How to Differentiate Carotid Obstructions
Adriaan van Es
Leiden University Medical Centre in Leiden, the Netherlands
Publicationdate
In patients with an acute stroke and
an intracranial large vessel occlusion, we need to know if there is carotid
pathology and if so what kind of pathology we are dealing with.
This is important for procedural
planning and the technical execution of endovascular treatment. Furthermore,
carotid artery pathology determines secondary profylaxis with either carotid
endarterectomy, stenting or anti-platelet therapy.
The most common carotid obstruction
is caused by atherosclerosis.
In this article we will discuss how to
differentiate this type of carotid obstruction from an obstruction caused by a
carotid dissection or a pseudo-occlusion
Other pathology that we will discuss
is the floating thrombus, the carotid web and the isolated internal carotid
artery.
An isolated internal carotid artery is an unfavourable configuration of
the circle of Willis which can lead to severe ischemia in case of a ICA
occlusion.
A carotid web is an entity that is increasingly recognized as an
important cause for ischemic stroke in especially young females.
Overview
Atherosclerosis
Atherosclerotic plaques are
mostly located at the level of the
bulbus. Atherosclerosis is usually
bilateral and frequently calcifications
can be seen.
Subtotal stenosis
In a high-grade atherosclerotic stenosis
the flow through the internal carotid is severely decreased and results in a collapse
and consequently a small caliber of the vessel
distal to the occlusion.
Occlusion
In a total occlusion the contrast has a { or curly bracket-like configuration.
Dissection
In the case of a ICA dissection the bulbus is not involved and the
contrast in the proximal ICA has a flame-shaped configuration. The total diameter of the ACI
is widened due to the formation of a mural hematoma. The narrowed eccentric true lumen is surrounded by a
crescent-shaped mural on transversal imaging. The
compressed true lumen can be occluded in case of severe compression.
Pseudo-occlusion
This simulates an occlusion
of the lower cervical part of the internal carotid, but is actually the
result of a stop at the carotid T-top. Contrast that tries to enter the
internal carotid will give a waterpaint appearance due to this outflow
obstruction.
Carotid web
This is a thin shelf-like luminal protrusion of the
intimal fibrous tissue that extends from the posterior aspect of the proximal internal carotid artery bulb into the lumen.
The carotid web is increasingly being associated with ischemic stroke in young
individuals, especially females.
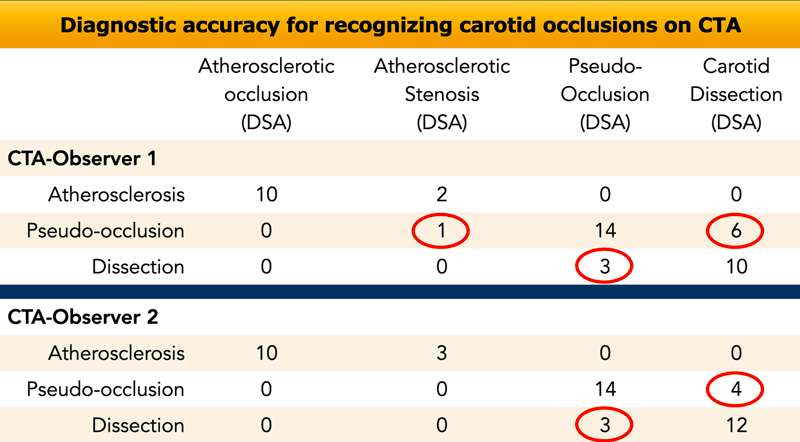
There is a problem diagnosing carotid dissection versus pseudo-obstruction.
In a study in which the CTA-findings
were compared to tDSA (golden standard for carotid lesions), the results showed
that there was a high accuracy in diagnosing atherosclerotic occlusions and
high grade stenoses of the internal carotid artery.
Only one atherosclerotic stenosis was
misdiagnosed as a pseudo-occlusion.
On the other hand pseudo-occlusions were misdiagnosed as carotid dissection and dissections were misdiagnosed as pseudo-occlusions quite frequently (red circles).
In the chapters below we will discuss how to differentiate dissection from pseudo-occlusion.
Tandem occlusions are intracranial occlusions
combined with a severe (>70% ) stenosis or occlusion of the ICA.
They are found
in up to 30% of all patients presenting with a large vessel occlusion.
The accompanying
ICA pathology is not a contra-indication for endovascular therapy for the
intracranial occlusion, regardless of the underlying ethiology of the ICA stenosis/occlusion.
However identifying carotid pathology is important for planning and execution of the endovascular procedure.
Atherosclerosis
Typical findings in an atherosclerotic stenosis or occlusion are:
- Atherosclerotic stenosis of the ACI is mostly located at the level of the bulbus.
- Frequently there are calcified plaques.
- Atherosclerosis is usually a bilateral disease.
These patients are usually
older and have cardiovascular risk factors.
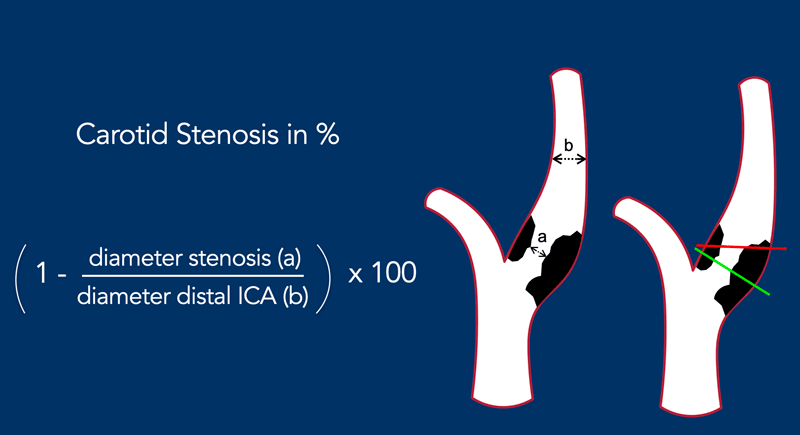
ICA stenosis measurement
The illustration shows the formula for measuring the degree of stenosis according to the NASCET (North American Symptomatic Carotid Endarterectomy Trial).
The diameter of the stenosis (a) should be measured perpendicular to the longitudinal axis of the vessel (green line) and not in a pure axial plane (red line), because then you may underestimate the degree of stenosis.
It is compared to the diameter of the normal vessel at about 6 cm distal to the stenosis (b).
In the formula the degree of stenosis is calculated.
Calcifications are common in atherosclerotic
stenosis and CTA has a high sensitivity in detecting these calcified
structures.
Sometimes a bias in the exact
evaluation of stenosis degree may be caused by the high attenuation values of
the calcified plaques.
This might lead to an overestimation of the degree of
stenosis.
Furthermore, heavily calcified plaques can be a challenge for the
interventional neuroradiologist as the stenosis needs to passed with a large
bored guiding catheter or long sheath (at least 6 Fr).
Near occlusion
In a severe stenosis or near occlusion the diameter of the ACI above the level of the stenosis is diminished and less than the caliber of the contralateral ICA and the ipsilateral ECA.
In a total occlusion the contrast has a { or curly bracket-like configuration, which is unlike an occlusion in a dissection or in a pseudo-occlusion.
 Click on image for an enlarged view. Small distal caliber of the distal ICA and a drop in systolic peak velocity.
Click on image for an enlarged view. Small distal caliber of the distal ICA and a drop in systolic peak velocity.
Near occlusion (2)
In this case the common carotid artery has a normal diameter (image 1).
There is a severe stenosis with a partly calcified plaque at the level of the bulbus (2).
The ICA above the stenosis shows a small caliber (3). See also the arrow in the sagittal reconstruction.
The criteria for near occlusion are:
- Caliber of distal ICA smaller compared to the contralateral ICA (image 3).
- Caliber of the distal ICA less than the ipsilateral external carotid (ECA on image 3).
The peak velocity with US-doppler normally increases in relation to the severity of a stenosis, but when there is a near-occlusion the systolic peak velocity will drop to very low levels like in this case (20 cm/sec).
Continue with the sagittal images...

You can scroll through the sagittal images.
Notice the calcified plaque at the level of the bulbus and the small caliber of the distal ICA, which is less than the caliber of the ECA.
Treatment
Treatment strategy for near occlusion
(NO) is still controversial. In the analyses conducted in randomized controlled
trials such as the North American Symptomatic Carotid Endarterectomy Trial
(NASCET) and the European Carotid Surgery Trial (ECST), it was reported that
the risk of stroke was low with medical treatment, and surgical therapy was not
beneficial for internal carotid NO.However, an 11%–33% risk of ipsilateral
stroke within the first year has also been reported in medically treated
patients.
Furthermore, other authors have reported a significantly lower risk of future stroke after Carotid endarterectomy or Carotid artery stenting in these patients.
Seeking safe interventional procedures could, therefore, be worthwhile especially with the current improvements in carotid stenting technique .
Occlusion
In a total atherosclerotic occlusion the contrast has a { or curly bracket-like configuration.
The stop will be at the level of the bulbus.
Carotid Dissection
A carotid dissection is the result of
a tear in the intima of the vessel wall.
As blood enters between the layers of
the vessel wall an intramural hematoma is created.
This intramural hematoma results in the following:
- Dilatation of the total ICA-diameter
- Compression of the true lumen
- The hematoma can be a source of emboli and lead to a cerebrovascular accident
Dissections cause about 2% of all ischemic strokes, but account for 10%−25% of ischemic strokes in young people.
Patients sometimes present with pain in the neck and may have a history of a previous trauma.
On CTA a dissection presents with the
following findings:
- On axial images there is an eccentric and narrowed lumen of the ICA.
- There is expansion of the ICA (↑ of the total diameter).
- The bulbus is spared unlike in atherosclerotic disease.
- A dissection generally stops prior to entering the skull.
- The emboli that originate from the intramural hematoma are erythrocyte rich thrombi and result in very dense thrombi in the intracerebral vessels on a non-enhanced CT (dens vessel sign).
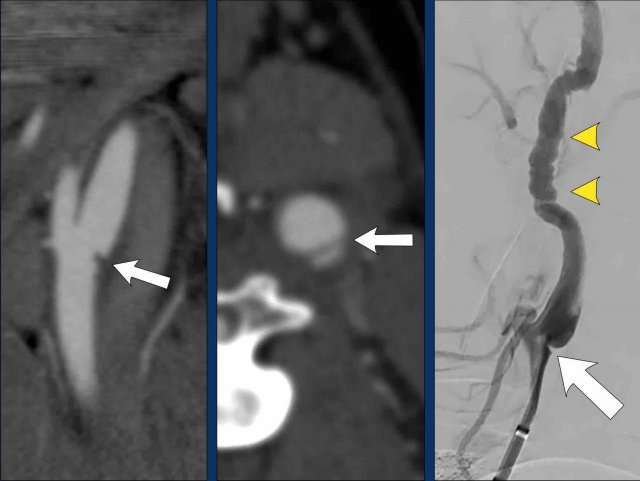
Flame-shaped ICA
These images show the typical flame-shaped presentation of a carotid dissection on sagittal CTA reconstructions and DSA.
Notice that on the CTA reconstruction you can follow the contours of the dilated ICA above the level where the contrast stops.
Also notice how similar the images are, when you compare the CTA with the DSA.
String sign
In most cases a dissection will present with a flame-shaped appearance like in A, but when the lumen is less compressed and still partially patent you may get the "string sign" as in B.
Look below the skull base
When you consider the possibility of a dissection, t is important to study the axial images just below the skull base as in this case.
On the left side there is a normal ICA and ECA (the high density structure in between them is the styloid process).
On the right side we see a normal ECA and medial to the jugular vein is the dilated ICA (circle).
The lumen does not fill with contrast.
The combination of an occlusion in an enlarged and dilated ICA means that we are dealing with a dissection.
A dissection stops at the skull base
This patient has a carotid
dissection.
In A we see the compressed lumen in
an eccentric position (green arrow).
The diameter of the ICA is enlarged
by the intramural hematoma (red arrowheads).
When we follow the ICA cranially, the
dissection continues up to image E (arrowheads).
At the level of the skull base, where
the ICA enters the carotid canal (vertical petrous segment) , the dissection
stops and the ICA has a normal appearance (yellow arrow).
Hyperdense thrombi
A typical finding in dissection are
hyperdense thrombi as in these two patients.
Whenever you see these kind of extremely
hyperdense thrombi, think of dissection and scroll down to just below the skull
base.
These thrombi are almost completely composed of erythrocytes.
Dissection on DSA
All the findings that we discussed on CTA are similar and even more obvious on DSA.
- The catheter is at the level of the bulbus, which is normal.
A couple of centimeters above the bulbus the lumen of the ICA is eccentric and compressed by a mural hematoma (better seen on detailed view 2).
At the level of the skull base (yellow stippled line) the vessel returns to normal. - Detailed view showing contrast material that has entered the hematoma.
Notice that the total diameter of the ICA is enlarged. Arrow indicates the true lumen. - After endovascular treatment the patency of the ICA has been restored.
The mural hematoma is for a large part lysed through the iv-treatment of recombinant tissue plasminogen activator (rt-PA, alteplase) prior to endovascular treatment. The intima flap is still visible. Again you can seen the intimal flap stopping at the level of the skull base.
Pseudo-Occlusion
Pseudo-occlusion of the cervical internal carotid artery refers to an isolated occlusion of the distal intracranial ICA that mimicks an extracranial ICA occlusion on CTA or DSA.
In pseudo-occlusion it looks as if there is a total occlusion in the ICA just above the level of the bulbus.
The contrast that enters the ICA has difficulty to move up further cranially, because of the stagnant blood within the ICA, since the ICA has no major side branches.
The contrast will only slowly penetrate this stagnant blood column and this results in a waterpaint appearance.
On CTA you will see a gradually diminishing contrast density in the ACI with a water paint appearance.
The problem is the outflow obstruction at the level of the carotid T-top.
A
pseudo-occlusion is never seen in combination with a more distal occlusion.
For
example, in case of a M2 occlusion there will be sufficient outflow of the
distal ICA through the other patent M2
division and the ACA.
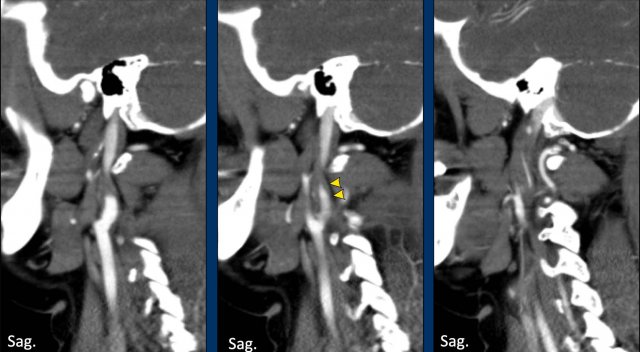
Two cases of a carotid pseudo-occlusion.
In the first case (left) the contrast
stop is rather abrupt, although a small zone of diminishing contrast density can
be seen.
In this case the differentiation between a pseudo-occlusion and a dissection or atherosclerotic occlusion
can be difficult.
However, we do not see the typical flame shape
configuration of the bulbus as seen in a dissection and we see no signs of
atherosclerosis (no plaque or calcifications).
In the second case the gradually
dimishing contrast density is cleary seen over a longer course (arrowheads).
This
is clearly a carotid pseudo-occlusion.
Continue with the DSA images...
Pseudo-occlusion with DSA
The DSA gives us comparable images.
In this patient during catheter angiography, first there was a typical waterpaint appearance of the contrast in the ICA, which simulated a proximal occlusion in the ICA.
However the catheter could easily be advanced into
the distal ICA.
After a more
forceful contrast injection there is a typical carotid-top occlusion on the
lateral view (just above the level of the ophthalmic artery.
There is no contrast filling
of the intracerebral vessels.
Floating Thrombus
On the saggital view there is a longitudinal filling defect
in the proximal internal carotid artery (arrowheads).
This filling defect is a
floating thrombus attached to a atherosclerotic plaque located at the carotid
bulb (white arrow).
In the axial plane this floatig thrombus causes a central filling defect in the ICA also now as a “donut sign” (arrowhead).
In case of an
accompanying intracranial occlusion of a large vessel endovascular therapy is
initiated to open this intracranial occlusion.
An isolated floating thrombus
(no large vessel occlusion) is treated with heparine or
anti-platelet therapy .
Carotid Web
A carotid web is a shelf-like lesion along the posterior wall of the internal carotid artery bulb and an under-recognized cause of stroke in young individuals.
Several studies suggest that patients with a carotid web have a high risk of recurrent stroke.
In the MR CLEAN study 30 patients with a carotid web ipsilateral to the stroke were identified.
In this study 1 out of every 6 patients with a symptomatic carotid web had a recurrent stroke within 2 years, suggesting that medical management alone may not provide sufficient protection for patients with a carotid web.
On the saggital view of the CTA the shelf-like protusion on the dorsal wall of the ICA bulbus is seen.
This is the typical configuration location for a carotid web.
However, for the definite diagnosis of a carotid web a ridge connecting the lateral and medial wall of the internal carotid artery must be seen in the axial view (arrow right image).
Carotid webs can differ in size.
In this case the
carotid web is much smaller than in te previous example.
However, the imaging
criteria for the diagnosis of a carotid web still apply.
On the sagittal images
a self-like protrusion is seen on the dorsal aspect of the internal carotid
artery (arrow left image).
On the axial images the ridge of the carotid web
is seen connecting the lateral and medial wall of the internal carotid artery (arrow).
If you only look at the axial images,
you may miss a web.
The red arrow points at the ICA and
ECA, but no web is seen..
Only with by angulating the axial
plane perpendicular to the longitudinal axis of the ICA (green line and green
arrow) you will notice the web (ridge
connecting the lateral and medial wall of the ICA.
Of course the sagittal
reconstructions are superior for detecting a web.
Correlation carotid web and cerebral ischemia
These DSA images cleary demonstrate
the mechanism by which carotid webs cause cerebral infarctions.
On the first
angiographic images you might first a stenosis
(white arrow left image).
On the next image the web is clearly delineated (yellow arrow).
On in the late arterial phase view t stasis of contrast is seen directly cranial of the web.
It is clear, that in this region, due to
turbulence and stasis thrombi can develop and can cause cerebral emboli.
Isolated Carotid
An isolated carotid means that the
ICA supplies blood to the ipsilateral anterior and middle cerebral artery, but
that there is no connection to the contralateral side or posterior circulation,
because the anterior (Acom) and posterior (Pcom) communicating artery are
missing as an anatomic variant.
This is one of the many variants of
the circle of Willis.
Patent circle of Willis
Let us first describe the most common
situation.
In 90% of patients the circle of
Willis is patent.
When these patients present with an
acute stroke as a result of a dissection, they usually have an embolus in the
middle cerebral artery.
In those cases it is sufficient to
treat the intracranial occlusion and the dissected carotid artery can be left
untreated.
The collateral circulation over the
patent circle of Willis will take over the blood flow to the middle cerebral
artery.
Non-patent circle of Willis
In 10% of cases the circle of Willis
is insufficient.
In this case both the anterior and
posterior communicans artery are absent.
If there is an occlusion of the ACI,
then the patient is at risk for a massive stroke in both the anterior and
middle cerebral artery territory, since there is no collateral flow from the
contralateral ICA.
We will demonstrate this scenario in
the following case...
Case
A 35-year-old woman presented at the ER with speech difficulties and a paresis of the right arm.
The NECT did not show signs of a bleeding or infarction.
On the CECT there was normal enhancement of the intracerebral vessels, which means no intracerebral occlusion.
Within 20 minutes she was treated with IV trombolyse, which resulted in partial recovery.
One hour later however there was a deterioration with hemiparalysis on the right and aphasia.
The NIHSS was 27.
Subsequently she was transported to the intervention center.
Continue with the CTA of the neck...
The CTA of the neck shows the typical flame shape of the proximal ICA indicating a dissection.
Continue with the axial slices...
The axial image shows a dilated left ICA with an eccentric compressed lumen.
In conclusion there is a 35-year old women with a massive stroke (NIHSS = 27), a carotid occlusion as a result of a dissection, but no intracranial occlusion.
At that moment the questions were:
- Could there be a variant of the circle of Willis?
- And if so, why was there normal contrast enhancement of the left middle cerebral artery on the CTA?
The DSA of the left ICA confirmed the dissection (arrowheads) by demonstrating the flame shaped configuration of the proximal ICA .
Subsequently a DSA of the right ICA
and the left vertebral artery was performed.
The angiography of the right ICA showed
an absent Acom as not contrast crossed from right to left. In addition,
contrast injection in the left vertebral artery showed an absence of a Pcom.
This was proof of the diagnosis "Isolated carotid artery".
 Poor perfusion in the anterior and middle cerebral artery territory (all penumbra, no infarct core on CBV images (not shown)
Poor perfusion in the anterior and middle cerebral artery territory (all penumbra, no infarct core on CBV images (not shown)
Now what is the explanation for the contrast filling of the left middle cerebral artery as the left ACI is occluded and there is no collateral flow through the circle of Willis?
The explanation is, that there are
small collaterals between the external carotid artery (ECA) and the ICA.
This is enough to to fill the ACM
with contrast , but this is not sufficient for adequate perfusion of the left
hemisfere.
This is clearly demonstrated on the perfusion images.
During the interventional procedure the flow was restored due to repositioning of the intimal flap caused by the catheter manipulation.
Carotid stent placement was considered but not
performed.
The patient was treated with Fraxiparine
After 24 hours there was a NIHSS: 2 with only a mild aphasia, after 3 months the NIHSS was down to 0.
Follow-up MRI after one month showed
a small left frontal infarction (white arrow).
The left ICA was patent and showed a remaining
of the intramural hematoma with high signal on the T1W-image (arrowhead).