TI-RADS - Thyroid Imaging Reporting and Data System
Habib Ahmad and Aad van der Lugt
Radiology department of the Erasmus Medical Center in Rotterdam
Up to 67% of the population evaluated with US will have an incidental thyroid nodule.
The high prevalence of thyroid nodules combined with the generally indolent growth of thyroid cancer present a challenge for optimal patient care.
The Thyroid Imaging Reporting and Data System (TI-RADS) of the American College of Radiology (ACR) was designed in 2017 with the intent to decrease biopsies of benign nodules and improve overall diagnostic accuracy.
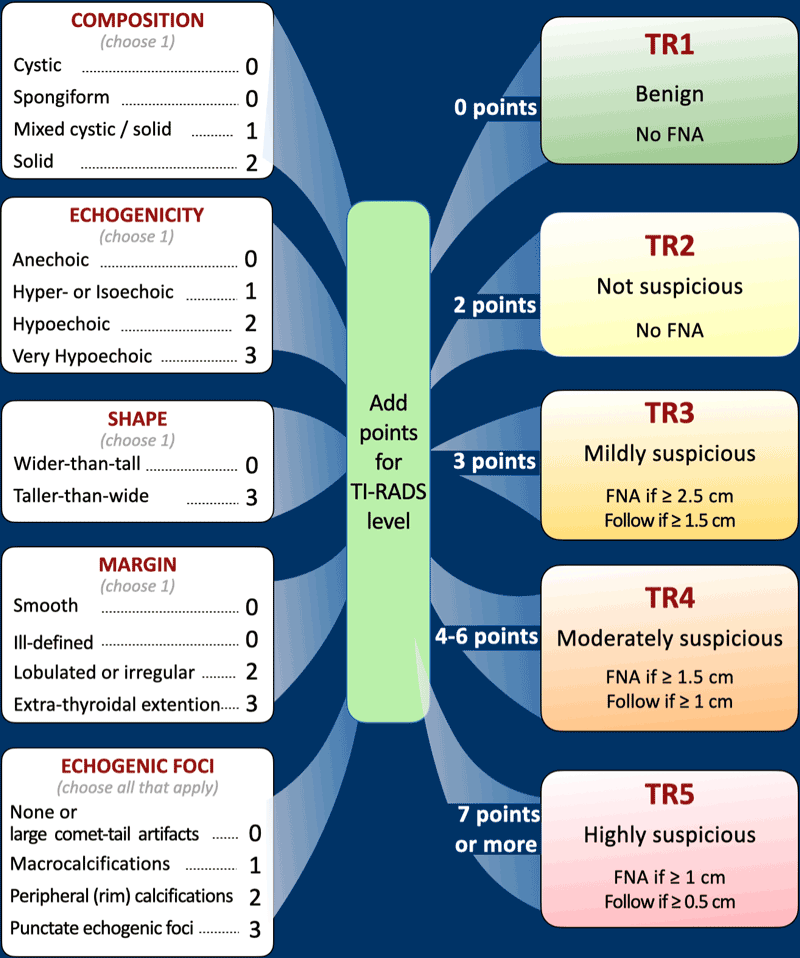
TI-RADS categories
The five ultrasound features of thyroid nodules used in TI-RADS are: composition, echogenicity, shape, margin and punctate echogenic foci. Each item is given points.
The points are added from all categories to determine the TI-RADS level, each with a recommendation.
Nodules smaller than 5 mm do not need any follow-up, even if they are TI-RADS 5.
This is because it is very unlikely that nodules smaller than 5 mm will become a clinical significant malignancy.
The cutoff point of 2.5 cm for fine needle aspiration (FNA) in mildly suspicious TR3 lesions is based on studies showing that thyroid carcinomas don’t have a decreased survival until they reach this threshold value.
The ACR-TIRADS category has been shown to have good correlation with the malignancy risk in large studies.
The risk of malignancy is:
- TR1: 0.3%
- TR2: 1.5%
- TR3: 4.8%
- TR4: 9.1%
- TR5: 35%
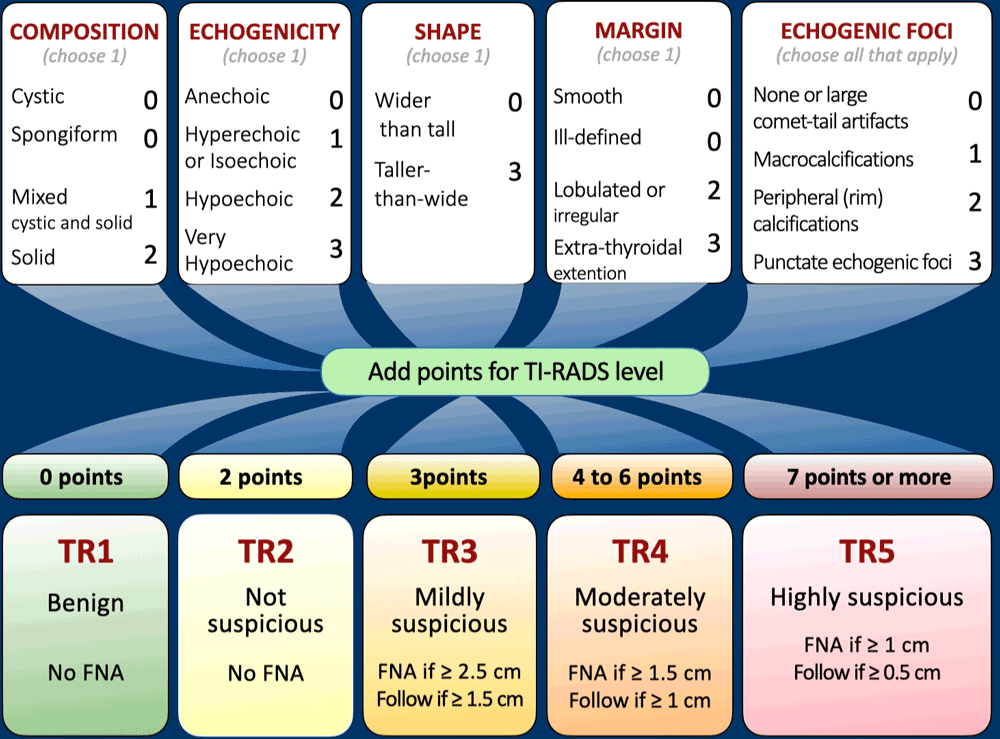
This table is the horizantal version.
Click for a larger image.
There are several exceptions for TI-RADS, where this system cannot be used for.
Each of these exceptions have a greater risk of thyroid cancer than the otherwise normal adult population:
- Children
- FDG-PET avid thyroid nodules
- Lymphadenopathy
- Known risk factors for thyroid malignancy, like MEN type 2
Composition
Cystic lesions or lesions that are almost completely cystic are benign and no further points will be added (TI-RADS 1).
This is also true for spongiform lesions which are always benign and no further characterization using ultrasound features is needed.
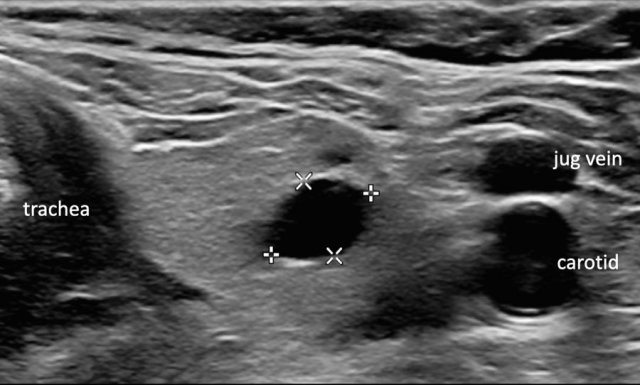
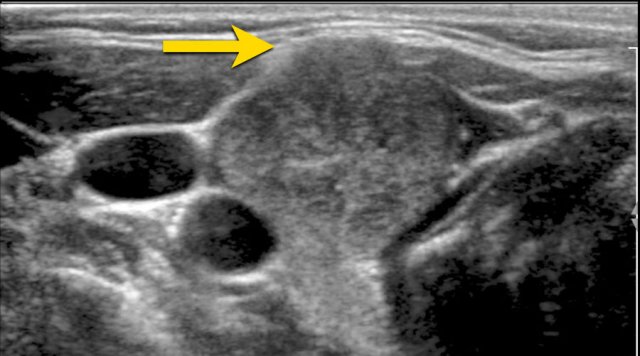
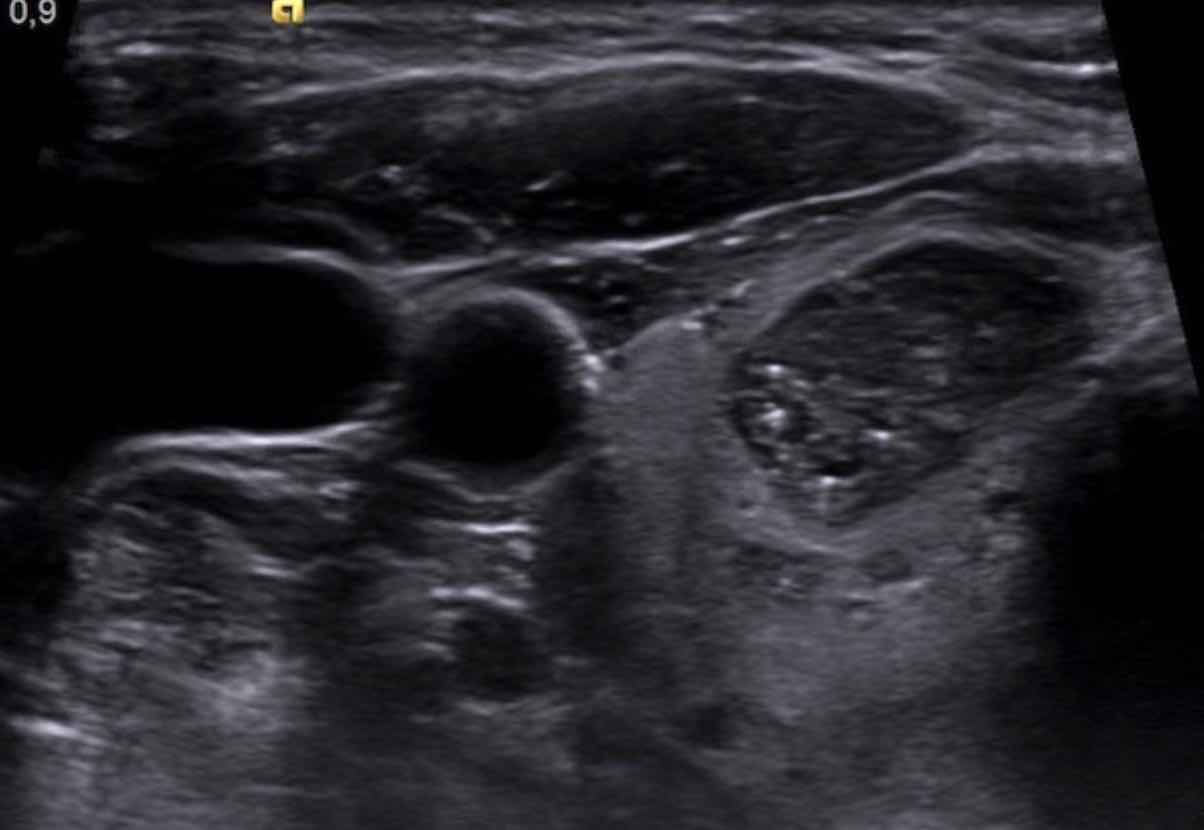
Cyst
Here a typical cyst.
No further evaluation is needed.
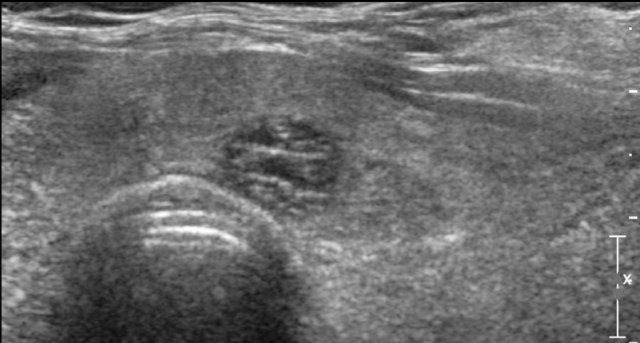
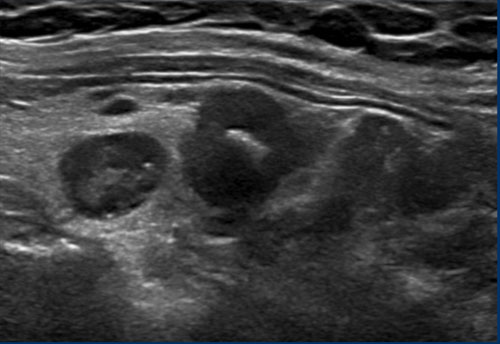
Spongiform
Spongiform nodules have a sponge-like appearance, with at least 50% cystic composition of tiny cystic parts.
No further characterization is needed.
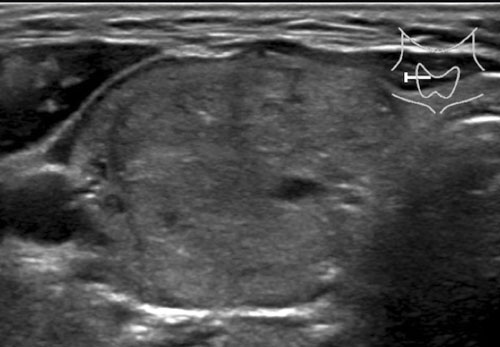
Mixed cystic/solid
In mixed cystic/solid lesions the amount of cystic and solid parts is not important.
This lesion gets 1 point for the mixed cystic/solid composition.
Solid lesions
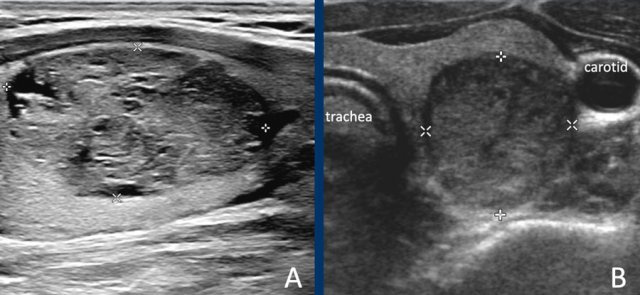
The lesion in A is almost completely solid.
While there are small cystic parts, it is not considered a spongiform nodule, because the small cystic parts are far less than 50% of the total nodule.
The lesion in B is completely solid.
In solid nodules at least 95% of the nodule should be solid.
This percentage should be an estimation, it is not needed to calculate this.
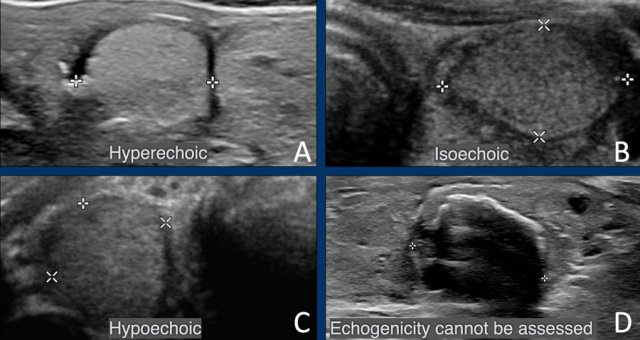
Echogenicity
An anechoic lesion should be completely black, which means that it is cystic.
No further characterization is needed.
Hyperechoic and isoechoic lesions both get 1 point, so for the score it does not matter.
The echogenicity is compared with normal thyroid parenchyma
Hypoechoic means that a lesion is more hypoechoic than normal thyroid parenchyma.
If the echogenicity cannot be assed, for example because of calcifications, 1 point is given for the echogenicity.
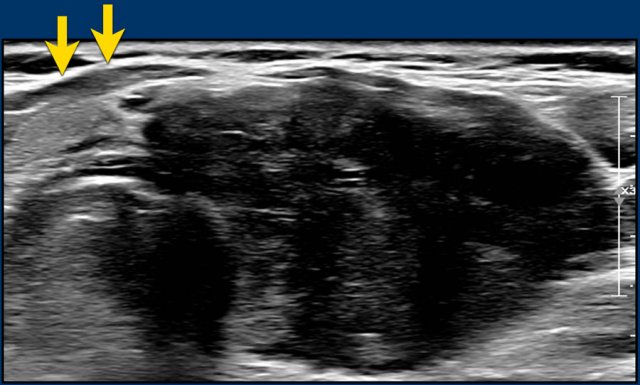
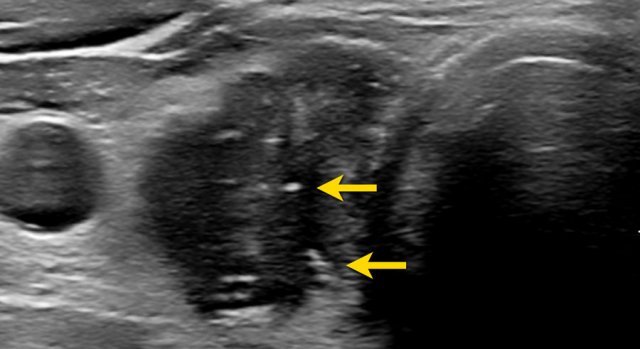
A very hypoechoic lesion is more hypoechoic than normal muscle.
Notice that the tumor is more hypoechoic in comparison to the strap muscles (arrows).
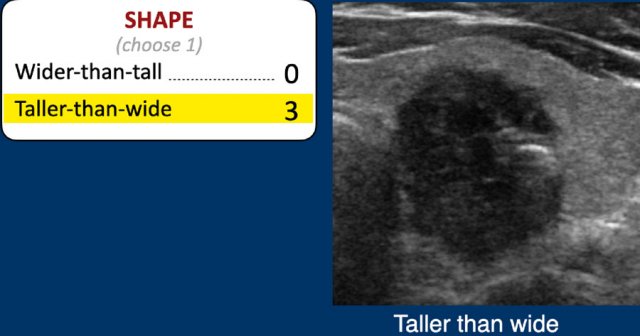
Shape
The shape should be assesed in the axial plane.
A taller-than-wide shape is a strong predictor of malignancy, and therefore gets 3 points.
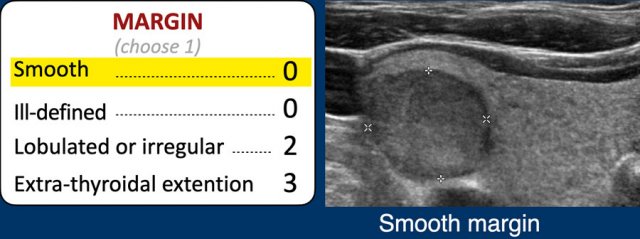
Margin
The margin is often best assessed on the anterior side.
- Smooth: the margin is completely smooth
- Ill-defined: the margins of the nodule cannot be clearly defined from the thyroid parenchyma. This is a benign feature and should be distinguished from the irregular margin.
- Lobulated or irregular: margins are lobulated, spiculated, irregular or angulated.
- Extra-thyroidal extension: difficult to analyze on ultrasound, there should be clear invasion of nearby structures. Bulging of the nodule in nearby structures is not enough.
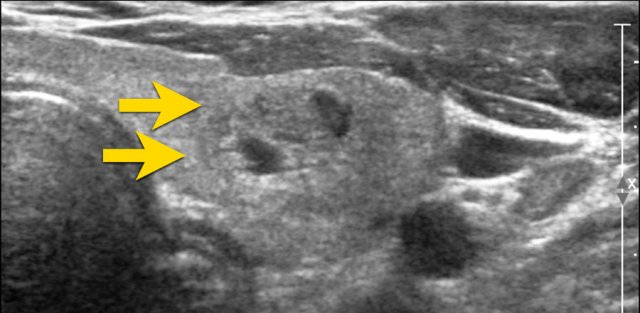
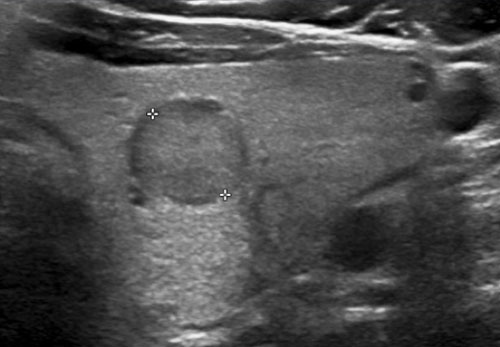
Ill-defined nodule.
Notice how only some small parts of the border of the nodule can be defined (arrow).
Most of its margin is indistinct from the thyroid parenchyma.
0 points in TI-RADS.
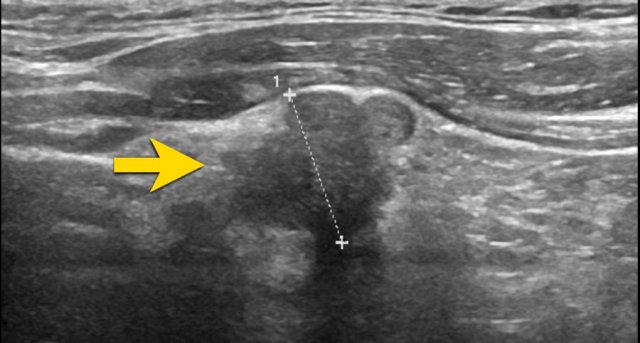
A nodule with irregular angulated margins.
2 points in TI-RADS.
The image shows an irregular lobulated margin of the anterior surface.
2 points in TI-RADS.
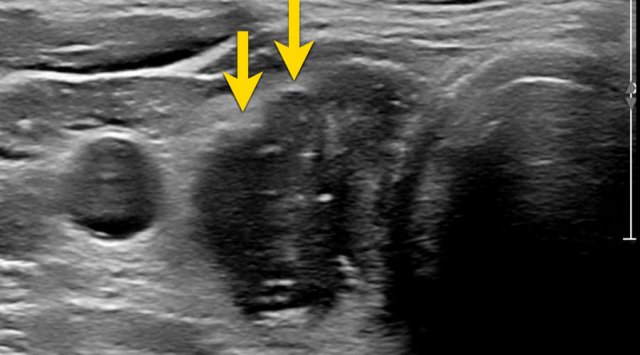
There is a nodule which has exophytic growth with compression of the nearby structures.
However, there is no frank invasion, there this does not classify as extra thyroidal extension.
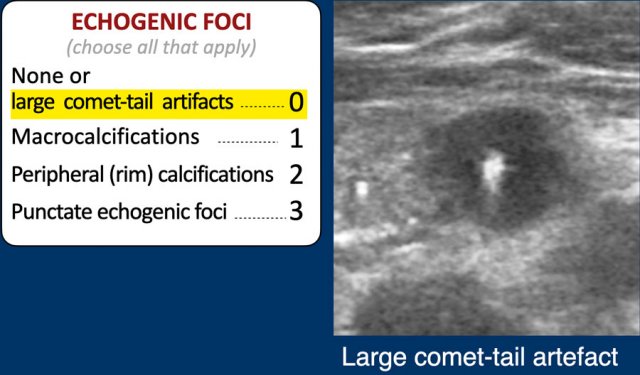
Echogenic foci
Comet tail artefact
Echogenic foci is the only category where multiple options are possible and you have to choose all that apply.
Points will be added to the total score.
This means that when both punctate echogenic foci and rim calcifications are present, the TI-RADS points are 3 + 2 = 5 points
0 points is given for:
- No echogenic foci.
- Large comet tail artefacts > 1 mm (figure).
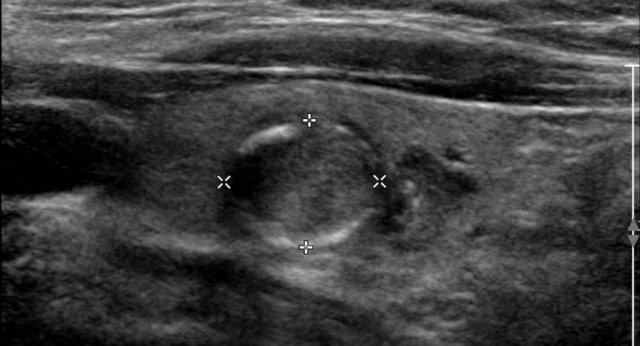
Macrocalcification
This nodule has large macrocalcifications with acoustic shadowing.
TI-RADS: 1 point.
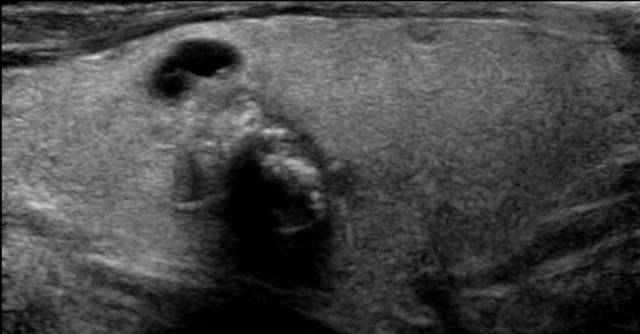
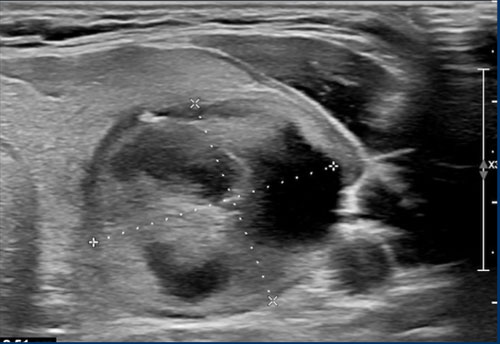
Rim calcification
Peripheral rim calcifications can be complete or incomplete.
TI-RADS: 2 points.
Microcalcifications
Punctate echogenic foci are also knows as microcalcifications. They are a strong predictor of malignancy and therefore get 3 points.
The ACR lexicon further defined this category, because in the normal thyroid there also may be echogenic foci visible.
Punctate echogenic should be called in the situation where they are obvious and only visible within the nodule.
Small comet tail artifacts with a length less than 1mm are also included in this category.
TI-RADS: 3 points.
Growth
Growth of a nodule according to TI-RADS is also defined, and is in accordance with the ATA guidelines.
There should be either:
- ≥20% increase in at least two nodule dimensions, with a minimal increase of 2 mm or
- ≥50% or greater increase in volume
If there is no change in size for 5 years, the nodule can be considered as having a benign behavior, and further follow up is not needed. Comparison should be made with the oldest study available, and not (only) the last one.
If there is interval growth without fulfillment of FNA criteria, the next follow-up should be after 1 year, regardless of the TI-RADS category.
Multiple Nodules
When there are multiple nodules, there should be no more than 4 nodules classified. FNA is not recommended of more than 2 nodules.
In the case of multiple nodules, the nodule fulfilling the TI-RADS FNA criteria should be sampled, which is not necessarily the dominant or largest nodule.
Overdiagnosis and Overtreatment
Once a thyroid nodule is detected, the binary question remains, is it benign or malignant?
Depending on the published series referenced, 6%–13% of thyroid nodules chosen for FNA will yield malignancy (1).
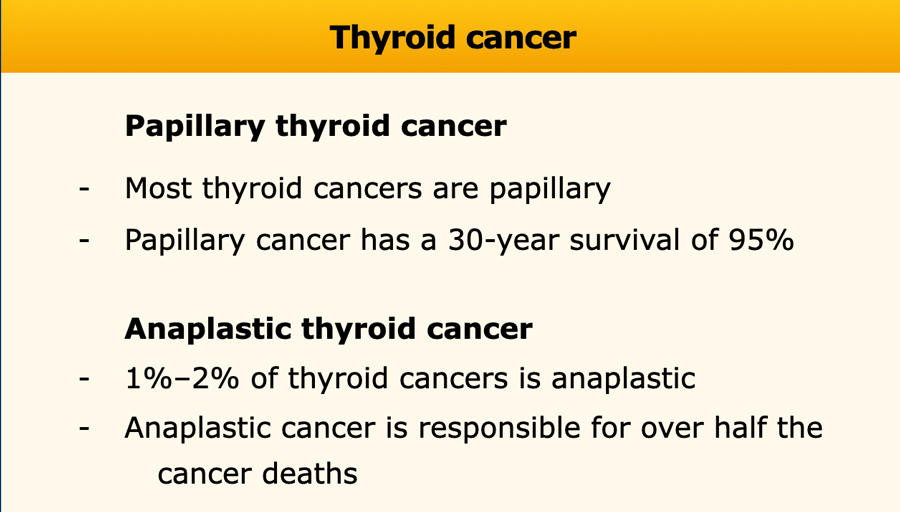
The majority of thyroid cancers detected incidentally are papillary in origin.
Unlike its malevolent associate anaplastic thyroid cancer, which while accounting for only 1%–2% of thyroid cancers is responsible for over half the cancer deaths, papillary thyroid cancer is very benign.
Since papillary is the dominant thyroid cancer and is well differentiated, the prognosis is remarkably good, with a reported 30-year survival of 95% (1).
As most of these cancers would never have caused symptoms during life, the increased diagnostic scrutiny is causing overdiagnosis.
Our research focus should be the discovery of the small percentage of thyroid cancers that are aggressive and alter life spans.
Examples
Composition
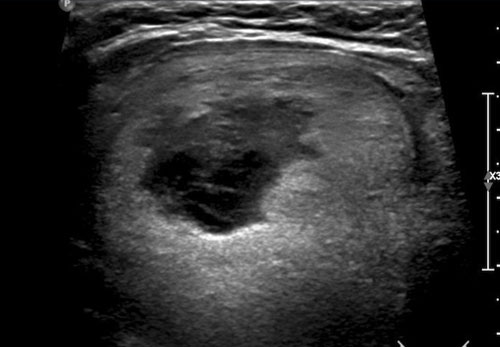
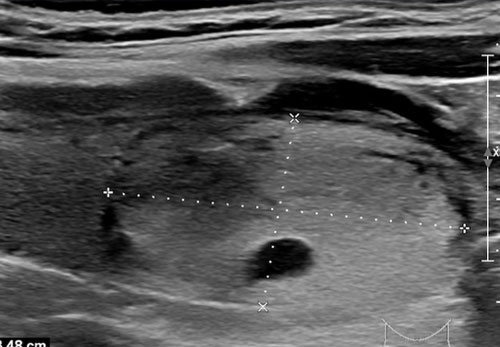
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
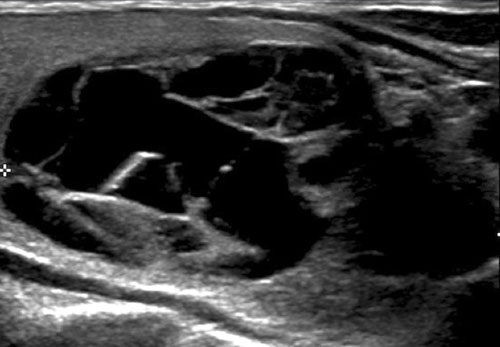
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
There is a mixed composition with a cystic component in the center.
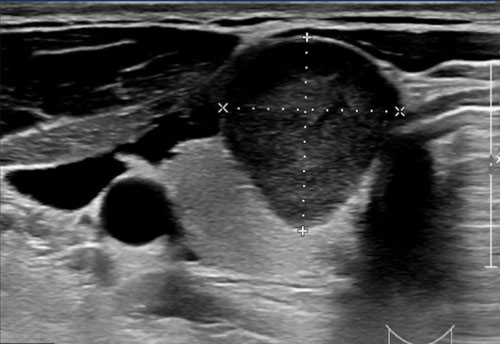
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
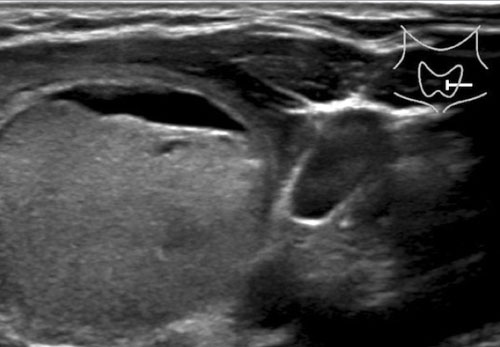
This is mostly a solid lesion.
The cystic part is s o small, that 2 points are given for composition.
Echogenicity
First study the image.
Then continue reading.
There is posterior acustic enhancement.
This means that this could be a cystic lesion.
In such cases color-doppler can be helpful, but unfortunately was not performed.
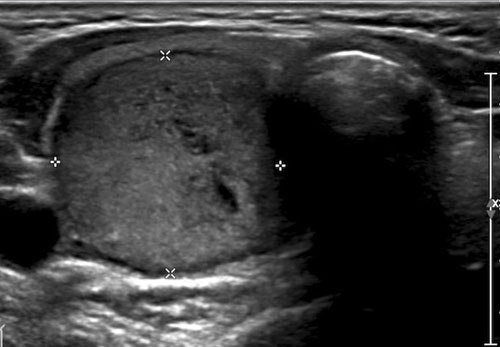
Study the image and score for TI-RADS.
Then scroll the image for the TI-RADS score.
This nodule is hypoechoic compared to the normal thyroid tissue which is seen on the ventral side of the nodule.
2 points for hypoechoic echogenicity.
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
This is a hyperechoic nodule.
This means 1 point for echogenicity.
Shape
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
3 points for the shape, which is taller than wide.
Margin
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
Then continue reading.
Although the margin is ill-defined on the cranial side, this still means 0 points for the margin.
Echogenic foci
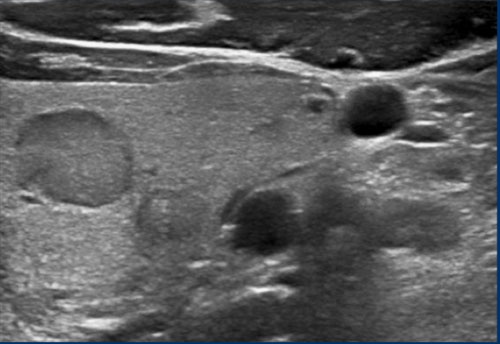
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
Then continue reading.
Only 1 point for the macro calcification.
This is a TI-RADS 5 lesion mainly due to the very hypoechoic echogenicity.
Maybe the lesion is also taller than wide, which would mean 3 extra points.
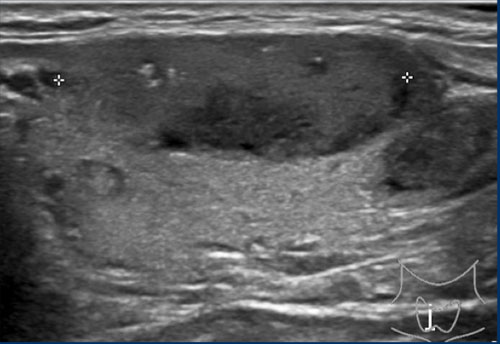
Study the image and score for TI-RADS.
Scroll the image for the TI-RADS score.
Notice the very subtle echogenic foci.
A total of 6 points results in a TI-RADS score 4..