.
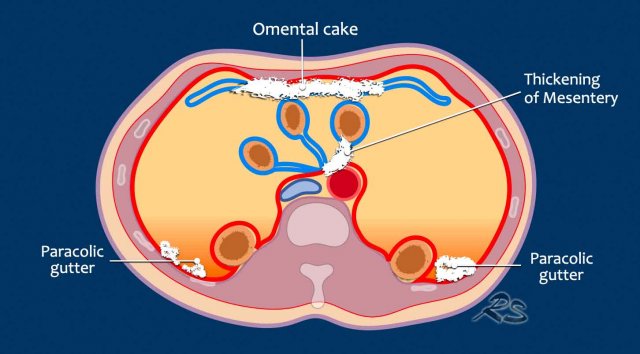
Where to look for Peritoneal Carcinomatosis
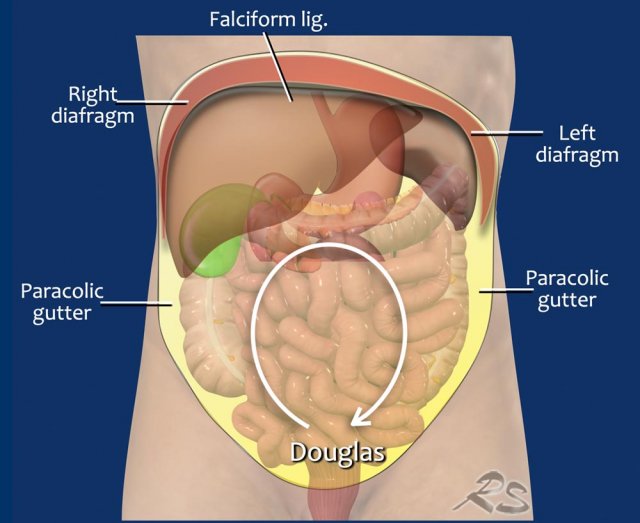
Specific regions are prone as a target for metastatic peritoneal spread.
The reason for this is the physiologically clockwise stream of intra-abdominal fluid which originates from changes in the intraabdominal pressure while breathing.
Tumor cells travel with this current and attach to the peritoneum along the way.
The current flows clockwise along:
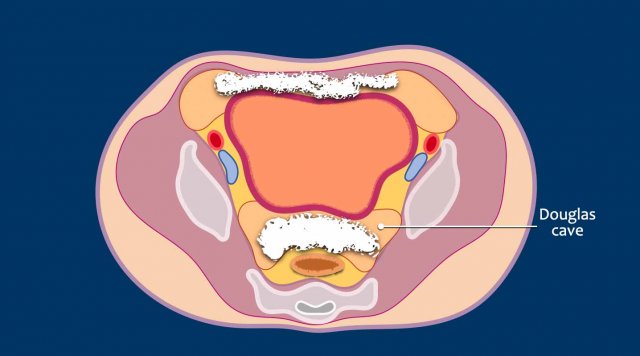
- Rectouterine-rectovesical pouch (Douglas pouch)
- Right paracolic gutter
- Right diaphragm
- Falciform ligament
- Left diaphragm
- Left paracolic gutter and back to Douglas pouch
- Continuous stream through the mesenterial folds and around the omentum.
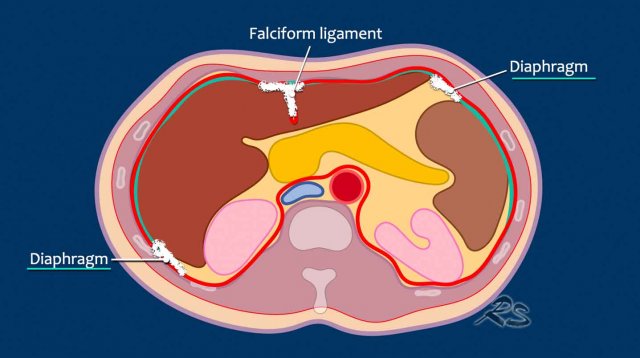
In the upper abdomen the diaphragm and the falciform ligament needs your extra attention.
In the mid abdomen the omentum, mesentery and paracolic gutter needs your attention.
Mesenteric tumor deposits can be well seen when the mesentery is surrounded by ascites.
When patients have a lot of intra-abdominal fat, the mesenteric deposits stand out against the low attenuating surrounding fat.
In the pelvis the most important spot is the rectouterine-rectovesical pouch (Douglas pouch).
Sometimes tumor spread is seen all the way anterior to the bladder, but not on the bladder wall itself, as the bladder is an extraperitoneal organ.
However, the cranial dome of the bladder and the urachus are separated
from the abdominal compartment by a layer of parietal peritoneum which forms a
potential target for tumor cells.
Especially in a full bladder, peritoneal
tumor deposits can be visualized anterior of the bladder against the anterior
abdominal wall.
This is not perivesical
pathology, since the perivesical space is extraperitoneal and does not
communicate with the intraperitoneal cavity.
Imaging Findings
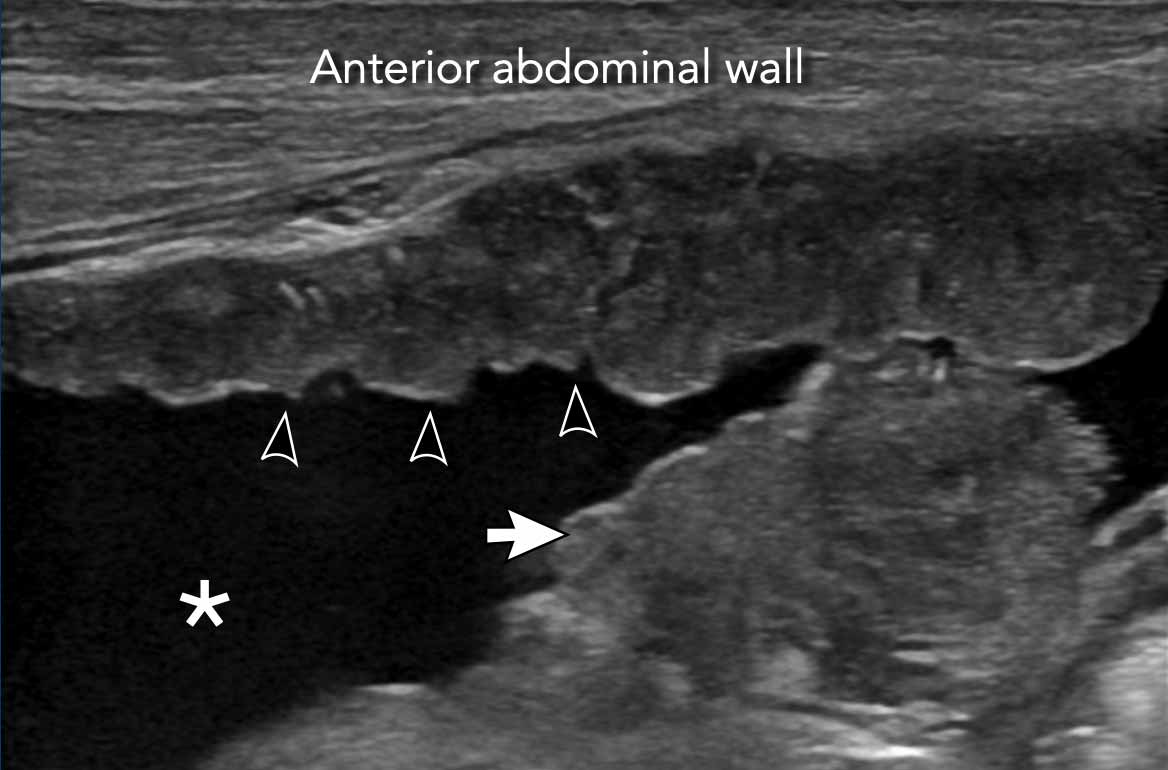
Ascites
The presence of ascites is an ominous finding since peritoneal nodules produce these fluids and could therefore be the first hint that PC is present.
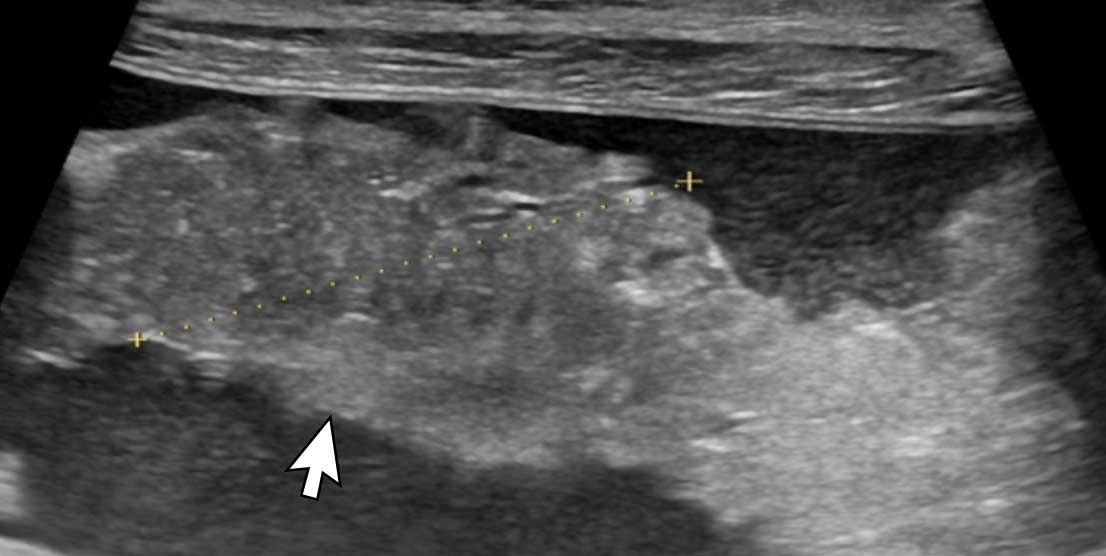
Image
This ultrasound image of a patient who presented with ascites (asterix) demonstrates both tumor deposits on the parietal peritoneum (arrowheads) as well as a large tumor mass on the visceral peritoneum (white arrow).
Thickening of the Mesentery
Both ultrasound and CT can depict the thickened
peritoneal layers of the mesentery.
Especially in the presence of ascites,
the thick mesentery is well appreciated on both image modalities.
Image
There is a small amount of ascites.
Thickened
mesentery is seen connected to a small bowel at the end typical for mesenteric
involvement.
This image is of another patient who presented with ascites.
Image
The thickened mesentery (aterix) is seen connected to a small bowel at the end.
This is typical for mesenteric involvement of peritoneal carcinomatosis.
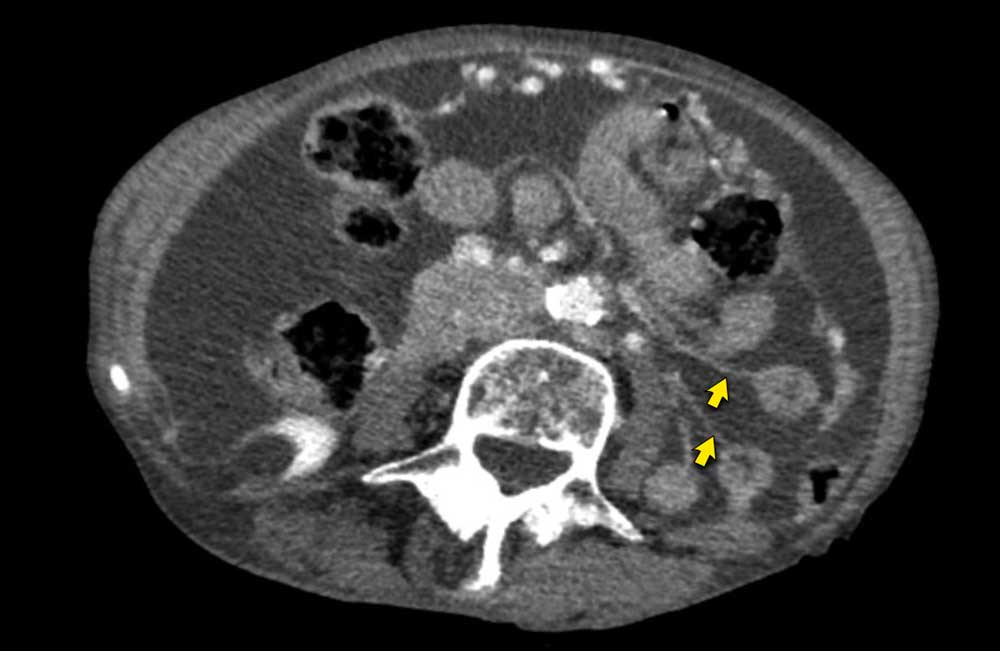
On CT the thickening of the mesentery can also be appreciated.
Image
The thin sheet
like structures are the slightly thickened mesentery.
At the end, a small bowel is attached.
In the absence of ascites you would not be able to detect this subtle thickening.
As a rule of thumb, being able to visualize the mesentery is an ominous feature, especially if nodularity is present.
In the absence of large amounts of ascites it is more difficult to detect thickening of the mesentery.
Look for
nodular or thickened linear lesions surrounded by fat on the mesenteric side of the bowel.
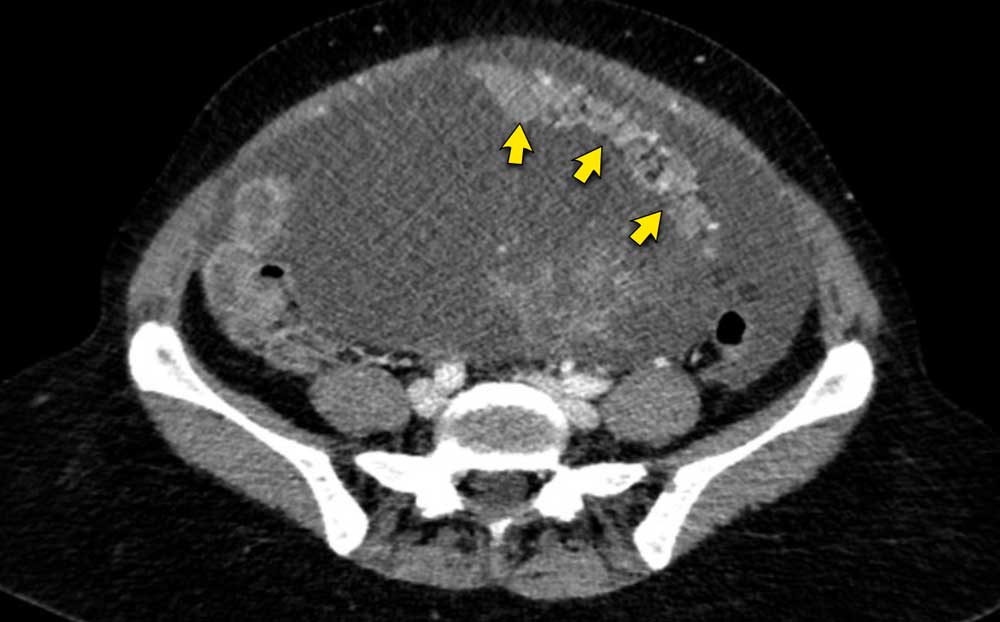
Image
CT image of a patient with peritoneal carcinomatosis.
A small amount of ascites is present in the anterior right corner.
Thick nodular lines perpendicular to the bowel are present.
This represents extensive mesenteric involvement (arrows).
Omental cake
The omentum is one of the first intra-abdominal
structures that is involved by peritoneal cancer.
The so-called omental cake
is the result of extensive tumor deposits in the greater
omentum.
It has a very typical appearance on both ultrasound and CT.
Image
Ultrasound image of an omental cake floating in ascites.
An omentum with peritoneal cancer is nodular and heterogeneous compared to the normal omentum.
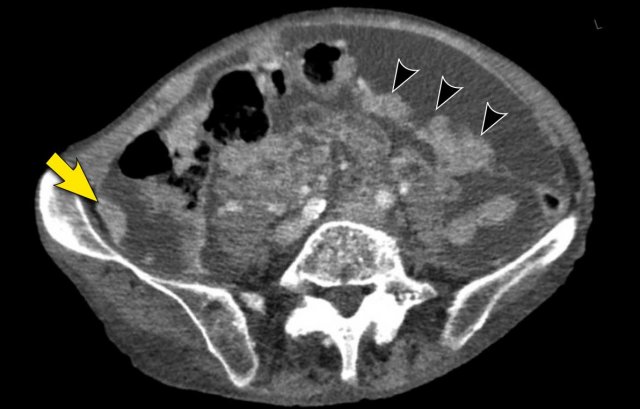
Image
CT image of an omental cake floating in ascites (arrows).
The omentum is located in the left abdomen extending from the outer gastric border downwards.
The image shows a cleary heterogenous nodular appearance typical for omental cake.
The white dots in the omentum are probably vessels.
Paracolic gutter
Any location inside the abdomen covered by peritoneum can be target for peritoneal deposits.
Typical other locations are the paracolic gutter, the rectovesical or rectouterine space, the falciform ligament and on the abdominal side of the diaphragm.
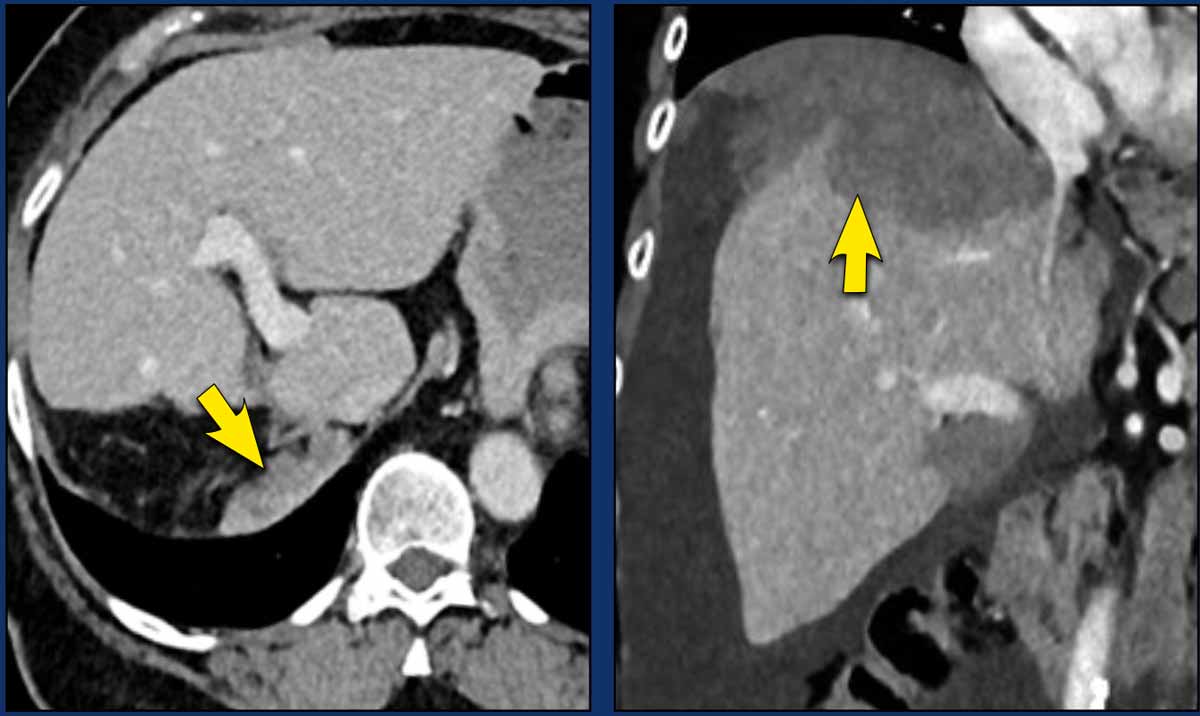
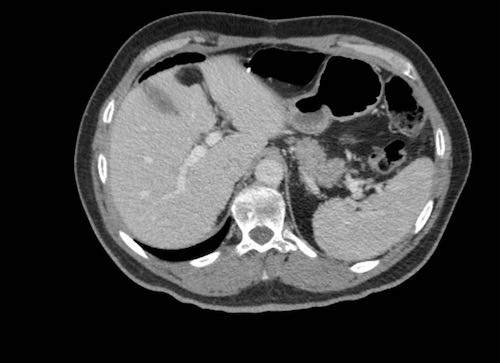
Diaphragm
As a result of respiration, free tumor cells are
sucked against the abdominal side of the diaphragm.
These deposits are usually
underestimated or overlooked on axial images and much better appreciated on
coronal or sagittal views.
In this case, tumor deposits are obvious and cover the liver peritoneum.
Scroll through CT images

Case 1
Scroll through the images.
Can you detect all peritoneal implants?
This patient was operated and the entire peritoneum was covered with miliary tumor deposits.

Case 2
Scroll through the images.
Can you detect all peritoneal implants?
Case 3
Scroll through the images.
Can you detect all peritoneal implants?
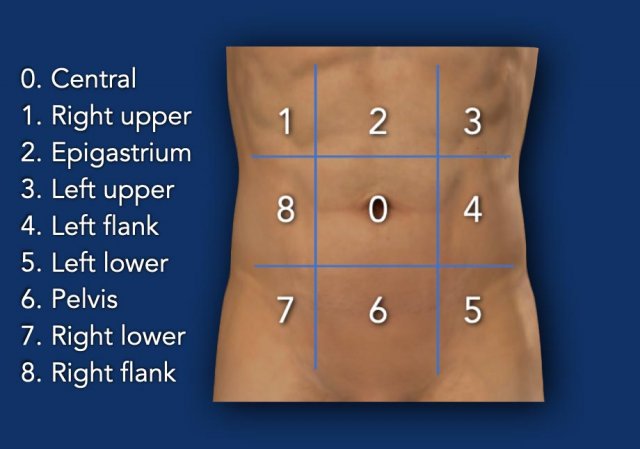
Peritoneal Cancer Index
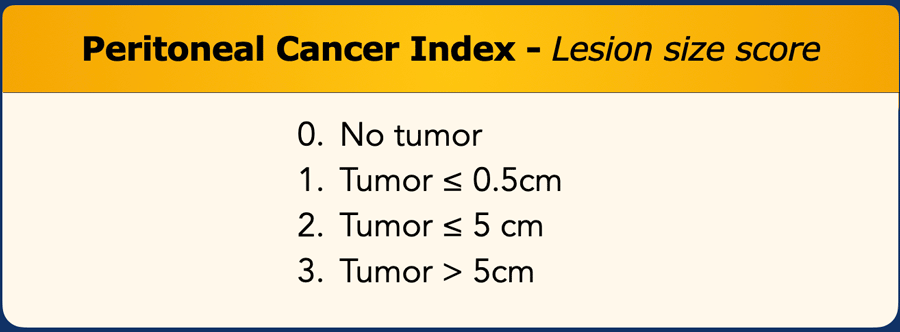
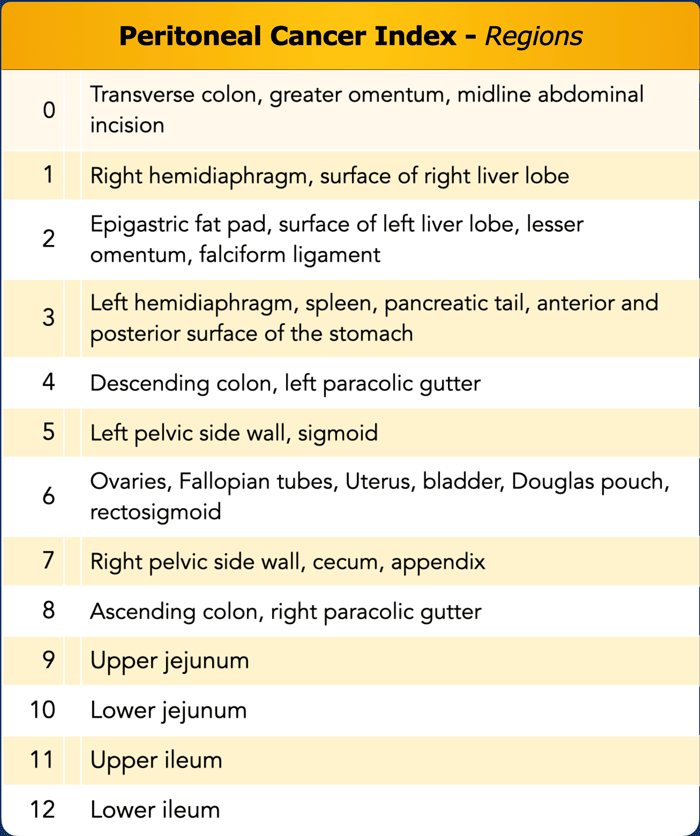
To get an idea of the
extent of disease, the PCI score is a widely used scoring system.
The abdominal cavity is divided into 13
regions.
Regions 0 - 8 are clockwise orientated in the cavity (figure).
Regions 9 -12 represent the proximal and distal jejunum and the proximal and distal ileum.
Especially the mesentery is important to review.
In every region, a score from 0 to 3 is given depending on the lesion size.
In total there are 13 regions and the maximum score is 13 x 3 = 39.
It is important to mention that in case of small “confluent” disease, 3 points should be given even though the thickness is less than 5cm.
The final score level will indicate whether or not a patient is potentially eligible for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS + HIPEC).
For instance a score > 20 in case of a colorectal tumor with peritoneal spread is considered a contraindication for extensive surgery with only little to no survival benefit compared to chemotherapy.
Likewise extensive spread to the small bowel mesentery may render a patient inoperable because of the risk of short bowel, even when other regions are not affected.
Follow up after CRS+HIPEC
Even though the procedure encompasses extensive resections of peritoneal surfaces, there is a high risk of recurrence.
New nodules can grow from both previously unresected peritoneal areas but also from now new “non peritonealized” areas.
Assessing all 13 regions in follow up is a good standardized method to address all these potential areas of recurrence.
Risk factors
Risk factors for metachronous peritoneal carcinomatosis are a high T-stage at primary presentation, tumor perforation, surgical complications at primary resection and failure to undergo adjuvant chemotherapy when initially indicated.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar.
If you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.