Thymic masses and mimics
Bram Geurts and Hanke Schalkx
Radboud University Medical Center in the Netherlands
Publicationdate
Thymic tumors are in many cases an incidental finding during CT examinaton for another reason.
Most patients with thymic tumors are asymptomatic at the time of diagnosis and many thymic tumors are not easily diagnosed histopathologically.
Therefore, imaging plays an important role in the evaluation of thymic lesions.
Introduction
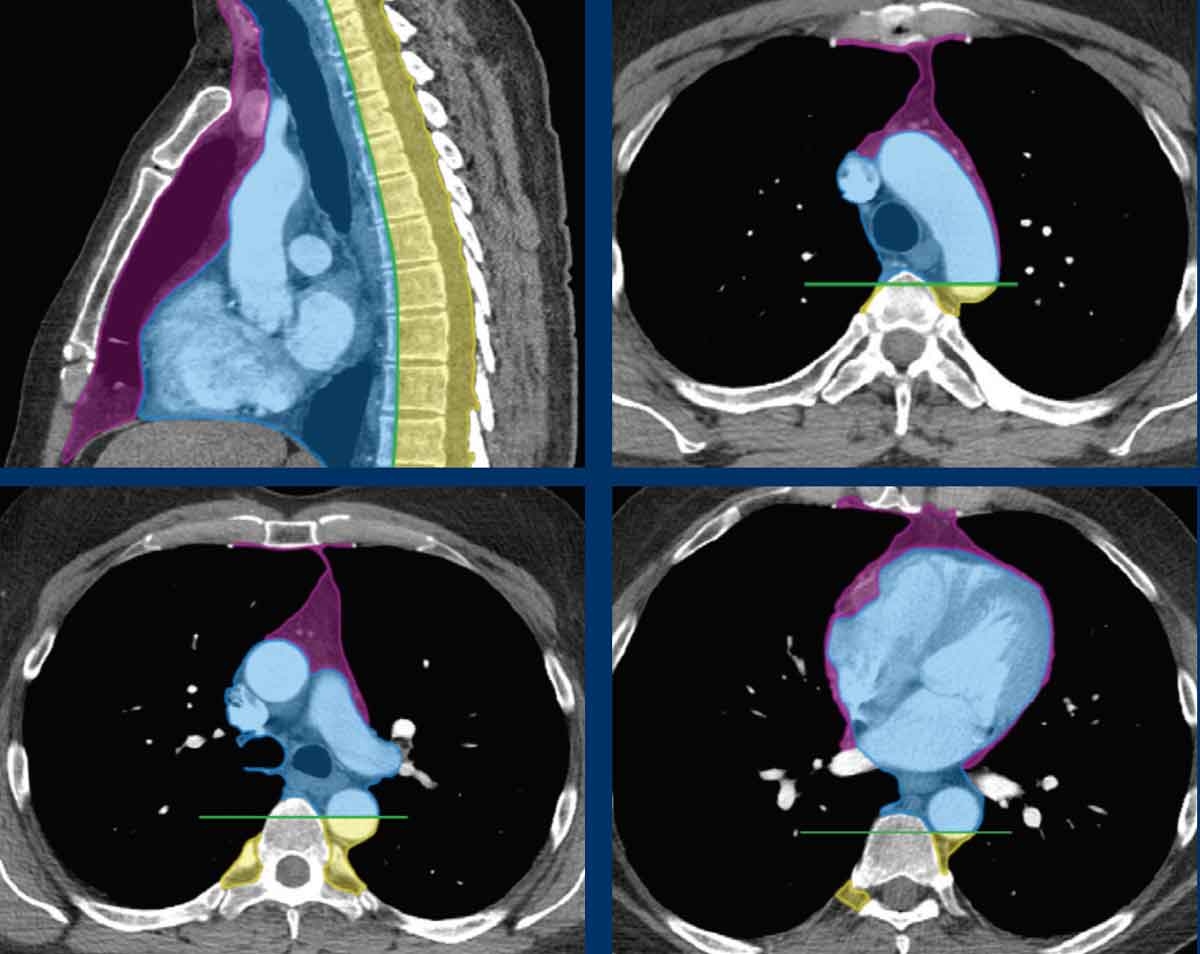
ITMIG Classification of Mediastinal Compartments
Most radiology classifications in the past have been based on arbitrary landmarks outlined on the lateral chest radiograph and dividing the mediastinum in an anterior, middle and posterior compartment.
A new scheme based on cross-sectional imaging, principally multidetector computed tomography (CT), has been developed by the International Thymic Malignancy Interest Group (ITMIG) and is now accepted as a new standard.
This ITMIG division scheme defines prevascular, visceral, and paravertebral compartments based on boundaries delineated by specific anatomic structures at multidetector CT.
The prevascular compartment contains the thymus, fat, lymph nodes and the left brachiocephalic vein.
Notice that the posterior border is the anterior aspect of the pericardium as it wraps around the heart in a curvilinear fashion.
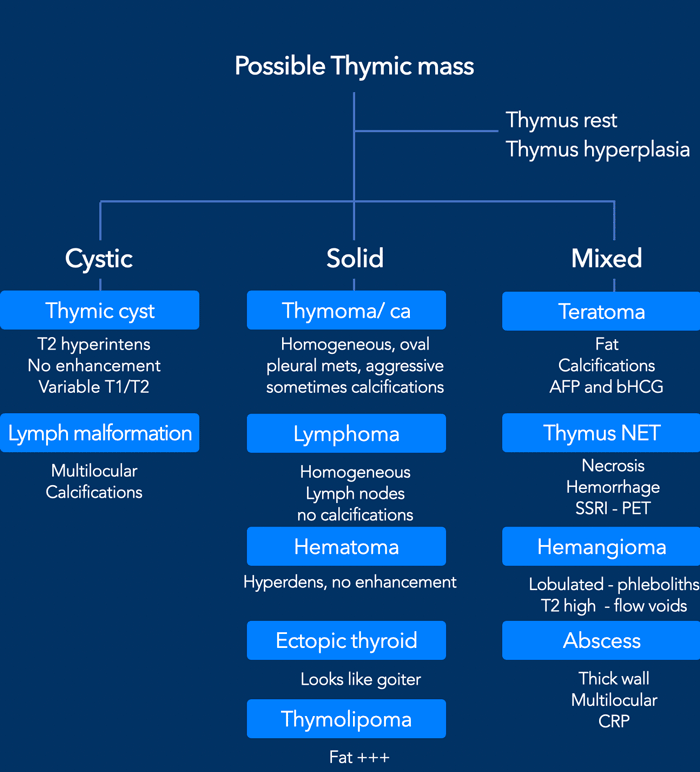
Differential diagnosis
When you are confronted with a possible thymic mass you have to distinguish a normal thymus and thymic hyperplasia from thymic neoplasms and lymphoma.
A normal but large thymus aswell as a hyperplastic thymus is triangular in shape and has a normal signal intensity on T1W- and T2W-images and contains either extracellular or intracellular fat.
The most common neoplasms of the prevascular mediastinum include thymoma, thymic carcinoma, thymic neuroendocrine tumors, teratoma and lymphoma.
Nonneoplastic lesions include substernal extension of thyroid goiter, thymic hyperplasia, cystic lesions such as thymic and pericardial cysts and vascular-lymphatic abnormalities.
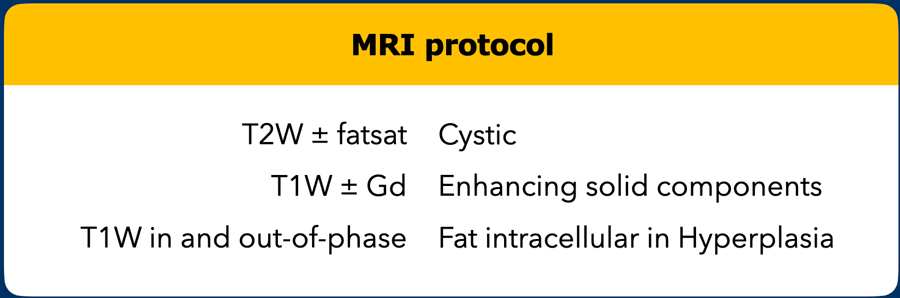
MR protocol
Although most thymic masses are found incidentally on chest CT, MRI is the best imaging tool to further differentiate a possible mass.
T2W-images help to detect cystic components.
T1W-images in- and out-of-phase help to detect intracellular fat and to distinguish a normal thymus and thymic hyperplasia from thymic neoplasms and lymphoma.
Gadolinium is used to detect solid components.
Fat saturation can be applied either in the T1W- or the T2W-series.
Normal thymus
The normal thymus is relatively large in infancy and grows considerably immediately after birth.
The maximum size is achieved at puberty and then the thymus undergoes progressive involution with fatty replacement.
A normal thymus in adults has an arrowhead shape, straight regular margins.
It contains fat, but no calcification and cyst formation and the density is equal to the surrounding muscle.
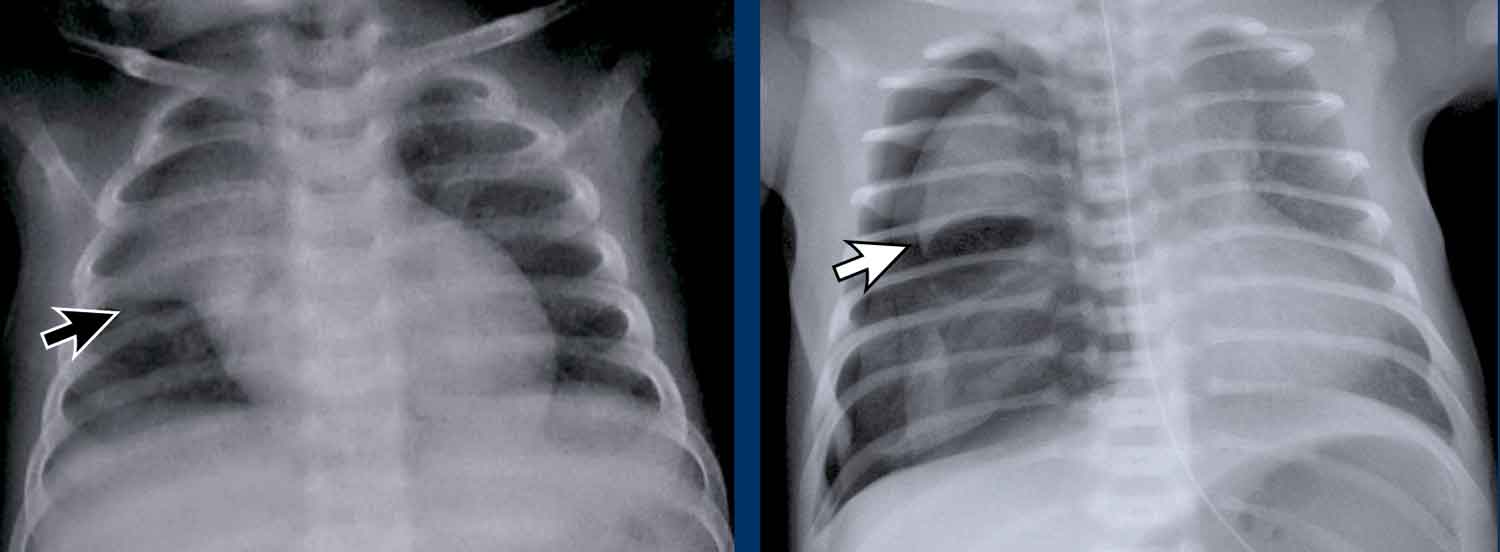
In neonates the thymus can be quite large, especially when there is respiratory stress and may present on a chest X-ray with the sail sign (black arrow).
The thymic sail sign is a normal finding in infants and should not be confused with the spinnaker-sail sign, where the thymic lobe is laterally and superiorly displaced due to a pneumomediastinum (white arrow).
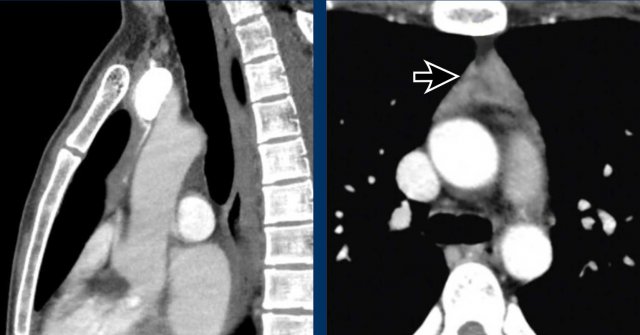
These images are of a 24-year old male.
First study the images.
Question: is this a normal thymus?
Images
Although this thymus is quite large, it has a normal triangular shape and it contains fat (arrow).
This is a normal thymus.
Thymus hyperplasia
Graves' disease
Case 1
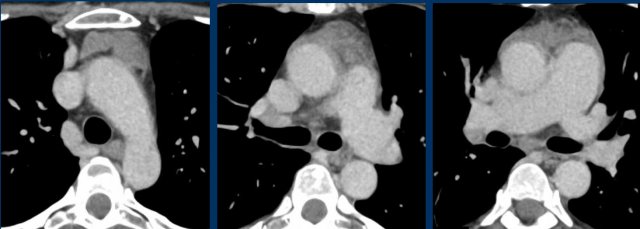
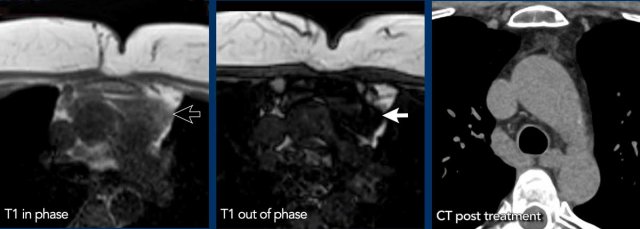
These images are of a 65-year-old woman with a history of Graves' disease, an autoimmune disorder that involves overactivity of the thyroid.
A CT was performed because of hemoptoe.
First study the images.
What is your opinion?
Images
There is a large bulky thymus that contains macroscopic fat.
This is a typical picture of thymus hyperplasia.
Thymic hyperplasia in Graves' disease is related to excess thyroid hormones and thyrotropin receptor antibody.
It usually improves after successful treatment of Graves' disease.
Although not necessary, a MRI was performed.
Images
The out-of-phase fast gradient-echo image shows signal loss as we would expect.
The CT shows normalization of the thymus after treatment of the Graves’ disease.
When you measure the signal intensity, you will find a drop in signal intensity.
The percentage in signal drop is called the signal intensity index (SII).
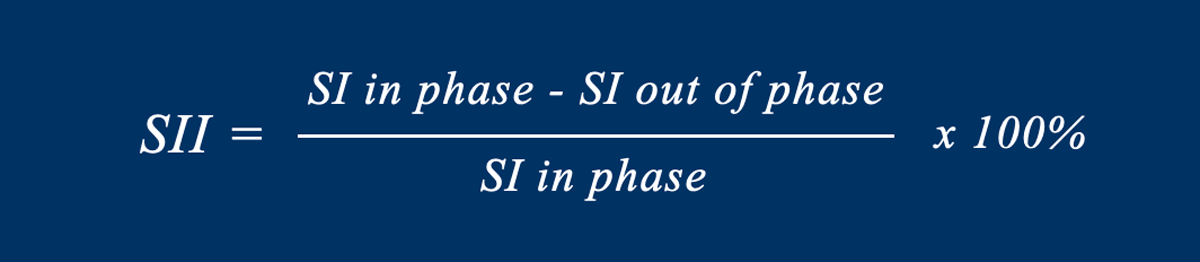
Signal intensity index
The Signal intensity index (SII) is the amount of signal drop divided by the original amount of signal.
A SII more than 9% has a 100% sensitivity and specificity for the diagnosis hyperplasia.
The SII is more reliable than the chemical shift ratio.
In this case the SII was 77%.
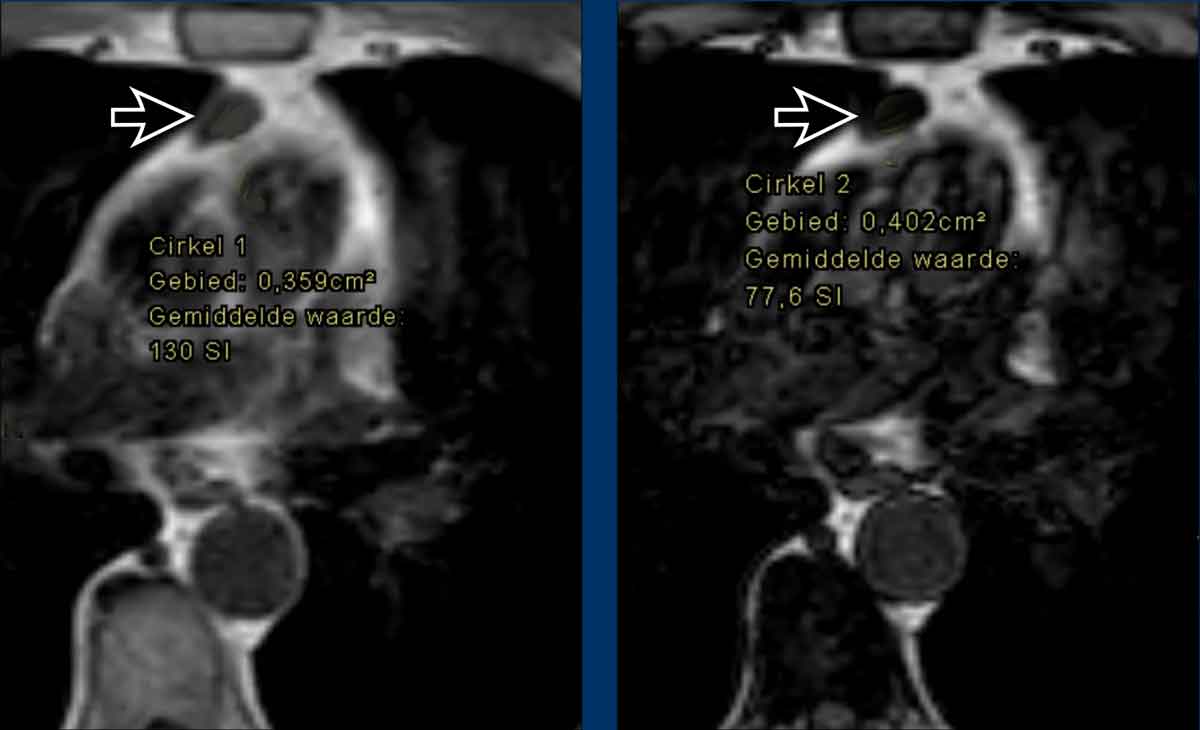
Case 2
Here another case.
The signal drop is from 130 to 77.
This means that we are dealing with thymic tissue.
Rebound thymic hyperplasia
Thymic hyperplasia may be a rebound effect.
First the thymus will decrease in size as a result from stress from chemotherapy, steroids, radiation therapy, burns or other severe systemic stressors.
When the stress is gone, the thymus will increase in size and may become even much bigger than its original size.
After this rebound effect it may take several months for the thymus to return to its normal size.
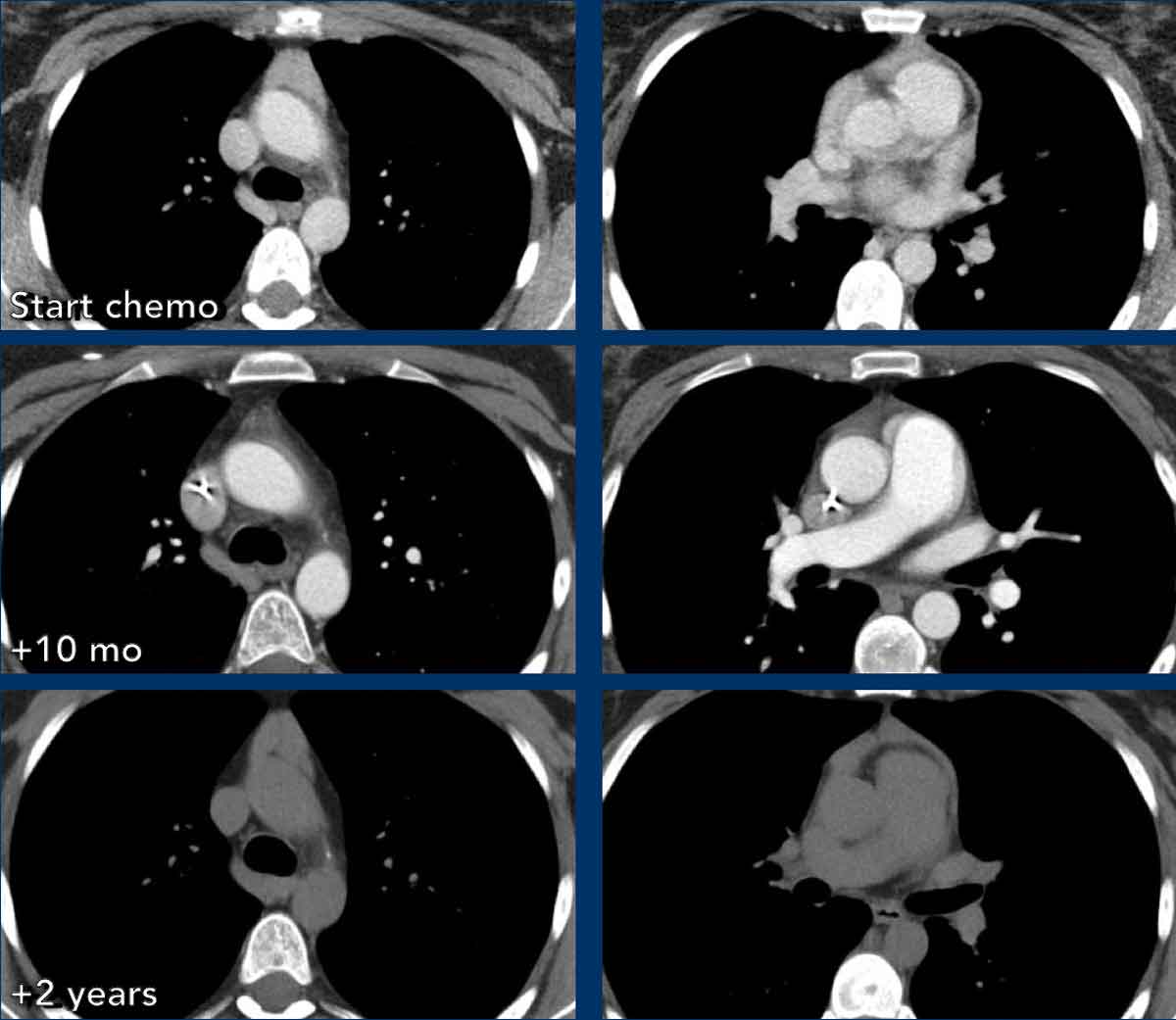
Case 3
These images are of a 24-year-old woman, who had an osteosarcoma and was treated with chemotherapy.
Images
At the start of the therapy there is hyperplasia of the thymus.
At 10 months follow up the thymus is atrophic.
Two years later there is rebound hyperplasia.
Case 4
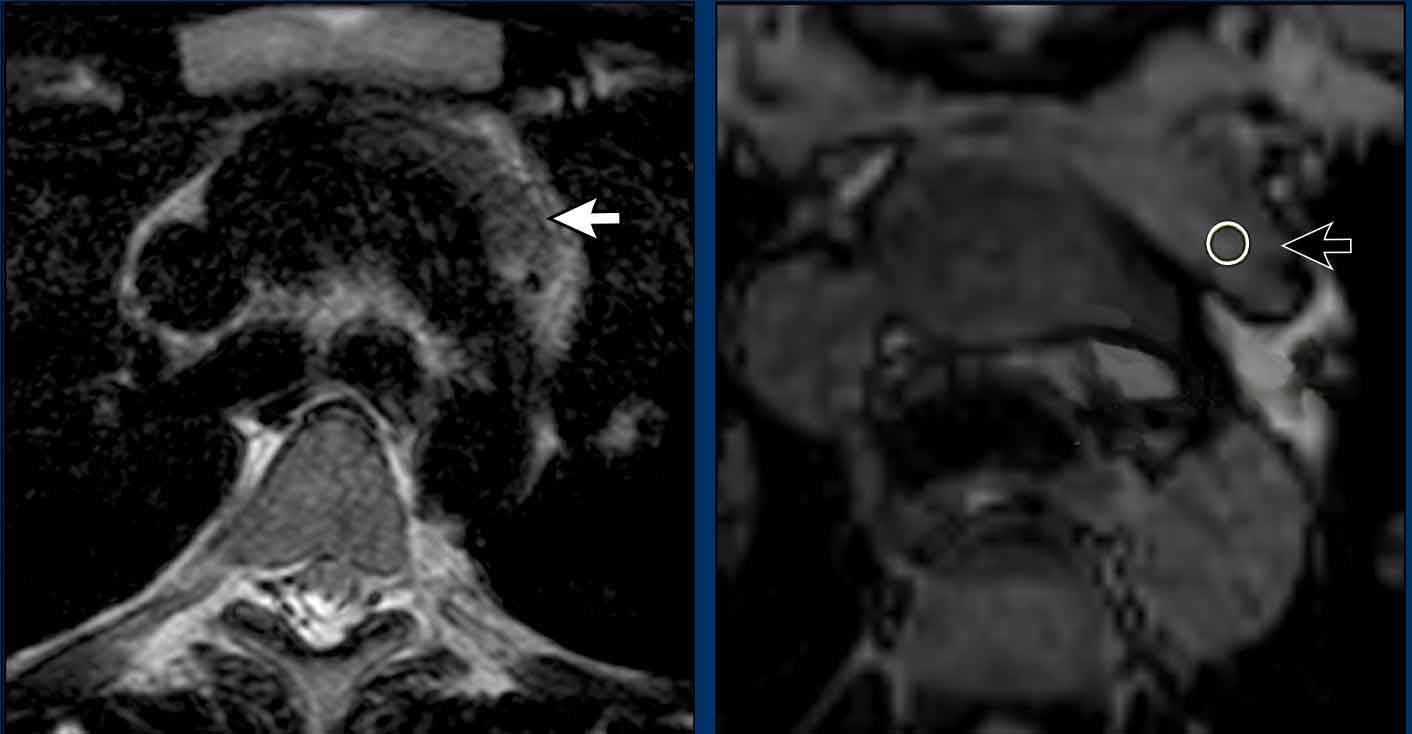
These images are of a 19-year-old man M19, who had a CT to rule out pulmonary emboli.
An incidental mass was seen in the prevascular space.
The most likely diagnosis was thymic hyperplasia and an MRI was performed to further differentiate this mass.
Continue with the MRI...
On the T2W-image the lesion was slightly intense.
On the out-of-phase image there wasn't much signal drop.
The SII was less than 9%.
Because the patient didn't have any complaints and especially no symptoms that could be associated with lymphoma and because a thymoma is a rare tumor, it was decided to do a six months follow up.
At six months follow up there is a normal thymus.
It was concluded that this was thymus hyperplasia or a large thymus rest, which involuted during the six months.
Myasthenia gravis
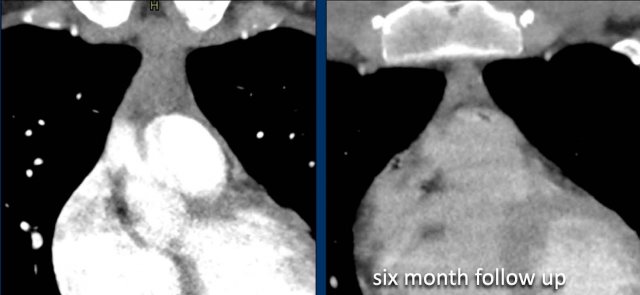
The thymus is believed to play an important role in the pathogenesis of myasthenia gravis, an autoimmune disease mediated by antibodies against the acetylcholine receptor of skeletal muscles.
75% of patients with myathenia gravis has an abnormal thymus.
After resection of the thymus 70-80% of the patients will show improvements.
Cystic masses
True cysts are uncommon and look just like any other cyst in the body.
Cystic degeneration in thymoma is a relatively frequent but focal event. In rare cases, the process proceeds to the extent that most of the lesion becomes cystic.
Mediastinal teratomas usually present as a heterogeneous mass with fat and calcifications. About 15% present as a pure cystic lesion.
Pericardial cysts are pure cystic lesions most commonly located in the right anterior cardiophrenic angle, but sometimes they have an unusual location.
Thymic cyst
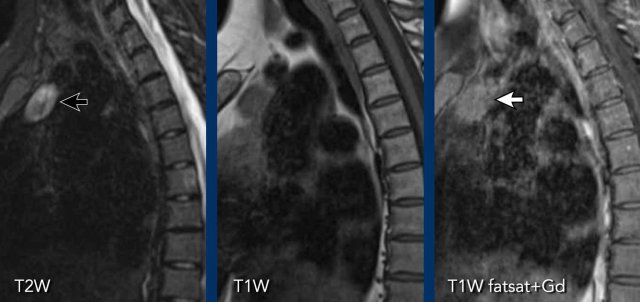
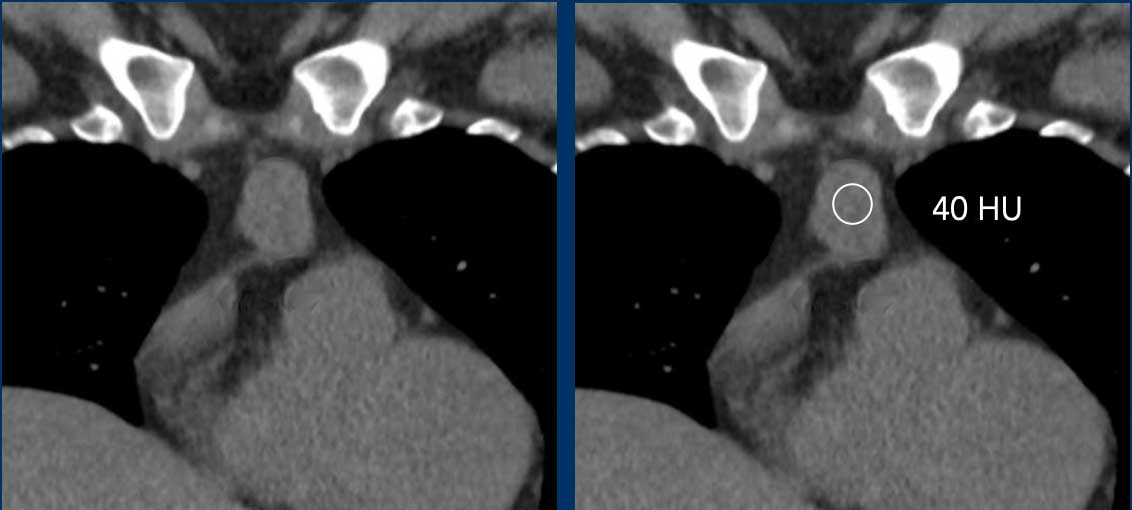
These images are of a 48 year old woman.
On a TWK-MRI an incidental thymic mass was seen.
Continue with the CT images...
On a NECT the lesion has a soft tissue density of 40 HU.
The most likely diagnosis was a thymoma.
The lesion was resected and to our surprise turned out to be a cyst.
The explanation for the confusing imaging findings is that the cyst contained a protein-rich substance which explained the high density on the NECT.
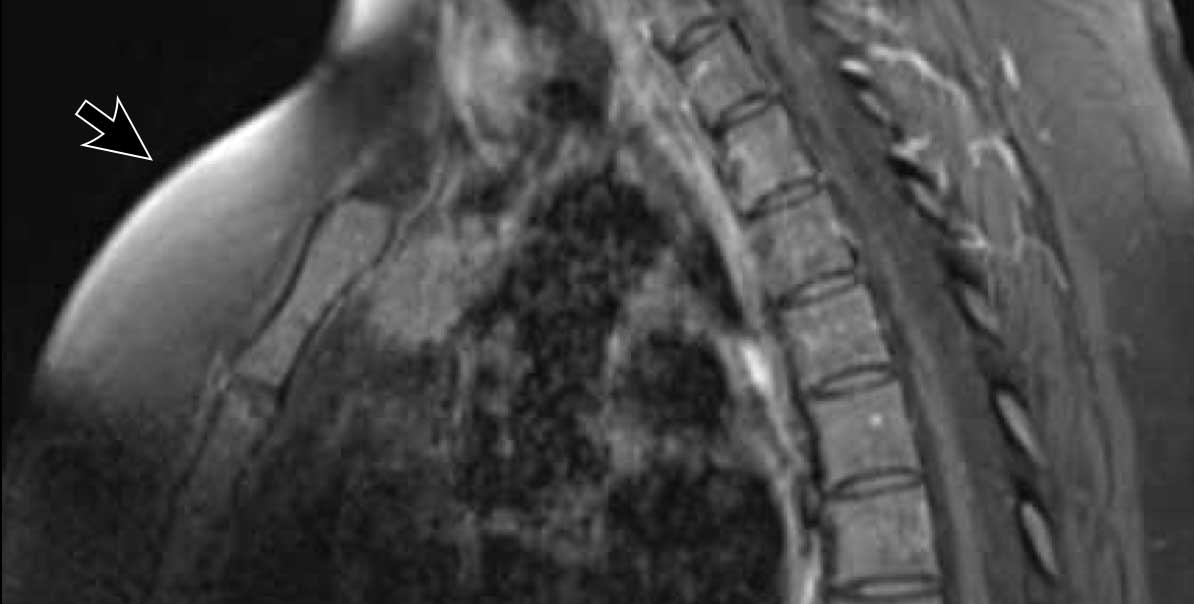
What looked like enhancement on the T1W-image with fatsat is probably due to inhomogeneous fat saturation.
Continue with the next image...
Notice the inhomogeneous fat saturation (arrow).
This resulted in pseudo-enhancement and a wrong diagnosis.
Final diagnosis
Thymic cyst.
Cystic Thymoma
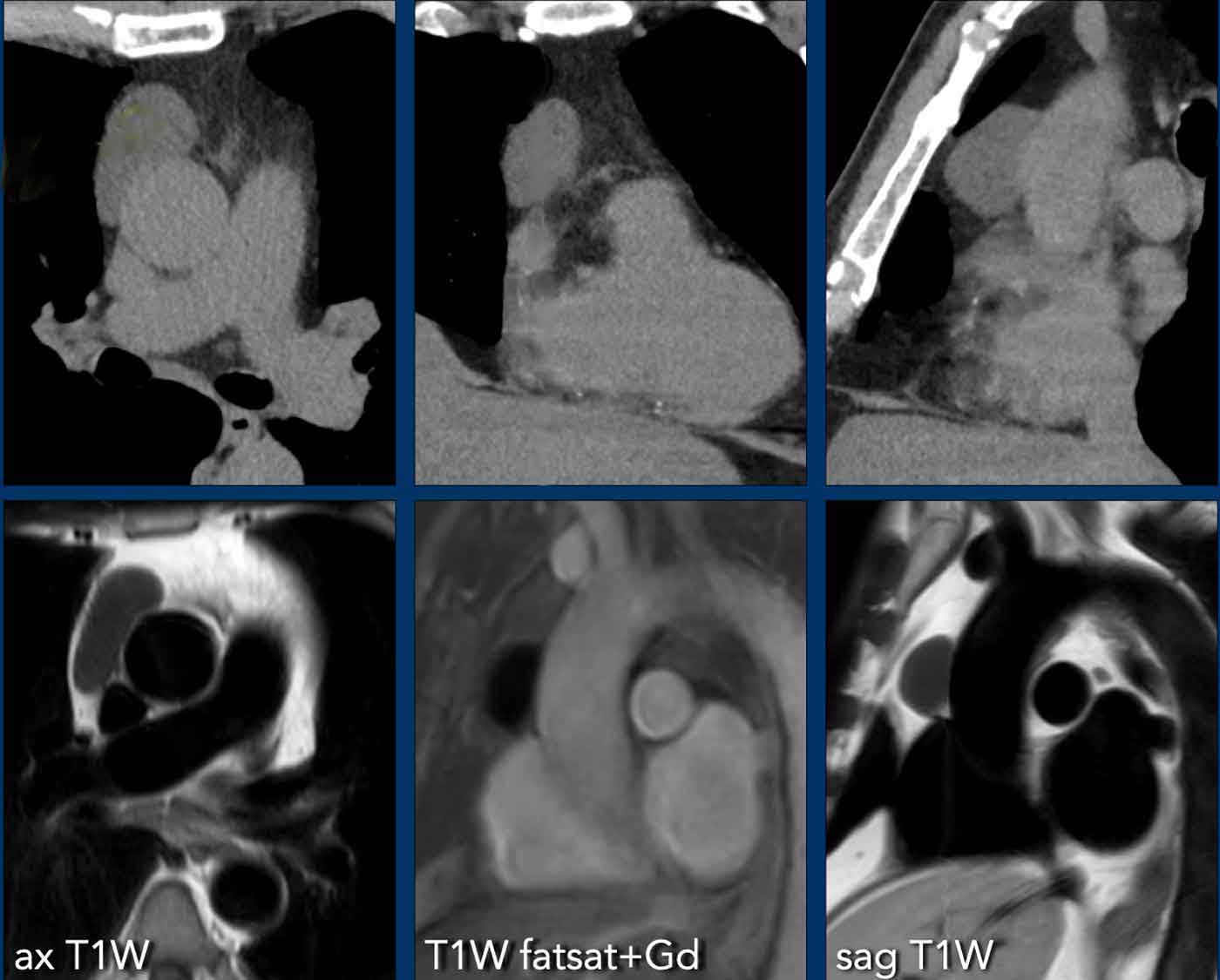
These images are of a 71 year old man.
On a chest CT an incidental thymic mass was seen.
Study the images. What is your opinion.
Images
Part of the lesion is enhancing and there are some calcifications probably located in the wall.
When a thymic lesion has solid parts, then the rule is..."when in doubt, take it out".
The lesion was resected based on the CT-findings and turned out to be a cystic thymoma.
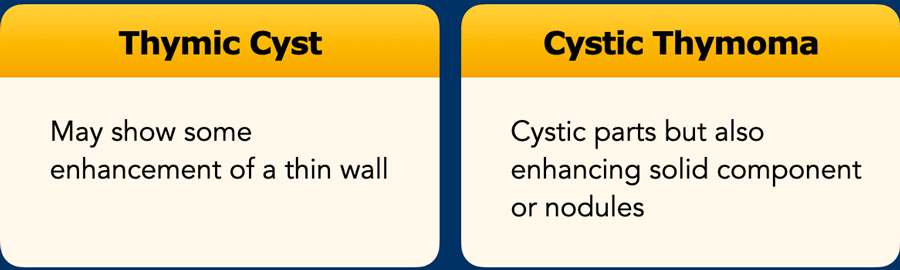
Cyst versus cystic thymoma
A cyst may show some enhancement but it should only be enhancement of thin walls.
There should be no nodules or solid components.
Sometimes this differentiation can be very difficult and in such cases a follow up is recommended first at 6 months and the yearly up to five years.
The follow up can be done with MR or in some cases with CT.
Pericardial cyst
Images
On CT the lesion in the prevascular space has a water density.
On MRI there is no enhancement.
This was a pericardial cyst.
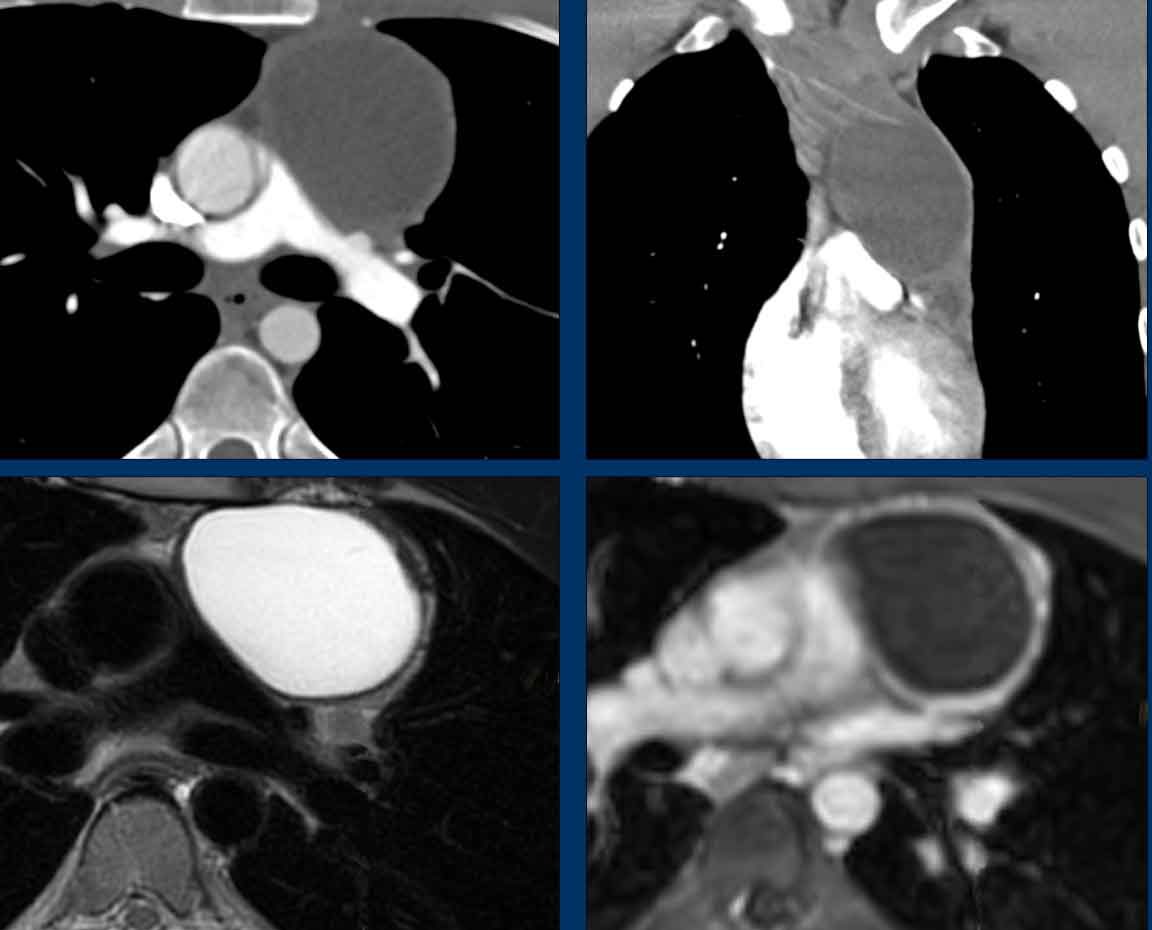
Lymphoma
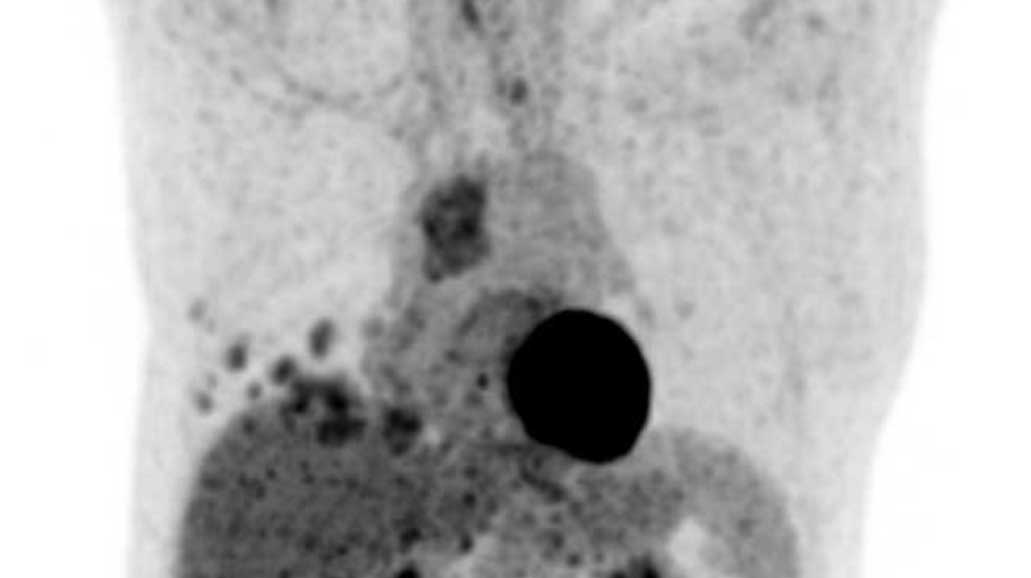
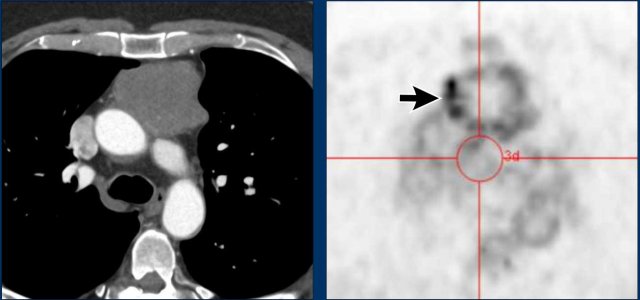
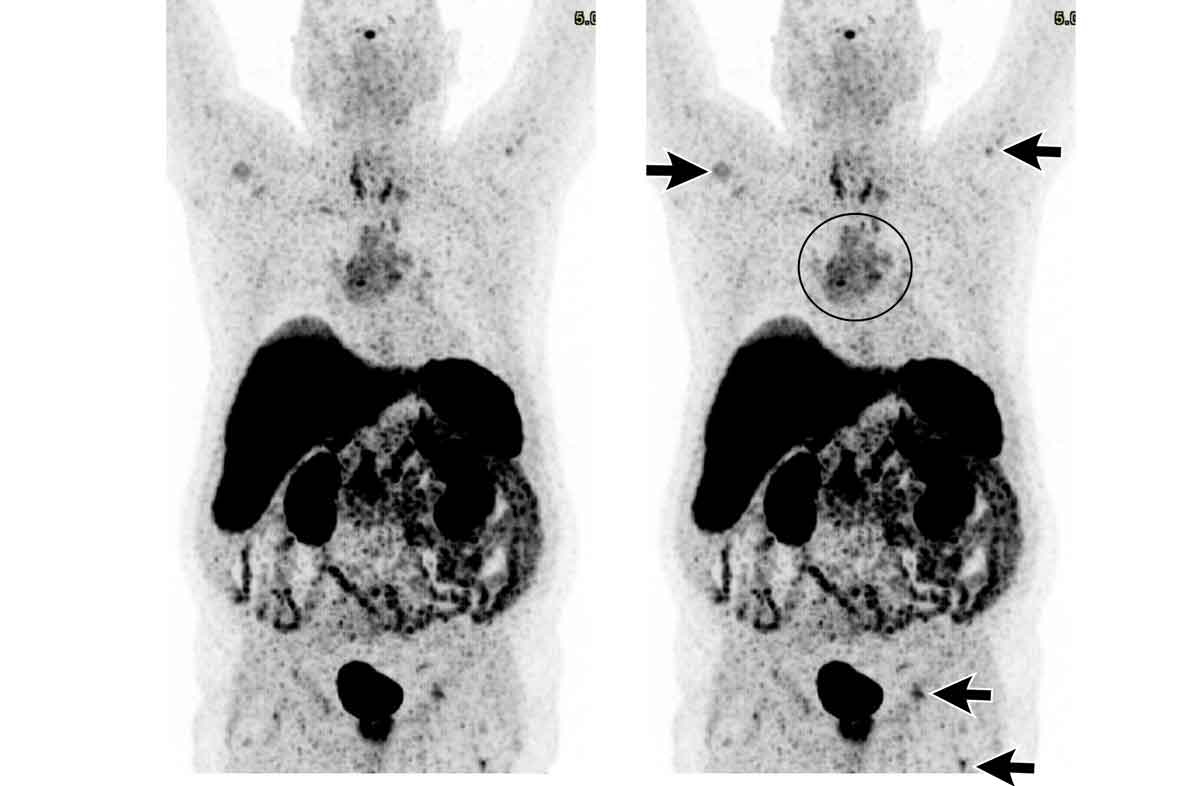
These images are of a 34-year-old female with dyspnoe.
Study the images.
What is your opinion?
Images
There is a cystic mass in the prevascular mediastinal space.
There are thick enhancing walls.
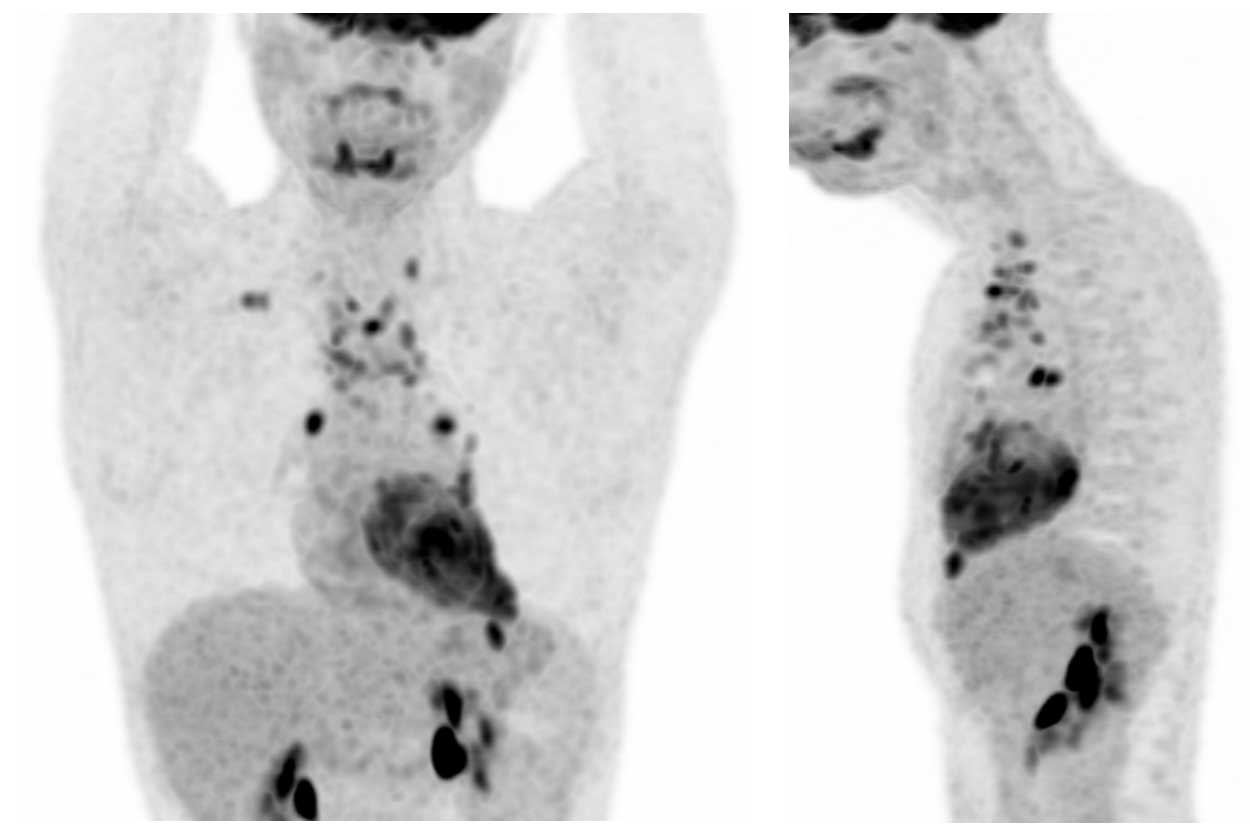
Because it still wasn't clear what we were dealing with a PET was performed.
Continue with the PET images...
Based on the PET-findings which diagnosis is the most likely?
Is it a cystic thymoma, complicated cyst, neuroendocrine tumor or a lymphoma?
Images
The PET shows multiple lesions, which must be pathologic lymph nodes.
Discussion
A thymoma is almost never accompanied by lymphadenopathy.
An infected cyst could also give rise to lymphadenopathy, but not so widespread as in this case.
Final diagnosis
Cystic lymphoma.
Solid masses
Thymoma/carcinoma
Thymic epithelial neoplasms are a group of malignant tumors that includes thymoma, thymic carcinoma, and thymic neuroendocrine tumors.
Thymic tumors are classified as thymomas, thymic carcinomas, and neuroendocrine thymic tumors (NETT).
Thymoma is the most common tumor in the prevascular mediastinal compartment, but still is a rare tumor.
It is linked to myasthenia gravis and other autoimmune paraneoplastic diseases.
Case 1
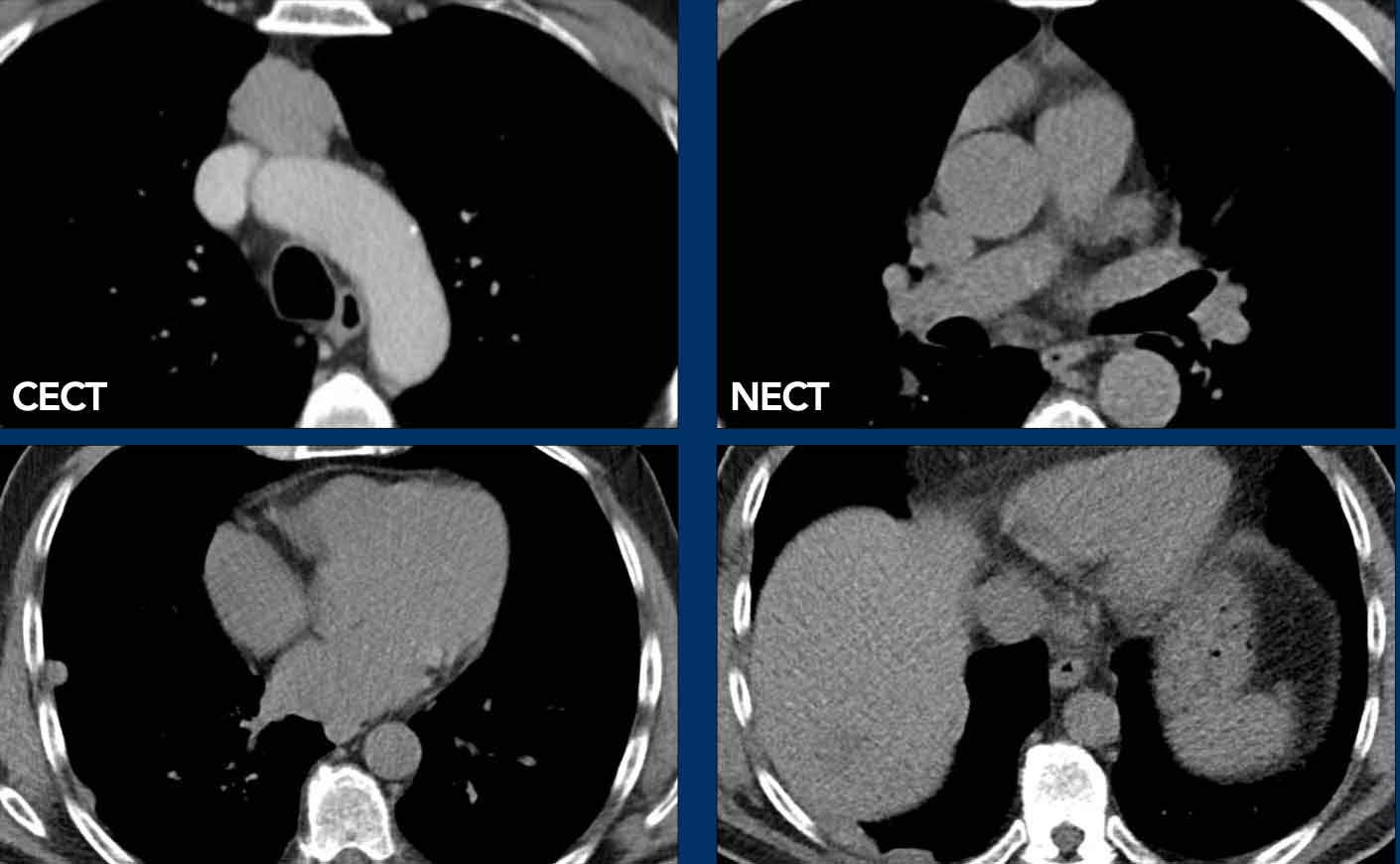
These images are of a 60-year old male with chest pain, who had a chest CT for calcium scoring.
First study the images.
What is your opinion?
Images
There is a solid mediastinal mass and there are pleural lesions.
Discussion
The pleural lesions were only seen on the right side and this is typical for pleural drop metastases of a thymoma.
They are the result of direct invasion of the pleura and are not hematogenous metastases and are only seen on one side.
Continue with the PET...
The PET shows the mass in the mediastinum and the multiple pleural metastases only on the right side.
Case 2
These images are of a patient who had a resection of a thymoma.
In the follow up scan on the left a pleural metastasis was detected.
Notice that in retrospect there already was a tiny pleural lesion on the preoperative scan.
The lesson is, that when you think of a thymoma, you have to study the pleura with extreme attention.
"You will only find what you are looking for".
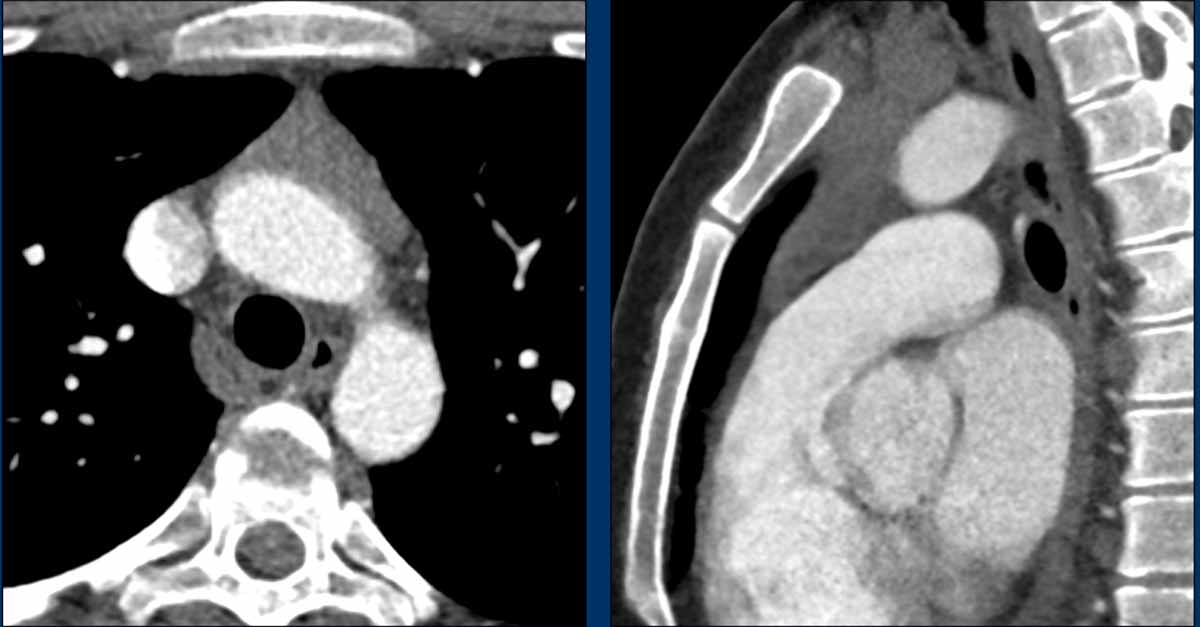
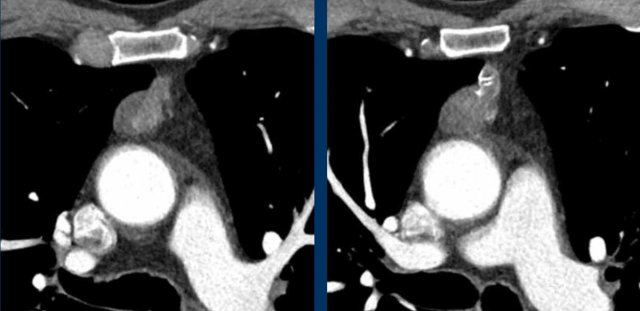
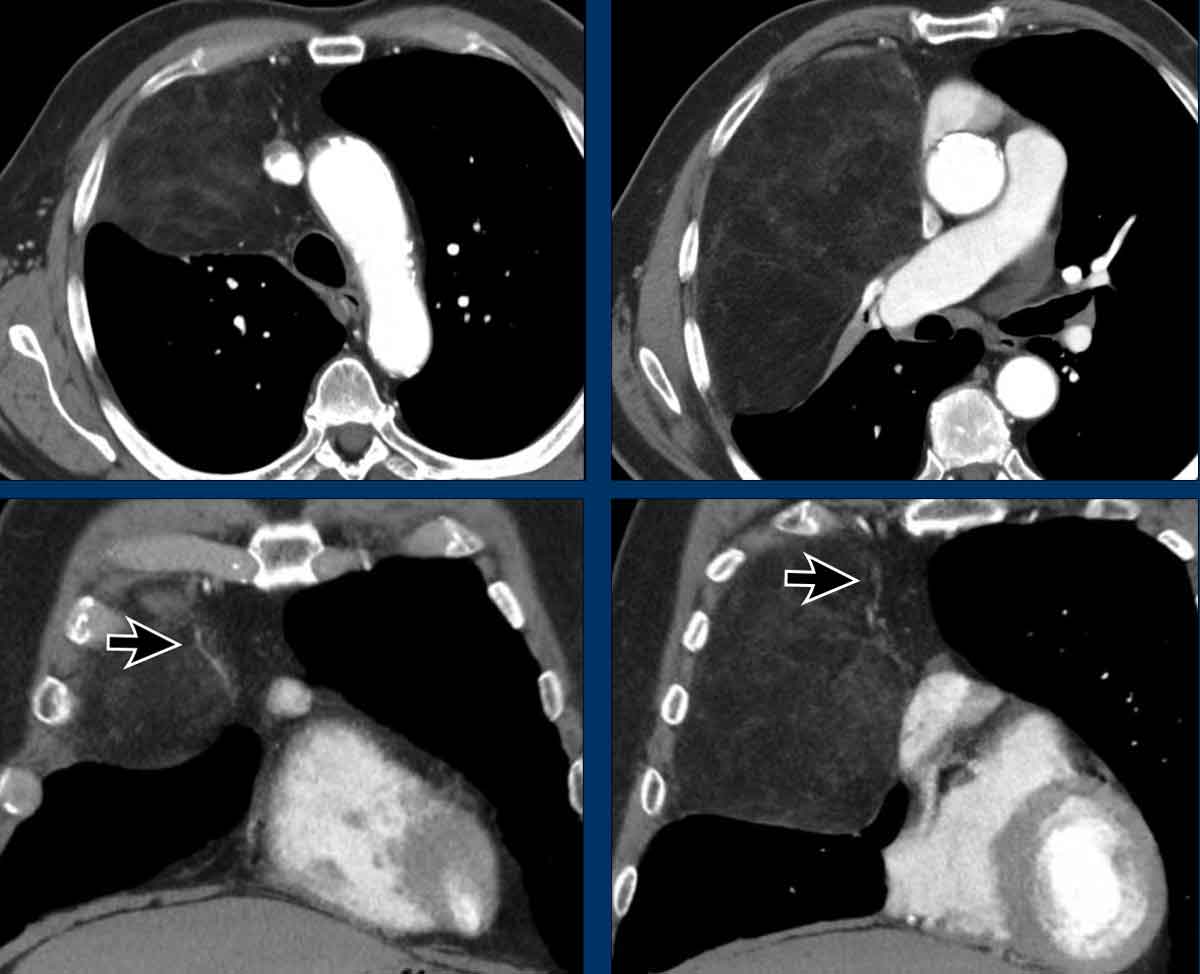
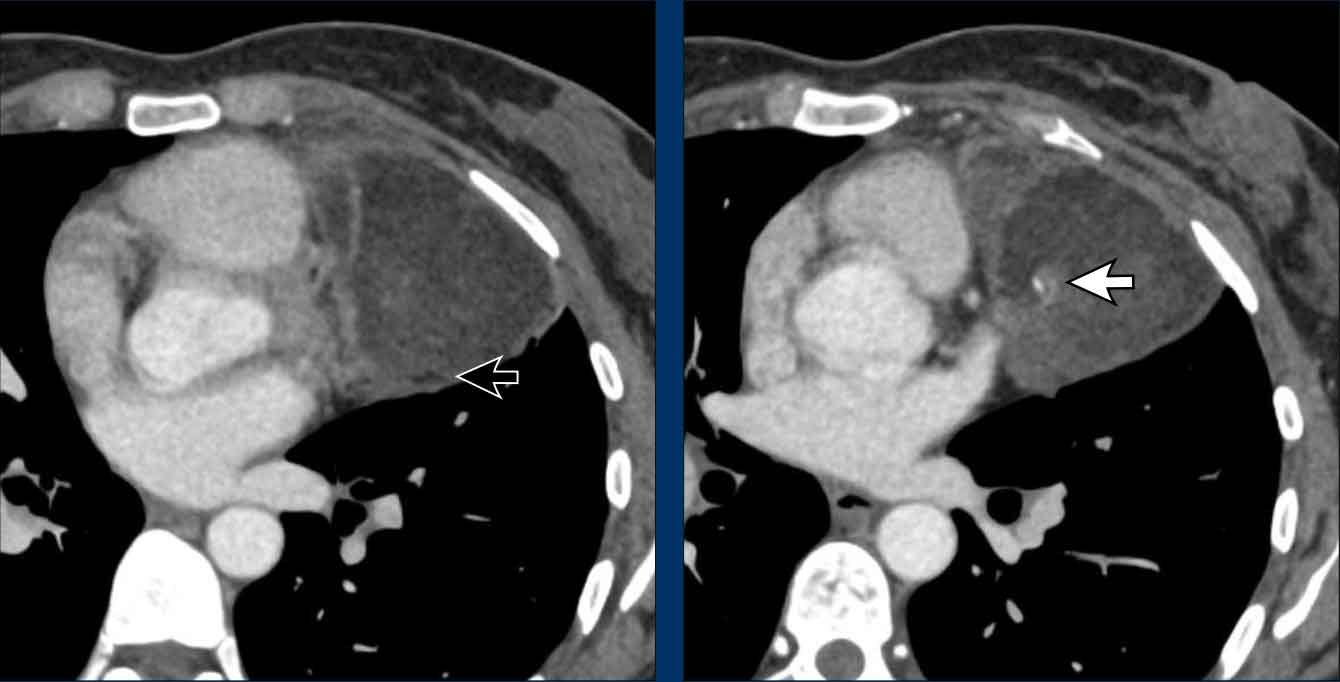
Thymic carcinoma
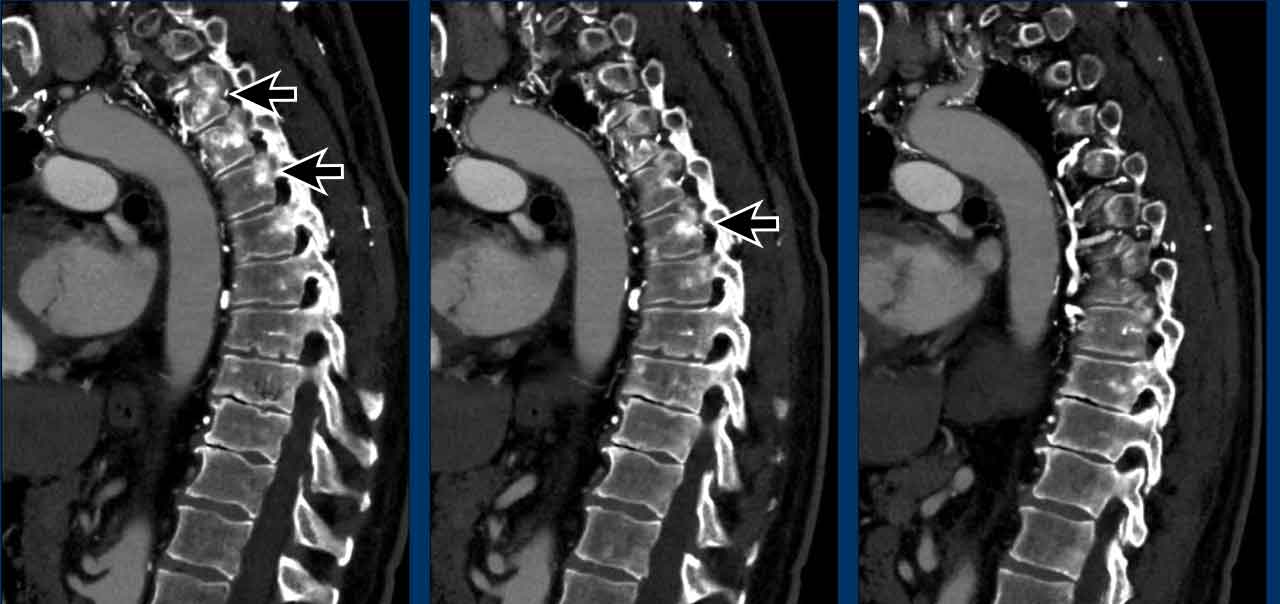
Case 1
These images are of a patient with a thymus carcinoma.
Notice the irregular activity in the periphery of the lesion on the PET.
The tumor was resected.
In the follow up a CT was made.
Continue with the follow up CT...
On the CT new hyperdense structures were seen in the vertebrae (arrows).
They were not there on a previous CT.
What is your opinion?
First study the images and then continue reading.
Images
Note the presence of dilated venous collaterals. This is explained by the fact that during surgery, the brachiocephalic vein is ligated, which can lead to the development of significant venous collaterals. The hyperdense structures observed in the vertebral bodies are not indicative of sclerotic metastases, but rather a consequence of venous congestion. These findings represent enhancement due to venous congestion, not metastatic disease. On a non-contrast CT, this hyperdensity would not be visible.
Continue with a later follow-up scan...
On a later follow up scan the venous congestion is not visible anymore.
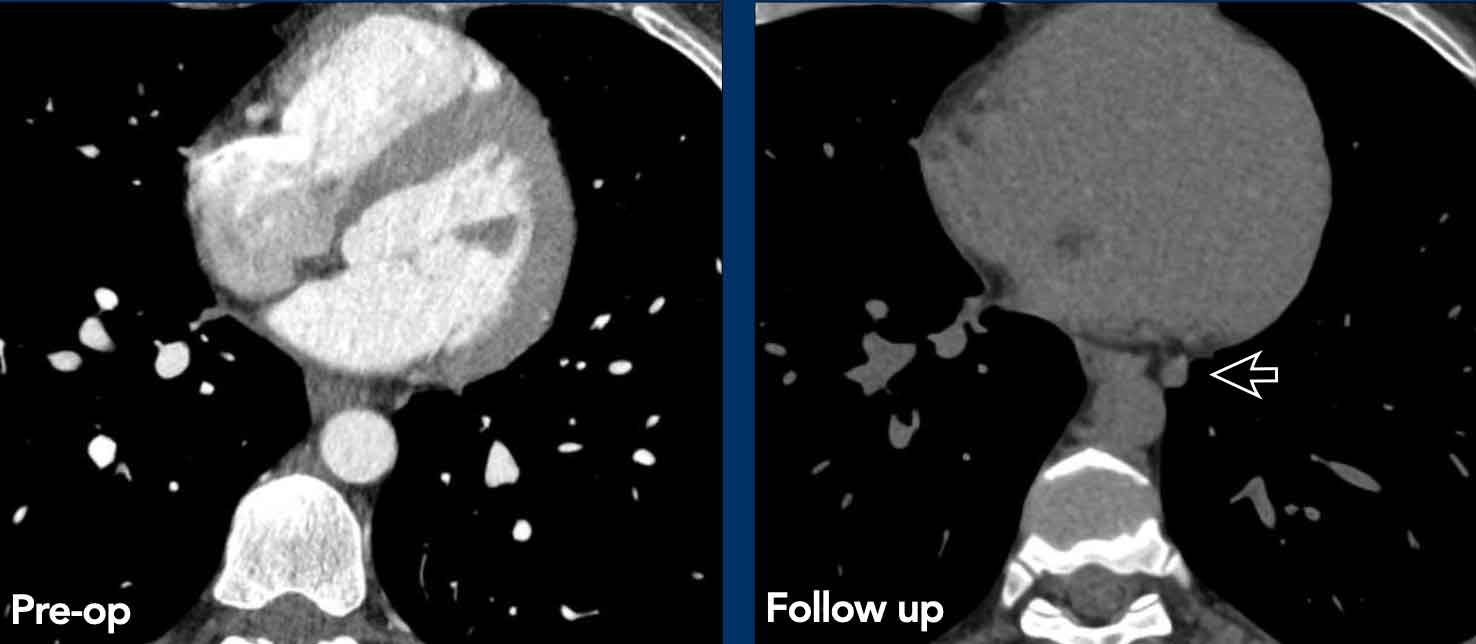
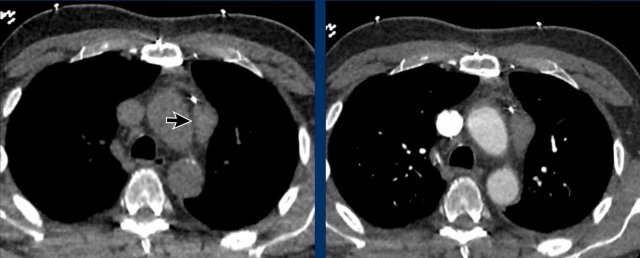
Case 2
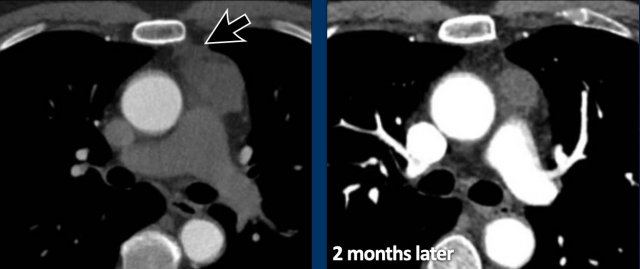
These images are of a 43-year-old male with chest pain.
Images
There is a mass in the prevascular mediastinum.
The border is irregular and the lesion is positive on a PET-CT.
Discussion
The most likely diagnosis was a thymoma, probably invasive or even a carcinoma.
Continue with a preoperative scan two months later...
Two months later a preoperative scan was performed.
It is clear that the lesion is smaller.
However the surgeon decided to resect the lesion anyway and it turned out to be a thymus carcinoma.
We have no clear explanation for what happened here.
There is some reaction in the soft tissues surrounding the tumor on the first scan (arrow).
Maybe there was some inflammation within the tumor and surrounding tissues, which made the tumor look bigger.
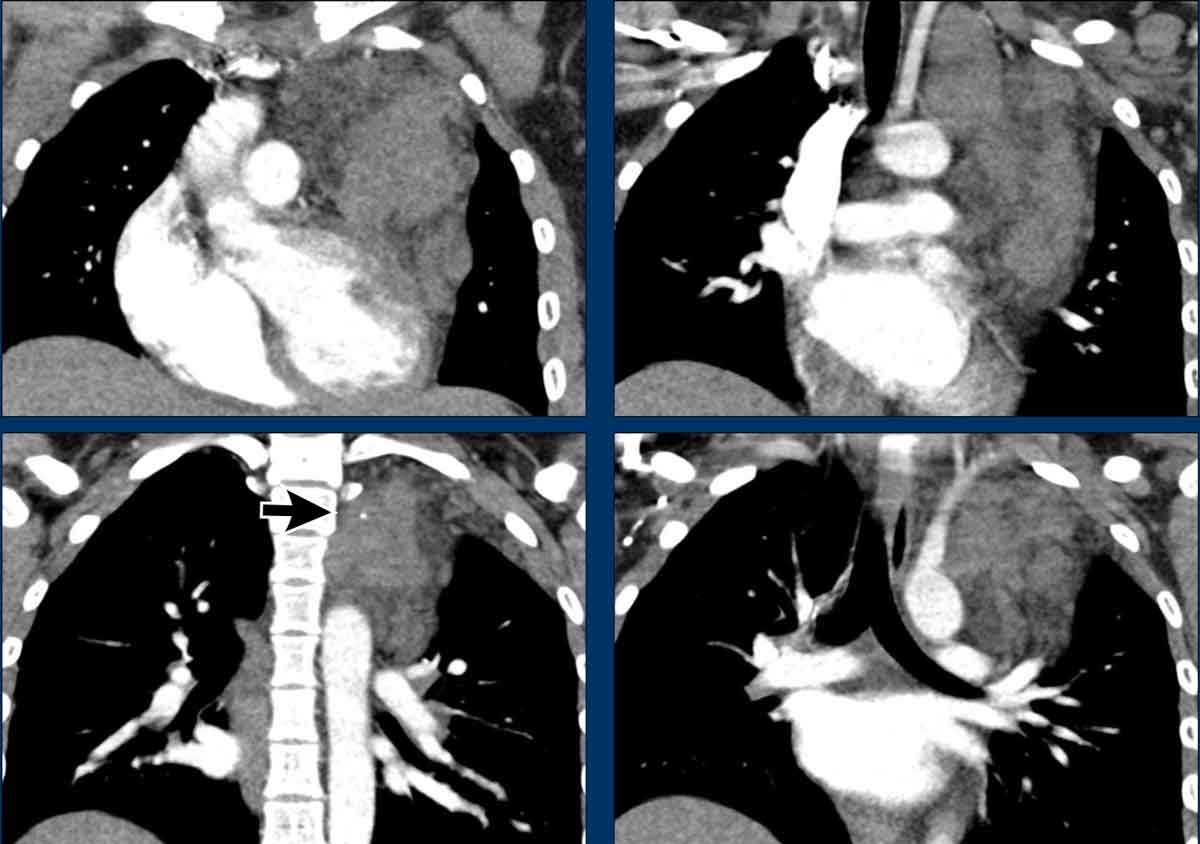
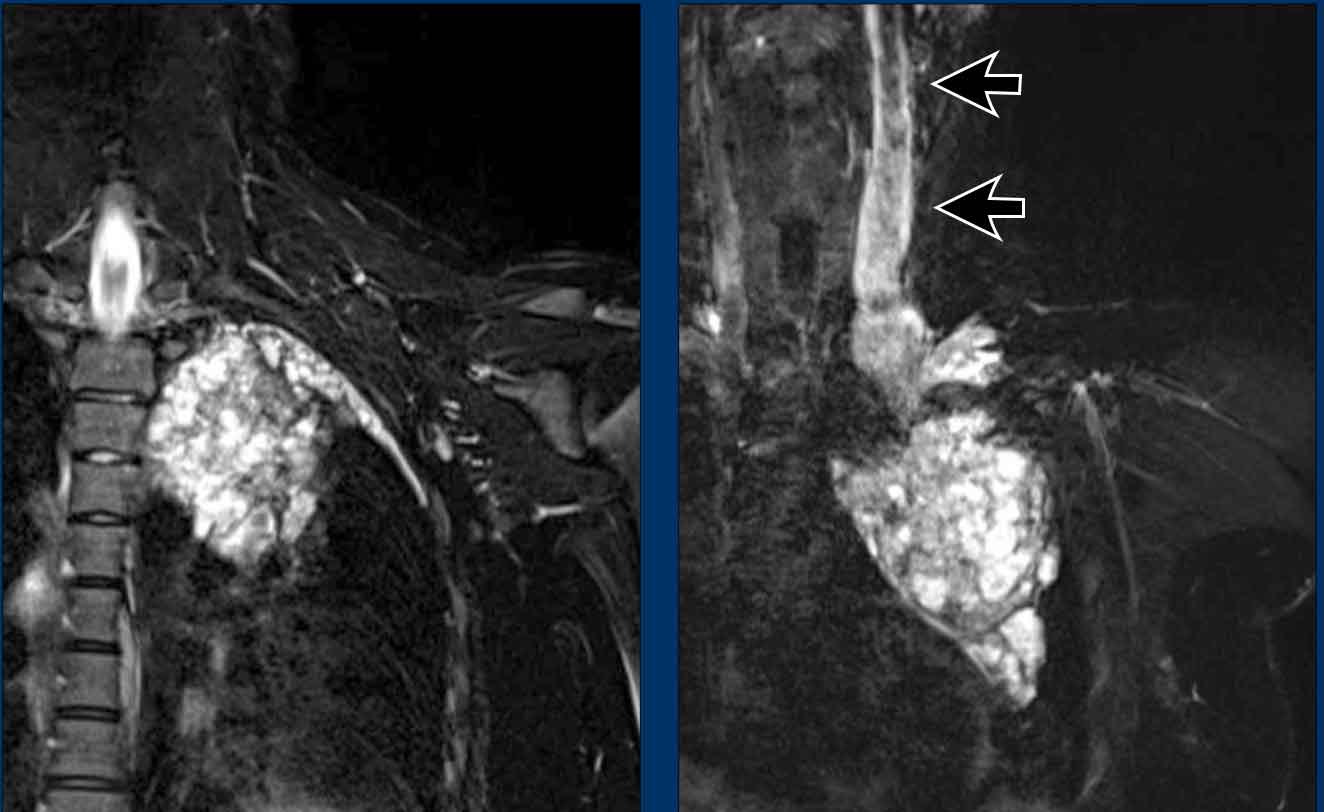
Neuroendocrine tumor of the thymus
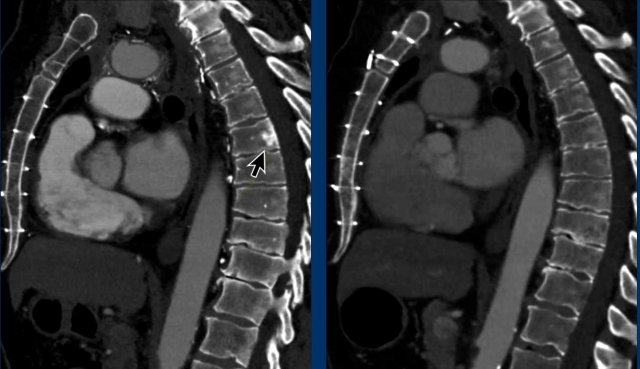
Case
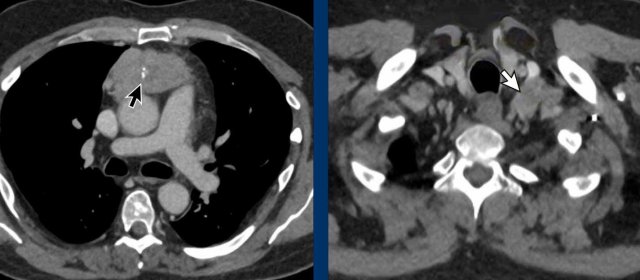
These images are of a 36 year-old male with Cushing syndrome, who had a resection of a pituitary adenoma.
The Cushing however persisted and a mediastinal mass was detected.
Images
Solid mass with central calcifications (black arrow).
Notice that the mass has an irregular margin on the left side.
The left supraclavicular lymph node is enlarged (Virchow's node: white arrow).
This is not a regular PET-CT but a Dotatoc PET, which is used to detect neuro-endocrine tumors and their metastases.
There are several bone metastases (arrows).
Final diagnosis
Neuroendocrine tumor of the thymus (NETT)
Neuroendocrine tumors of the thymus are rare neoplasms.
They are very aggressive and often present with invasion of the surrounding mediastinal structures and are associated with endocrinopaties like Cushing’s syndrome, acromegaly and MEN-1 syndrome.
Thymolipoma
Images
There is a large mass in the prevascular space of the mediastinum containing mainly fat and some vessels (arrows).
Discussion
In such a case it is not possible to differentiate between a thymolipoma and a liposarcoma.
The tumor was resected and turned out to be a thymolipoma.
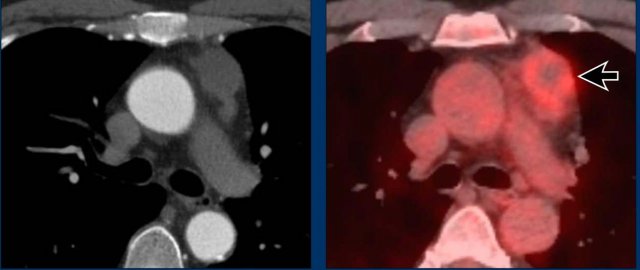
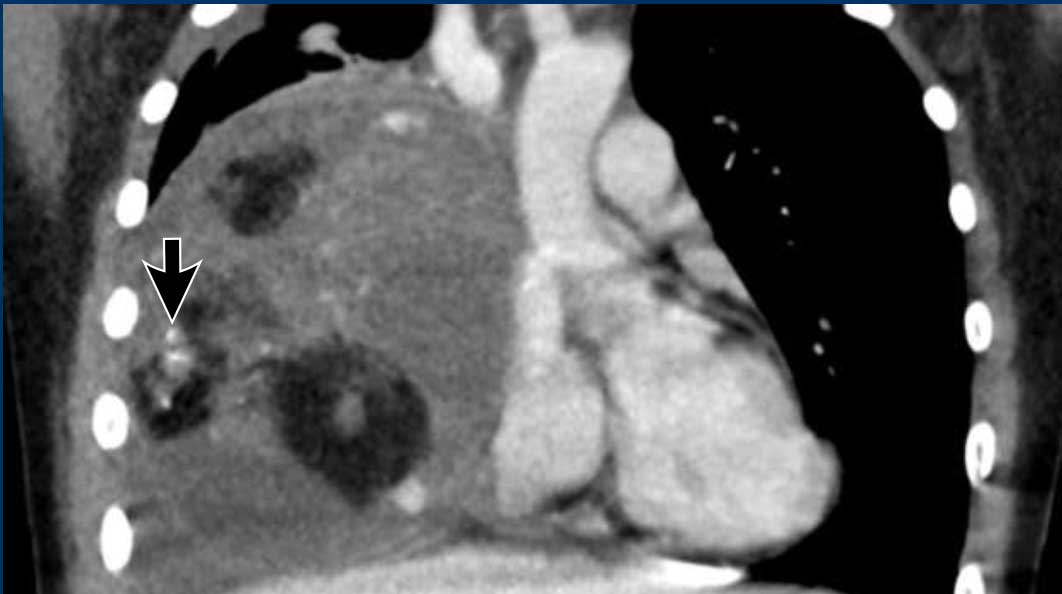
Lymphoma
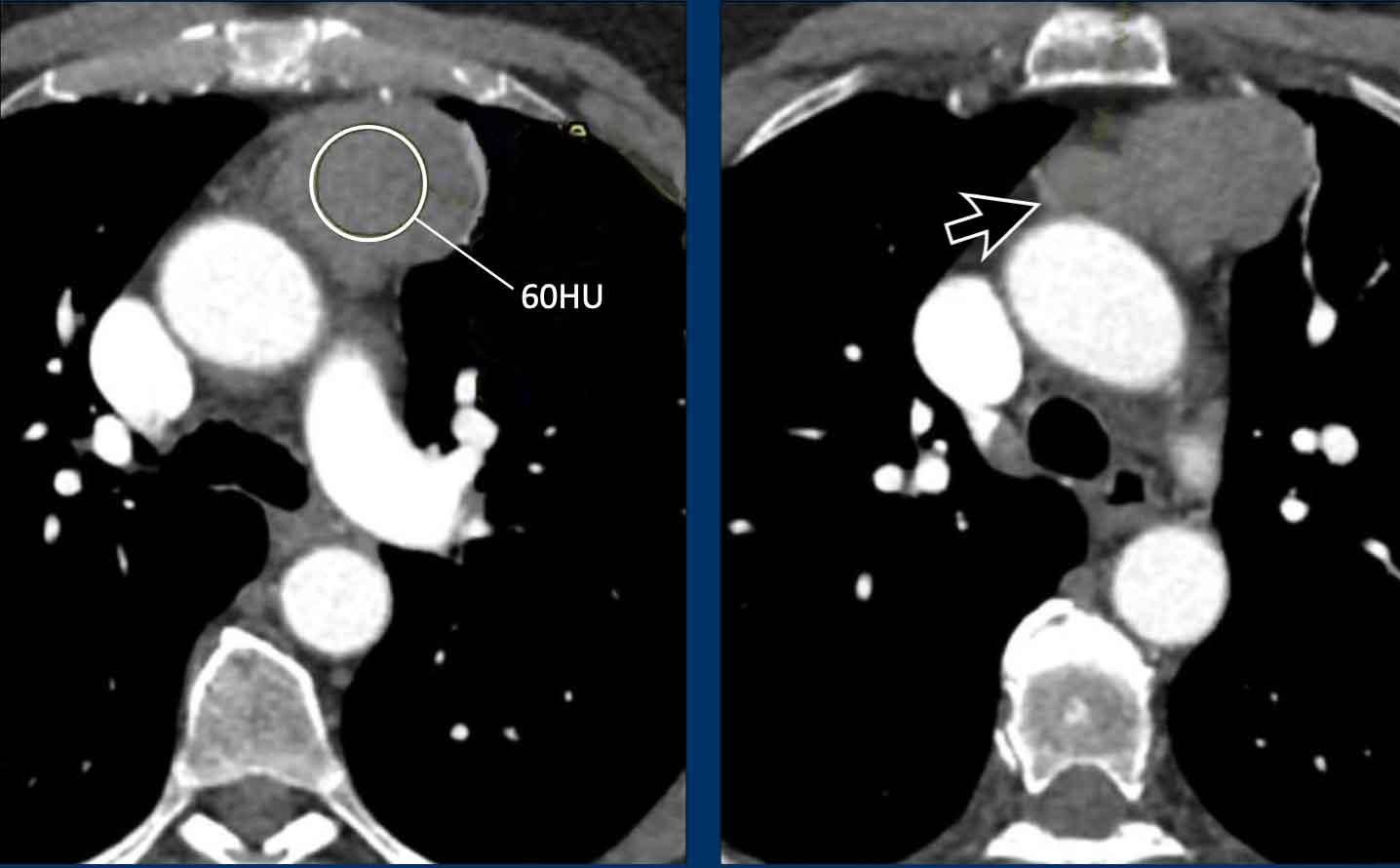
These images are of a 60-year old female.
She had cardiac arythmias and on a chest CT an incidental mass was seen.
First study the images.
Question: what is the most likely diagnosis?
Images
The mass has a high density on the post contrast scan.
There is no macroscopic fat.
The border is somewhat irregular.
And there is a second mass (arrow). On other levels more masses were seen.
Discussion
When there are multiple masses the most likely diagnosis is a lymphoma.
Whenever lymphoma is in your differential diagnosis, you need tissue sampling and you want to start chemotherapy as soon as you know what kind of lymphoma it is.
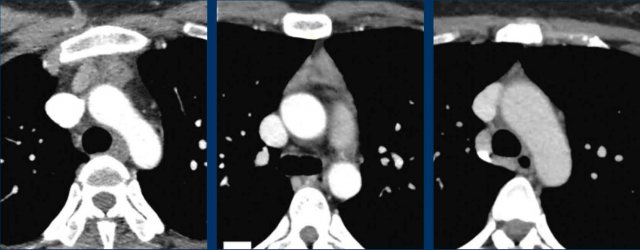
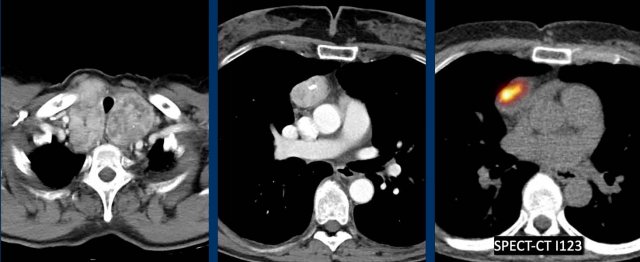
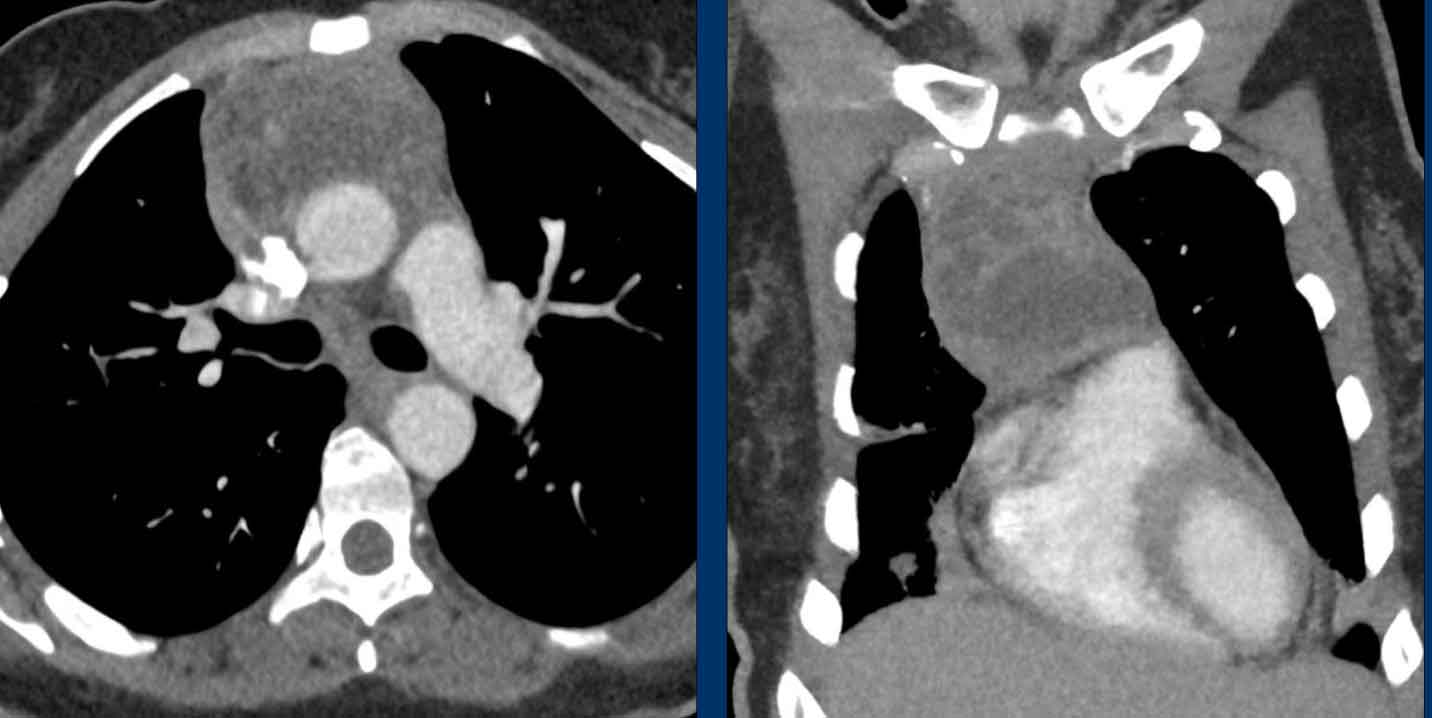
Ectopic thyroid
These images are of a 37-year old female.
She had a pneumonia and did not recover well and a CT was performed.
First study the images.
Question: what is the most likely diagnosis?
Images
There is a strong enhancing mass in the prevascular space.
Notice that it looks the same as the enhancing mass in the thyroid region.
Ectopic thyroid just looks like a goiter.
Sometimes there is a connection with the normal thyroid gland and sometimes the normal thyroid gland is absent.
You can proof the diagnosis with thyroid scintigraphy.
Here a companion case.
There is a thyroid goiter and an enhancing mass in the prevascular space of the mediastinum.
I-123 is a radioisotope of iodine used for a thyroid uptake scan.
In this case the uptake is seen on a SPECT-CT.
Hematoma
These images are of a 68-year-old male, who recently had a coronary bypass surgery.
He complained of dyspnoe.
There was a high D-dimer level and a CT was performed to look for pulmonary emboli.
Images
There is a mass in the prevascular mediastinum.
The density was 44HU both on the NECT aswell as on the CECT.
However we need to realize, that this scan is performed to detect pulmonary emboli and is in an early phase.
So we are not sure if there would be any enhancement in a later phase.
Discussion
Because of the recent surgery (notice the clips) it was concluded, that this most likely was a hematoma.
On a follow up scan the hematoma had resolved.
Venous malformation
These images are of a 15-year-old female with a mediastinal mass.
The question was if this was a lymphoma.
Images
There is a large inhomogeneous mass with soft tissue density and fat density.
There is also a small calcification (arrow).
Continue with the MRI...
Images
On the T2W images with fatsat the lesion is lobulated and notice the wide efferent vein with a flow void.
The calcification on the CT must be a phlebolith.
Final diagnosis
Venous malformation.
Mixed masses

Teratoma
These images are of a 19-year-old female with chest pain.
Scroll through the images.
What is your opinion?
Then continue with the next image.
Image
There is a large mediastinal mass which contains cystic and solid parts and also fat and calcifications (arrow).
This is a classical teratoma.

These images are of a 35-year-old female who complains of coughing and chest pain for about a week.
Scroll through the images.
What is your opinion.
Is this a cystic thymoma, a teratoma, a lymphoma or a thymolipoma?
Continue with the next images.....
This case illustrates, that sometimes you have to study all the images in order to find the fat (black arrow) and the calcifications (white arrow) in a teratoma.
These images are of a 36-year-old male who presented with a large mediastinal mass.
Scroll through the images.
What is your opinion.
Images
The large mass compresses the trachea, which is narrowed.
The mass shows enhancement of the wall and areas within the mass.
Discussion
Based on the imaging findings the differential diagnosis was:
- Anaplastic thyroidcarcinoma
- Thymuscarcinoma
- Teratoma
Although a biopsy was suggested, the next step should be to determine tumor markers AFP and bHCG.
The AFP was very high (12000) and the final diagnosis of a teratoma was made and the patient could start with chemotherapy the same day with good results.
Mediastinal Abscess
These images are of a 34 year old female with a recurrence of acute myeloid leukemia.
Now she is coughing with fever and the CRP is 365.
First look at the images.
What is your opinion.
Is this a cystic thymoma, teratoma, lymphoma or abscess?
Images
On CT the lesion shows enhancement of a surrounding wall and of septa within the lesion.
Because of the lab findings the most likely diagnosis was an abscess.
She was succesfully treated with antibiotics.
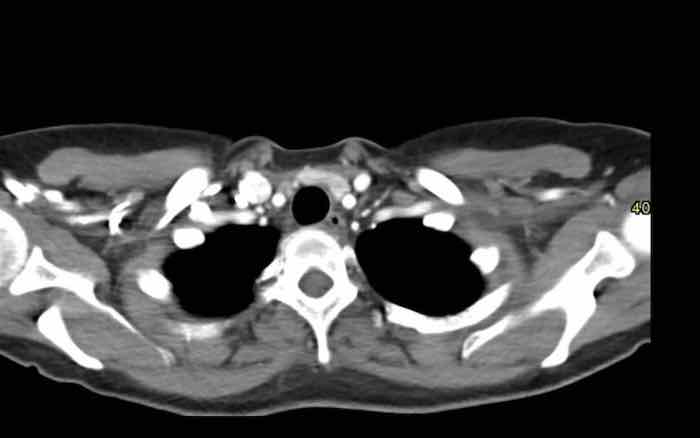
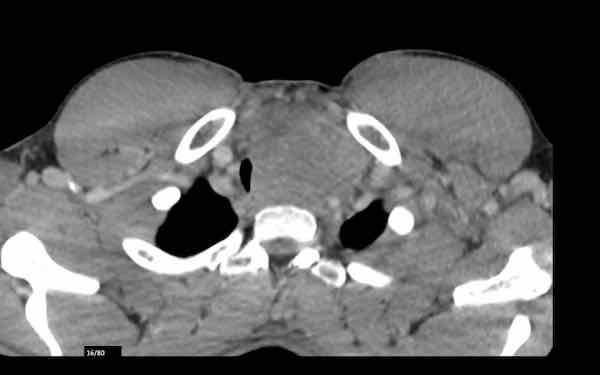
These images are of a 28-year-old female.
A mediastinal mass was seen on CT to look for pulmonary emboli.
Images
There is a mass in the prevascular space.
There are some calcifications.
Continue with the MR-images...
Images
The MRI better demonstrates that this a mixed lesion with cystic parts (T2W) and solid enhancing parts.
No signal drop on the out-of-phase T1W image.
Final diagnosis
This turned out to be a cystic thymoma.
Although most thymomas present as oval shaped solid enhancing masses, some may contain cystic parts and calcifications.
This can make it very difficult to differentiate them from teratomas.
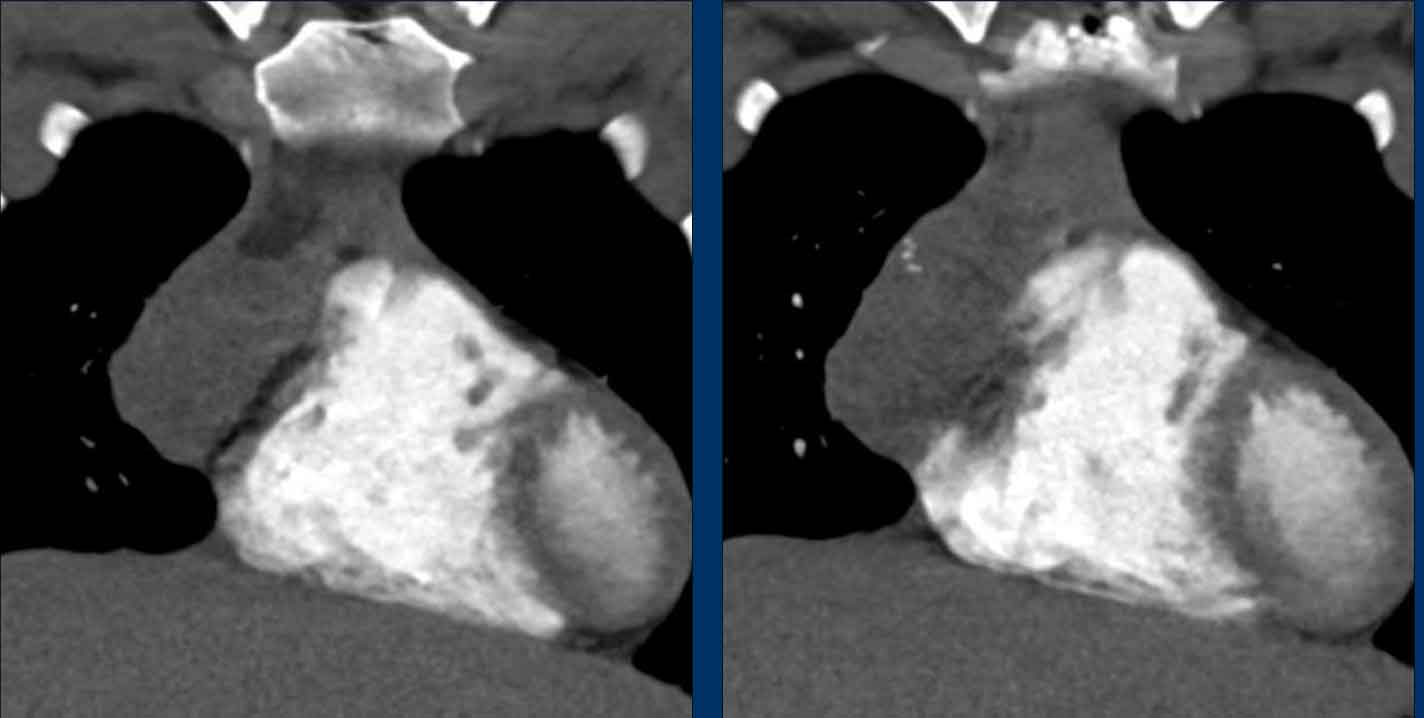
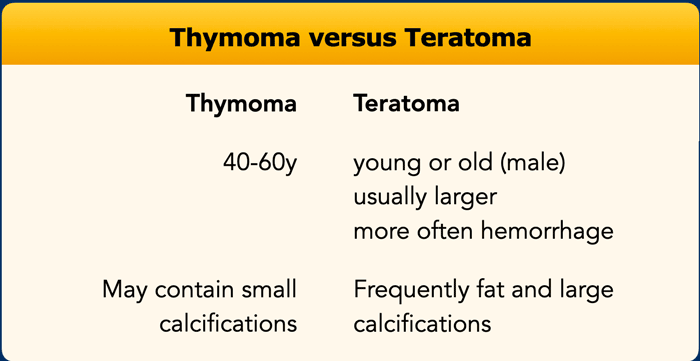
Thymoma versus Teratoma
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.