Neck Masses in Children.
Annemieke Littooij, Cécile Ravesloot and Erik Beek
Radiology department of the University Medical Center Utrecht in the Netherlands
Publicationdate
A mass in the neck is a common finding in children.
In this article we present a pictorial essay of neck masses in children and provide a diagnostic approach based on the location of the lesion and whether it is cystic or solid.
Ultrasound is the imaging method of choice and in many cases a definite diagnosis is possible, especially if the lesion is cystic.
MRI is of value in large lesions, to determine whether the lesion infiltrates into deep spaces.
CT is sometimes applied in acutely ill patients with infections to assess whether an abscess is present.
In suspected malignant lymphoma ultrasound can demonstrate which node is most accessible to image guided biopsy or excision, while PET/CT is used for staging.
Introduction
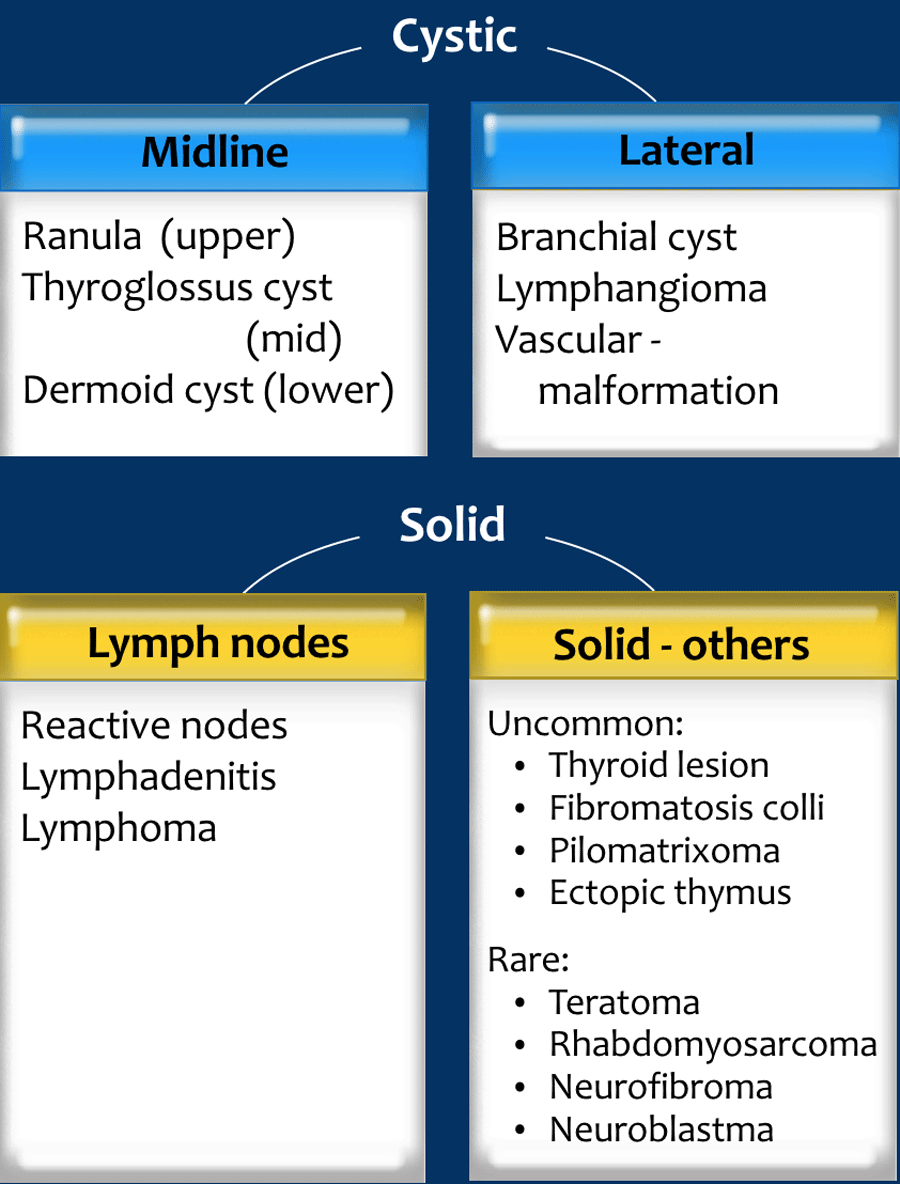
Diagnostic approach
In a neck lesion in a child, ultrasound can usually determine whether a lesion is cystic or solid.
- Cyst
In cystic lesions the diagnosis can frequently be made based on the location of the lesion (see next figure). - Lymph node
If the lesion is solid the next step is to assess whether it is a lymph node or something else.
Often more than one lymph node is enlarged. Try to differentiate between reactive nodes, lymphadenitis due to TB or cat-scratch disease and malignant lymphoma. - Solid - not a lymph node
If a solid lesion is not a lymph node look for a possible site of origin, like the salivary gland, the thyroid gland or the sternocleidomastoid muscle.
Subcutaneous solid lesions sometimes have a typical appearance, like pilomatrixomas, lipomas or hemangiomas.
In many cases however a solid lesion will be non-specific and a diagnosis can only be made through biopsy or excision.
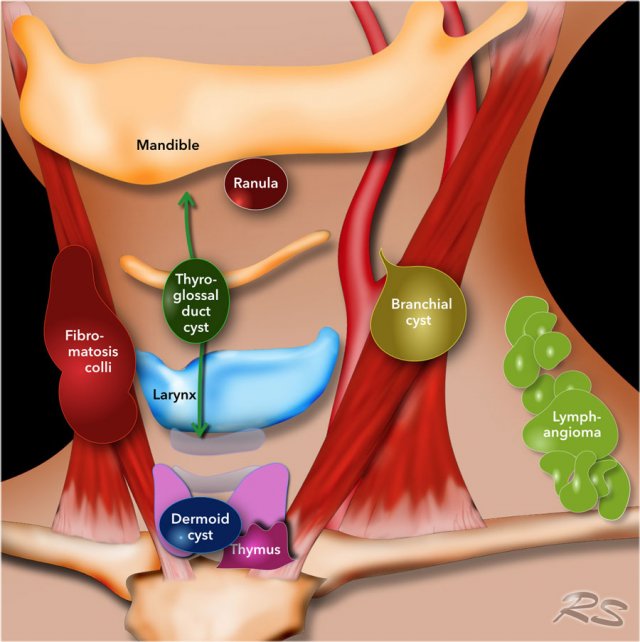
Location of cystic lesions
Once you have decided that the lesion is cystic its location will often point to its nature (figure).
Midline lesions
Midline lesions are either thyroglossal duct cysts, dermoid cysts or ranulas.
Older children can be asked to protrude their tongue.
A thyroglossal duct cyst will move upward with the hyoid bone.
Ranulas have a typical location in the floor of the mouth.
Off-midline lesions
Off-midline lesions can be branchial cleft cysts or lymphangiomas.
Branchial cleft cysts often contain debris.
Anteriorly located lymphangiomas are often multicystic.
In the posterior neck they are often single.
Cystic lesions
In neck lesions we first try to figure out whether a lesion is cystic or solid.
In clear cystic lesions this is straightforward.
It can however be a problem if the cyst has been inflamed or when a cyst has bled, since children often present with a preexistent lesion that has bled.
Try to elicit swirling of the contents by compressive movements of the probe or by changing the position of the child and look for acoustic enhancement.
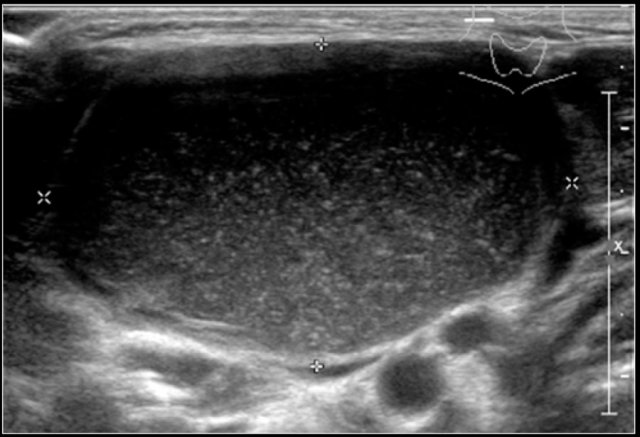
The video shows a swelling, that appeared overnight in a 13-year-old girl.
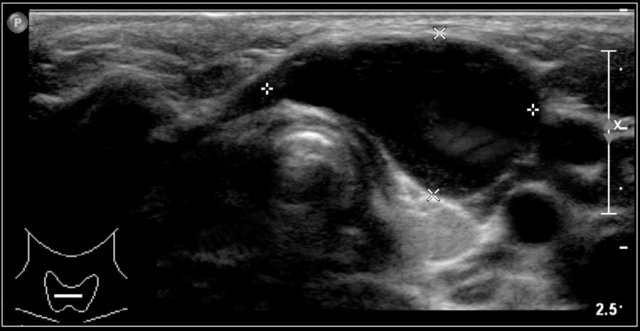
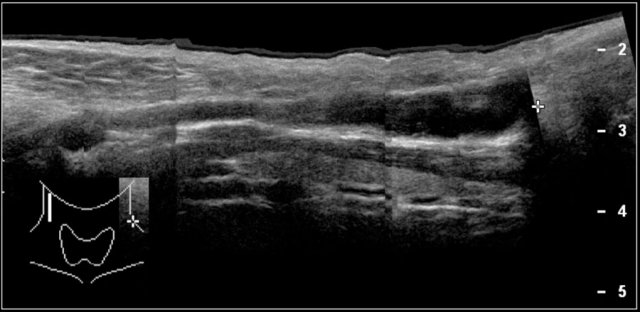
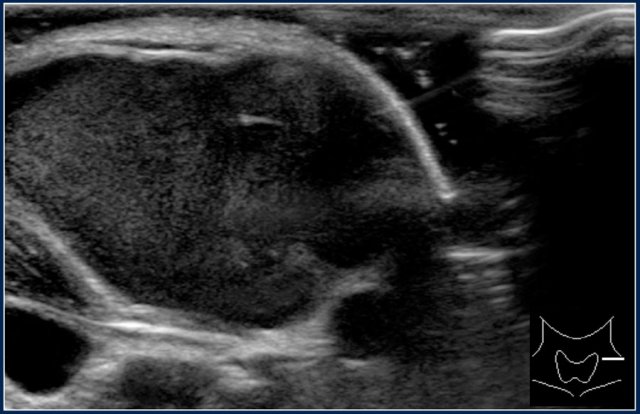
A hypo-echoic lesion is seen superficial to the carotid artery and deep to the sternocleidomastoid muscle.
No movement of the lesions content was seen when pinged with the probe.
When the girl was asked to sit upright the contents swirled.
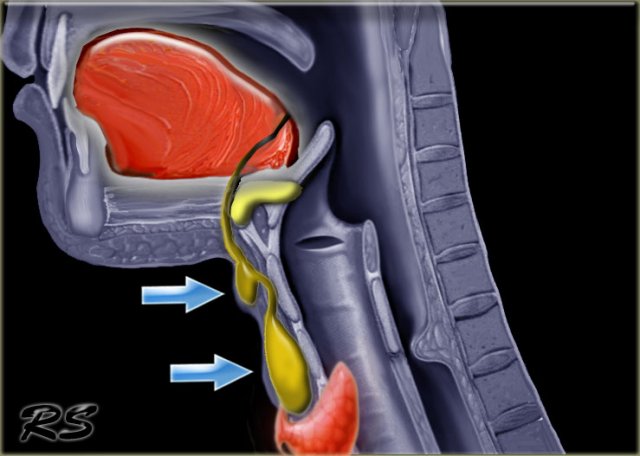
Thyroglossal duct cyst
Thyroglossal duct cysts are common lesions in children.
The thyroglossal duct runs from the base of tongue at the foramen caecum to the thyroid gland.
The embryonic thyroid gland travels through the duct to reach its final normal position.
Normally, the thyroglossal duct then involutes, but when the duct persists, a thyroglossal duct cyst can develop anywhere along this tract (figure).
Thyroglossal duct cysts move upward if the tongue is protruded or during swallowing (see next movie).
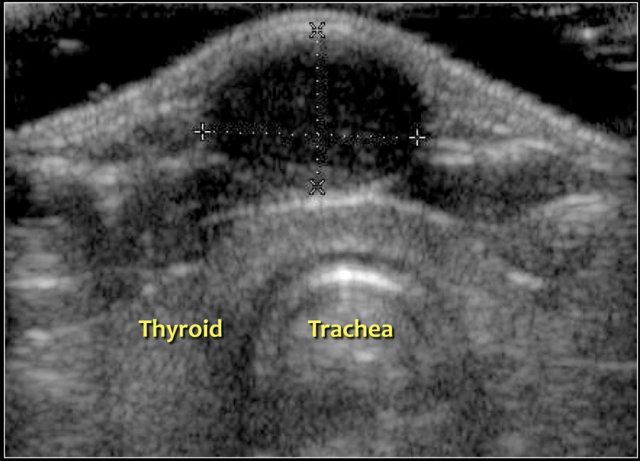
Ultrasound is usually sufficient to make the diagnosis.
Always look for the presence of a normal thyroid gland and make an image of it.
This videoclip demonstrates the upward movement of the thyroglossal duct cyst together with the hyoid bone during swallowing.
Thyroglossal duct cysts can be anechoic or hypo-echoic with internal echoes, due to infection, hemorrhage, or proteinaceous content.
The majority of thyroglossal duct cysts is located within 2 cm of the midline.
Here a tranverse image of a hypoechoic thyroglossal duct cyst with some internal echoes located in the midline.
Here a tranverse image of an anechoic thyroglossal duct cyst just left of the midline.
Dermoid cyst
Dermoid cysts are inclusion cysts, that contain epithelium and skin adnexa like hair follicles, sebaceous glands and sweat glands.
7% of dermoid cysts occur in the head and neck region, especially around the orbit and in the midline of the neck, with a predilection for the suprasternal notch.
Here a typical homogeneous hyper-echoic oval lesion, representing a dermoid cyst, which was located in its favorite location, the suprasternal notch.
In the neck dermoid cysts are generally homogeneously hyperechoic, although they can be inhomogeneous.
The differentiation from a thyroglossal duct cyst can be difficult if the dermoid cyst is located near the hyoid bone.
The content of thyroglossal duct cysts is usually hypo-echoic and may contain internal echoes, while dermoid cysts generally have a more homogeneous hyper-echoic content.
Here an unusual inhomogeneous appearance of a dermoid cyst in front of the thyroid gland (figure).
The most common location of a dermoid cyst in the head-neck region is around the orbit, typically at the upper outer corner.
On ultrasound they are anechoic and one should look for the presence of a bony lining.
If the integrity of the bony lining is uncertain, a CT or MRI is necessary to determine possible intracranial extension.
Here a typical orbital dermoid cyst.
It was firm on palpation and located at the lateral border of the orbit.
On ultrasound it is anechoic with remodelling of the underlying bone.
Branchial cleft cyst
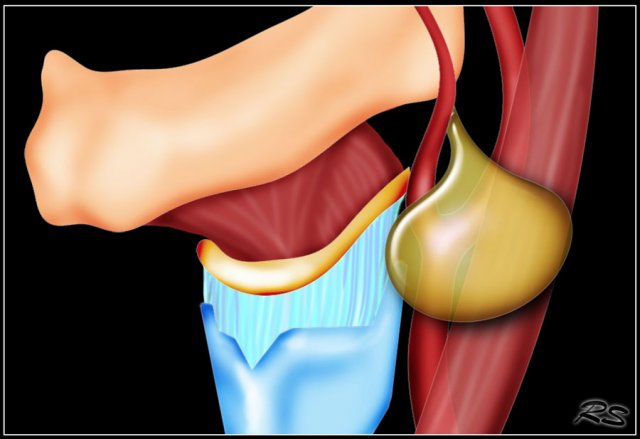
Most branchial cysts are remnants of the second brancial cleft.
Cysts at the level of the thyroid gland can be remnants of the third or fourth branchial cleft.
Incomplete obliteration results in either a cyst (75%), a sinus or a fistula (25%).
Cysts present as painless masses, sometimes appearing suddenly after internal hemorrhage.
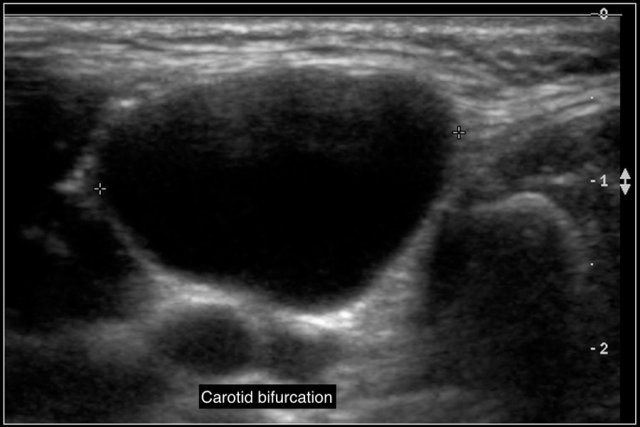
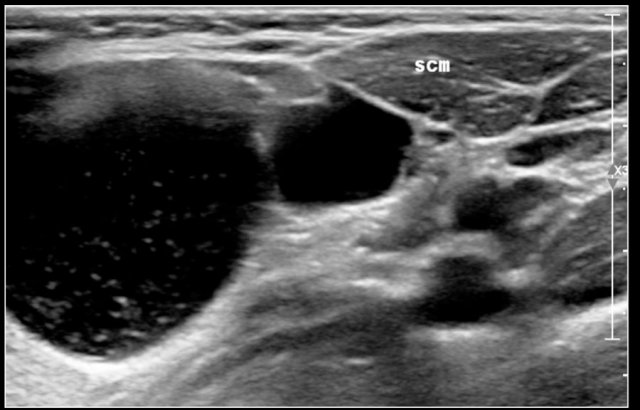
They are located along the anterior border of the sternocleidomastoid muscle, lateral to the common carotid artery, and if more cranially between the internal and external carotid artery.
Sometimes a beak sign may be seen as a curved rim of the lesion pointing medially between the internal and external carotid.
On ultrasound they often contains internal echoes caused by debris, which consists of cholesterol crystals.
The cyst is usually compressible, which results in movement of the content.
This may not be the case in a cyst with a fresh internal hemorrhage.
They can inflame and present with an empyema.
Here another branchial cyst with a typical location superficial to the carotid artery bifurcation.
Branchial sinuses
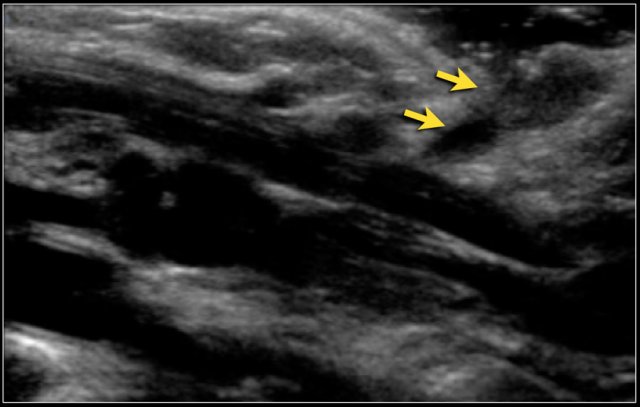
Branchial sinuses are blind ending tracts, presenting anterior of the sternocleidomastoid muscle.
Branchial second arch fistulas end in the tonsillar fossa, as can be demonstrated with a contrast fistulogram or MRI.
With ultrasound a tract can often be seen to travel upwards, but it is usually not possible to depict the proximal ending.
Here a two-year-old boy with a dirty spot in the right lower neck.
A small tract could be seen to extend inwards.
At operation a second branchial fistula was excised.
Here a ten-year-old girl with a pit in the right neck, anterior of the sternocleidomastoid muscle.
On US a long cystic lesion can be seen which can be traced up to the right submandibular region.
At operation, the fistula extended towards the right tonsillar fossa and was excised.
Lymphangioma
Lymphangiomas are cystic lesions, caused by maldevelopment of the lymph channels.
The majority occur in young children, with 90% in the head and neck region.
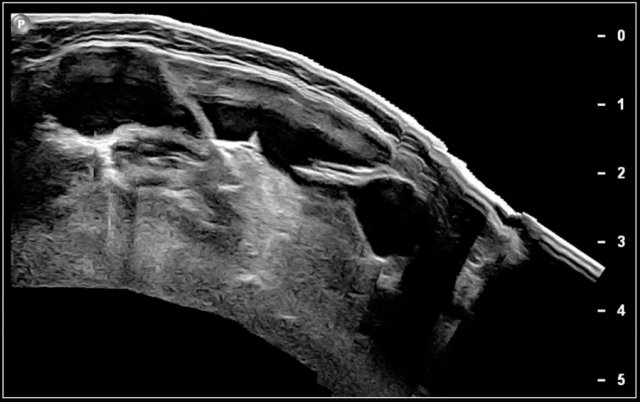
In the posterior neck a lymphangioma usually has one or more larger cysts.
In the anterior neck a lymphangioma can consist of innumerable small cysts, and may infiltrate deeply into the neck or mediastinum.
This is also called a hygroma colli.
The sonographic appearance depends on the size and number of cysts.
Larger cysts are mostly anechoic or may contain some debris.
A microcystic lymphangioma can be hyper-echoic due to the high number of closely related reflecting walls.
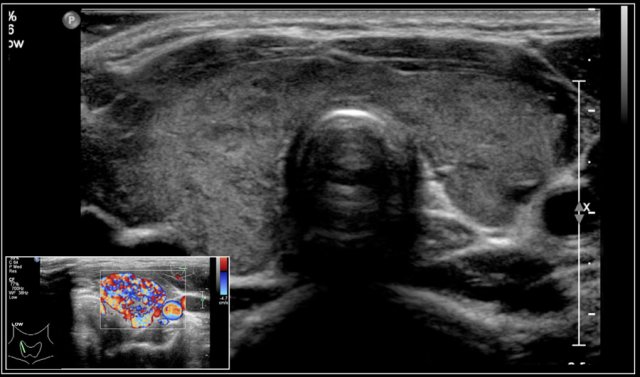
Here an ultrasound of a typical lymphangioma.
MRI was performed because the extension of the lesion was not clear.
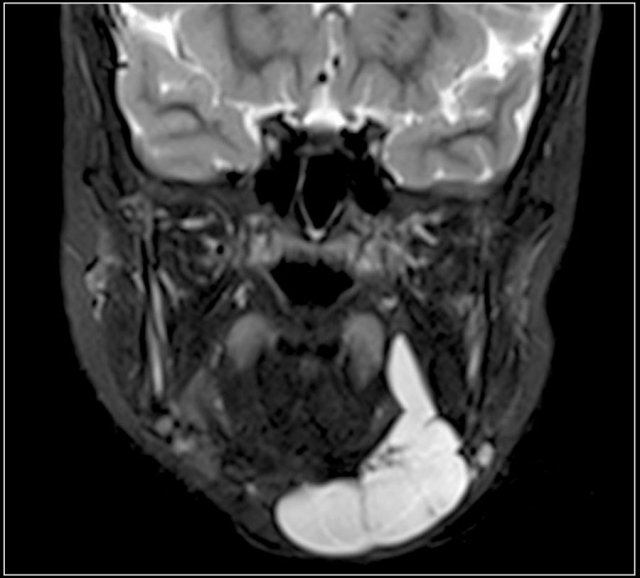
Here the T2-weighted image of the same patient.
On T1-weighted images the content has a variable signal intensity, depending on its protein or blood content.
It generally has a high signal intensity on T2-weighted images.
Contrast enhanced T1 can show enhancement of the wall.
Here an ultrasound image of a six-year-old girl with a sudden swelling in the left neck.
There were several small anechoic cysts and one large cyst containing internal echoes, which were probably the result of a bleeding in a preexistent lymphangioma.
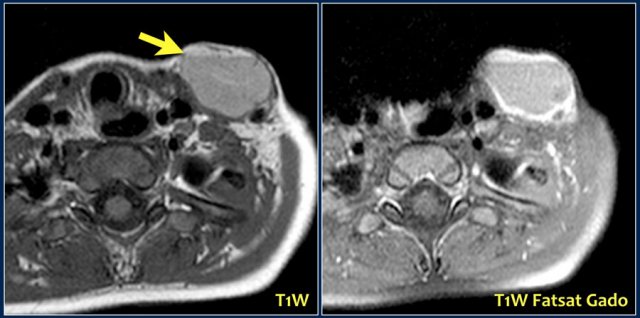
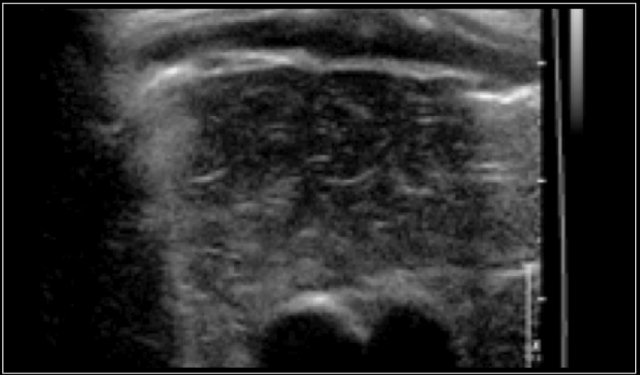
A 3-year-old boy presented suddenly with a supraclavicular mass.
Ultrasound showed a lesion with echogenic debris.
A hemorrhage in a preexisting lymphangioma was suspected.
Continue with the MRI.
The T1-weighted image shows a slightly hyperintense lesion with a fluid-fluid level (arrow).
After gadolineum administration there is enhancement of the cyst wall.
The lesion subsided with conservative therapy.
Ranula
A ranula is a fluid filled cyst originating from the sublingual salivary gland.
It can extend into the floor of the mouth and be visible on inspection of the oral cavity.
It can also extend through or over the mylohyoid muscle and is then called a "plunging ranula"
and present as a submental or submandibular mass.
Here an image of a sixteen-year-old boy with a firm swelling under the tongue on the left side.
Ultrasound showed an anechoic mass continuous with the sublingual salivary gland.
Jugular ectasia
In some children a swelling can appear in the lower neck during straining.
This is often caused by dilatation of the internal jugular vein as can easily be demonstrated by ultrasound that will show the variations in caliber of the vein.
An example is shown on the video of a seven-year-old boy, initially suspected of a laryngocele.
Solid lesions - Lymph nodes
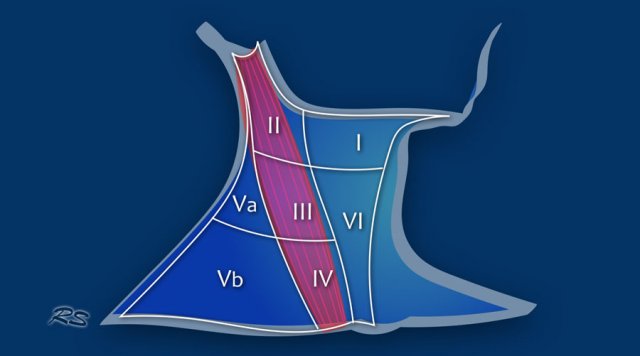
This image shows a commonly used classification for the location of lymph nodes.
- Level 1
Submental and submandibular nodes - Level 2
Nodes along the internal jugular vein, above the level of the hyoid bone - Level 3
Nodes along the internal jugular vein, between the hyoid bone and cricoid cartilage - Level 4
Nodes along the internal jugular vein, below the cricoid cartilage - Level 5
Posterior to the sternocleidomastoid muscle, above the clavicles - Level 6
Anterior to the thyroid gland
Normal lymph nodes are always visible with ultrasound in children.
A normal lymph node:
- Is sharply delineated
- Is oval
- Has an echogenic center
- Has a short axis < 10 mm.
The normal jugulodigastric node which is located below the mandibular angle can have a short axis of 15 mm.
Enlarged lymph nodes in the neck are very common in children.
In most cases these are reactive nodes as a reaction to a nearby infection.
Less commonly it is due to a primary infection of the lymph nodes itself, which is called lymphadenitis.
Usually the terms reactive lymphadenopathy and lymphadenitis are used synonymously.
Although ultrasound cannot always reliably distinguish lymphadenitis from a malignant lymphoma, the following table can be helpful to decide whether an excision biopsy should be done or that a "wait and scan" policy can be adopted.
Supraclavicular lymph nodes should always be considered to be malignant until proven otherwise.
Reactive lymph nodes
Reactive lymph nodes are a reaction to nearby inflammation.
They are slightly enlarged and more hypoechoic than normal with a broader echogenic center.
Here a six-year-old boy with weight loss, fatigue and lymphadenopathy.
On ultrasound a string of enlarged lymph nodes with preservation of a echogenic hilum was seen.
Excision biopsy showed reactive lymph nodes.
Here a two-year-old girl with a palpable swelling in the left neck since a few weeks.
On ultrasound the lymph nodes are enlarged with preservation of the echogenic hilus and normal perfusion.
It was decided to wait and see and the nodes slowly shrunk.
Bacterial or viral lymphadenitis
A bacterial or viral lymphadenitis is an infection of the node itself.
Bacterial lymphadenitis is often caused by Staphylococcus aureus or B-hemolytic Streptococcus.
The nodes, which are frequently located in the submandibular region, are painful and the skin is warm and red.
Bacterial lymphadenitis has an acute onset and is usually unilateral.
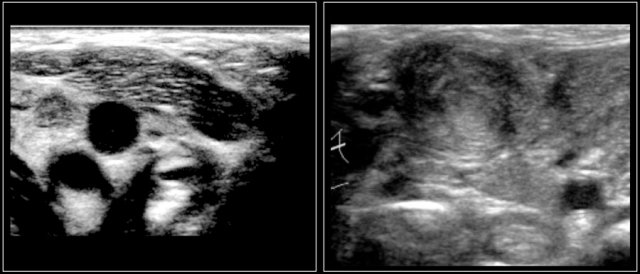
The ultrasound image is of a one-year-old boy with a swelling in the neck for three weeks.
A partly liquefied lymphnode is seen with infiltration of the surrounding subcutaneous fat.
The swelling disappeared on antibiotic treatment.
Abscess formation is clinically difficult to detect, and ultrasound is also not reliable.
Signs of liquefaction are areas with a detectable wall and more hypoechoic center or areas with mobile, moving echoreflections.
According to the literature there are 30% false-positive ánd false-negative results.
Here a one-year-old boy with a swelling in the right neck for one week.
Ultrasound shows an enlarged lymph node with areas of liquefaction.
It was incised and drained, after which the infection subsided.
Cat-scratch disease
Cat-scratch disease is caused by Bartonella henselae.
The infection is the result of a scratch or bite of a cat.
It is the most common cause of chronic axillary lymphadenopathy.
The symptoms are often mild and lymph node swelling can be prolonged.
The clinical diagnosis can be difficult and PCR results are insensitive.
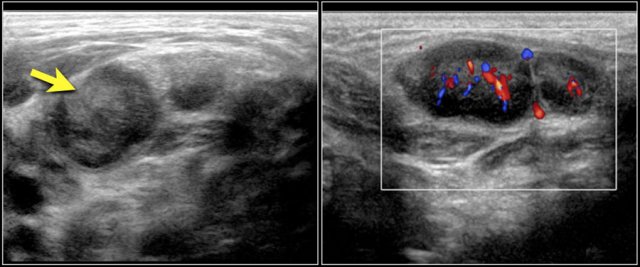
On ultrasound the affected nodes are round, heterogeneously hypoechoic, hypervascular, and with some surrounding inflammation.
The nodes are a bit tender but not painful.
They can be difficult to distinguish from malignant nodes.
Here an ultrasund image of a sixteen-year-old girl, who was treated for recurrence of acute lymphatic leukaemia.
Six months after the last treatment, she developed a swelling in the left shoulder region.
A hypoechoic node without any internal structure was seen.
It was excised.
The final diagnosis was, surprisingly, Bartonella henselae.
Cat-scratch disease 2
Here a video of a fifteen-year-old boy with a swelling in the neck.
There are multiple lymph nodes with surrounding infiltrated tissue.
Continue with next video.
After a week suppuration was seen.
Aspirated pus was positive for Bartonella henselae.
The boy was successfully treated with antibiotics.
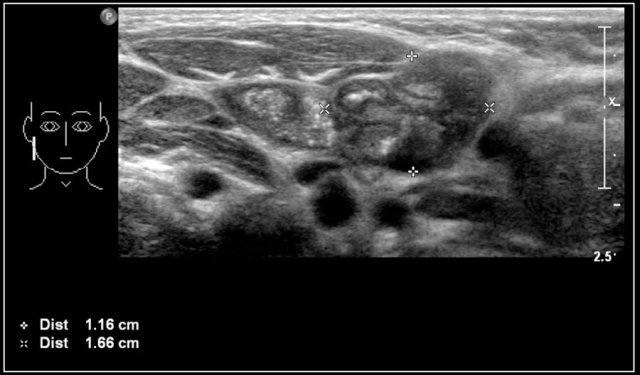
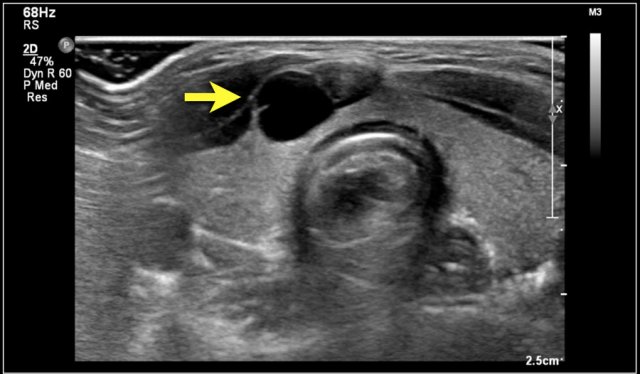
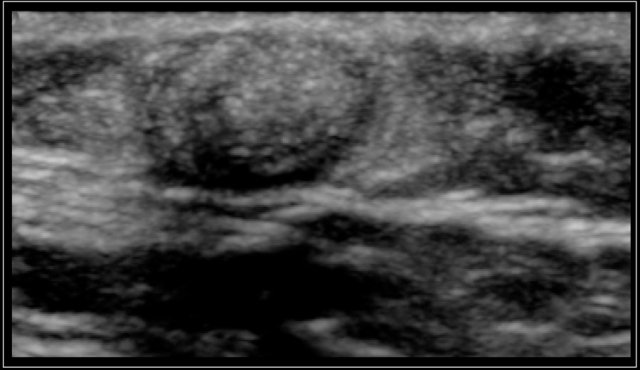
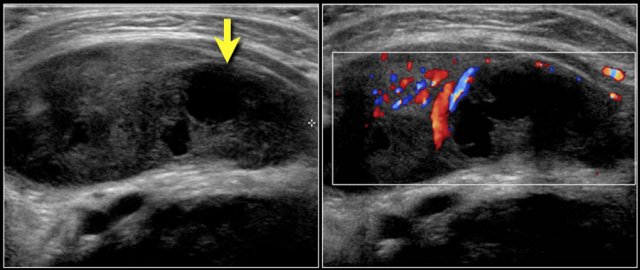 Two-year-old boy with a progressive swelling in the neck. No effect of antibiotics. An atypical Mycobacterium infection (avium) was confirmed. The anechoic parts (arrow) in the node are often seen in atypical Mycobacteria infection.
Two-year-old boy with a progressive swelling in the neck. No effect of antibiotics. An atypical Mycobacterium infection (avium) was confirmed. The anechoic parts (arrow) in the node are often seen in atypical Mycobacteria infection.
Mycobacteria
Infection with atypical Mycobacteria generally occurs in patients between one and five years of age.
There are few clinical symptoms, most often only a palpable mass.
The enlarged lymph nodes are usually unilateral and in the pre-auricular or submandibular area.
There is often a pronounced skin discoloration.
Tuberculosis (TB) and atypical Mycobacteria frequently present with a single enlarged node and some smaller satellite lesions.
There is central necrosis, thickening of the overlying skin, surrounding inflammation and after a while a confluent mass.
Fistulas may be present.
Calcifications are seen more commonly in TB infections than in atypical Mycobacterial infections, especially after treatment.
Continue with next image...
Three months later the swelling is still present.
The deeper lymphnode has liquefied.
After another four months a lymph node had undergone liquefaction and discharged in the surrounding tissue.
Here an ultrasound image of a 6-year-old boy with a swelling in the neck.
Fine calcifications are seen in the lymph node.
The Mantoux and Qferon test were positive, but cultures for tuberculosis were negative.
The patient was treated with tuberculostatics with good result.
Malignant lymphoma
Malignant lymphoma presents with painless lymphadenopathy.
In Hodgkin lymphoma the cervical nodes are most commonly involved, while in non-Hodgkin lymphoma the nodes of the Waldeyer ring are often involved.
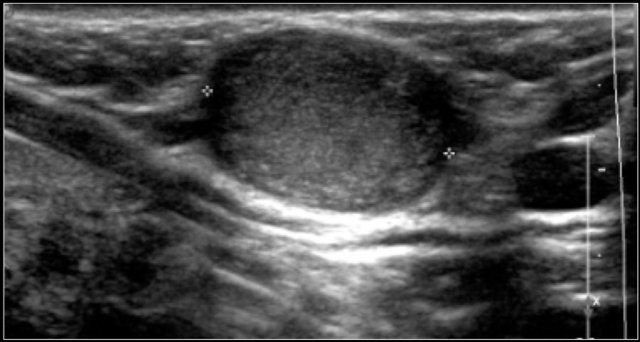
On ultrasound the affected nodes are round, homogeneously hypoechoic and the normal echogenic hilum is absent.
The diagnosis is made by ultrasound-guided biopsy or excision.
PET/CT will demonstrate the extension of the disease.
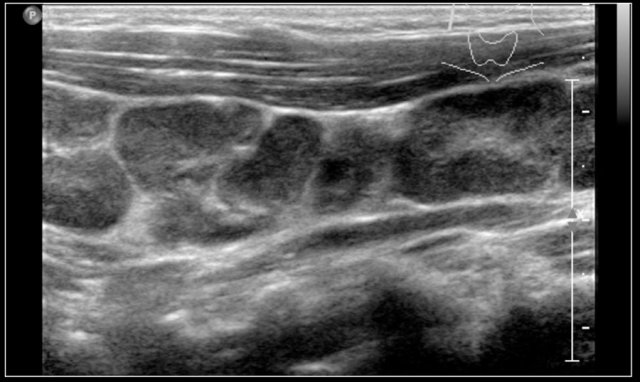
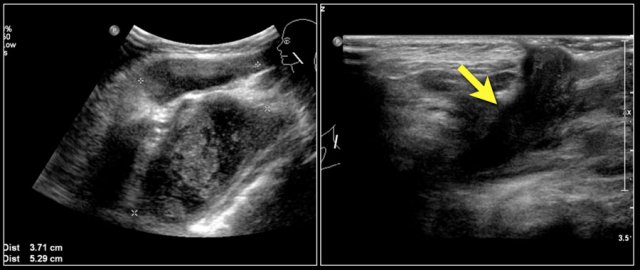
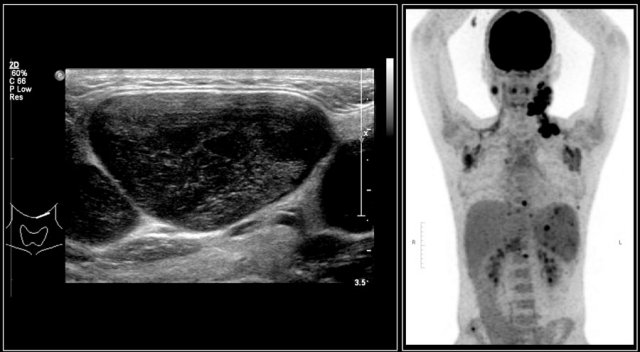
The images are of a fourteen-year-old boy with a painless swelling in the left neck.
The ultrasound shows several enlarged hypoechoic lymhnodes, that lack an hyper-echoic hilum.
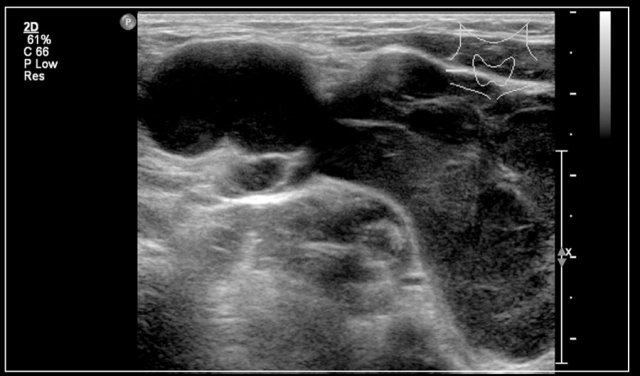
Here another fourteen-year-old boy with a painless swelling in the left neck.
Ultrasound showed several enlarged lymhnodes.
Continue with the MR and PET/CT...
A coronal STIR image shows the pathologic lymph node masses similar to the PET-CT.
The diagnosis was Hodgkin's lymphoma.
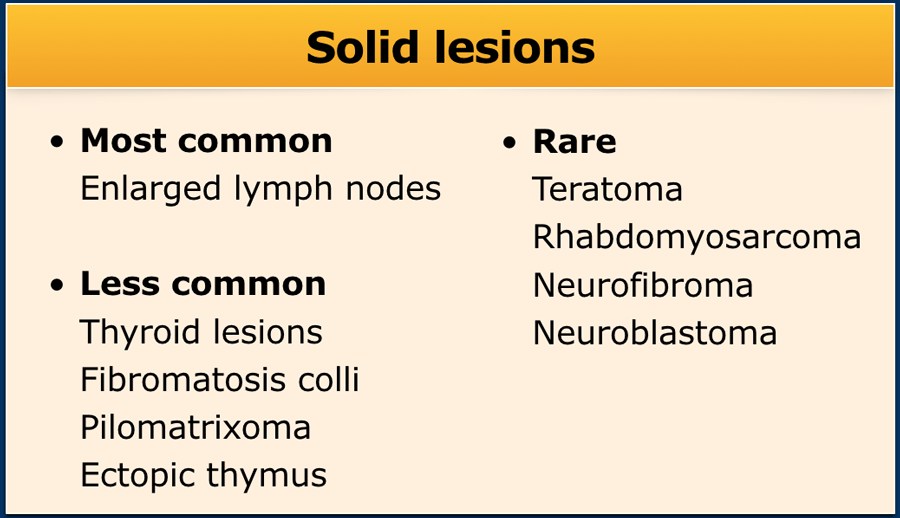
Solid lesions - not lymph nodes
The most common cause of a solid lesion in the neck is an enlarged lymph node as we just discussed.
Other solid lesions in the neck are far less common.
They are listed in the table.
In many cases the imaging findings in a solid lesion will be non-specific and a diagnosis can only be made through biopsy or excision.
Thyroid lesions
Congenital anomalies
The most common anomalie is a partial or complete agenesis of the gland.
In partial agenesis the gland is ectopic and located anywhere between the base of the tongue and the thyroid cartilage.
Mostly near or in the tongue, a lingual thyroid.
Here an image of a newborn with an abnormal thyroid test.
No thyroid gland is visible in the neck, neither in its usual position nor higher up in the neck.
Thyroid nodules
Thyroid nodules are common.
They can be single or multiple.
Some are purely cystic but most are solid.
On ultrasound they are isoechoic with the normal gland.
In a goiter a multitude of solid nodules are seen.
If there is concern about a possible malignancy fine needle aspiration can be done.
Preferably a technician of the cytology department is present to make a quick assessment of the retrieved cells to ascertain that thyroid cells are aspirated, and not only blood.
This is an ultrasound image of a six-year-old girl with a small cyst with a septum in the right thyroid lobe.
It remained unchanged over a year.
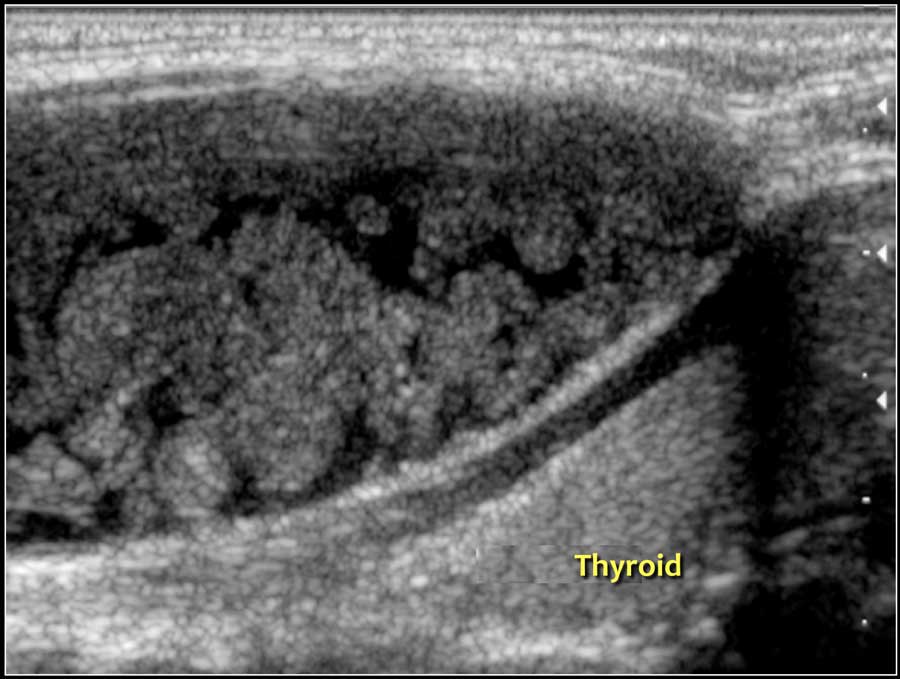
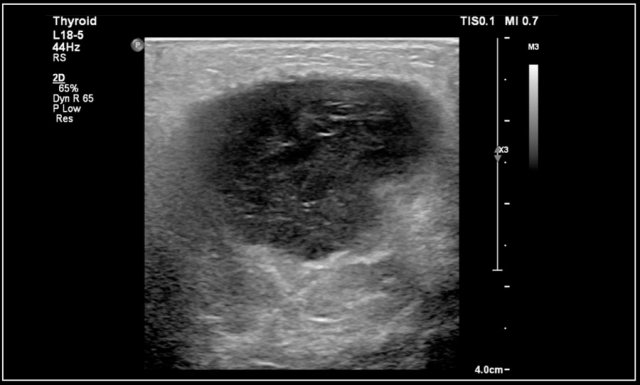
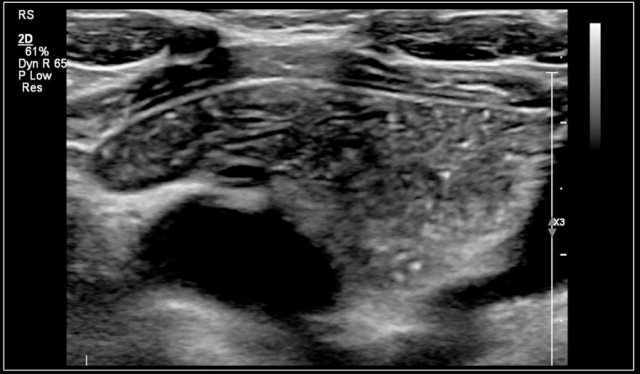
 Hashimoto's thyroiditis: An enlarged thyroid gland with a diffuse inhomogeneous structure and hyperemia is seen in a ten-year-old girl
Hashimoto's thyroiditis: An enlarged thyroid gland with a diffuse inhomogeneous structure and hyperemia is seen in a ten-year-old girl
Thyroiditis
The most common forms of thyroiditis are Hashimoto's thyroiditis and Graves disease.
Both Hashimoto's thyreoiditis and Graves disease can present as an enlarged and hyperemic thyroid.
Hashimoto's thyroiditis or chronic lymphocytic thyroiditis is an auto-immune disease.
It presents with hypothyroidism.
Although primarily a disease of the middle-aged it can present in children.
On ultrasound the gland is diffusely enlarged and inhomogeneous.
On color doppler the blood flow is often normal but can be increased like in Graves' disease.
In a later stage the gland shrinks.
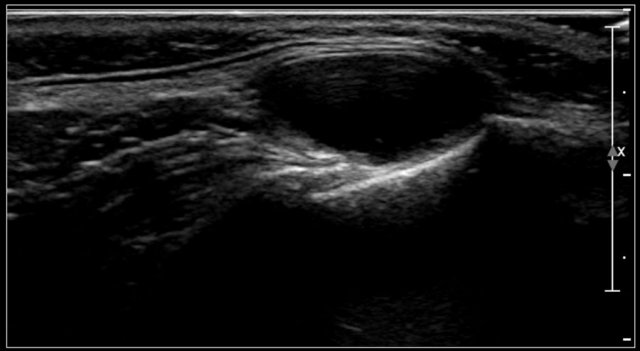
In Graves disease the thyroid gland is also enlarged and shows an increased perfusion.
On color Doppler it has been described as an inferno in red and blue.
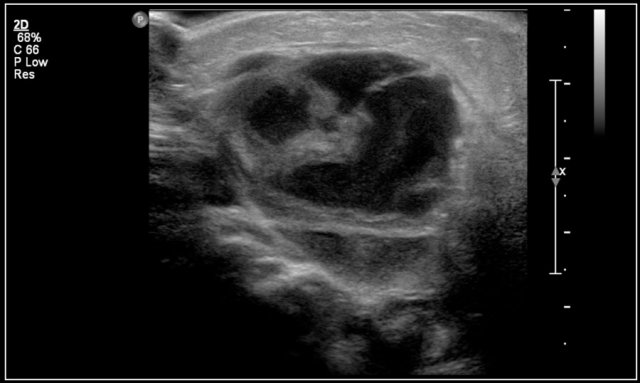
Here an image of a 16-year-old girl with hyperthreoidism.
A diffusely enlarged thyroid gland is seen with hyperemia.
The final diagnosis was Graves disease.
She was treated with I-131.
Thymus
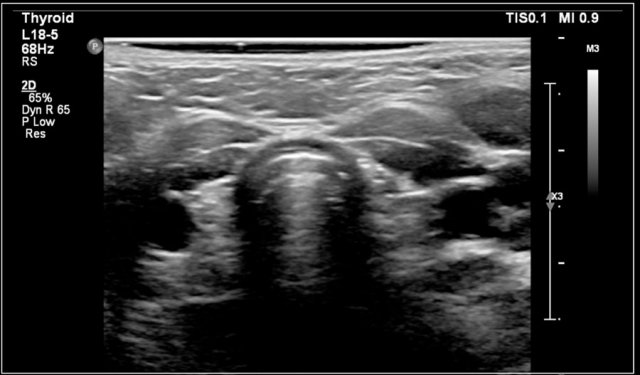
The thymus is located in the upper mediastinum and can be visualized with a suprasternal scan plane.
With increasing age its echogenicity increases and becomes more granular.
Ultrasound is ideal to demonstrate the thymus as a cause of a widened upper mediastinum in infants.
Sometimes the thymus causes a swelling in the suprasternal notch on straining.
Such a herniating thymus can be demostrated with ultrasound.
The thymus is located in the upper mediastinum and can be visualized with a suprasternal scan plane.
Ultrasound image of the thymus in an eight-year-old boy.
Here a video of a six-month-old boy with a mass which was sometimes visible in the suprasternal notch.
While crying the thymus was seen to herniate in front of the trachea.
Ectopic thymus
Ectopic thymic tissue may occur anywhere along the path of descent through the thymopharyngeal duct.
When it presents as a neck mass, it can be mistaken for a tumor.
The ectopic part of the thymus has the same echo characteristics as the normal thymus.
The video shows an ectopic thymic remnant, which was an incidental finding in the neck, detected on a MRI of the brain in a 2-year-old boy.
The ectopic thymus has the ultrasound characteristics as the normal gland.
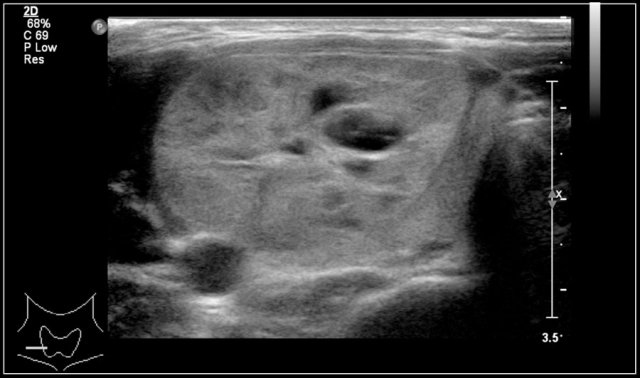
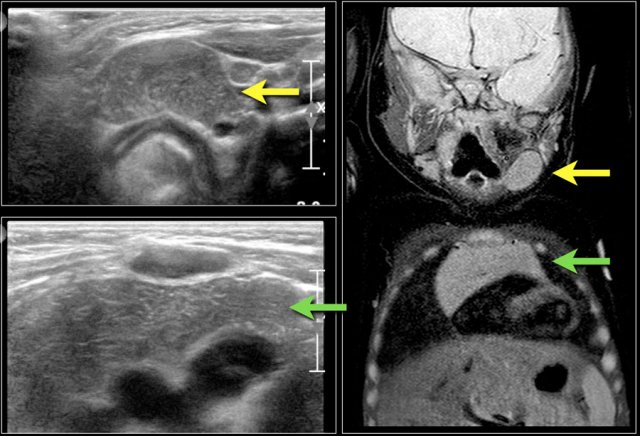
Here images of a six-month old boy with a vocal cord paralysis.
The MRI examination shows a mass between the parotid and submandibular gland (yellow arrow).
The signal characteristics are equal to the thymus (green arrow).
Ultrasound confirmed an ectopic thymic remnant (yellow arrow), with identical sonographic characteristics as the orthotopic thymus (green arrow).
Left: orthotopic thymus; right: ectopic thymus
Fibromatosis colli
Fibromatosis collis is a swelling of the sternocleidomastoid muscle in a newborn.
It is probably caused by pressure necrosis of the muscle during delivery.
Contrary to common belief it is not caused by hemorrhage.
50% of affected babies are born in breech.
The swelling becomes apparent one to three weeks after birth.
Sometimes a torticollis is noted.
The swelling will usually regress spontaneously within a few months.
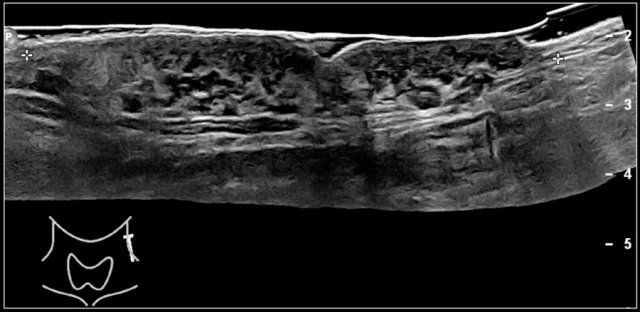
On ultrasound an enlargement of the sternocleidomastoid muscle is seen.
It can affect the whole muscle or part of it.
The sternal head is always affected, and often the cleidal head as well.
It can be hypo-, iso- or hyperechoic.
Longitudinal images of the swelling will demonstrate its muscular origin.
Here a video of a two-month-old boy with a torticollis.
A mass is seen within the enlarged sternocleidomastoid muscle.
The diagnosis is fibromatosis collis
Vascular anomalies
Vascular anomalies are classified into proliferative vascular tumors and vascular malformations.
This classification is important as the treatment is different.
Some vascular tumors will regress spontaneously or after administration of beta-blockers.
Vascular malformations however need excision, sclerosing, or embolisation, if treatment is requested.
The classifications of these lesions is constantly changing and beyond the scope of this article.
A recent article on vascular anomalies provides a new classification (2).
Hemangioma
Hemangiomas are benign vascular neoplasms.
They are the most common tumors of infancy.
60% of hemangiomas are seen in the head-neck regio.
They usually appear in the first weeks after birth, show rapid growth, followed by spontaneous involution.
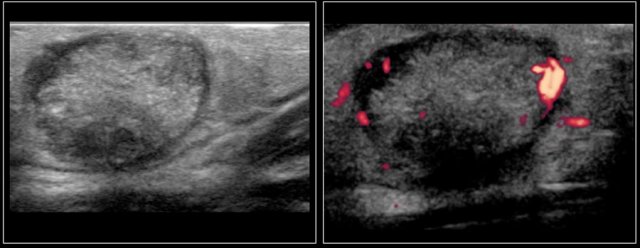
Here we see images of a highly vascular lesion in the left submandibular region, which was present at birth.
Three months later it had decreased in size.
A soft swelling was present on the side of the head in a six-week-old boy.
It was small at birth and showed rapid growth.
This is typical for an infantile hemangioma.
Venous malformation
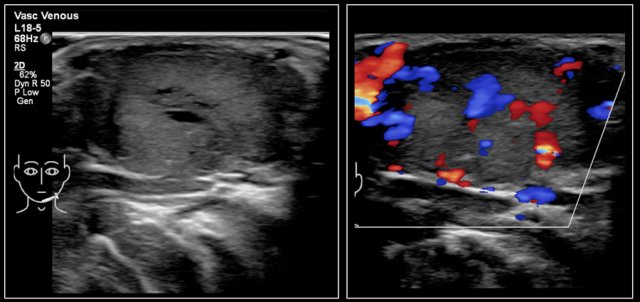
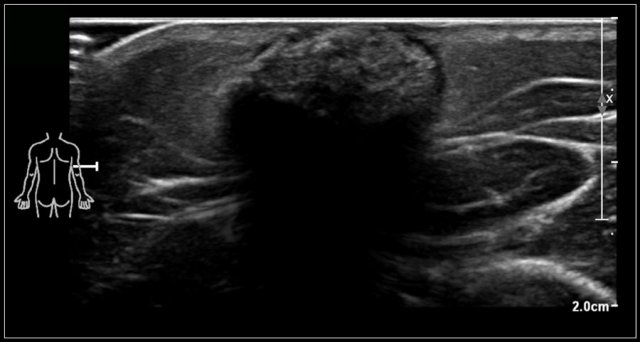
A six-month-old boy presented with a swelling in the left neck at birth.
Several ultrasound examinations could not differentiate between a hemangioma or a venous malformation.
At six months of age, the ultrasound showed a lesion, which was mostly composed of vessels which increased in size on straining.
On color Doppler the lesion showed increased flow while crying.
The final diagnosis on imaging and on clinical examination was a venous malformation.
 Firm tumor in the right temporal area of a 2-year-old boy. Ultrasound shows an echogenic lesion with a well demarcated wall and slight posterior shadowing, characteristic for a pilomatrixoma.
Firm tumor in the right temporal area of a 2-year-old boy. Ultrasound shows an echogenic lesion with a well demarcated wall and slight posterior shadowing, characteristic for a pilomatrixoma.
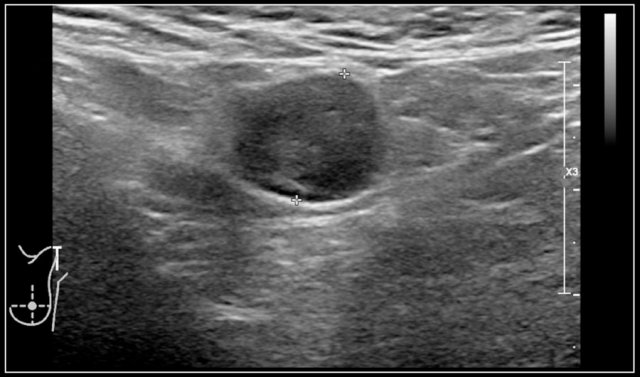
Pilomatrixoma
A pilomatrixoma or epithelial inclusion cyst of Malherbe is a benign skin lesion associated with hairfollicles.
It presents as a firm, mobile, painless swelling.
Sometimes a blue discoloration is present.
They vary in size from a few millimetres to 3 centimetres.
The majority occurs in the head and neck region.
On ultrasound a pilomatrixoma presents as an oval tumor lcated between the cutis and subcutis.
It is hyperechoic, sometimes with calcification and acoustic shadowing.
The wall is often hypoechoic and on color Doppler tiny vessels can be seen in the wall.
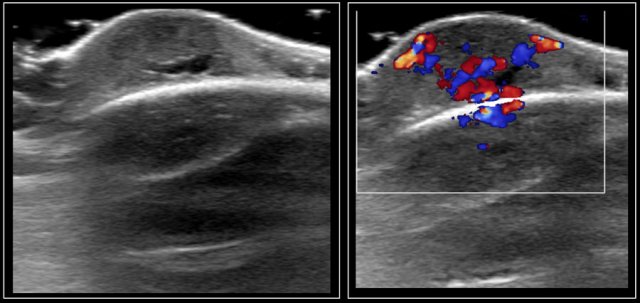
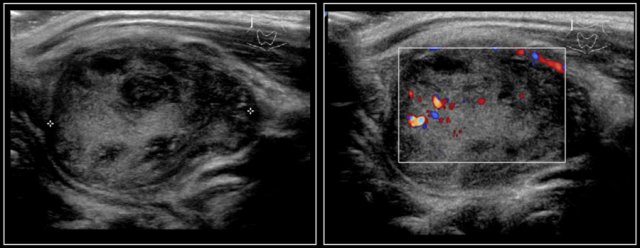
These images are of a firm mass in the neck of a 17-year-old girl.
A cytologic sampling was inconclusive.
Ultrasound shows a typical pilomatrixoma, confirmed at pathology after excision.
Some perfusion in the wall of the pilomatrixoma is seen.
Large pilomatrixoma on the upper arm of a 12-year-old girl.
Salivary glands
Enlargement of the salivary glands can be diffuse or focal.
Diffuse swelling mostly affects the parotid glands.
If it is bilateral it can be caused by autoimmune diseases (like Sjögren's disease) or infections (HIV).
On ultrasound many small hypoechoic lesions are present.
Unilateral swelling can be caused by a bacterial parotitis.
Hemangioma is the most common parotid gland tumor of childhood, which involute in the course of a few months.
Teratoma
Teratomas of the neck are rare in children.
Teratomas are composed of all three germ layers.
They often present at birth.
On ultrasound they are composed of solid and cystic parts and often contain calcifications.
They can have a close connection to the thyroid gland.
If the extension is unclear MRI can be done.
Here we see a midline tumor in the anterior neck of a three-day-old boy.
Calcifications and solid and cystic parts are seen. Pathology was compatible with a mature teratoma.
Paraganglioma
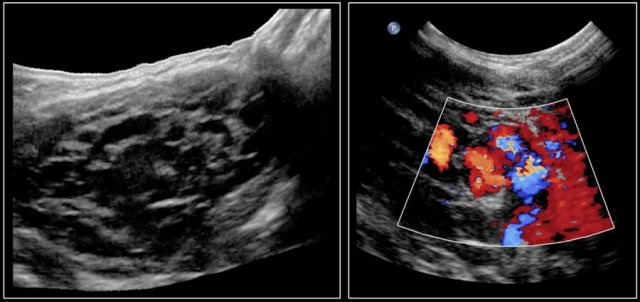
Here images of a 17-year-old boy with a swelling in the neck, thought to represent a branchial cleft cyst.
An echogenic solid mass was seen with moderate perfusion on color doppler examination.
No specific diagnosis could be made.
The final pathologic diagnosis was a paraganglioma, a very uncommon finding in children.
Neurofibroma
Here a large neurofibroma in the subcutaneous tissue in the neck of a 10-year-old boy with a known neurofibromatosis.
Neuroblastoma
Neuroblastoma usually presents as an abdominal mass in young children.
In the neck it accounts for 1-5% of neuroblastomas.
On ultrasound a heterogeneously echogenic mass is seen, often with some calcifications (1).
Here a ten-month-old girl with a lump in the neck.
Ultrasound shows a inhomogeneous mass with some calcifications.
There were also three enlarged lymph nodes with calcifications.
Imaging could not make a definitive diagnosis.
Pathology showed a neuroblastoma.
Video of neuroblastoma.