MRI examination
Ivo Schoots, Mario Maas and Robin Smithuis
Radiology department of the AMC in Amsterdam and the Rijnland hospital in Leiderdorp, the Netherlands
Publicationdate
Diabetes-related foot problems like osteomyelitis and Charcot neuro-osteoarthropathy are associated with a high morbidity and high healthcare costs.
A red hot foot in a patient with diabetic neuropathy is a diagnostic problem.
In this overview we will focus on two questions:
- Is this an active Charcot foot or is it osteomyelitis?
- Is this a Charcot foot with superimposed infection?
Overview
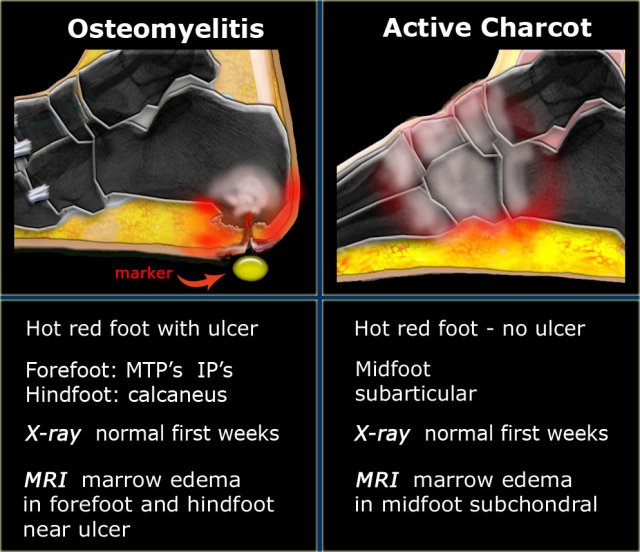
Osteomyelitis versus Charcot
Osteomyelitis:
Osteomyelitis in a diabetic with neuropathy is infection of the bone that usually results from contiguous spread of a skin ulcer.
Consequently, the most common location for osteomyelitis is not in the midfoot, but at the pressure points of the forefoot (metatarsal heads, IP joints) and in the hindfoot at the plantar aspect of the posterior calcaneus.
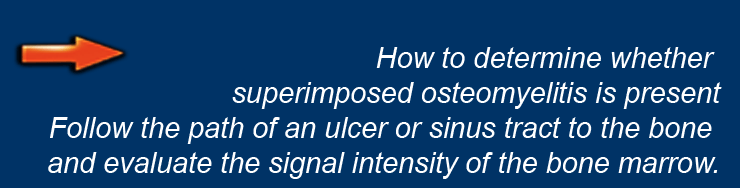
To determine whether osteomyelitis is present, place a marker on the ulcer or sinus tract and track it down to the bone and evaluate the MR- signal intensity of the marrow (1).
Active Charcot:
Unlike osteomyelitis, Charcot neuro-osteoarthropathy is primarily an articular disease, which is most commonly located in the midfoot.
In the early stage radiography will not demonstrate bone abnormalities, but MRI will show subchondral bone marrow edema.
The subcutaneous soft tissues are not typically involved.
Signal intensities on MRI will not discriminate between active Charcot Joint and osteomyelitis.
Location, i.e. bone or joint and ulcer or not, are the clues to the right diagnosis.
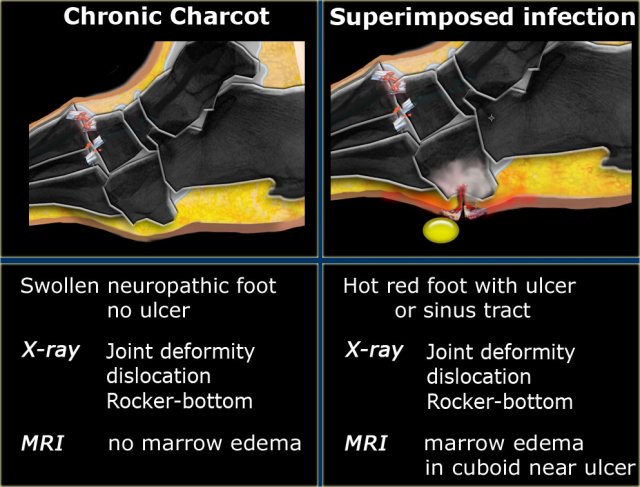
Chronic stage of Charcot:
The chronic stage of Charcot no longer shows a warm and red foot, but the edema usually persists.
Joint deformity, subluxation and dislocation of the metatarsals lead to a rocker-bottom type deformity in which the cuboid becomes a weight-bearing structure.
The deformity of the foot with abnormal pressure distribution on the plantar surface coupled with reduced or loss of sensation, makes the foot vulnerable and leads to callus and blister formation aswell as foot ulceration.
Charcot with superimposed osteomyelitis:
Foot ulceration can subsequently lead to infections, such as cellulitis and osteomyelitis, and this may eventually lead to amputation.
The simplest method to determine whether osteomyelitis is present is to follow the path of an ulcer or sinus tract to the bone and evaluate the signal intensity of the bone marrow (1).
Osteomyelitis in chronic Charcot is usually located in the midfoot, while osteomyelitis in diabetic neuropathy without Charcot is usually in the forefoot and hindfoot.
Osteomyelitis
While diagnosing osteomyelitis is important, it is unfortunately also difficult.
Clinical and laboratory signs and symptoms are generally unhelpful.
The clinical diagnosis relies on the identification and characterization of an associated foot ulcer, a method that is often unreliable.
It is important to mark the skin or subcutaneous abnormality, i.e. ulcer or sinus tract and to find its relation to the area of bone abnormality.
The probe-to-bone test, i.e. palpation of bone with a sterile blunt metal probe in the depths of infected pedal ulcers was thought to be highly correlated with ostemyelitis.
In later studies, however, it had a relatively low positive predictive value (7).
On plain radiographs, bone infection may not show up on the first 2 weeks and in a later stage the radiographic characteristics of neuro-osteoarthropathy and osteomyelitis overlap.
In both cases there will be demineralization, destruction and periosteal reaction of the bones, particularly when neuro-osteoarthropathy presents at a later stage.
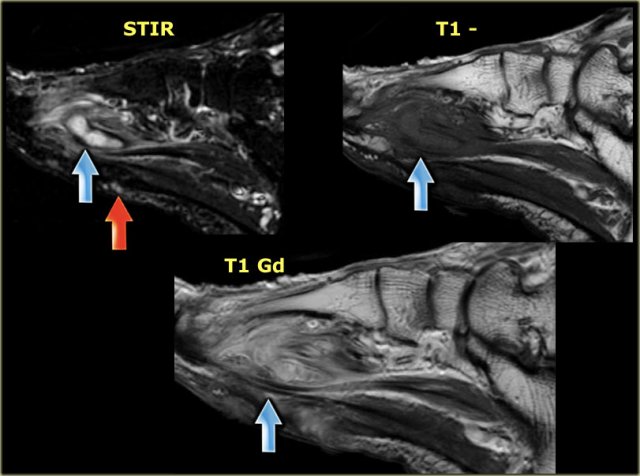
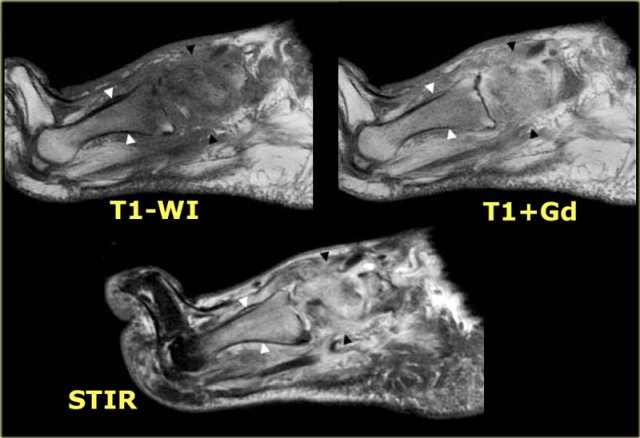
Here, images of a patient with a small cutaneous defect and subcutaneous edema at the metatarsals.
A secondary sign, an abscess, is shown in the forefoot, with high signal intensity on STIR, low or intermediate signal on intensity T1W, and ring-enhancement of the borders showing high signal intensity on T1+Gd.
Charcot neuro-osteoarthropathy
Charcot neuro-osteoarthropathy is a degenerative disease with progressive destruction of the bones and joints.
It is seen in patients with neurological disorders with sensory loss of the feet, including tabes dorsalis, leprosy, diabetic neuropathy, and other conditions involving injury to the spinal cord.
In 1868 Jean-Martin Charcot gave the first detailed description of the neuropathic aspect of this condition in a patient with syphilis.
Today, diabetes mellitus is the most common etiology associated with Charcot osteoarthropathy, with the joints of the foot and ankle being most commonly affected.
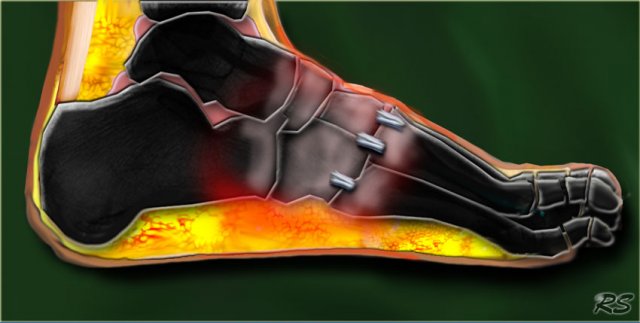
Here an illustration with the key MR-features of acute Charcot neuro-osteoarthropathy:
- Subarticular marrow edema in the midfoot
- Subcutaneous soft tissues are relatively uninvolved.
The exact nature of Charcot arthropathy is unknown.
The neurotraumatic theory states that Charcot arthropathy is caused by an unperceived trauma to an insensate foot. The sensory neuropathy renders the patient unaware of the osseous destruction that occurs with continuous ambulation.
The neurovascular theory suggests that the underlying condition leads to the development of autonomic neuropathy, causing the extremity to receive an increased blood flow, which in turn results in a mismatch in bone destruction by increased osteoclastic activity and bone synthesis (1).
The image shows a progressive neuro-osteoarthropathy of the tarsometatarsal joints (Lisfranc dislocation) with subchondral cysts, erosions, joint distention and dislocation.
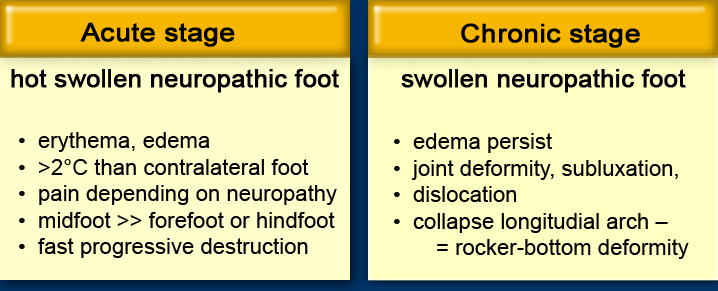
Acute Charcot
Acute active Charcot neuro-osteoarthropathy is defined by clinical signs.
There should be neuropathy and a warm and swollen foot.
The skin temperature should be 2?C or more at the site of maximum deformity of the affected foot compared with a similar site on the contralateral foot.
Osteomyelitis should be excluded and fever is not present.
Serum C-reactive protein level is normal or only a slightly elevated.
The differential diagnosis is infection (osteomyelitis, cellulitis, septic arthritis), inflammation (gout, rheumatoid arthritis) and deep vein thrombosis.
In this early stage, radiographic abnormalities are not present.
The acute stage of Charcot neuro-osteoarthropathy shows rapid and progressive bone and joint destruction within days or weeks.
Immobility by total contact casting can prevent further bone and joint destruction.
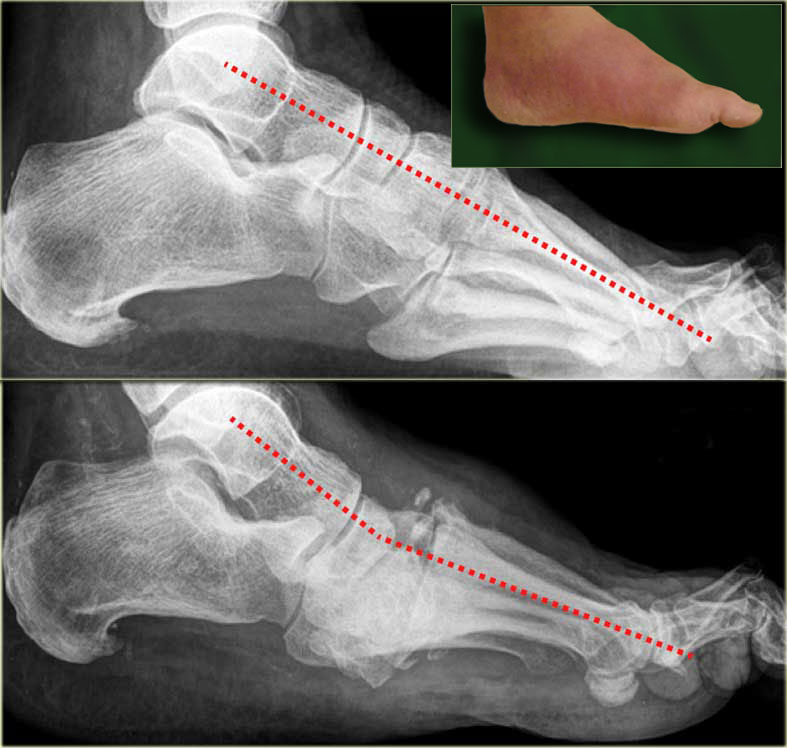
Here a radiograph of a patient with diabetic neuropathy and a red hot foot.
In the acute stage, the radiographs are normal and may not exclude the diagnosis of acute Charcot neuro-osteoarthropathy.
Within 4 months there is progressive decrease of calcaneal inclination with equinus deformity at the ankle.
There is destruction of the tarsometatarsal joint with the typical rocker-bottom deformity.
Bony debris is seen on the dorsal aspect of the foot.
In the acute stage, MRI shows only subchondral bone marrow edema.
Here MRI images of a patient with acute Charcot neuro-osteoarthropathy.
The bone marrow edema typically is not restricted to one or two bones, but is seen in the entire midfoot.
Bone marrow edema and its enhancement are typically centered in the subchondral bone, suggesting articular disease.
The subcutaneous tissues are relatively normal and there is no ulcer or other signs of infection.
Chronic Charcot
The chronic inactive stage no longer shows a warm and red foot.
The edema usually persists.
Crepitus, palpable loose bodies and large osteophytes are the result of extensive bone and cartilage destruction.
Joint deformity, subluxation and dislocation of the metatarsals lead to a rocker-bottom type deformity in which the cuboid becomes a weight-bearing structure.
This results in excessive skin callus formation, blisters and foot ulceration.
At the stage of chronic inactive Charcot osteoarthropathy, bone healing and change of active periosteal reaction will proceed into inactive periosteal reaction and sclerotic borders.
The classic radiographic description of neuro-osteoarthropathy is that of the five D' s.
Debris may be present and effusions may decompress along fascial planes, carrying bony debris far from the joint.
Dislocation is the result of ligamentous laxity.
On the far left, a normal radiograph in the acute stage of Charcot.
Subsequently progressive Charcot neuro-osteoarthropathy is seen with dislocation of the Lisfranc joint.
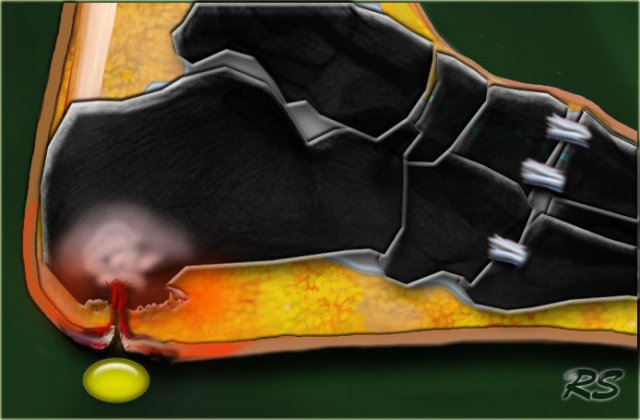
Charcot with superimposed osteomyelitis
To determine whether osteomyelitis in a Charcot foot at MR imaging is present, follow the path of an ulcer or sinus tract to the bone and evaluate the signal intensity of the bone marrow.
If there is bone marrow edema, osteomyelitis is very likely.
If there is bone marrow edema in the absence of a cutaneous defect, active Charcot may be present.
If it is normal, both active Charcot as well as osteomyelitis is not likely.
 Charcot foot with rocker-bottom deformity and ulceration beneath the bony protuberance of the cuboid
Charcot foot with rocker-bottom deformity and ulceration beneath the bony protuberance of the cuboid
On the left a typical rocker-bottom deformity of the foot due to collapse of the longitudinal arch.
Abnormal pressure on the cuboid has led to ulceration.
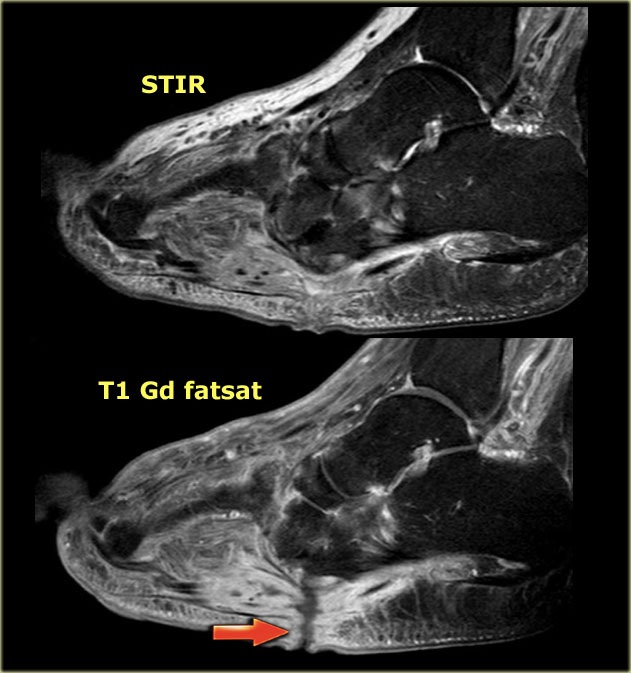
 STIR and T1W images in Charcot neuro-osteoarthropathy with a plantar ulcer (asterix) and osteomyelitis of the cuboid.
STIR and T1W images in Charcot neuro-osteoarthropathy with a plantar ulcer (asterix) and osteomyelitis of the cuboid.
In a patient with Charcot neuro-osteoarthropathy and a rocker-bottom foot, the cuboid bone is an important location of osteomyelitis.
If the T1-weighted image at that location shows low signal intensity in combination with a cutaneous defect, osteomyelitis is extremely likely.
On the left STIR and T1-weighted images of a patient with active Charcot neuro-osteoarthropathy with a plantar ulcer along the bony protuberance of the cuboid.
There is abnormal signal intensity in the cuboid bone next to the ulcer, indicative of osteomyelitis.
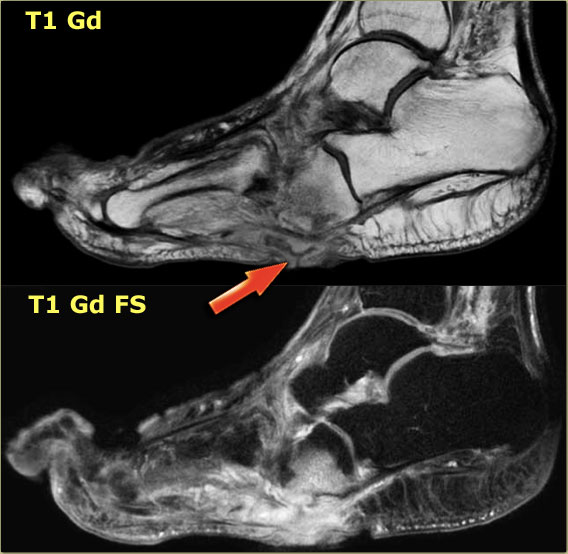
Here the contrast enhanced images with and without fat saturation.
Enhancement of the cuboid bone and adjacent soft tissues on postcontrast images, together with the plantar ulcer, makes osteomyelitis very likely.
On the left a patient with Charcot neuro-osteoarthropathy with a subcutaneous fistula tract (arrow).
This patient has subcutaneous edema and swelling.
When we follow the fistula tract to the bony protuberances of the cuboid, there is no marrow edema at the midfoot.
This makes yet osteomyelitis unlikely.
Ghost sign
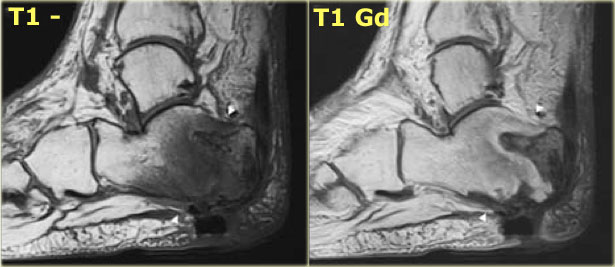
The ghost sign is indicative of neuro-osteoarthropathy with superimposed osteomyelitis.
The "ghost sign" refers to poor definition of the margins of a bone on T1-weighted images, which become clear after contrast administration.
Here, a patient with neuro-osteoarthropathy and superimposed osteomyelitis.
The areas of osteomyelitis are more pronounced on the contrast-enhanced T1-weighted image as compared to the native T1-weighted image.
The bone marrow edema, which is of low signal intensity on the T1-weighted image without contrast enhances and becomes as bright as normal bone marrow.
MRI protocol
The MRI examination includes special attention for positioning of the foot. It must be placed in the center of the magnet, to obtain homogeneous fat suppression.
Markers have to be placed over ulcers or sinus tracts.
T1 and STIR or T2 fatsat sequences are needed.
Because of the curvature of the foot, fat suppression is more uniform with the use of STIR than with T2- weighted imaging with chemical fat saturation.
However, STIR cannot be combined with contrast administration.
As an alternative to spectral fat saturation technique, Dixon chemical shift imaging is described (8).
Sagittal views are for evaluation of midfoot involvement, the plantar surface and the posterior calcaneus.
A view parallel to the toes is adequate for imaging the metatarsophalangeal and interphalangeal joints.
Contrast is used to better depict devitalized regions, abscesses, sinus tracts and joint or tendon involvement.