Thoracic Ultrasound in Acute Abdomen
Adriaan van Breda Vriesman¹, Julien Puylaert² and Robin Smithuis¹
¹Alrijne hospital in Leiden and ²the Amsterdam University hospital in the Netherlands
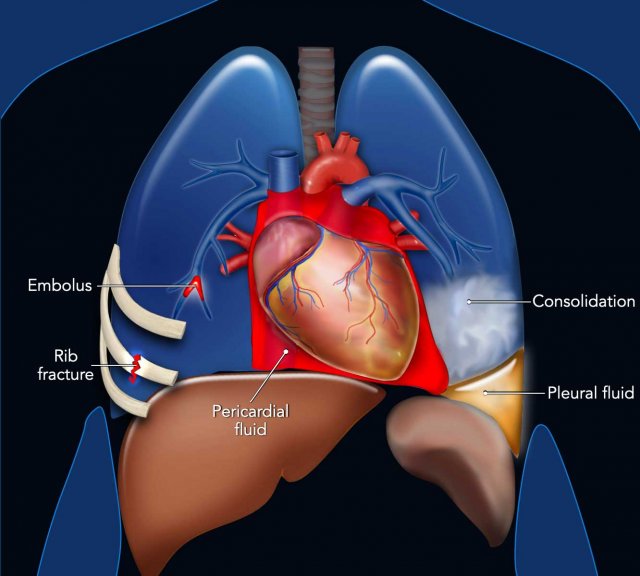
The etiology of abdominal symptoms may occasionally be linked to thoracic pathology.
A sole focus on abdominal findings can lead to misdiagnosis and incorrect management.
In instances of unexplained acute abdominal pain, radiologists should broaden their diagnostic approach to include potential thoracic conditions.
Introduction
Abdominal pain usually arises from structures within the abdomen. Occasionally, however, abdominal complaints may be the most prominent or single presenting feature of thoracic disease, mainly occurring in the paediatric and geriatric populations
The most common diagnoses that may present with abdominal symptoms are:
- Pneumonia, especially in the pediatric population.
- Pulmonary embolism.
- Pericarditis and cardiac tamponade.
- Rib fractures
Pneumonia
The clinical manifestations of pneumonia can present atypically, with abdominal pain as the primary symptom, potentially mimicking acute conditions such as cholecystitis, appendicitis, or diverticulitis.
This presentation may arise from referred pain due to pleural or diaphragmatic irritation caused by infection, typically affecting the basal lung regions.
In classic pneumonia, the bronchi in the consolidated lung remain aerated, producing an air bronchogram, which appears on ultrasound as bright branching reflections and reverberations.
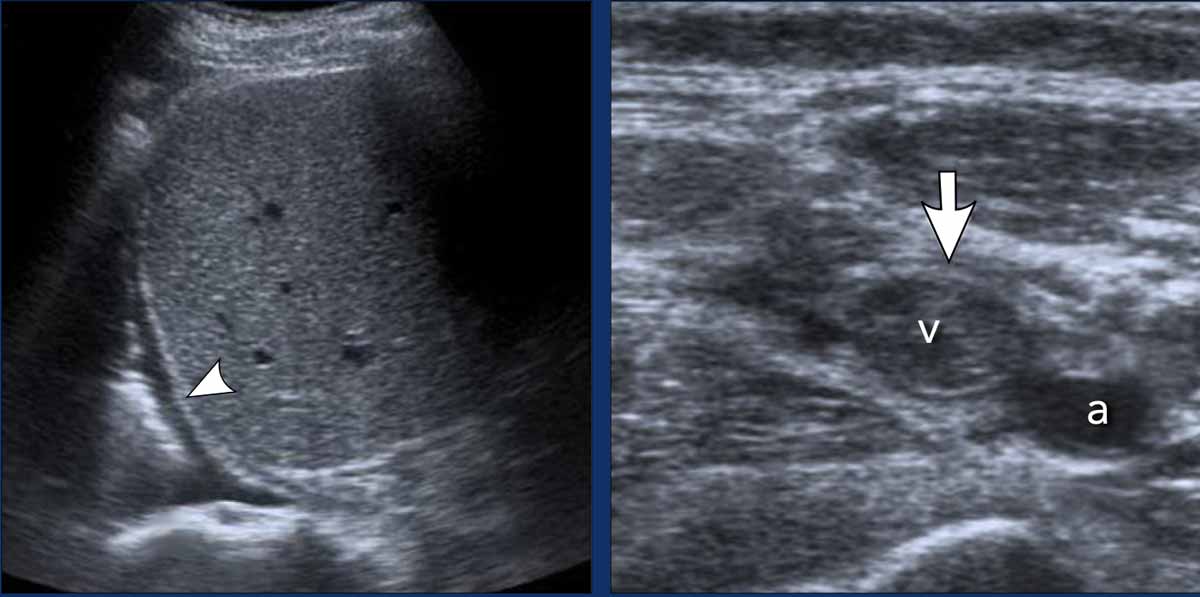
Image:
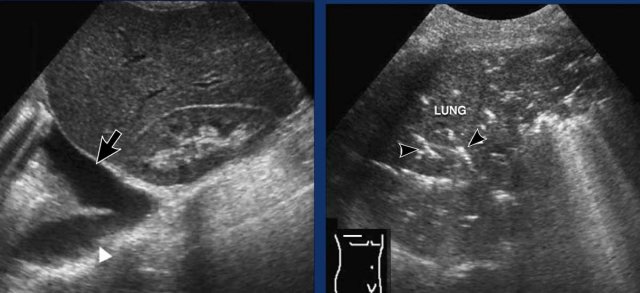
An 8-year-old boy with pneumonia presenting clinically as appendicitis.
A transhepatic ultrasound reveals consolidation in the right lower lung (arrow) with associated air bronchograms (arrowheads).
The appendix was normal (not shown).
Continue with the chest X-ray...
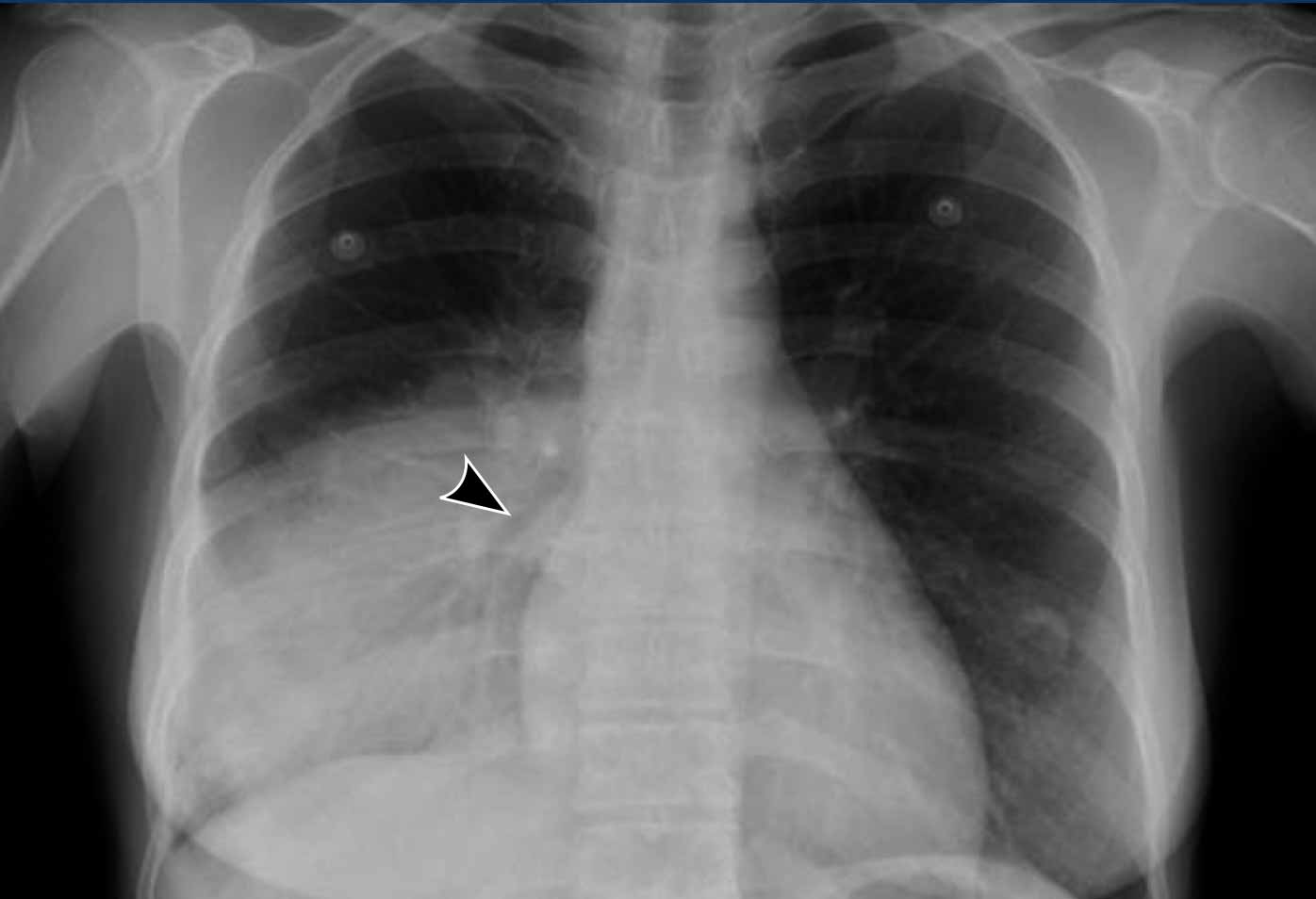
Images
PA and lateral chest X-rays reveal consolidation dorsobasally in the right lower lobe, consistent with pneumonia, clearly visible on the lateral view (black arrow), but difficult to detect on the PA view (white arrow).
These images are of a 47-year-old woman with pneumonia, clinically simulating as a cholecystitis.
Images
Transhepatic ultrasound detects a right-sided pleural effusion (arrow).
The gallbladder appeared normal (not shown).
Intercostal ultrasound shows pulmonary consolidation with air bronchograms (arrowheads).
Continue with the chest X-ray...
The chest radiograph confirms right lower lobe pneumonia with an air bronchogram (arrowhead).
Note that the right border of the heart remains visible because the middle lobe is normal.
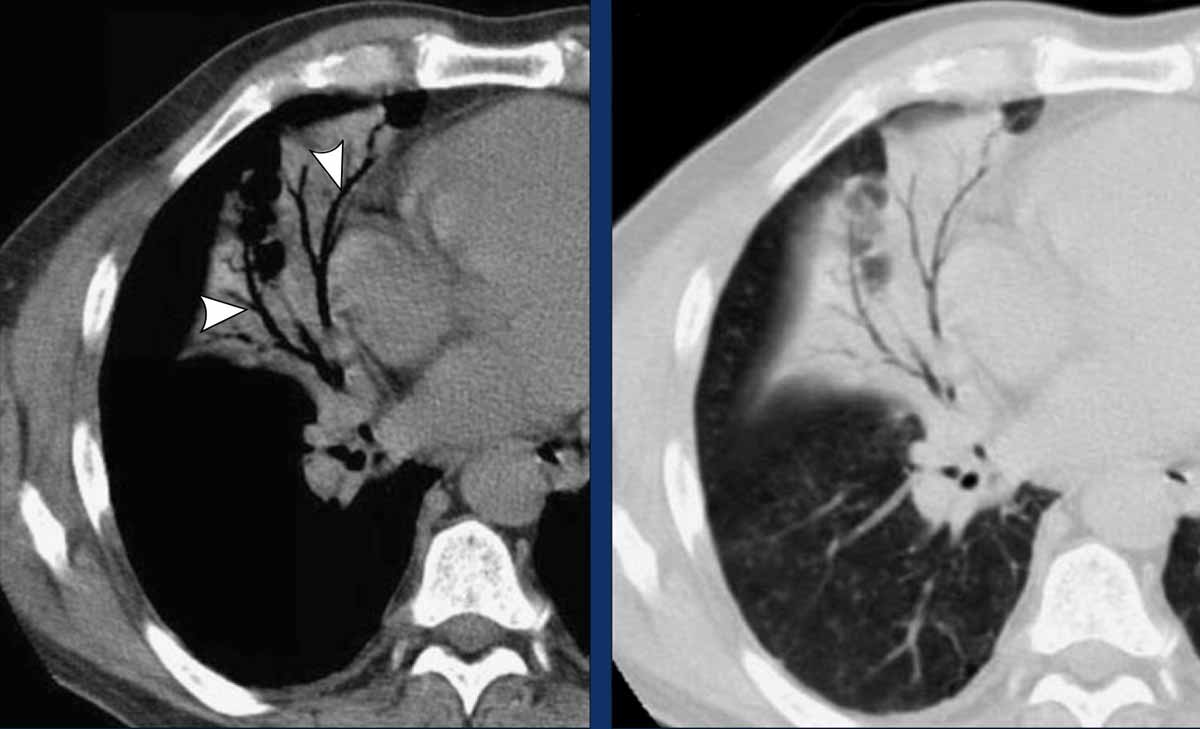
Air bronchograms are also a characteristic feature of pneumonia on CT.
These images are of a 72-year-old man with pneumonia, presenting with non-specific acute abdominal pain.
Images
Non-enhanced abdominal CT, also depicting the basal parts of the lung, shows middle lobe consolidation with characteristic air bronchograms (arrowheads).No abdominal abnormalities were found
Pulmonary embolism
Ultrasound or abdominal CT, both can detect indirect signs of embolism such as unilateral pleural effusion, which is present in half of all patients. During ultrasound the patient’s history can be obtained, and if suggestive of pulmonary embolism the examination can be quickly supplemented with compression ultrasound of the deep veins of the lower limbs, as pulmonary embolism and deep venous thrombosis represent the spectrum of one disease.
These images are of a 53-year-old woman with acute pulmonary embolism, presenting with clinical signs of cholecystitis.
Images
Transhepatic ultrasound depicts unilateral pleural fluid (arrowhead). The gallbladder was normal (not shown). During ultrasound the patient revealed that the complaints had started shortly after an intercontinental flight.
Compression ultrasound detects thrombosis in the left femoral vein (arrow).
A CT was performed and revealed emboli in the right lower lobe artery and a small pleural effusion.
Ultrasound and abdominal CT can both identify indirect signs of pulmonary embolism, such as unilateral pleural effusion, which occurs in approximately 50% of cases. During ultrasound examination, a targeted patient history can be obtained, and if pulmonary embolism is suspected, the assessment can be promptly extended to include compression ultrasound of the deep veins of the lower extremities. This is clinically relevant, as pulmonary embolism and deep vein thrombosis represent different manifestations of the same thromboembolic disease spectrum.
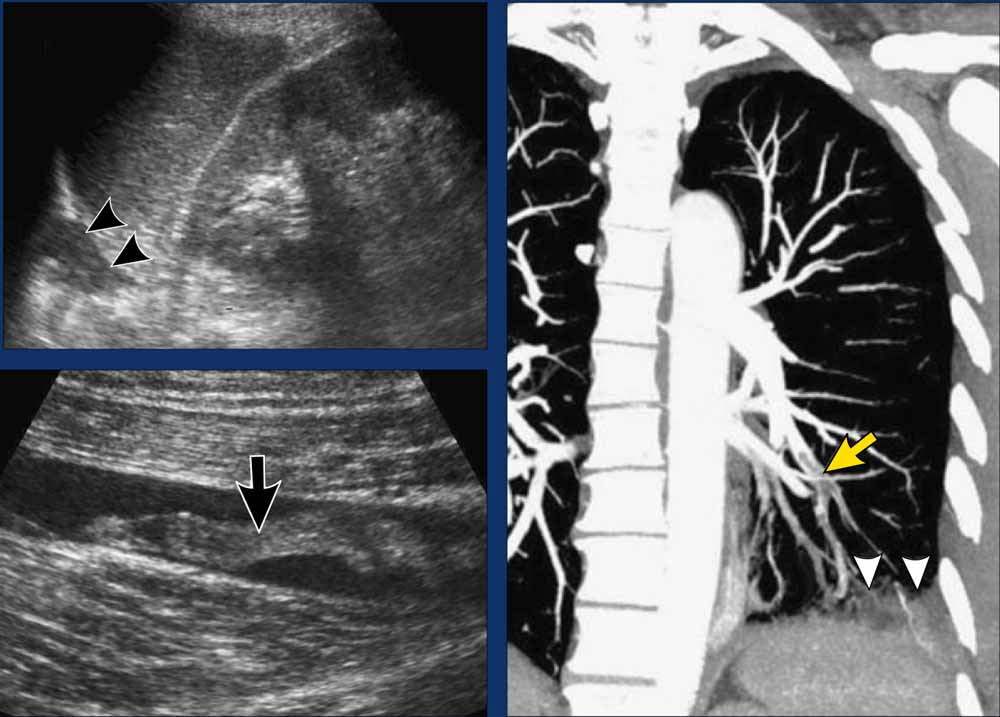
Case Presentation
The following images pertain to an 81-year-old male with acute pulmonary embolism, initially presenting with clinical features mimicking sigmoid diverticulitis.
Imaging Findings
- Ultrasound, utilizing the spleen as an acoustic window, demonstrates subtle pulmonary consolidation or pleural fluid (arrowheads), with no detectable abdominal abnormalities.
- Ultrasound reveals thrombosis (arrow) in the left popliteal vein.
- Coronal maximum intensity projection (MIP) CT image depicts emboli within the left lower lobe pulmonary artery (yellow arrow) and pulmonary infarction (arrowheads), corresponding to the consolidation observed on ultrasound.
Abdominal CT may show, if the imaging delay allows sufficient venous contrast enhancement, thrombus in iliac veins or in the inferior vena cava (fig).
Pericarditis and Cardiac Tamponade
In patients with pericarditis or hemopericardium, fluid accumulation within the pericardial space can lead to cardiac compression, resulting in hemodynamic compromise. This may progress to cardiac tamponade, characterized by systemic venous congestion and a life-threatening reduction in cardiac output.
Cardiac tamponade can be a challenging clinical diagnosis, as its classic manifestations—such as hypotension, tachycardia, and dyspnea—are nonspecific, and the clinical presentation may be atypical. Some patients may primarily present with acute abdominal pain and vomiting, likely due to venous congestion from right-sided heart failure or mesenteric ischemia caused by hypoperfusion.
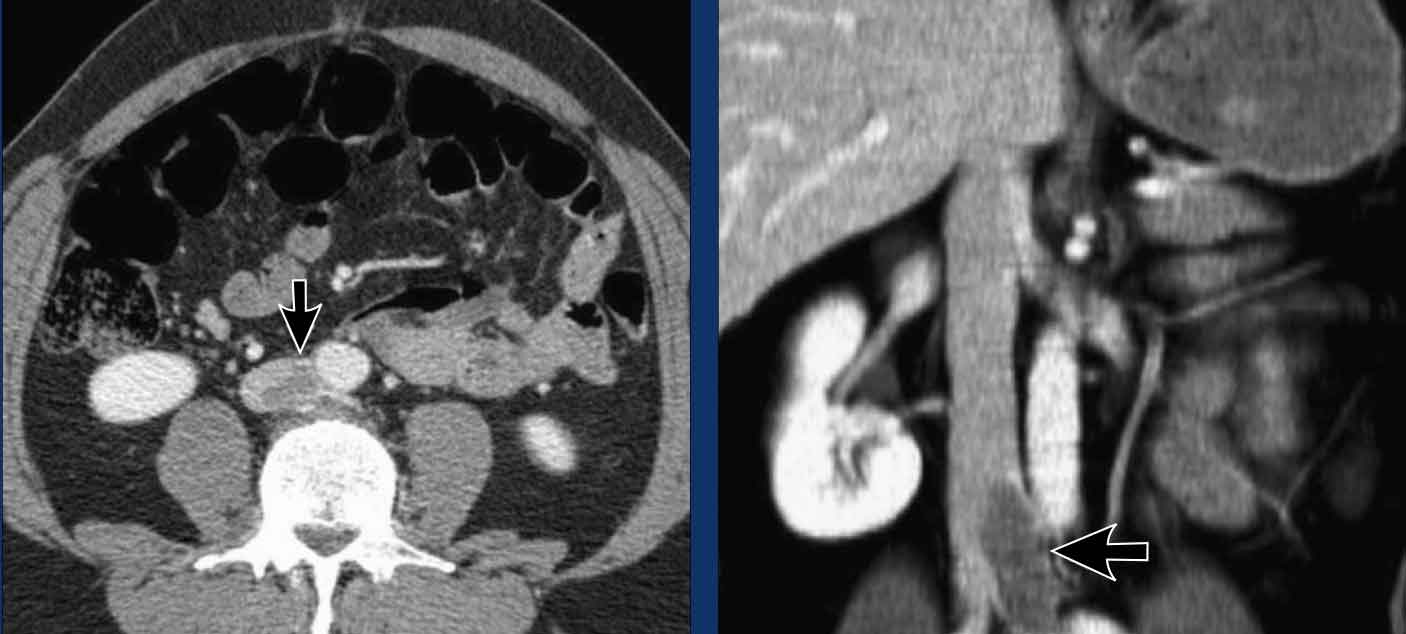
A 52-year-old man presented with infectious acute pericarditis and acute epigastric pain.
Imaging Findings
- Parasternal ultrasound demonstrated a pericardial effusion with pericardial thickening (arrowheads). No abdominal abnormalities were detected.
- Contrast-enhanced CT confirmed the presence of a pericardial effusion surrounded by an enhancing, thickened pericardium (arrow).
Pericardial drainage yielded an inflammatory exudate, likely of viral origin. Following treatment of the pericarditis, the patient’s abdominal symptoms gradually resolved.
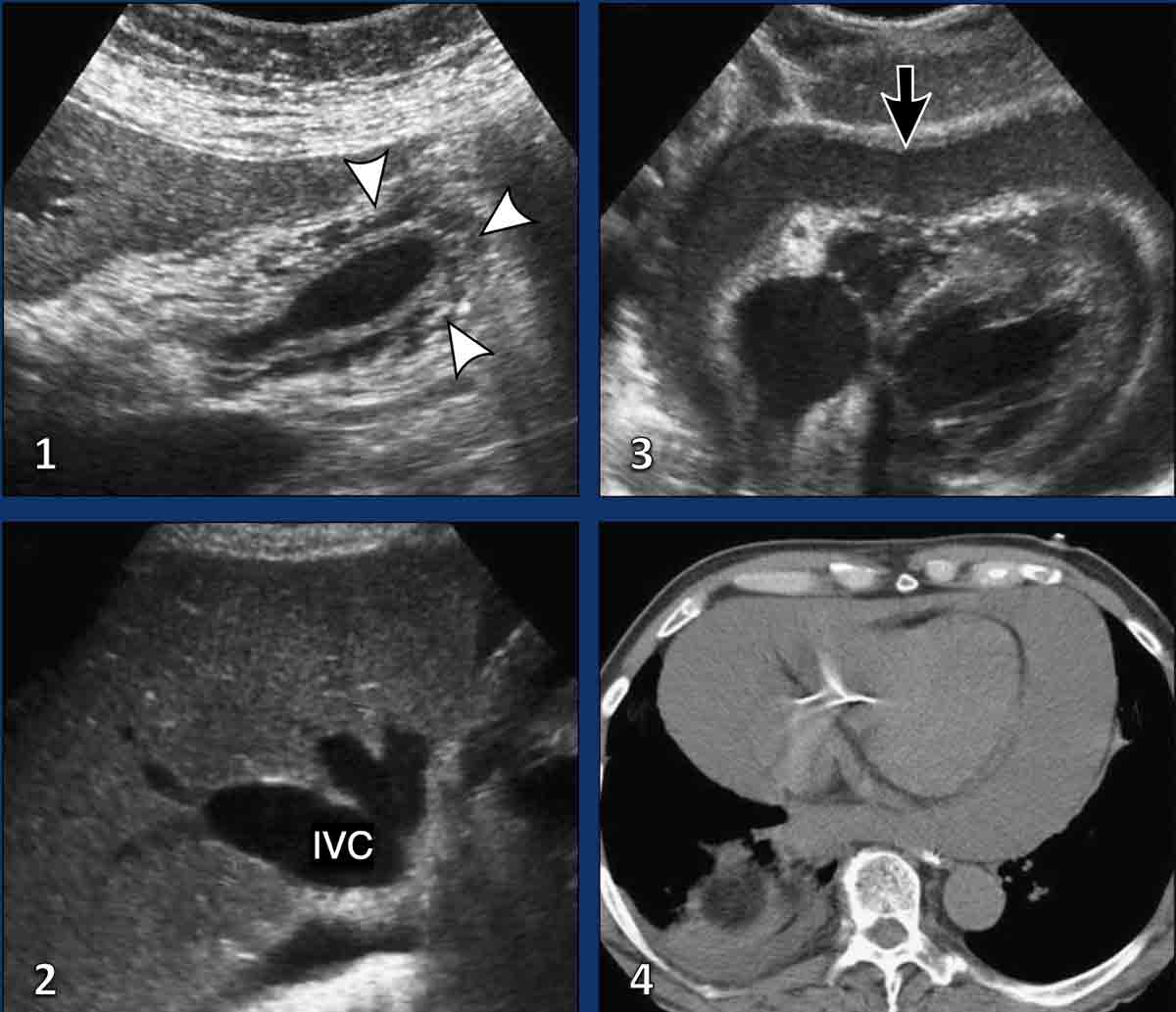
Case Presentation
A 49-year-old man with cardiac tamponade, presenting primarily with upper abdominal pain.
Imaging Findings
- Longitudinal ultrasound of the gallbladder reveals diffuse wall thickening (arrowheads). Although this finding could suggest cholecystitis, the absence of gallstones and gallbladder distension suggests an extrinsic cause.
- Transverse ultrasound of the liver demonstrates a dilated inferior vena cava (IVC) and enlarged hepatic veins (arrowheads), indicative of right heart failure.
- Parasternal ultrasound identifies a large pericardial effusion (arrow), consistent with idiopathic acute pericarditis as the underlying cause.
- CT imaging of another patient with cardiac tamponade, presenting with acute abdominal pain and vomiting.
Non-contrast CT demonstrates a large pericardial effusion with attenuation values greater than that of water (+35 HU), suggestive of hemopericardium. This diagnosis was confirmed by pericardiocentesis.
A recent insertion of a pacemaker was the underlying cause.
Following pericardial drainage, the patient’s abdominal symptoms resolved.
Rib Fractures
The clinical presentation of a rib fracture is typically straightforward, characterized by localized tenderness and sharp chest pain following a fall or direct thoracic trauma.
However, we have encountered several patients with unsuspected lower rib fractures who presented with acute abdominal pain in the absence of thoracic symptoms.
Most of these patients had no history of trauma, suggesting that the rib fractures were insufficiency fractures, often secondary to severe coughing. In oncologic patients, such fractures may be pathological in nature.
Ultrasound has proven highly effective in detecting rib fractures, with a sensitivity exceeding that of radiography.
By scanning the area of tenderness with the transducer aligned parallel to the long axis of the rib, a fracture can be identified as a disruption of the echogenic anterior cortex, often accompanied by a hematoma.
While ultrasound is a valuable diagnostic tool, CT provides the highest accuracy for detecting rib fractures, particularly when viewed using the appropriate bone window settings.
Case Presentation
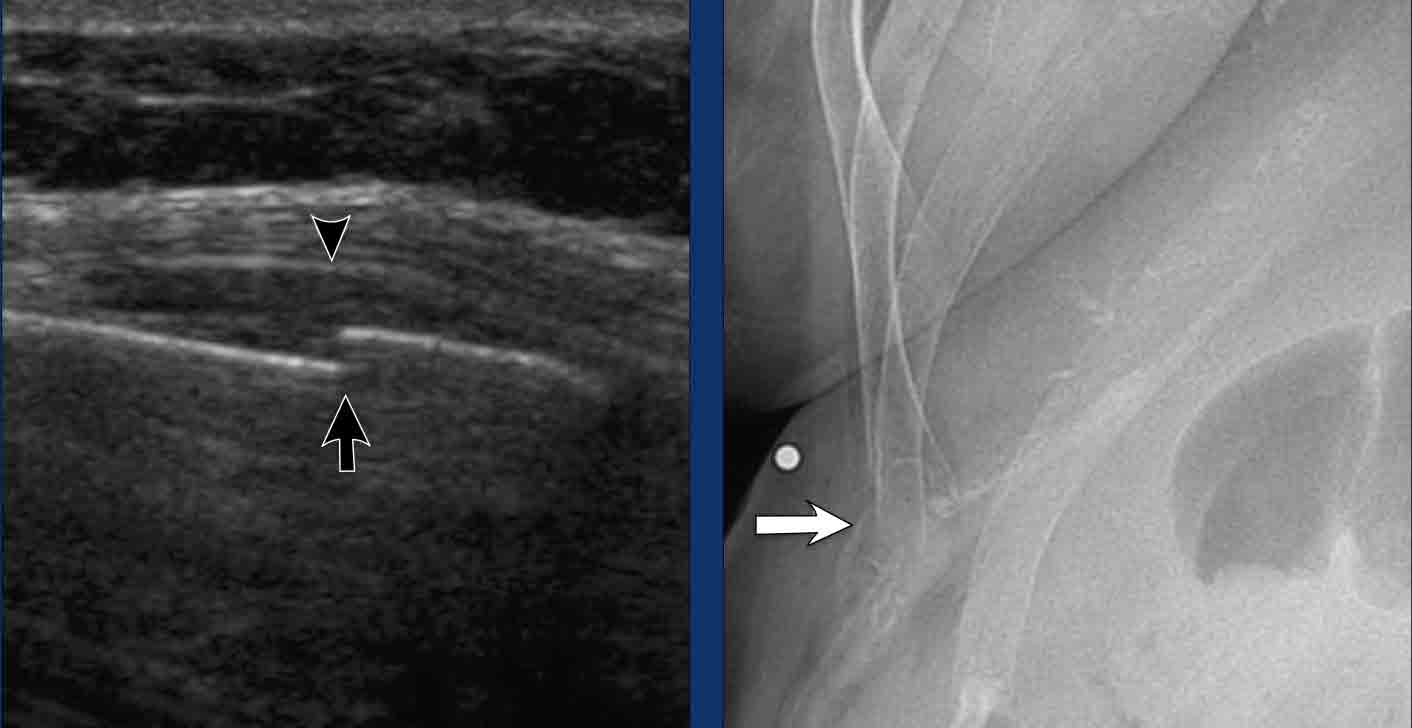
An 84-year-old woman with a rib fracture, complaining of acute right upper abdominal pain. She denied any history of trauma.
Imaging Findings
- Transverse ultrasound exactly at the spot of maximum pain depicts a moderately displaced rib fracture (arrow) with a small haematoma (arrowhead). No other abnormalities were found.
- Radiography confirms acute fracture of the distal anterior 11th rib (arrow)