Perianal Fistulas
Susanne Tonino and Robin Smithuis
Radiology Department of the Medical Centre Alkmaar and the Rijnland hospital, Leiderdorp, the Netherlands.
Publicationdate
Perianal fistula is a common disorder that often recurs because of infection that was missed at surgery.
Preoperative MR can help to prevent recurrence.
In this review we will address the anatomy, pathogenesis, classification and scanning protocol of perianal fistulas.
by Susanne Tonino and Robin Smithuis
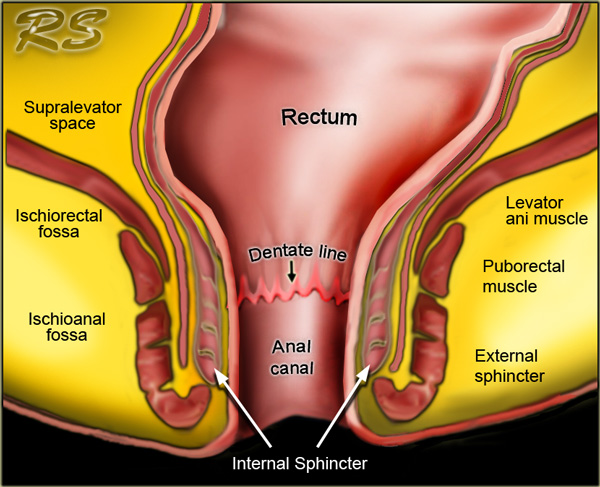
Anatomy
The anatomical anal canal extends from the perineal skin to the linea dentata.
Surgically, the anal canal extends from the perineal skin to the anorectal ring.
This is the circular upper border of the puborectal muscle which is digitally palpable upon rectal examination.
The anorectal ring lies approximately 1-1,5 cm above the linea dentata.
The total length of the surgical anal canal is about 4-5 cm.
The anal sphincter is comprised of three layers:
- Internal sphincter: continuance of the circular smooth muscle of the rectum, involuntary and contracted during rest, relaxes at defecation.
- Intersphincteric space.
-
External sphincter: voluntary striated muscle, divided in three layers that function as one unit.
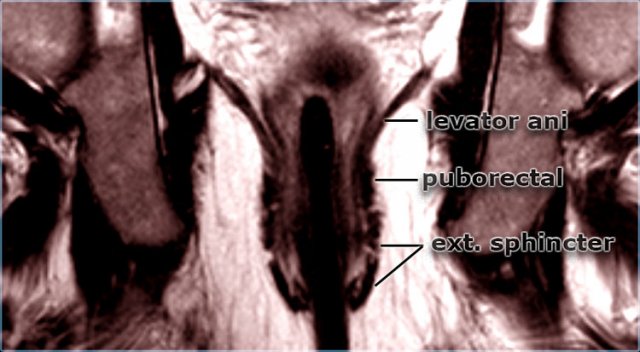
These three layers are continuous cranially with the puborectal muscle and levator ani (figure).
The puborectal muscle has its origin on both sides of the pubic symphysis, forming a 'sling' around the anorectum.
The puborectal muscle is contracted at rest and accounts for the 80? angulation of the anorectal junction.
It relaxes during defecation.
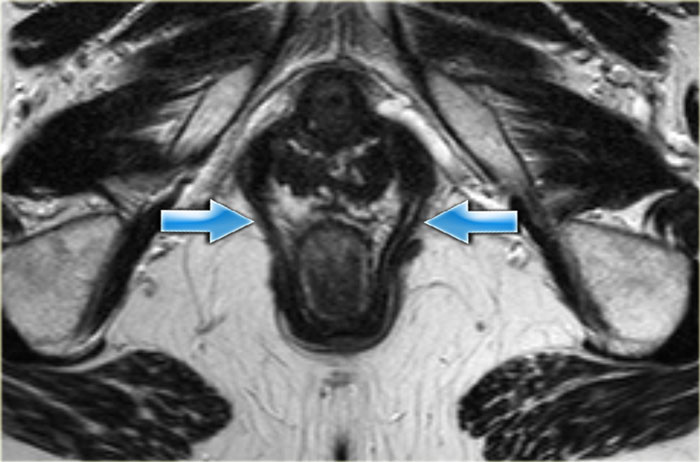
On axial and coronal MR-images the different layers of the anal sphincter and the surrounding structures can be displayed perfectly.
Perianal fistula
A perianal fistula is an abnormal connection between the epithilialised surface of the anal canal and the skin.
The causes of perianal fistulas:
-
Primary
- Obstruction of anal gland which leads to stasis and infection with absces and fistula formation (most common cause).
- Secondary
- Iatrogenic (hemorrhoideal surgery)
- Inflammatory bowel diseases (Crohn's disease more common than colitis ulcerosa)
- Infections (viral, fungal or TB)
- Malignancy
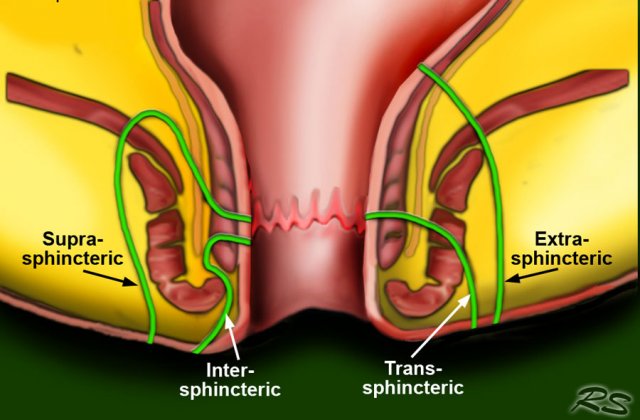
Classification
The most widely used classification is the Parks Classification which distinguishes four kinds of fistula: intersphincteric, transsphincteric, suprasphincteric and extrasphincteric.
The most common fistulas are the intersphincteric and the transsphincteric.
The extrasphincteric fistula is uncommon and only seen in patients who had multiple operations.
In these cases the connection with the original fistula tract to the bowel is lost.
A superficial fistula is a fistula that has no relation to the sphincter or the perianal glands and is not part of the Parks classification.
These are more often due to Crohns disease or anorectal procedures such as haemorrhoidectomy or sphincterotomy.
MR Protocol and Reporting
Protocol
A localizer in three directions is needed in order to align the T2 sequences axial and coronal to the anal canal.
Any localizer that properly displays the anal canal can be used.
We use a TRUE FISP, which is the name that Siemens uses for a steady-state precession gradient-echo sequence (GE: FIESTA, Philips: balanced FFE).
T2W images without fatsat better display the anatomy, while the fatsat images better depict the fistulas.
Reporting
When you describe a fistula, it is important to mention the following characteristics:
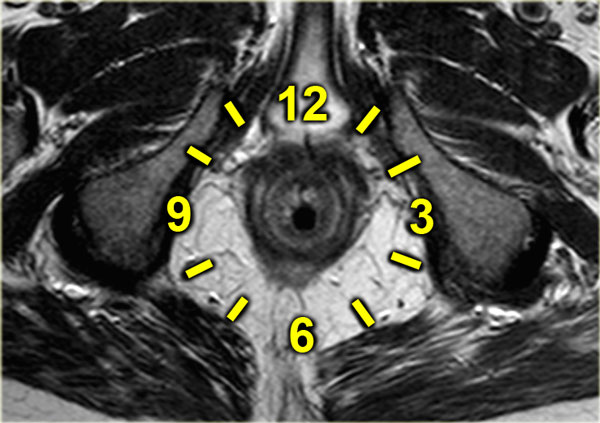
- Position of the mucosal opening on axial images (using the anal clock).
- Distance of the mucosal defect to the perianal skin on coronal images.
- Secondary fistulas or abscesses.
The drawing on the left illustrates the anal clock, which is the surgeon's view of the perianal region when the patient is in the supine lithotomy position (2).
This scheme corresponds to the orientation of axial MR images of the perianal region.
Examples of Perirectal Fistulas
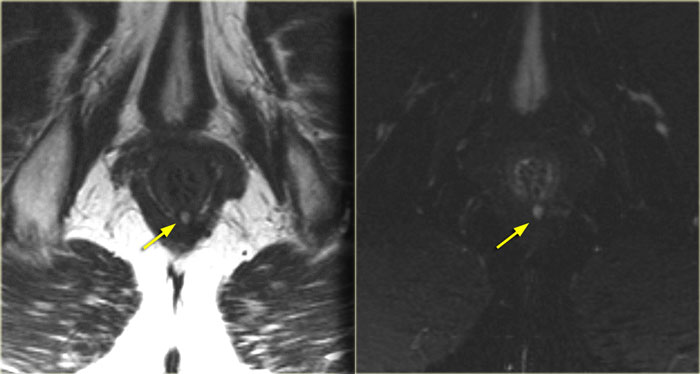
Intersphincteric fistula
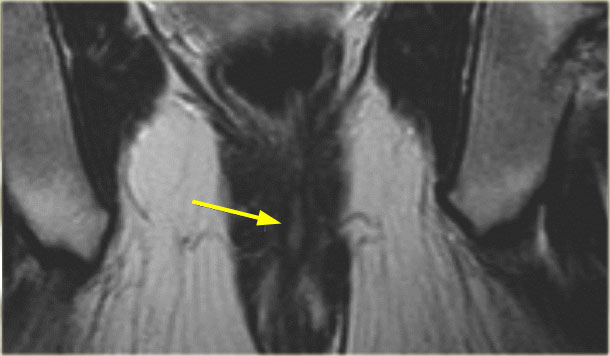
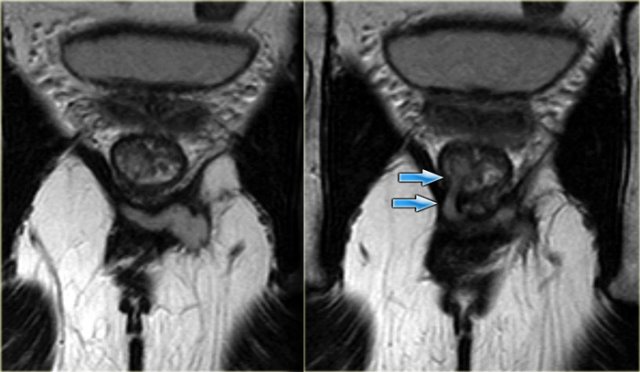
On the left axial T2W images with and without fat saturation.
An intersphincteric fistula is located at 6 o'clock.
Continue with coronal images.
On the coronal image the fistula runs caudally towards the skin.
There is no connection with the external sphincter.

On the left coronal images of another patient with an intersphincteric fistula.
Use the arrows to scroll through the images.
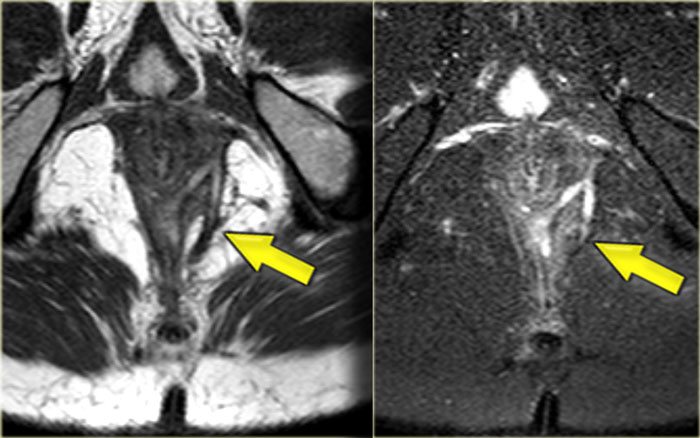
Transsphincteric fistula
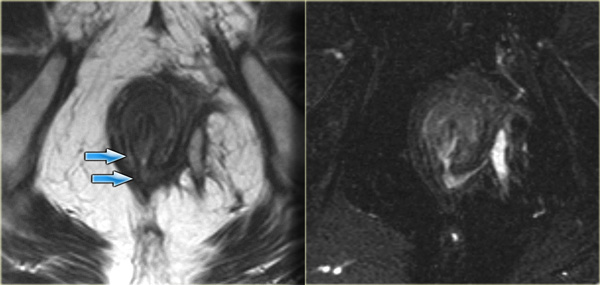
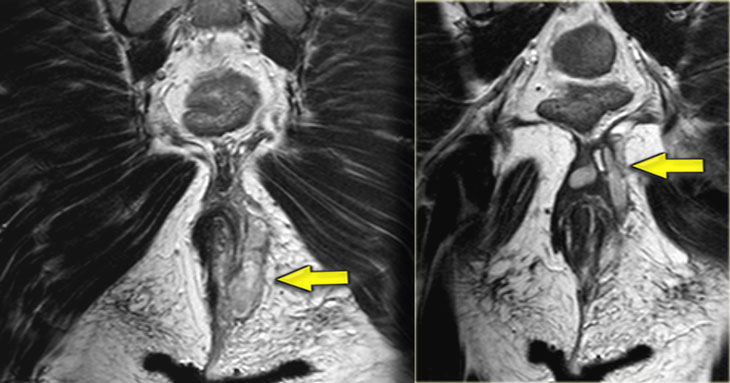
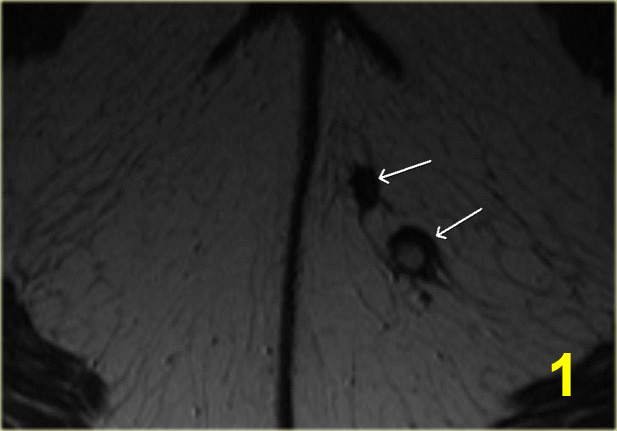
On the left an axial T2WI and T2WI + fatsat of a transsphincteric fistula.
The defect through the internal and external sphincter at 6 o'clock is clearly visible and more apparent on the fat sat images.
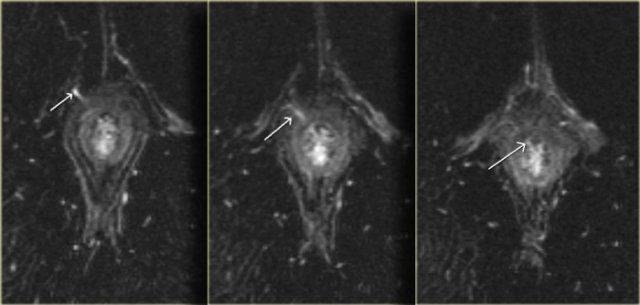
On the left axial T2W-fatsat images of a transsphincteric fistula with the mucosal opening at 11 o'clock.
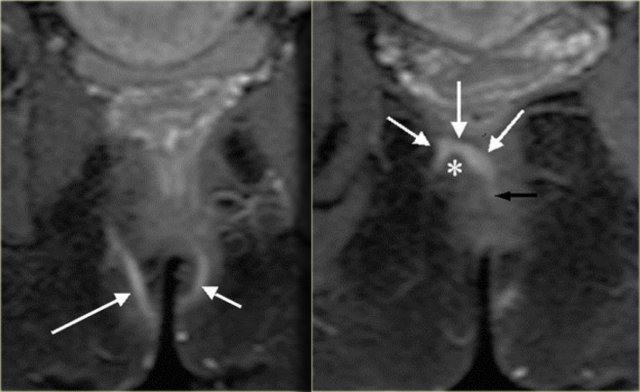
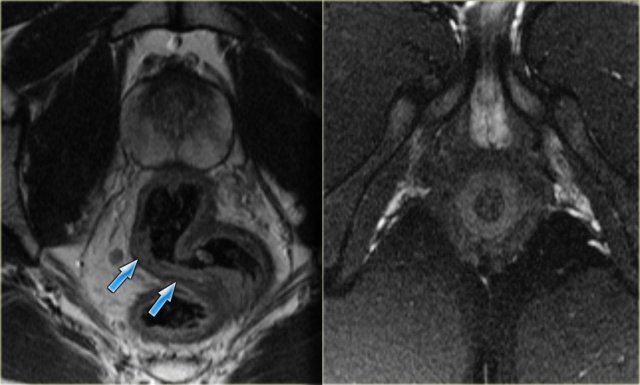
On the left an example of a suprasphincteric fistula.
There are two tracts in the ischioanal region.
The right sided tract runs over the puborectal muscle (asterisk) and the mucosal opening lies at the
level of the linea dentata (black arrow).
Extrasphincteric fistula
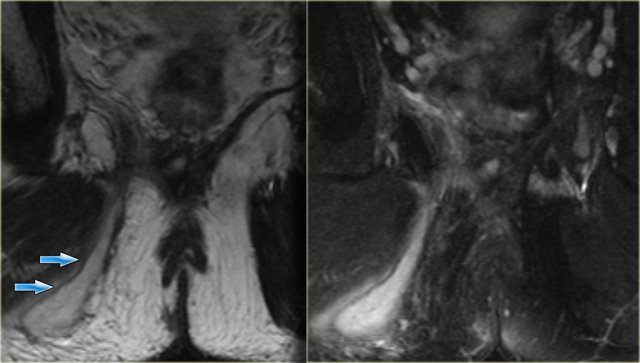
On the left coronal T2W-images of a small abscess in the left ischioanal fossa, the fistula runs through the levator ani.
It is therefore above the sphincter complex and extrasphincteric.
Complex fistula
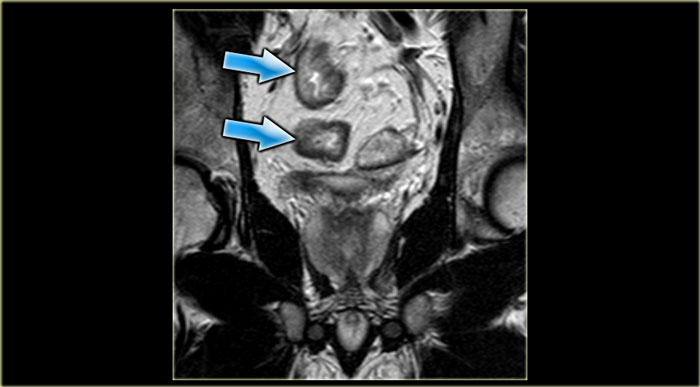
On the left an example of a complex fistula.
Two tracts in the left buttock form a single tract (no. 1-2).
This fistula breaks through the external sphincter (no. 4).
In the intersphincteric space it divides again into two tracts (no. 5).
One ends blindly in the intersphincteric space (no. 6).
The other breaks through the internal sphincter with the mucosal defect at 1 o'clock.
Crohn's disease
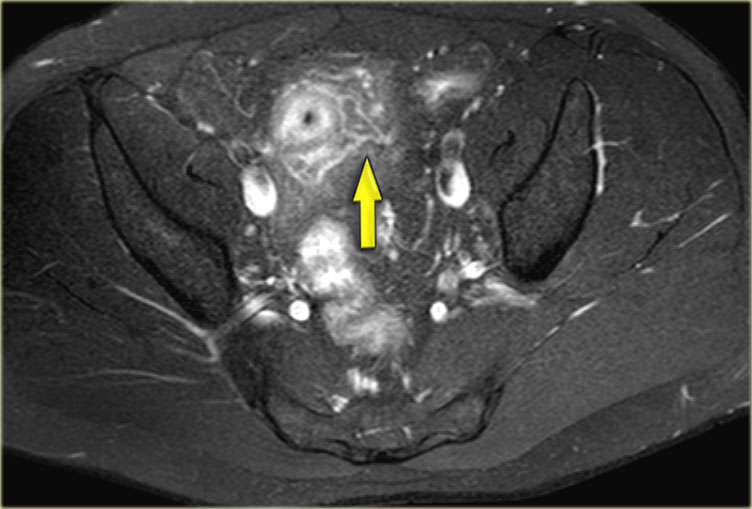
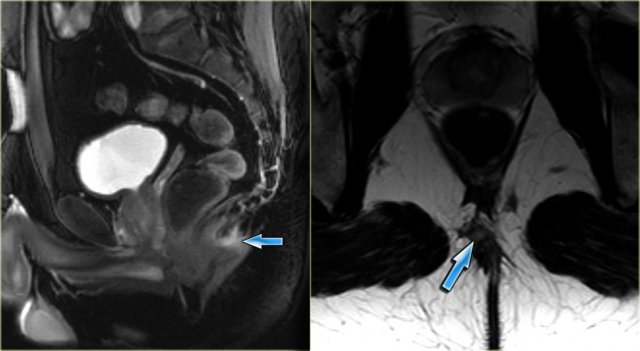
On the left a patient with a perianal fistula who has Crohn's disease.
Continue with the coronal images.
On the coronal images the thickening of the bowel wall is demonstrated.
Axial fatsat images depict the transmural inflammation with infiltration of the mesenteric fat.
Treatment
Treatment is focussed on the elimination of the primary and secondary tracts, prevention of
recurrence and to retain continence.
The treatment given depends on the anatomy of the fistula, if it is a simple fistula with a
low mucosal defect is can be probed in the OR to identify the mucosal defect at the
linea dentata, then the tract can be opened.
This is only possible if the external sphincter is not involved.
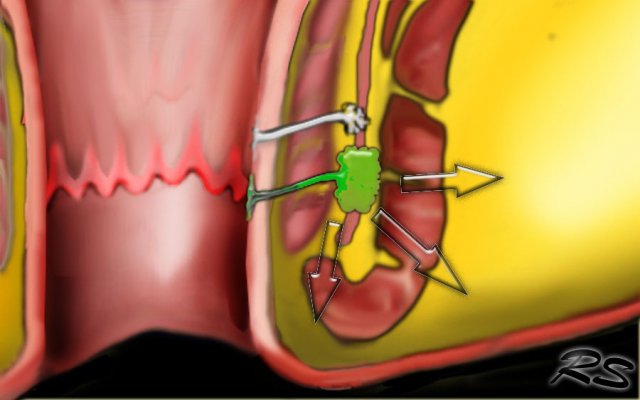
Seton fistulotomy is a technique where a rubber ligature or vessel loop is pulled through the
fistula, it then is tightened every 2 weeks or so in order to obtain pressure necrosis so that
the Seton is slowly pulled through the muscle.
This has the advantage that the muscle is slowly cut and fibroses at the same time in order
to cause as little damage as possible to the sphincter complex.
If there is an extrasphincteric fistula, the lower part is opened.
The mucosal defect, which is by definition in the rectum, is then surgically closed.
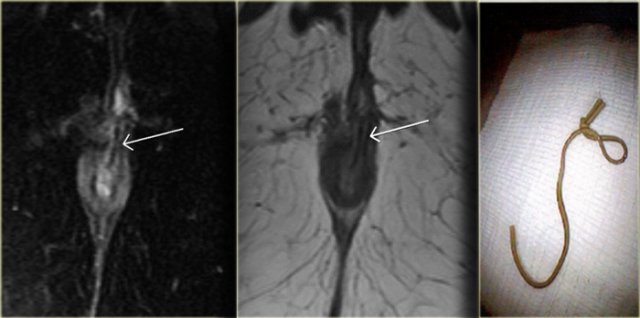
This patient was already known to have an intersfincteric fistula, the mucosal defect is at 1 o'clock.
In the tract there is a linear structure with a low signal intensity.
This is the Seton which was inserted to treat the fistula.
Differential diagnosis
Sinus pilonidalis
On the left an example of a sinus pilonidalis.
There is a small abscess just above the nates.
There is no relation with the sphincter complex.
Proctitis
On the left images of a patient who presented with anal complaints.
No fistula was seen.
There is, however, a diffuse thickening of the rectal mucosa due to a proctitis.
Abscess in the Ischioanal space
An abscess in the ischioanal space with no connection to the sphincter complex