Ultrasound of the Neonatal spine
Erik Beek and Simone ter Horst and Robin Smithuis and Rutger Jan Nievelstein
Department of Radiology of the Wilhelmina Childrens Hospital, University Medical Center Utrecht and the Alrijne hospital in Leiderdorp, the Netherlands
Publicationdate
Ultrasound is the preferred modality in neonates with suspected occult spinal dysraphism (OSD).
OSD implies the presence of one or more spinal cord anomalies, which can cause tethering of the spinal cord and possible neurological and bladder or bowel function deficits.
Ultrasound is easy to perform, since the posterior arch of the vertebra is not yet ossified, providing a perfect acoustic window.
Especially the lumbosacral part of the spinal canal with the conus medullaris and the cauda equina can be beautifully depicted with a high resolution linear array probe.
Classification of Spinal dysraphism
Spina bifida aperta
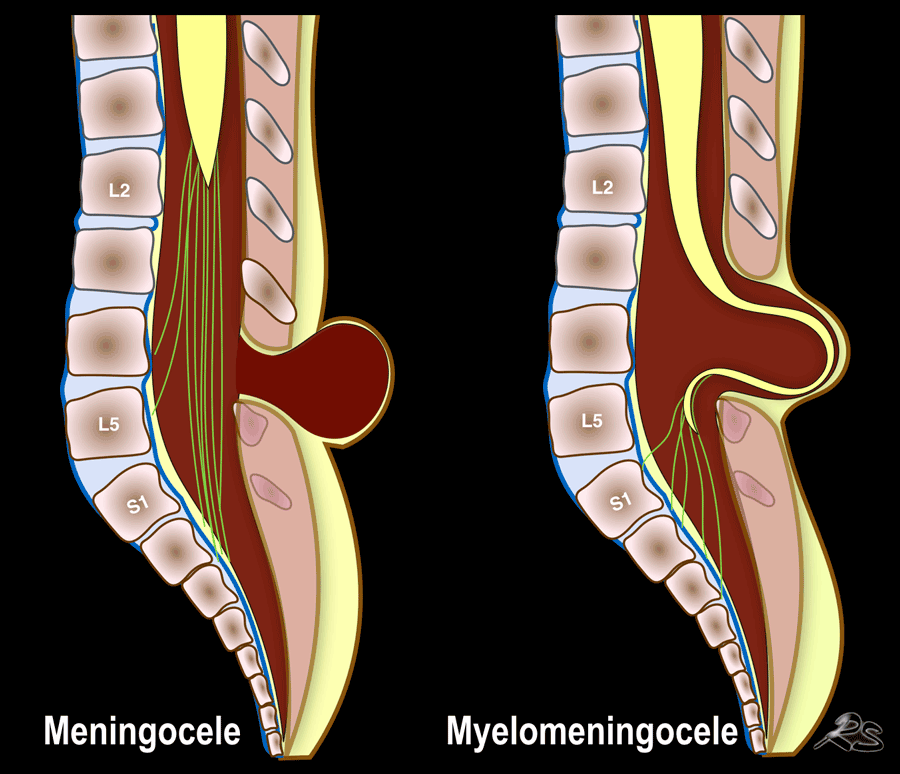
Spinal dysraphism or spina bifida is a congenital anomaly resulting in a defective closure of the neural arch.
It is classified into open (spina bifida aperta) and closed dysraphism (spina bifida occulta).
Open dysraphism presents with a swelling over the back which is noticed at birth and may contain meninges and CSF, called meningocele or contain parts of the spinal cord or nerves, called myelomeningocele.
Ultrasound should not be used to image open spinal dysraphism at the lesion itself.
It does not add much and can lead to infection.
Ultrasound can be used to examine more cranial parts of the vertebral column, searching for additional anomalies and is useful to measure the size of the ventricles of the brain after closure of the myelomeningocele.
Spina bifida occulta
In closed or occult spinal dysraphism, also called spina bifida occulta, there is an intact covering of the skin.
The anomaly is suspected when there are skin changes like hair tufts, hemangiomas, pigmented spots, cutaneous dimples or a subcutaneous mass.
Another reason to perform ultrasound is when there is a congenital anomaly that is associated with OSD like anal atresia.
The term OSD implies the presence of one or more spinal cord anomalies, which can cause tethering of the spinal cord and possible neurological and bladder/bowel function deficits.
The terms thickened or fatty filum terminale, spinal lipomas, split cord malformations, dermoid cyst, and syringohydromyelia are all different forms of OSD.
Normal anatomy
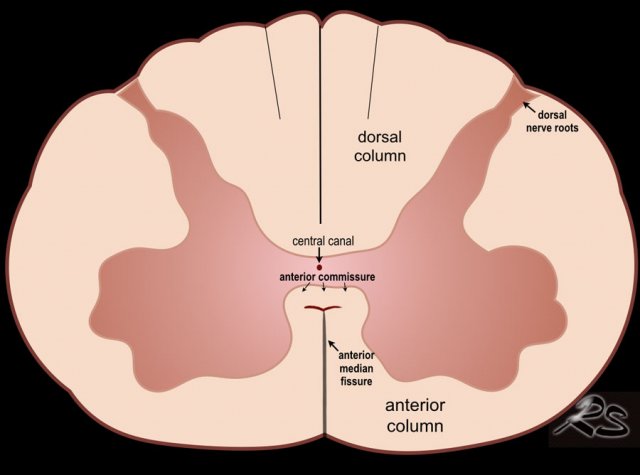
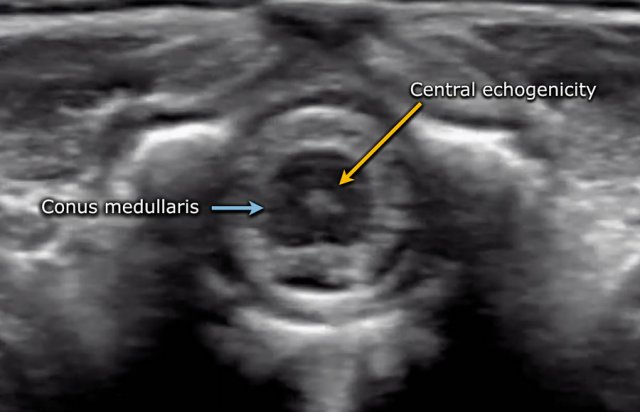
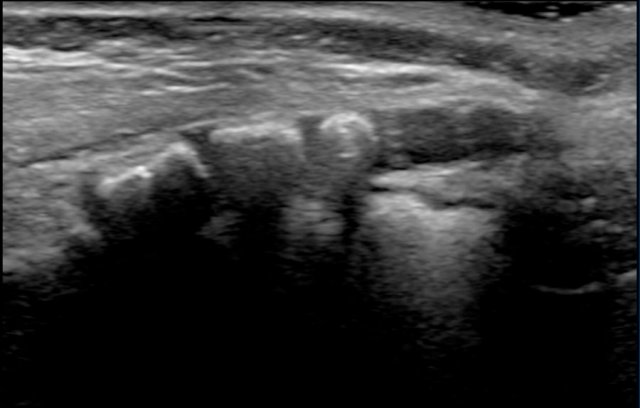
The spinal cord is depicted as a very hypoechoic structure with a central echogenicity.
This central echogenicity is supposed to represent the interface between the anterior commissure and the median anterior fissure, and not the central canal.
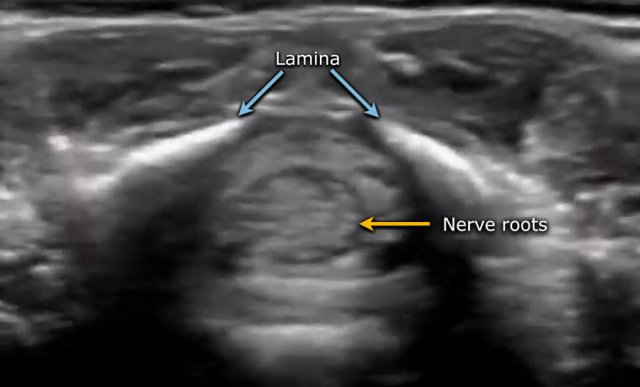
Axial image of the spinal cord with central echogenicity.
Axial image of the cauda equina.
The lower end of the cord is thickened, which is the lumbar intumescence.
The cord tapers in a sharp cone (blue arrow).
The cauda equina is seen as a bunch of moving strands.
If the baby is lying in the decubitus position, the strands will gravitate to the dependent posterior side.
If the baby is examined in the prone position with a pillow under the abdomen, the stands will move ventrally.
The filum terminale can be seen as a thin echogenic thread.
The dural sac ends at approximately S2.
More distally fatty tissue is present.
Video of the normal sagittal anatomy.
Always obtain axial views.
The movement of the nerve roots is better seen in the transverse plane compared to the sagittal plane and it is easier to assess intraspinal pathology like a thickened filum.
Film in right decubitus position.
The nerve roots are clustered in the dependent side, but move freely.
When the nerve roots do not move freely, it can be a sign of OSD.
Position of the conus medullaris
The normal position of the conus is at L!.
It should not be below L2.
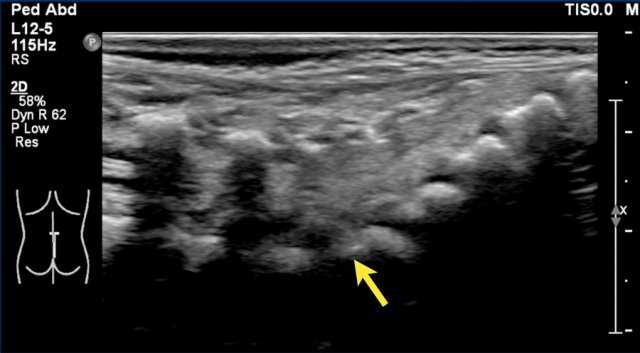
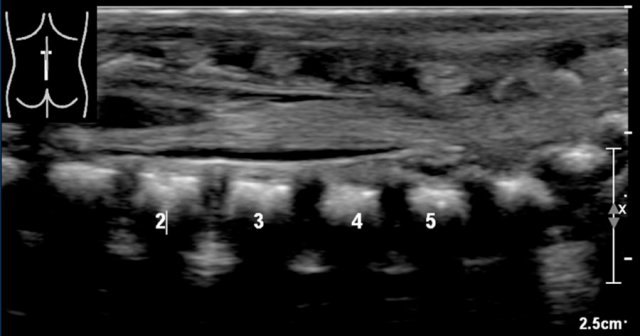
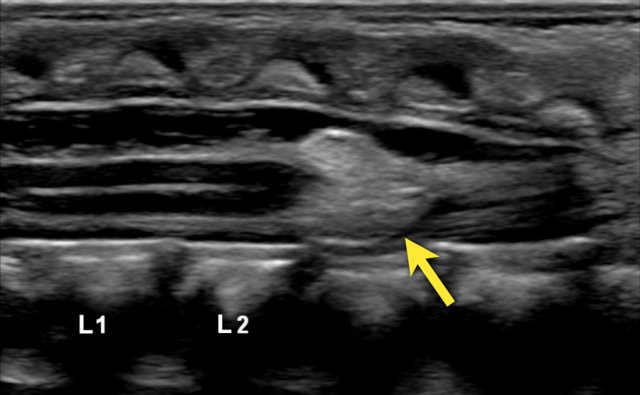
The best way to determine the position of the conus medullaris is by identifying the lumbosacral junction at the lordotic angle between the lumbar and sacral vertebrae (arrow).
It can be helpful to flex and extend the pelvis to see the point of motion of the sacrum.
In this newborn the lumbosacral junction is less clearly seen because there is no acute angle.
The numbers that we've put in, might be wrong.
If one is uncertain, make a panoramic or dual image of the lumbosacral vertebral column and compare the vertebral count from below upwards with a lateral plain film.
The coccyx, if not yet ossified, is composed of hypoechoic cartilage.
It usually has a kyphotic shape.
On transverse views it should not be confused with a fluid collection or an abscess.
Normal variants
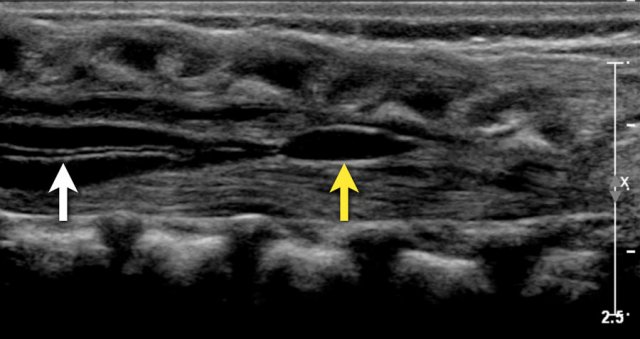 Two-week-old girl with a sacral simple. There is a slight hydromyelia (white arrow) and a cyst in the filum terminale (yellow arrow), both are normal variants.
Two-week-old girl with a sacral simple. There is a slight hydromyelia (white arrow) and a cyst in the filum terminale (yellow arrow), both are normal variants.
Central canal
In this image the central canal is visible as a thin anechoic line in the spinal cord (white arrow).
Although this is sometimes associated with pathology it is frequently seen as a normal finding.
Ventriculus terminalis
A small cyst is seen in the proximal filum terminale.
This is called a ventriculus terminalis (or fifth ventricle).
Sometimes it is seen in the conus medullaris.
It is formed during embryogenesis and usually regresses completely during early childhood.
If it stays persistent, it typically measures less than 2 cm in craniocaudal dimension and 2 mm in transverse dimension and is detected as an asymptomatic and incidental finding in adults.
Here a sagittal image of a three-months-old girl who was imaged because of a skin discoloration of the lower back.
The spinal anatomy was normal and there was no sign of OSD.
There is a straight coccyx, which is a normal variant.
Usually the coccyx has a anteriorly bent tip, but sometimes it is straight or even dorsally bent, which is also a normal variant.
Pathology
Tethered cord
In many cases occult spinal dysraphism may not cause any symptoms.
However in some cases there may develop neurological problems due to tethering of the cord.
A tethered cord is a pathologic fixation of the spinal cord in an abnormal caudal location, so that the cord suffers mechanical stretching, distortion and ischemia with growth and development.
In these cases ultrasound is well suited to image the contents of the spinal canal and to look for findings that are associated with a tethered cord (Table).
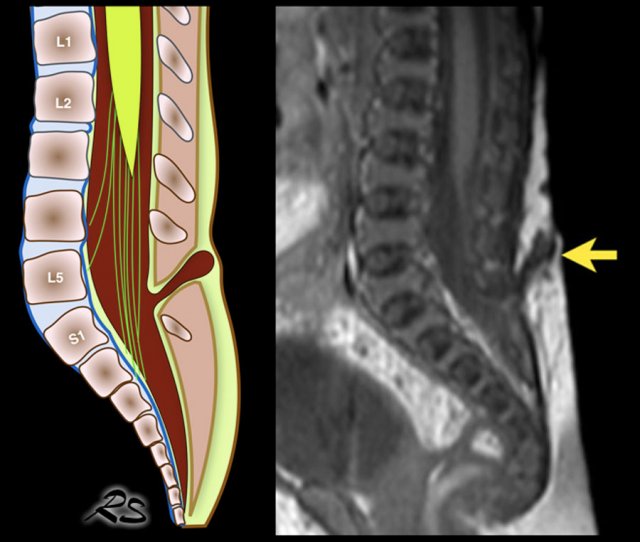
Low conus medullaris
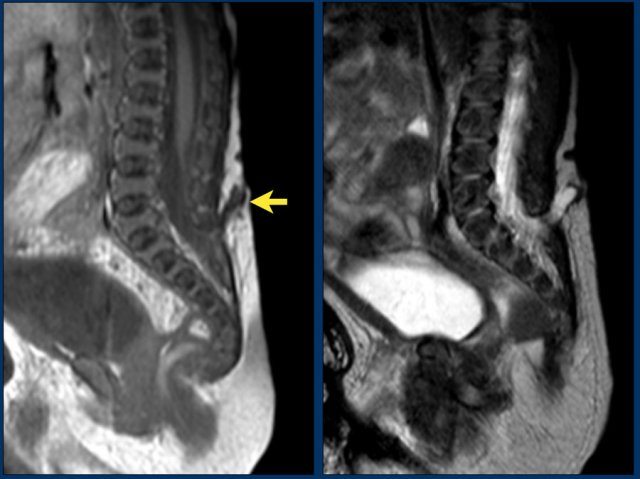
Newborn girl with a cloacal malformation.
The conus medullaris is at L5.
No lipoma visible.
Findings were confirmed at MR imaging which was acquired at the age of 9 months.
Continue with the MR.
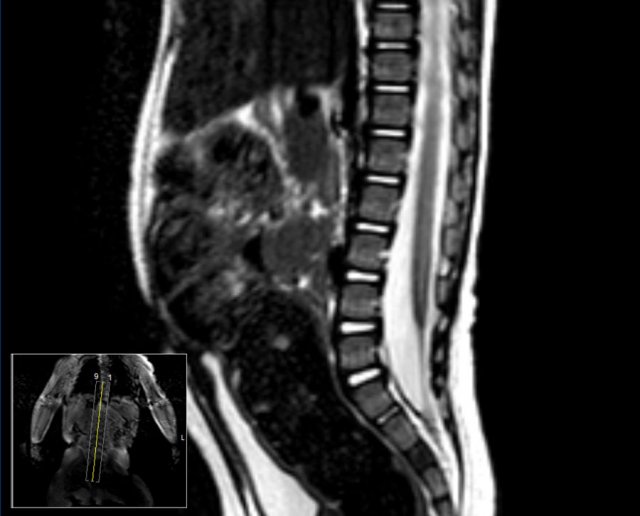
MR image at the age of 9 months.
The conus medullaris is now seen at L4.
Thickened filum terminale
Study the image.
What are the findings?
Findings:
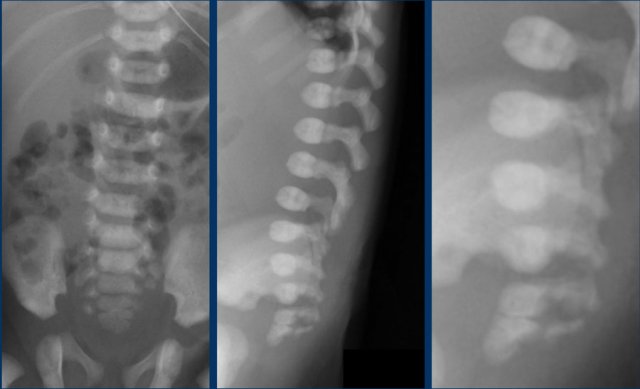
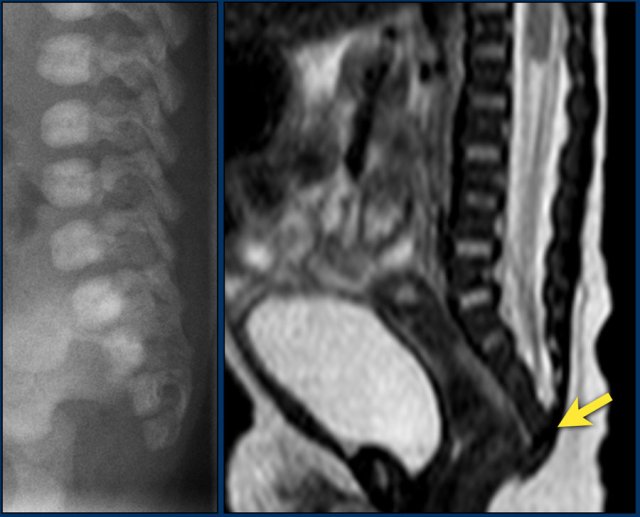
The plain film shows a fusion of S4 and S5.
This was a newborn boy with an anorectal malformation.
An ultrasound was performed to look for signs of occult spinal dysraphism.
This is the transverse video
There is a thickened filum with a low ending conus medullaris at L3-L4 and a mild hydromyelia.
Continue with the sagittal video.
On the sagittal video the low ending conus medullaris is seen at L3-L4.
Continue with the MRI.
The MRI also depicts:
- Hydromyelia
- Low ending conus medullaris.
- Thickened filum terminale
The upper limit of normal for the width of the filum terminale is 2 mm.
If it is thickened it often shows fatty infiltration with hyperechoic tissue.
In healthy newborns, the tip of the conus medullaris is located between L1 and L2.
The tip should not be positioned below L2-3.
Hydromyelia
A hydromyelia is the abnormal widening of the central canal by cerebrospinal fluid. This condition may be either focal or diffuse, extending through the entire length of the spinal cord.
It can be associated with several congenital abnormalities including diastematomyelia, Arnold‐Chiari malformation, myelomeningocele and lipomeningocele.
If there is a fluid collection in the cord outside the central canal it is called syringomyelia.
Because it is often not possible to separate these two entities on imaging, it is better to use the term syringohydromyelia.
Transverse images will show the transition of the normal cord into the cord which surrounds a CSF collection
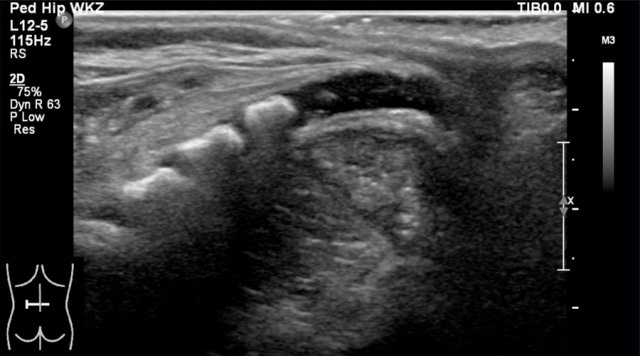
Spinal lipoma
A spinal lipoma is an encapsulated deposit of fat, neural tissue, meninges or fibrous tissue which extends from the posterior subcutaneous tissue through a midline defect of the fascia, muscle or bone to communicate with the spinal canal or meninges.
A spinal lipoma is seen as an echogenic mass, mostly in the lower spinal canal.
The conus can be too low and buried in the lipoma.
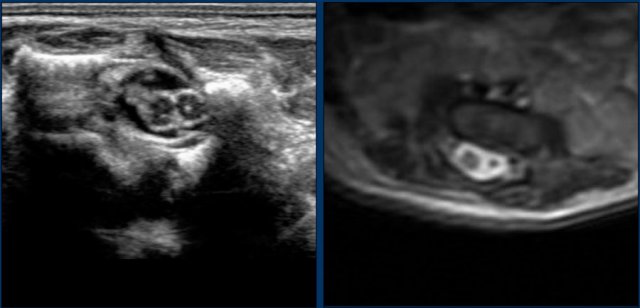
Here a sagittal image of a newborn boy with anal atresia.
The conus is blunted and ends at L2-L3.
There is an echogenic mass which is likely a lipoma.
The filum is thickened.
Small lipomas are often led alone. Bigger lipomas in symptomatic patients are removed.
On a transverse video the ecogenic mass just below the cord terminus is seen.
Dorsal dermal sinus
This is a connection between the skin and the dural sac, sometimes into the spinal cord.
It presents with a dimple, discoloration of the skin or hairy patches.
The conus medullaris can be too low.
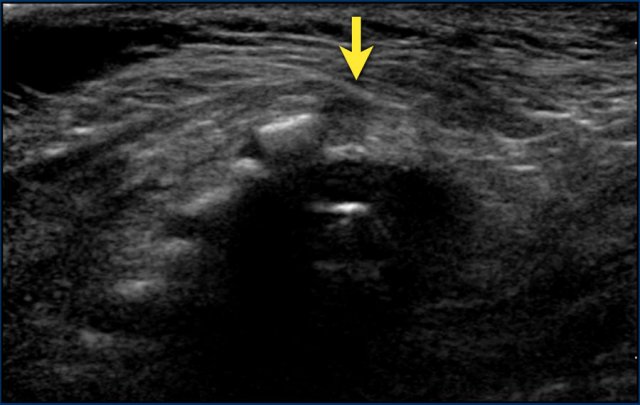
Three-day-old girl with a red stain on the lower back, a tuft of hair and a dimple.
US shows a tract from the skin towards the dural sac at the S1-S2 level, compatible with a dorsal dermal sinus .
The conus medullaris is at a normal level and there is no other intraspinal pathology present.
A T1-weigthed image shows the sinus tract from the skin towards the S1-S2 level.
The conus medullaris is too low at L3-L4.
Dermal sinus tracts are especially important lesions to recognize because they can extend to the spinal canal and represent an increased risk of infection such as meningitis and spinal cord abscess.
Diastematomyelia
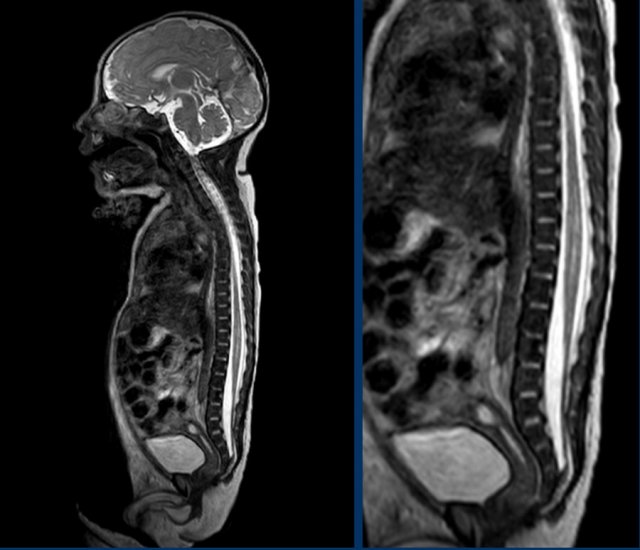
Diastematomyelia, also named split cord malformation, is a longitudinal split of the spinal cord.
At the point of division, there may be an osseous, fibrous or cartilaginous dividing septum.
Diastematomyelia is commonly associated with a vertebral column abnormality and a tethered spinal cord.
The ultrasound diagnosis is usually straightforward.
Here images of a newborn, who had several antenatal anomalies.
There was a lateral rocker bottom feet deformity, lumbar kyphoscoliosis and swelling on the lower back.
The spinal US and MR show a longitudinal split of the spinal cord at the thoracolumbar level.
The bifid cord is asymmetric in volume.
Additional plain films of the lumbar spine and pelvis showed thoracic and lumbar hemivertebrae.
There was also a dislocated left hip.
Blunt cord terminus
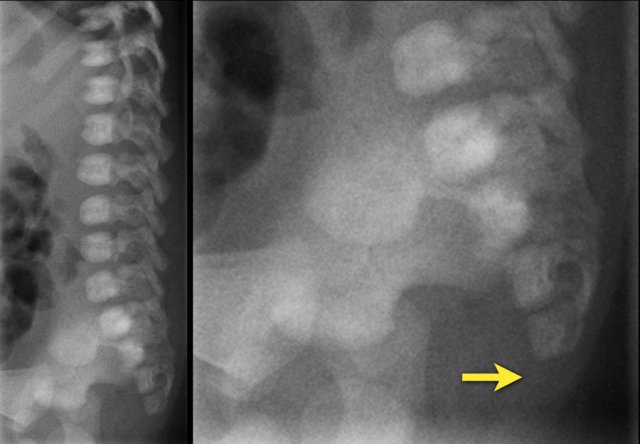
This image is of a newborn girl with an anorectal malformation.
The distal sacrum below S4 is absent (arrow).
Since an anorectal malformation is frequently associated with spinal pathology, an ultrasound was performed.
If a plain film of the vertebral column demonstrates an anomaly of the sacrum, there is a 50% change of an intraspinal anomaly.
In most cases there is a low ending tethered cord.
In some cases however the cord ends at the normal position, but is deformed.
This is a so-called blunt cord terminus.
There is generally a wedge-shaped ending in which the dorsal side reaches further caudally than the ventral side.
Continue with the ultrasound.
Ultrasound of the spine shows a blunt cord terminus at T12-L1.
A blunt cord terminus is a sign of caudal regression syndrome characterized by abnormal development of the lower end of the spine.
On ultrasound the absent coccyx is also visible.
Continue with the MRI.
Sagittal T2-weigthed image showing the cord terminus at Th12.