Acute Scrotum in Children
Gael J. Lonergan
Chief of Radiology of the Children's Hospital of Austin, Washington, DC
Publicationdate
This article is based on a presentation given by Gael Lonergan at the 'Teaching in Holland' course and adapted for the Radiology Assistant by Robin Smithuis.
In this overview we will discuss the following subjects:
- Torsion of testis and appendage
- Infection: epididymitis, epididymoorchitis, orchitis
- Trauma
- Hernia
- Idiopathic scrotal edema
by Gael J. Lonergan
Testicular torsion
Torsion occurs when an abnormally mobile testis twists on the spermatic cord, obstructing its blood supply.
Patients present with acute onset of severe testicular pain.
The ischemia can lead to testicular necrosis if not corrected within 5-6 hours of the onset of pain.
Torsion can be intermittent and can undergo spontaneous detorsion.
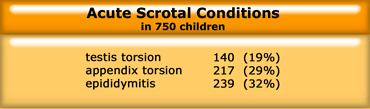
In a child with an acute scrotum, testicular torsion is not the most common condition (Table).
Torsion of testicular appendices represents the more common cause of scrotal pain.
Typically, it has a more gradual onset than testicular torsion and patients may endure pain for several days before seeking medical attention.
Testicular appendage torsion appears as a lesion of low echogenicity with a central hypoechogenic area adjacent to the epididymis.
Most of the time however, we don't see it and we do the US just to exclude a testicular torsion.
We should see torsion of testicular appendices more as a diagnosis of exclusion.
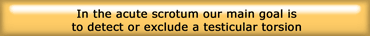
So although torsion of the testicular appendix and epididymitis are more common, our goal is mainly to detect or exclude a testicular torsion.
We want to be able to tell the surgeon whether or not it is a surgical emergency.
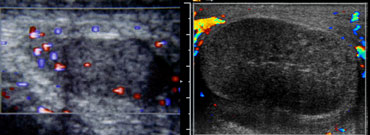
 Testicular torsion: Optimal setting for color on normal side, followed by examination of symptomatic side.
Testicular torsion: Optimal setting for color on normal side, followed by examination of symptomatic side.
Color doppler
Complete absence of intratesticular blood flow and normal extratesticular blood flow on color Doppler images is diagnostic, if the flow is normal in the contralateral testis. Yet, the presence of flow within the testis does not exclude the presence of torsion, because incomplete vascular obstruction can sometimes occur or intermittent torsion.
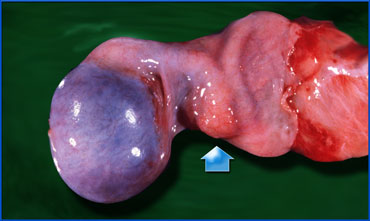
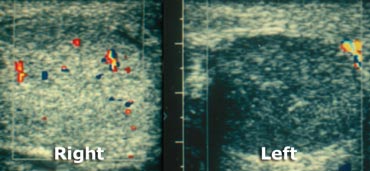
The case on the left shows a testicular torsion of the left testis.
This case is very obvious because there is no flow on the affected side, but also a difference in echogenicity.
With prolonged torsion, the testis is typically hypoechoic and inhomogeneous and is often accompanied by a surrounding hydrocele.
By the time these sonographic findings occur, surgical salvage of the testicle is unlikely.
Use at least a 10 MHz linear transducer.
Always start with the examination of the normal side and optimize the settings for low flow, low resistance and low velocity.
The background 'noise' should just be visible in the asymptomatic testis.
Once you have a good image of the normal side, don't touch any of the settings' and go to the symptomatic side.
In the very young child it can be difficult to examine the testes because they are very small and mobile.
The prepubertal testis has a volume of about 1-2 cc, while the postpubertal testis has about 30cc.
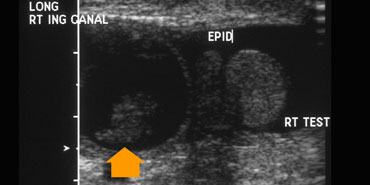
With age the testis increases in echogenicity, so in a very young child the small testis can be difficult to differentiate from the surrounding fat, especially if it is retracted into the inguinal canal (figure).
At the start of the examination you can put your finger on the inguinal canal, so that the testis can not move around.
Color Doppler imaging has limited sensitivity for detecting blood flow in pediatric patients with a testicular volume of less than 1cc.
On the left two more cases.
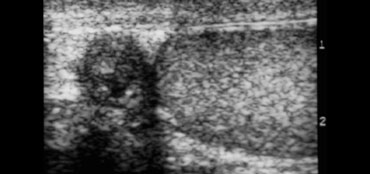
On the far left a child of 10 months old with torsio testis.
There is more flow in the tissues around the testis than in the testis itself and that is abnormal, unless the child has cellulitis.
The case next to it is an older child.
The gray scale ultrasound shows an abnormal testis.
So this could be torsio or orchitis, but the absent flow tells us, that this definitely is a torsio testis.
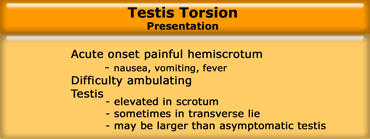
Presentation
The testis is usually elevated as a result of the torsion and the shortening of the cord itself and may be in a transverse lie.
The affected side can be larger from the swollen testis itself, a hydrocele or skin thickening.
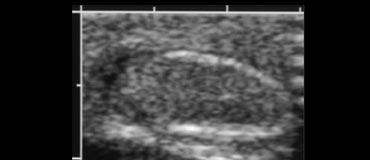
Gray scale Ultrasound
Gray scale ultrasound is helpfull, not in making the diagnosis, but in predicting the outcome.
For the first 4-6 hours there is a normal architecture.
During this period the testis is salvagable, so a normal appearance on gray scale means good outcome.
After this period the testis becomes heterogeneous and enlarged over the next 4-24 hours and the epididymis and scrotal wall may swell and become hypoechoic.
A worsening appearance of the testis on gray scale US correlates with decreased viability (1).
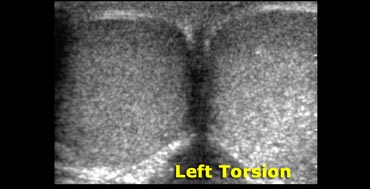
The way to look at differences in echogenicity, is to get a transverse image of both testes.
The images on the left show the affected side to be bigger and more echogenic.
This testis is probably not salvagable.
The testis may appear more echogenic or less echogenic, it doesn't matter, as long as there is a difference, there is a poor outcome.
Epididymitis
Epididymitis is the most common inflammatory process involving the scrotum and more common in adults.
Infections generally originate in the lower urinary tract from the bladder, urethra or prostate and are typically caused by urinary tract pathogens or sexually transmitted organisms (Chlamydia or gonorrrhhea) .
Epididymitis also occurs in children, but is then due to infection with Streptococcus or Staphylococcus.
In urinary tract abnormalities also infection with E.Coli is seen.
A sterile chemical epididymitis can result from reflux of sterile urine through the ejaculatory ducts, for instance if the ureter inserts in the prostatic urethra, this may lead to increased pressure in the vas deferens. .
On the left a child with a meningocele who had epididymitis.
Due to increased bladder pressure and contractions against a closed sphincter, there was reflux not only into the left ureter and porstate, but also into the epididymis, which resulted in epididymitis.
The case on the left shows the typical features of epididymitis.
The epididymis is swollen and heterogeneous.
There is a hydrocele and scrotal wall thickening.
With color doppler there is increased flow.
A normal epididymis has only limited colorflow.
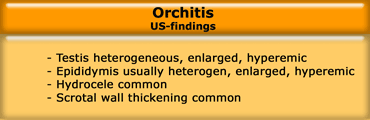
Orchitis
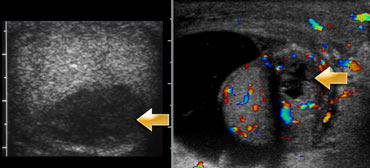
Orchitis is characterized by focal, peripheral, hypoechoic testicular lesions that are poorly defined, amorphous, or crescent-shaped.
Orchitis also exhibits testicular hyperemia on color Doppler sonography images and is usually accompanied by epididymal hyperemia due to concomitant epididymitis.
A reactive hydrocele is also frequently associated with epididymoorchitis.
Focal testicular infarction can occur as a complication of epididymitis when swelling of the epididymis is severe enough to constrict the testicular blood supply.
This appears as a hypoechoic intratesticular mass devoid of blood flow.
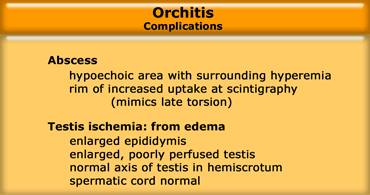
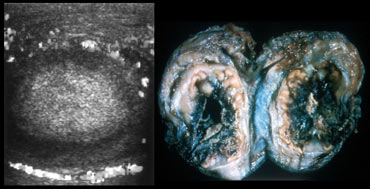
The complications of orchitis are abscess formation and ischemia.
The case on the left is a young patient, who came a week before with a hyperemic testis and epididymitis.
Due to ongoing infection, the pressure within the testis increased leading to infarction.
This is not due to torsion, but can be easily mistaken for torsion.
On the left two cases with abnormal areas within the testis probably due to absces formation.
Trauma
Hematocele
In trauma there is either a hematocele or testicular hematoma.
In the acute phase the hemorrhage is echogenic and in the chronic phase it is hypoechoic.
A hematocele results from scrotal or intra-abdominal hemorrhage.
It represents bleeding between the leaves of the tunica vaginalis and appears as a complex fluid collection.
With time, this collection can develop loculations, which appear as thick septations.
It is important to be able to tell if the testis is intact, because if there is a rupture, this can sometimes be treated surgically.
On the left a patient with a typical hematocele.
Testicular rupture
Testicular rupture is seen as focal alterations of testicular echogenicity correlating with areas of intratesticular hemorrhage or infarction in a patient with a hematocele.
A discrete fracture plane is identified in fewer than 20% of cases, although visible alterations in the testicular contour are a common finding.
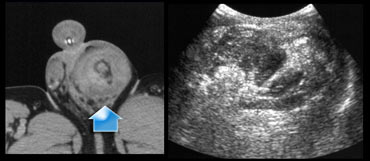
On the left a complicated case.
The ultrasound demonstrated a large hematocele.
There was doubt whether the echogenic structure indeed was a testis.
MR was performed and no testicular tissue was found, so we have to conclude that the echogenic structure is a result of fresh hematoma.
On the left another patient with a rupture, that was seen on the abdominal CT.
On US there was a large heterogeneous area with no identifiable testis due to rupture.
Hernia
 LEFT: herniated bowel in preterm.RIGHT: left-sided hernia in constipated child due to intermitted herniation of sigmoid.
LEFT: herniated bowel in preterm.RIGHT: left-sided hernia in constipated child due to intermitted herniation of sigmoid.
Hernias in children are common especially in premature infants.
Sometimes we can see them on plain films as we see in the case on the left.
If they are filled with bowel, they are easy to detect, but sometimes these hernias are only filled with soft tissue
The ultrasound examination starts with the child lying down and is then continued in the standing position.
The bowel or omentum is visible separate from the testis (figure).
The intestinal loop descends through the unclosed processus vaginalis.
An incarcerated hernia is a cause of acute scrotal pain.
Peristalsis suggests viability and absence of peristalsis is worrisome for incarceration.
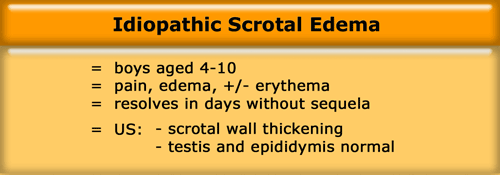
Idiopathic Scrotal Edema
Idiopathic scrotal edema is seen in school-aged boys.
They present with scrotal skin swelling.
So the clinical question is, if there is torsion or infection.
At examination the testes and epididymes are normal and all that we see on US is skin edema.
If this is all we see and the child does not have fever or elevated white count, which can be seen in cellulitis, than we can make the diagnosis of Idiopathic scrotal edema.
Although this is an idiopathic disease, so we don't know what it is, it is nevertheless important to make this diagnosis.
It is far more reasuring for parents to be told, that their child has a specific diagnosis, that it is benign and will go away with time.
That is better, than telling them, that you don't know what it is, but it is no torsion, so you don't really worry about it.