Vascular Anomalies of Aorta, Pulmonary and Systemic vessels
Marilyn J. Siegel and Robin Smithuis
Mallinckrodt Institute of Radiology, Washington University School of Medicine in St. Louis, USA and the Rijnland Hospital in Leiderdorp, the Netherlands
Publicationdate
This review is based on a presentation by Marilyn Siegel and was adapted and illustrated for the Radiology Assistant by Robin Smithuis.
Marilyn Siegel is specialized in pediatric and chest radiology.
The second edition of her book entitled Pediatric Body CT will be out next week.
In this review we will discuss the most common vascular anomalies of the aorta, pulmonary vessels and systemic veins in the chest.
Most of these anomalies are found in children, but sometimes they are discovered later in adulthood.
Many of these anomalies are asymptomatic or 'leave alone' lesions, but some of these anomalies are symptomatic and need to be treated.
As a radiologist we have to be familiar with these anomalies.
A simple mouse click on an item on the left will bring you directly to this subject.
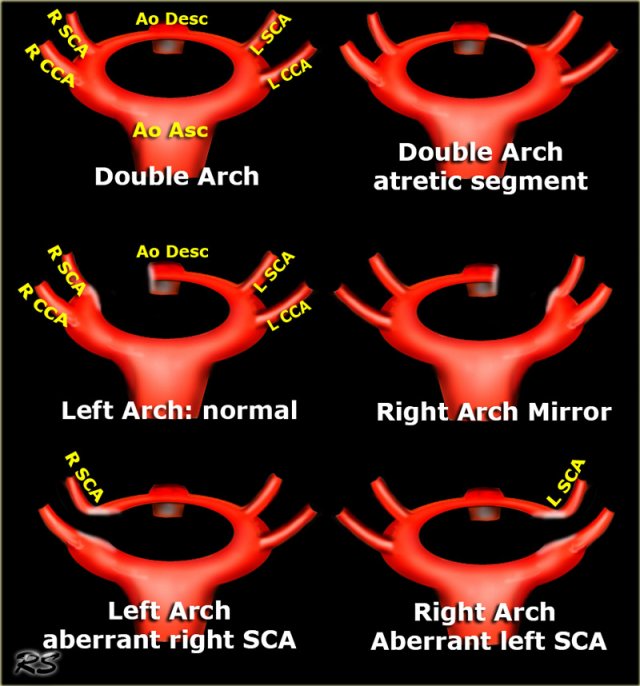
Overview of Arch Anomalies
- Aberrant Right subclavian artery
Most common arch anomaly.
Not a true ring.
Usually asymptomatic.
Sometimes dysphagia lusoria when dilated suvclavian artery compresses esophagus posteriorly. - Innominate artery compression syndrome
In children the brachiocephalic (innominate) artery is located more to the left and may compresses the trachea anteriorly. - Right Arch Mirror Image
Mirror-image variety of the left arch.
Asymptomatic.
Associated congenital heart disease in 98%, mostly tetralogy of Fallot. - Right Arch with Aberrant left subclavian
Left subclavian artery is the last branch.
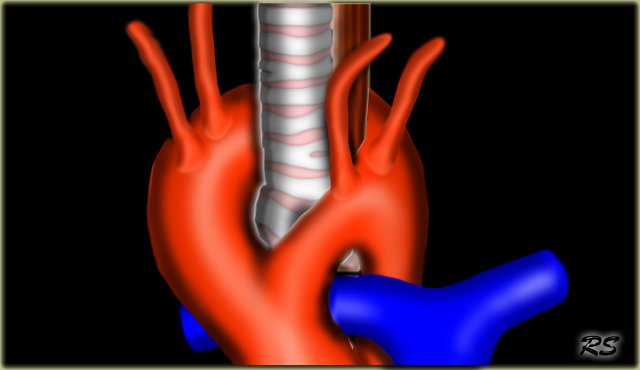
Obstructing anomaly. - Double Aortic Arch
Complete ring encircles esophagus and trachea.
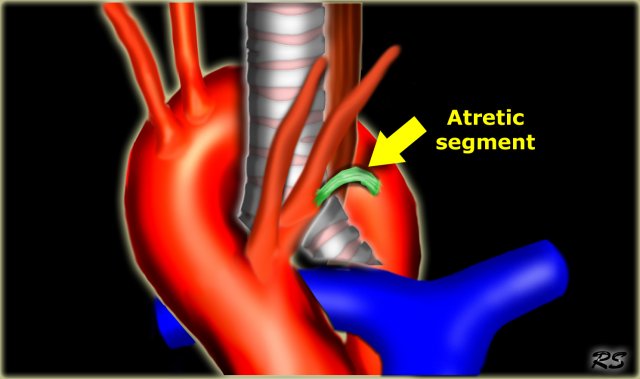
Four vessel sign. - Double Arch with Atretic Segment
Left arch is very small and has atretic posterior segment.
Still a four vessel sign.
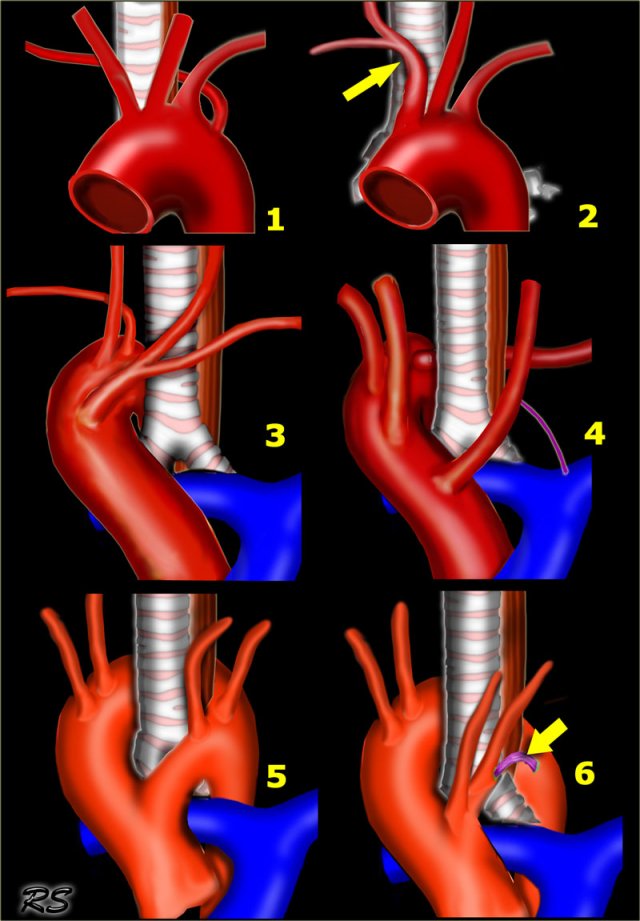
Embryology
- Double Arch:
- In the embryo a double arch with two brachiocephalic vessels on each side is present.
- If double aortic arch persists, it forms a vascular ring around trachea and esophagus.
- Double Arch with Atretic Segment:
- Posterior part of the left arch becomes atretic.
- This nonpatent remnant persists as a fibrous cord tethering the anterior left arch to the descending aorta.
- Normal Left Arch:
- The posterior part of the right arch involutes.
- The two brachiocephalic vessels on the right form the right innominate artery.
- Right Arch with mirror branching:
- Mirror image of normal left arch.
- Posterior part of the left arch involutes.
- The two brachiocephalic vessels on the left form the left innominate artery.
- Left Arch with aberrant right subclavian artery:
- Right arch between the right subclavian and right common carotid artery involutes.
- First branch is the right common carotid, followed by the left carotid and the left subclavian artery. The last branch is the right aberrant subclavian artery.
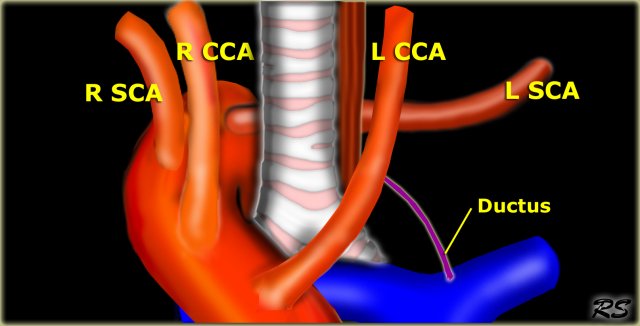
- Right Arch with aberrant left subclavian artery:
- Mirror image of the left arch with aberrant right subclavian artery.
- Left arch between the left subclavian and left common carotid artery involutes.
- First branch is left common carotid, followed by right carotid and right subclavian artery. The last branch is the left aberrant subclavian artery.
When you look at these illustrations, you have to realize, that these are views from above, while CT-images have a 'view from feet'.
On a CT-image the ascending aorta will be on the upper part of the image and the descending aorta will be on the lower part.
Aortic Arch Anomalies
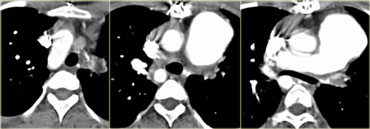
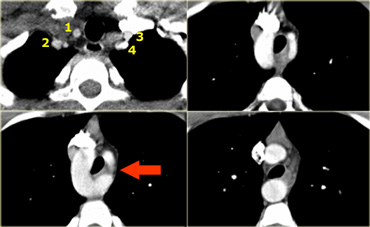
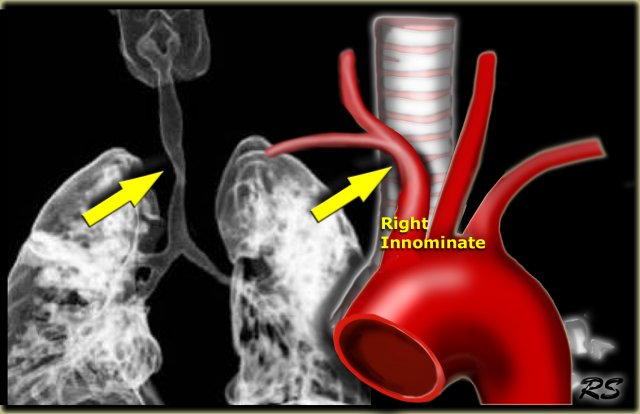
Right Arch Mirror Image
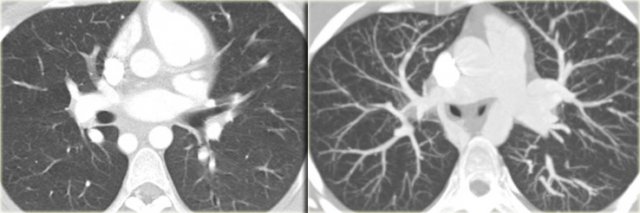
This is the mirror-image variety of the left arch.
On the left a 2 year old girl with wheezing and coughing.
Study the images and then continue.
You have to realize, that axial CT-images are viewed from the feet, while the illustrations above are viewed from above
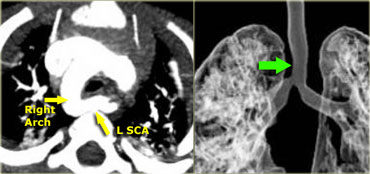
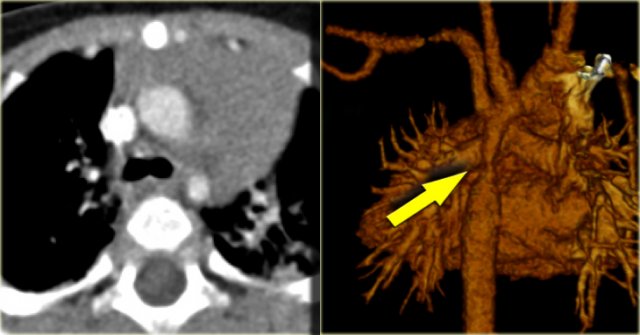
On the axial image there is a right arch
On the volume rendered image there is mirror image branching of the brachiocephalic arteries, no aberrant subclavian artery, so this is a right arch mirror image.
This anomaly is asymptomatic, because there is no obstructing ring.
Almost all of these patients however come to our attention because they have associated congenital heart disease in 98% of cases.
This patient had a mirror image aortic arch and a VSD.
On the left an adult who was operated in his childhood for a Tetralogy of Fallot (pulmonary stenosis, right ventricular hypertrophy, VSD, overriding aorta).
At surgery the VSD was patched and the pulmonary outflow tract was enlarged.
Notice that there is also a right arch.
In the United States there are now more than one million adults who have survived their congenital heart disease.
In the ER you will see these patients because they age and get chest pain like many adults do and so you will see these anomalies more frequently.
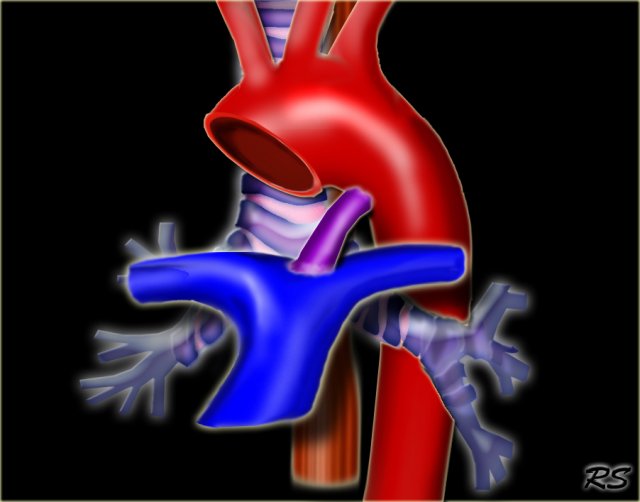
Right Arch with Aberrant left subclavian
The Right Aortic Arch with an aberrant left subclavian is an obstructing arch anomaly.
The first branch of the aorta is the left common carotid, followed by the right subclavian artery and the left common carotid.
This also is a true ring.
The ligamentum ductus arteriosus between the arch at the level of the left subclavian artery and the left pumonary artery completes the ring.
If this ligament is very short, there will be a lot of compression.
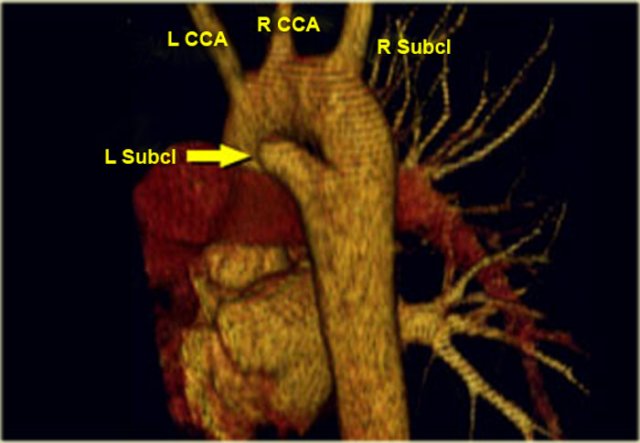
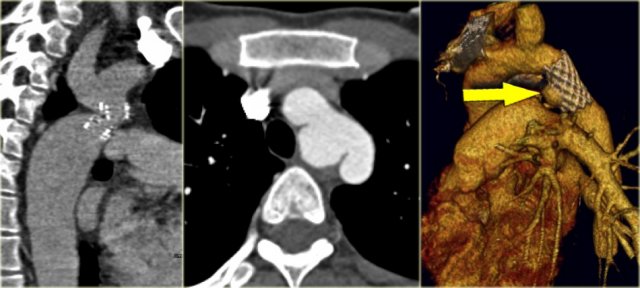
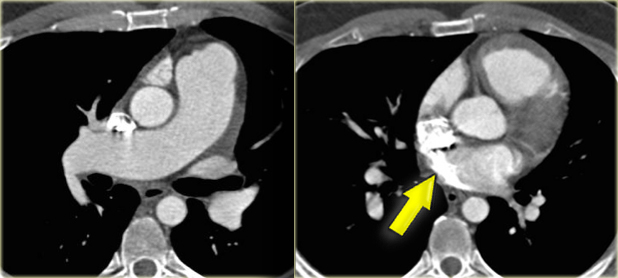
On the left a patient with a right arch with an aberrant left subclavian (indicated by the yellow arrow).
Scroll through the images on the left.
Again you have to realize that the axial CT-images have a 'view from feet'.
Which vessels are indicated by the yellow and green arrow?
There is a right arch and the left subclavian artery is the last branch of the aortic arch, indicating that this is an aberrant left subclavian.
Medially to the left subclavian artery we see the left common carotid, that originates from the right side and has an oblique course to the left.
The yellow arrow indicates the azygos vein.
The green arrow indicates the left superior intercostal vein, a normal variant, that we will discuss later.
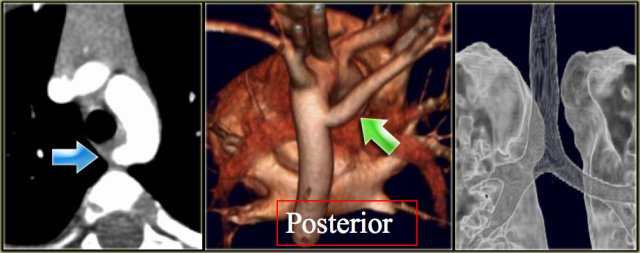
Same patient.
Posterior oblique view of volume rendered image to show the aberrant left subclavian artery.
In a mirror type right arch, the left subclavian is the first brach and forms the left innominate together with the left common carotid.
On the left images of a symptomatic child.
On the axial image there is a right arch with the left subclavian artery that comes off on the posterior side and runs behind the trachea and the esophagus.
The compression of the trachea is demonstrated on the volume rendered view.
Double Aortic Arch
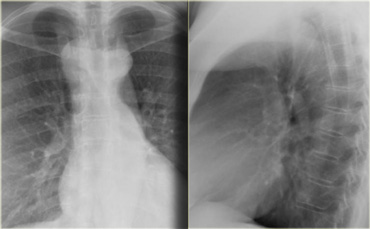
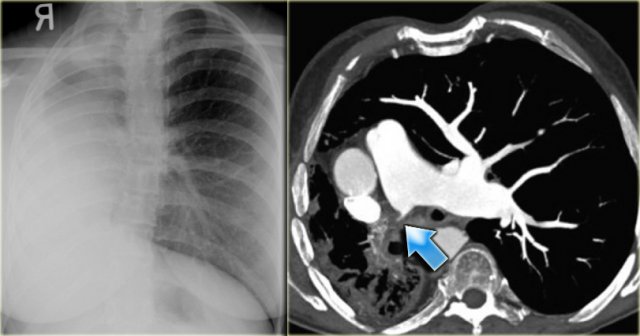
On the left a chest film of a 6-month old boy with stridor and cough.
The trachea is deviated to the left, otherwise the chest film is normal.
So there is some mass effect on the right side.
On the left the reconstructions demonstrating a double aortic arch.
There are branches coming off the right arch and branches coming off the left arch.
The right arch is typically larger and higher than the left.
There is a complete ring that encircles the esophagus and the trachea and usually there is stridor or dysphagia.
Two brachiocephalic arteries arise on each side separately (four vessel sign).
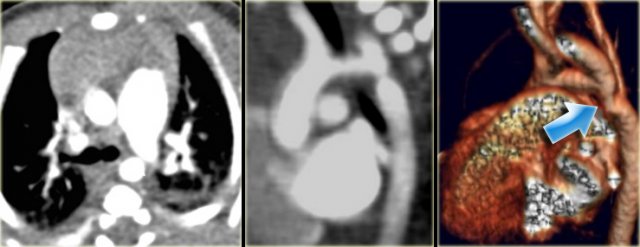
On the left a chest film of a young adult with a cough.
There is a right paratracheal mass.
The differential diagnosis is tumor, adenopathy or vessel (right arch, dilated azygos vein, dilated aberrant right subclavian artery).
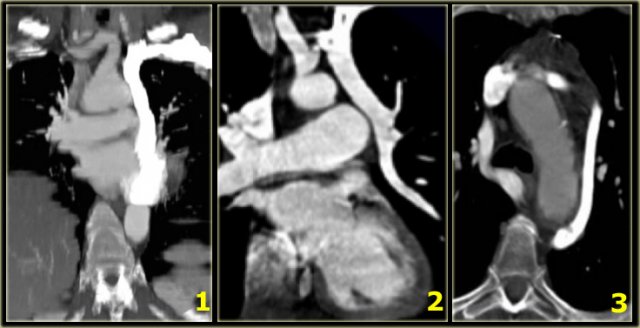
On the left axial images and posterior view of volume rendered reconstruction.
Describe the findings and then continue.
The findings are:
- four vessel sign
- double arch
- right arch higher and larger
- esophagus and trachea are completely encircled
The narrowing of the trachea is seen on the axial images, but better appreciated on the MPR and Volume Rendered image.
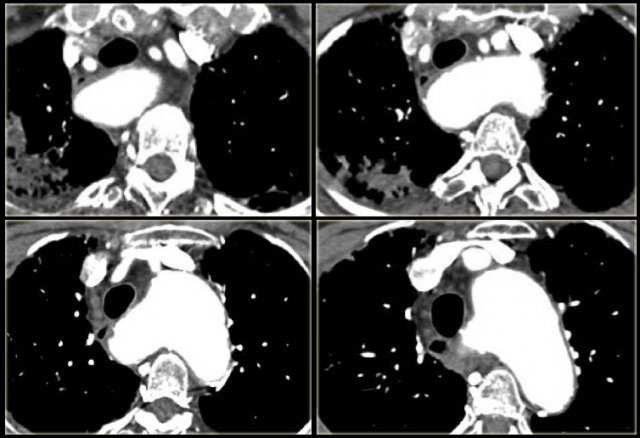
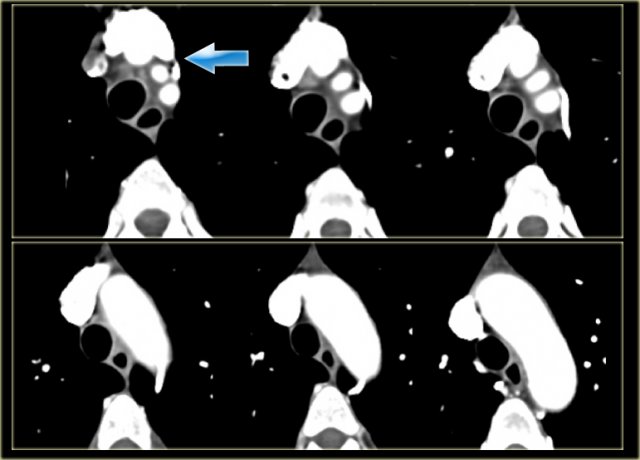
On the left preoperative and postoperative MDCT studies of a 2-month-old female infant with double aortic arch presenting with stridor and repeated apnea.
The smaller left arch is partially resected.
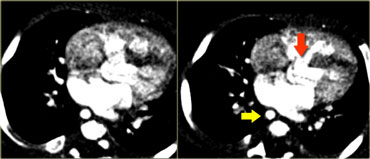
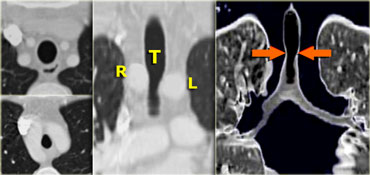
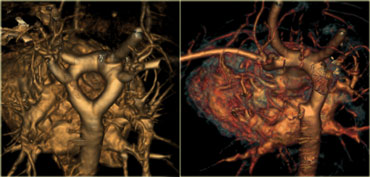
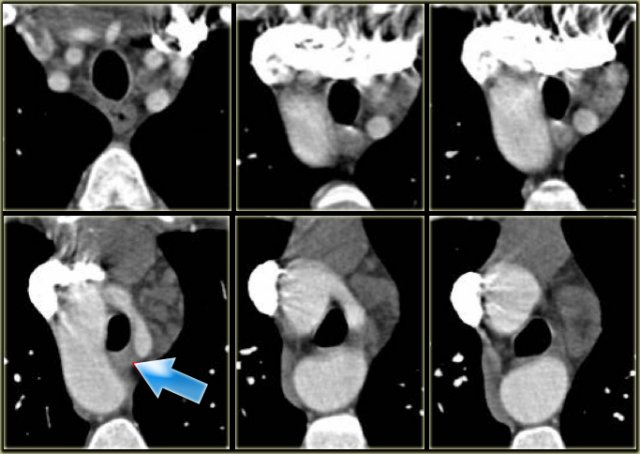
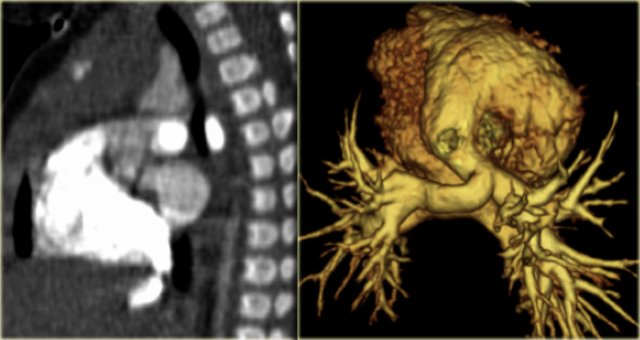
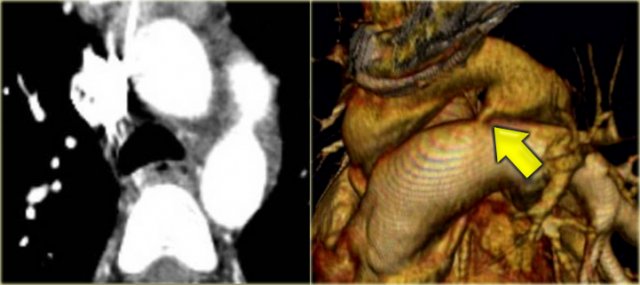
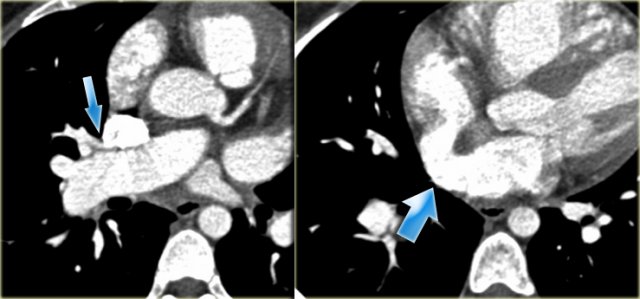
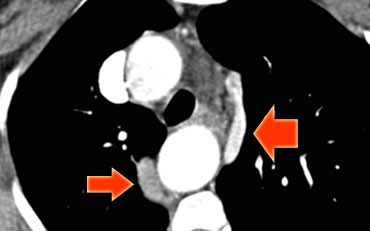
Double Arch with Atretic Segment
Occasionally the double arch can have an atretic segment.
You should not confuse it for a right arch.
The left arch is just very small and there is still a four vessel sign.
On the left a dominant right arch and a small left arch.
The atretic segment is marked by the arrow.
Notice the four vessel sign.
On a posterior view the interruption is nicely demonstrated.
Remember that there is still a ring, so there is still obstruction.
Another case on the left.
Do not call this a right arch.
It still is a double arch and there is a atretic fibrotic segment on the posterior side of the left arch, that completes the ring.
Notice the four vessel sign.
Same patient.
Always look at the airways.
On the recoonstruction the impression on the trachea is better appreciated.
Left Arch Aberrant Right SCA
- Also known as arteria lusoria.
- Most common arch anomaly.
- Not a true ring
- Usually asymptomatic.
On the left a young patient, who has a CT for another reason.
Study the images and then continue.
Notice that there is a left arch, but the right subclavian artery is the last brachiocephalic artery to branch off the arch.
Only rarely these patients become dysphagic (dysphagia lusoria) , when the origin of the right subclavian artery becomes dilated.
On a barium study of the esophagus you will see a posterior impression with an oblique course directed towards the right shoulder.
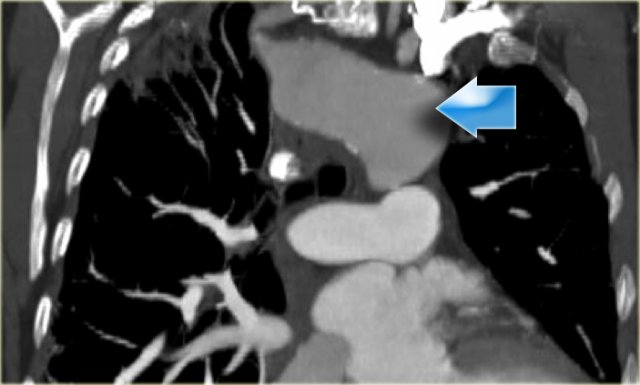
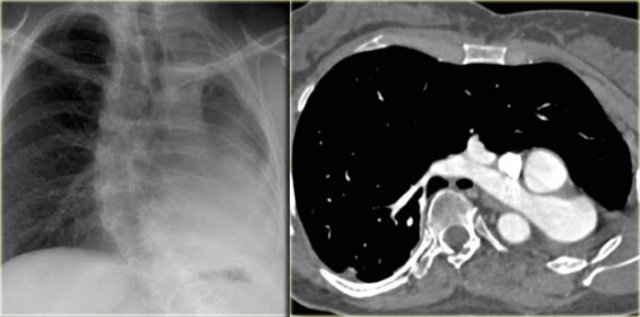
On the left a 78 year old woman with dysphagia.
There is consolidation in the right upper lobe, maybe due to aspiration.
There is a dilated vessel that compresses the esophagus and it originates from the left-sided aorta, i.e. an aberrant right subclavian artery.
On the left the same patient with dilated aberrant right subclavian artery.
Coronal reconstruction.
On the left another patient with an aberrant right subclavian.
Scroll through the images.
When you follow the artery from inferior to superior, it starts on the left side of the arch and travels obliquely behind the esophagus to go to the right.
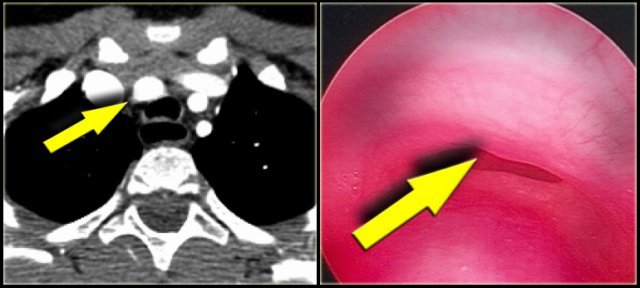
Innominate artery compression syndrome
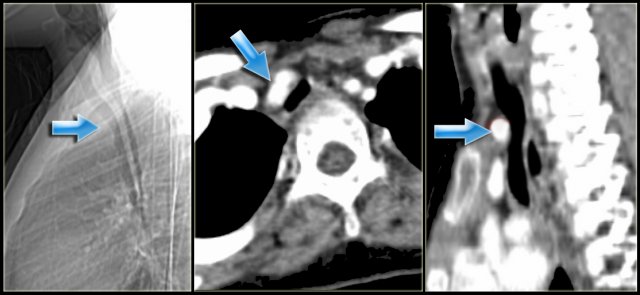
On the left a sagittal scanogram, axial image and sagittal reconstruction of a 5 year old girl with noisy breathing and occasional episodes of cyanosis.
First look at the images then continue.
The findings are:
- anterior compression of the trachea
- brachiocephalic (innominate) artery is located more to the left and compresses the trachea
The diagnosis is the innominate artery compression syndrome.
In infants the innominate artery arises more to the left than in adults, so it's got to go in front of the trachea.
It may compress the trachea, leading to stridor, cough and dyspnea.
This compression decreases with age and these patients will outgrow it.
The compression in the innominate artery compression syndrome is located on the right anterior side and at the level of the thoracic inlet.
This is much higher than in the double arch or Right Aortic Arch with Aberrant left subclavian
On the left another case with mild compression on the trachea.
Aortic Coarctation
- Narrowing at level of distal arch / descending aorta.
- Chest film: 'figure 3' sign, inferior rib notching.
- Intervention when gradient > 20 mm Hg.
- Associated with bicuspid aortic valve (75%), cerebral aneurysms (5-10%) and Turner syndrome (20% have coarctation)
On the left a 2 month old boy with heart failure.
First study the image, then continue
The findings are:
- Large thymus which is normal for a 2 month old.
- Striking discrepancy between diameter of ascending and descending aorta.
The diagnosis is coarctation, which is nicely demonstrated on the posterior view of the reconstruction.
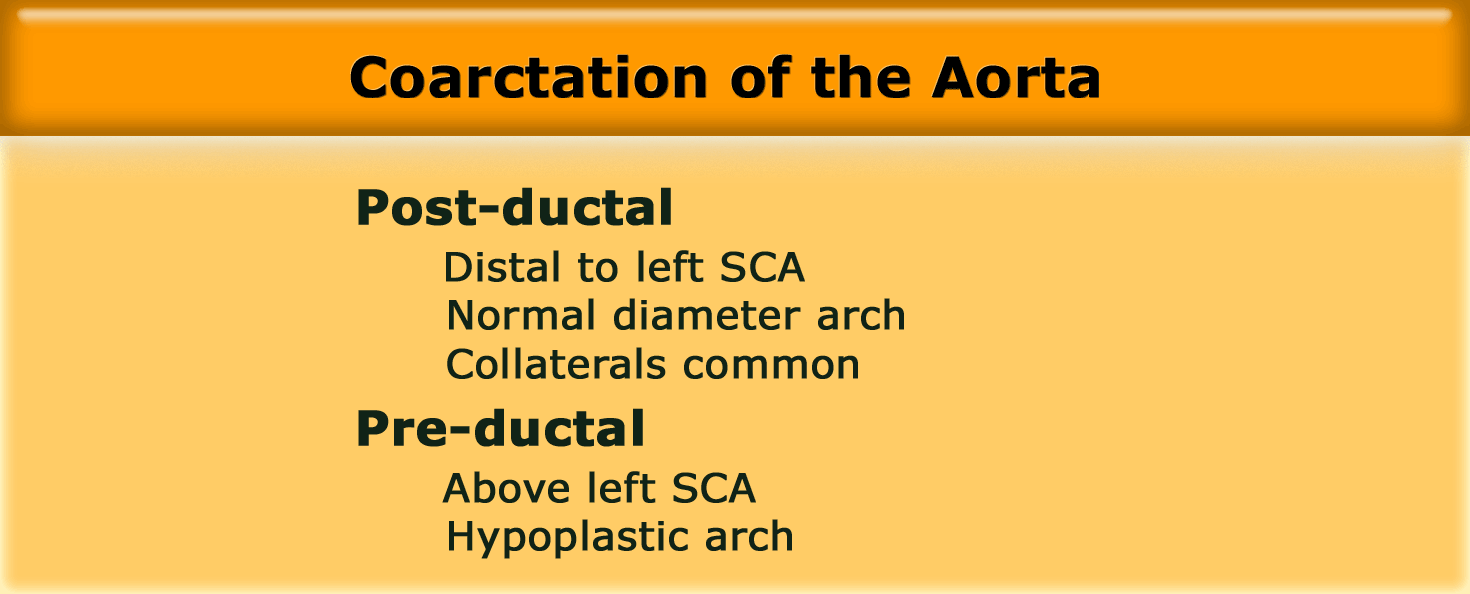
There are two types of coarctation.
The type we usually see is the post-ductal type, which is distal to the left subclavian artery.
The uncommon pre-ductal type is seen in neonates.
They present with severe heart failure, mostly within the first week of life, usually on the first day.
The occlusion is in front of the left subclavian.
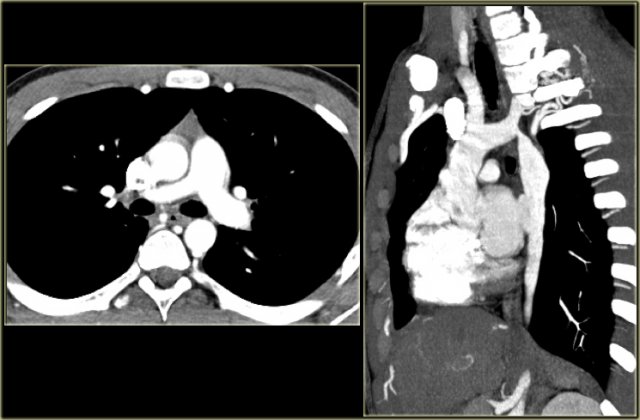
First study the axial image followed by the sagittal reconstruction, then continue.
The findings are:
- Big internal mammarian arteries on the axial image due to a high grade stenosis as a result of a coarctation. Probably could not make the diagnosis based on the axial images alone.
- Post-ductal coartation only seen on sagittal reconstruction.
- Intercostal collaterals.
The intercostal collaterals typically occur between the 3rd and the 8th rib.
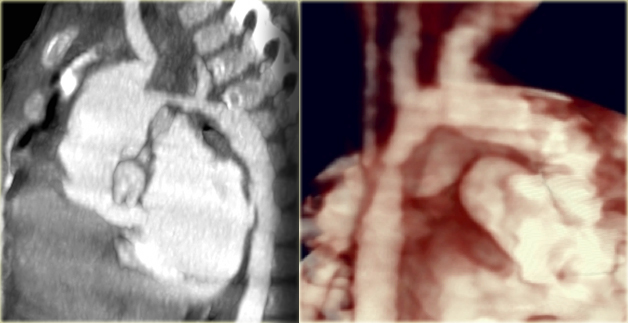
On the left two neonates with the pre-ductal type of coarctation.
The stenosis is in front of the left subclavia and there is arch hypoplasia.
Collaterals do not occur, probably because they don't have time to develop.
Coarctation is treated with angioplasty, stent placement or patch aortoplasty.
The image on the far left is the result after angioplasty.
Next to it a patient who was treated with a stent.
Notice that the stent is obstructing the orfice of the left subclavian artery.
On the far left a patient who was treated with a stent.
The stent ruptured causing restenosis.
Next to it two patients with pseudo-aneurysm.
One after angioplasty and another who developed a pseudo-aneurysm after stent placement.
They have to be repaired because they will rupture.
Pseudo-aneurysms are seen in
- 10% after angioplasty.
- 30% after patch aortoplasty.
Pulmonary arterial anomalies
They most common anomalies of the pulmonary arteries are listed in the table on the left.
Pulmonary agenesis
- Also called congenital interruption of the pulmonary artery.
- Unilateral absence of the pulmonary artery.
- Small lung and hilum.
- Compensatory hyperinflation of contralateral lung with herniation.
On the left a young adult, who had cyanotic spells as a child.
She is now in good health and comes in for another reason.
On the chest film the differential is atelectasis, pneumonia or maybe a tumor.
The CT shows, that he right lung is not developed and the space around the atresic pulmonary artery is filled with fibrofatty tissue with collaterals.
So this is pulmonary agenesis.
If many collaterals develop there will also be some development of the lung.
On the left another case of absent pulmonary artery with absence of lung development.
On the CT the left lung is absent.
These patients may be totally asymptomatic.
Pulmonary Sling
On the left a 4 month old girl with abnormal echo, benign heart murmur and no respiratory or feeding difficulties.
The sagittal reconstruction shows an anomalous vessel on the posterior side of the trachea.
There is a little mass effect on the trachea.
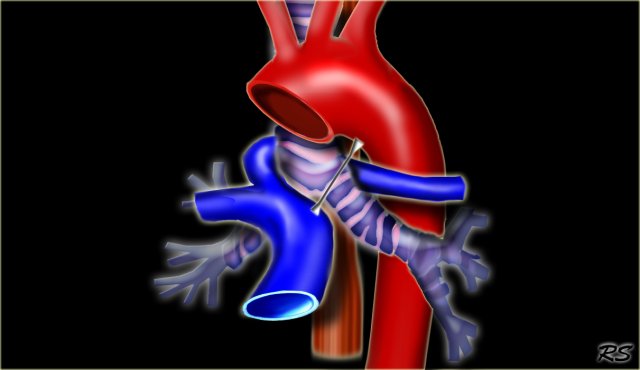
In pulmonary sling the left PA originates from the right PA and courses between the esophagus and the trachea, where it compresses the right main bronchus.
Pulmonary sling is seen more frequent in children as it is more symptomatic than in adults, because the chest is smaller, but you can also encounter it in adults.
On the left images of a child with wheezing and dyspnea.
The left PA comes off the right PA and runs between the esophagus (with nasogastric tube) and the trachea.
Some of these patients also have long segment stenosis in the trachea because of cartilagenous rings.
Patent Ductus Arteriosus
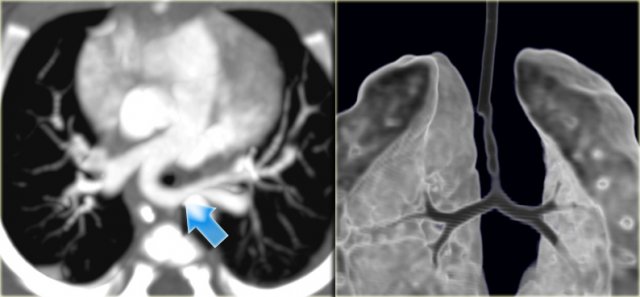
On the left an adolescent with a murmur.
On axial image and reconstruction the patent ductus arteriosus is seen.
The ductus arteriosus is the communication between the pulmonary artery and the proximal descending aorta.
It shunts blood in utero from the right ventricle to the aorta to bypass the non-functioning lungs.
On the first day of life there is a functional closure and an anatomic closure with fibrosis in the first two weeks.
If it does not close these patients come to attention either with a murmur or later with pulmonary hypertension.
On the left a young adult with a murmur.
The cardiologists are not interested in the flow direction, but just want to confirm the diagnosis.
Notice the connection between the pulmonary artery and the descending aorta.
When the duct closes it may also calcify.
This a normal variant.
Pulmonary venous anomalies
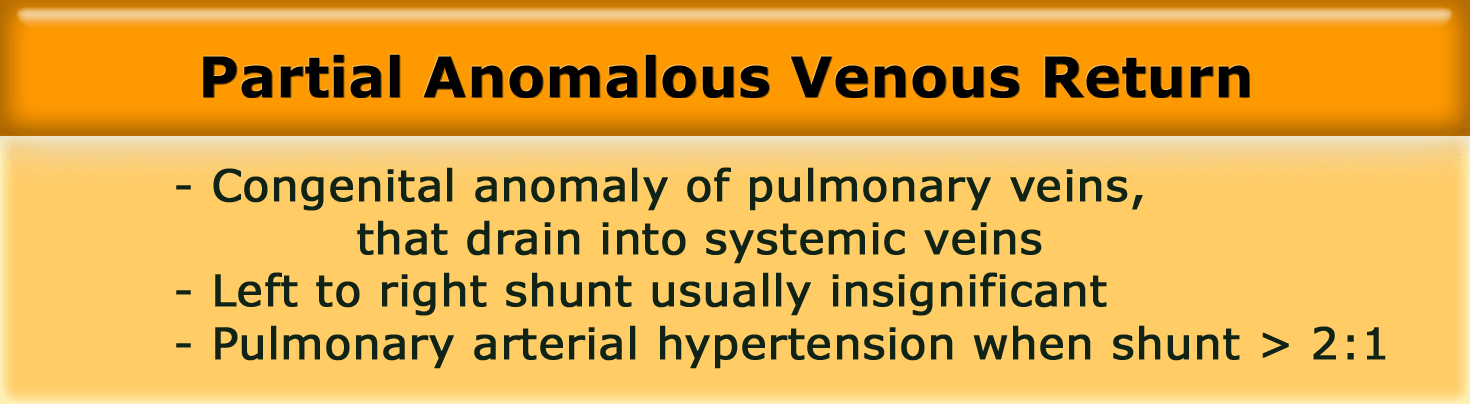
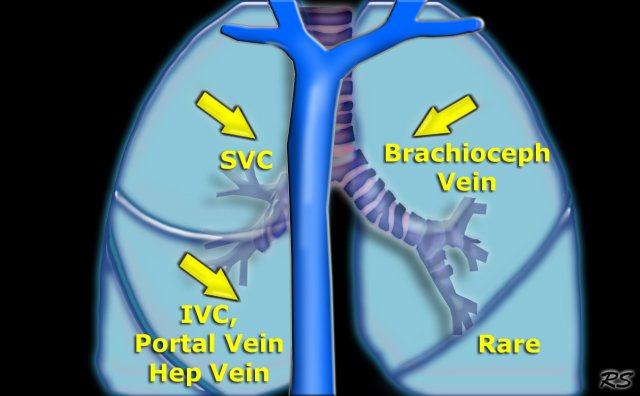
Partial Anomalous Venous Return
The most common features of Partial Anomalous Venous Return are listed in the table on the left.
The anomalous veins drain into the following structures:
- RUL: SVC association with sinus venosus-type ASD.
-
RLL: IVC (usually), sometimes Portal or Hepatic vein.
Can be isolated finding or combined with pulmonary hypoplasia (Scimitar syndrome). - LUL: Brachiocephalic vein (isolated finding).
- LLL: rare (if you find a case publish it).
Right upper lobe anomalous venous return
On the left a 2 month old, who is asymptomatic but has a murmur on physical examination.
There is a connection between the SVC and a pulmonary vein, so this is an anomalous venous return.
All these partially anomalous pulmonary venous returns are left to right shunts, but when small, they are clinically insignificant.
When there is a significant shunt, they may cause (late) pulmonary hypertension as seen in the case on the left.
The chest film in this adult shows large pulmonary arteries and a large right atrium and ventricle as a result of pulmonary hypertension.
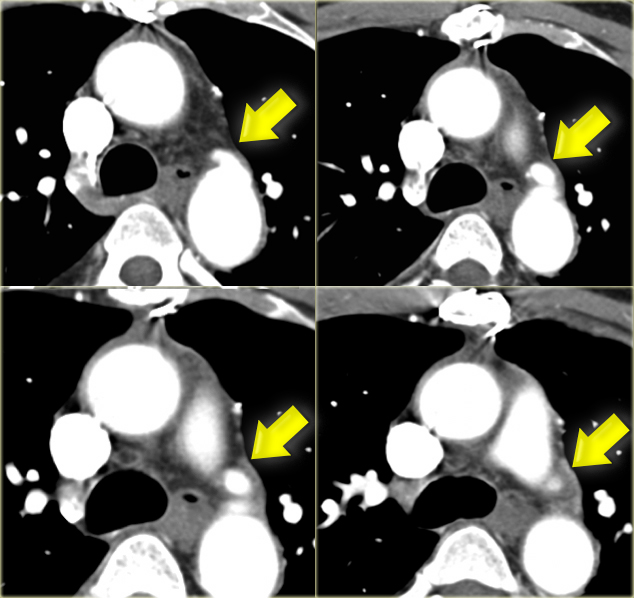
Right upper lobe anomalous return (2)
On the left a patient with a murmur.
Study the images and then continue.
- There is an anomalous return of the right upper lobe to the SVC.
- At a slightly inferior level there is also an ASD.
- Contrast is seen going almost immediately into the left atrium.
- This type of ASD is called the sinus venosus-type ASD.
On the left a similar case.
Notice the anomalous return of the right upper lobe vein into the VCS and the additional ASD at a lower level.
Right lower lobe anomalous return
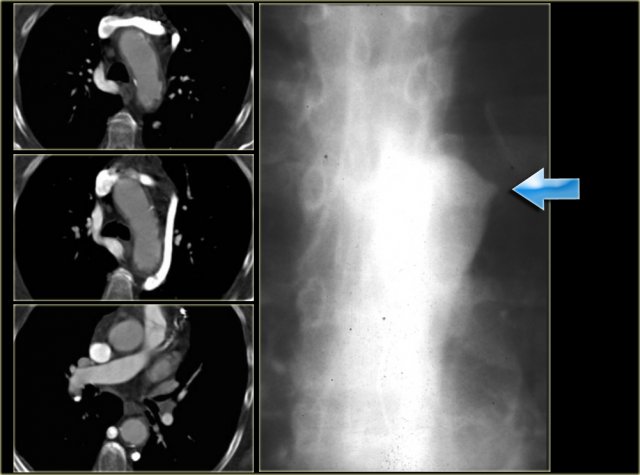
On the left a right lower lobe anomalous return.
The vein drains into the IVC.
The anomalous vein gently curves to the right cardiophrenic angle and is shaped like a Turkish sword ('Scimitar')
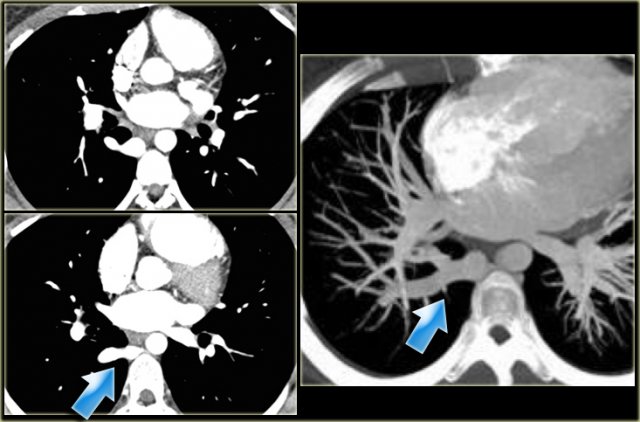
On the left another right lower lobe anomalous return.
The vein drains into the azygos vein.
Upper lobe veins may also drain into the azygos vein.
On the left a 10 year old girl suspected of having pneumonia.
Study the images carefully, because there are three findings and then continue reading.
The findings are:
- Small right lung due to hypoplasia
- Anomalous venous return
- Right aortic arch
This patient has a scimitar syndrome and also a right arch.
So the lesson is, that when you see one anomaly, look for another one.
Scimitar syndrome
The features in scimitar syndrome are listed in the table on the left.
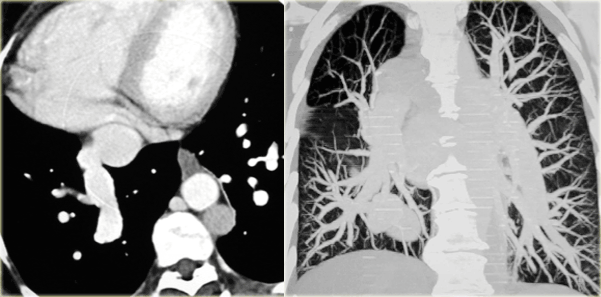
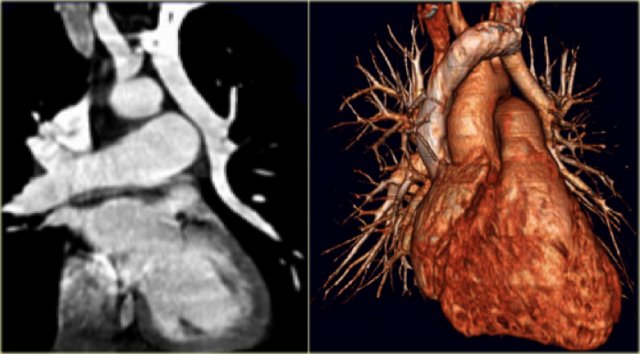
On the left another patient with a scimitar syndrome.
There is a hypoplastic right lung with mediastinal shift and there is anomalous venous return.
Notice that on the coronal MIP you can nicely see the difference in vascularization of the lungs with hypovascularity on the right.
Scroll through the images on the left.
Notice how the left upper lobe vein runs from the hilum cranially into the brachiocephalic vein.
The differential diagnosis of a left upper lobe anomalous venous return into brachiocephalic veins is a left Superior Vena Cava (SVC).
A left SVC however drains into the coronary sinus.
Systemic veins
Left Superior Vena Cava
- Represents persistent left common cardinal vein
- Passes anterior to left main bronchus and drains into dilated coronary sinus
- 0.5% of general population and 5% of patients with congenital heart disease
- Small Right SVC in 90% of cases
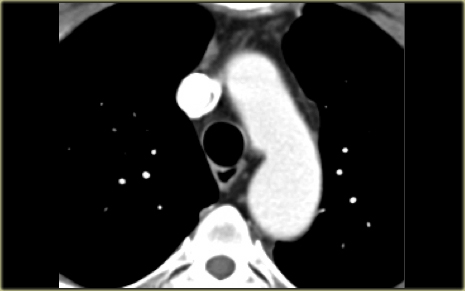
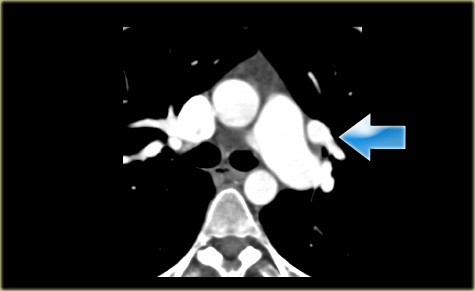
Describe the images on the left and then continue reading.
On the left side there is a vascular structure, that runs inferiorly below the level of the left hilum and enters into a dilated coronary sinus.
The diagnosis is left or double superior vena cava.
Left Superior Intercostal Vein.
This is an anastomosis between the accessory hemiazygos vein and the left brachiocephalic vein.
It courses along the lateral margin of the aortic arch ('aortic nipple').
It is a normal variant and if you look for this structure you will frequently notice it.
Catheters or pacemaker leads may course along left side of mediastinum.
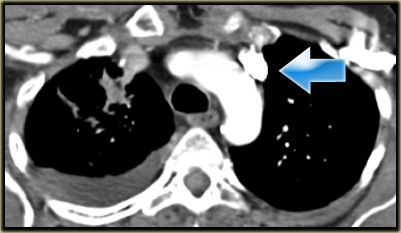
On the left a patient with a left superior intercostal vein.
Notice the 'aortic nipple sign'.
On the left another example of a left superior intercostal vein.
It courses along the lateral margin of the aortic arch from the the accessory hemiazygos vein to the left brachiocephalic vein.
Summary of left paramediastinal structures
-
Left VCS:
- from subclavian vein to coronary sinus
-
Anomalous LUL pulmonary vein:
- from left pulmonary hilum to brachiocephalic vein.
-
Left superior intercostal vein:
- from accessory hemiazygos vein to left brachiocephalic vein.
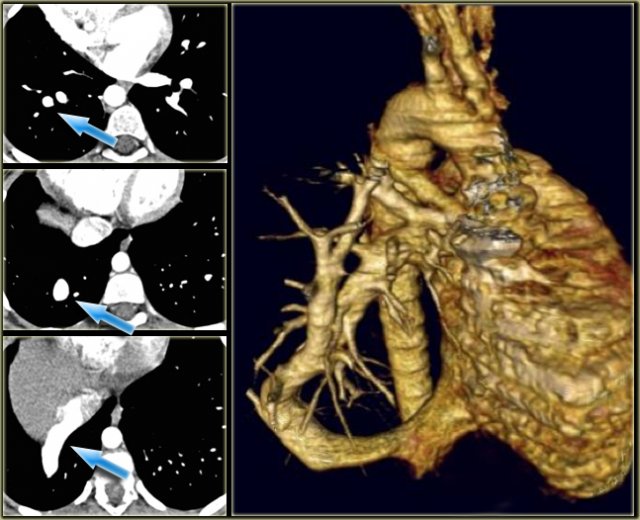
Azygos Continuation of IVC
- Abcense of hepatic segment of IVC with azygos continuation.
- IVC interrupted above level of renal veins.
- Association with congenital heart disease and polysplenia.
Technique and Protocol
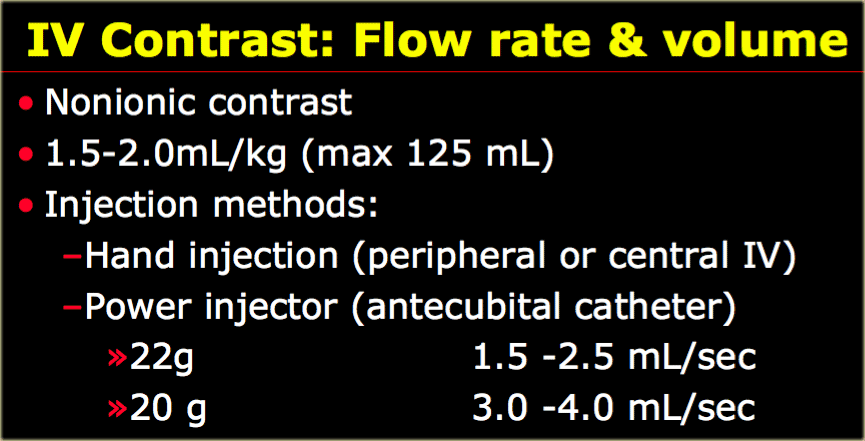
Ideally a 64 slice scanner is used, but even a 4-slice scanner will suffice for studying vascular anomalies.
The technique for these anomalies in the chest is the same as we use for pulmonary embolus detection.
Thin collimation is used in combination with a fast table speed in order to get the highest resolution with the lowest radiation exposure.
Usually a pitch of 1.5 is used.
In children we preferably do not use thin collimation, because of the higher radiation exposure, but these anomalies can be very small (voorbeeld dia 18), so thin collimation is necessary.
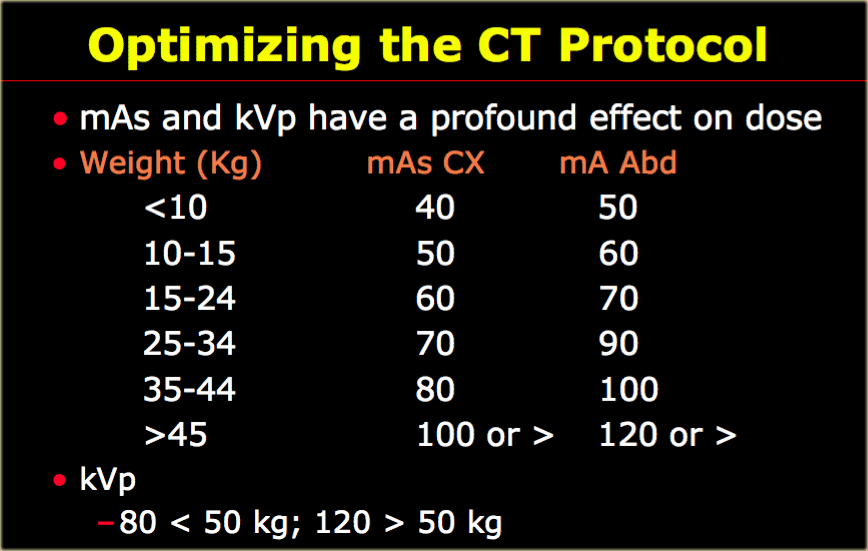
mAs and kVp
In a child with a weight of less than 10Kg 40mAs will work in the chest.
In children with a weight more than 45 Kg adult protocols are used with 100 mAs or more.
In small children under 50 kg you can decrease the kVp to 80 and that works very well in the chest.
Remember in the chest there is inherent contrast from the lungs and by dropping the kVp you enhance this contrast.
On the left a 3-year old.
Non-breath hold images with 50mAs and 80 kVp on a 16 row detector.
Although the axial images are a little bit grainy, the reconstructions are just fine.
Do these patients need sedation?
Well most of the time they don't.
If you can get the patient on the table and they are relatively still, even if they are breathing, you will get good studies.
If you can't get the patient on the table, because they prefer the floor, you've got to sedate.
In about 20-25% of pediatric studies we use sedation.
If the catheter is not in the antecubital vein, hand injection is preferred.
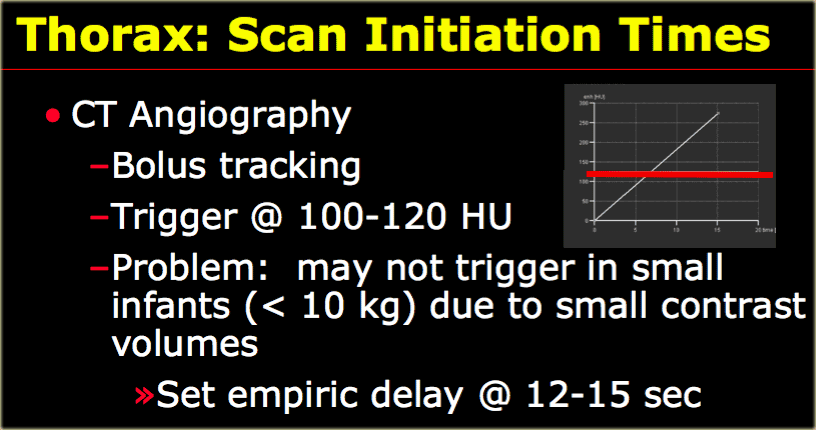
Scan Initiation Time
Bolus tracking is used and the trigger is set at 120 HU.
This may not always work, because in small children the amount of contast may be too small to trigger or due to breathing the cursor may fall to the lungs.
If bolus tracking does not trigger, start the scan at 15 seconds.
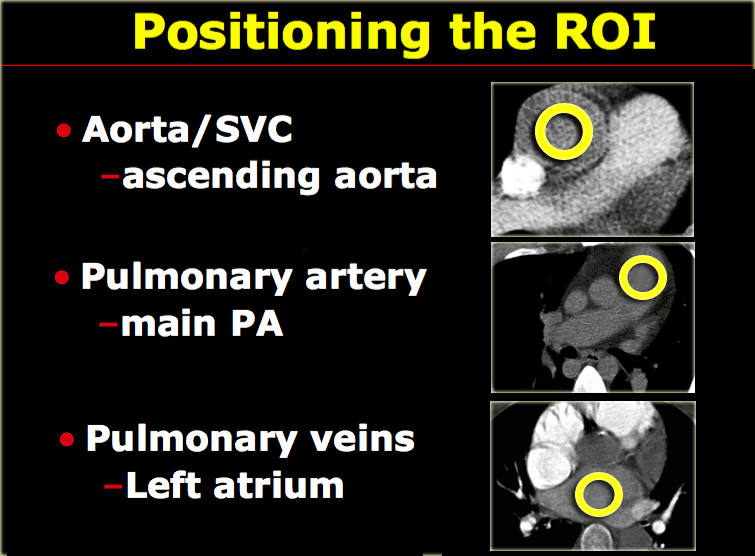
Positioning the ROI
- Ascending aorta for aorta and superior vena cava
- Main PA for pulmonary arteries
- Left Atrium for pulmonary veins
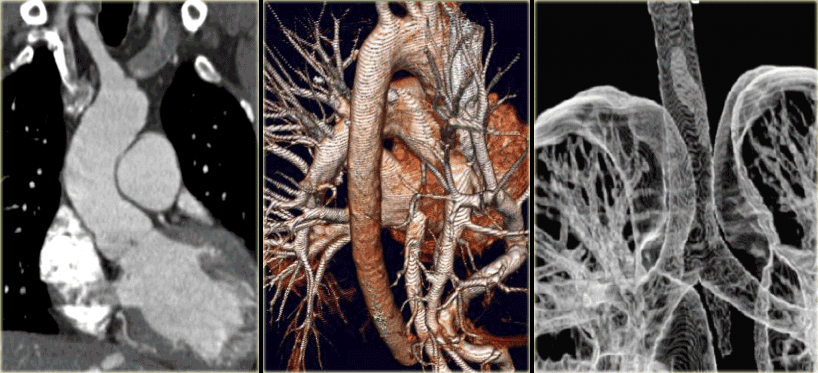
Post-processing
Multiplanar reconstructions (MPR), volume rendered techniques (VRT) and maximum intensity (MIP) are very helpful.
There is no role for shaded surface or mini-IP's.
On the left an external and internal rendering which provides in contrast to MPR real 3D information.
In volume rendering the posterior view is preferred to get a good look at the arch and descending aorta.
If you want to study peripheral vessels you will need thick slab maximal intensity projections.
For instance if you study arteriovenous malformations or discrepancy in lung flow.
Notice that on the coronal MIP you can nicely see the difference in vascularization of the lungs with hypovascularity on the right in a patient with scimitar syndrome.
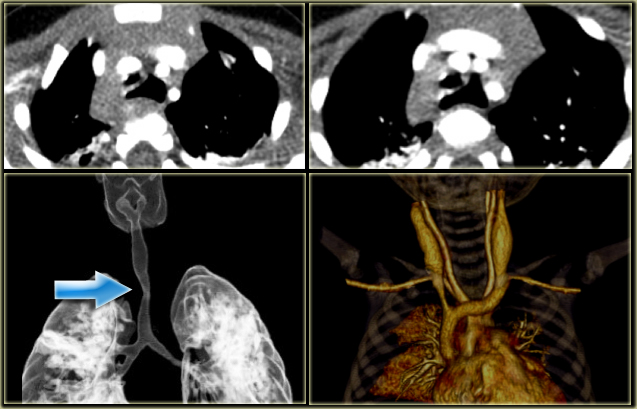
3D reconstructions are helpful when there are short focal lesions like coarctation or when vessels course obliquely (figure).
Adding 3D reconstructions to axial images will increase the sensitivity from 90% to 100% (Lee, Siegel AJR 182:777-784 )
On the left a 17-day old boy with minimal cyanosis, mild heart failure and upper extremity hypertension.
On axial images you will have trouble diagnosis coarctation, because it is focal and in the same plane as the axial image.
If you want to read more about pediatric body CT, buy:
Pediatric Body CT, 2nd edition. Lippincott Williams & Wilkins, Philadelphia. 2008 (3) by Marilyn Siegel.