Bladder Cancer - VI-RADS
Ailin Dehghanpour¹, Martina Pecoraro¹, Valeria Panebianco¹, Thierry Boellaard², Robin Smithuis³ and Ivo Schoots⁴
¹Radiology Departement of Sapienza University, Rome, Italy and ²NKI, ³Alrijne Hospital and ⁴Erasmus MC in the Netherlands
Multiparametric MRI of the bladder is a highly accurate diagnostic and non-invasive tool for detecting and locally staging bladder cancer.
We will discuss the Vesical Imaging Reporting and Data System (VI-RADS) which was introduced in 2018 [1].
The goal of the VI-RADS is to standardize the acquisition, interpretation and reporting of bladder MRI.
The critical challenge in locally staging bladder tumors is the differentiation between muscle-invasive and non-muscle-invasive cancers.
Introduction
The main goal of locally staging bladder tumors is to differentiate between muscle-invasive (T2 or greater) and non-muscle-invasive (T1 or lower) cancers, as this delineation leads to significant changes in patient management.
Non muscle-invasive lesions require local treatment (TURBT) while muscle-invasive lesions require neoadjuvant therapy usually followed by radical cystectomy and eventually adjuvant therapy.
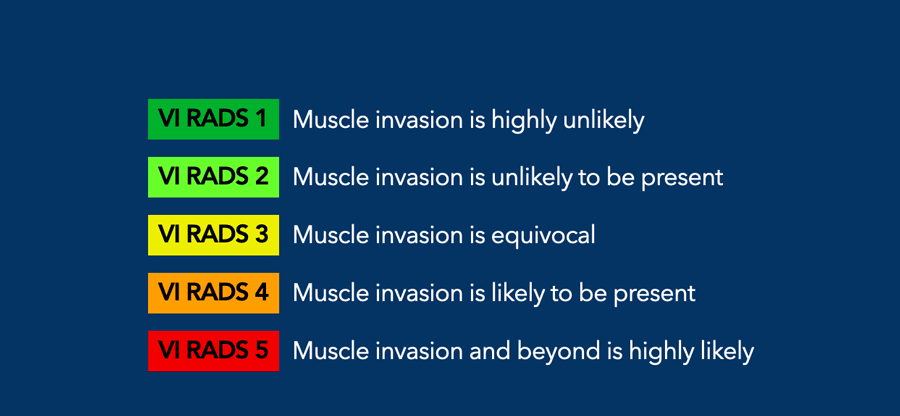
VI-RADS addresses this challenge by establishing the risk of muscle invasion using a 5-point scale derived from three categories:
- T2W - Structural category
- DWI - Diffusion category
- DCE - Contrast-enhanced category
Anatomy
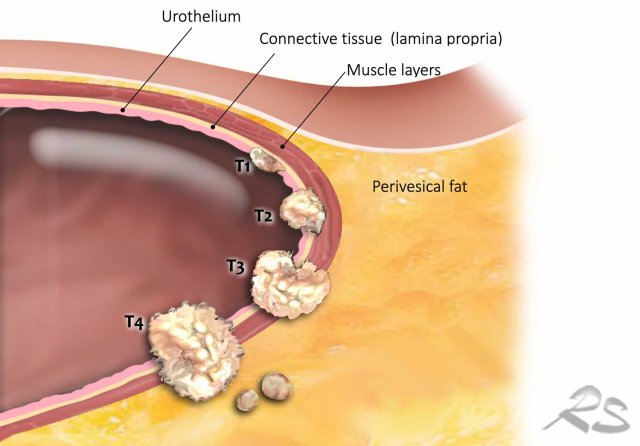
The bladder wall consists of three layers:
- Inner layer or mucosa, including the superficial urothelium and the underlying connective tissue called lamina propria.
- Muscualr layer or muscularis propria, which is the detrusor muscle.
- Perivesical fat.
TNM system - T staging
- T1: no invasion of muscle layer.
- T2a: superficial muscle invasion (inner half).
- T2b: deep muscle invasion (outer half).
- T3a: tumor invades microscopically the perivesical adipose tissue.
- T3b: tumor invades macroscopically the perivesical adipose tissue
- T4a : tumor invades adjacent organs.
- T4b: tumor invades distant tissues outside the pelvis.
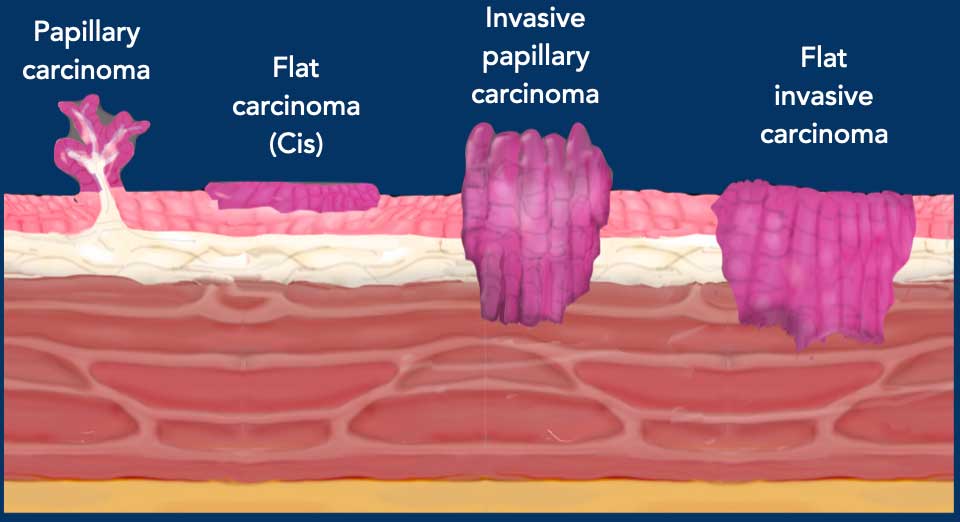
There are three types of bladder tumors:
- Papillary tumors with endoluminal growth, with or without a tumor stalk. The stalk is characterized by hypointensity in T2W and DWI sequences, while it appears hyperintense on DCE sequences.
- Flat superficial tumors or carcinoma in situ, which are contained in the mucosa and do not extend through the other layers.
- Flat invasive carcinomas or sessile tumors with intramural growth.
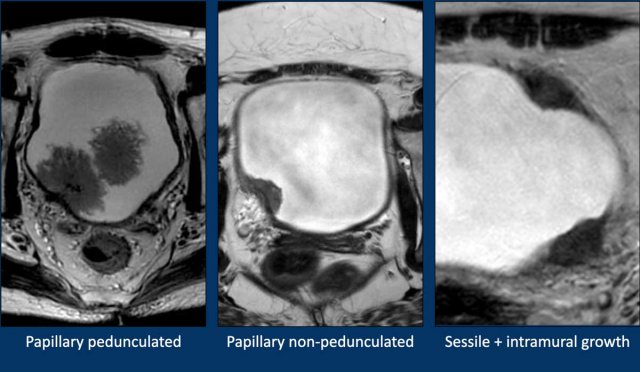
Here three MR-examples:
- Papillary pedunculated tumor.
- Papillary non-pedunculated tumor.
- Flat invasive carcinomas or sessile tumors with intramural growth.
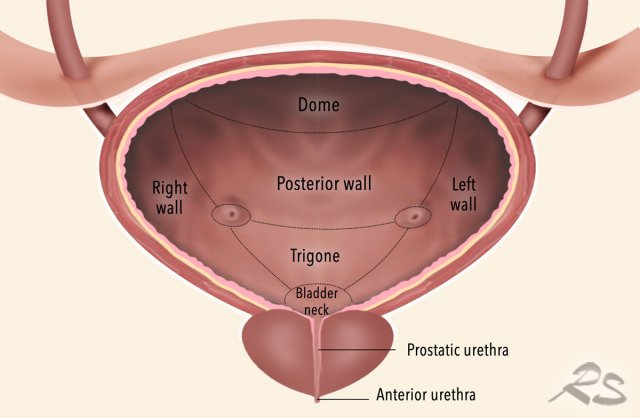
The bladder is anatomically divided into four parts: the apex or dome, body, fundus, and neck.
For the localization of a bladder tumor, the VI-RADS document recommends the use of a map that divides the bladder into 12 parts:
- Anterior urethra
- Prostatic urethra
- Bladder neck
- Trigone
- Posterior wall
- Right wall
- Left wall
- Dome
- Anterior wall
- Right ureteral orefice
- Left ureteral orefice
- Verumontanum
Overview
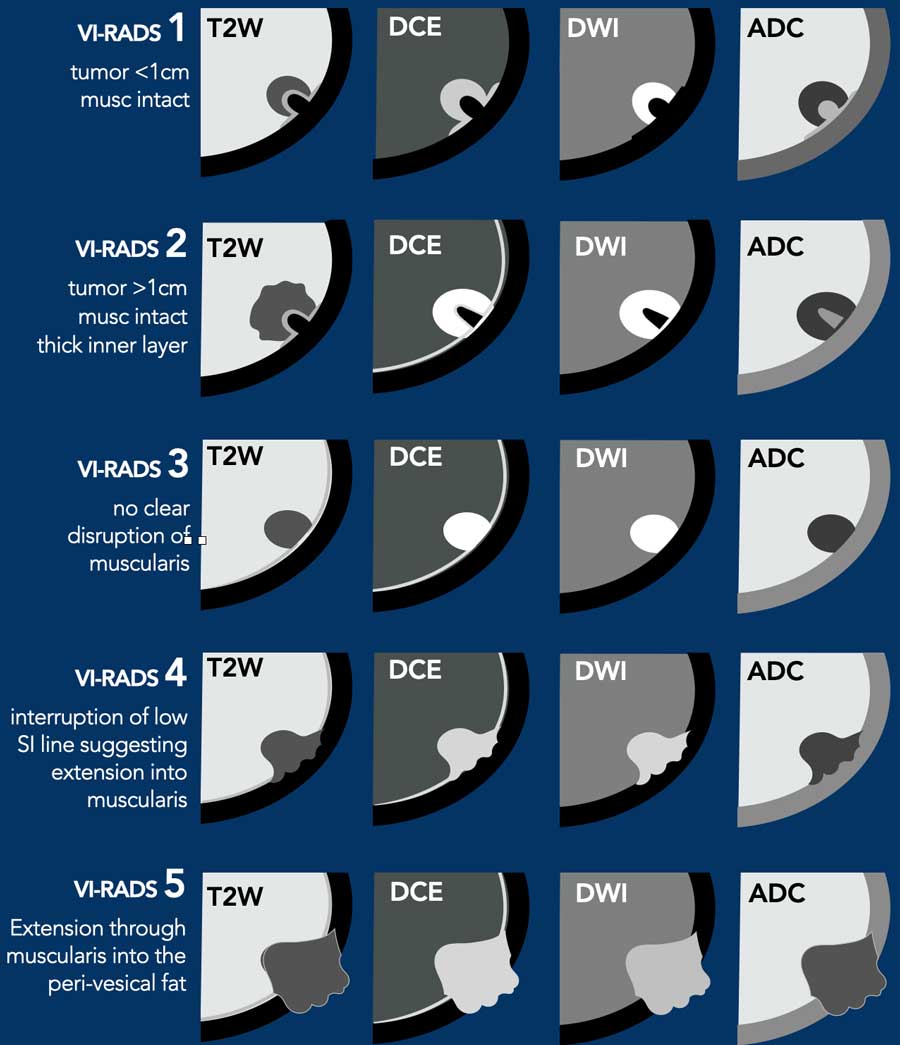
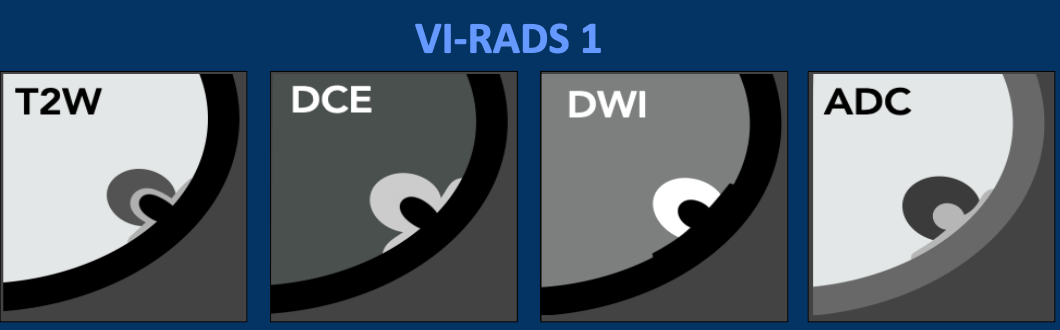
VI-RADS 1
- T2W - continuous low signal line of muscularis propria. Lesion < 1 cm. With or without tumor stalk and/or a thickened inner layer.
- DCE – low signal intensity of line of muscolaris propria early enhancement of inner layer.
- DWI - continuous intermediate signal line of muscolaris propria.
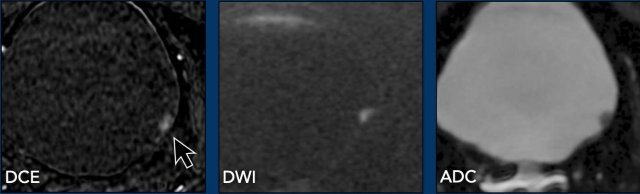
VI-RADS 2
- T2W - like VI-RADS 1 but lesion > 1 cm. papillary tumors with a stalk and/or a high signal intensity thickened layer, and sessile tumors with a thickened inner layer.
- DCE - early enhancement of inner layer
- DWI - continuous intermediate signal line of muscularis propriae. Papillary tumors will have low SI stalk.
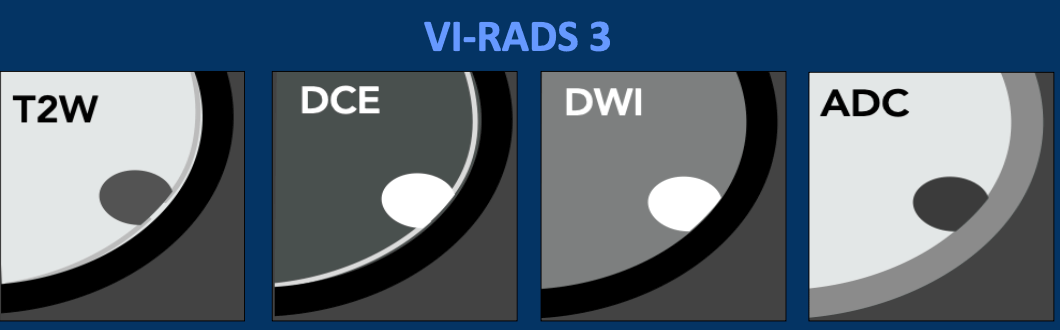
VI-RADS 3
- T2W - Absence of a stalk in a papillary tumor or absence of a high signal intensity thickened inner layer in a sessile tumor, while still maintaining the continuous low signal intensity of the muscularis propria.
- DCE – lack of VI-RADS 2 findings continuous, low signal intensity of the muscularis propria.
- DWI - continuous low signal line of muscularis propriae.
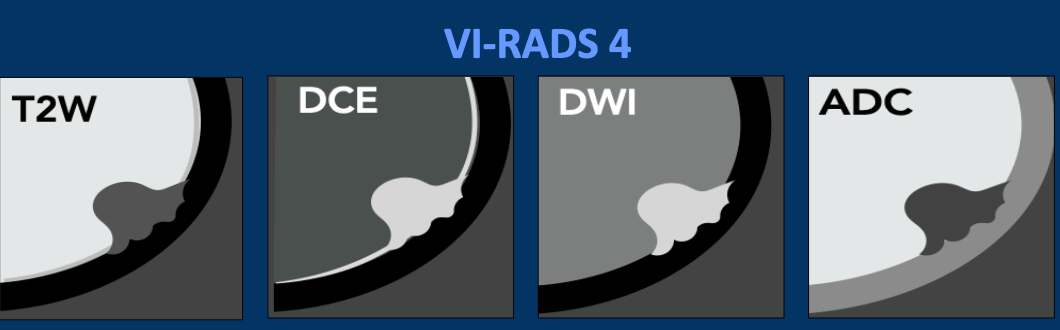
VI-RADS 4
- T2W - interruption of low signal intensity line of muscularis propria, representing muscle invasion.
- DCE - focal extension of early enhancement into the muscularis propria.
- DWI - tumor with high signal intensity on DWI and low signal intensity on ADC, extending focally into the muscularis propria.
VI-RADS 5
- T2W - tumor extends into peri-vesical fat.
- DCE - early enhancement into the extravesical adipose tissue.
- DWI - tumor high on DWI and low SI on ADC, extending throughout the entire bladder wall and into the extravesical fat.
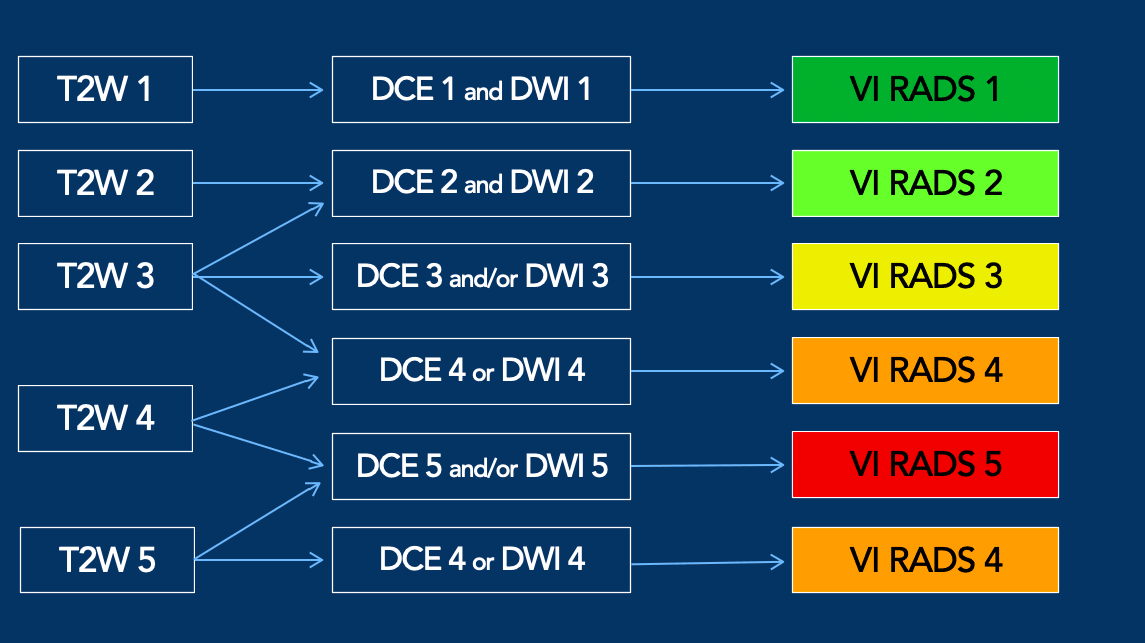
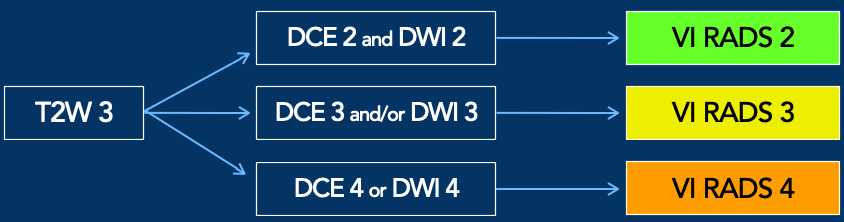
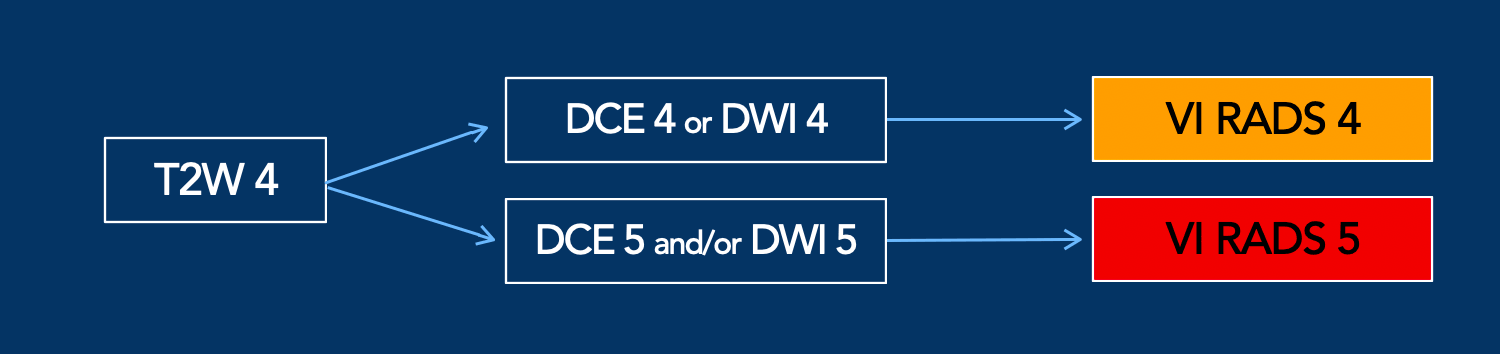
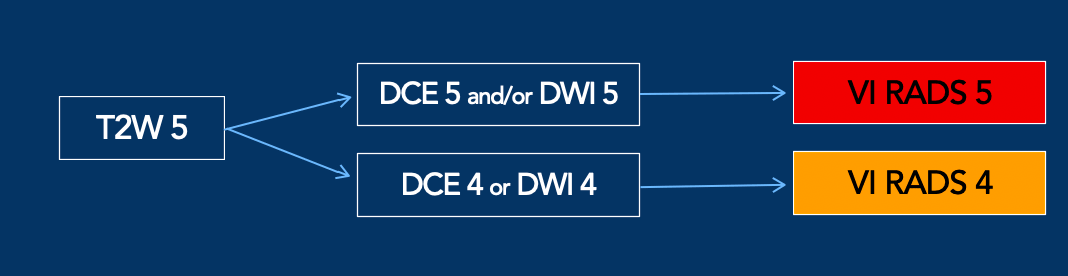
T2W sis the first sequence to be considered in the assignment of VI-RADS score (1).
However, the presence of definitive muscular invasion (VI-RADS 4 and 5) is determined by DWI and DCE.
This means. that if there is any discordance between T2W and DWI, then DWI should be the dominant sequence to maximize accuracy.
If DWI is suboptimal, DCE should be used as the dominant sequence (1).
For instance if the T2W-score is 4 and the DWI- or DCE-score is 5, then the assignement is VI-RADS 5 (see table).
On the other hand if the T2W-score is 5, while the DWI-score is 4, then the assignement is VI-RADS 4.
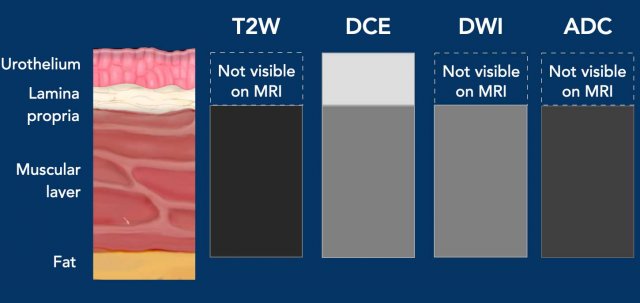
MR anatomy
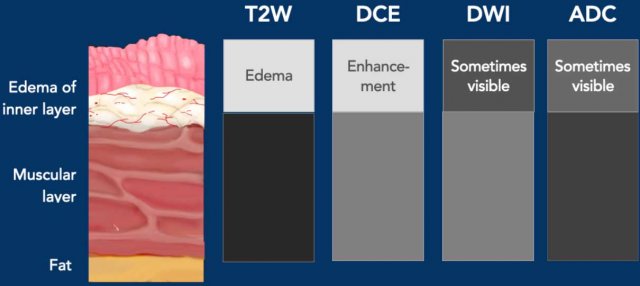
On T2W-images the muscular layer is
identified as a continuous low signal intensity line.
The inner layer, composed of urothelium
and lamina propria, is not usually visible on T2W
except in case of edema.
Bladder cancer demonstrates intermediate signal intensity
compared to urine and muscle signal
intensity (2).
On dynamic-contrast enhanced imaging (DCE), the inner layer demonstrates early enhancement usually in non muscle-invasive lesions. The muscular layer demonstrates late and progressive enhancement when non-interrupted, while bladder cancer demonstrates early enhancement.
On DWI the muscular layer is
visualized as an intermediate signal intensity layer. The inner layer cannot be
visualized. Cancer demonstrates restricted diffusion with high signal intensity
on DWI and low signal intensity on the ADC map.
In case of inflammation, the inner layer may show thickening and hyperintensity due to edema.
On T2W-images the edema will give a high signal of both the urothelium and the lamina propria, which will have some hyperemia.
On DWI and ADC the edematous inner layer is sometimes visible.
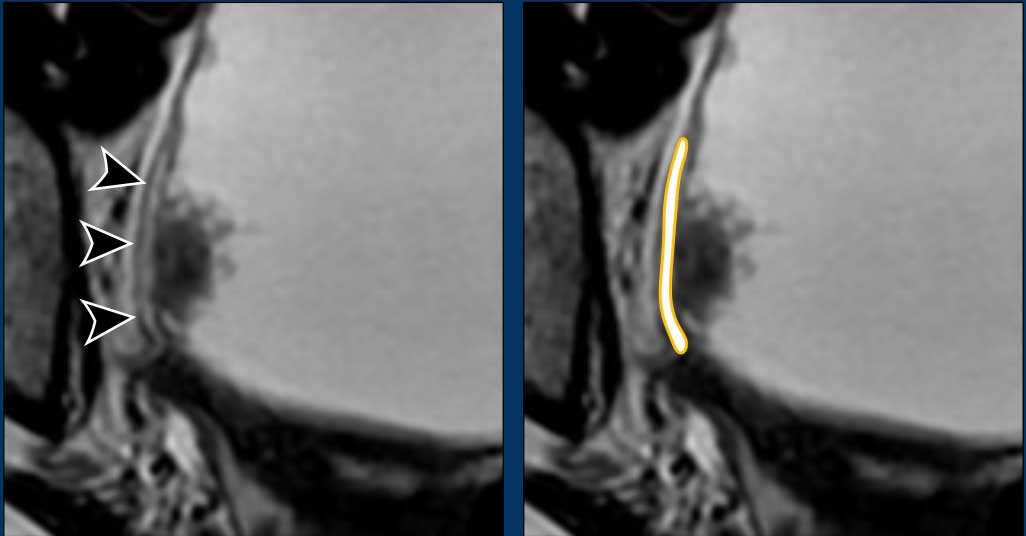
Here an example of edema of the inner layer on a T2W-image.
Edema
has high signal on T2W but urine also.
However because the edema is within the bladder wall, you can distinguish it.
On DCE images the edematous inner layer may show early enhancement due to the hyperemia (arrowheads).
VI-RADS
VI-RADS 1
- T2W - Sc1: Continuous low signal intensity line, indicating the integrity of the muscular layer, in lesions smaller than 1 cm. In the case of papillary tumors, they may present with or without a stalk and/or a thickened inner layer.
- DCE 1: Low signal intensity line of muscular layer, early enhancement of inner layer in lesions < 1 cm.
- DWI 1: continous intermediate signal intensity line of muscular layer in lesions <1 cm.
In the case of papillary tumors, they may present with or without a stalk and/or low signal intensity thickened inner layer.
Image
- There is a small lesion (< 1 cm) on the left postero-lateral bladder wall.
- There is full integrity of the low signal intensity line of the muscular layer
- T2-score: 1.
Continue with the DCE and Diffusion images.
Images
- DCE: the tumor shows early enhancement (arrow).
Notice also that the inner layer shows some enhancement. There is no enhancement within the muscular layer. - Diffusion: restricted diffusion with high SI on DWI and low SI on ADC.
Final VI-RADS score: 1
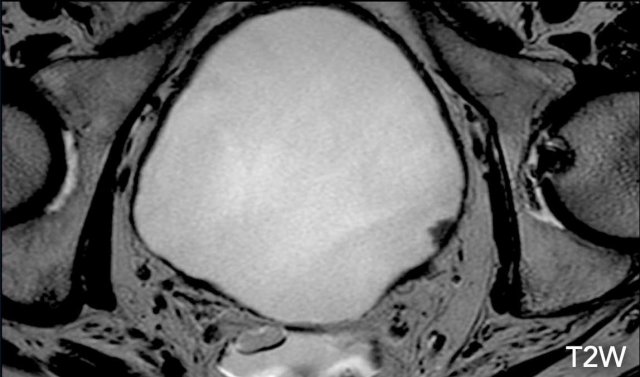
VI-RADS 2
- T2W Sc 2: Continuous low signal intensity line in lesions > 1 cm. In the case of papillary tumors with a stalk and/or a high signal intensity thickened layer, and in the case of sessile tumors with a thickened inner layer.
- DCE 2: Low signal intensity line of muscular layer doesn't show early enhancement in lesions > 1 cm.
- DWI 2: Continous intermediate signal intensity line of muscular layer in lesions > 1 cm.
In the case of papillary tumors with a low SI stalk and/or a low signal intensity thickened layer.
In the case of sessile tumors with a low/intermediate SI thickened inner layer in DWI.
Image
There is a papillary pedunculated lesion on the postero-lateral left bladder wall.
The diameter of the lesion is > 1 cm.
There is complete integrity of the muscular layer (T2W Score: 2).
Posterior to this lesion, there is a smaller second lesion indicated by arrow (T2W Score: 1).
Continue with the DCE image...
The tumor shows enhancement.
There is also enhancement of the inner layer adjacent to the lesion on the DCE sequence.
Continue with the diffusion images...
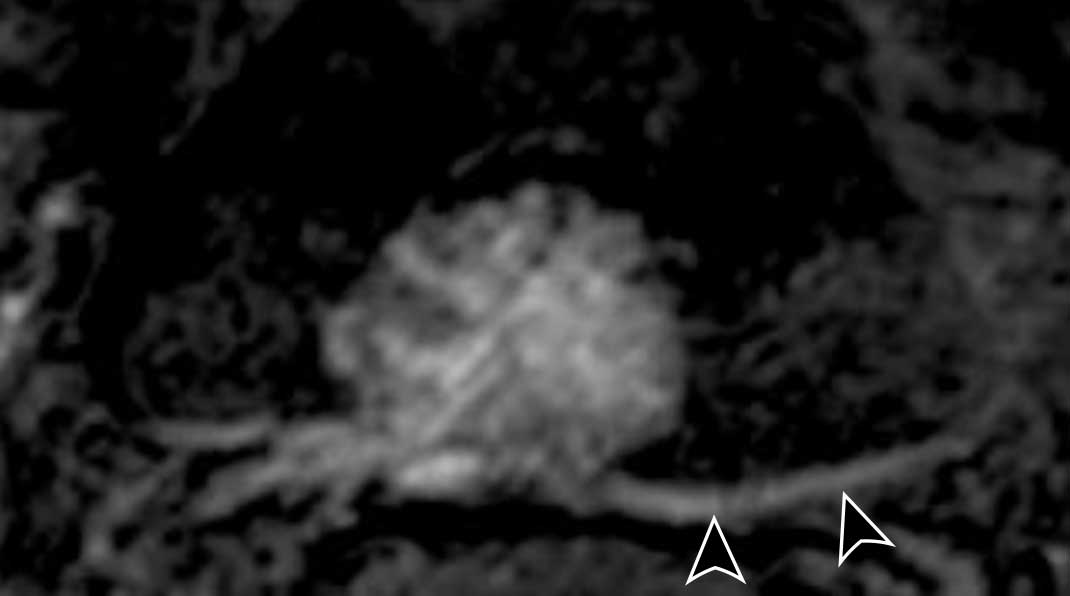
Images
You can appreciate the high signal intensity of the tumor on DWI and low
intensity in ADC sequence.
The tumor stalk has low intensity on DWI and
high intensity on ADC.
Score
- T2W: 2
- DCE: 2
- DWI/ADC: 2
Final VI-RADS score: 2
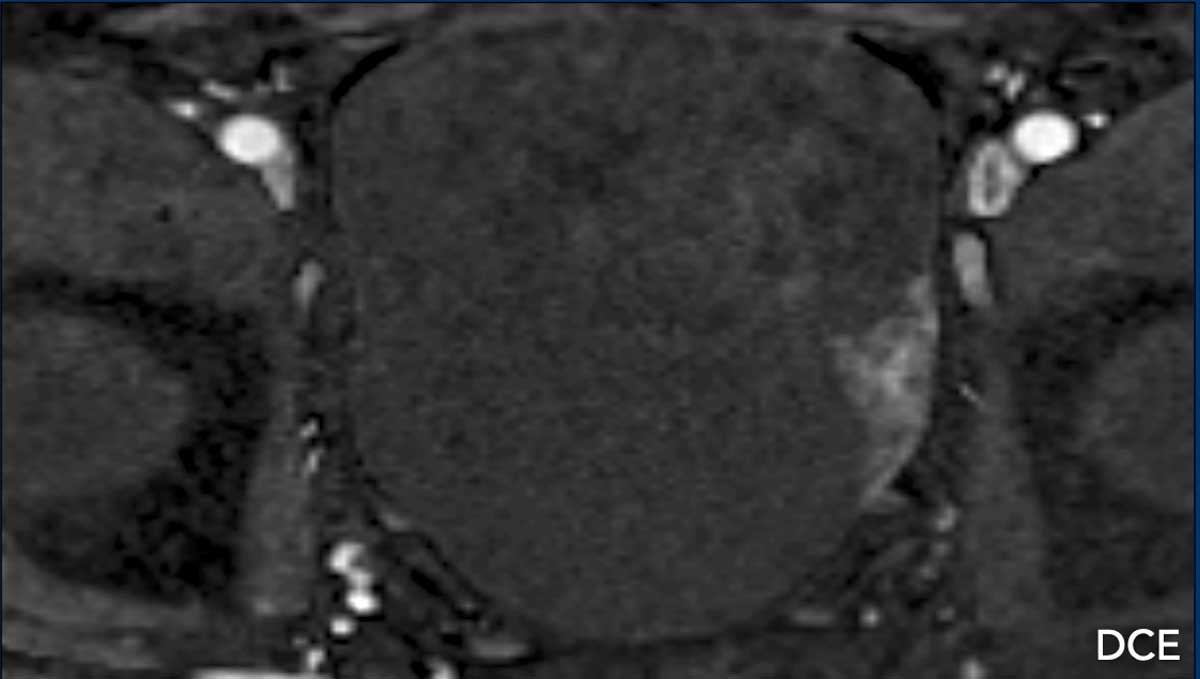
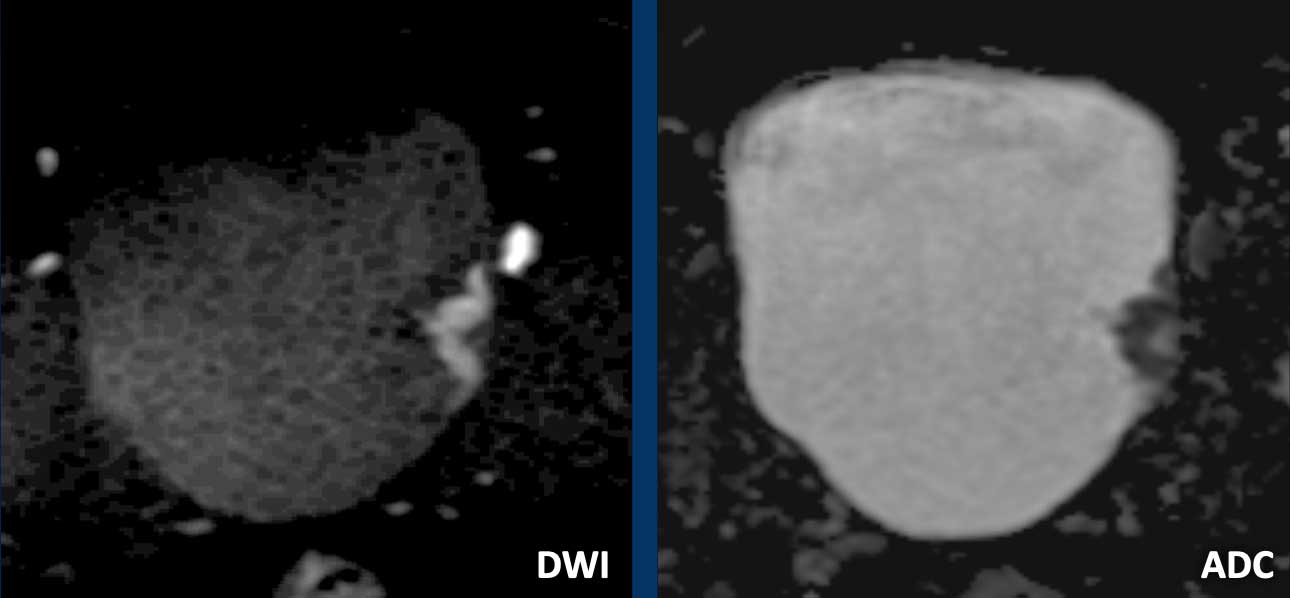
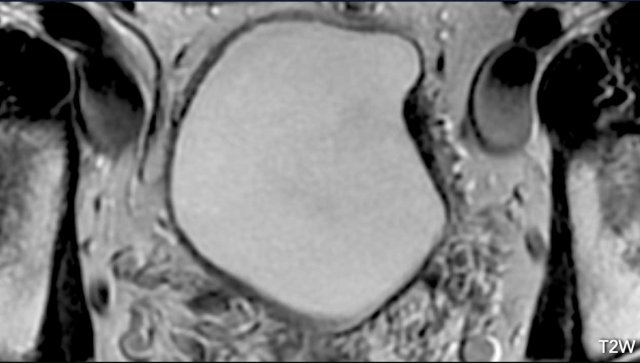
VI-RADS 3
- T2W Score 3: Absence of a stalk in a papillary tumor or absence of a high signal intensity thickened inner layer in a sessile tumor, while still maintaining the continuous low signal intensity of the muscularis propria.
- DCE 3: Lack of category 2 findings while still maintaining the continuous low signal intensity of the muscularis propria.
- DWI 2: lack of category 2 findings while still maintaining the continuous low signal intensity of the muscularis propria.
First look at the images.
What are the findings?
Image
There
is a sessile tumor on the lateral left bladder wall.
Since
there is no tumor stalk and inner layer, but there is also no clear
interruption of the muscular layer, this should be scored as T2W: 3.
Continue...
Next step is to study the DCE and diffusion images to differentiate between VI-RADS 2, 3 and 4.
Continue with the DCE and diffusion images...
Images
In the DCE sequence, there is a lack of
category 2 findings while still maintaining the continuous low signal intensity
of the muscularis propria.
Also, in DWI sequence there is no
clear disruption of the muscle layer.
Final VI-RADS score: 3
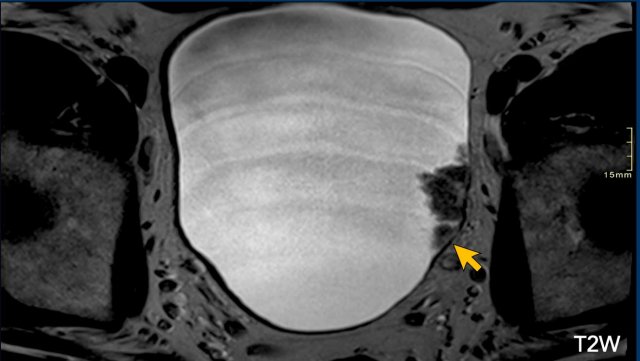
VI-RADS 4
T2W Score 4: Interruption of low signal intensity line of muscolaris propria, representing muscle invasion.
DCE 4: The tumor shows focal extension of early enhancement into the muscularis propria.
DWI 4: Tumor with high signal intensity on DWI and low signal intensity on ADC, extending focally into the muscularis propria.
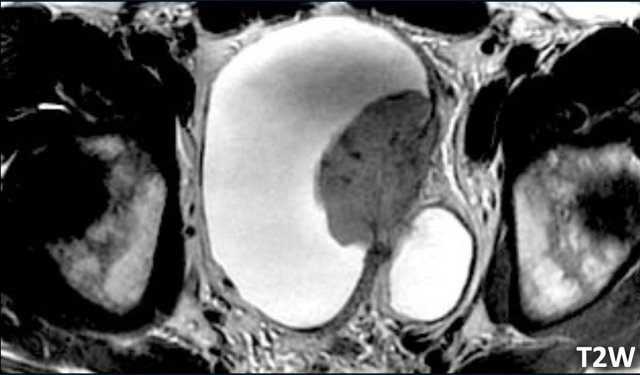
First look at the T2W-image.
What is your opinion?
Image
There is a large papillary tumor
on the left lateral bladder wall which infiltrates the hypointense line of the muscularis propria.
This is a difficult case to evaluate, as it looks like there is fat infiltration.
However T2W-images wiIl frequently overestimate fat invasion due to partial volume.
The next step is to study the DCE and diffusion images to differentiate between VI-RADS 4 and 5.
The DCE and DWI images will differentiate between VI-RADS 4 and 5.
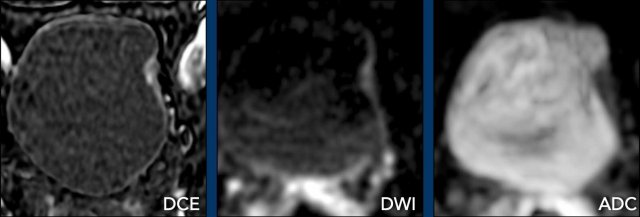
Continue with the DCE and DWI images...
Study the images.
What are the findings?
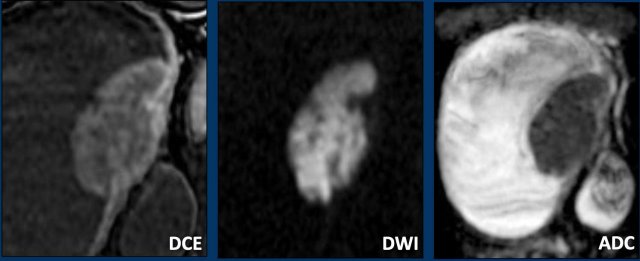
Findings
- DCE: The early enhancement of the muscular layer is clearly evident in the DCE sequence.
The tumor itself is hypovascular and does not extend through the enhancing muscular layer. - DWI/ADC: There is interruption of the muscularis propria, but no fat infiltration.
Conclusion
T2W 4/5, DCE 4 and DWI/ADC 4
Final
VI-RADS score: 4
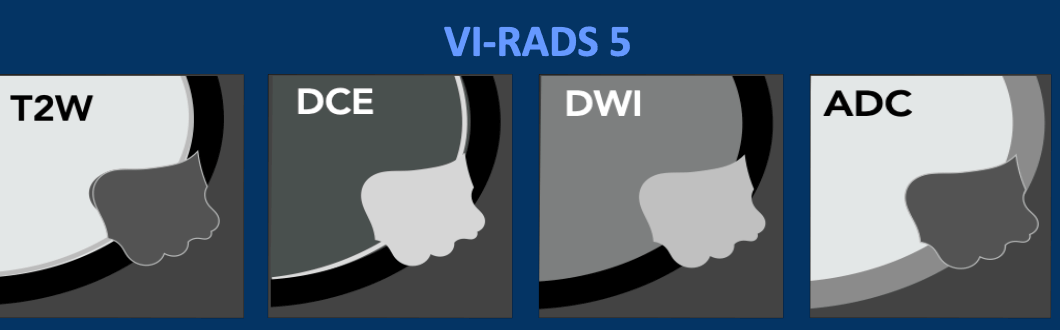
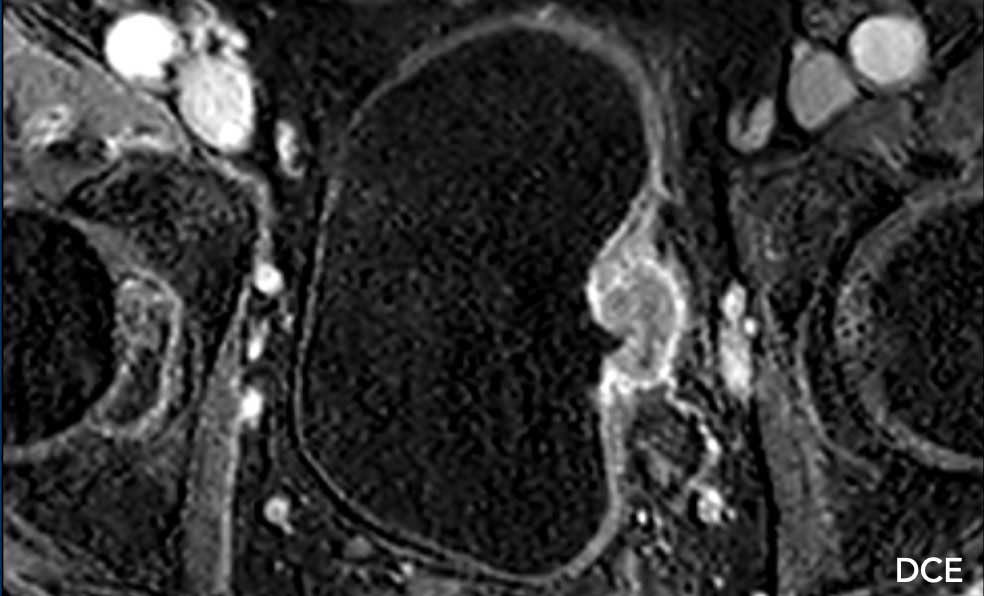
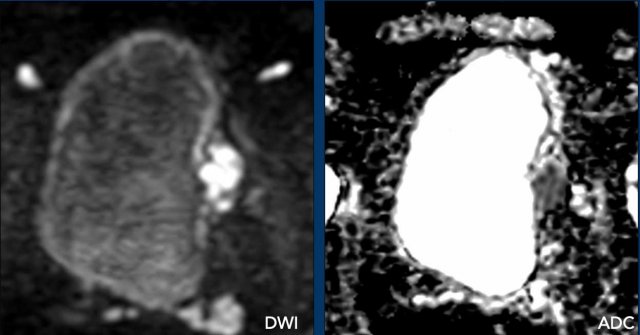
VI-RADS 5
- T2W Score 5
Tumor extends into peri-vesical fat. - DCE 5
The tumor shows extension of early enhancement into the extravesical adipose tissue. - DWI 5
Tumor with high signal intensity on DWI and low signal intensity on ADC, extending throughout the entire bladder wall and into the extravesical fat.
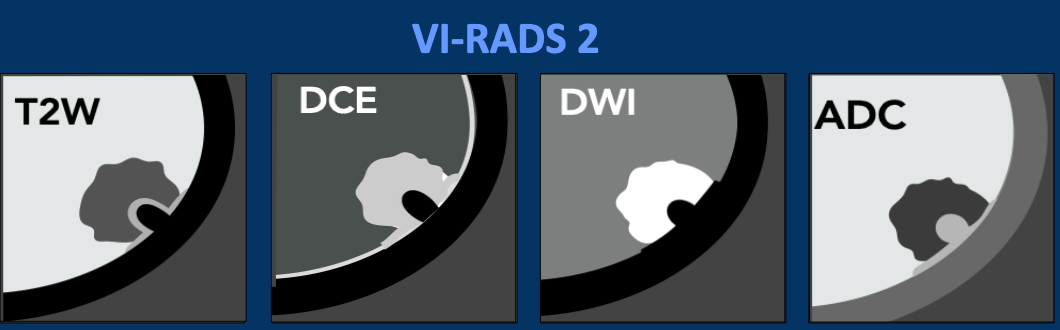
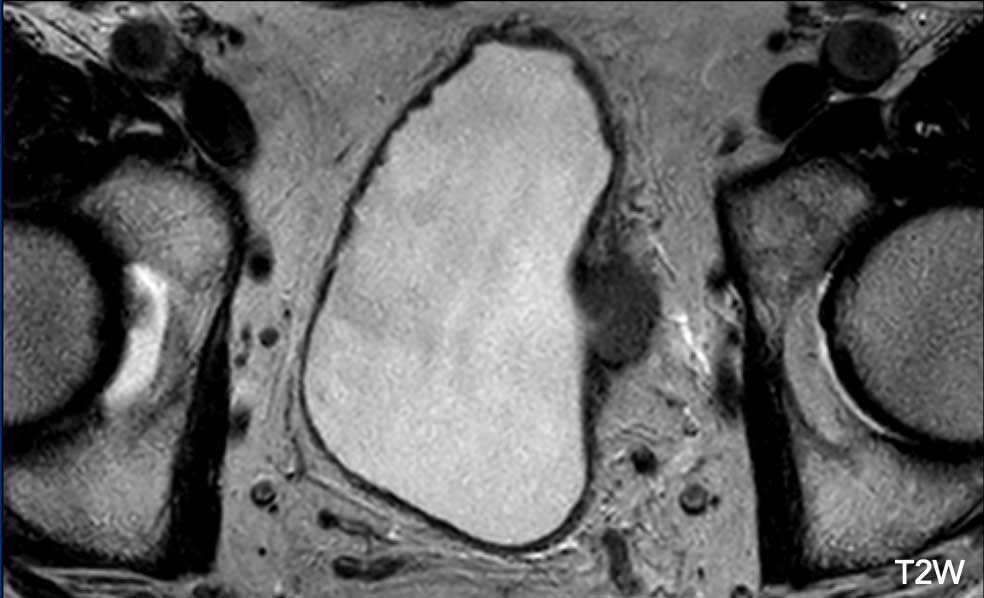
Image
There is a papillary non-pedunculated tumor on the right lateral wall.
You can appreciate perivesical fat infiltration by the tumor beyond the muscular layer.
This is a T2W score 5.
Continue with the next images...
Next step is to study the DCE and diffusion images to differentiate between VI-RADS 4 and 5.
Continue with the DCE and diffusion images...
DCE
There is early enhancement of the tumor invading the prevesical fat.
DWI/ADC
High signal
intensity of the lesion invading the perivesical fat is observed on the DWI
sequence, while there is low signal intensity on the ADC sequence.
Conclusion
T2W 5, DCE 5, DWI/ADC 5.
Final VI-RADS score: 5
MR protocol
Patient Preparation
Intramuscular antispasmodic agents should be administered to reduce motion and susceptibility artifacts from bowel peristalsis.
Figures
- Without antispasmodic agents
- With antispasmodic agents
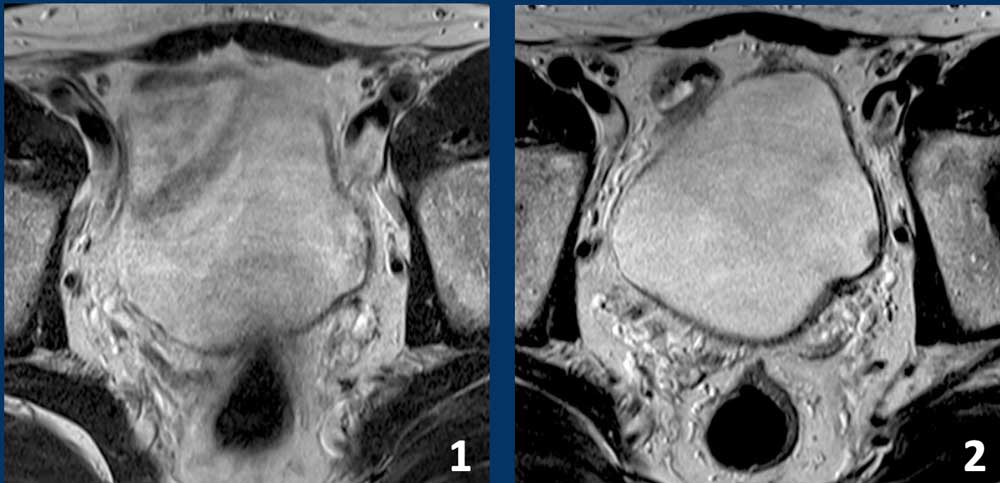
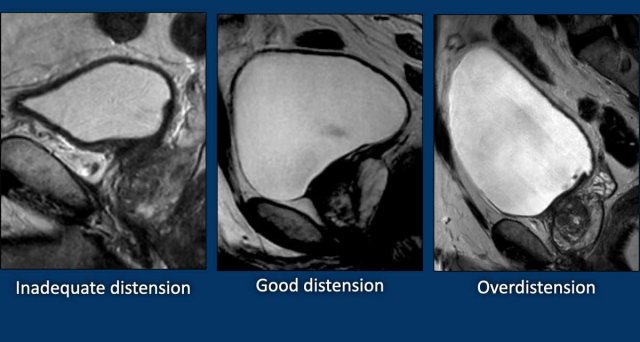
Bladder distension
Optimal bladder distension is crucial for accurate tumor staging.
These images are all of normal bladders.
- Inadequate distension
there is a thick and uneven appearance of the bladder wall, potentially leading to misdiagnosis or overestimation of tumor staging. - Proper bladder distension.
Instruct the patient to void 1–2 hours before imaging or drink 500–1000 ml of water in the 30 minutes before the examination, depending on tolerance.
The convexity of bladder dome suggest optimal bladder distension (2). - Overdistension.
This can induce discomfort-related motion artifacts and may obscure the extent of bladder cancer.
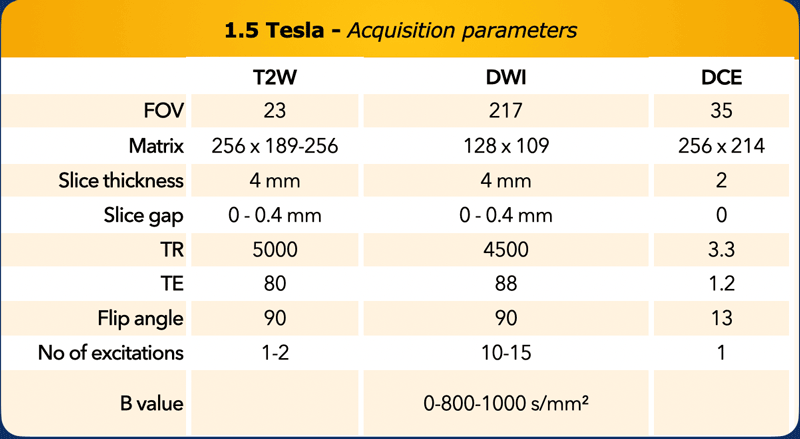
Acquisition parameters for a 1.5 Tesla scanner.
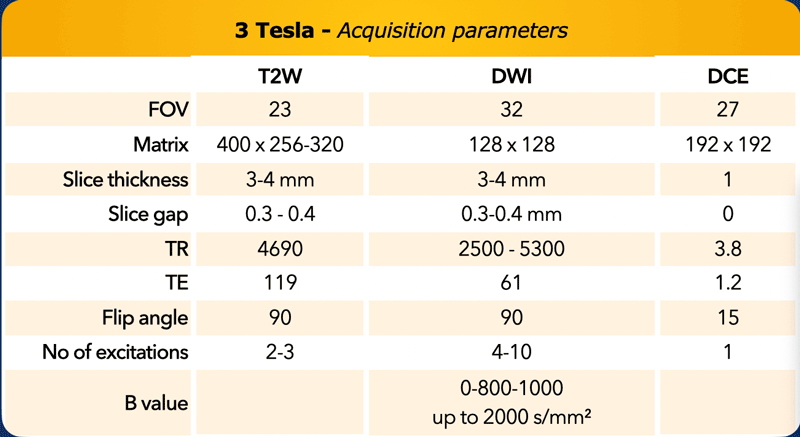
Acquisition parameters for a 3 Tesla scanner.