Shoulder Rotator cuff injury
Robin Smithuis, Frank Smithuis and Henk-Jan van der Woude
Alrijne hospital in Leiderdorp, Amsterdam University Medical Centre and the Onze Lieve Vrouwe Gasthuis in Amsterdam, the Netherlands
Publicationdate
The rotator cuff plays an important role in the stabilization of the glenohumeral joint during movements of the arm.
Rotator cuff tears are the most common cause of shoulder pain and result in loss of strength and loss of stability of the shoulder.
In this article we will discuss:
- The role of MRI in detection of full thickness tears.
- MR arthrography for depiction of partial thickness tears and co-existing intra-articular pathology.
- MRI as preoperative imaging tool to assess quality of soft tissue structures involved in cuff pathology.
- Depiction of anatomical variations of osseous outlet in patients with impingement symptoms.
Anatomy
Rotator cuff
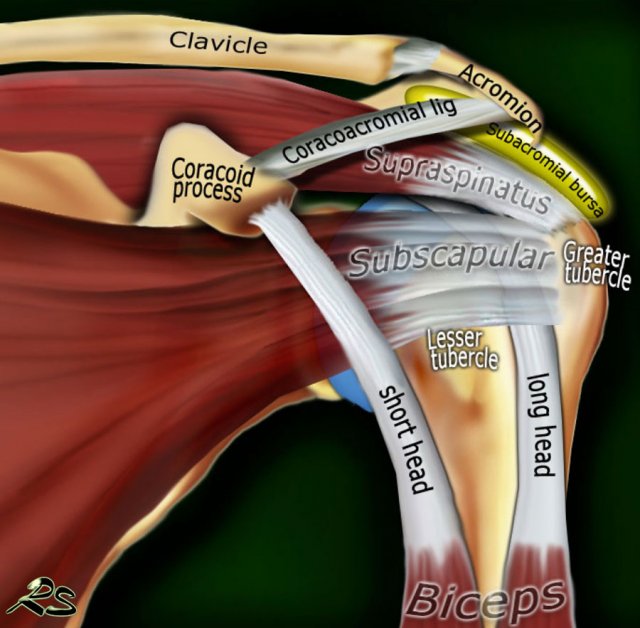
The rotator cuff is composed of the tendons of the subscapularis, supraspinatus, infraspinatus and teres minor, that attach to the proximal humerus.
The main function of the rotator cuff is to stabilize and center the humeral head in the glenoid cavity during movements of the arm by compressing the humeral head against the glenoid.
The rotator cuff – as the name suggests – also plays a major role in the internal and external rotation of the arm.
Subscapularis
The subscapularis is located anterior to the scapula with insertion of the tendon on the lesser tuberosity.
The subscapularis muscle is a powerful internal rotator which also supports the arm during abduction and adduction. Dislocation of the long head of the biceps will result in rupture of part of the subscapularis tendon.
Supraspinatus
The supraspinatus muscle is located in the suprascapular fossa with insertion of the tendon on the greater tuberosity. The supraspinatus muscle initiates the abduction of the arm, which is continued by the deltoid muscle, which is the great abductor and extensor of the arm.
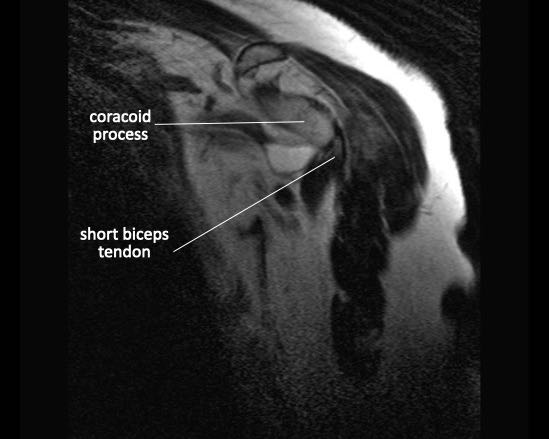
Long head of the biceps
The long head of biceps tendon is anatomically and functionally related to the rotator cuff. The tendon arises from the supraglenoid tubercle and its proximal segment is intra-articular. It exits the gleno-humeral joint and passes through the rotator interval between the subscapularis and supraspinatus tendons into the bicipital groove of the proximal humerus
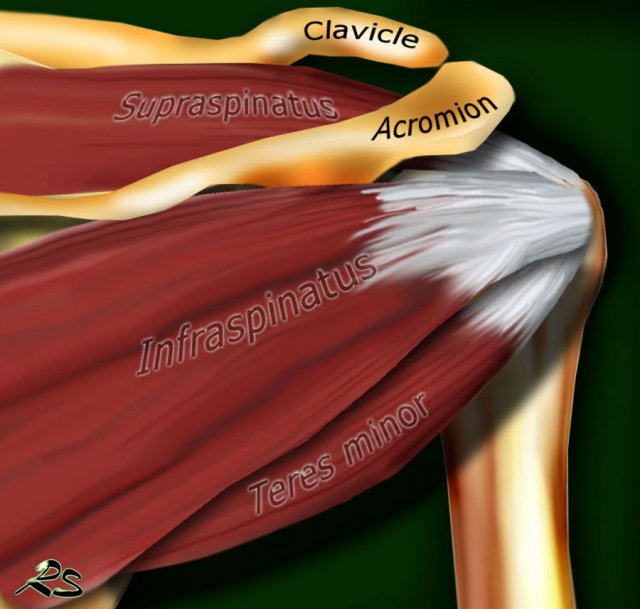
Infraspinatus
The infraspinatus muscle is located posterior to the scapula, inferior to the scapular spine. The tendon of the Infraspinatus muscle attaches on the posterior aspect of the greater tuberosity.
The infraspinatus muscle is a strong external rotator and additionally assists in both abduction and adduction.
Teres minor
The teres minor muscle is located inferior to the infraspinatus muscle.
The tendon attaches on the greater tuberosity.
The teres minor muscle’s function consists primarily of external rotation and adduction of the arm.
Other structures that stabilize the glenohumeral joint are the joint capsule, labrum and glenohumeral ligaments.
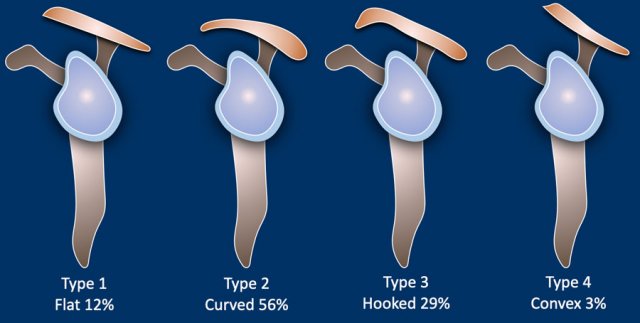
Acromion types
Four types of acromial arch are described.
In the Bigliami classification type 1-3 were described. later a fourth convex type was added.
Type 2 with the curved shape is the most common type.
Type 3 with a hooked shape is the only type that is associated with an increased incidence of shoulder impingement.
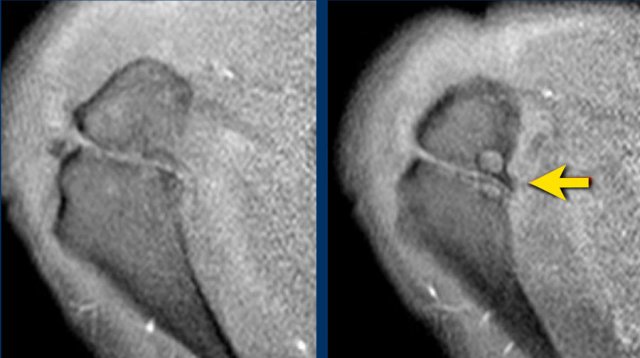
Os Acromiale
Failure of one of the acromial ossification centers to fuse will result in an os acromiale.
It is present in 5% of the population.
Usually it is an incidental finding and regarded as a normal variant.
An os acromiale may cause symptoms due to arthrosis in the acromio-acromion articulation or due to impingement because if the os acromiale is unstable, it may be pulled inferiorly during abduction by the deltoid, which attaches here.
On MR an os acromiale is best seen on superior axial images.
An os acromiale must be mentioned in the report, because in patients who are considered for subacromial decompression, the removal of the acromion distal to the synchondrosis may further destabilize the synchondrosis and allow for even greater mobility of the os acromiale after surgery and worsening of the impingement (4).
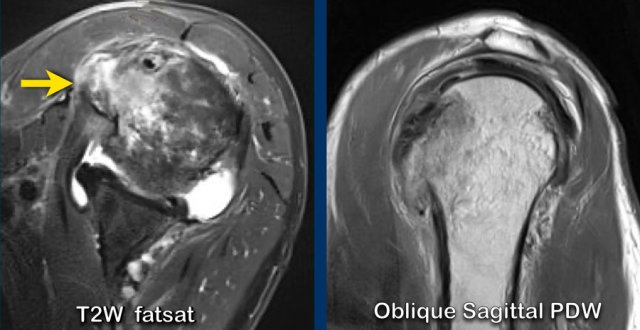
The axial MR-images show an os acromiale with degenerative changes, i.e. subchondral cysts and osteophytes (arrow).
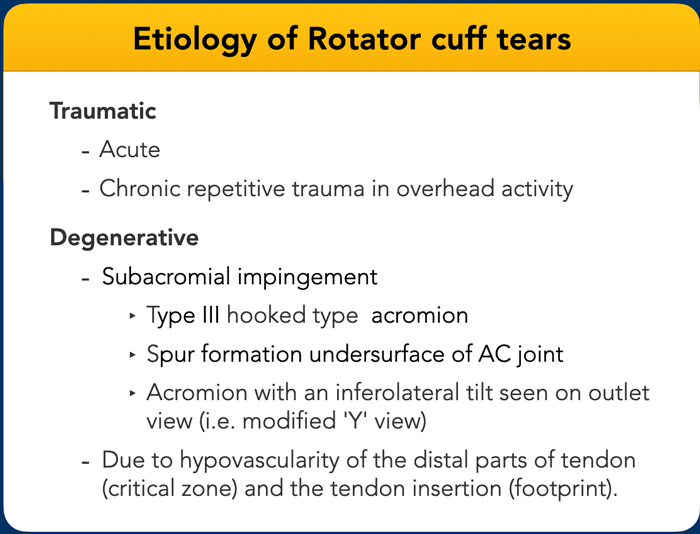
Etiology of rotator cuff tears
The etiology of rotator cuff tears can be traumatic, like in a direct trauma to the subscapular muscle and tendon or a more chronic tear of the supraspinatous tendon due to repetitive trauma in overhead sports-activity.
This is usually seen in younger people.
In older people the cause of rotator cuff tears is degenerative as seen in subacromial impingement or due to hypovascularity in specific parts of the tendons.
Partial thickness tears
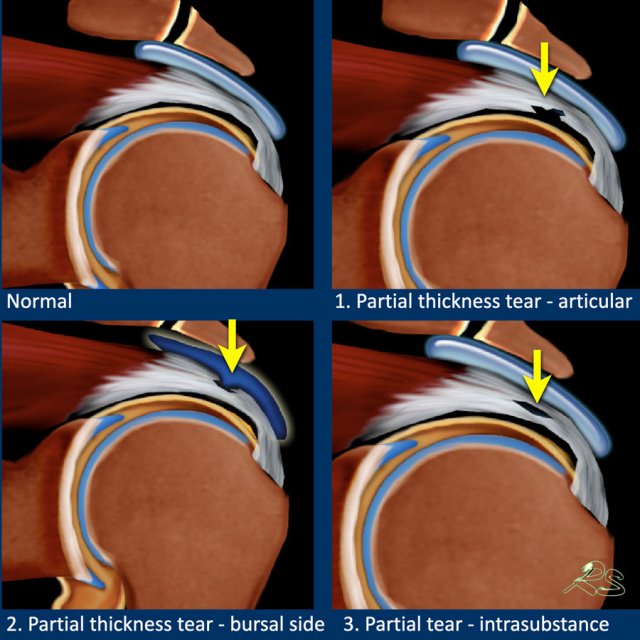
Partial thickness tears are rotator cuff tears that do not have a full transmural extension from the articular side to the bursal side.
Partial thickness tears can be divided into:
- Articular-sided tears
located at the undersurface of the tendon and connected to the glenohumeral joint. - Bursal-sided tears
located at the bursal surface and connected to the subdeltoid bursa. - Intrasubstance tears
located within the tendon without a comminucation to the joint or bursa.
Articular-sided partial tears are more common than bursal-sided, because the eccentric forces are more intense on articular side and the fibers on the articular side are weaker and healing is reduced.
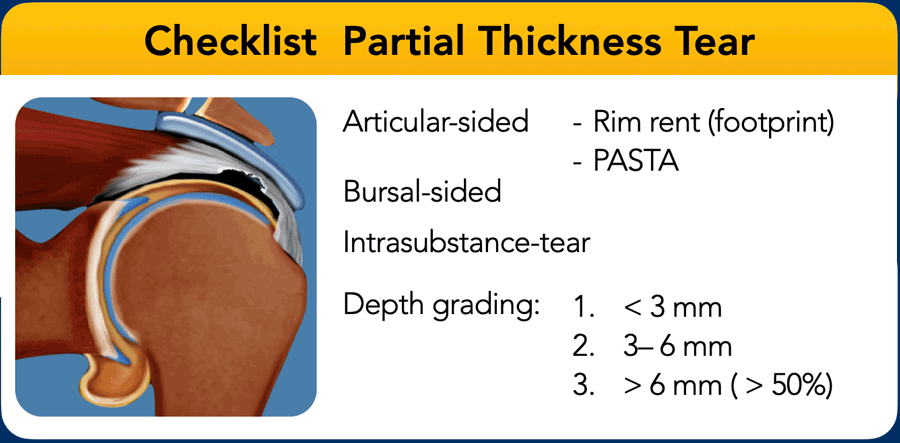
Partial thickness tears are best visualized on coronal PD and T2WI with and without fat suppression.
MR arthrography is very sensitive for detection of even small PTT, but only on the articular surface.
The ABER position allows assessment of both the vertical and interstitial component.
Report on the extent of tendon involvement : more or less than 50% of the tendon thickness.
Partial thickness tears may progress to full thickness tears.
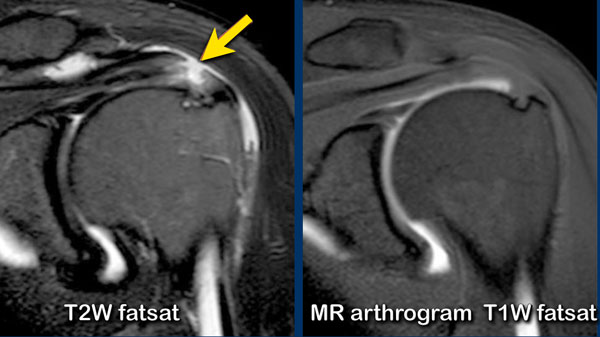
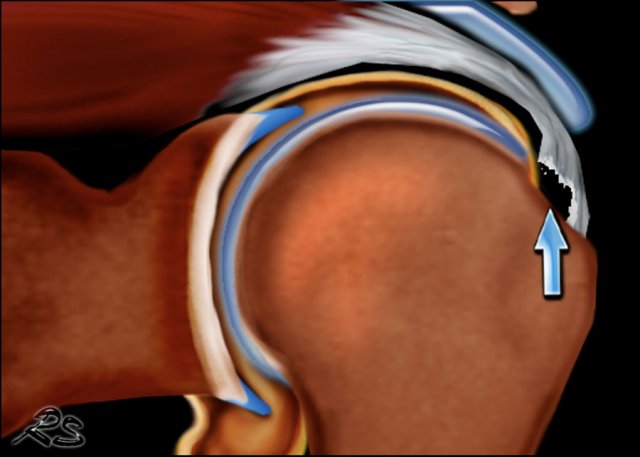
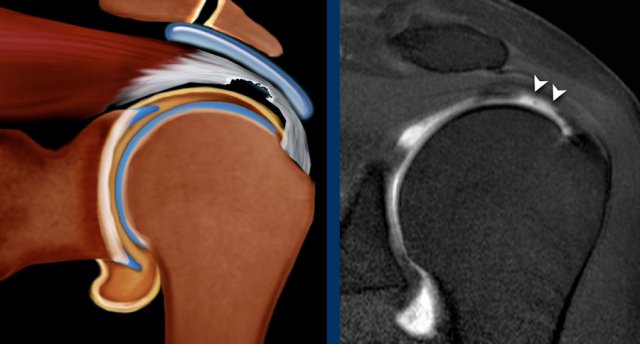
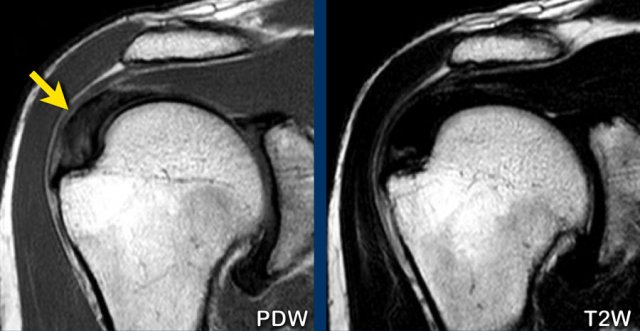
Bursal-sided tears cannot be detected on a MR arthogram, because the intra-aticular contrast cannot fill the defect (figure).
On MR partial thickness tears have a signal intensity equal to water on T2WI in the focal defect.
The most frequent locations are:
- Supraspinatus: anterior half of < 1 cm from insertion.
- Supraspinatus: articular undersurface tear at the site of the tendon attachment to the greater tuberosity, also called rim-rent tear or partial articular surface tendon avulsion (PASTA lesion).
- Postero-superior part of the supraspinatus in combination with the antero-inferior part of the infraspinatus tendon.
Images
On the T2W-image there is a large bursal-sided tear.
Notice that on the MR-arthrogram the tear is not visible, as the intra-articular contrast cannot reach the defect in the tendon.
Rim-rent tear
Rim-rent tears are a common type of partial-thickness rotator cuff tears.
They are commonly overlooked on MRI, possibly because of failure to appreciate the high incidence of these types of tears and failure to inspect the anterior-most fibers of the rotator cuff [ref].
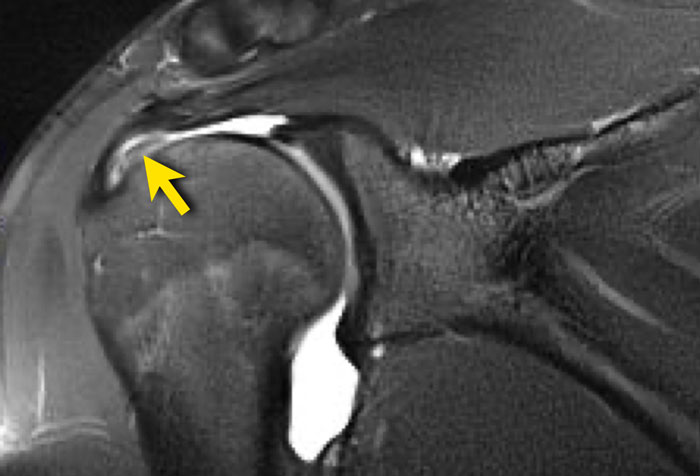
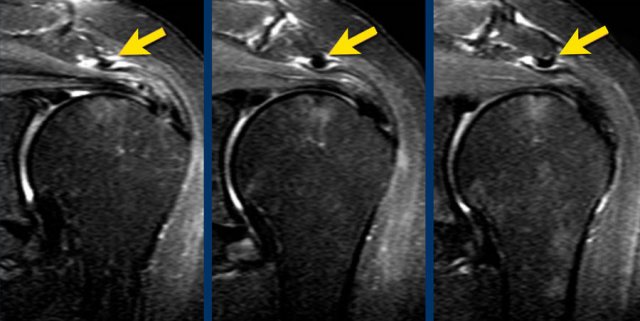
The image is a coronal T1-weighted fat-suppressed MR arthrogram.
It shows a partial articular-sided tear of the distal supraspinatus tendon or rim-rent tear, also called PASTA lesion - partial articular supraspinatus tendon avulsion.
Here a PASTA lesion in another patient.
Images
Illustration and coronal T1 fat-suppressed MR arthrogram.
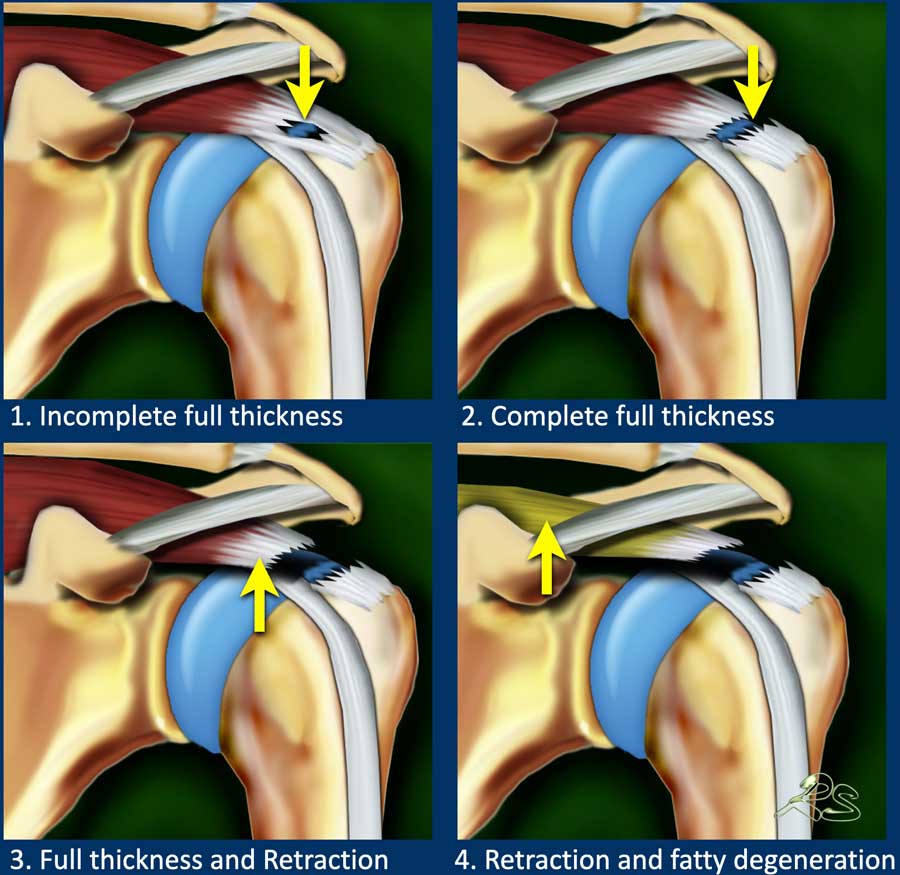
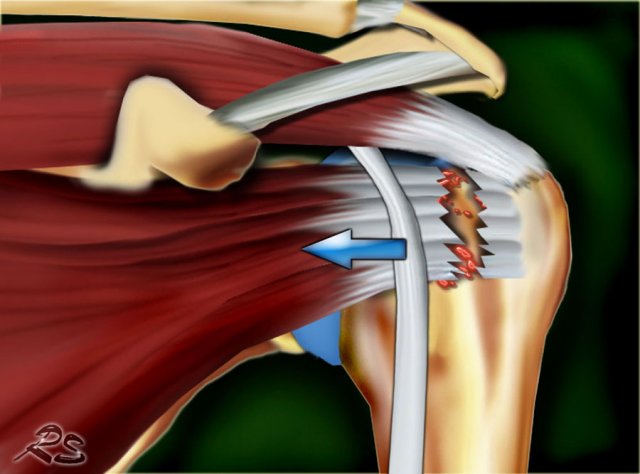
Full Thickness tears
Full thickness tears (FTT) extend from the bursal surface all the way to the articular surface.
Full thickness tears can be divided into:
- Incomplete FTT
There is a full thickness tear but only part of the tendonwidth is involved. - Complete FTT
A full thickness tear is complete when the whole tendon is ruptured. - Complete FTT+ retraction
The FTT is complicated by retraction of the muscle. - Complete FTT+ retraction+ atrophy
The FTT is complicated by retraction of the muscle, atrophy and fatty infiltration resulting in a poor prognostic outcome.
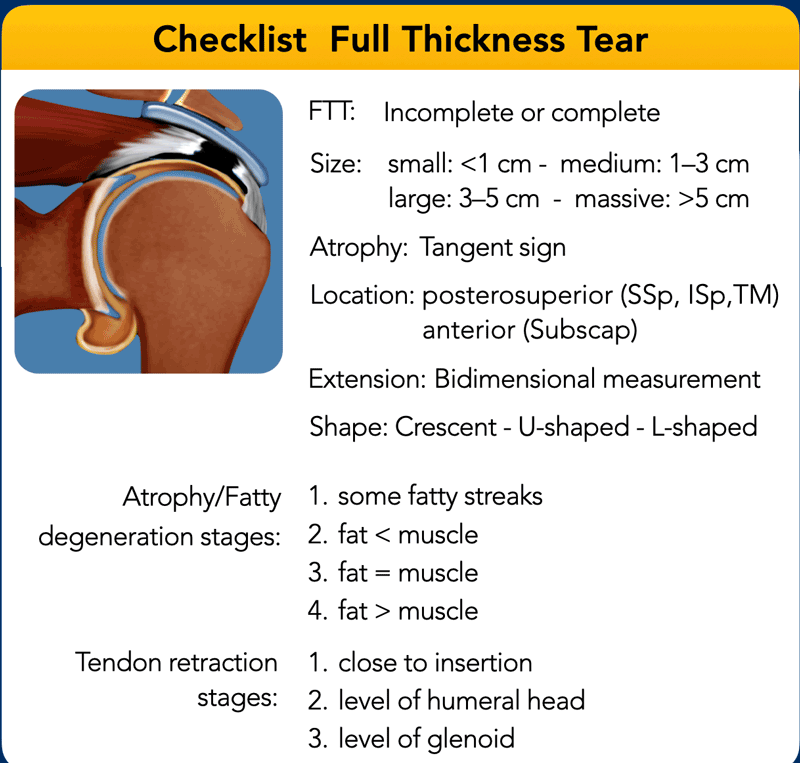
The table shows the checklist for full thickness tears.
Incomplete full thickness tears
The hall mark on MRI of an incomplete full thickness tear is a gap filled with fluid on T2WI.
However sometimes the gap within the tendon can be filled with debris or granulation tissue and the signal will not equal water.
Images
There is an incomplete small full thickness tear of the distal supraspinatus tendon with no retraction.
There is some cyst formation in the humeral head at the insertion site with some bursal reaction and intratendinous signal increase due to tendinosis.
Scroll through the images.
What are the findings?
There is a full thickness tear of the anterior part of the supraspinatus tendon going from the articular side to the bursal side.
Since the posterior fibers of the supraspinatus tendon are intact, this is called an incomplete full thickness tear of the supraspinatus tendon.
There is no retraction.
Complete full thickness tears
Click on image to enlarge and then scroll through the images.
There is a full thickness tear of the supraspinatous tendon with some retraction and muscle artophy.
Notice the fatty streaks in the teres minor, supra- and infraspinatus muscle.
The most common location of full thickness tears are:
- Supraspinatus
Distal anterior part of the supraspinatus is the most common tear.
Sometimes with extension posteriorly to the infraspinatus or extension anteriorly to the rotator cuff interval capsule, biceps tendon and subscapularis. - Infraspinatus
Isolated infraspinatus tears are uncommon, but sometimes seen in athletes. - Subscapularis
Isolated subscapularis tears are uncommon, but sometimes seen after an acute abduction and exorotation trauma. Frequently combined with injury or dislocation of the biceps tendon. - Teres minor
Teres minor tears are rare, but can be seen after posterior dislocation with posterior capsule injury.
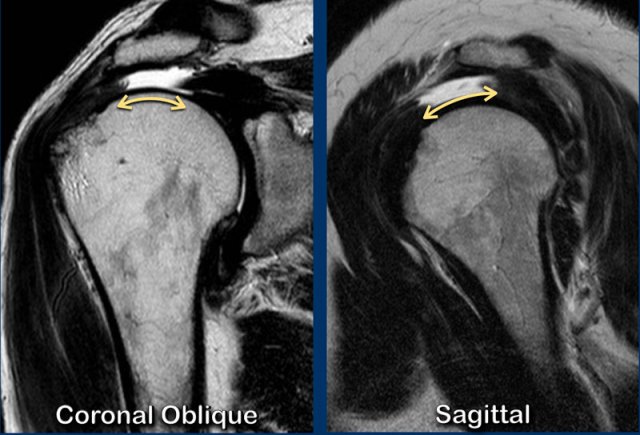
Measurement of the extention of a full thickness rotator cuff tear in two directions.
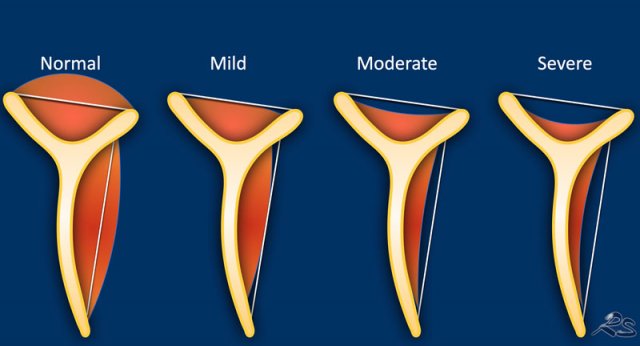
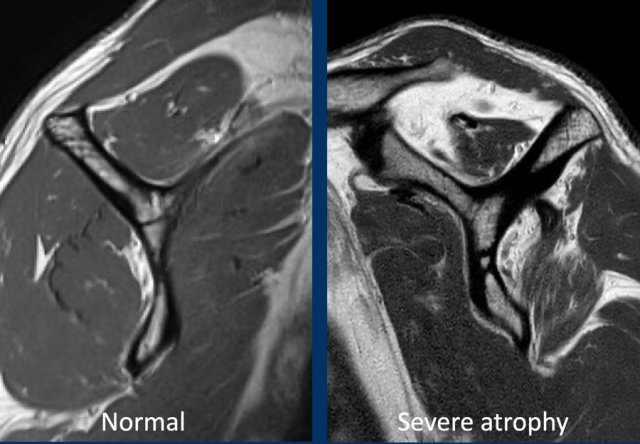
Muscle atrophy - Tangent sign
Measurement of muscle atrophy by Warner is based on the oblique sagittal plane image medial to the coracoid process.
A line is drawn from the edge of the coracoid to the inferior scapular tip and from the scapular spine to the coracoid process.
If the muscle is convex above the line, there is no atrophy.
If the muscle is just below this line, moderate atrophy is present.
If there is barely any muscle visible, there is severe atrophy.
The left image shows a normal muscle anatomy on a sagittal image.
The image on the right is of a patient with a full thickness tear of both the supra- and infraspinatus tendon with retraction.
There is fatty atrophy of the supra- and infraspinatus muscle.
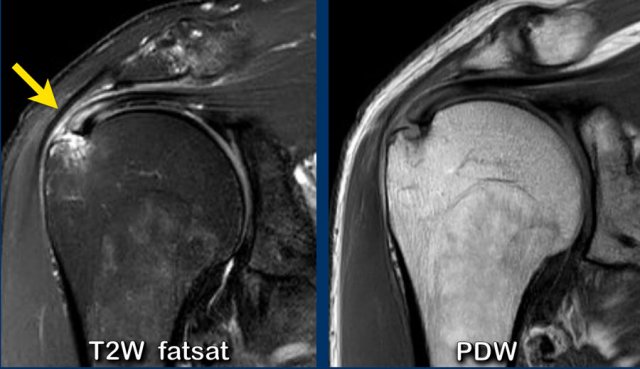
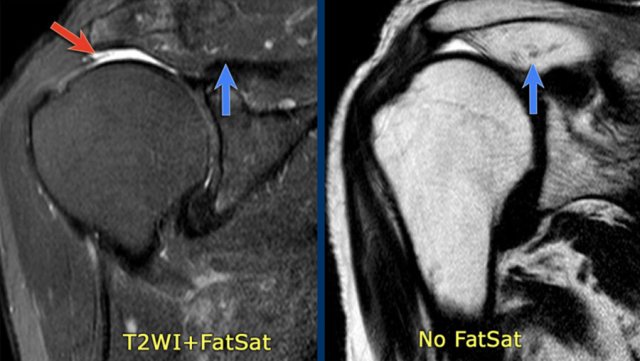
On fat suppressed images it can be difficult to appreciate the muscle atrophy and fat replacement.
Images
On the fat suppressed image on the left you might think that the supraspinatus muscle is normal (blue arrow).
However on the image without fat suppression you can appreciate the extreme muscle atrophy and fatty replacement with high signal (blue arrow).
The red arrow indicates the full thickness tear of the supraspinatous tendon.
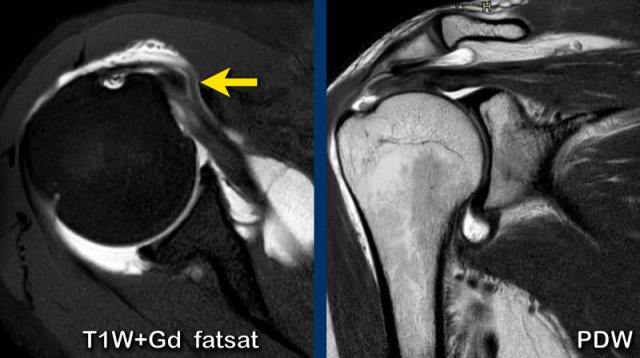
Sometimes it can be difficult to differentiate a partial tear from a full thickness tear.
When you look at the first image, it looks like an articular-sided partial thickness tear.
However there is irregular extension of contrast on subsequential MR arthrogram slices from the articular side on the left to the bursal side on the right indicating a full thickness tear.
Biceps tendon
The long head of the biceps tendon inserts at the superior glenoid tubercle. Then it runs through the glenohumeral joint and the rotator interval to exit the joint anteriorly within the intertubercular sulcus.
The biceps tendon contributes in prevention of superior migration of the humeral head.
Biceps tendon injuries are:
- tendinopathy
- partial thickness tear
- complete disruption
- dislocation extra-articular (figure)
 Dislocation of long head biceps tendon with a partial thickness tear of the subscapularis tendon and a full thickness tear of the supraspinatus tendon
Dislocation of long head biceps tendon with a partial thickness tear of the subscapularis tendon and a full thickness tear of the supraspinatus tendon
Dislocation of long head biceps tendon
Disruption of the transverse humeral ligament may lead to medial dislocation of the biceps tendon.
The biceps tendon may shift in or beneath the subscapularis tendon with subscapularis tendon disruption.
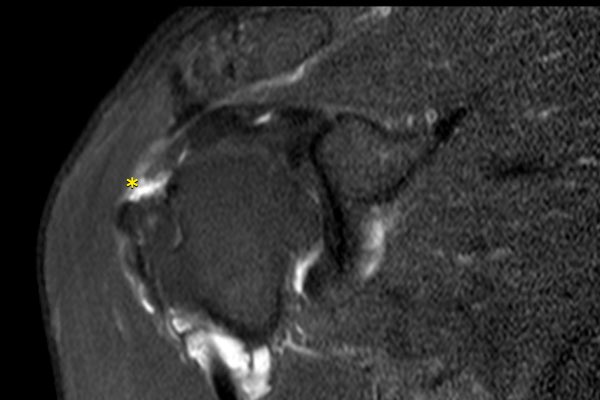
Images
MR arthrography with axial T1-weighted fat-suppressed and coronal PD images.
There is medial dislocation of the biceps tendon within the subscapularis tendon (arrow).
There is a partial thickness tear of the subscapularis tendon.
On the PDW-image there is a fluid filled gap at the distal insertion of the supraspinatus tendon and contrast extending into the subacromial-subdeltoid space indicating a full thickness tear of the supraspinatus tendon.
Subscapularis tendon
Subscapularis tears are seen after direct trauma, forced abduction and exorotation or with recurrent anterior shoulder dislocation
Images
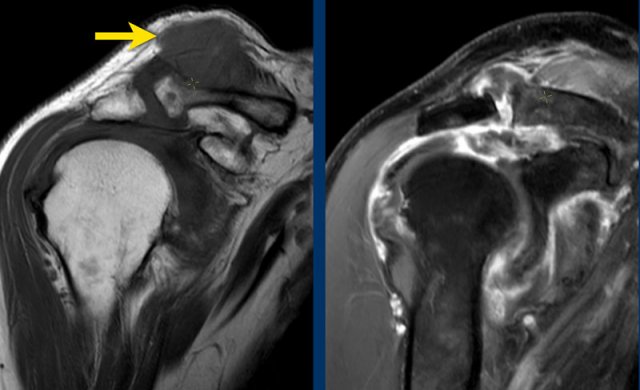
Subscapularis tear after direct trauma.
There is retraction of the subscapularis tendon anteriorly with peritendinous edema on axial PD-weighted and coronal T2-weighted fat-suppressed images (asterix).
The biceps tendon is not dislocated (arrowhead).
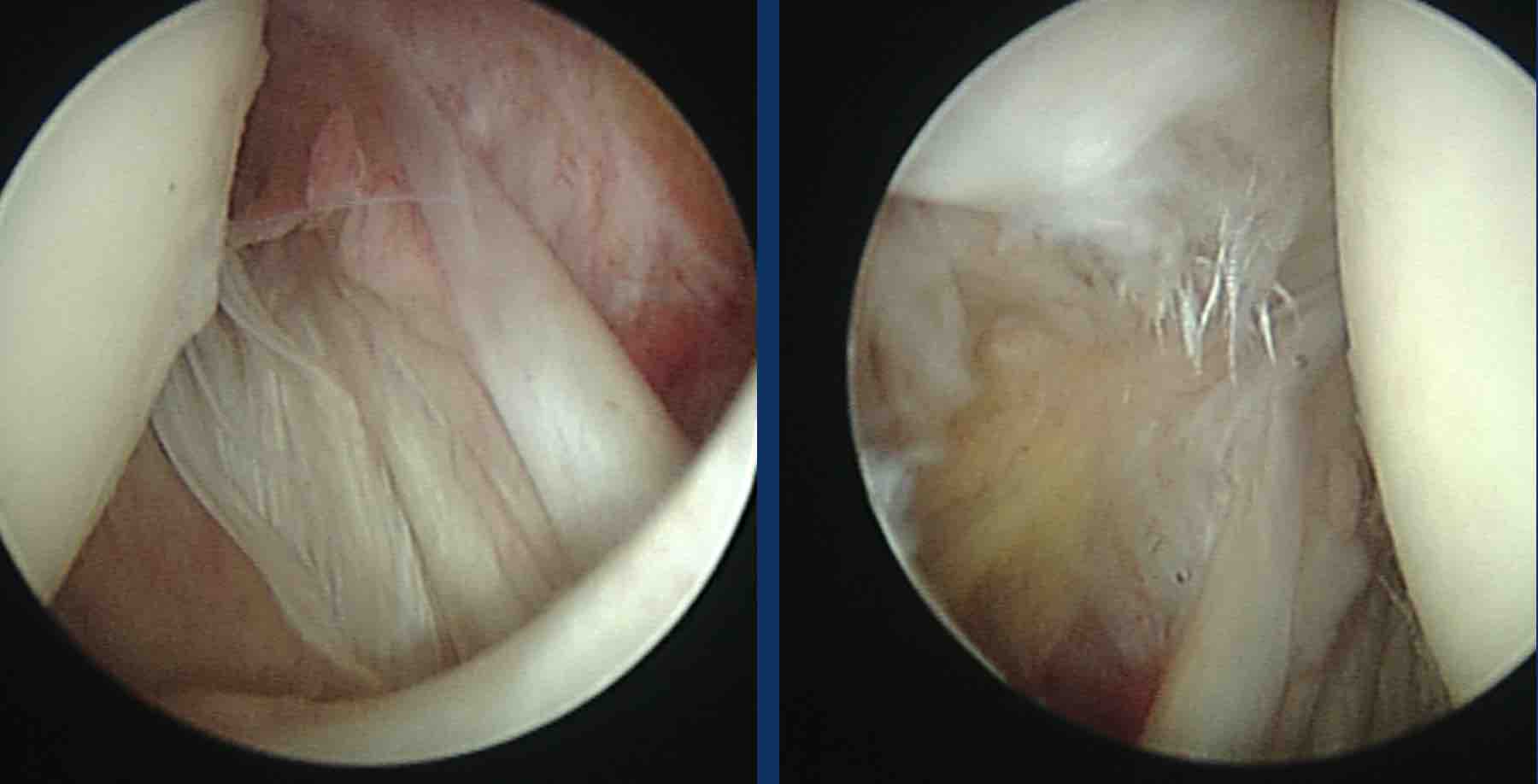
This patient had a direct anterior shoulder trauma.
Images
Axial T2-weighted fat suppressed and oblique sagittal PD image.
There is an incomplete rupture of the subscapularis tendon combined with edema due to fracture of the lesser tubercle.
Shoulder impingement
When you raise your arm to shoulder height, the space between the acromion and rotator cuff narrows.
The acromion can rub against or "impinge" on the tendon and the bursa, causing irritation and pain.
Impingement and damage to the rotator cuff tendons are the most common shoulder problems that occur in the narrow subacromial space and these two problems can exist separately or together.
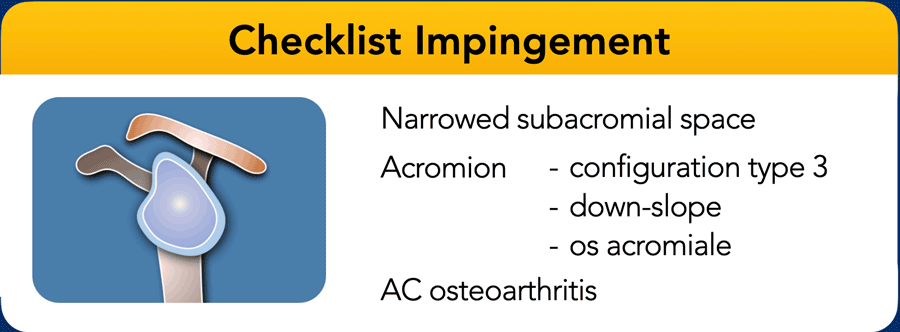
In any shoulder examination we should look for signs of impingement like a narrowed subacromial space, abnormal shape of the aromion or osteoarthrosis.
Types of impingement
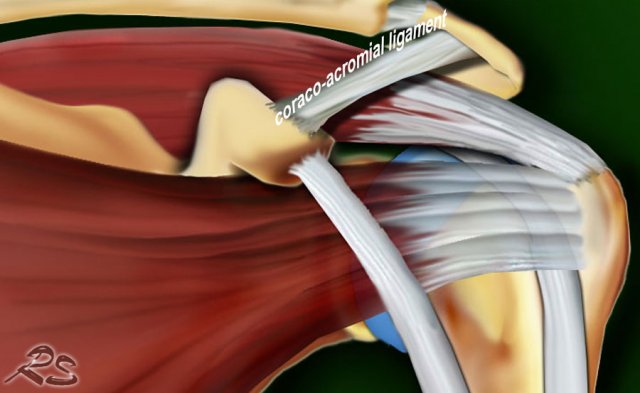
- Primary extrinsic impingement
Impingement of cuff tendons and subacromial bursa due to shape of acromion, down-sloping, presence of bony spurs acromion and osteoartritis AC-joint, os acromiale or thickening of coraco-acromial ligament (normal: 2-3 mm).
- Secondary impingement from instability
Most common cause of impingement in athletes. - Internal (posterosuperior) impingement
Frequently in overhead throwing athletes in extreme abduction and exorotation. Degeneration and partial cuff tears of posterior SSp and Isp, combined with posterosuperior labral fraying, edema posterior greater tuberosity and cartilage lesion
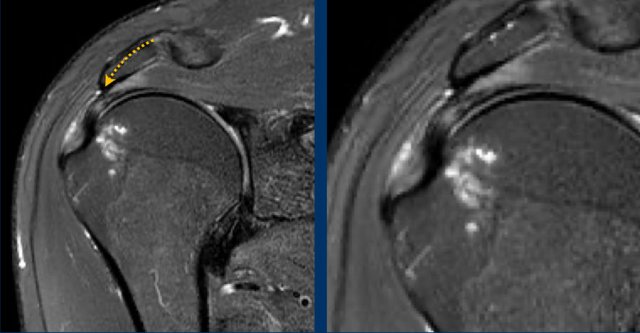
Images
Primary extrinsic impingement due to dowsloping of the acromion with tendinosis of the supraspinatus tendon
Thickening or calcification of the coracoacromial ligament can also cause impingement.
In this patient the coracoacromial ligament is thickened and compresses the supraspinatus tendon.
Tendinosis
Rotator cuff tendinosis is degeneration of the tendon. It is also called tendinitis or tendinopathy.
Common MRI-findings are:
- Mild to moderate thickening of the tendon
- In more severe cases myxoid changes and edema with swelling
- There is increased signal intensity, but it does not equal the signal intensity of water.
- Frequently seen in the supraspinatus tendon near the humeral attachment
- Pitfall: magic angle in morphologically normal tendon
Images
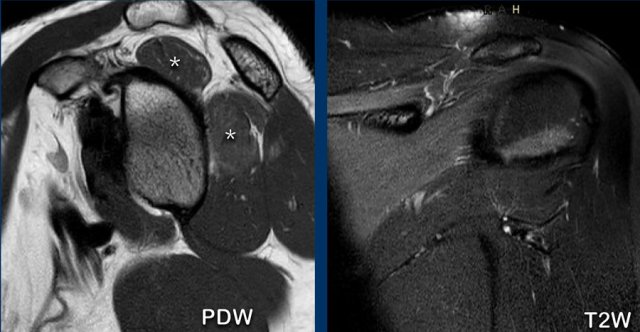
Tendinosis with thickening of the supraspinatus tendon.
ONly on PDW-images you will see increased signal.
Calcifying tendinosis
This is a painful shoulder condition characterized by calcium deposits in the rotator cuff.
In most cases there is spontaneous resolution, but in some cases the pain and dysfunction persist.
This is more often seen in women age 30-50y.
Ultrasound
US will show the presence, location and size of the calcium deposits and can help in guidance for therapeutic needling and lavage.
In the resting phase the deposits appear hyperechoic and arc shaped.
In the resolving phase the deposits are non-arc shaped, fragmented, cystic and nodular.
In the reabsorption phase increased Doppler vascularity can be seen.
MRI
Usually the MRI shows low signal intensity on all sequences, but sometimes there is high signal on T2W-images representing edema in the resorptive phase.
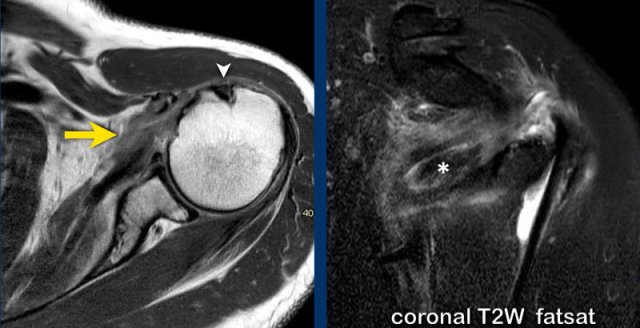
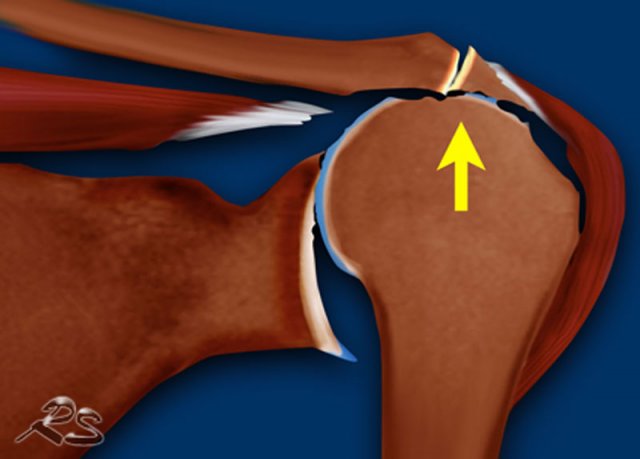
Rotator cuff arthropathy
Rotator cuff arthropathy is a pattern of joint degeneration due to loss of stabilizing function by the rotator cuff.
The rotator cuff provides a net inferiorly directed force, balaced by a superiorly directed force by the deltoid muscle.
In rotator cuff arthropathy the following findings can be seen:
- Massive rotator cuff tear
- Glenoid erosion, cartilage loss, cysts and osteophyte formation, collaps of humeral head
- Superior migration of humeral head with femoralization of humeral head and acetabularization of the coraco-acromial arch
Signs of irrepairability and indication for reverse total shoulder arthroplasty are:
- static superior migration
- narrowed or absent acromiohumeral interval
- fatty infiltration > 50% of RC muscles
Hamada classification for rotator cuff arthropathy:
- Acromio humeral distance > 6 mm
- Acromio humeral distance < 5 mm
- Acromio humeral distance < 5 mm and acetabularization of the coracoacromial arch
- Narrowing of glenohumeral joint
- 4a without acetabularization
- 4b with acetabularization - Humeral head necrosis present sometimes with humeral head collaps
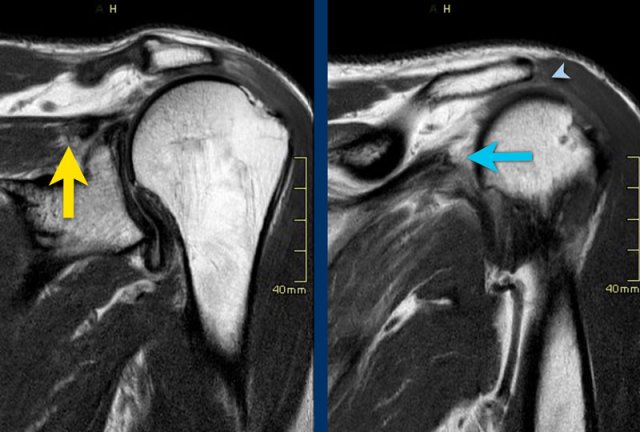
case 1
The images show a narrowed subacromial space (arrowhead) secondary to a rotator cuff tear with retraction of both the supraspinatus tendon (yellow arrow) and of the infraspinatus tendon (blue arrow).
case 2
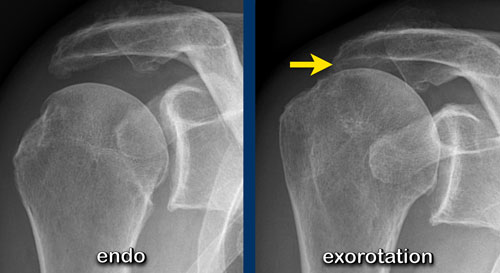
This patient has a narrowed subacromial space.
Notice that the narrowing is well seen on the image with the shoulder in exorotation position, while it is not seen on the endorotation view.
case 3
These images show an acromioclavicular cyst, also referred to as Geyser sign, which is secondary to rotator cuff pathology.
The fluid extends superiorly into and outside a degenerated AC joint with disruption of inferior AC joint capsule.
Parsonage Turner syndrome
Parsonage–Turner syndrome is a neuritis involving the brachial plexus.
It is also referred to as idiopathic brachial plexopathy or neuralgic amyotrophy.
It is characterized by sudden, excruciating pain in the shoulder, followed by severe weakness.
Parsonage–Turner syndrome is a rare disorder that generally involves one upper limb, mostly the axillary nerve, the upper trunk of the brachial plexus, the suprascapular nerve, and the long thoracic nerve are affected.
It may present with symptoms of an isolated peripheral nerve lesion, although the pathology is thought to lie more proximally.
Images
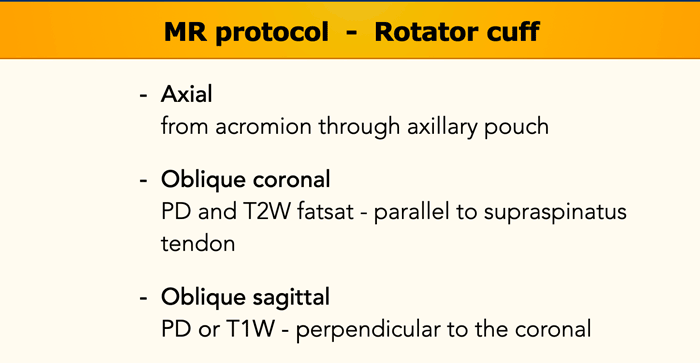
Oblique sagittal PD image and coronal T2 fat-suppressed image.
Slightly increased signal of SSp and Isp when compared to the subscapularis and teres minor and mild atrophy, consistent with Parsonage Turner syndrome.