Pulmonary Hypertension and Thromboembolic disease
Onno Mets¹, Lilian Meijboom¹, Robin Smithuis²
¹University Medical Center Amsterdam and ²Alrijne Hospital in Leiden, the Netherlands
Publicationdate
Pulmonary hypertension (PH) is characterized by elevated blood pressure within the pulmonary arteries, which increases the workload for the right ventricle (RV).
RV failure is the leading cause of morbidity and mortality in these patients. Diagnosis can be challenging, as symptoms often develop gradually and are non-specific (dyspnea, fatigue,
syncope, chest pain, leg edema, or ascites).
Definitive diagnosis requires right heart catheterization—an invasive procedure that is not typically performed in the early stages of the disease.
The radiologist can play a key role in identifying imaging signs of pulmonary hypertension.
Specifically, the radiologist should:
- Recognize imaging features of PH and associated cardiac remodelling.
- Identify congenital cardiovascular anomalies and other thoracic pathologies that may suggest a specific underlying etiology of PH.
- Detect imaging signs of chronic thromboembolic pulmonary hypertension (CTEPH), the only potentially curable form of PH.
We thank Prof.dr.
Harm Jan Bogaard for his comments on the manuscript draft.
Role of Radiology
Steps in diagnosing Pulmonary Hypertension
- Evaluate imaging studies for signs suggestive of pulmonary hypertension (PH).
Do not disregard incidental imaging findings that may indicate the presence of PH. - Subsequently, assess for imaging features that may help determine the underlying etiology of PH. These may include cardiovascular abnormalities, pulmonary parenchymal disease, or evidence of chronic thromboembolic pulmonary hypertension (CTEPH), and can guide the selection of further diagnostic imaging modalities and referral pathways.
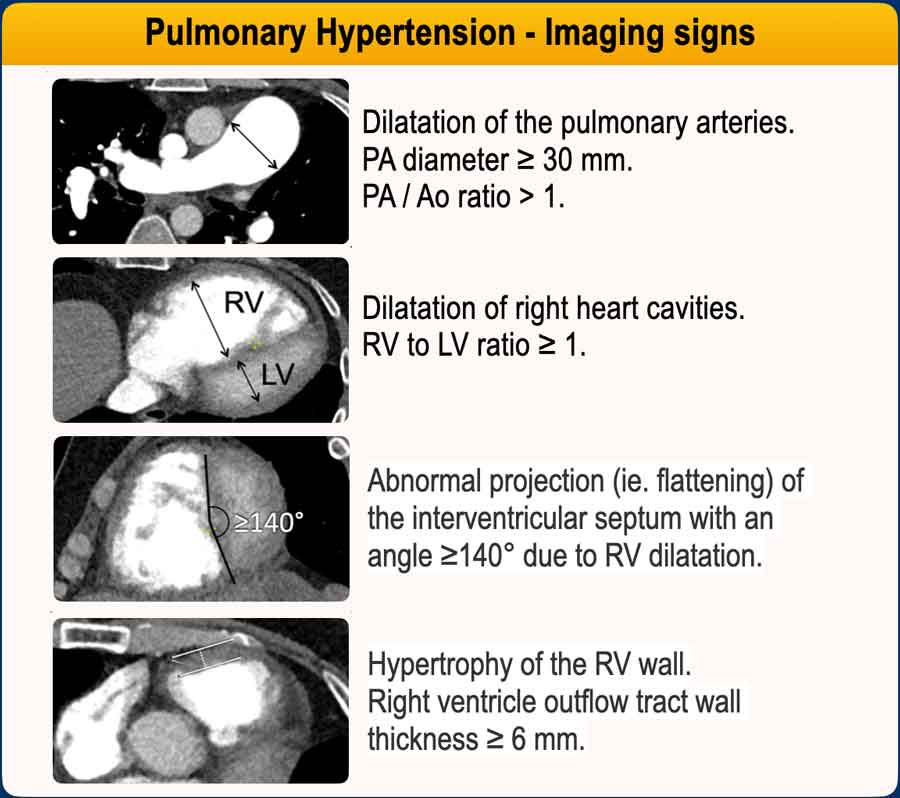
Imaging features of PH
The following imaging findings on CT indicate a high resistance and high pressure in the pulmonary vascular bed, suggestive of PH:
- Main pulmonary artery (MPA) enlargement
MPA diameter >30 mm.
MPA/Ao ratio >1. - Right ventricular dilatation
RV/LV ratio >1 on axial images. - Flattened or bowed interventricular septum
Abnormal projection (ie. flattening) of the interventricular septum with an angle ≥140° on a short axis view. - Hypertrophy of RV wall
Right ventricle outflow tract wall thickness ≥ 6 mm.
Additional findings include:
- Dilated right atrium, which is often seen in chronic pressure elevation.
- Dilatation of the inferior vena cava and hepatic veins, due to elevated right-sided pressures.
- Segmental artery-to-bronchus ratio >1, especially in the upper lobes.
Possible causes of PH
When there is a suspicion of PH, the next step is to look for features that help identify the cause and guide further imaging.
Radiologic approach to identify PH etiology:
- Cardiac causes?
Check for congenital defects (e.g., atrial septal defect (ASD), partial anomalous pulmonary venous return (PAPVR), valvular disease, or pericardial thickening or calcification). - Severe lung disease?
Look for extensive fibrosis or emphysema. - Chronic thromboembolic disease?
Look for filling defects, vessel caliber changes, and/or mosaic attenuation.
PH results from unresolved blood clots that scar and block pulmonary arteries. Identification is important, because chronic emboli can be treated surgically (PEA) or with balloon angioplasty (BPA), making it potentially curable. - Subtle parenchymal signs of pulmonary arterial hypertension (PAH) or pulmonary veno-occlusive disease (PVOD)?
Look for centrilobular ground-glass opacities, smooth interlobular septal thickening, or a dilated main pulmonary artery.
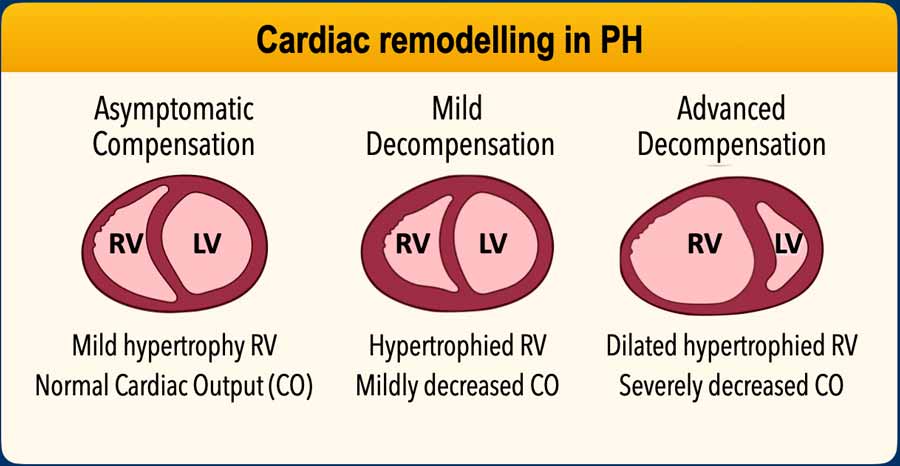
Cardiac remodelling in PH
1. Initial Compensation – Right Ventricular (RV) Adaptation
- Increased pressure in the pulmonary arteries will raise the RV afterload.
- RV hypertrophy: The right ventricle adapts by increasing muscle mass (concentric hypertrophy) to generate higher pressure.
- Preserved function: Initially, this adaptation helps maintain cardiac output.
2. Progressive Strain – Maladaptation
- RV dilatation: Over time, the RV begins to dilate as it struggles to overcome resistance.
- Decreased contractility: The hypertrophied RV eventually weakens, leading to reduced stroke volume.
3. Right Heart Failure
- RV failure: The ventricle can no longer pump effectively.
- Systemic congestion: Leads to liver congestion, ascites, peripheral edema.
- Decreased left heart preload: As the RV fails, less blood reaches the left heart, reducing systemic output.
Dilatation of RV
The images show a normal right and left ventricle compared to a dilated right ventricle.
Proposed cut-off values for right heart dilatation on axial CT:
- Right atrium: ≥ 65mm (women) and ≥ 70mm (men)
- Right ventricle: ≥ 55mm (women) and ≥ 60mm (men)
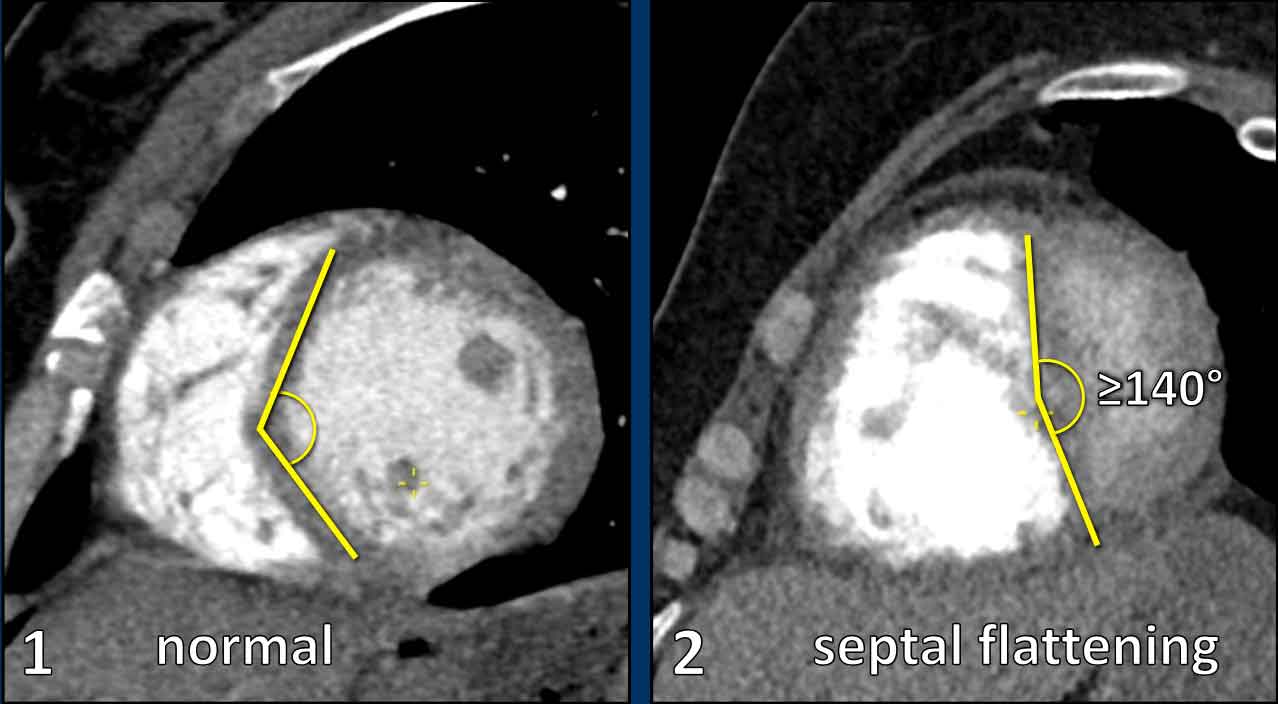
In the short-axis view, a normal left ventricle demonstrates a circular to elliptical configuration.
The interventricular septum contributes to the circular contour of the ventricular wall.
Septal flattening or leftward bowing is indicative of pressure overload and right ventricular dilatation.
Pressure measurements in PH
 Swan-Ganz catheter inserted into the left pulmonary artery to measure the pulmonary arterial wedge pressure (PAWP).
Swan-Ganz catheter inserted into the left pulmonary artery to measure the pulmonary arterial wedge pressure (PAWP).
Under normal conditions, the pulmonary vascular bed is characterized by low resistance and low pressure, and a high blood flow volume.
The definitive diagnosis of pulmonary hypertension is established by right heart catheterization, which is an invasive procedure to measure the pulmonary artery pressure.
PH is diagnosed when the mean pulmonary artery pressure (mPAP) is ≥ 20 mmHg at rest.
Elevated pulmonary arterial pressure can result from:
- Precapillary PH
Increased pulmonary vascular resistance due to small vessel obstruction or loss of pulmonary vasculature as a result of chronic emboli. - Postcapillary PH
Elevated left heart pressures as a result of left-sided heart disease leading to increased pulmonary venous and capillary pressure.
Pulmonary Arterial Wedge Pressure (PAWP)
Also known as wedge pressure—is a key hemodynamic measurement used to estimate left atrial pressure and helps distinguish between pre-capillary and post-capillary PH.
The wedge pressure is measured as follows:
- During right heart catheterization, a catheter (Swan-Ganz) is inserted into a pulmonary artery branch.
- The balloon at the tip is inflated to temporarily occlude the vessel.
- This isolates the pressure distal to the occlusion, which reflects left atrial pressure because there are no valves between the pulmonary capillaries and the left atrium. The wedge pressure will be high in left heart disease and low in other causes of PH.
Pulmonary Vascular Resistance (PVR)
The pulmonary vascular resistance is expressed in Woods Units (mmHg x L/min) and is the resistance that must be overcome for blood to flow through the circulatory system.
It is a variable that reflects the size (diameter and length) of the vascular bed.
It can be calculated by the formula: PVR = (mPAP - PAWP) / CO (cardiac output).
Intravascular pressure measurements through right-sided catherization, as well as clinical and imaging findings, help to subdivide PH into five different groups, as defined by the World Health Organization (WHO).
WHO groups
The WHO classifies pulmonary hypertension (PH) into five groups based on their underlying causes and mechanisms.
Group 1 – Pulmonary Arterial Hypertension (PAH)
PH caused by pathology of the smallest pulmonary arteries, which become narrowed or stiff. This remodelling increases the resistance of the vascular bed, where the right ventricle has to work against, eventually leading to right heart failure. PAH can be idiopathic, inherited or related to conditions like HIV or systemic sclerosis.
Group 2 – PH due to Left Heart Disease
PH due to left heart dysfunction arises from an impaired ability to effectively handle pulmonary venous return. This results in elevated left atrial pressure, which is passively transmitted backward through the pulmonary veins and capillaries, leading to increased pressure in the pulmonary arteries. In advanced stages, secondary remodelling of the pulmonary arterial vasculature may occur, contributing a precapillary component to the disease process.
Group 3 – PH due to Lung Disease or Hypoxia
PH resulting from chronic lung diseases and/or hypoxia leads to narrowing or obliteration of the peripheral pulmonary arteries, thereby reducing the pulmonary vascular bed and consequently increasing vascular pressure.
Group 4 – PH due to pulmonary arterial obstruction
The most common cause of arterial obstruction is chronic thromboembolic pulmonary disease. Although rare, this form is important because it is potentially curable.
Group 5 – PH with Unclear or Multifactorial Causes
PH linked to conditions with complex or unknown mechanisms, such as sarcoidosis, certain hematologic disorders, splenectomy, metabolic diseases, and complex congenital heart defects.
Pressure measurements
In all five WHO groups the mean pulmonary arterial pressure (mPAP) is above 20 mmHg.
In all groups except for PH resulting from left heart disease (group 2) the wedge pressure (PAWP) will be low and the pulmonary vascular resistance (PVR) will be high.
In isolated post-capillary PH resulting from left heart disease or unclear causes (group 2 and 5) the wedge pressure is high and the pulmonary vascular resistance is low.
Sometimes there is a combined pre- and post-capillary PH with a high wedge pressure and a high vascular resistance.
Pulmonary arterial hypertension
PAH
Pulmonary arterial hypertension (PAH) is classified under WHO group 1.
PAH, also known as primary pulmonary hypertension, is a form of pulmonary hypertension caused by pathological changes in the pulmonary arteries, which become thickened, stiffened, or narrowed.
As a result of this arteriopathy, the right side of the heart must work against increased pulmonary vascular resistance. Over time, this leads to right ventricular dysfunction and an inability to maintain adequate pulmonary blood flow.
PAH may be idiopathic (IPAH), heritable (HPAH), or associated with other conditions such as HIV infection, systemic sclerosis, congenital heart disease or PAH with features of venous involvement (PVOD).
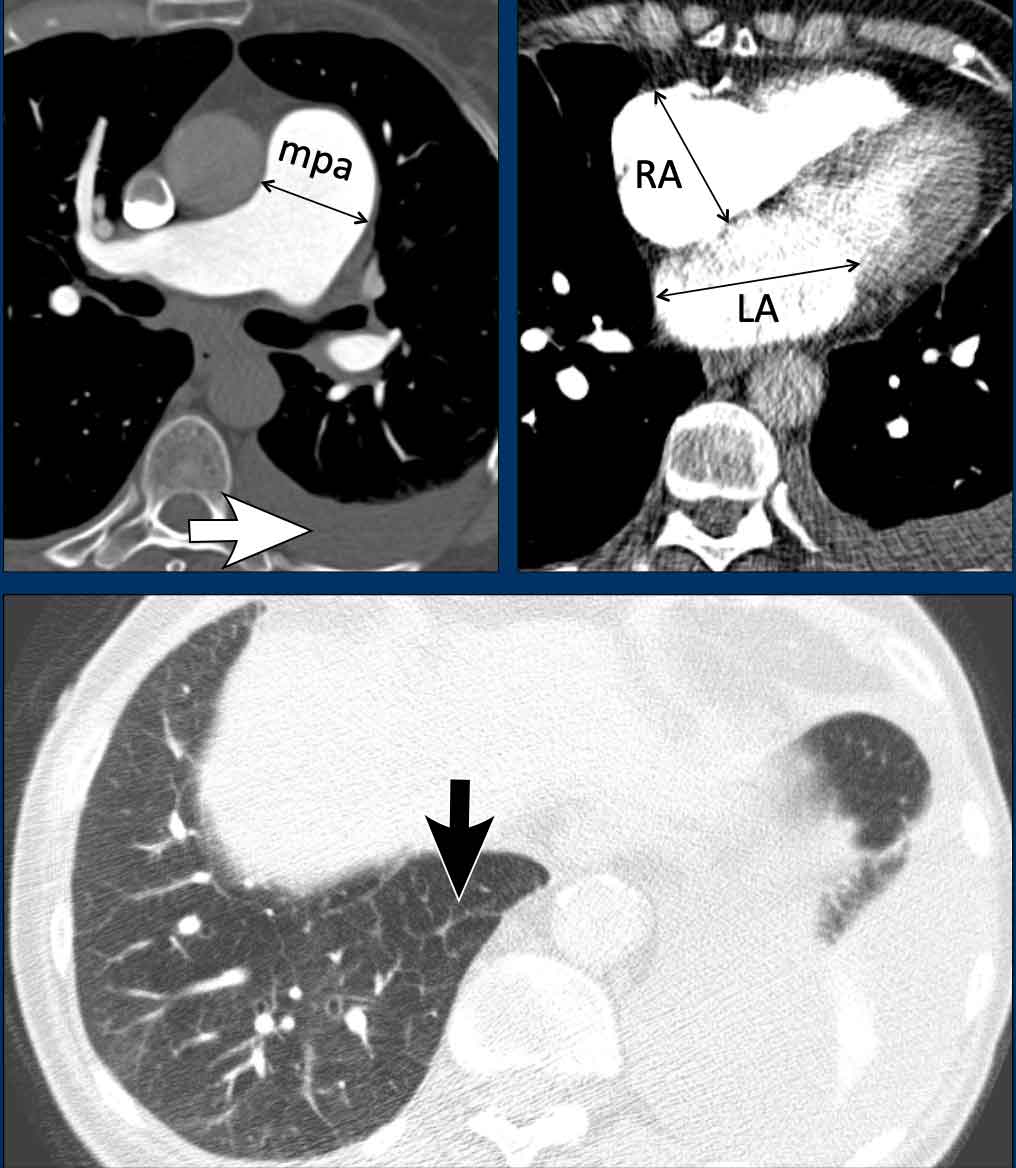
These images are of a young female with idiopathic PAH.
Imaging findings
- Mild dilatation of the main pulmonary artery
- Mild dilatation of the right ventricle.
- Mild wall thickening of the right ventricle outflow tract (arrow).
The left atrium has a normal size. - Normal lung parenchyma.
PVOD
Pulmonary veno-occlusive disease (PVOD) is a rare subtype of PAH.
It is caused by narrowing and obliteration of the small pulmonary veins (venules), as opposed to other causes of group 1 pulmonary hypertension in which the pre-capillary arteries are primarily involved.
The venous occlusion leads to post-capillary pressure build-up and subsequently pulmonary arterial hypertension.
The classic CT triad in PVOD includes:
- Smooth interlobular septal thickening.
- Centrilobular ground-glass opacities.
- Enlarged mediastinal and hilar lymph nodes resulting from chronic lymphatic congestion.
PH due to left heart disease
Pulmonary hypertension due to left heart disease is asseigned to WHO group 2.
It occurs when the left heart is unable to effectively accommodate or eject the blood returning from the lungs.
This results in a backward transmission of pressure into the pulmonary circulation, first leading to elevated pulmonary venous pressure and subsequently also elevated arterial pressure.
It may result from:
- Systolic dysfunction (i.e., impaired left ventricular contraction)
- Diastolic dysfunction (i.e., reduced ventricular filling due to myocardial or pericardial stiffness)
- Severe valvular disease, particularly mitral or aortic valve pathology.
Given the high prevalence of cardiac disease, this is the most common form of pulmonary hypertension.
Images
In this patient with left heart disease the findings are:
- Dilatation of the main pulmonary artery.
- Dilatation of the right atrium and mild thickening of the myocardium of the right ventricle.
- Dilatation of the left atrium
- Pleural fluid (white arrow).
- Smooth interlobular thickening (black arrow).
PH due to cardiac anomalies
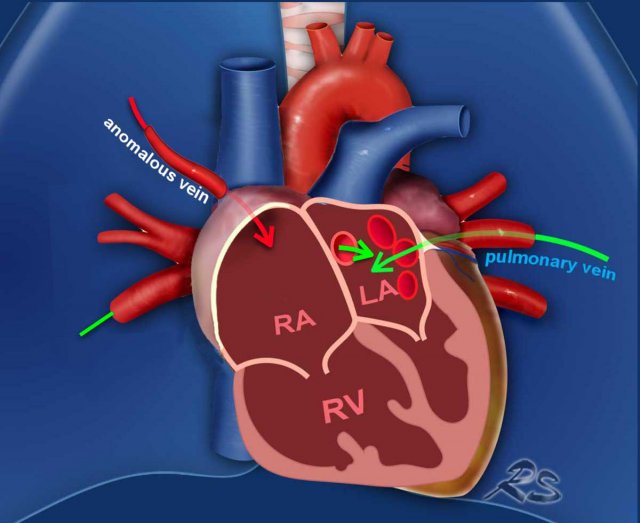
Partial anomalous pulmonary venous return (PAPVR)
In partial anomalous pulmonary venous return, one or more pulmonary veins abnormally drain into the systemic venous circulation (mainly into the superior vena cava on the right, and into the left brachiocephalic vein on the left side), instead of the normal drainage into the left atrium.
Depending on the shunt volume, chronically increased pulmonary circulation from this shunt can result in endothelial injury, smooth muscle hypertrophy, and vascular fibrosis, ultimately leading to elevated pulmonary vascular resistance, and the development of pulmonary hypertension.
Illustration
In this case, most pulmonary veins drain normally into the left atrium (green arrows).
However, the right upper lobe pulmonary vein is anomalous and drains via the superior vena cava into the right atrium rather than the left atrium (red arrow).
This anomalous venous return creates a left-to-right shunt, leading to volume overload of the right atrium and right ventricle.
These images are of a patient with pulmonary hypertension secondary to partial anomalous pulmonary venous return (PAPVR).
Imaging Findings
The right lower lobe pulmonary veins are not connected to the left atrium (LA) but instead drain into the superior vena cava (arrows).
Note the bilateral dilatation of the pulmonary arteries, consistent with elevated pulmonary arterial pressure.
Atrial Septal Defect (ASD)
In an Atrial Septal Defect (ASD), there is a communication between the left and right atrium.
Since left atrial pressure is higher, blood flows from the left atrium to the right atrium.
This increases blood volume in the right heart and pulmonary circulation.
The chronically elevated flow and pressure in the lung circulation causes endothelial damage, vascular remodelling and an increased pulmonary vascular resistance.
Illustration
Example of a sinus venosus superior defect.
This is a subtype of ASD, in which there
is an abnormal interatrial communication between the left atrium and the
superior cavo-atrial junction (arrow).
Since this subtype of ASD frequently coexists with PAPVR, always check for both conditions.
Example of a sinus venosus superior defect.
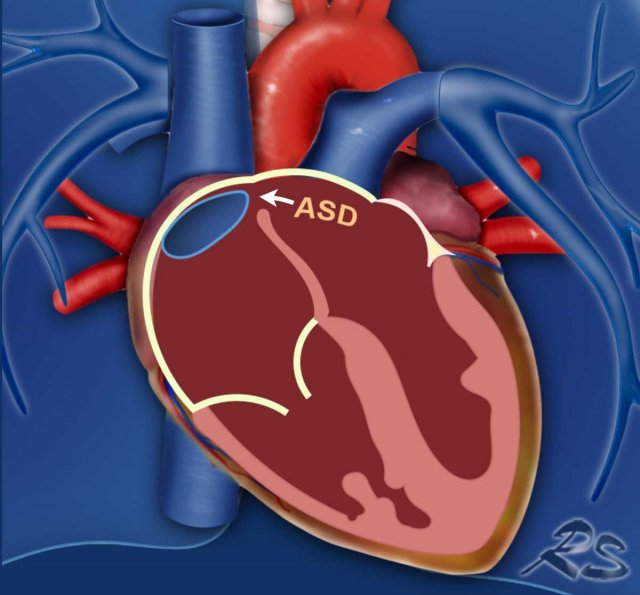
Images
- There is an abnormal communication between the left atrium and the superior cavo-atrial junction (arrow).
- Dilatation of the pulmonary artery.
- Coronal reconstruction demonstrating the abnormal communication between the left atrium and the superior cavo-atrial junction (arrowheads).
- Severe dilatation of the right atrium and ventricle due to the left-to-right shunt.
PH due to lung disease
Pulmonary hypertension secondary to chronic lung diseases and/or hypoxia is categorized under WHO Group 3. It results from both structural and functional alterations in the pulmonary vasculature due to underlying pulmonary pathology. In this context, the small pulmonary vessels may be lost or undergo vasoconstriction and remodelling, leading to a reduced vascular bed and a subsequent increase in pulmonary arterial pressure.
Common etiologies include chronic obstructive pulmonary disease (COPD) and pulmonary fibrosis. Obstructive sleep apnea and chronic exposure to hypoxic conditions at high altitudes may also play a role in its development.
Images
This patient has a combination of
emphysema and pulmonary fibrosis.
The dilated and hypertrophic right ventricle, and flattening of the
intraventricular septum are the result of PH.
Chronic thromboembolic pulmonary hypertension
The most common disease of WHO group 4 (pulmonary arterial obstruction) is chronic thromboembolic pulmonary hypertension (CTEPH).
CTEPH occurs when thrombi fail to fully resolve following an acute pulmonary embolism.
This results in persistent thrombotic obstruction, vascular scarring, and arterial remodelling, which impair pulmonary blood flow and elevate pulmonary artery pressure.
Because these obstructions can potentially be treated with pulmonary endarterectomy (PEA) or balloon pulmonary angioplasty (BPA), CTEPH is the only potentially curable form of pulmonary hypertension.
Imaging findings
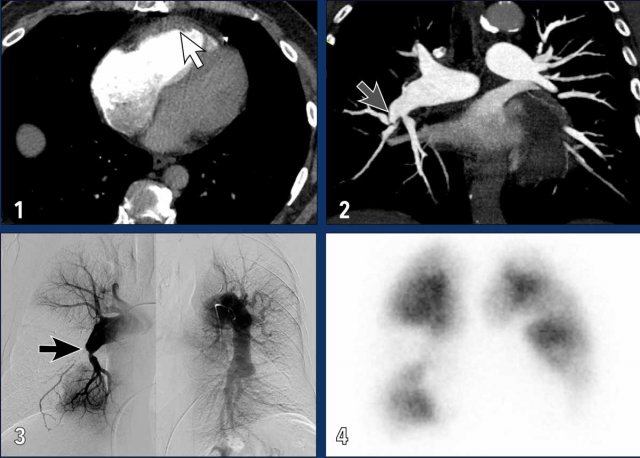
These images are of a patient with severe CTEPH.
- Dilatation of RA and RV with muscular hypertrophy of RV (white arrow).
- Web causing stenosis of this segmental pulmonary artery; one of the features of chronic thromboembolic disease (grey arrow).
- Pulmonary angiogram showing total occlusion (black arrow) and stenosis of segmental pulmonary arteries, with large perfusion defects.
- Wedge shaped perfusion defects on a perfusion scan.
Differentiation Acute vs Chronic Emboli
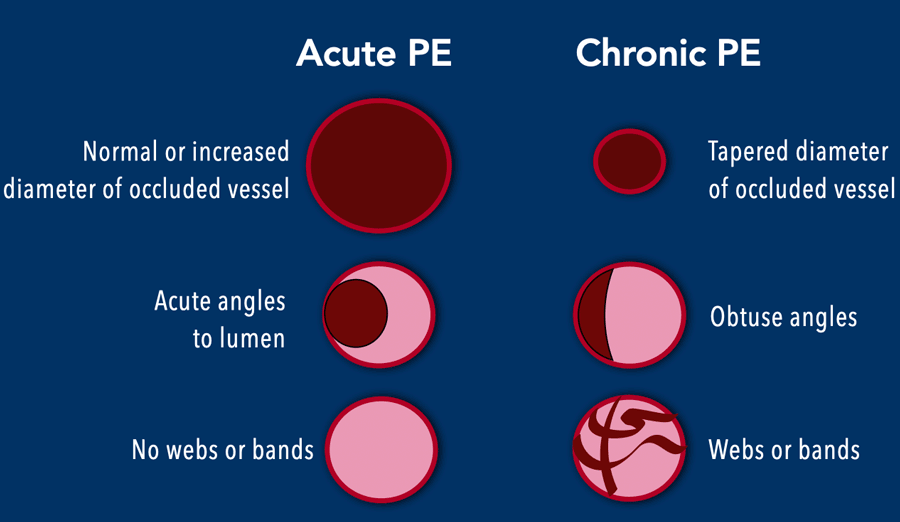
When pulmonary emboli are present, how do we differentiate acute from chronic disease?
- The diameter of occluded vessels in acute PE is normal or slightly increased, while in chronic PE the occluded vessels are tapered.
- Partial filling defects in acute PE typically show acute angles to the vessel lumen, while obtuse angles are seen in chronic disease due to the wall adhering morphology.
- Intraluminal webs and bands may be seen in chronic disease due to partial recanalization of the prior occlusive thrombus.
- Bronchial artery dilatation further points towards longstanding abnormalities in the pulmonary arterial flow, with recruitment of the systemic arterial blood flow as alternate source.
Please note that a combination of cloth morphology may be present, which should point you towards the diagnosis of acute PE on top of pre-existing chronic thromboembolic disease.
This is an important finding that is often overlooked.
Computed tomography pulmonary angiography (CTPA) is the imaging modality of choice for the diagnosis of pulmonary embolism (PE).
When interpreting a CTPA, several outcomes should be evaluated:
- No abnormalities.
- No evidence of PE, but presence of alternative pathology (cardiovascular or non-cardiovascular) suggesting the underlying etiology of pulmonary hypertension.
- Acute pulmonary embolism, with or without hemodynamic compromise due to flow obstruction.
- Acute-on-chronic thromboembolic disease.
- Chronic thromboembolic disease (CTED) without radiologic signs of pulmonary hypertension.
- CTED with radiologic signs of pulmonary hypertension (suggestive of CTEPH).
Diagnosis of CTEPH
For the definitive diagnosis of CTEPH, the following criteria are required:
- CT findings consistent with chronic thromboembolic disease.
- Intravascular measurements confirming the presence of pre-capillary pulmonary hypertension.
- Mismatched perfusion defects on ventilation/perfusion (V/Q) scan or SPECT/CT perfusion imaging.
- A history of continuous anticoagulation therapy for at least 3 months.
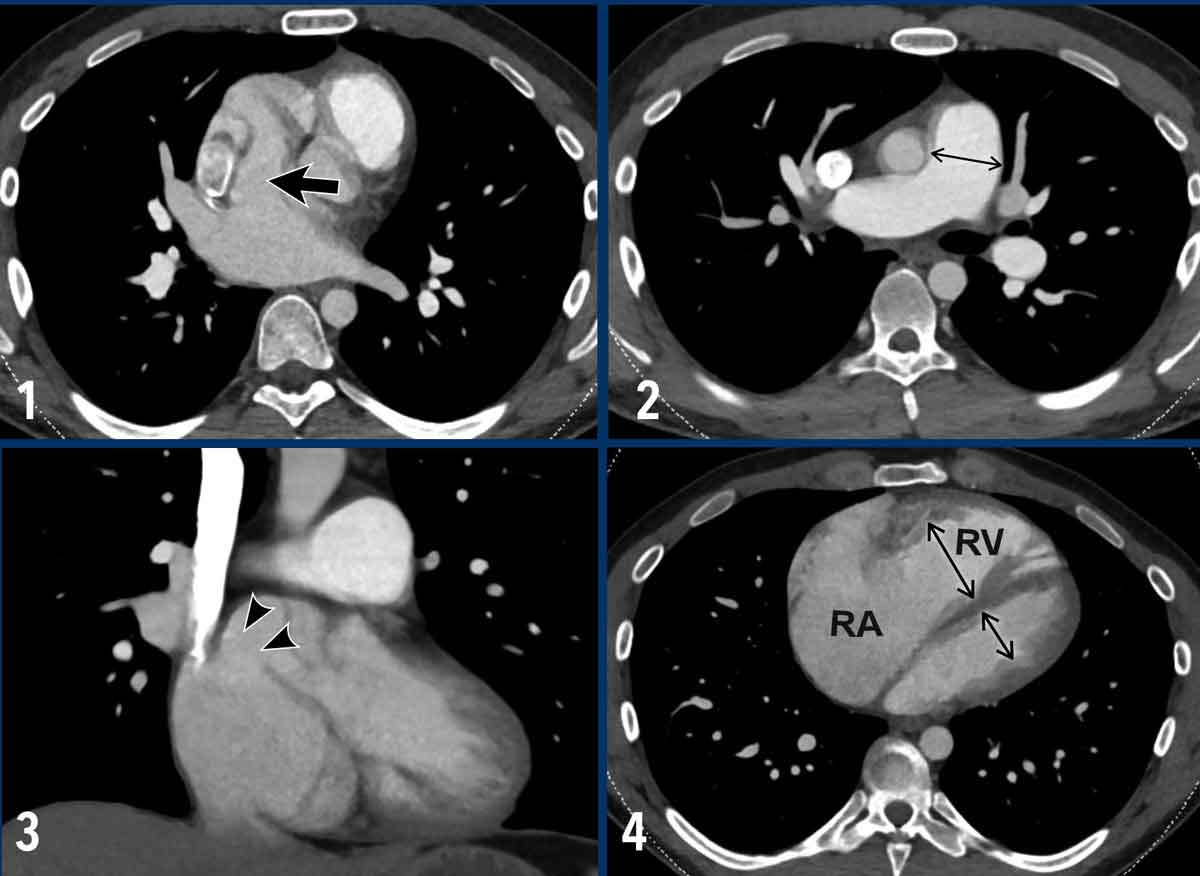
Cardiac remodelling in pulmonary emboli
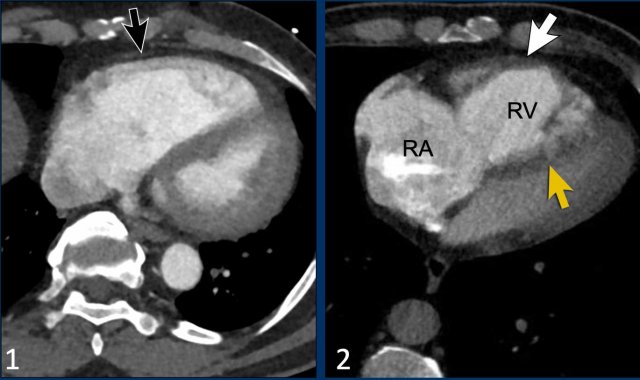
Looking at remodelling of the right ventricle can help to differentiate between acute and chronic emboli.
Here we have two examples of patients with pulmonary emboli and cardiac remodelling.
Images
- There is right ventricular dilatation with septal flattening, but no evidence of RV wall hypertrophy (black arrow), consistent with an acute increase in RV afterload.
This can be seen in patients with acute pulmonary embolism. - In contrast, in this patient there is dilatation of the right ventricle and atrium with interventricular septal flattening, accompanied by RV wall thickening (white arrow).
This suggests chronic pressure overload and is indicative of longstanding pulmonary hypertension.
This can be seen in patients with chronic thromboembolic pulmonary hypertension.
Bronchial artery hypertrophy in CTEPH
Bronchial artery dilatation further suggests longstanding abnormalities in pulmonary arterial flow, with recruitment of systemic arterial circulation as an alternative source of pulmonary perfusion.
Image
Dilatation of bronchial arteries (arrows) in a patient with PH.
Notice the widened pulmonary arteries.
Pulmonary endarterectomy (PEA)
Pulmonary endarterectomy for CTEPH is a surgical and technically demanding procedure - performed under cardiopulmonary bypass and deep hypothermic circulatory arrest - to remove organized thromboembolic material from the pulmonary arteries.
Imaging
- Pre-endarterectomy (Images 1-2): wall adhering thrombotic material is seen in both the right and left pulmonary arteries (indicated by white arrows). Notable dilatation of the main pulmonary artery (asterix) and hypertrophy of the wall of the right ventricular outflow tract (green arrowhead) is also present.
- Post-endarterectomy (Images 3-4): The pulmonary arteries on both sides are cleared of thrombotic material.
This is the organized thrombotic material that was excised from both the right and left pulmonary arteries, including the segmental branches.
Balloon Pulmonary Angioplasty (BPA)
Balloon Pulmonary Angioplasty (BPA) is a catheter-based interventional procedure used to treat CTEPH.
BPA is a minimally invasive alternative to surgery for patients with:
- Inoperable CTEPH (e.g., distal disease not accessible by surgery).
- High surgical risk.
- Residual pulmonary hypertension after pulmonary endarterectomy (PEA).
Images
Before BPA there is acute tapering and occlusion of a basal segmental pulmonary artery of the right lower lobe.
After BPA the artery is patent, with restored flow into the segmental arteries.
Pulmonary artery sarcoma
The most important mimicker of chronic thromboembolic disease is pulmonary artery sarcoma, a rare primary malignant tumor arising from the vessel wall.
It typically presents as a central filling defect within the pulmonary artery and may initially be mistaken for thrombus.
Although signs of flow obstruction and right heart strain may be present, right ventricular hypertrophy is often absent due to the rapid progression of the tumor.
Imaging features suggestive of a pulmonary artery sarcoma include:
- An expansile intraluminal mass, which may have an extravascular infiltrative component.
- Involvement of the pulmonary valve and/or right ventricular outflow tract.
- Absence of ancillary signs of chronic thromboembolic disease.
- Enhancement after contrast administration.
- FDG-PET avidity (frequent, but may be low or absent).
- Growth despite anticoagulant therapy.
Images
- There is a large filling defect within the central pulmonary arteries.
- Notably, there is no distinct right ventricular hypertrophy or dilatation.
- Progressive size despite anticoagulation therapy.
- Metabolic activity on FDG-PET imaging.
Conclusion
Pulmonary hypertension (PH) is a relative rare but very important disease. Since initial signs of PH may appear incidentally on imaging, radiologists play a vital role in recognizing the condition.Thrombus morphology in thromboembolic disease and cardiac remodelling are important imaging clues. Identifying these signs can help diagnose CTEPH, which is the only potentially curable form of PH.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a gift.