Cystic Lung Disease - Differential diagnosis
Joline Trap-de Jong¹, Marcela Spee-Dropková² and Robin Smithuis³
¹St Antonius hospital Nieuwegein, ²Groene Hart hospital Gouda and ³Alrijne hospital Leiden the Netherlands
Publicationdate
In this article we describe an algoritm to establish a differential diagnosis in cystic lung disease.
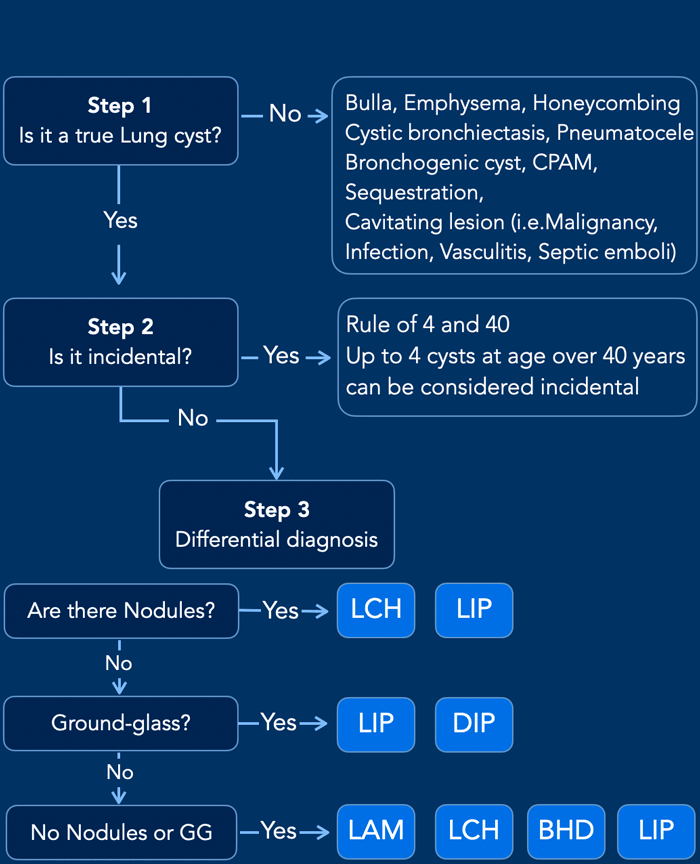
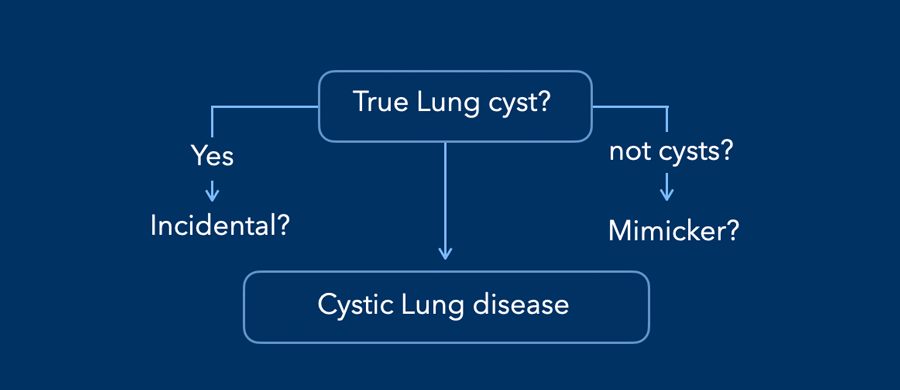
When you encounter something in the lung that looks like a lung cyst, you should ask yourself the following three questions:
- Is it truly a lung cyst or something else?
- Is it just an incidental finding without any clinical significance or should we consider a cystic lung disease?
- How do we establish a differential diagnosis when we think of a cystic lung disease?
Diagnostic Approach
Step 1 - Is
it a true pulmonary cyst or a cyst-like lesion
A pulmonary cyst is any circumscribed air-containing structure in the lung
parenchyma with a thin (< 2 mm) and usually regular wall.
In the next paragraph we will discuss how cysts can be differentiated from cavities, emphysema, pneumatoceles etc.
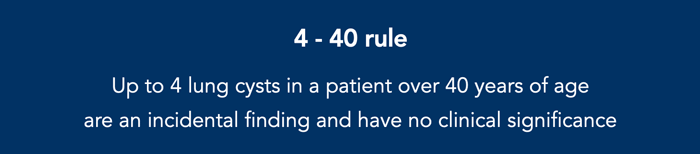
Step 2 - Is it an incidental finding or should we worry
A small number of lung cysts may be
seen with aging (Araki et al, 2015).
Cysts are regarded as incidental
finding without any clinical significance if there are no more than 4 cysts in
individuals older than forty years.
That’s why our rule of thumb is ‘the rule of
4 and 40’.
Step 3 - You are probably dealing
with a cystic lung disease
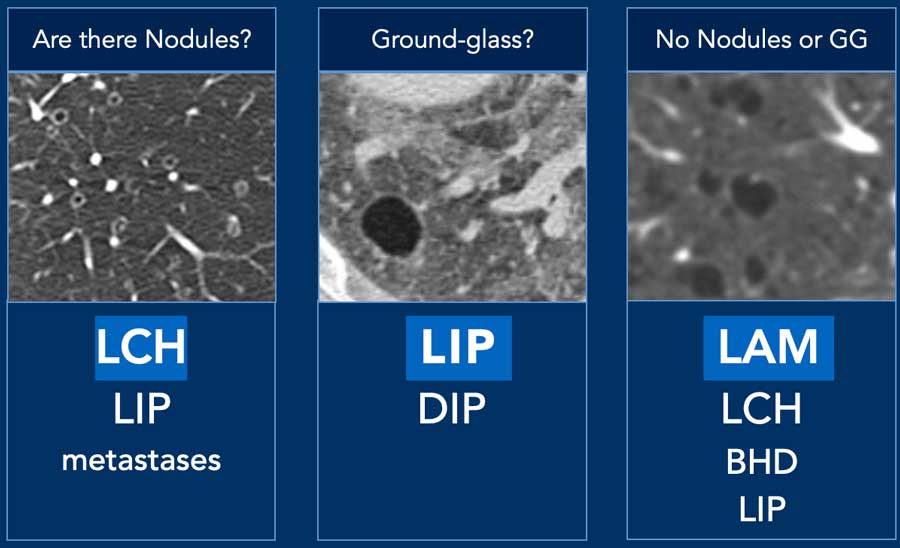
Are there also Nodules - Think LCH and LIP.
Any Ground-glass - Think LIP and DIP
No Nodules or Ground-glass - Think BHD, LAM, LCH and LIP.
LCH - Langerhans Cell
Histiocytosis is a multi-organ disease strongly associated with smoking. There can
be nodules, cavitating nodules and bizarre cysts that typically spare the pleural
recesses.
LIP - Lymphocytic Interstitial Pneumonia is associated with
autoimmune diseases such as Sjogren, and also with HIV. The cysts are often
seen together with some ground-glass or reticulation, and sometimes with small
nodules. The cysts are limited in number and predominantly located in lower
lung fields.
DIP – Desquamative Interstitial Pneumonia is smoking related. The cysts
are located within an area of ground-glass, with a basal, peripheral and
symmetric distribution. Often there are fibrotic changes within the ground-glass.
LAM – Lymphangioleiomyomatosis is a genetic disorder mostly in women (in a sporadic form) or in the context of tuberous sclerosis complex. Typically numerous small and round cysts in diffuse distribution, sometimes with pleural effusion (chylothorax). Patients can also present with renal angiomyolipomas.
BHD - Birt-Hogg-Dubé syndrome is a hereditary condition associated with
skin tumors and an increased risk of RCC. Limited number of cysts are predominantly
located in the periphery of the lower lung fields.
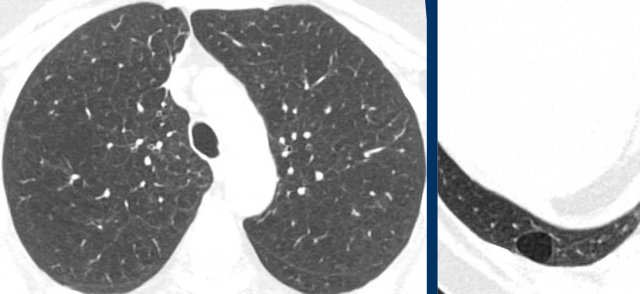
Step 1: Is it a pulmonary cyst or a cyst-like lesion
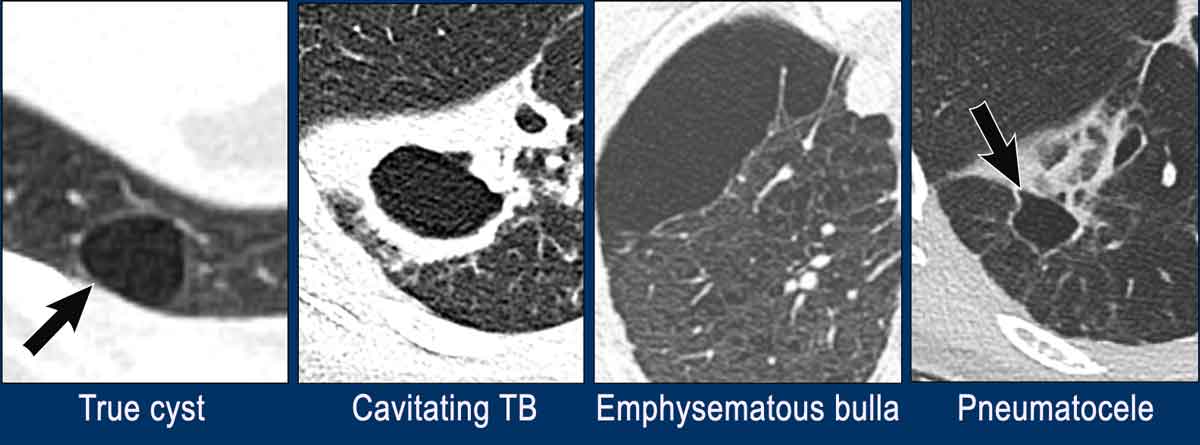
Solitary lesion
A simple cyst has a fine thin surrounding wall.
In the figure some solitary lesions that may simulate a lung cyst.
- Simple true pulmonary cyst with a smooth thin wall.
- Cavitation
with a thick irregular wall in a case of TB.
This can also be seen in malignancy, other infections or vasculitis. - Emphysematous bulla without a wall in a patient with centrilobular emphysema
- Pneumatocele. This can look like a simple cyst, but usually there is a history of a chest trauma or ventilation with barotrauma or infection.
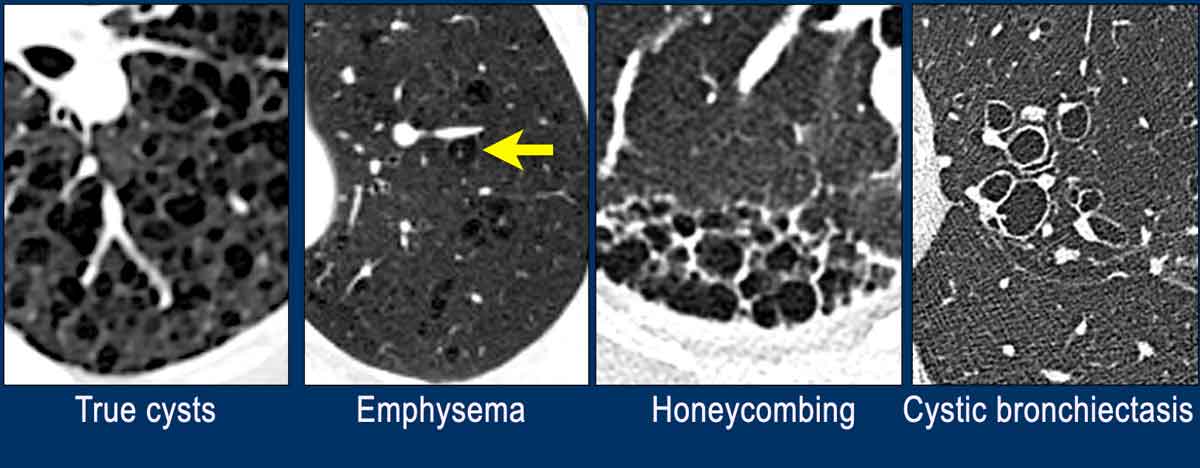
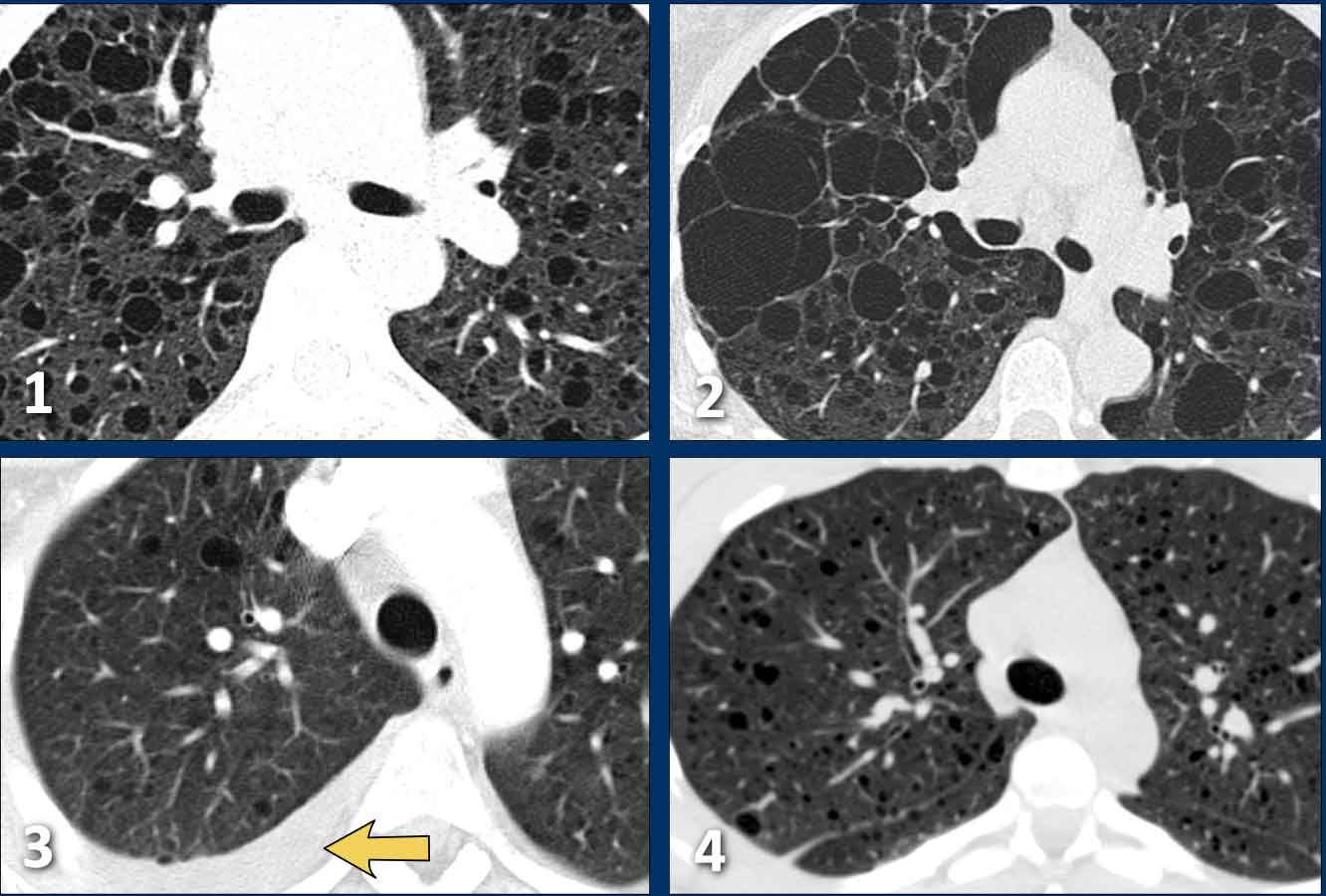
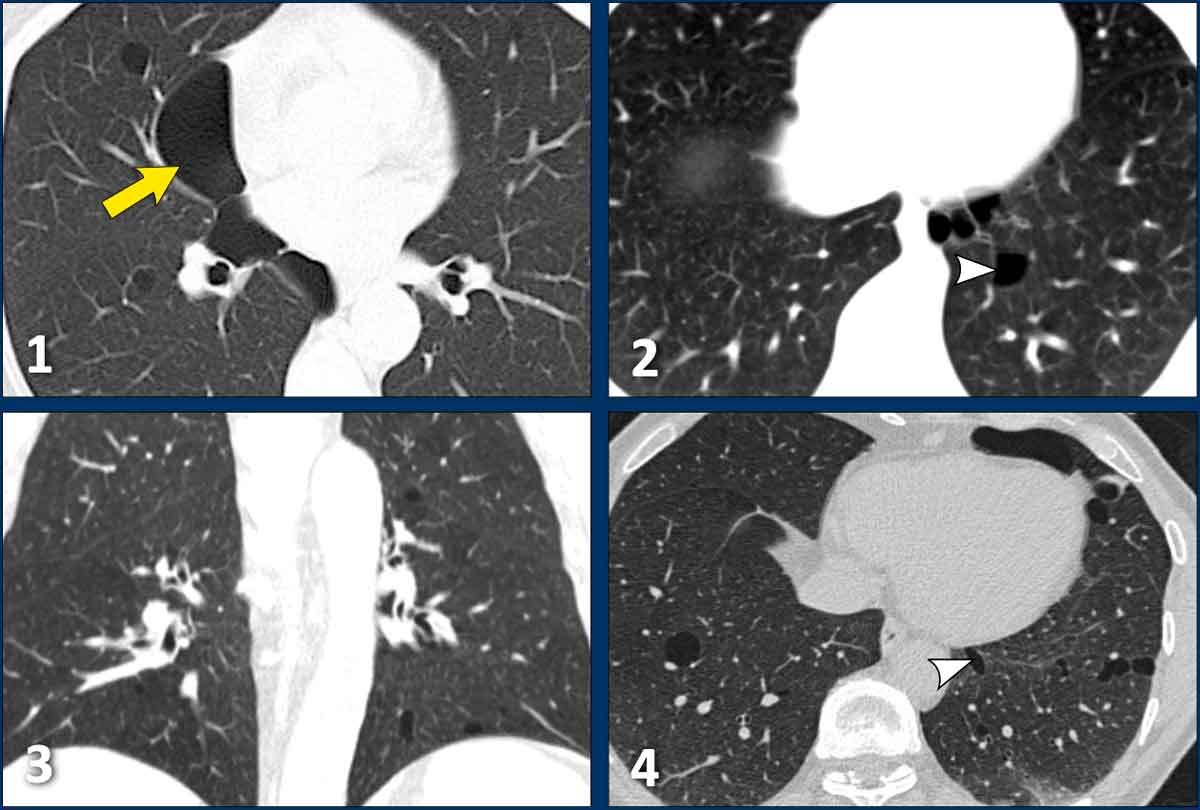
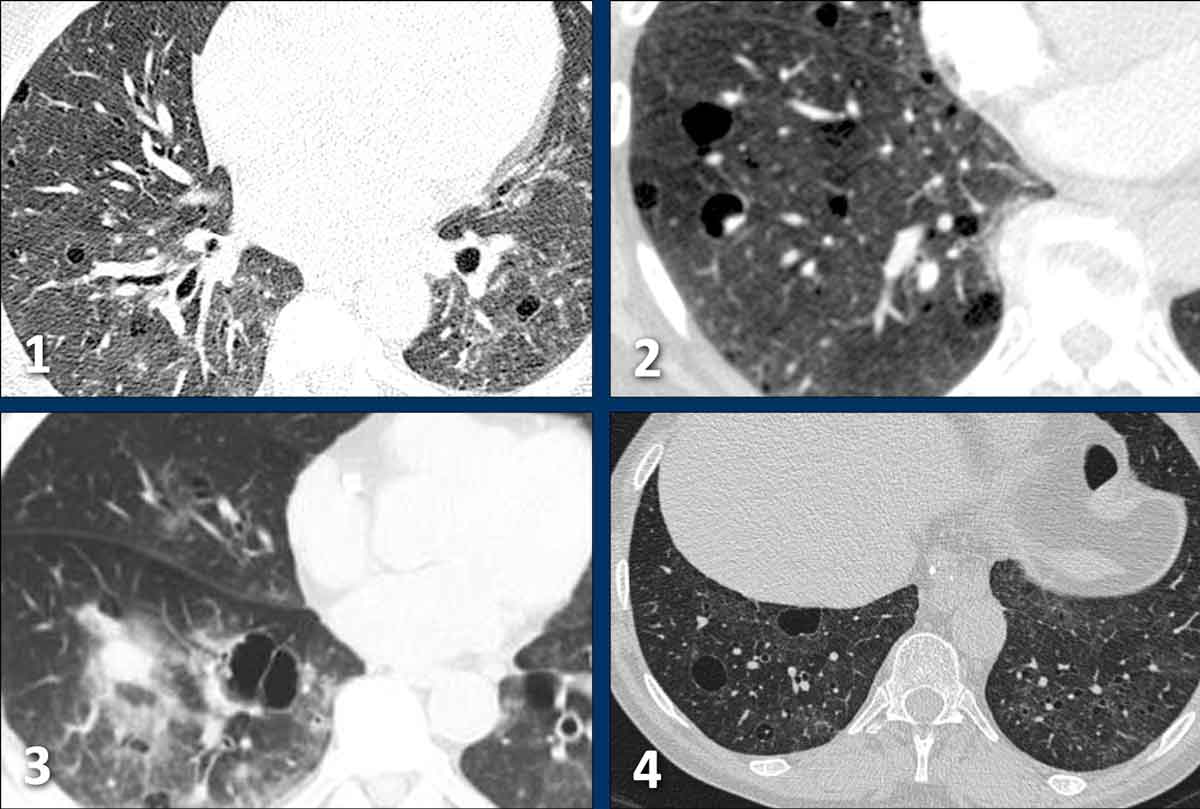
Multiple lesions
When there are multiple findings that
look like cysts, one should distinguish a true cystic lung disease from other
mimicking diseases as well (figure).
- Multiple lung cysts with fine walls in a patient with advanced LCH. This is a true cystic lung disease.
- Centrilobular emphysema, seen as black holes without a wall. Notice the central dot sign (arrow). Emphysema can be a real mimicker and we will discuss it in more detail later.
- Honeycombing as a stack of thick walled cysts in the periphery of the lower lobes in patients with lung fibrosis.
- Cystic bronchiectasis, seen as cystic tubes. This is usually not a problem as we can scroll through the images, but it can sometimes be challenging.
Step 2 - Is it an incidental finding
In young patients lung cysts should
not be regarded as a normal finding.
As a rule of thumb you can consider up to four cysts in a patient over forty
years of age as an incidental finding.
Don’t hold on to this rule too strong
when a patient is clinically suspected of a cystic lung disease (i.e. screening
scan for BHD or recurrent pneumothorax)
Step 3 - Differential Diagnosis
When you study a HRCT of a patient
with lung cysts, a good start is to see if the cysts are associated with
nodules or with ground-glass.
Other findings to consider are:
- Cyst pattern
- Distribution
- Patients characteristics
Nodules
When there are cysts together with
(maybe cavitating) nodules, the most likely diagnosis is LCH, which has an
upper zone predominance.
Ground-glass
The combination of cysts and ground-glass is not common and the most likely
diagnosis is LIP.
No nodules or ground-glass
Simple cysts without ground-glass or nodules are mostly seen in LAM, which is almost
only seen in women.
In smokers the most likely diagnosis is advanced LCH.
BHD and LIP are less common.
Another approach to the differential diagnosis is to consider the following: cyst pattern, distribution and patients characteristics.
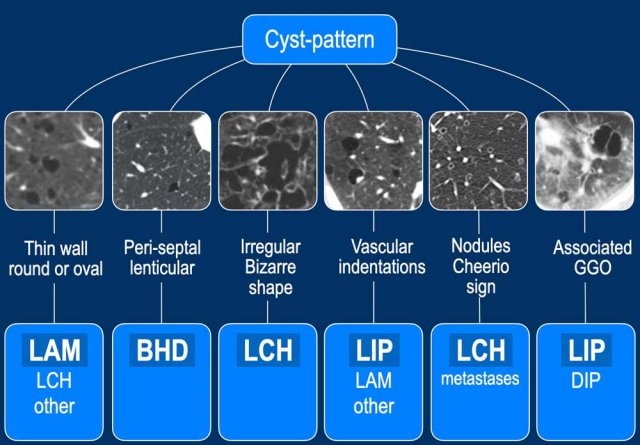
Cyst pattern
In this table more cysts-patterns are included.
For instance in BHD the cysts can have a lenticular shape and are frequently in peri-septal location.
Vascular indentations are quite specific for LIP.
The so called cheerio sign is seen in LCH.
This table is adapted from the article " a validated model for the imaging diagnosis of cystic lung disease" by Wallace T. Miller (reference)
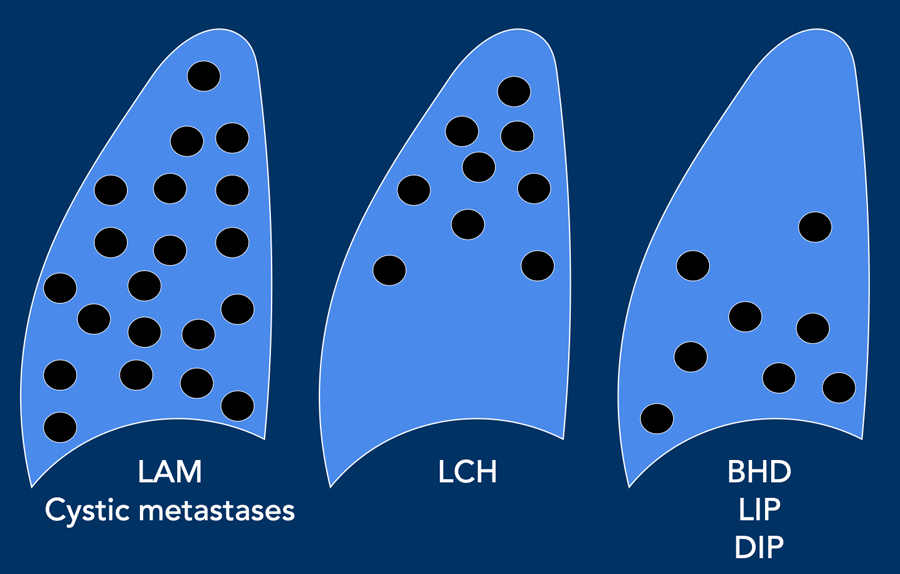
Distribution
The distribution and number of the cysts can be helpful.
- LAM cysts are usually evenly spread and numerous.•
- LCH has an upper lobe preference and the pleural recesses are typically preserved.
- BHD, LIP and DIP have a lower lobe preference and usually
only a few cysts are seen.
Patients characteristics
In this table the patients characteristics of the most common cystic lung diseases.
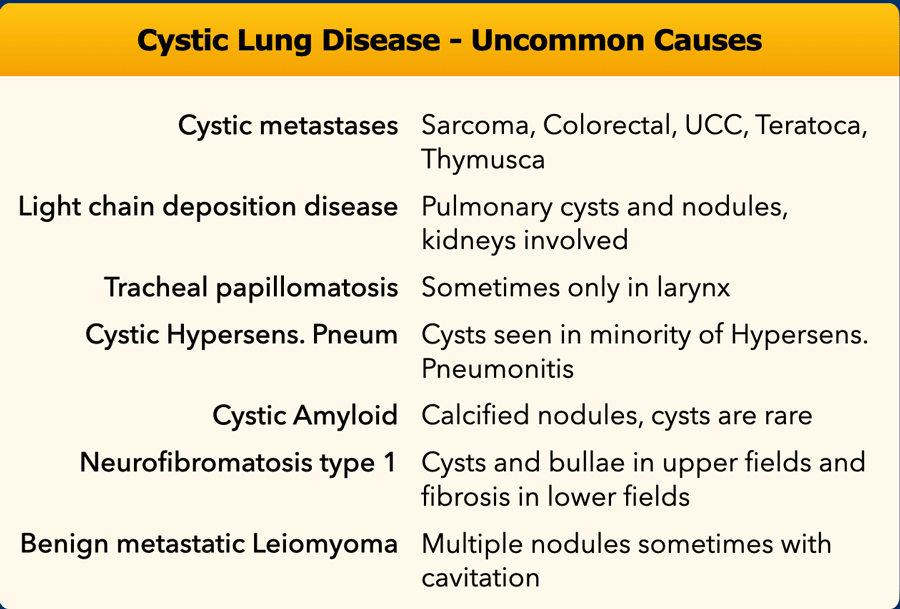
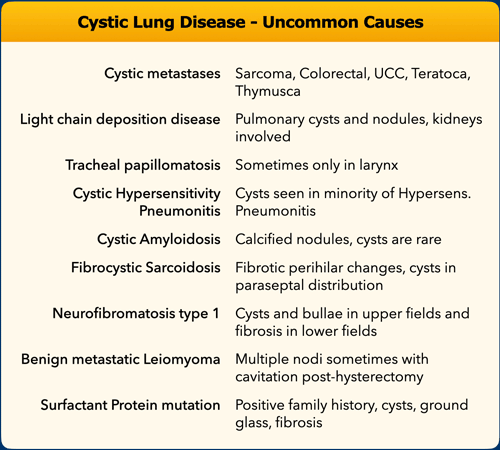
Uncommon causes
When the cysts do not fit into the diagnosis of the usual suspects (LAM, BHD, LCH, LIP), then think of uncommon causes of cystic lung disease.
LAM - Lymphangioleiomyomatosis
Lymphangioleiomyomatosis (LAM) is an indolent, progressive disease exclusively seen in women as a sporadic genetic mutation, unless associated with tuberous sclerosis complex, which can be sporadic or inherited.
Patients are usually symptomatic with dyspnea, cough, chest pain, and hemoptysis.
Some patients present with spontaneous pneumothorax, pleural effusion (chylothorax) or angiomyolipomas can also be seen.
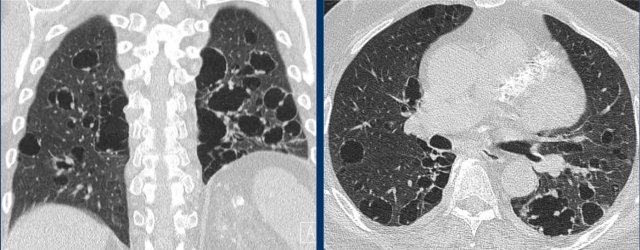
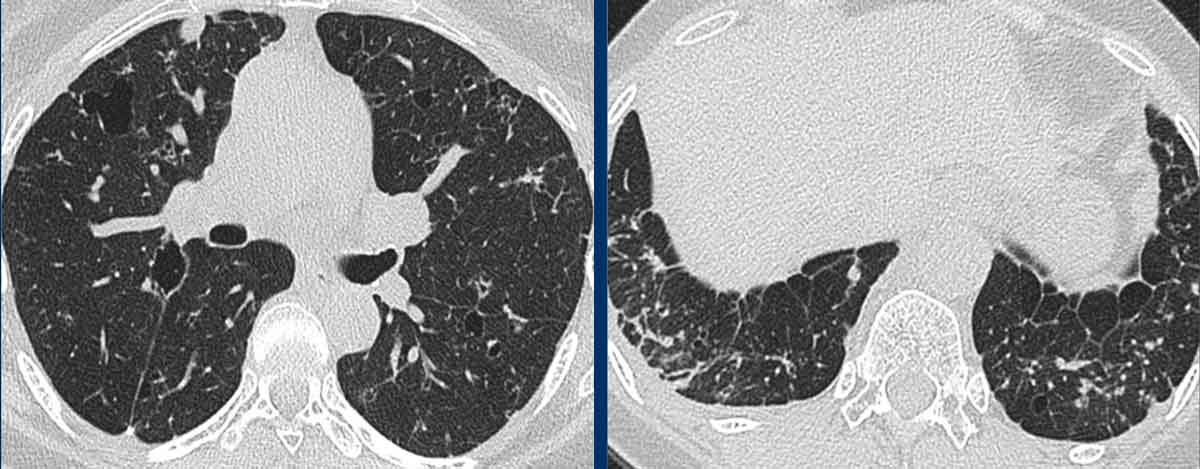
LAM presents with a large number of round and regularly shaped cysts spread throughout the parenchyma.
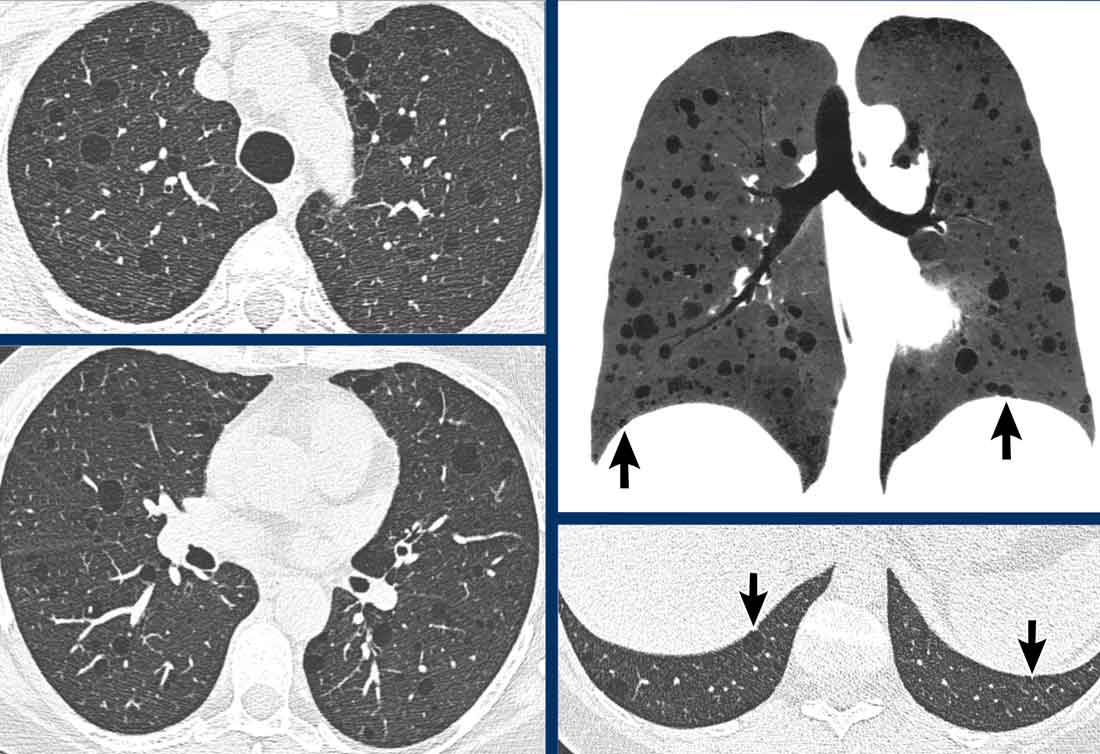
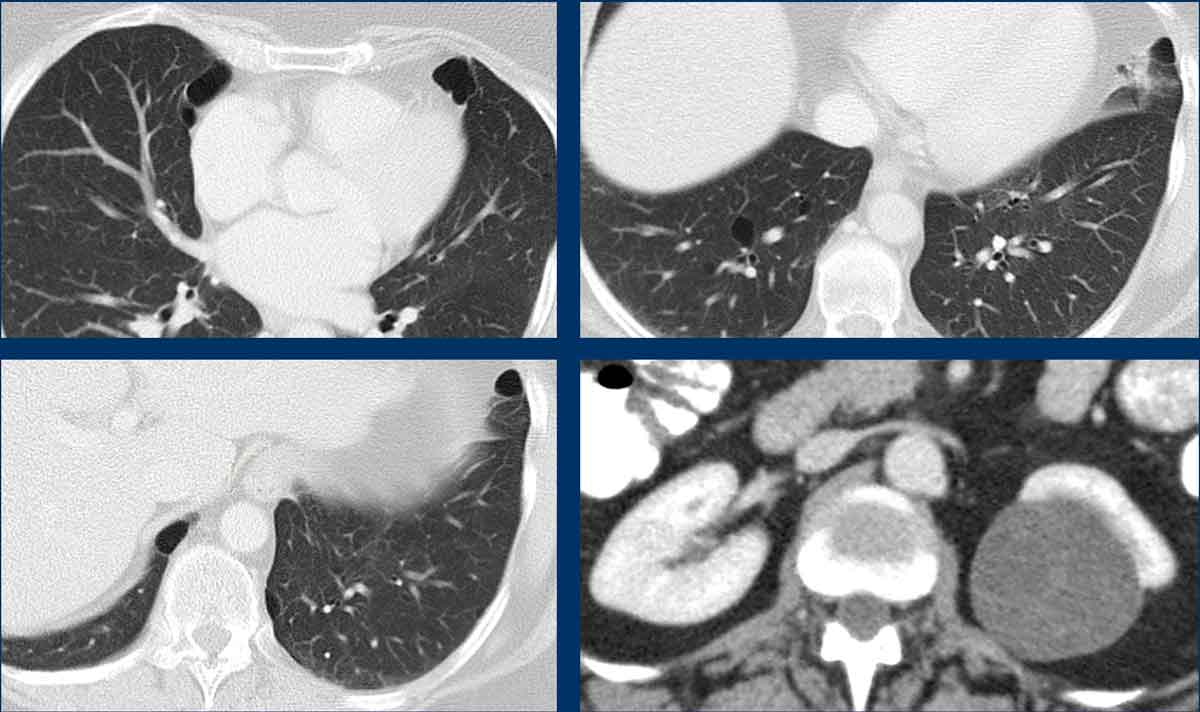
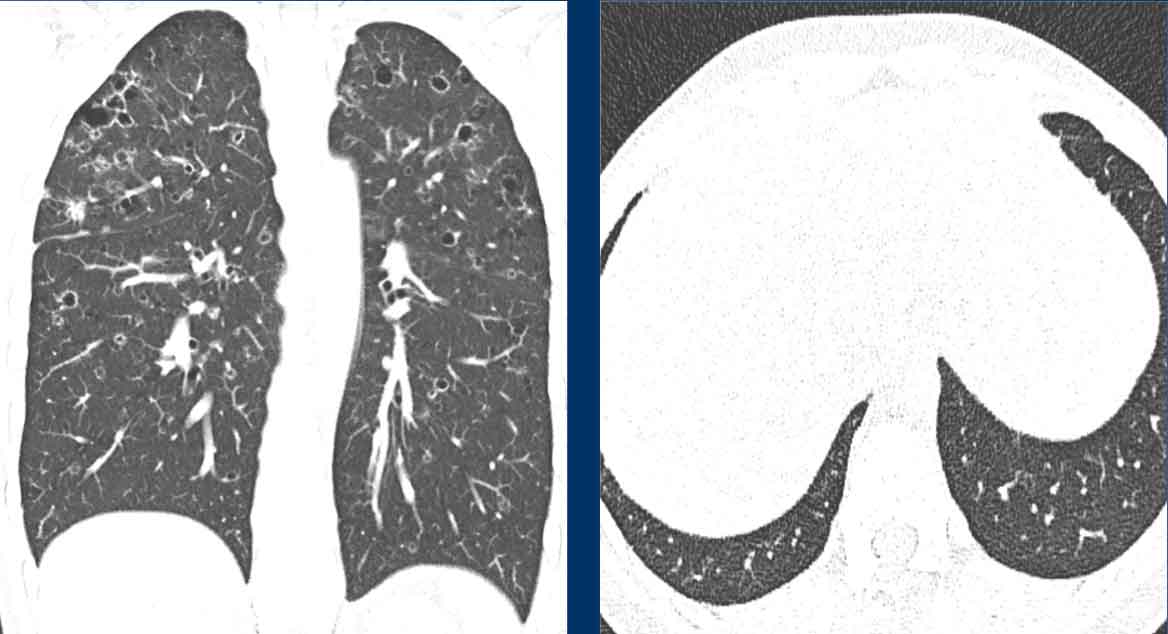
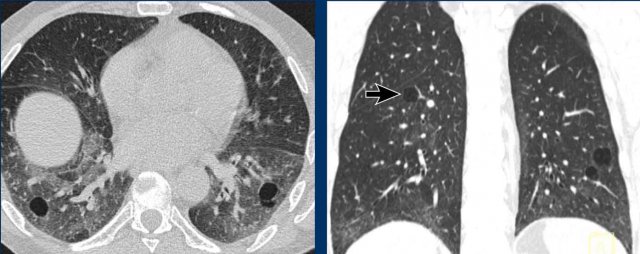
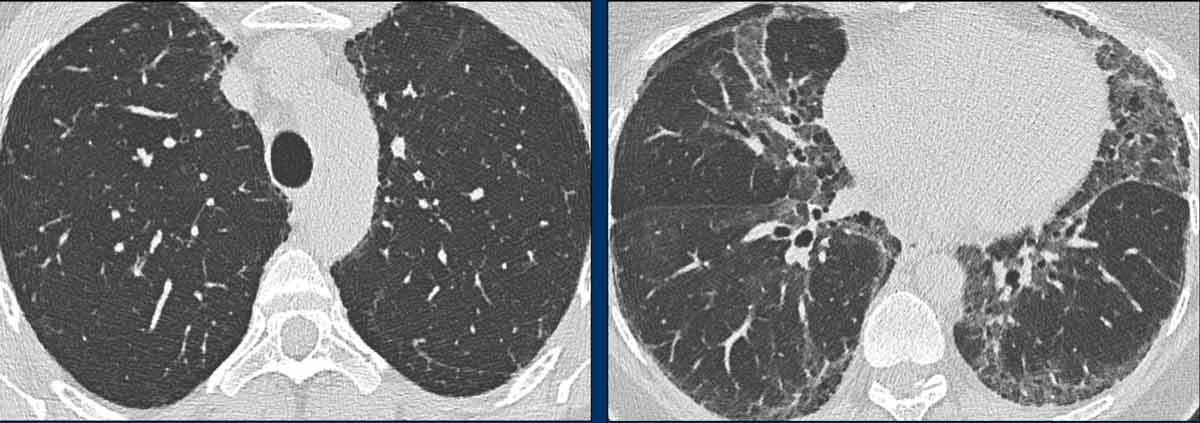
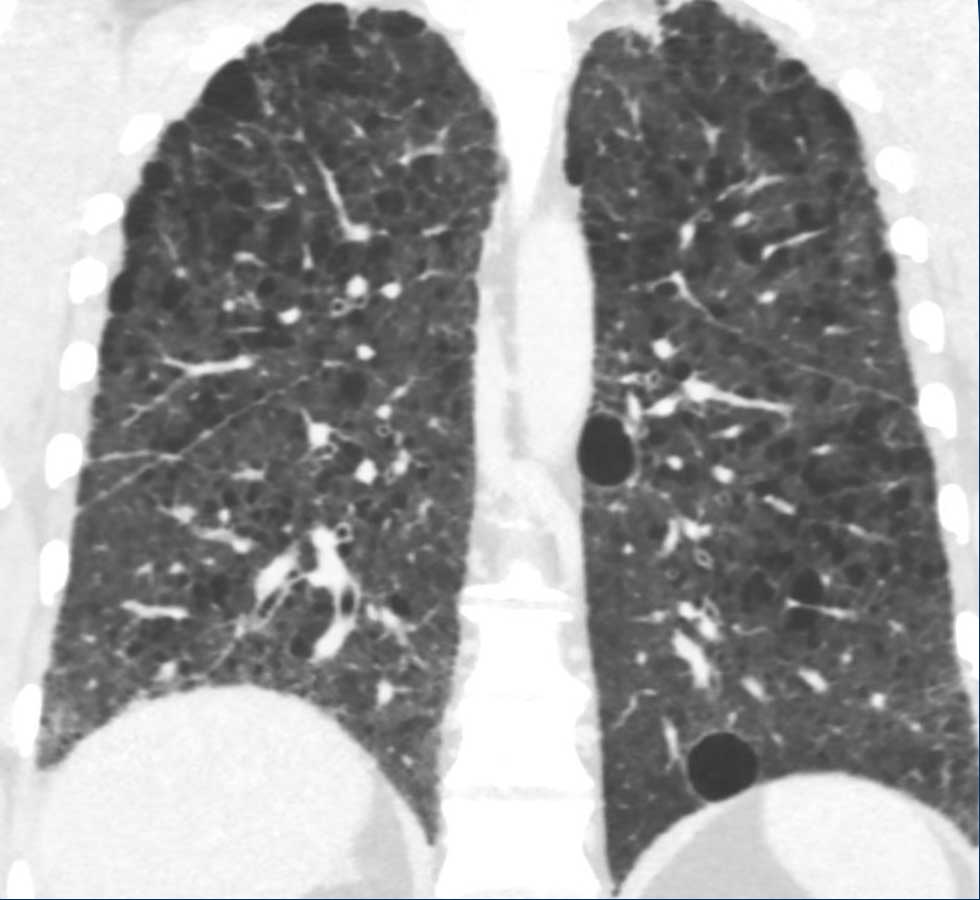
Images
- Numerous cysts in a young woman. Notice the regular round shape and diffuse distribution.
- Severe case of LAM. When there is a history of smoking, the differential diagnosis would be (advanced) LCH.
- Pleural effusion (chylous fluid) in a patient with LAM.
- Diffuse distribution in LAM.
These images are of a 39-year-old woman with dyspnoe.
What is the most likely diagnosis?
Findings
There are multiple thin-walled cysts.
Notice that the cysts are evenly spread throughout the lungs.
The pleural recesses are also involved (arrows).
This means that we can skip the diagnosis LCH.
The most likely diagnosis is LAM.
This is another example of LAM.
There are multiple thin-walled cysts evenly spread throughout the lungs, typical for LAM, but in this case it is combined with a pleural fluid collection on the right (arrow).
LAM cells may lead to blockages of the lymph system in the chest and create a
chylous pleural effusion.
LAM is the only cystic lung disease
in which we can see the combination of cysts and pleural fluid.
In addition, multiple angiomyolipomas
were seen in the upper abdomen.
This patient turned out to have TSC (tuberous
sclerosis complex) associated LAM.
The prevalence of angiomyolipomas in
sporadic LAM is 40-50 % and in TSC-LAM approximately 80 %.
This is a case of severe LAM with
diffusely affected lung parenchyma.
Generally, LAM is a progressive disease
with a poor prognosis.
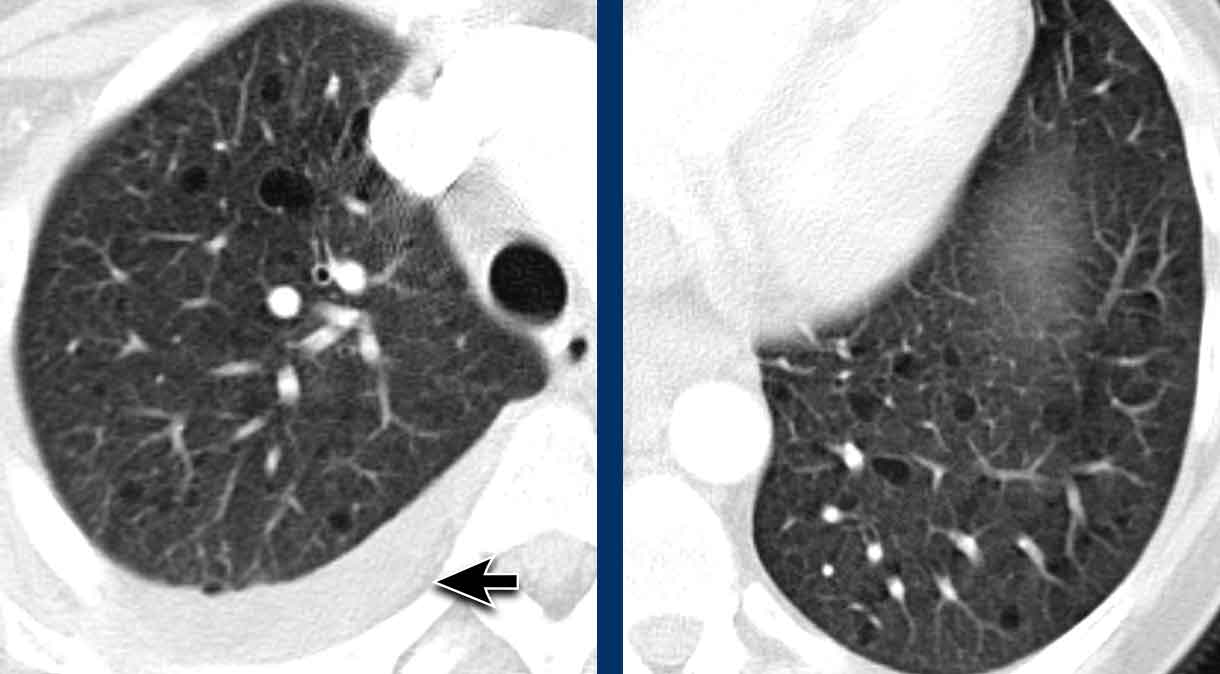
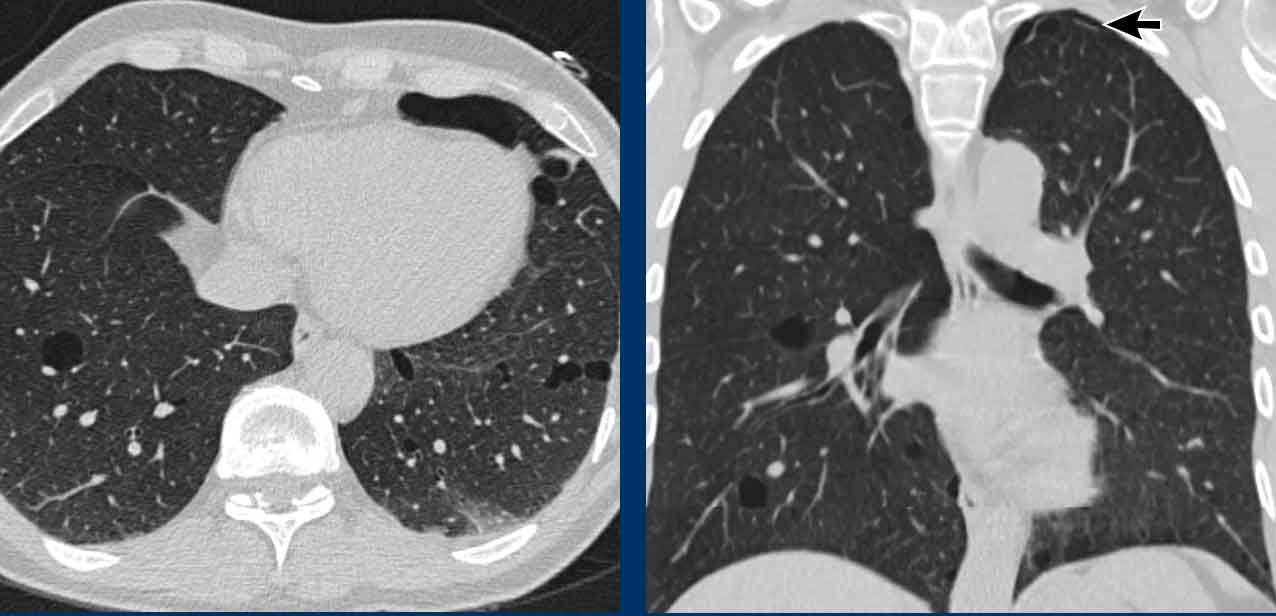
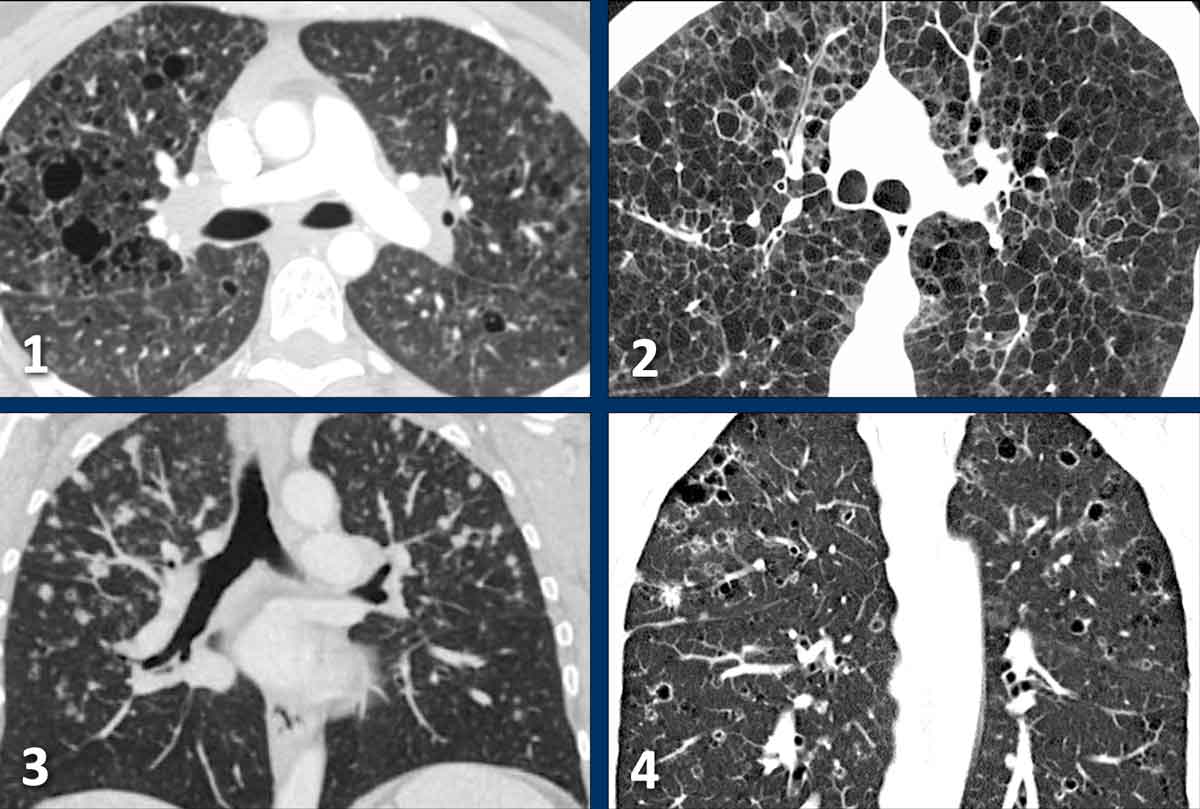
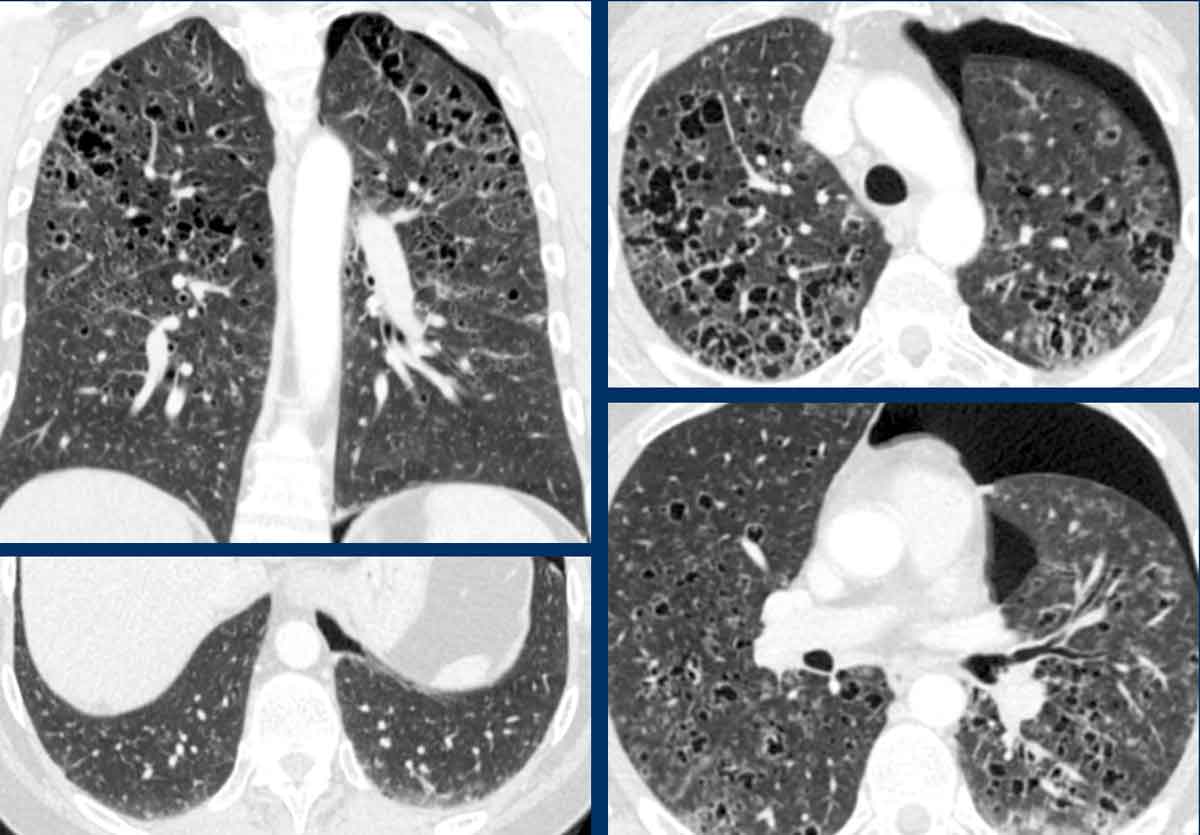
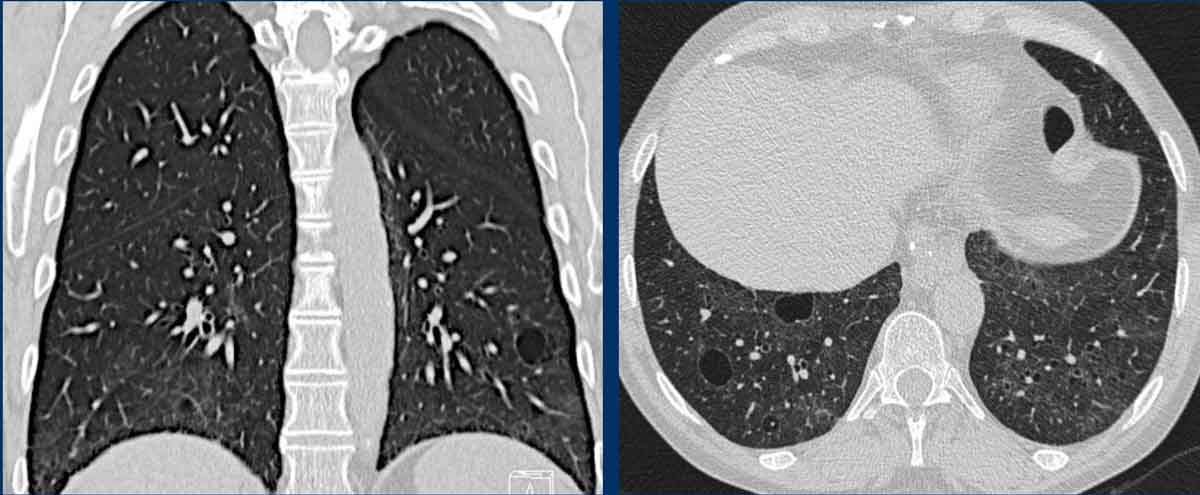
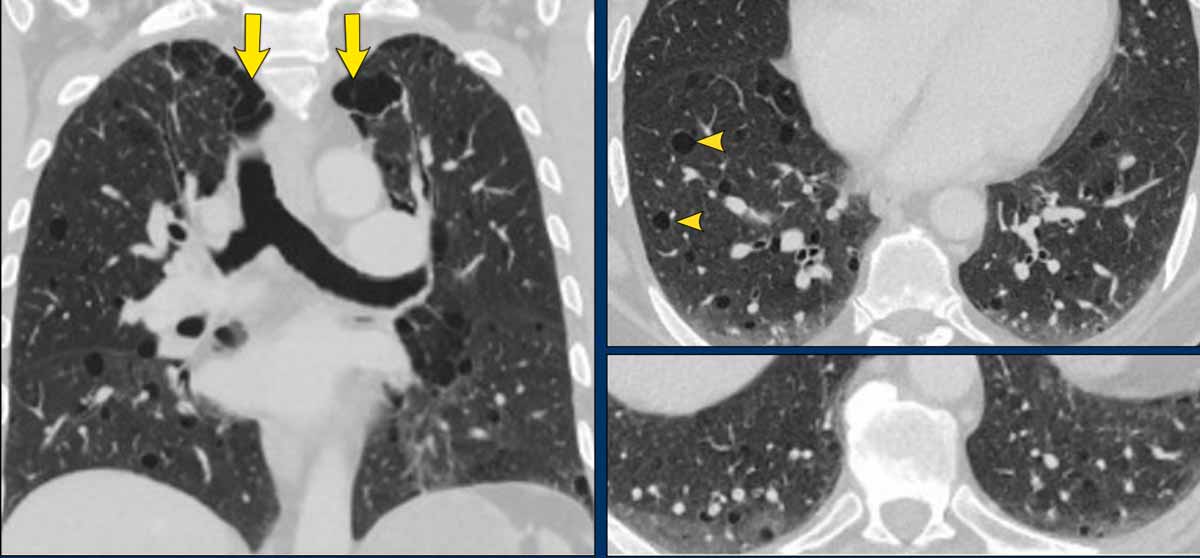
BHD - Birt-Hogg-Dubé syndrome
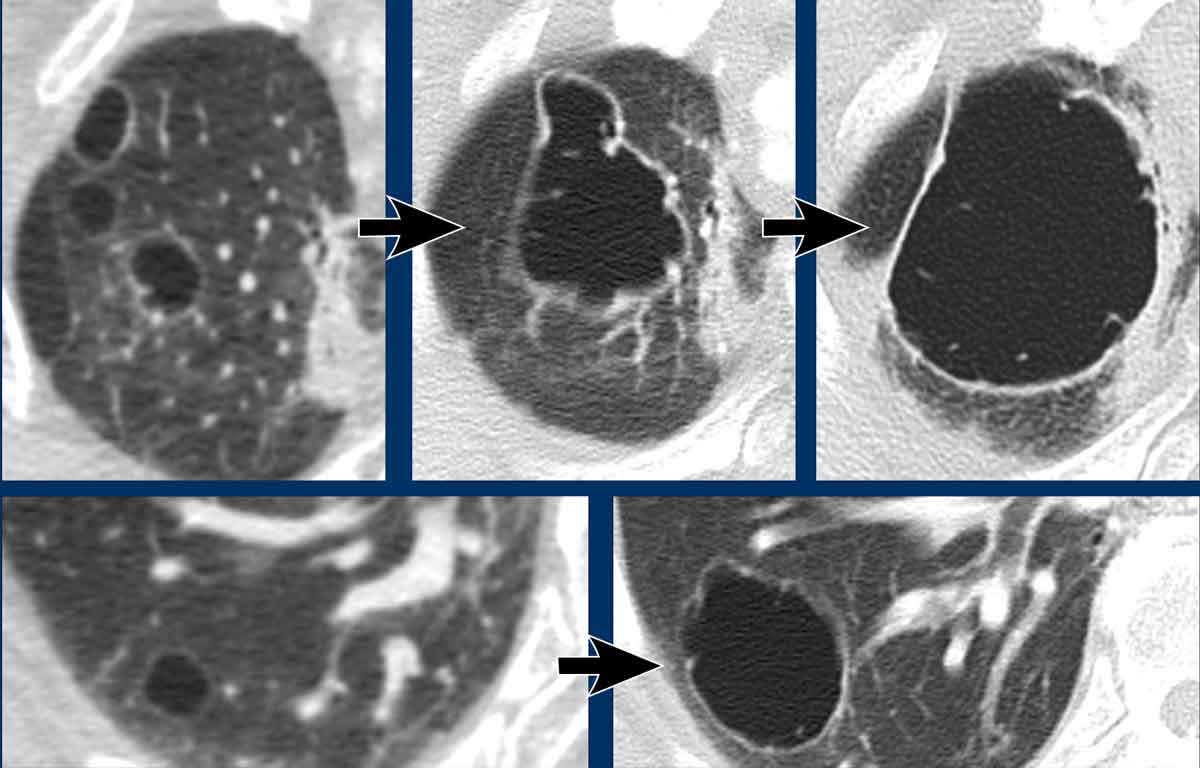
Birt-Hogg-Dubé syndrome is a autosomal dominant genetic disorder with a 25% risk of renal cancer.
The cysts in the lungs are asymptomatic apart from possible recurrent pneumothoraces.
BHD cysts have a lower field and peripheral predominance.
They sometimes have borders defined by interlobular septa giving them a typical triangular or lenticular shape (arrowheads in 2 and 4).
BHD cysts are not numerous, usually less than 50 cysts. Sometimes there are really few cysts with a very subtle appearance (image 3), but it should not be missed.
It is important to make the diagnosis because these patients and their family need to be screened for renal tumors.
Often these patients will have one or more family members with a history of renal cancer or pneumothorax.
This can guide you to the diagnosis.
Images
- BHD cysts. Some are adjacent to the pleura (yellow arrow) or fissures. Cysts in the lower zones may also be seen in LIP.Paraseptal emphysema shows upper zone predominance.
- Lower zone predominance and triangular shaped (arrowhead) cysts in BHD.
- Notice the very subtle appearance with lower zone predominance.
- Typical BDH cysts
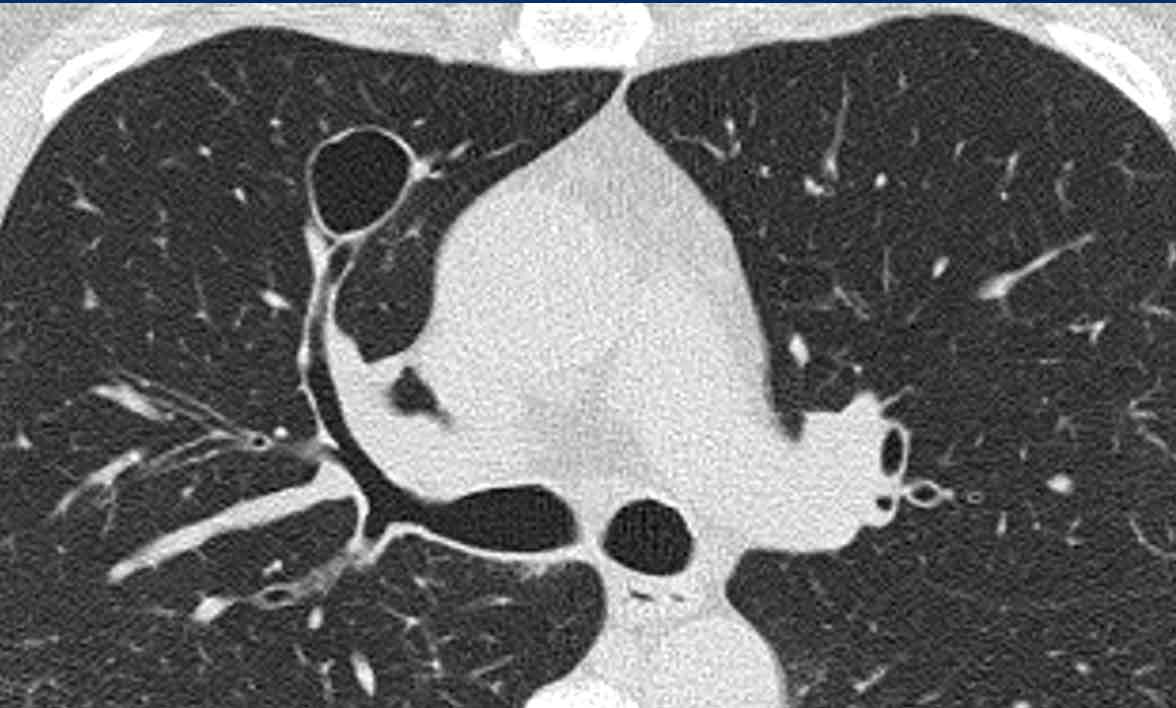
These images are of a 56-year-old woman, who had recurrent pneumothorax and now again presents with a pneumothorax (arrow).
Study the image.
Are these cysts or mimickers?
Is this an incidental finding or do you think it is a cystic lung disease?
What is the most likely diagnosis?
Findings
There are multiple thin-walled cysts - more than four. Notice the localisation near fissures and in the periphery of the lung.
Conclusion
This is a case of Birt-Hogg-Dubé syndrome (BHD).
Discussion
The two cystic lung diseases that frequently present with a pneumothorax, are LAM and BHD.
LAM presents as simple cysts, which are thin walled, round or oval and regularly shaped with a diffuse distribution.
The peripheral and perifissural location of BHD cysts often gives the cysts sharp angles that causes them to have a lenticular shape.
When cysts have this typical appearance, they have an extremely high specificity for the diagnosis of Birt-Hogg-Dubé syndrome.
This is another case of Birt-Hogg-Dubé syndrome.
The cysts are typically located in the periphery of the lung near the mediastinum (black arrow) and close to the fissure (white arrow).
This is another companion case with very few and small cysts in a patient with Birt-Hogg-Dubé syndrome.
Sometimes you need to study the lung fields very carefully not to overlook the cysts and miss the diagnosis of BHD.
In this case you can imagine, that if the CT is performed for another reason, that you can easily miss these tiny cysts.
Remember that when you see more than four cysts and they are truly cysts, you need to do something with the findings.
These patients should go to a pulmonologist for further work up.
This patient had a CT for work up of a renal tumor.
In the radiology report the cysts in the lungs were described as bullae.
These cysts however are typical BHD-cysts in the periphery of the lungs, while bullae are seen in patients with emphysema and are located in the upper lung fields.
Especially when you only see a few cysts, then think of BHD.
The family need to be screened for BHD-syndrome and renal tumors.
Finally a more severe case of BHD with larger cysts.
This patient presented with a pneumothorax.
Notice the drain (arrow).
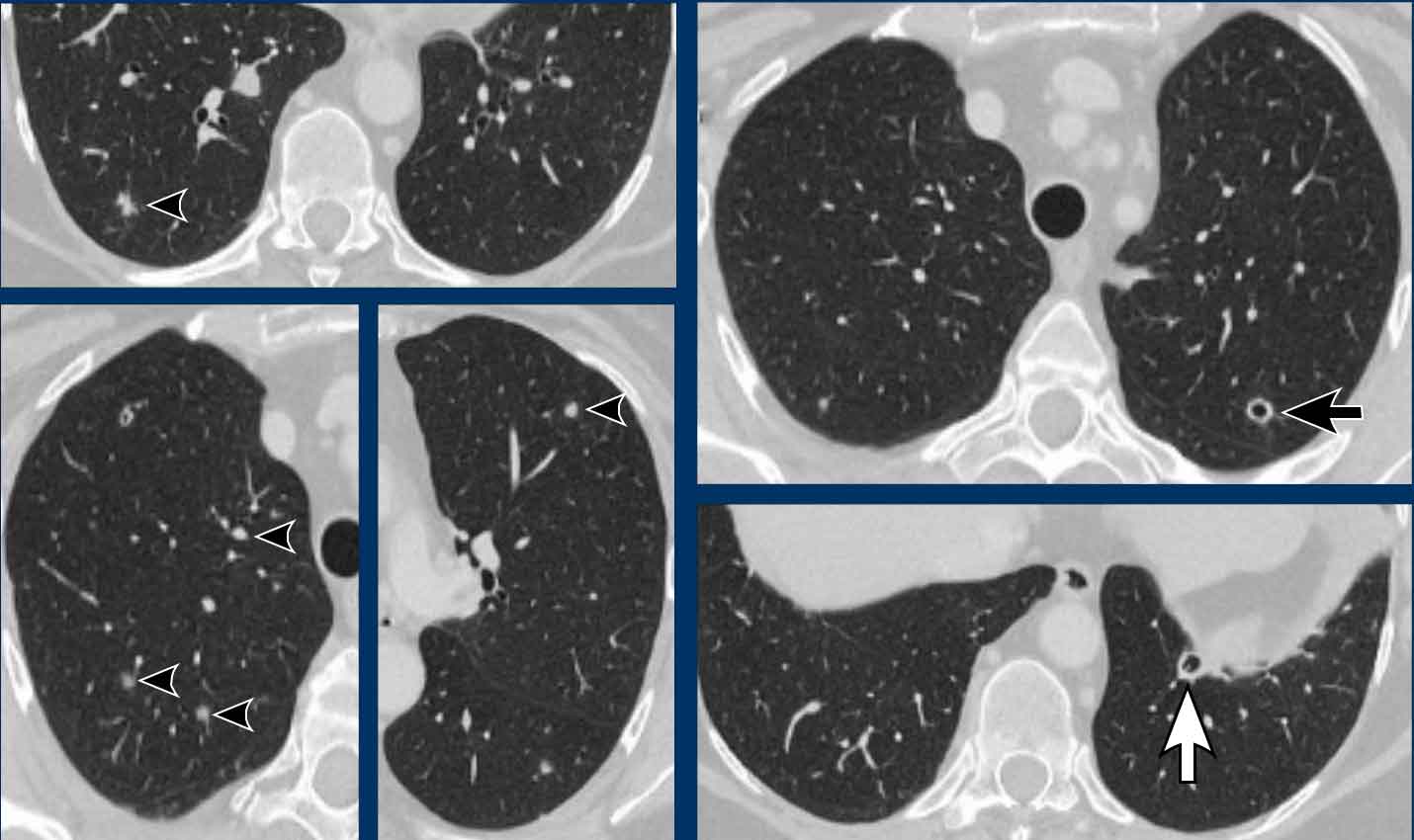
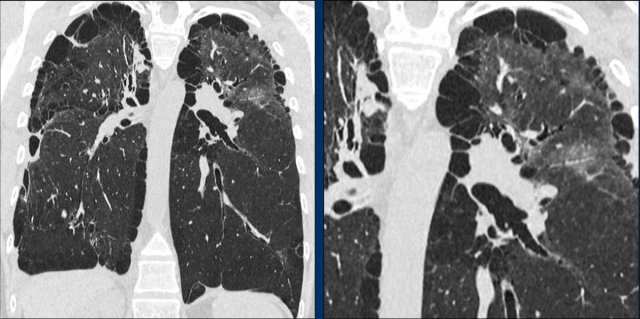
LCH - Langerhans Cell Histiocytosis
The etiology of Langerhans Cell Histiocytosis is unknown, but cigarette smoking plays a primary role.
Patients are at increased risk of lung cancer.
LCH starts as nodules, that cavitate and transform into cysts with an irregular shape (bizarre cysts, due to confluence of two or more cysts).
Images
- Bizarrely shaped cysts in a man with LCH.
- Extreme case of advanced LCH resembling emphysema. In a woman without a history of smoking, this could also have been a case of severe LAM.
- Multiple nodules, some cavitating, with an upper zone predominance (unlike metastases), and complete sparing of the pleural recesses.
- A combination of bizarre cysts, nodules and cavitating nodules with upper zone predominance.
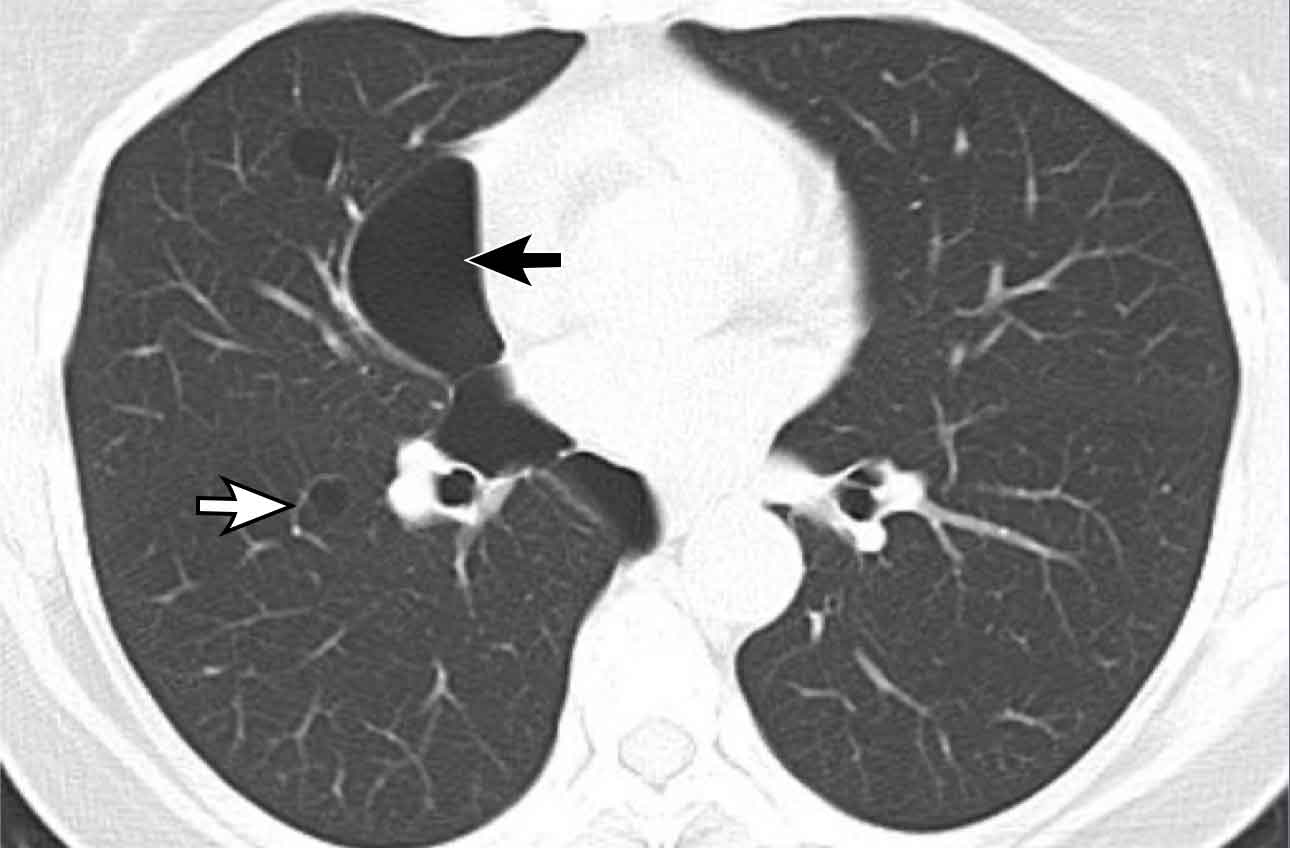
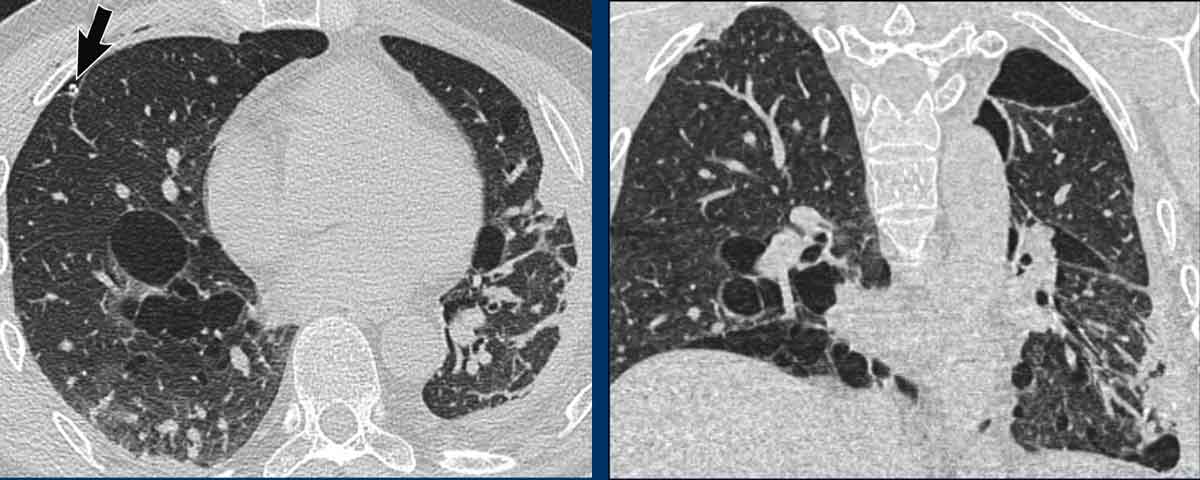
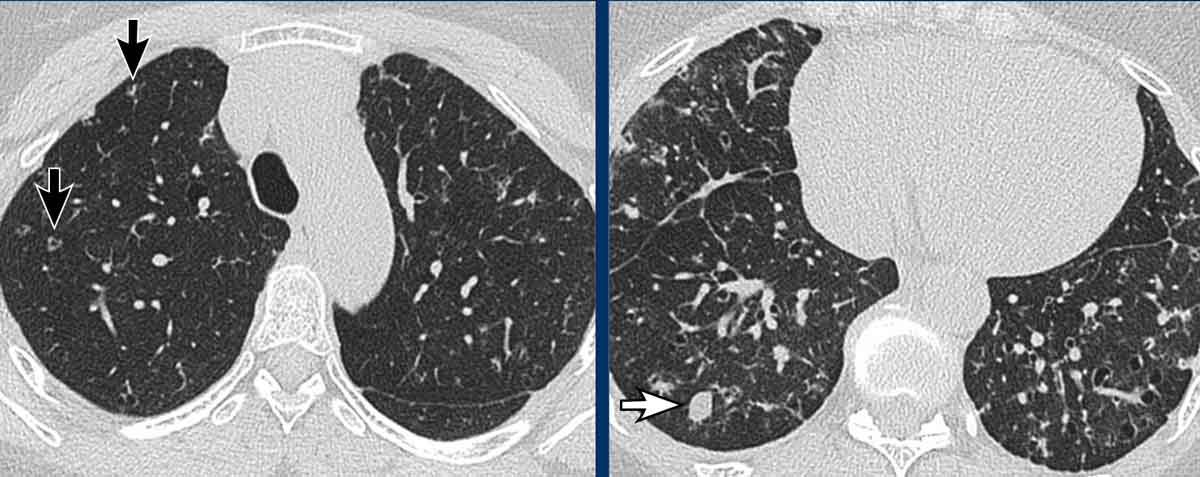
These images are of a 66-year-old man, who is a smoker and complaints of dyspnoe.
Study the image.
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
There are multiple cysts.
Some are irregularly shaped and some have a cheerio sign as a result of cavitation within the nodule (white arrows)
There are also some nodules (black arrows).
Discussion
The combination of these findings in a smoker is typical for the diagnosis LCH.
Continue...
On the coronal reconstruction it is obvious, that the cysts predominantly involve the upper and middle lobes and spare the lung bases.
Especially when LCH is still in the nodular phase, this distribution can be a helpful sign in the differentiation of metastases, which have a lower lobe preference.
This is a similar case.
Notice that the cysts predominantly involve the upper and middle lobes.
The pleural recesses are preserved.
The cysts have caused a pneumothorax.
LCH mimicker 1
This is an example of nodules and cavitating nodules wíth involvement of the pleural recesses.
These were metastases of a transitional cell carcinoma.
The distribution is helpful in the differentiation of metastases and LCH.
Some lung metastases show primary cavitation and some show cavitation as a result of treatment.
LCH mimicker 2
These are images of two different patients.
Study the image.
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
Although at first glance these images look similar, you may notice that on the left we have true cysts with a wall in a patient with advanced LCH, while on the right some appear to have a wall, but most of them do not.
This is centrilobular emphysema.
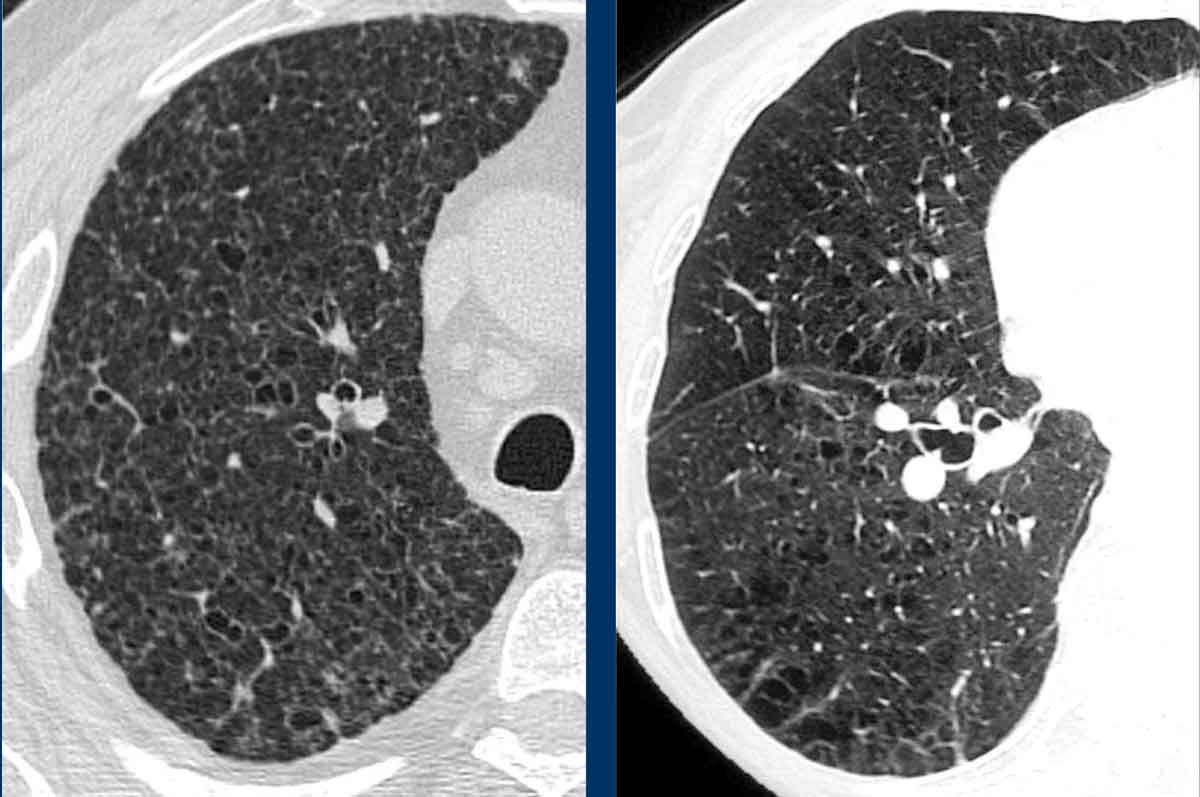
LIP - Lymphoid Interstitial Pneumonia
Lymphoid Interstitial Pneumonia is an interstitial lung disease of unknown etiology, that is characterized by infiltration of lymphocytes.
It is associated with systemic diseases (especialy M. Sjögren).
It can present as simple cysts only, but more often in combination with ground glass, reticulation and/or nodules. Some cyst may have a subtle septum, which may mimick a central dot as seen in emphysema (Figure 1 and 4).
Images
- Simple cysts in diffuse ground-glass
- Simple cysts in LIP. Sometimes you can see vascular indentations or septa. These septa can mimic a central dot as in centrilobular emphysema.
- Simple cysts in an area of ground glass.
- Simple cysts with subtle reticulation and ground-glass.
These images are of a 55-year-old man with dyspnoe.
There is a history of mixed connective tissue disease (MCTD) and he does not smoke.
Study the image.
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
The most characteristic finding is the combination of cysts and ground glass.
Discussion
The most likely diagnosis based on the findings is LIP.
The history of MCTD is also helpful.
The diagnosis of DIP is unlikely, since the patient does not smoke and in DIP all the cysts must be localized within an area of ground glass. Here one of the cysts is clearly located within an area of normal lung tissue (arrow).
These images are of a 60-year-old woman with Sjögren's disease, who had a HRCT to screen for interstitial lung disease.
Study the image.
Are these cysts or mimickers?
What is the most likely diagnosis?
Findings
There are a few cysts (more than four, not all shown), so we are probably
dealing with a cystic lung disease. There is some ground glass in the lower
lung fields and some thickened interlobular septa.
Discussion
The combination of cysts and ground-glass limits the differential diagnosis to
LIP and DIP.
In a patient with Sjögren's disease, the diagnosis is LIP.
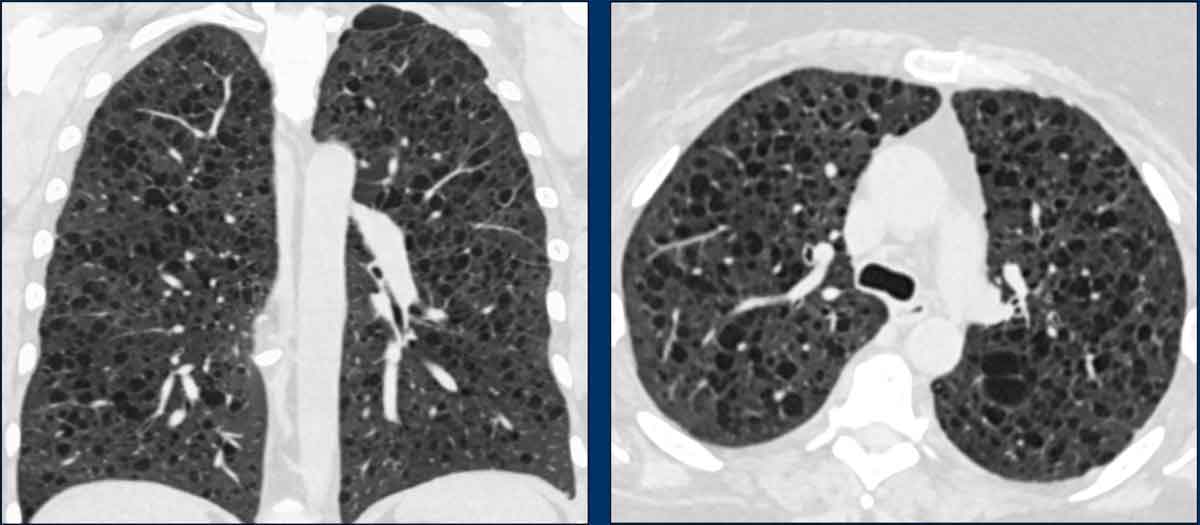
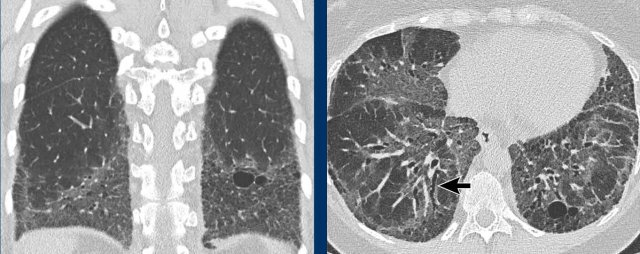
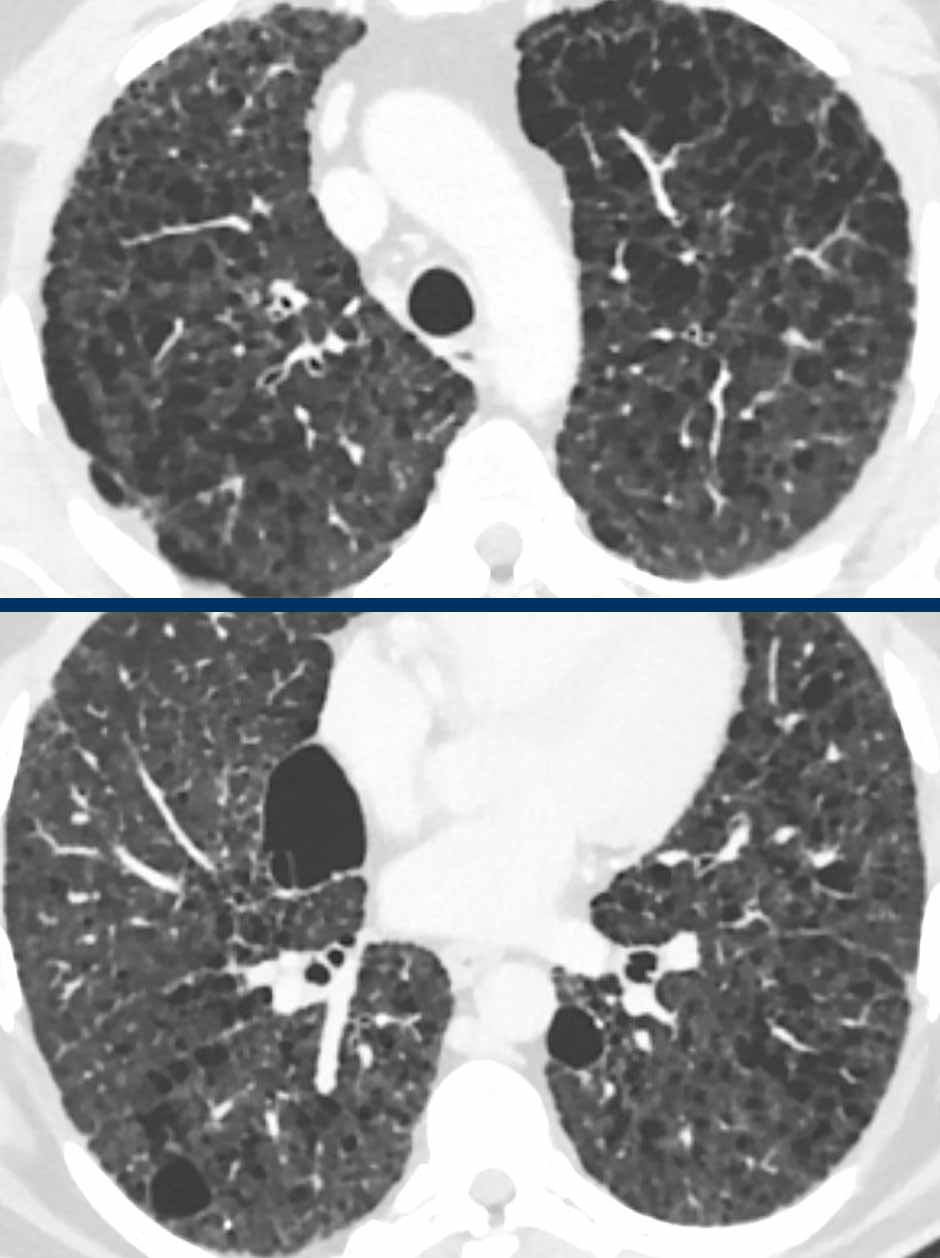
DIP - Desquamative Interstitial Pneumonitis
Desquamative interstitial pneumonitis has a strong association with smoking.
DIP presents as symmetrical cysts within ground-glass with a predominance basally and in the perifery
Often there are also signs of fibrosis.
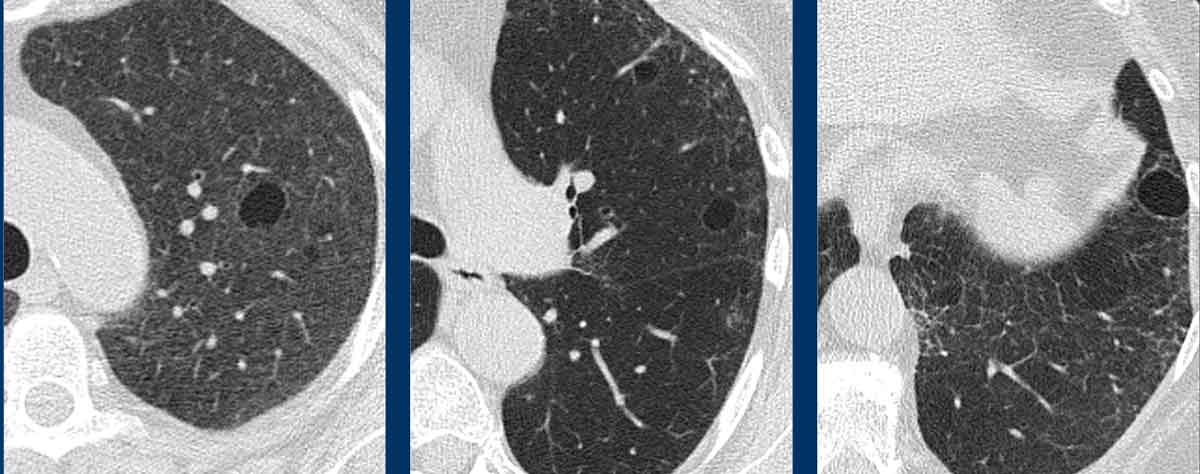
These images are of a 65-year-old woman with dyspnoe and a history of smoking.
Findings
There are thin-walled cysts within areas of ground glass and subtle fibrosis.
Notice the traction bronchiectasis (arrow).
Continue with more images of this patient...
The main differential diagnosis of pulmonary cysts in combination with ground-glass is DIP and LIP.
The most likely diagnosis is DIP, because the patient is a smoker and because the cysts are only located within areas of ground glass.
DIP cysts are located in the periphery of the lower lung fields and frequently combined with fibrosis.
DIP can also have a diffuse
distribution.
This case is an example.
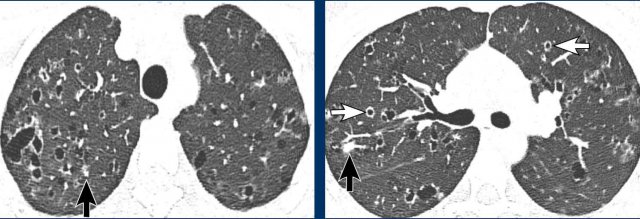
Emphysema
Some examples of emphysema are included here because emphysema can sometimes simulate a cystic lung disease.
Images
- Centrilobular and paraseptal emphysema. Notice the resemblance to 2, but the different distribution (upper versus lower zones) and the presence of central dots (white arrow) helps to distinguish.
- This is not emphysema but a Birt-Hogg-Dubé case with simple cysts in the lung parenchyma and peripleural cysts.
- Paraseptal emphysema.
- Centrilobular emphysema with central dot sign (black arrowheads). Notice the subtle difference with advanced LCH (see Figure 2 above at LCH), which shows more prominent septa or walls.
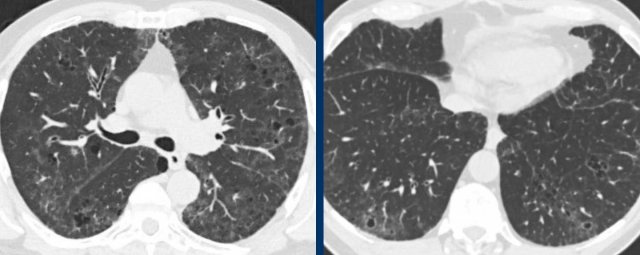
These images are of a 58 year old man with Covid infection since a week.
Findings
Bilateral ground-glass with multiple small cyst-like
lesions.
Discussion
This could be mistaken for a cystic lung disease or for infection with
pneumatoceles.
But notice the subtle ‘central dot’ in some of the lesions (yellow arrows) and in the detail (black arrow).
This is consistent with
centrilobular emphysema.
The emphysema is better visible due to the surrounding
ground-glass.
Uncommon diseases
When the cysts do not fit into the diagnosis of the usual suspects (LAM, BHD, LCH, LIP), then think of uncommon causes of cystic lung disease.
Light chain deposition disease
LCDD is seen frequently as a complication of lymphoproliferative diseases or as a precursor of multiple myeloma.
In LCDD usually the kidneys are involved and only in a minority of cases the lungs are involved.
These images are of a patient with light chain deposition disease (LCDD).
Findings
Typically the walls of the cysts show nodular
thickenings.
Cystic metastases
Lung metastases usually appear as nodules, sometimes with cavitation.
However, in a few cases lung metastases present as true cysts.
Think of cystic lung metastases in a patient with new or progressive lung cysts and a history of malignancy, without another explanation for the lung cysts.
These images are of a patient with a history of thymic carcinoma.
Findings
On a routine follow-up scan some new
cysts with a thin wall appeared.
During further follow up these cysts became
larger and developed a slightly irregular wall.
This turned out to be cystic
metastases of the thymic carcinoma.
Cystic Hypersensitivity Pneumonitis
These images are of a 55-year-old
man, who presents with dyspnoe and coughing.
He has a parrot and does not
smoke.
Findings
There are a few thin-walled cysts in areas with ground glass.
Discussion
The main differential diagnosis of lung cysts in combination with ground-glass
is DIP and LIP.
However when someone has a parrot, you might also consider
hypersensitivity pneumonitis.
And although it is very uncommon, this proved to be hypersensitivity pneumonitis with cystic changes.
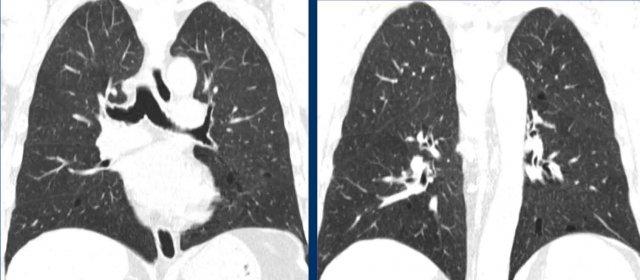
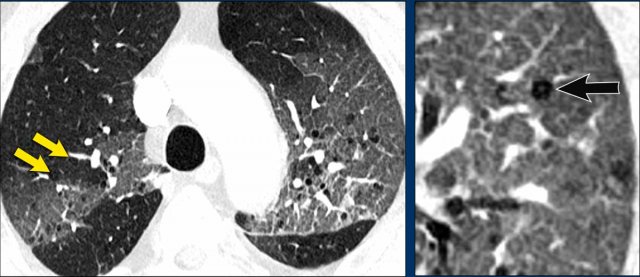
Benign metastasizing leiomyoma
Benign metastasizing leiomyoma is a rare disorder that affects women with a history of uterine leiomyoma, which is found to metastasize most commonly to the lungs, where it presents with nodules, that sometimes cavitate and form cysts.
These images are of a 46-year-old woman. She
has a history of hysterectomy because of uterus myomatosus, and at physical
examination she has a struma.
She does not smoke.
Findings
There are a few thin-walled cysts in combination with nodules (white arrow) and cavitating nodules with a cheerio sign (black arrow).
Continue with the next images...
As always we want to have a good look at the pleural recesses.
We can skip the diagnosis LCH, because the pleural recesses are involved.
In a non-smoker this diagnosis was already unlikely.
High in the differential diagnosis is metastatic disease.
However no malignancy was found.
This proved to be benign metastatic leiomyoma.
Neurofibromatosis type 1
This is a 59 year old man with
neurofibromatosis type 1 (NF1). Although he is a non smoker, there are paraseptal emphysema-like
changes with bullae in the upper fields (arrows).
Multiple smaller cysts are scattered
throughout the parenchyma (arrowheads), including in the pleural recesses.
This combination of bullae in the upper fields and cysts in the middle and lower fields can typically be seen in NF1, together with some fibrotic changes.
Fibrocystic Sarcoidosis
This is an example of fibrocystic
sarcoidosis.
Notice the fibrotic perihilar changes with elevated and distorted
hila (consistent with sarcoidosis), together with the cysts that have an
appearance similar to paraseptal emfysema.
There was no history of smoking and no centrilobular emfysema, which makes the diagnosis of normal paraseptal emfysema unlikely.
Surfactant Protein mutation
These images are of a 45-year-old male patient presenting with mild exertional dyspnea.
Two of his older brothers died from interstitial lung disease without a clear diagnosis, and his mother underwent a lung transplant due to pulmonary fibrosis.
The patient's CT scan reveals extensive and widespread lucencies.
Initially, these were interpreted as emphysema, but the patient has no history of smoking.
While many lucencies appear emphysematous, most lack a central dot.
Additionally, some definite true cysts with walls are observed.
Langerhans Cell Histiocytosis (LCH) was considered due to the bizarre shape of some lucencies, but pleural involvement and a negative CD1a test ruled it out.
Given the positive family history and atypical lung abnormalities, a genetic disease was deemed most likely.
This case was ultimately attributed to a Surfactant Protein C (SP-C) mutation.
Alveolar lining fluid requires surfactant to prevent alveolar collapse at end-expiration, which is facilitated by the interaction of phospholipids with the hydrophobic surfactant proteins SP-B and SP-C.
Genetic mutations in SP-B and SP-C can lead to cystic disease, ground-glass opacities, and fibrosis.
This condition is a distinct and uncommon entity within Familial Pulmonary Fibrosis (FPF).
Our patient primarily exhibits cystic disease, with a small amount of ground-glass opacities and no obvious signs of fibrosis to date.
Solitary cyst
In this chapter we will show you some cases of solitary cysts.
Use the diagnostic approach and try to come up with a differential diagnosis.
Case 1
These images are of a 67-year-old
woman who quit smoking twelve
years ago.
She now has an HRCT.
Findings
In the right lower lobe is a true cyst with a nice thin wall without any irregularities.
Discussion
This is regarded as an incidental cyst without any clinical meaning.
These incidental cysts are usually located in the periphery of the lower lobes.
Case 2
These images are of a 58-year-old man.
He has periods of productive coughing especially when he was lying on his left side.
No smoking history.
Study the images.
Is this a cyst or a mimicker and what
is the most likely diagnosis?
Findings
There is a cyst in the right upper lobe and this was the only cystic structure
in the lungs.
Discussion
You could think of an incidental cyst, but that cannot explain the coughing and
the wall is slightly thicker.
It was decided to do a follow up scan
Continue with the next images...
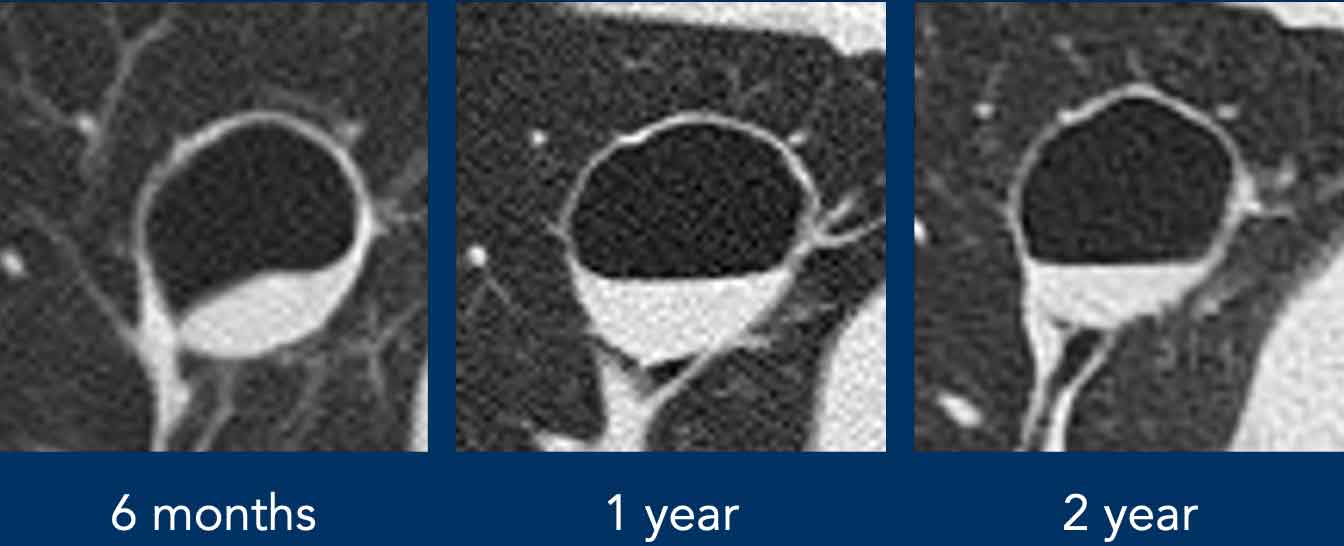
The follow-up image taken six months later reveals what appears to be wall thickening, prompting a PET-CT scan to assess for signs of malignancy.
The PET scan results were negative, and further monitoring was carried out, during which an air-fluid level was observed.
Given this finding, along with the lesion's proximity to the bronchus, the most likely diagnosis was a bronchogenic cyst.
Due to persistent symptoms, the cyst was surgically removed, and the diagnosis was subsequently confirmed.
The episodes of coughing were believed to be due to infected material within the cyst draining into the bronchial tree.
Bronchogenic cysts are congenital anomalies that have lost their normal connection to the bronchial tree.
They are typically filled with fluid, making this a rare presentation.
Case 3
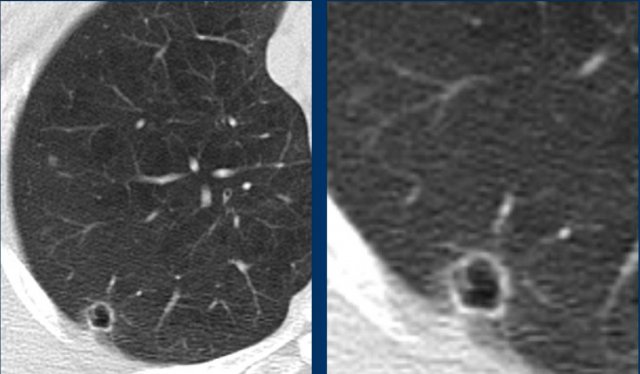
This image and detail are of a
56-year-old woman with a solitary cyst-like
lesion.
Study the image.
Is this a cyst or a mimicker and what is the most likely diagnosis?
Findings
There is centrilobular emphysema and an air-filled lesion with an irregular wall.
Discussion
The primary concern is the possibility of cystic lung cancer.
Proceed with the subsequent images for further evaluation...
A scan conducted one year prior identified a small nodule at the same location.
This is a highly concerning finding.
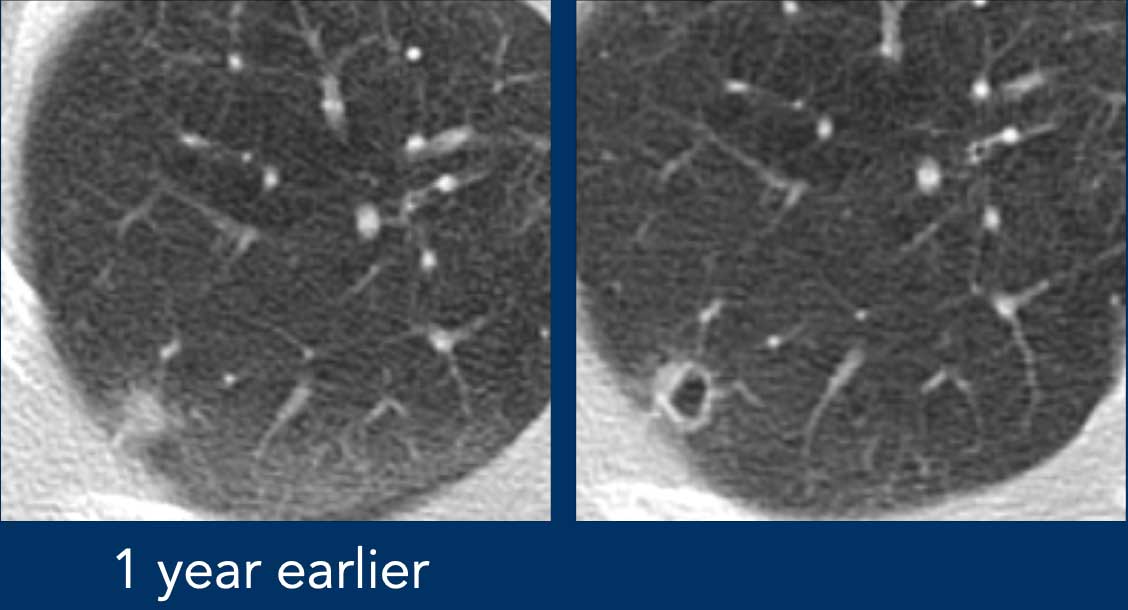
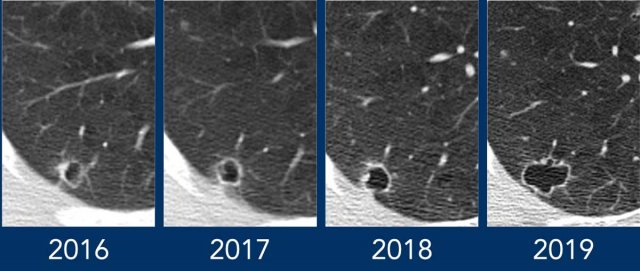
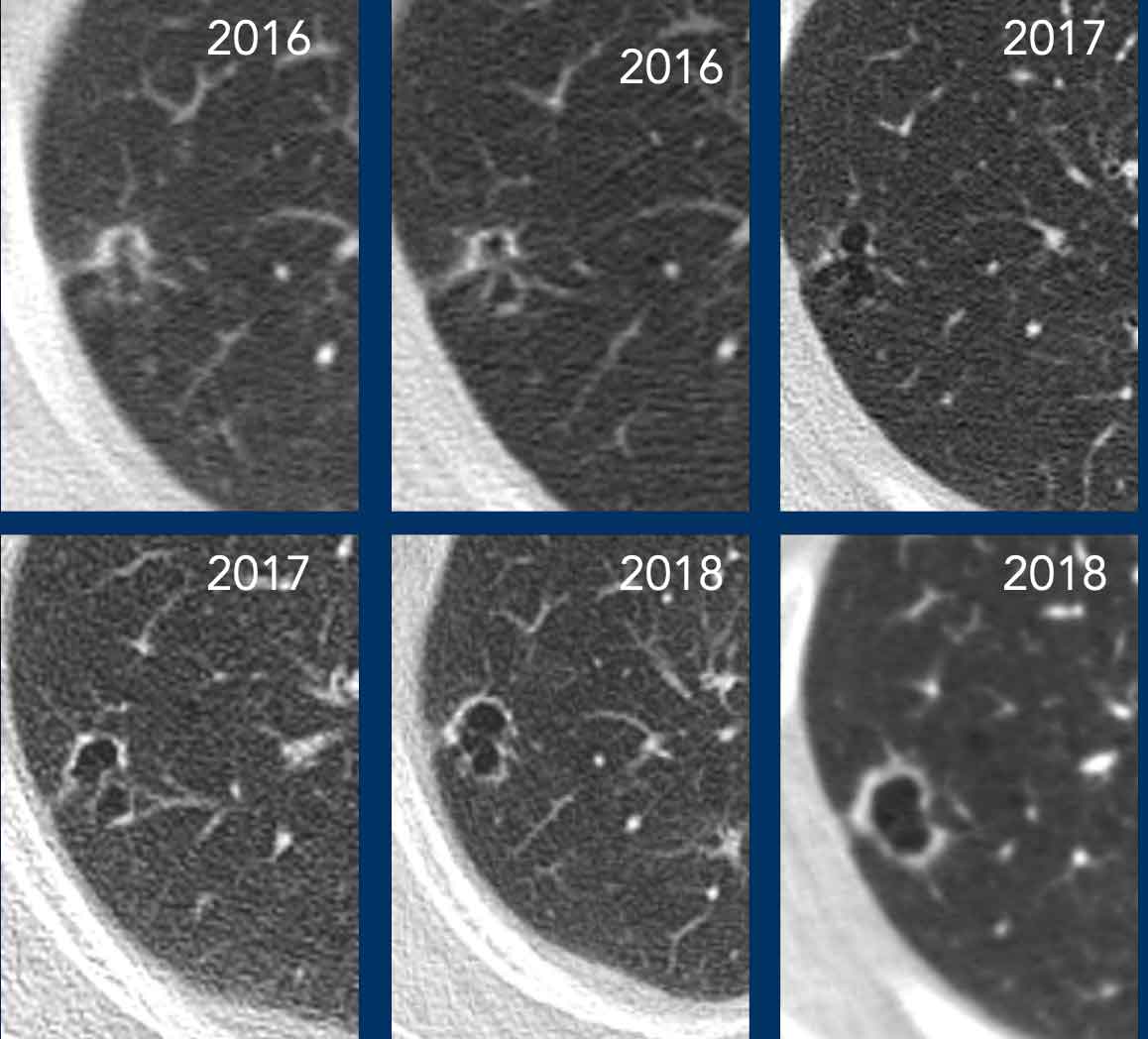
Continue...
It was decided to continue the follow
up.
Between 2016 and 2017 the wall becomes thinner.
This is probably the result of
progressive necrosis and is not a sign of benignity.
In 2019 a PET-CT was performed which again showed only minimal activity.
This also should not reasure you.
It can be explained by the minimal solid component.
Final diagnosis was non-small cell lung cancer.
Continue...
Case 4
This is a similar case of cystic lung cancer.
Read more about cystic lung cancer on the Radiology Assistant in the article of Onno Mets.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.