Temporal Bone Pathology
Eric Beek and Frank Pameijer
Radiology department of the University Medical Centre of Utrecht, the Netherlands
Publicationdate
The aim of this presentation is to demonstrate imaging findings of common diseases of the temporal bone.
CT is the imaging modality of choice for most of the pathologic conditions of the temporal bone, especially for those of the middle ear.
MRI is more useful for diseases of the inner ear.
Disease processes in the pontine angle and in the internal acoustic meatus are not discussed.
Normal variants
There are several normal variants which may simulate disease or should be reported because they can endanger the surgical approach.
Variants which may simulate disease:
- Cochlear cleft (otosclerosis)
- Petromastoid canal (fracture)
- Cochlear aqueduct (fracture)
Variants which may pose a danger during surgery:
- High jugular bulb or jugular bulb diverticulum
- Bulging sigmoid sinus
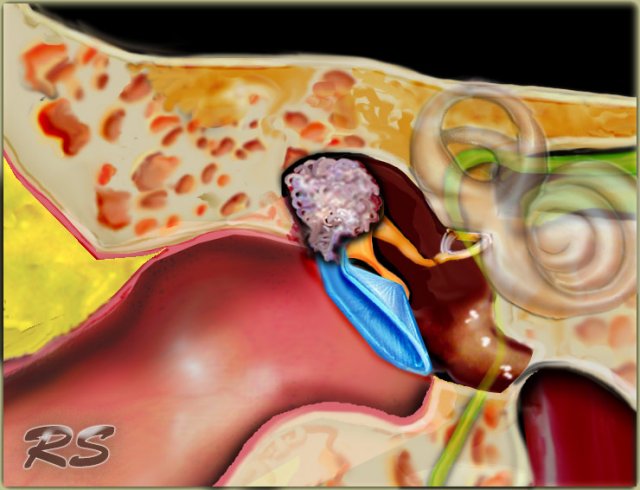
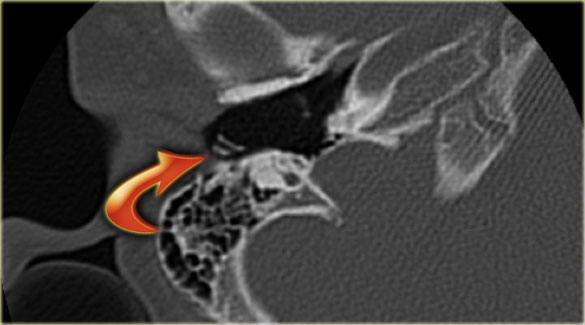
On the left an illustration of a cholesteatoma.
This will be discussed later.
Cochlear cleft
A cochlear cleft is a narrow curved lucency extending from the cochlea towards the promontory.
It is often visible in infants and children but can also be seen in adults.
It can be mistaken for a fracture line or an otosclerotic focus.
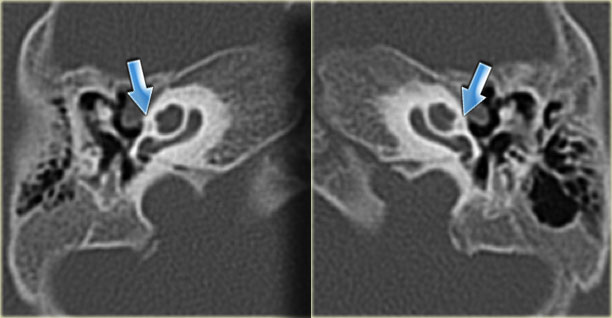
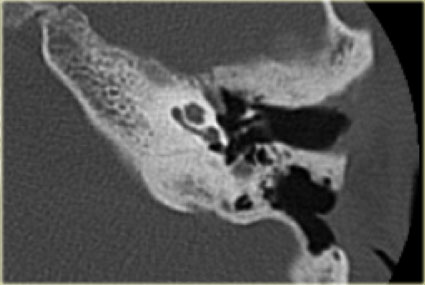
On the left an example of bilateral cochlear cleft in a one-year old boy with congenital hearing loss.
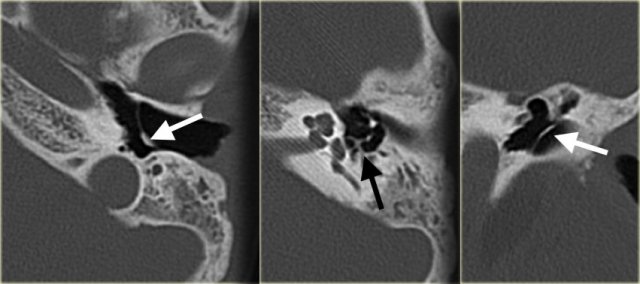
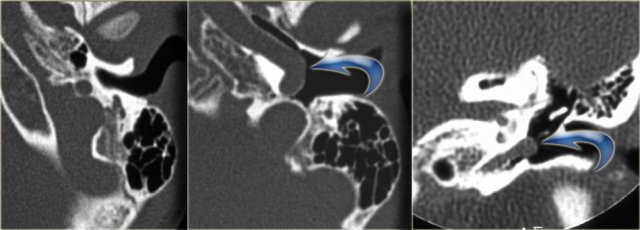
Petromastoid canal
The petromastoid canal or subarcuate canal connects the mastoid antrum with the cranial cavity and houses the subarcuate artery and vein.
Its diameter is around 0.5 mm.
It can be confused with a fracture line.
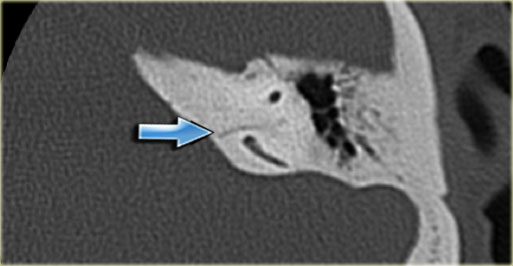
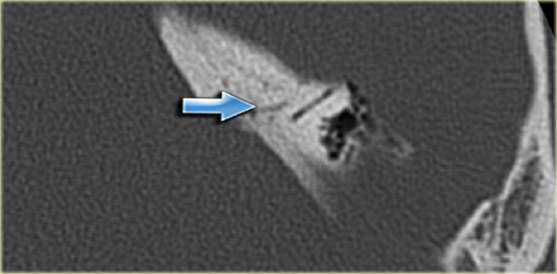
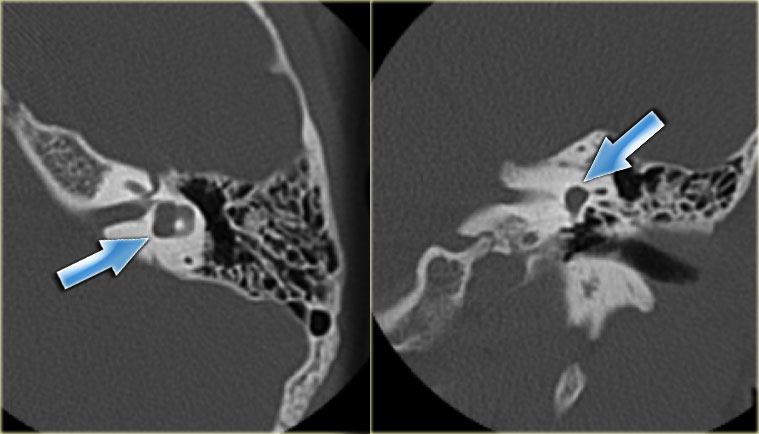
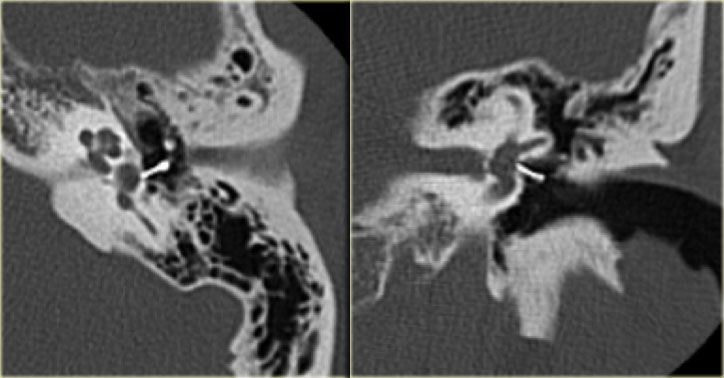
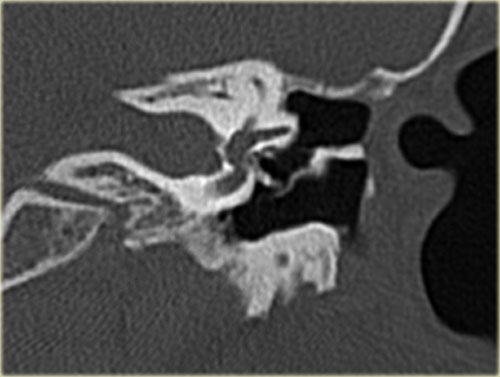
On the left a 40-year old female with a sclerotic mastoid.
The petromastoid canal is easily seen. (arrow)
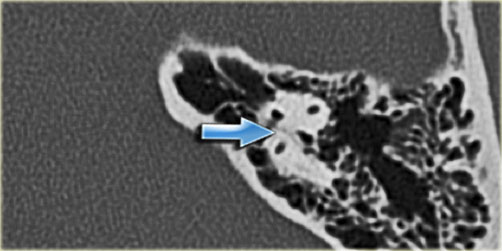
On the left a well-pneumatized mastoid.
The petromastoid canal is difficult to discern (arrow).
On the left another patient with a sclerotic mastoid.
The petromastoid canal is well seen.
If this patient would be a trauma victim, the canal could easily be confused with a fracture line (arrow).
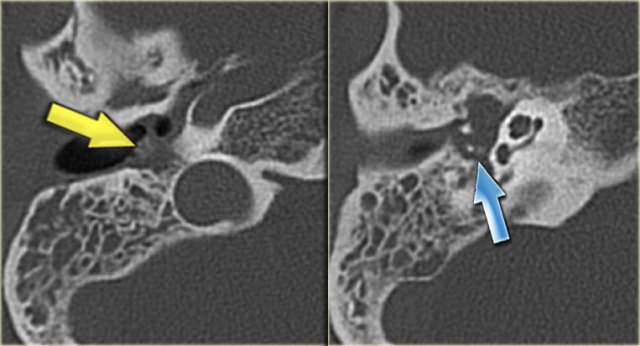
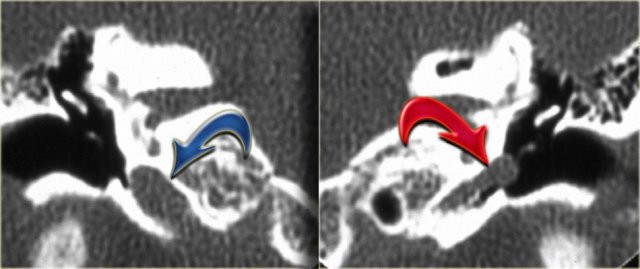
Cochlear aqueduct
The cochlear aqueduct connects the perilymph with the subarachoid space.
The cochlear aqueduct is a narrow canal which runs towards the cochlea in almost the same direction as the inner auditory canal, but situated more caudally.
It is a point where infected cerebrospinal fluid can enter the inner ear.
This can happen in patients with meningitis and cause labyrinthitis ossificans.
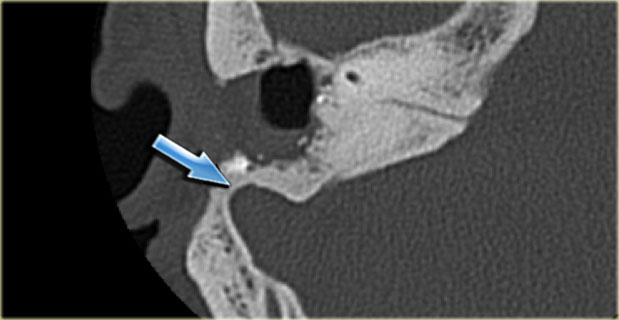
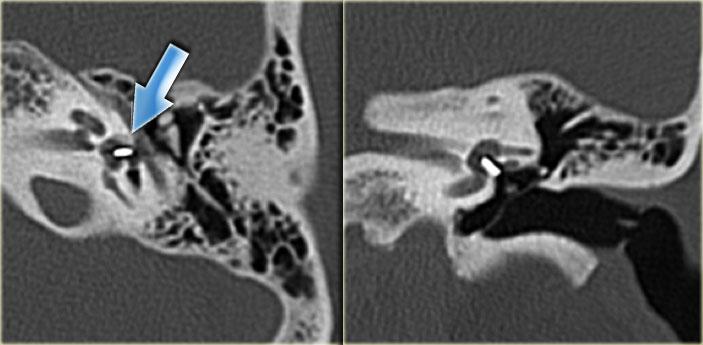
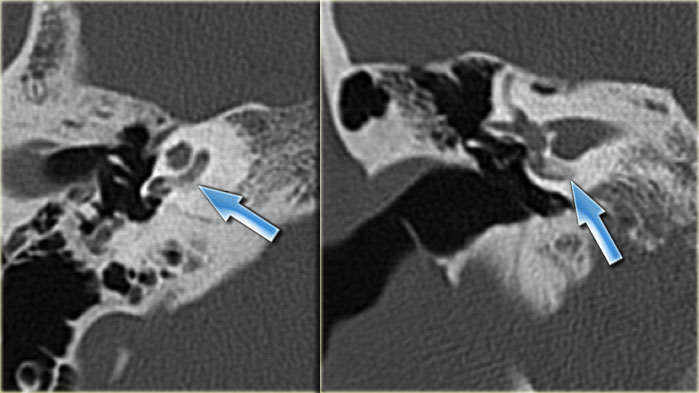
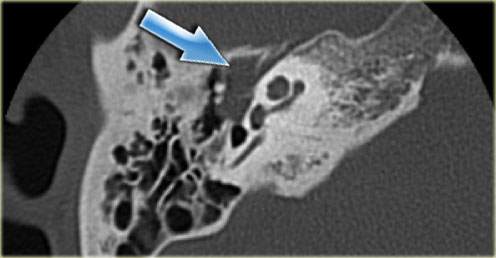
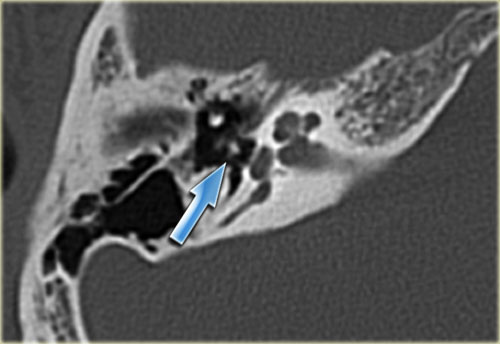
On the left a 58-year old male.
The blue arrow indicates the cochlear aqueduct coursing towards the cochlea.
This could be mistaken for a fracture line (arrow).
Note there is also opacification of the tympanic cavity and mastoid air cells.
High jugular bulb
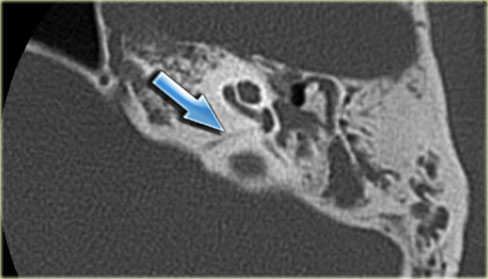
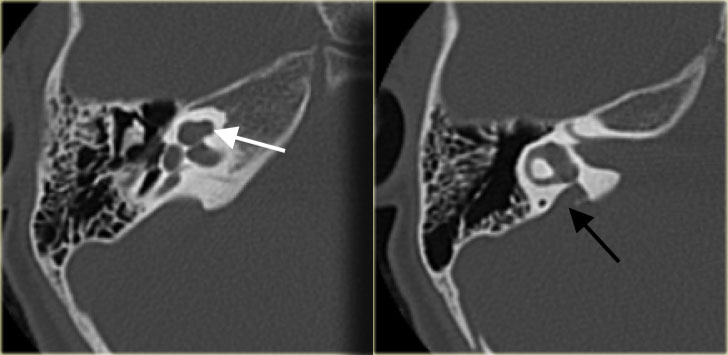
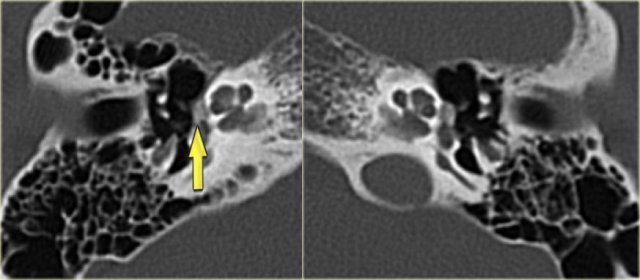
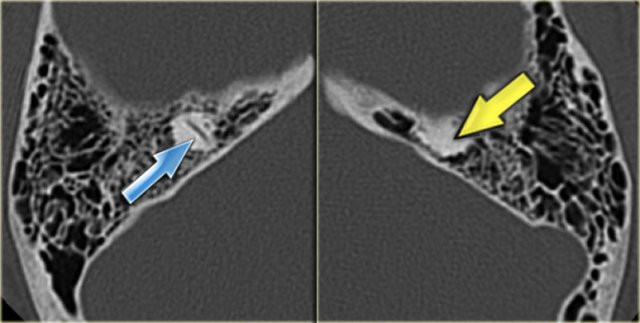
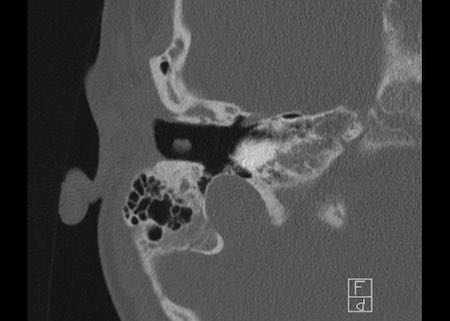
On the left axial and coronal images of a 64-year old male.
The jugular bulb rises above the lower limb of the posterior semicircular canal (arrows).
The jugular bulb is often asymmetric, with the right jugular bulb usually being larger than the left.
If it reaches above the posterior semicircular canal it is called a high jugular bulb.
If the bony separation between the jugular bulb and the tympanic cavity is absent, it is termed a dehiscent jugular bulb.
Rarely an outpouching is seen – this is known as a jugular bulb diverticulum.
Jugular bulb diverticulum
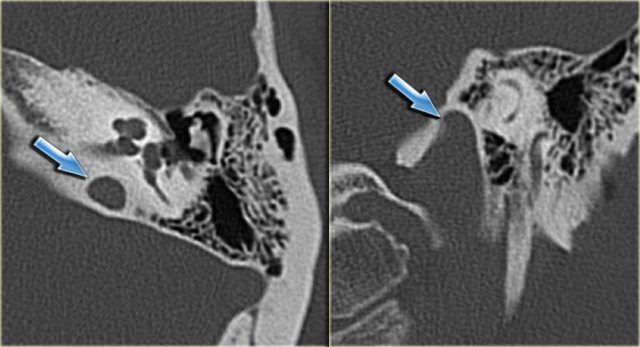
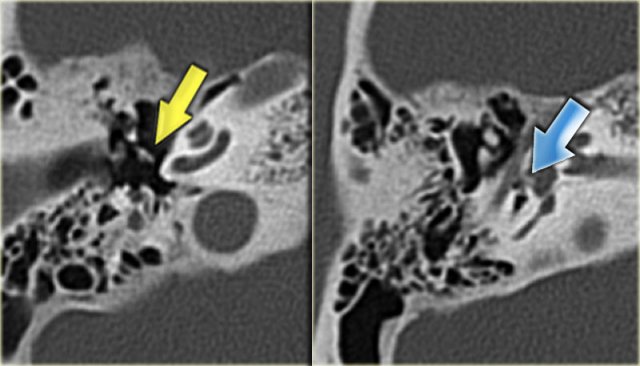
On the left axial and coronal images of a 50-year old male.
Incidental finding of a jugular bulb diverticulum (arrows).
Bulging sigmoid sinus
The sigmoid sinus can protrude into the posterior mastoid.
It can be accidentally lacerated during a mastoidectomy and therefore should be mentioned in the radiological report when present.
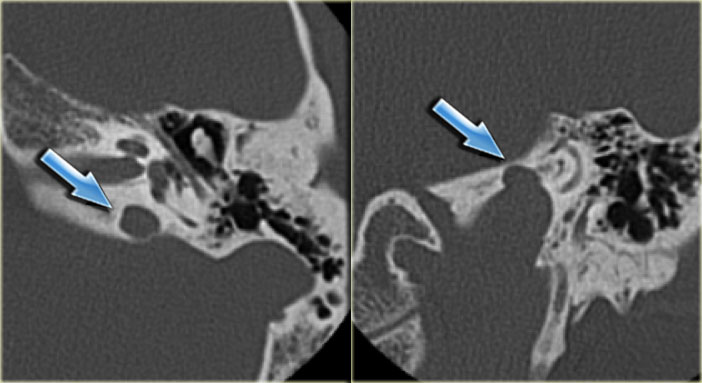
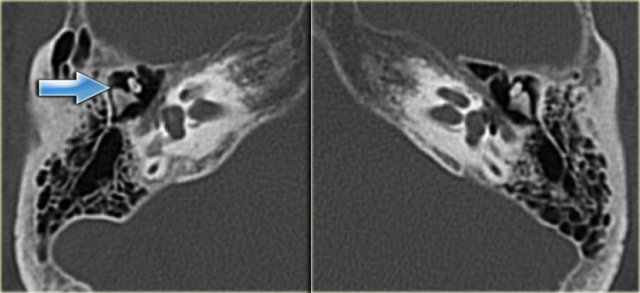
On the left an axial image of a 43-year old male, post-mastoidectomy.
The sigmoid sinus bulges anteriorly
Congenital anomalies
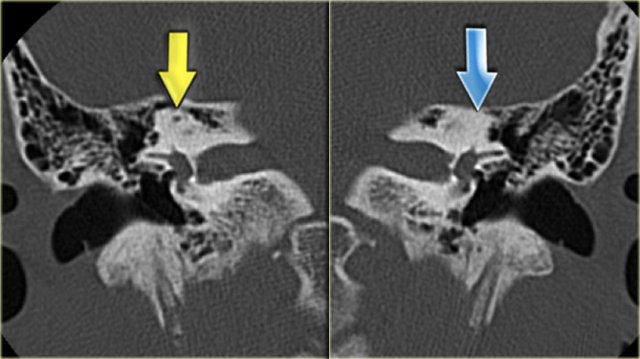
 Large vestibular aqueduct bilaterally (black arrows). The bony modiolus is not visible (white arrow).
Large vestibular aqueduct bilaterally (black arrows). The bony modiolus is not visible (white arrow).
Large vestibular aqueduct
The vestibular aqueduct is a narrow bony canal (aqueduct) that connects the endolymphatic sac with the inner ear (vestibule).
Running through this bony canal is a tube called the endolymphatic duct.
A large vestibular aqueduct is associated with progressive sensorineural hearing loss.
This progression is reportedly associated with minor head trauma, which exposes the inner ear to pressure waves via the large vestibular aqueduct.
The large vestibular aqueduct is associated with an absence of the bony modiolus in more than 90% of patients.
On the left a patient with a bilateral large vestibular aqueduct.
Notice that the bony modiolus is not visible.
On the left a 5-year old boy with bilateral progressive hearing loss.
A large vestibular aqueduct is seen (black arrow).
The cochlea has no bony modiolus. (white arrow).
External auditory canal atresia
In external ear atresia the external auditory canal is not developed and sound cannot reach the tympanic membrane.
A conductive hearing loss is the result.
It is important to note whether the atretic plate is composed of soft tissue or bone.
The extent of ossicular chain malformation can vary from a fusion of the mallear head and incudal body to a small clump of malformed ossicles, which is often fused to the wall of the tympanic cavity.
The mastoid portion of the facial nerve canal can be located more anteriorly than normal and this is important to report to the ENT surgeon in order to avoid iatrogenic injury to the nerve during surgery.
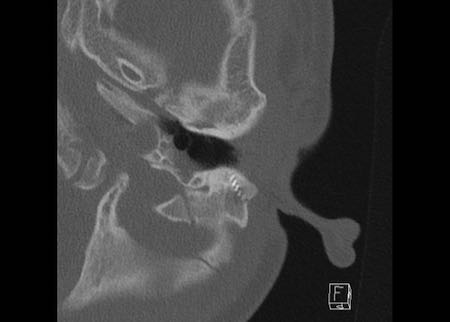
On the left a 2-year old boy with bilateral bony external auditory canal atresia.
The malleus and incus are fused (arrow).
The cochlea is normal.
Cochlear deformities
The cochlea develops between 3 and 10 weeks of gestation.
Early developmental arrest leads to an inner ear that consists of a small cyst, the so-called Michel deformity.
Developmental arrest at a later stage leads to more or less severe deformities of the cochlea and of the vestibular apparatus.
An incomplete partition of the cochlea is called a Mondini malformation
Instead of the normal two-and-one-half turns, there is only a normal basal turn and a cystic apex.
On the left a 2-year old girl.
The images are of a CT-examination is done prior to cochlear implantation.
A minor deformity of the cochlear apex is visible – there is no separation of the second and third turn and the bony modiolus is absent.
The vestibular aqueduct is normal.
Lateral semicircular canal malformation
Malformations of the vestibule and semicircular canals vary from a common cavity to all these structures to a hypoplastic lateral semicircular canal.
During embryogenesis the lateral semicircular canal is the last structure to form, thus in malformations of the semicircular canals the lateral canal is most commonly affected.
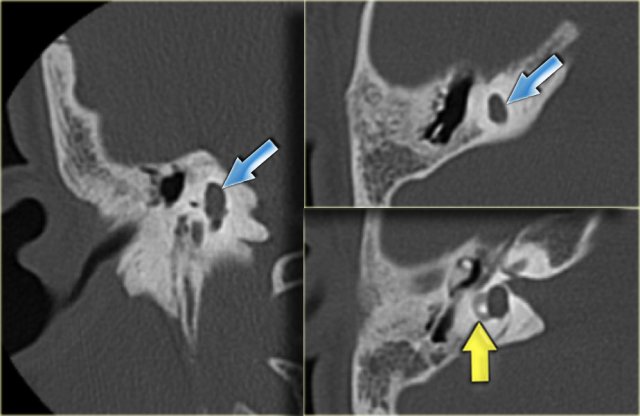
On the left a 10-year old boy, scheduled for cochlear implantation.
There is a widening and shortening of the lateral semicircular canal.
The vestibule is relatively large (arrow).
On the left a 16-year old boy, examined preoperatively for a cholesteatoma of the right ear.
As a coincidental finding, there is a plump lateral semicircular canal (yellow arrow) and an absence of the superior canal (blue arrow).
In the expected position of the superior canal only a bump is seen.
The posterior canal is normal.
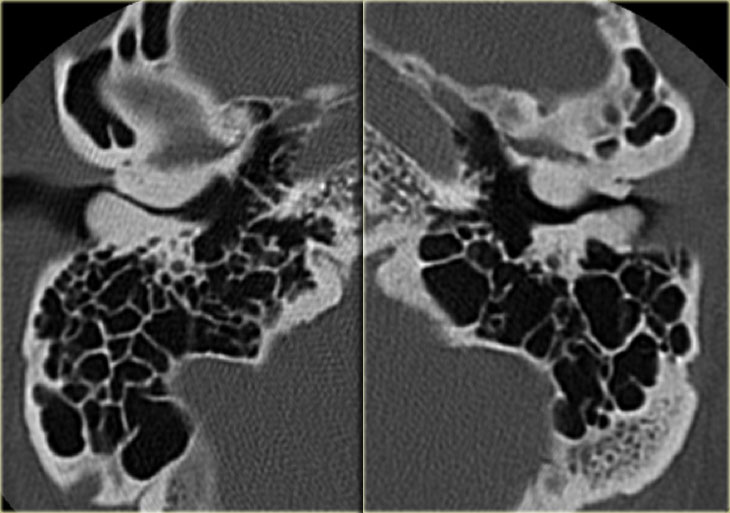
Chronic otitis media
For the ENT-surgeon the differentiation between chronic otitis media and cholesteatoma is important.
Both diseases often occur in poorly pneumatized mastoids.
An important finding which can help differentiate the two conditions is bony erosion.
Erosion of the lateral wall of the epitympanum and of the ossicular chain is common in cholesteatoma (around 75%).
Erosion can occur in chronic otitis, but reportedly in less than 10% of patients.
Displacement of the ossicular chain can be seen in cholesteatoma, not in chronic otitis.
Cholesteatoma can present with a non-dependent mass while chronic otitis shows thickened mucosal lining.
However, in both diseases the middle ear cavity can be completely opacified, obscuring a cholesteatoma.
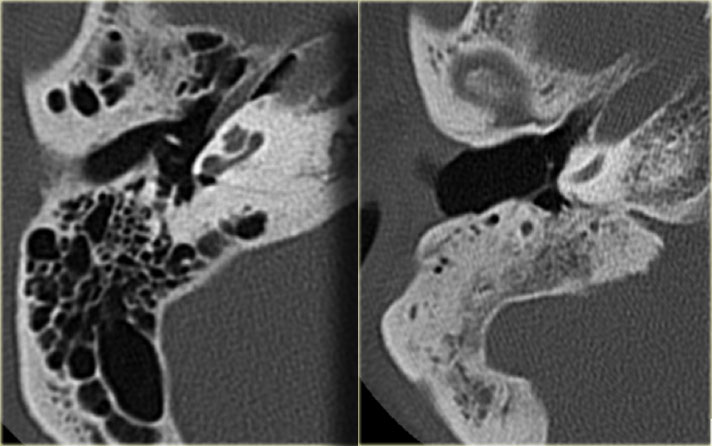
On the far left a 54-year old male with a normally pneumatized mastoid with aerated cells.
Next to it a 69-year old female.
The mastoid is completely sclerotic - no air cells are present.
On the left a 14-year old boy.
The eardrum is thickened.
A small amount of soft tissue (arrow) is visible between the scutum and the ossicular chain but no erosion is present.
This favors the diagnosis of chronic otitis media.
On the left an 11-year old girl with bilateral ear infections.
There is calcification of the eardrum (white arrow) and calcific deposits on the stapes and the tendon of the stapedius muscle (black arrow).
On the left a 37-year old female who was admitted with a peritonsillar abscess.
She
also suffered from chronic otitis media.
CT shows a tympanostomy
tube (yellow arrow) and almost complete
opacification of the
tympanic cavity and mastoid air cells with soft tissue.
Note: No air present in
the lumen of the tympanostomy tube
Calcification is visible
around the head of the stapes (blue arrow).
No erosions are present.
On the left a coronal reconstruction of the same patient.
CT shows the tympanostomy tube (yellow arrow) and complete opacification of the tympanic cavity and mastoid air cells with soft tissue.
Cholesteatoma
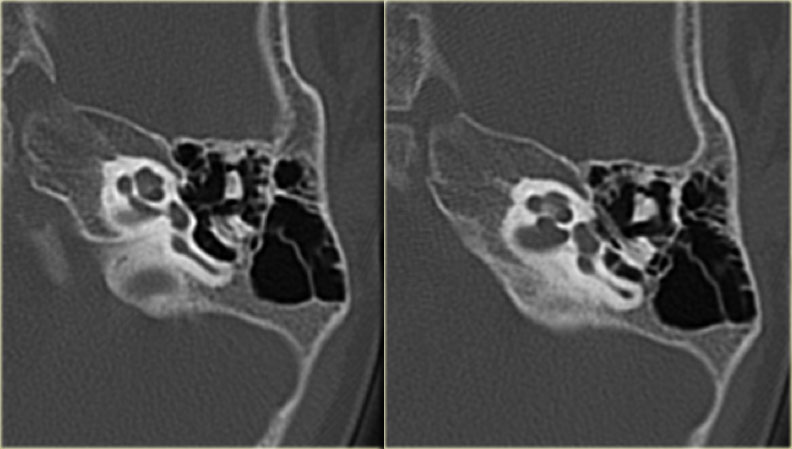
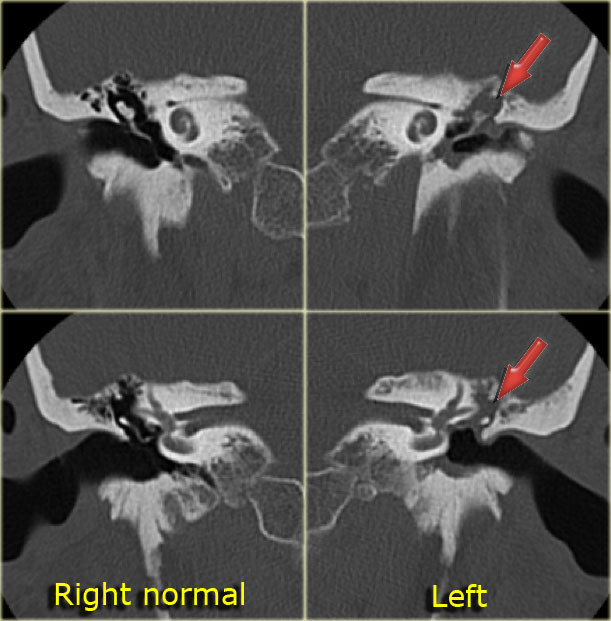
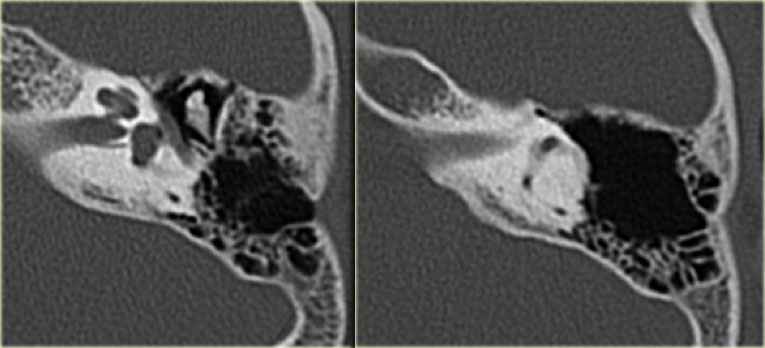
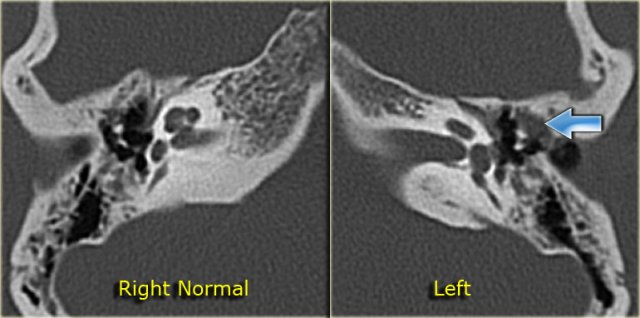 Cholesteatoma: 20-year old woman with recurrent otitis. Granulations on left ear drum. Soft tissue mass between ossicular chain and lateral tympanic wall, which is eroded. Right side for comparison.
Cholesteatoma: 20-year old woman with recurrent otitis. Granulations on left ear drum. Soft tissue mass between ossicular chain and lateral tympanic wall, which is eroded. Right side for comparison.
Cholesteatoma is believed to arise in retraction pockets of the eardrum.
It gradually enlarges over time due to exfoliation and encapsulation of the tissue.
Most cholesteatomas are acquired, but some are congenital.
The ENT surgeon often states that cholesteatoma is a clinical diagnosis.
Scraps of cholesteatoma are visible in the external auditory canal.
On CT a small cholesteatoma presents as a soft tissue mass.
In more extensive disease erosions may be present.
Large cholesteatomas can erode the auditory ossicles and the walls of the antrum and extend into the middle cranial fossa.
The most affected structures are:
- Auditory ossicles, especially the long process and lenticular processes of the incus as well as the head of the stapes
- Wall of the lateral semicircular canal
- Lateral epitympanic wall (the scutum)
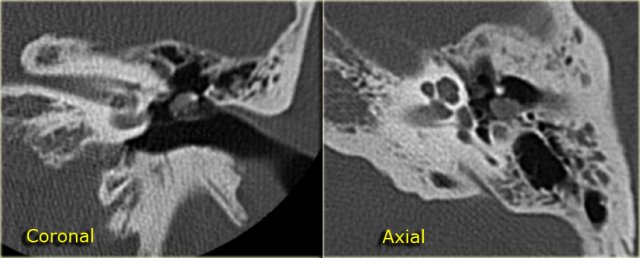
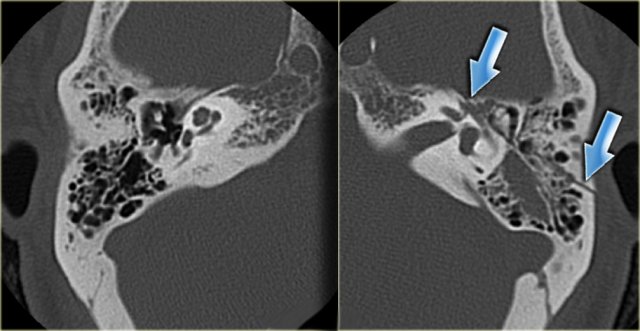
On the left a 20-year old woman with recurrent otitis.
There were granulations on the left ear drum.
CT demonstrates a soft tissue mass between the ossicular chain and the lateral tympanic wall, which is eroded.
this favors the diagnosis of cholesteatoma.
 20-year old woman with recurrent otitis. Granulations on left ear drum. Soft tissue mass between ossicular chain and lateral tympanic wall, which is eroded. Right side for comparison.
20-year old woman with recurrent otitis. Granulations on left ear drum. Soft tissue mass between ossicular chain and lateral tympanic wall, which is eroded. Right side for comparison.
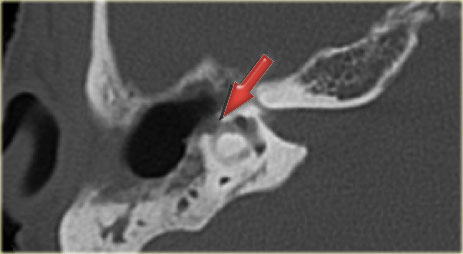
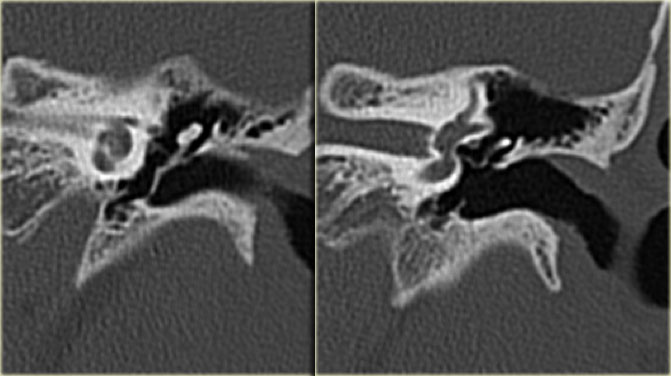
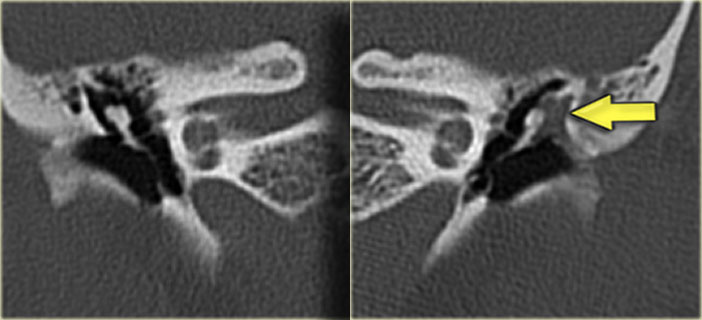
On the left the coronal images of the same patient as above.
Notice how the cholesteatoma has eroded the scutum (arrow).
There are two patterns of spread:
- Pars flaccida cholesteatoma
The lesion starts anterosuperiorly in 'Prussaks space', the area just below the scutum, which is limited by the tympanic membrane, the malleus, and the lateral ligament of the malleus.
A cholesteatoma will then extend laterally towards the ossicular chain and into the epitympanum. - Pars tensa cholesteatoma
The cholesteatoma begins posterosuperiorly and extends posteriorly towards the facial recess and tympanic sinus, and medially towards the ossicular chain.
On the left a large cholesteatoma in the right middle ear with destruction of the lateral wall of the tympanic cavity.
The body of the incus, which is lateral to the mallear head is also eroded (arrow).
CT signs of cholesteatoma are:
-
Soft tissue mass in the middle ear
- Especially if located in Prussaks space
- In advanced cholesteatoma the presence of aerated parts of the middle ear denote a mass and not an effusion
- Non-dependent soft tissue particularly favors a mass
-
Bony erosion in the following predilection sites:
- Scutum (lateral wall of the epitympanum)
- Lateral semicircular canal
- Tegmen tympani
- Long process of the incus and stapes superstructure
Erosion of the facial nerve canal is difficult to distinguish because the wall is often so thin that it is not visible at CT.
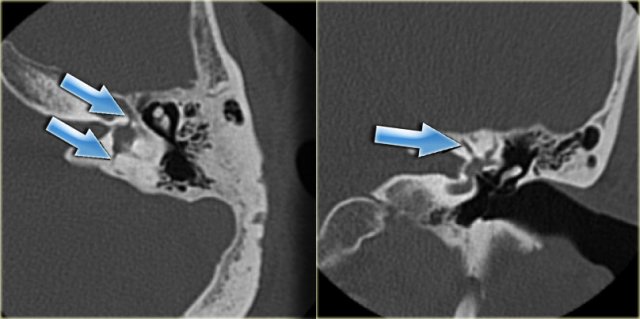
On the left a 50-year old male with hearing loss on the left side.
There is a soft tissue mass with erosion of the long process of the incus.
This location is typical of a pars tensa cholesteatoma.
On the left images of a cholesteatoma, which has eroded the ossicular chain and the wall of the lateral semicircular canal (arrows).
The thickened ear drum is perforated.
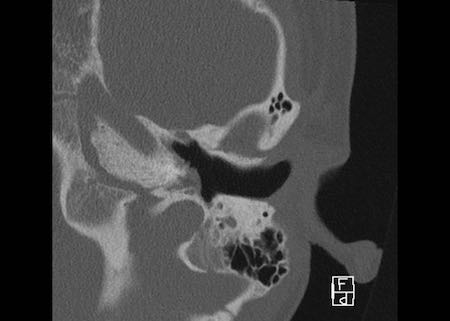
On the left images of a 6-year old boy.
A large cholesteatoma has resulted in a so called 'automastoidectomy', with severe erosion of the lateral tympanic cavity wall and destruction of the ossicular chain.
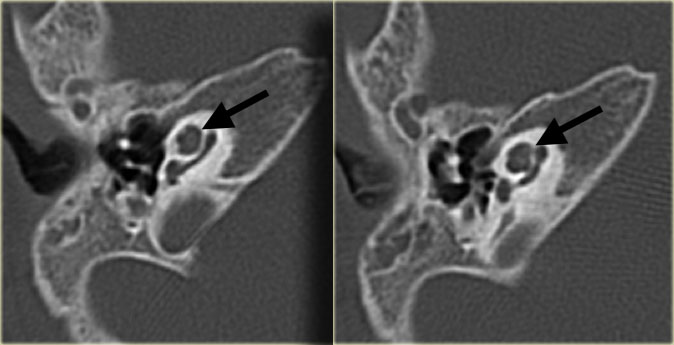
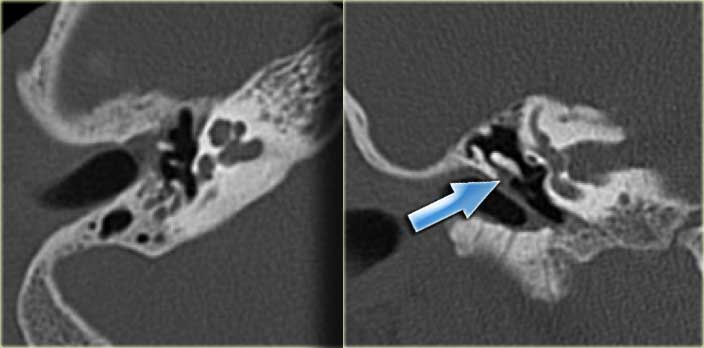
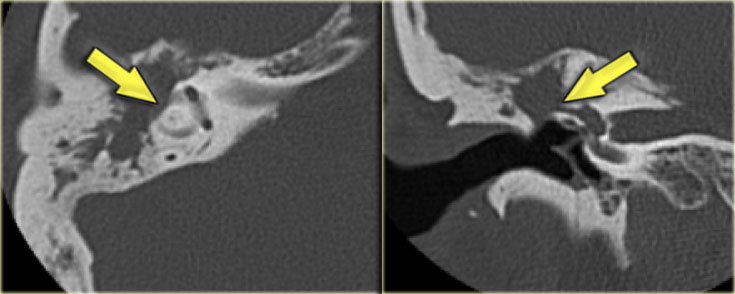
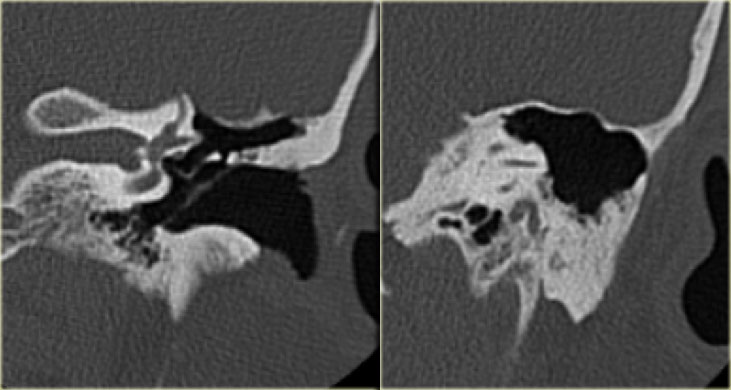
These images are of a 50-year old man who presented with a left- sided retraction pocket and otorrhoea.
CT shows erosion of the long process of the incus and of the stapedial superstructure.
All these findings favor the diagnosis of a cholesteatoma, but at surgery, chronic mastoiditis was found and no cholesteatoma was identified.
A minority of patients with chronic mastoiditis show bony erosions.
On the left coronal images of the same patient.
The scutum is blunted (arrow).
On the left an image of a 53-year old man complaining of vertigo.
He had undergone several ear operations in the past.
The CT shows erosion of the wall of the lateral semicircular canal (arrow) due to cholesteatoma.
 Cholesteatoma with lateral displacement of the incus with erosion of its lenticular process and of the stapes
Cholesteatoma with lateral displacement of the incus with erosion of its lenticular process and of the stapes
On the left a 22-year old man suffering from persistent otitis.
The right ear shows a soft tissue mass medial to the ossicular chain with lateral displacement of the incus with erosion of its lenticular process and of the stapes, compatible with a pars tensa cholesteatoma (arrow).
 Cholesteatoma with lateral displacement of the incus with erosion of its lenticular process and of the stapes
Cholesteatoma with lateral displacement of the incus with erosion of its lenticular process and of the stapes
On the left coronal images of the same patient.
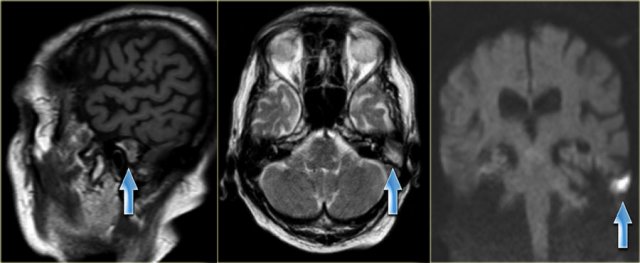 75-year old man with known recurrent cholesteatoma. The examination shows a mass with mixed intensity on sagittal T1 and high intensity on transverse T2 weighted images. It has a high intensity on diffusion weighted images, which indicates restricted diffusion. (arrows)
75-year old man with known recurrent cholesteatoma. The examination shows a mass with mixed intensity on sagittal T1 and high intensity on transverse T2 weighted images. It has a high intensity on diffusion weighted images, which indicates restricted diffusion. (arrows)
Cholesteatomas are of mixed intensity on T1-weighted pulse sequences and of high intensity on T2-weighted pulse sequences.
MRI is particularly useful for evaluating the extension of a cholesteatoma into the middle and/or posterior fossa, and for demonstrating possible herniation of intracranial contents into the temporal bone - especially after surgery.
After intravenous contrast MRI can distinguish granulation tissue from effusions.
Diffusion weighted MR can differentiate between a cholesteatoma, which has a restricted diffusion, and other abnormalities - especially granulation tissue - which have normal diffusion characteristics (figure).
Otosclerosis
Otosclerosis is a genetically mediated metabolic bone disease of unknown etiology.
It is sometimes called otospongiosis because the disease begins with an otospongiotic phase, which is followed by an otosclerotic phase when osteoclasts are replaced by osteoblasts and dense sclerotic bone is deposited in areas of previous bone resorption.
When this process involves the oval window in the region of the footplate, the footplate becomes fixed, resulting in conductive hearing loss.
Conductive hearing loss develops early in the third decade and is considered to be the hallmark of the disease.
However, involvement of other portions of the otic capsule can result in mixed sensorineural hearing loss.
The process starts in the region of the oval window, classically at the fissula ante fenestram, i.e. in front of the oval window (fenestral otosclerosis).
It can also occur around the cochlea (retrofenestral otosclerosis).
On the left a transverse CT-image of a 23-year old female with conductive hearing loss.
There is a subtle otosclerotic focus in the characteristic site: the fissula ante fenestram (arrows).
On CT the detection of otosclerosis can be difficult to the inexperienced eye because the spread of the disease is often symmetrical.
A small lucency at the fissula ante fenestram is typical for otosclerosis.
In more severe cases lucencies are also present around the cochlea.
Sometimes the whole otic capsule is surrounded by these 'otospongiotic' foci, forming the so-called fourth ring of Valvassori.
In a minority of patients the disease is unilateral.
This is virtually always limited to a lucency at the fissula ante fenestram.
On the left a 49-year old male with left sided conductive hearing loss.
There is a lucency anterior to the oval window (arrow) and between the cochlea and the internal auditory canal.
This is combined fenestral and retrofenestral otosclerosis.
Same patient.
Notice that the otosclerosis is seen on both sides.
 Metallic stapedial prosthesis. Lucency between vestibule and cochlea as a manifestation of otosclerosis (arrow)
Metallic stapedial prosthesis. Lucency between vestibule and cochlea as a manifestation of otosclerosis (arrow)
On the left a patient with a well-positioned metallic stapedial prosthesis: medially it touches the oval window and laterally it connects with the long process of the incus.
Notice the lucency between vestibule and cochlea as a manifestation of otosclerosis (arrow).
Trauma
On the left images of a 68-year old woman who experienced a traumatic head injury 50 years ago.
Three years ago she was diagnosed with total hearing loss of the right ear.
The image shows a subluxation of the incudomallear joint (arrow).
Left ear for comparison.
Fractures of the temporal bone are associated with head injuries.
The consequences of the intracranial injuries dominate in the early period after the trauma.
A temporal bone fracture can manifest itself with acute signs like bleeding from the ear or acute facial paralysis.
Hearing loss is of course not a life-threatening event.
Temporal bone fractures can be classified as longitudinal or transverse.
Longitudinal fractures generally spare the inner ear, which is more often breached by transverse fractures.
However, many temporal bone fractures are neither longitudinal nor transverse and a comprehensive description of the structures which are crossed by the fracture is needed.
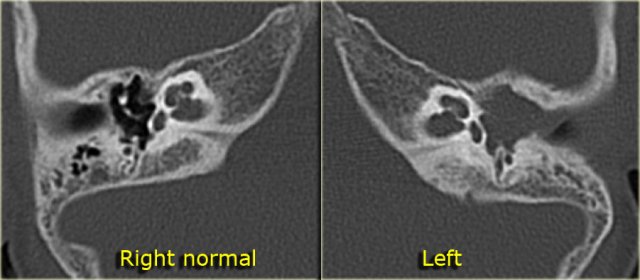
On the left images of a woman who had fallen down from the stairs three days earlier.
She suffered from severe sensorineural hearing loss on the left side.
A longitudinal fracture is visible, which courses anteriorly to the cochlea through the region of the geniculate ganglion (arrows).
There were no signs of facial nerve paralysis.
No fracture line could be seen across the inner ear.
Opacification of the middle ear, likely as a result of a hematotympanum.
Right ear for comparison.
Posttraumatic conductive hearing loss can be caused by a hematotympanum or a tear of the tympanic membrane.
In these cases the hearing loss usually resolves spontaneously.
In persistent conductive hearing loss there is usually a disruption of the ossicular chain.
The most common disruption is a dislocation of the incudostapedial joint which is often a subtle finding.
Disruptions can occur at the incudomallear joint.
Fractures of the long process of the incus or the crura of the stapes are difficult to diagnose.
Fractures of the inner ear are seen in posttraumatic sensorineural hearing loss.
Careful inspection is required in order to pick out these thin fracture lines.
Cochlear concussion with blood in the cochlea can be visualized with MRI.
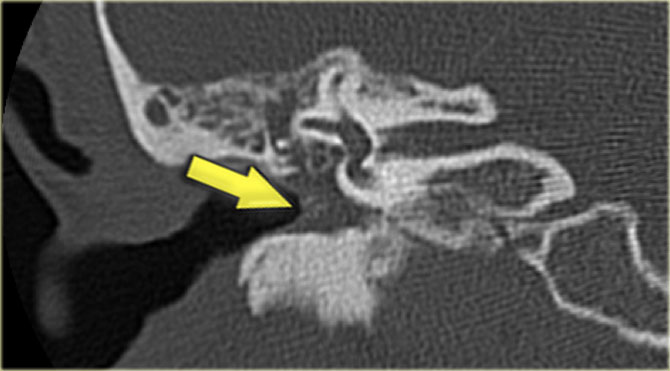
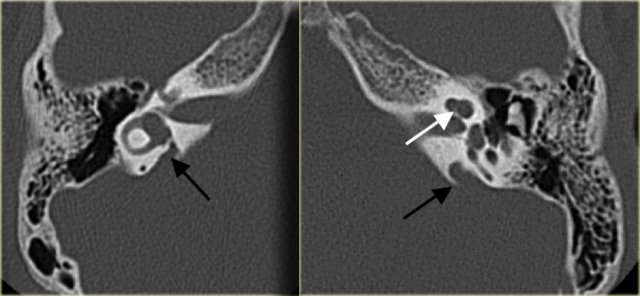
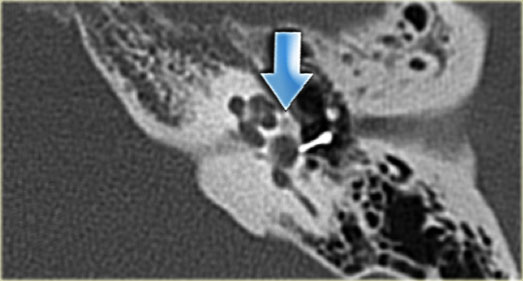
 Longitudinal fracture (yellow arrow) coursing through the mastoid towards the region of the geniculate ganglion. Dislocation of the incus with luxation of the incudo-mallear and incudo-stapedial joint (blue arrow).
Longitudinal fracture (yellow arrow) coursing through the mastoid towards the region of the geniculate ganglion. Dislocation of the incus with luxation of the incudo-mallear and incudo-stapedial joint (blue arrow).
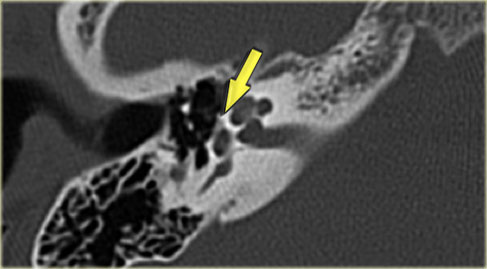
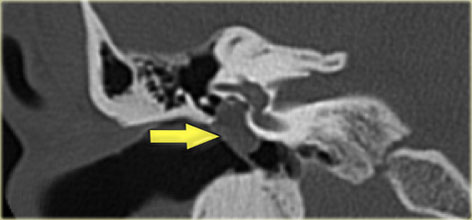
On the left images of a man who had suffered a traumatic head injury two months previously.
He complained of intermittent tinnitus.
There is a longitudinal fracture (yellow arrow) coursing through the mastoid towards the region of the geniculate ganglion.
There is a dislocation of the incus with luxation of the incudo-mallear and incudo-stapedial joint (blue arrow).
No involvement of the inner ear.
Left ear for comparison.
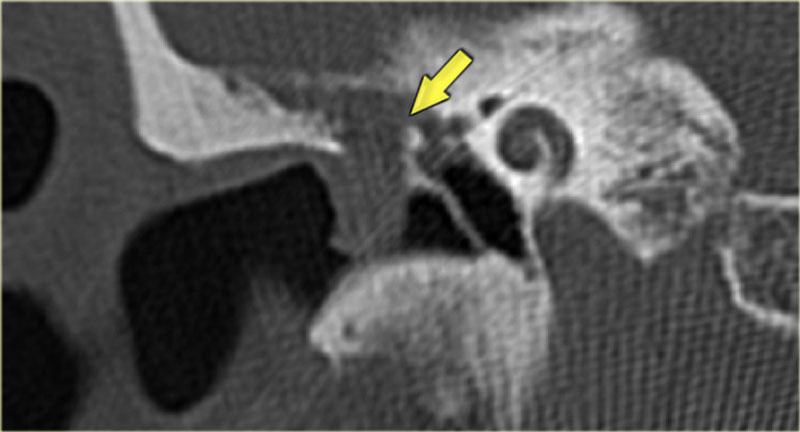
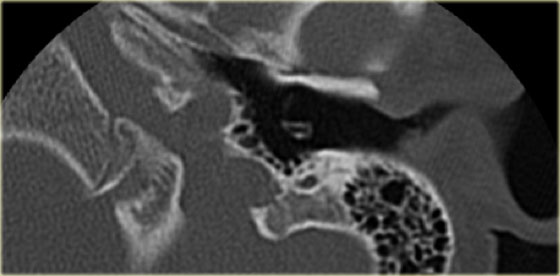
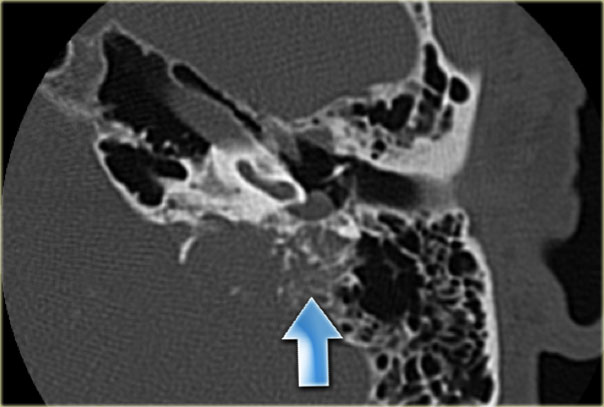
On the left images of a 54-year old male several years after head trauma, followed by left-sided hearing loss. There is a transverse fracture through the vestibule and facial nerve canal (arrows). The lateral semicircular canal is partially filled with dense material, compatible with labyrinthitis ossificans.
Facial nerve paralysis can be acute or delayed.
In acute posttraumatic paralysis a fracture line through the facial nerve canal - usually in the tympanic part - can be observed, sometimes with a bony fragment impinging on the canal.
In delayed facial paralysis the nerve is probably edematous and fracture lines can be absent.
On the other hand, a fracture line may be seen to cross the facial nerve canal without any associated nerve dysfunction.
Several normal structures may be mistaken for fractures:
- Petromastoid (subarcuate) canal
- Cochlear aqueduct
- Cochlear cleft
Vascular anomalies
A vascular anomaly can be suspected if the patient complains of pulsatile tinnitus or when there is a reddish or bluish mass behind the eardrum.
Vascular anomalies are:
- Aberrant internal carotid artery
- Dehiscent jugular bulb
Non-vascular anomalies which can also manifest as a retrotympanic mass:
- Glomus tumor
- Cholesterol granuloma
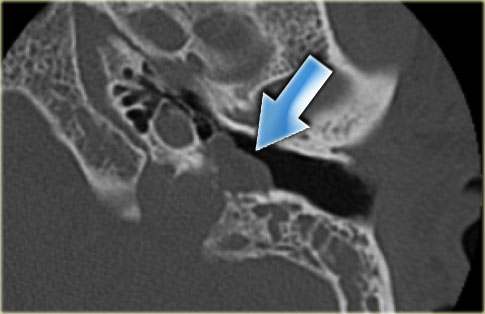
Aberrant internal carotid artery
In patients with an aberrant internal carotid artery the cervical part of the internal carotid artery is absent.
It is replaced by the ascending pharyngeal artery which connects with the horizontal part of the internal carotid artery.
It courses through the middle ear.
On the left coronal images of the same patient.
On the right side the internal carotid artery is separated from the middle ear (blue arrow).
On the left side the internal carotid artery courses through the middle ear (red arrow)
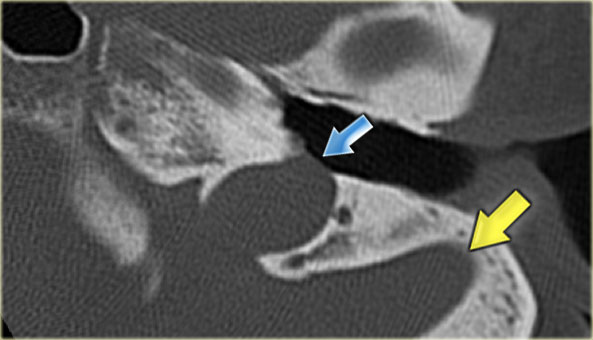
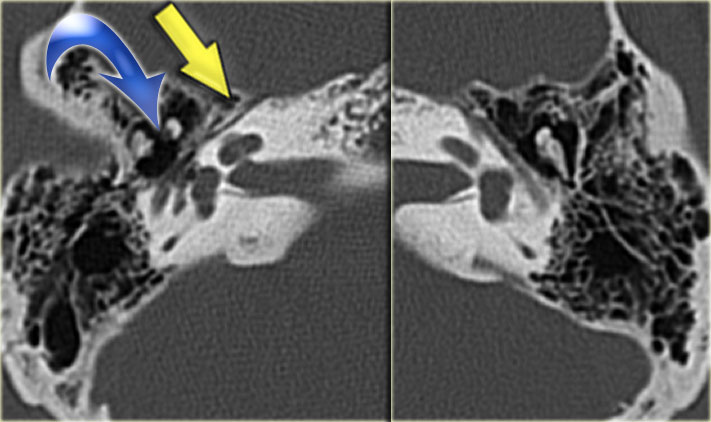
Dehiscent jugular bulb
On the left a dehiscent jugular bulb (blue arrow).
This can be dangerous during myringotomy.
Note also the bulging sigmoid sinus (yellow arrow).
Tumors
Tumors of the temporal bone are rare.
The following tumors can be seen:
- Exostoses
- External auditory canal carcinomas
- Glomus tumor
- Adenoma
- Congenital cholesteatoma
- EndoLymphatic Sac Tumor (ELST)
Schwannomas will not be discussed
Exostoses
On the left bilateral bony lesions of the external auditory canal, typical of exostoses.
Exostoses of the external auditory canal are usually multiple, sessile, and bilateral and can cause severe narrowing of the external auditory canal.
Exostoses are caused by contact with cold water and mostly seen in swimmers and surfers.
Osteomas are less common and mostly unilateral and pedunculated.
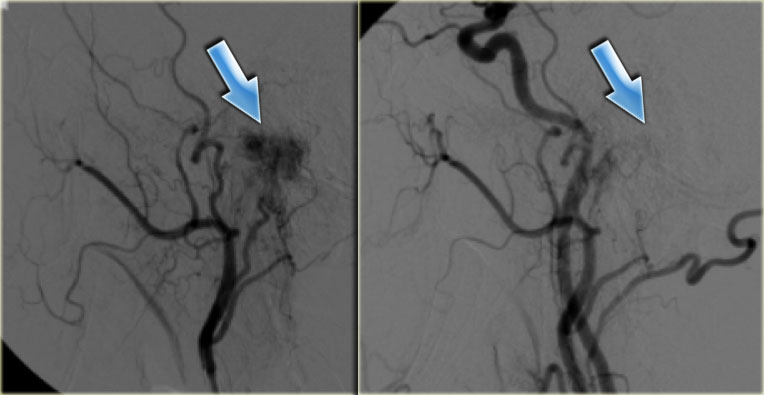
Glomus tumor
On the left images of a 57-year old male with a slowly progressive glomus jugulotympanicum tumor, visible as a mass on the floor of the tympanic cavity (arrow).
Mucus is seen in the meso- and epitympanum.
At CT, the glomus jugulotympanic tumor manifests as a destructive lesion at the jugular foramen, often spreading into the hypotympanum.
The bone can be permeated by tumor.
The glomus tympanicum tumor is typically a small soft tissue mass on the promontory.
Large tumors have a 'salt and pepper' appearance at MRI due to their rich vascularity with flow voids.
They enhance strongly after i.v. contrast.
Embolization
can diminish intra-operative blood loss.
On the left angiographic
images of the left external carotid artery before embolisation and the common
carotid artery after embolization (blue arrow).
Only a faint blush remains.
Glomus tumors arise from paraganglion cells which are present in the jugular foramen and on the promontory of the cochlea around the tympanic branch of the glossopharyngeal nerve.
Elderly persons are most commonly affected with a female predominance.
The presenting symptoms are conductive hearing loss, tinnitus, and pain.
At otoscopy a blue ear drum is seen.
Glomus tumors of the jugular foramen (also called glomus jugulotympanicum tumors) are more common than tumors which are confined to the middle ear (glomus tympanicum tumor)
 EndoLymphatic Sac Tumor: destructive process of the dorsal temporal bone, with some calcification (arrow). The location, destruction, and calcification are typical for ELST. A small extension of the tumor into the middle ear is present
EndoLymphatic Sac Tumor: destructive process of the dorsal temporal bone, with some calcification (arrow). The location, destruction, and calcification are typical for ELST. A small extension of the tumor into the middle ear is present
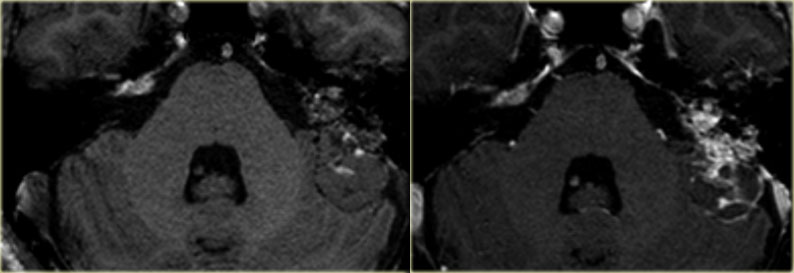
EndoLymphatic Sac Tumor (ELST)
ELST is a rare entity.
These tumors originate from the endolymphatic sac.
We will discuss them because their CT appearance is very typical.
At CT a destructive process is seen on the dorsal surface of the petrosal part of the temporal bone with punctate calcifications.
On MRI there is usually strong enhancement.
The amount of destruction in this case would be atypical for a meningioma.
On the left a large destructive process of the dorsal temporal bone.
Parts of the tumor show strong enhancement.
There is a cystic component on the dorsal aspect which does not enhance.
Notice the cystic component of the tumor on a T2W-image
Postoperative ear
The postoperative ear is often difficult to describe.
A previous CT-examination, if present, can be a lot of help.
The best one can do is to describe the extent of the previous operation, the state of the ossicular chain (if present), and the aeration of the postoperative cavity.
This cavity can be filled with swollen mucosa, recurrent disease or with some tissue implanted during the operation.
Attico-antrotomy
On the left images of a 15-year old girl with chronic otitis media, who was treated with an attico-antrotomy.
An entry into the antrum is created, but most of the mastoid air cells are still present.
The ossicular chain is preserved.
On the left coronal images of the same patient.
Notice the thickened and calcified eardrum.
Mastoidectomy
On the left images of a 42-year old male who was treated with a mastoidectomy.
The posterior wall of the external auditory canal and the ossicular chain are intact.
Almost all of the mastoid air cells are removed.
On the left coronal images of the same patient.
The posterior wall of the external auditory canal and the ossicular chain are intact.
Almost all the mastoid air cells are removed.
Tympanostomy tubes
If the Eustachian tube is assumed to be dysfunctioning, tympanostomy tubes can be inserted into the eardrum to facilitate the drainage of middle ear fluid.
In young children the course of the Eustachian tube between the middle ear and the nasopharynx runs more horizontally than in adults, predisposing to stasis of fluid in the middle ear and secondary infection.
After a while tympanostomy tubes are extruded by the eardrum and can be seen to lay in the external auditory canal.
The image on the left shows a dislocated tube lying in the external auditory canal.
Stapes prosthesis
Stapes prostheses are inserted in patients with otosclerosis to replace the native stapes, which is fixed in the oval window.
Steel stapes prostheses are easily visible.
Prostheses made of Teflon can be almost invisible.
One should describe the position of the prosthesis in the oval window and the integrity of its connection with the long process of the incus.
On the left images of a metallic stapes prosthesis.
The prosthesis is in a good position.
Medially it lies in the oval window, laterally it connects to the long process of the incus.
On the left a patient with a stapes prosthesis.
The metallic prosthesis is dislocated and lies in the vestibule.
A re-operation was performed and a new prosthesis was inserted.
Notice the small lucency at the fissula ante fenestram, a sign of otosclerosis (arrow).
On the left images of a patient with a synthetic stapes prosthesis.
It is connected to the long process of the incus (yellow arrow).
The tip lies in the oval window (blue arrow).
Incus interpostion
A remodelled incus can be used to repair the ossicular chain.
Most often it is inserted between the eardrum and the stapes superstructure.
The interposed incus can either be the patient's own or one from a cadaver.
Alternatively, a Partial Ossicular Replacement Prosthesis (PORP) or Total Ossicular Replacement Prosthesis (TORP) can be used.
On the left images of a 13 -year old boy.
Five years earlier a cholesteatoma was removed.
The following year the ossicular chain was reconstructed with a donor incus (arrow).
The malleus handle is present.
On the left coronal images of the same patient.
On the left axial images of a patient with a reconstruction of the ossicular chain with an autologous incus (arrow) between the ear drum and the stapes.
Postoperative meningocele
In postoperative imaging look for dehiscence of the bony covering of the sigmoid sinus and for interruption of the tegmen tympani.
A herniation of cranial contents can be present.
If the tegmen is disrupted and continuous soft tissue is present between the middle ear and the cranial contents, MRI can be used to demonstrate if there is a postoperative meningo (encephalo)cele.
On the left images of a 24 year old female.
She was operated at the age of 8 for chronic otitis media.
Since one year progressive hearing loss of the right ear.
CT shows a rounded mass (arrow) in the attico-antrotomy with erosion of the tegmen tympani.
An MRI depicts a mass in the mastoid abutting the dura.
At operation a large cholesteatoma was removed.
The dura was intact.
The defect was closed with a flap of the temporal muscle and a chain reconstruction was performed.
On the left an MRI image of the same patient.
The MRI depicts a mass in the mastoid abutting the dura.
The dura is intact.
Cochlear implants
Cochlear implantation is performed in patients with sensorineural deafness due to degeneration of the organ of Corti.
After implantation of a multichannel electrode a wide array of electrical pulses can be produced to stimulate the acoustic nerve.
The electrode is inserted into the scala tympani of the cochlea via the round window or via a drill hole directly into the basal turn (cochleostomy).
Post-operatively its position can be evaluated with CT.
Images
Eight-year-old boy with bilateral cochlear implants. Normal position in the right ear.
A well-inserted electrode is positioned with all its channels, visible as a string of beads, in the cochlea and spirals up in the direction of the cochlear apex.
Continue with the images of the left ear.
Malpositioned implant
case 1
The images show the left ear of the same patient were hearing was impaired.
The implant is not inserted deep enough, five
channels lie in the middle ear and the tip of the implant does not reach the
cochlear apex.
case 2
These images show an implant which is malpositioned.
The cochlear implant is inserted below the basal turn of the cochlea and ends up in the region of the geniculate ganglion.
Criteria for cochlear implantation are:
- Well pneumatized mastoid
- No signs of middle ear inflammation
- No calcification of the cochlea
MRI can demonstrate fibrous obliteration of the
cochlea, something which is not appreciated on CT.
MRI, on the other hand, can show a
fluid-filled cochlea while CT depicts small calcifications.
Therefore, a combination of both
modalities can be used.
MRI can also demonstrate absence of
the 8th nerve, which precludes cochlear implantation.
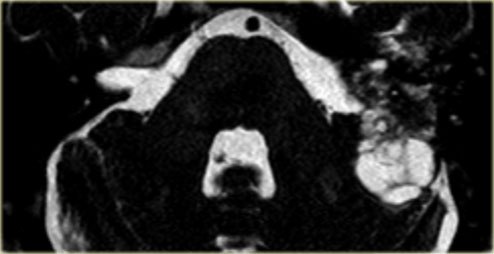
Labyrinthitis ossificans
Labyrinthitis ossificans is seen after meningitis.
It is a condition in which the inner ear is filled with fibrotic tissue, which calcifies.
It mostly affects the cochlea, but the vestibule and semicircular canals can also be involved.
On the left images of a 56-year old male, who is a candidate for cochlear implantation.
Small calcification in basal turn of cochlea as a result of labyrinthitis ossificans (arrows).
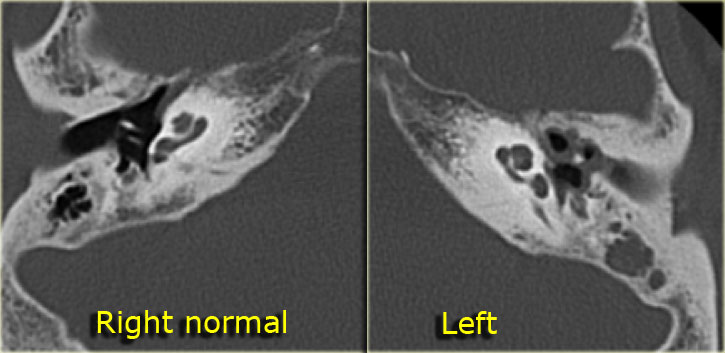
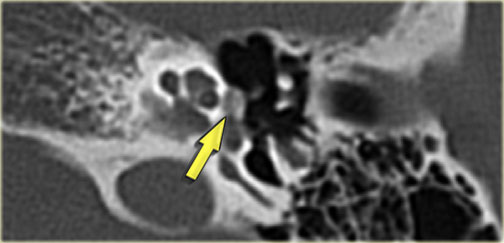
On the left images of a 14-year old boy with bilateral sensorineural hearing loss.
Calcification of superior semicircular canal on the left (yellow arrow).
Right ear for comparison (blue arrow).
On the left coronal images of the same patient.