Pathology of the Male Breast
Leonard M. Glassman
Publicationdate
This review is based on a presentation given by Leonard Glassman and adapted for the Radiology Assistant by Robin Smithuis.
We will discuss:
- Normal male mammogram
- Classic features of gynecomastia
- Lesions that require a biopsy
by Leonard M. Glassman
Normal Male Mammogram
When you do breast imaging in a male, always stick to the following rule:
'If it is not normal, gynecomastia or classically benign,
it needs a biopsy'.
So, first we're going to give you a couple of examples of the normal male breast, just to get used to what normal looks like.
Then we will discuss gynecomastia and finally discuss some specific tumors.
Obviously, the lesions in this last category will need a biopsy, unless you are sure that it is classically benign, like for instance a lymph node or lipoma.
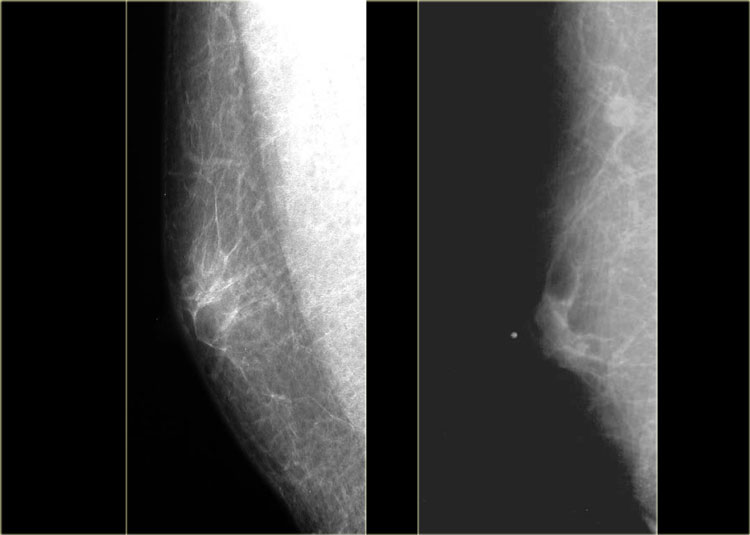
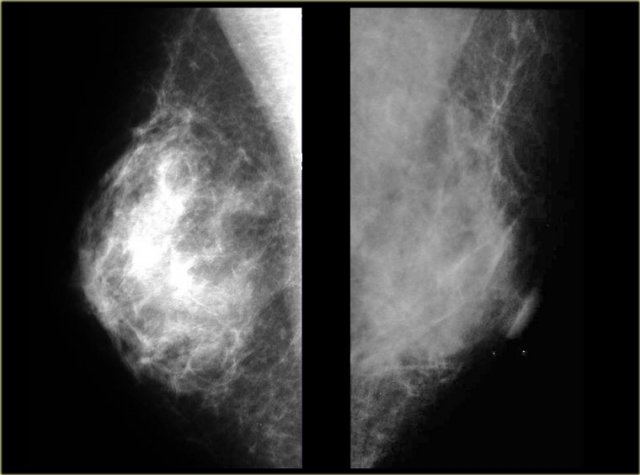
On the left two examples of a normal male mammogram.
The left image shows normal skin, a nipple and a small amount of connective tissue behind the nipple.
The image on the right shows a bit more connective tissue, but this is still normal.
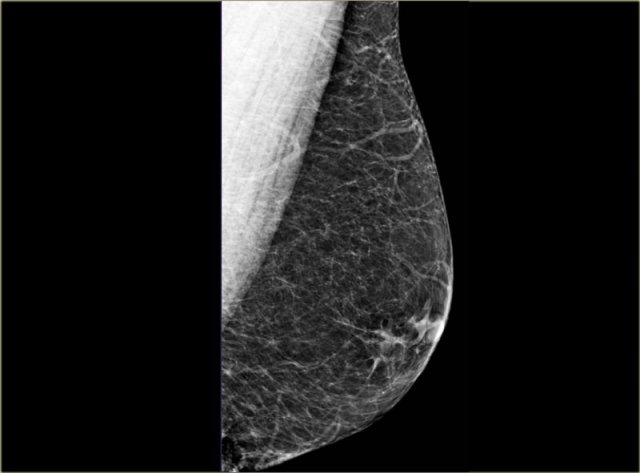
On the left another normal male breast.
There is more fatty tissue and there are a number of blood vessels.
There is a small amount of fibrous connective tissue, but basically most of this breast is just fat.
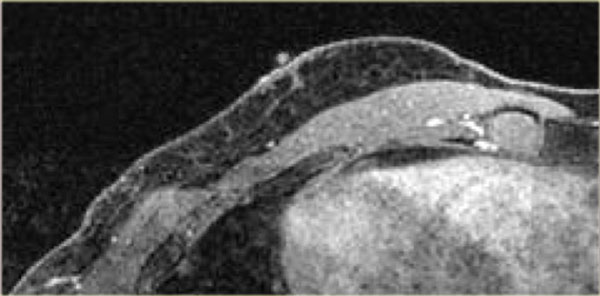
On the left a MRI of the normal male breast.
There is a small amount of connective tissue behind the nipple.
Gynecomastia
Gynecomastia is the most common abnormality in the male breast.
Clinically, it presents as a soft mobile tender subareolar mass.
Every word in this sentence is critical:
soft - mobile - tender - subareolar .
So it has to be soft and mobile.
It is tender in the acute phase, but not in the chronic phase.
Gynecomastia must be subareolar!
Any mass that is not subareolar is not gynecomastia.
Imaging pattern
There are three imaging patterns:
- Nodular glandular (acute florid phase)
- Dendritic (chronic fibrotic phase)
- Diffuse glandular
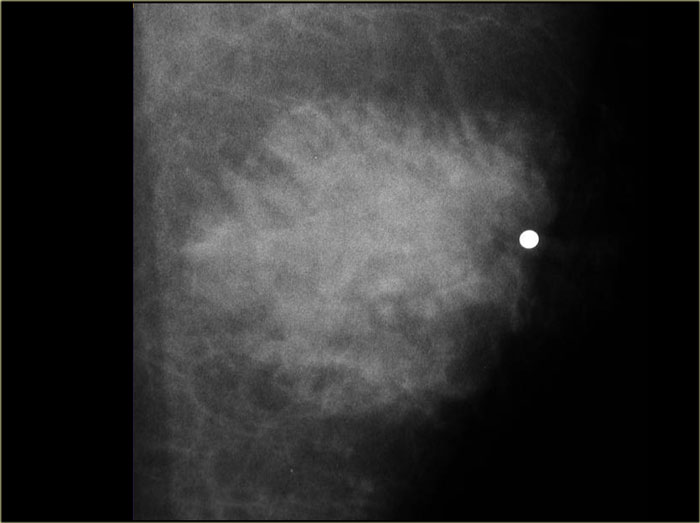
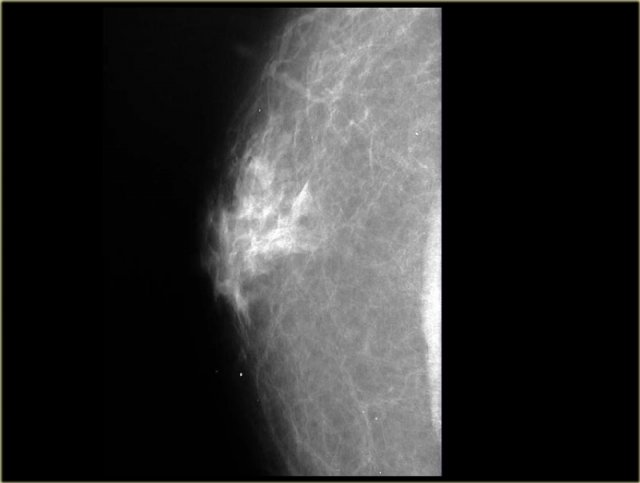
On the left a male breast with a nodular glandular pattern of gynecomastia.
There is a fan shaped density radiating from the nipple.
It may be more prominent in the upper outer quadrant and, more importantly, it blends into the surrounding fat.
If you think about the mammogram on the left as the breast of a woman instead of a man, than you might say that there is an ill-defined mass and you might conclude that this is a malignancy .
However, in a man this indistinct border is a sign of a gynecomastia.
Gynecomastia is simultaneous proliferation of ducts and stroma without encapsulation, so it must blend into the surrounding fat tissue.
There is no proliferation of lobuli, like there is in women.
So you will not see tumors that start in the lobuli, for example lactating adenomas, fibroadenomas, phyllodes tumors, and also invasive lobular carcinomas are extremely rare.
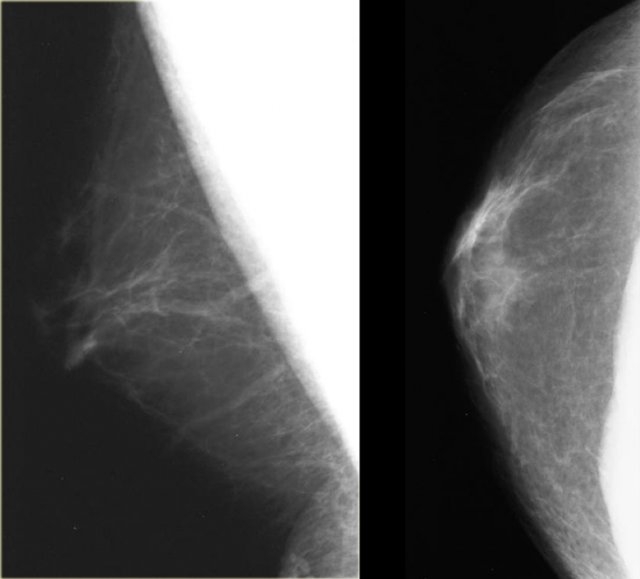
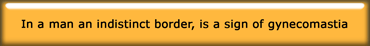
On the far left a mammogram of a male with gynecomastia and next to it a mammogram of an eight year old girl with juvenile hypertrophy.
Notice that they look very much the same.
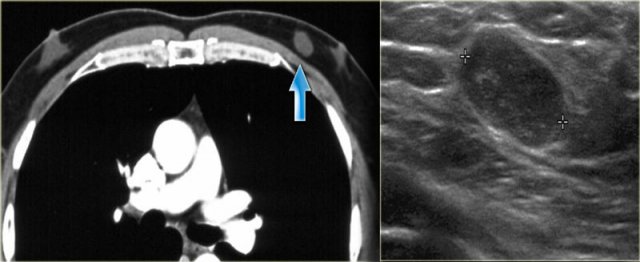
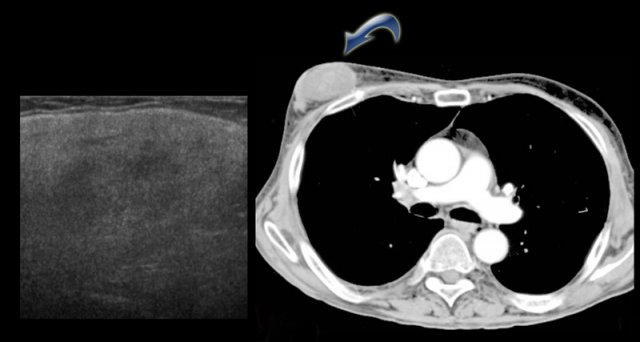
On the left unilateral gynecomastia.
This was an incidental finding on a CT-scan done for some other reason.
By definition gynecomastia is 2 cm or more of subareolar tissue in a non obese male.
It is a common 'normal' finding, that is seen in 55% of men at autopsy.
The peak incidence is 60 - 69 years.
It is significant if it is new or symptomatic.
In elderly males gynecomastia makes up 65% of all breast lesions.
25% is carcinoma and 10% are other lesions.
Nodular pattern
The nodular pattern of gynecomastia is seen in the florid early phase.
It begins as an increased number of ducts and epithelial proliferation with edema and cellular fibroblastic stroma.
This phase is reversible.
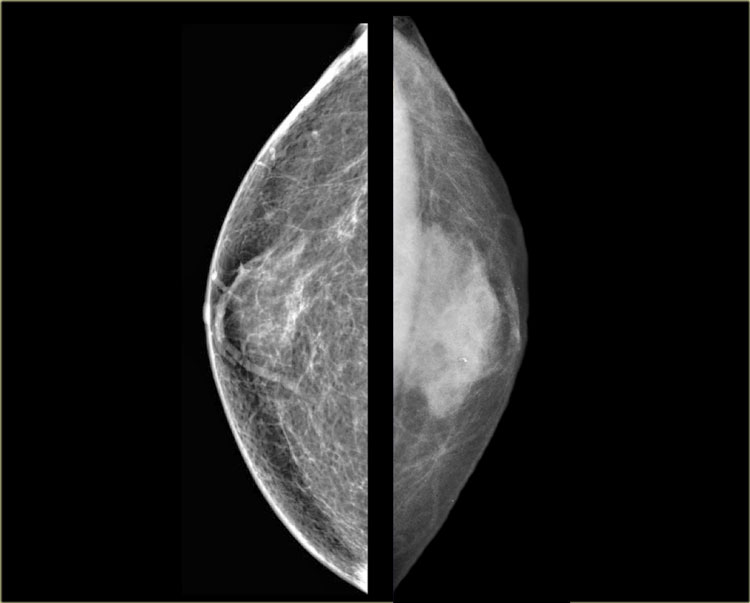
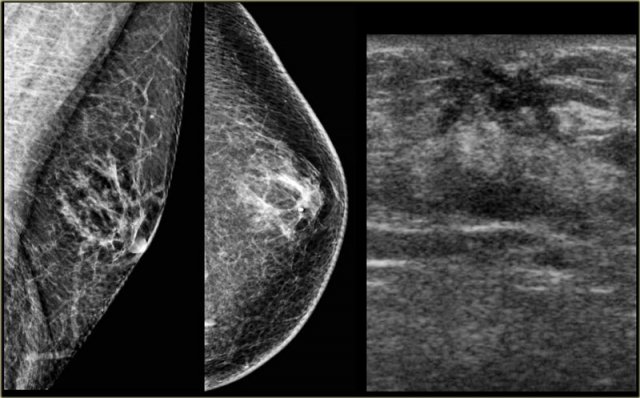
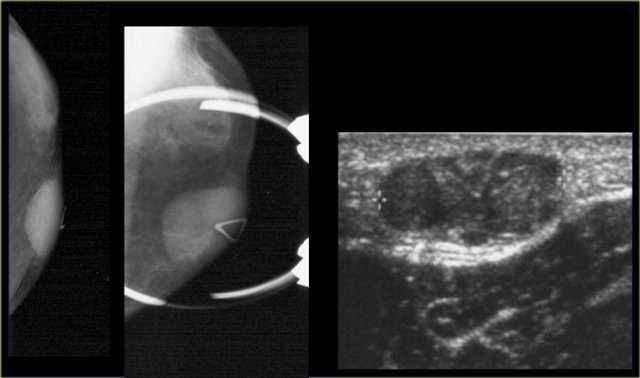
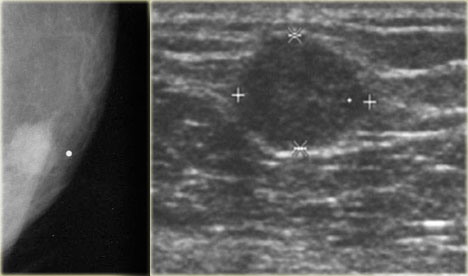
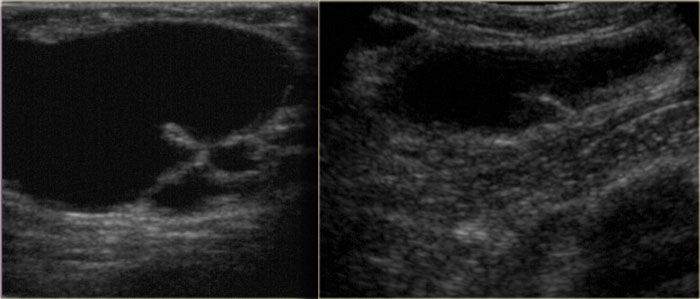
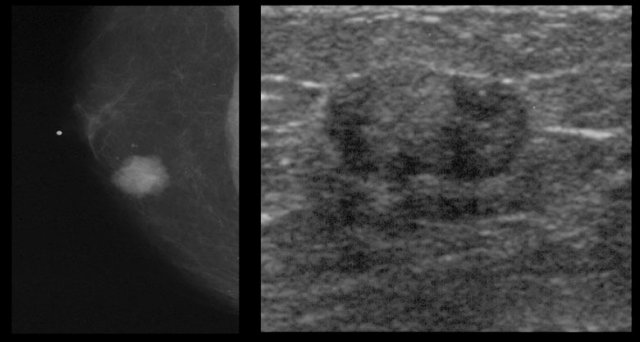
On the left a mammogram and an ultrasound image of a patient with a nodular glandular pattern of gynecomastia.
Notice that it is situated underneath the nipple.
The ultrasound image shows the typical appearance of gynecomastia: a hypoechoic mass with lobulation or even spiculation.
If this was seen in a woman, you would say that this is a mass with microlobulation and spiculation, i.e. Birads IV or V.
In a man this is typical for gynecomastia.
On the left the same ultrasound image, but now in the normal position.
Notice how 'malignant' it looks.
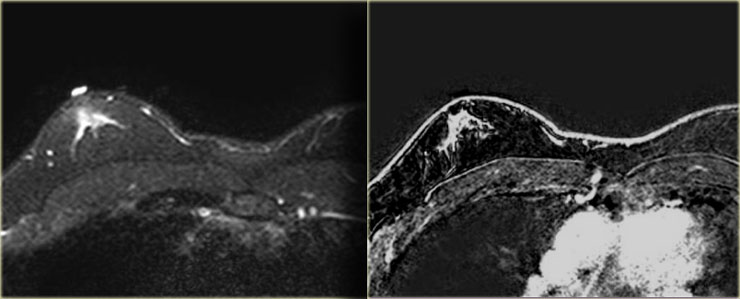
On the left a T2W-image with fatsat and a T1W-image after Gadolinium with fatsat.
A radiologist who was not used to looking at 'male' mammograms ordered the MR for problem solving.
Obviously this MR was performed for the wrong reason.
MR should not be used to solve a problem that can be solved with mammography.
Anyhow the MR shows gynecomastia of the nodular pattern.
Dendritic Pattern
The dendritic pattern is seen in the fibrotic or late phase.
There are dilated ducts, moderate epithelial proliferation and fibrosis.
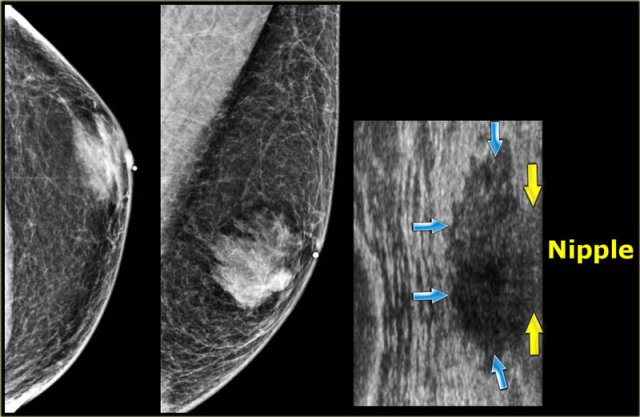
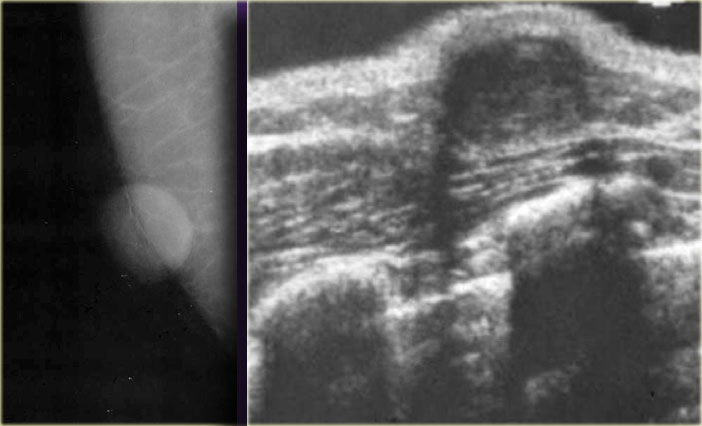
On the left a mammogram showing a subareolar density with prominent extensions into the fat.
Usually the density is smaller than in the nodular pattern.
On the mammogram on the left we can imagine, that there is fibrosis with extension into the fat.
This is different from the glandular edema-like appearance in the acute phase of gynecomastia.
The ultrasound shows a spiculated appearance.
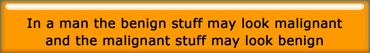
These cases clearly demonstrate that gynecomastia can have an appearance which we would call malignant in a woman.
Unfortunately some of the malignant lesions in a man can look benign and we will show some examples in the next chapter.
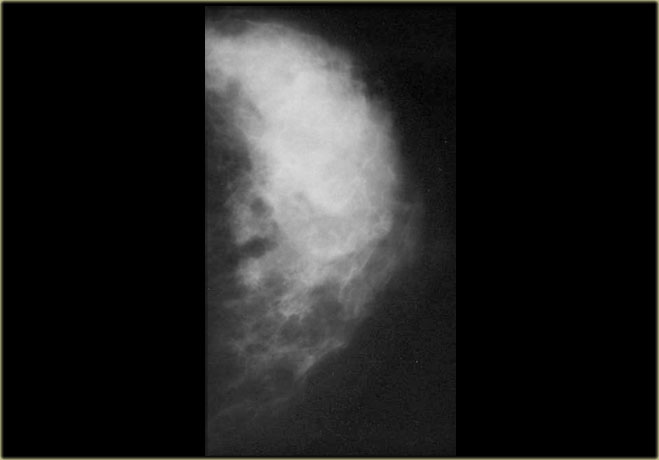
Diffuse glandular pattern
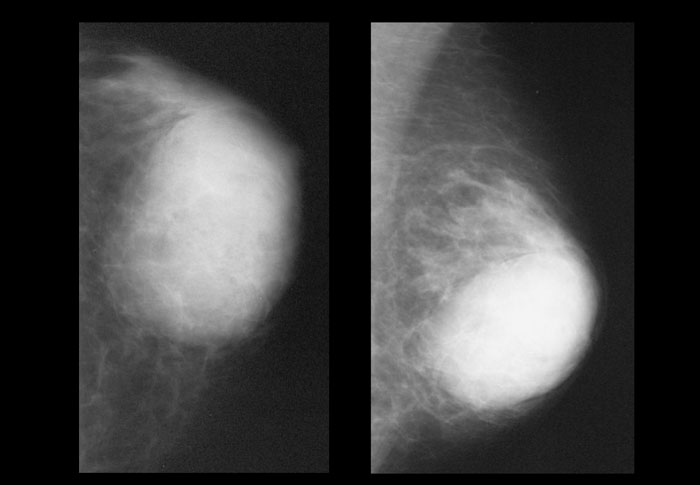
This pattern is seen in males with very high estrogen levels.
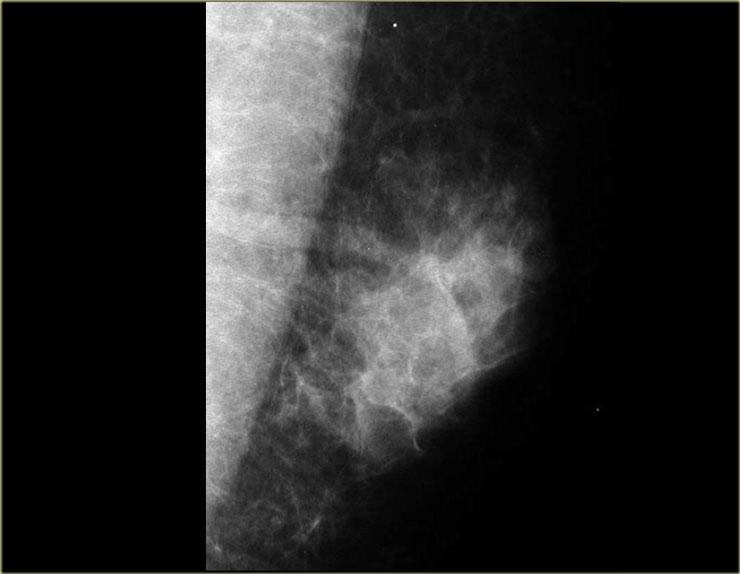
The images on the left simply look like small female breasts.
This was a patient who was on estrogen therapy for prostate carcinoma.
Pseudogynecomastia
This is usually bilateral and there is no palpable mass.
Remember that gynecomastia presents clinically as a soft, mobile, tender, subareolar mass.
Pseudogynecomastia results from excessive fat deposition in the breast area.
It is seen as a normal variant, in obesity and in neurofibromatosis.
Benign Lesions
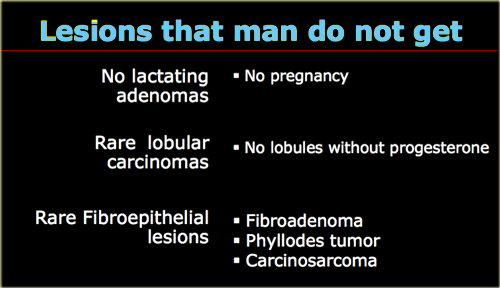
Let's first start with a list of lesions that should not be diagnosed in male patients, because they simply do not get these lesions.
A man does not get a lactating adenoma, because it is only seen in pregnancy.
Because there are very few lobules in a man, lobular tumors are extremely rare.
There are only a few invasive lobular carcinomas reported in men.
Fibroepithelial lesions are also extremely rare because they too start in the lobules.
So do not diagnose a fibroadenoma in a man, even if it looks like a fibroadenoma.
When you get a biopsy result that says fibroadenoma, get another pathologist.
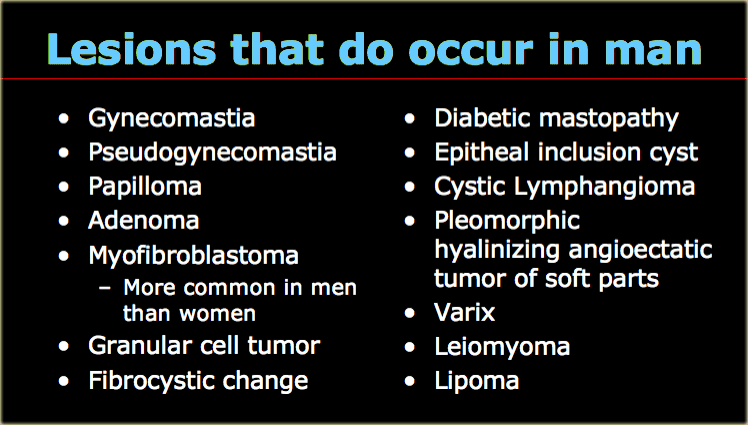
On the left lesions that do occur in males.
Exept for gynecomastia and pseudogynecomastia, in most of these lesions we will not get a diagnosis from imaging.
We just report that there is a Birads IV lesion and do a biopsy.
Myofibroblastoma
Myofibroblastoma is an interesting lesion because it is the only one lesion that is more common in men than in women.
It presents as a freely moveable, solitary, palpable, firm mass.
There are no calcifications.
The mean age is in the late 50's.
On the left a large lesion, that looks like a fibroadenoma.
Now we know that men do not get fibroadenomas.
The pathology diagnosis was myofibroblastoma and the lesion was treated with local excision.
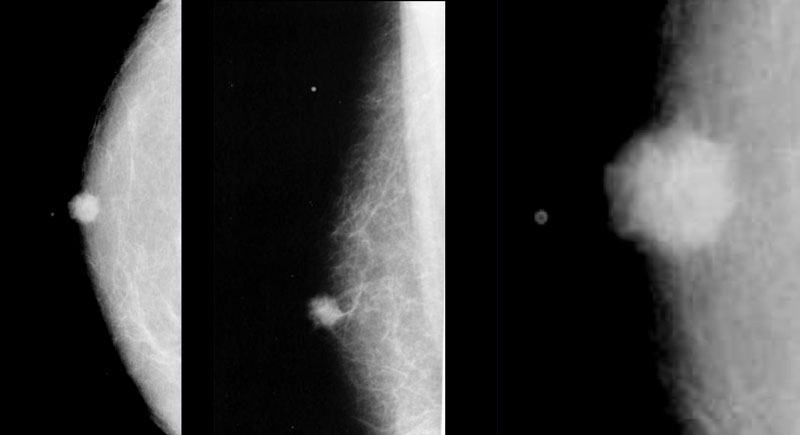
On the left another myofibroblastoma.
It presents as a circumscribed lobulated mass without calcification.
Notice that the lesion is eccentric to the nipple.
It is the lobulated mass that needs to be biopsied, not the retromamillary gynecomastia.
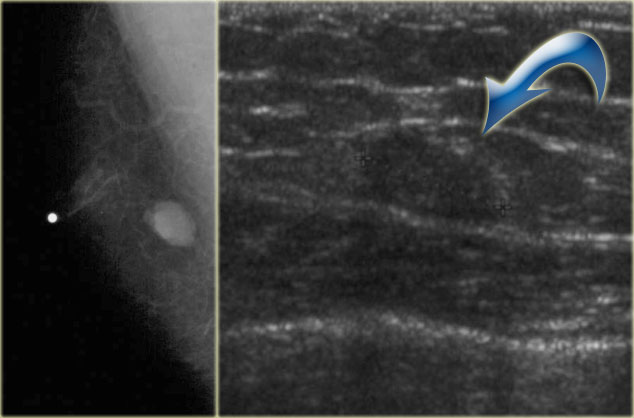
On the left another myofibroblastoma.
The nipple is marked and the lesion is not retromamillary.
On the ultrasound image the lesion is difficult to differentiate from the surrounding fat.
On the left another myofibroblastoma.
Even if this lesion was located behind the nipple, you would not diagnose this as gynecomastia, because it is a lobulated mass.
Granular Cell Tumor
This is a benign tumor of neural origin.
They occur anywhere in the body.
6% occur in the breasts.
They are typically seen in men in their 30's.
Usually they present as circumscribed in males, but sometimes they have a spiculated appearance.
Notice that the lesion on the left has a indistinct border as is usually seen in gynecomastia, but on the mammogram it is not located directly under the skin.
So this is not gynecomastia and a biopsy is necessary.
On the left another Granular cell tumor.
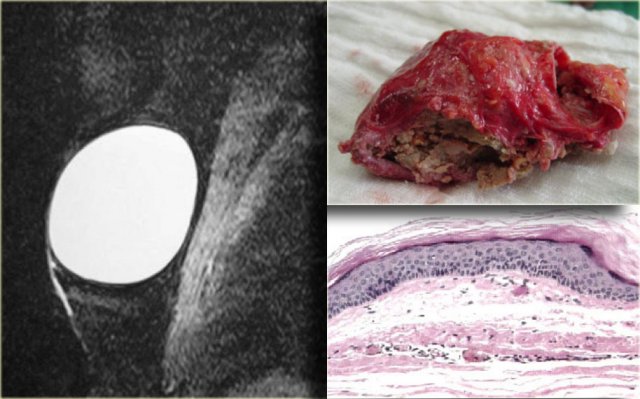
Epidermal inclusion cyst
Epidermal inclusion cyst is a skin lesion.
It presents as a round well circumscribed dense mass.
On the left a small epidermal inclusion cyst.
Notice how it raises the skin.
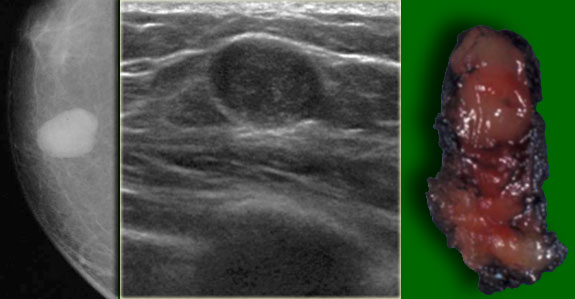
On the left a large epidermal inclusion cyst.
On the left a T2W image demonstrating the cystic nature and the pathology specimen.
Granulomatous Mastitis
Most are idiopathic.
Specific causes must be excluded like TB, Sarcoid and fat necrosis.
On the left is a male breast that looks like the breast of a female.
These lesions can sometimes be spiculated.
Varix
On the left a lesion that looks like a cyst, but remember that cysts originate in the lobules and men do not have lobules, unless they take estrogen.
This is a varix and if you puncture it, you get a big red surprise.
Leiomyoma
On the left a lesion, that looks like a fibroadenoma, but men do not get fibroadenomas.
It is a solid encapsulated mass and at biopsy it happened to be a leiomyoma.
If there are more than 2 mitoses per high power field the pathologist calls it a leiomyosarcoma.
Male Breast Cancer
Malignant disease in men just looks like malignant disease in women.
In the USA there are about 1700 new cases each year, which is 1% of all breast cancer.
There is a higher incidence in people from China and Africa due to hyperestrogenism secondary to parasitic liver disease.
These cancers present as a unilateral painless subareolar mass.
This subareolar location is just like in gynecomastia, but usually it is eccentric to the nipple.
It sometimes presents with bloody nipple discharge, which is unlike gynecomastia.
Usually it is invasive ductal cancer.
As stated above invasive lobular cancer is extremely rare.
Also DCIS is rare because there is no screening program for men, so they will present when there is a palpable mass.
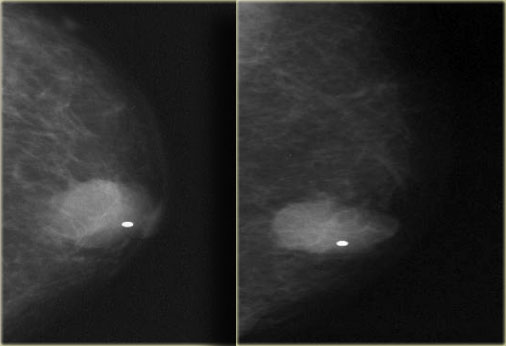
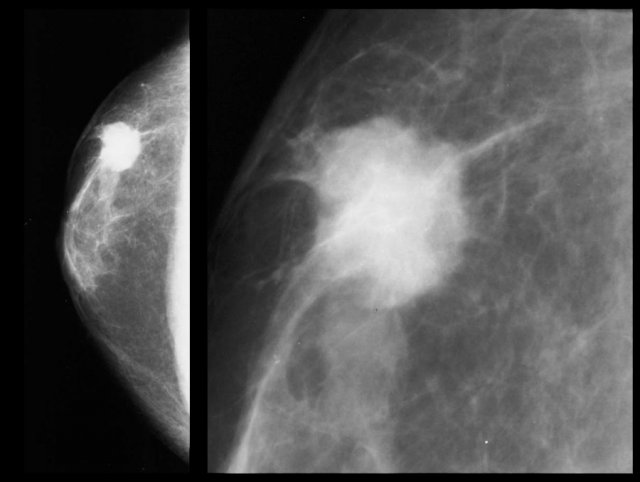
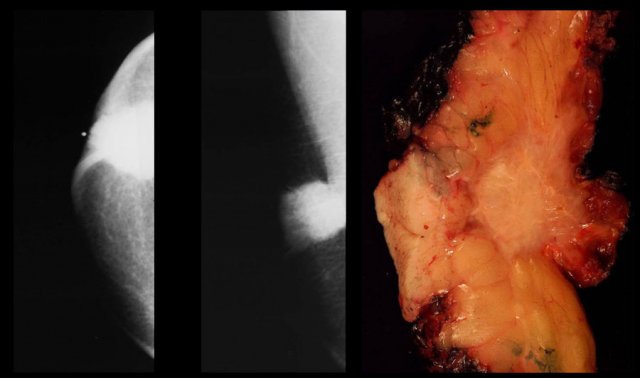
On the left an eccentric irregular mass with spiculae.
If this was a women you would have no trouble in diagnosing this as a cancer.
In a man it is the same.
Male breast cancer presents as a round, oval or irregular mass.
Calcifications are rare, but when they occur they are coarser than in women.
On the left a small invasive ductal carcinoma.
It is subareolar and central, but it is also encapsulated.
This is not gynecomastia.
Paget's disease of the nipple and skin ulceration are more common than in women.
On the left an invasive ductal carcinoma with skin retraction.
There is a long list of carcinoma risk factors and they are the same as in women:
- Advanced age
- Family history
- Jewish heritage
- Chest wall irradiation
- Hyperestrogenism
- Hyperthyroidism
- Exposure to hepatotoxins
- Occupational exposure to high heat (steel industry)
- BRCA 2 is seen in 4 - 16% of male breast cancer patients (40% in Iceland)
- Undescended testes
- Orchiectomy and orchitis
- Klinefelter's syndrome (47, XXY - 6% of all male breast cancer is in Klinefelter - 3% lifetime risk)
On the left a small eccentric encasulated invasive ductal carcinoma.
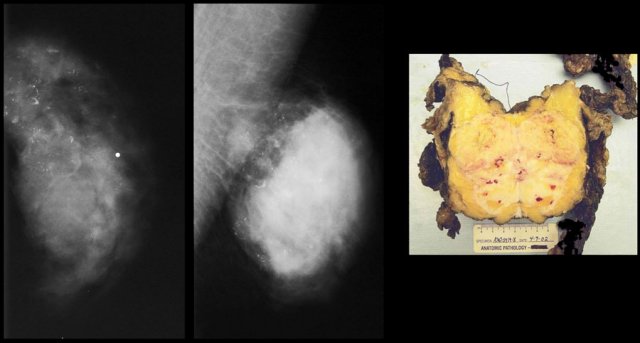
On the left a huge invasive ductal carcinoma with some coarse benign looking calcifications.
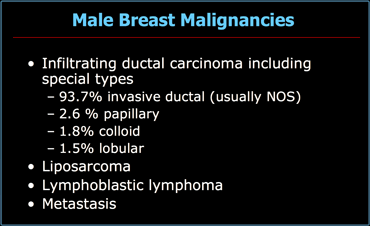
Other malignancies of the male breast
Malignancies other than ductal carcinoma are uncommon.
On the left a list of all malignancies in men.
Metastases
Metastases from prostate cancer are the most common metastases in males.
It results from hematogenous spread and is usually seen in patients with widespread disease.
It presents as round or lobulated non-calcified masses.
On the left a patient with two metastases of a small cell lung carcinoma.
Liposarcoma
A liposarcoma is a rare sarcoma.
It presents as a slowly enlarging painful mass.
It is usually of water-density and is not typically fatty.
On the CT on the left you can see the density of the lesion that proved to be a liposarcoma.
Conclusion
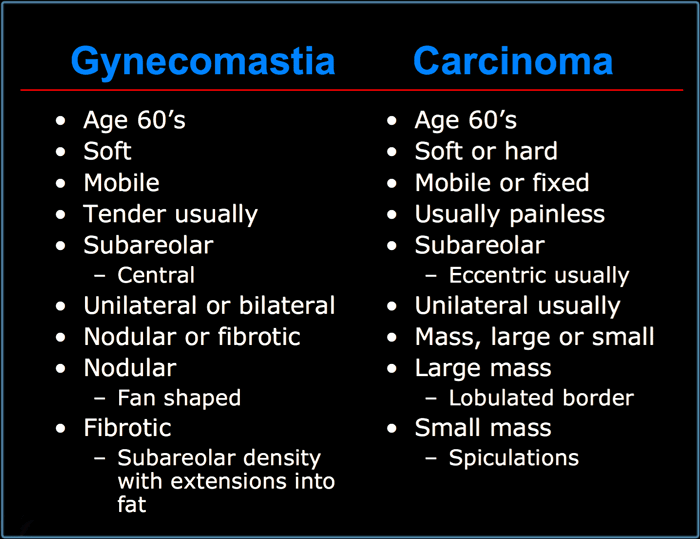
Gynecomastia versus Carcinoma
In conclusion we can say, that male breast disease either presents as mass, pain or nipple discharge.
Gynecomastia and invasive ductal cancer are the most common lesions in the male breast, but there are other rarer benign and malignant lesions.
Gynecomastia and carcinoma can usually be differentiated, but biopsy is sometimes necessary to separate them.
All lesions eccentric to the nipple need biopsy unless they are characteristically benign, i.e.contain fat or typical lymph node.
On the left a list of characteristics of gynecomastia versus carcinoma.
Notice that there are many similarities.
Both gynecomastia and carcinoma occur mostly at the age of 60 and can be soft, mobile, subareolar and unilateral.
So that does not help.
Carcinoma is usually eccentric, while gynecomastia is never eccentric.
Gynecomastia has to have extensions into the surroundig fat.
Carcinoma sometimes may have spiculations, that can look the same.
Actually we call it extension into the fat, if we think it is gynecomastia and spiculation, if we think it is a carcinoma.
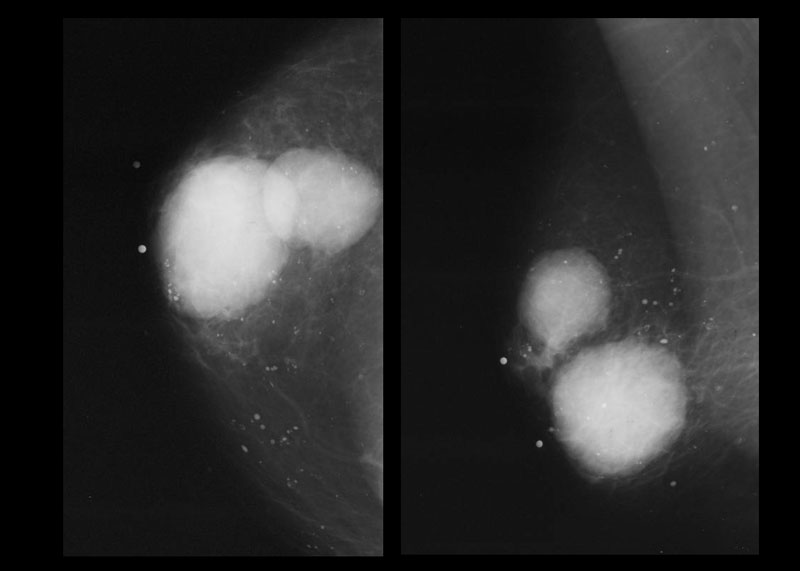
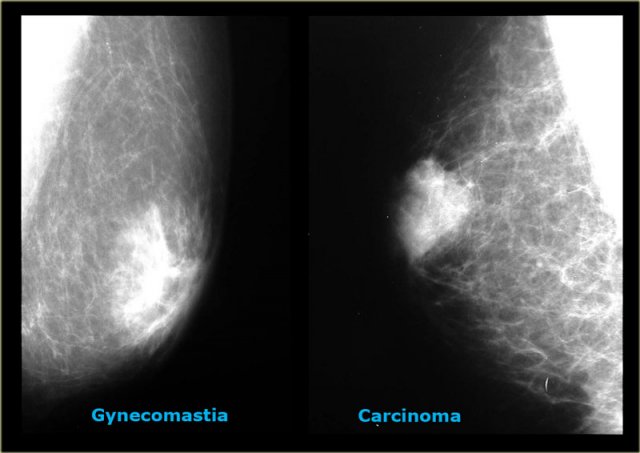
On the left two cases, that demonstrate, that it can be difficult to differentiate gynecomastia from carcinoma on a mammogram.
The carcinoma on the right is a little bit more encapsulated than the gynecomastia on the right.
In less than 10% of the cases a biopsy can be needed to make the differentiation.
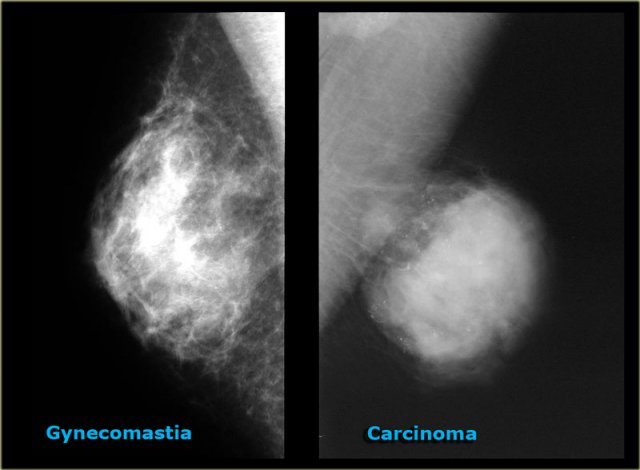
On the left two more cases.
On the far left there is diffuse gynecomastia.
On the right a huge cancer which is encapsulated.
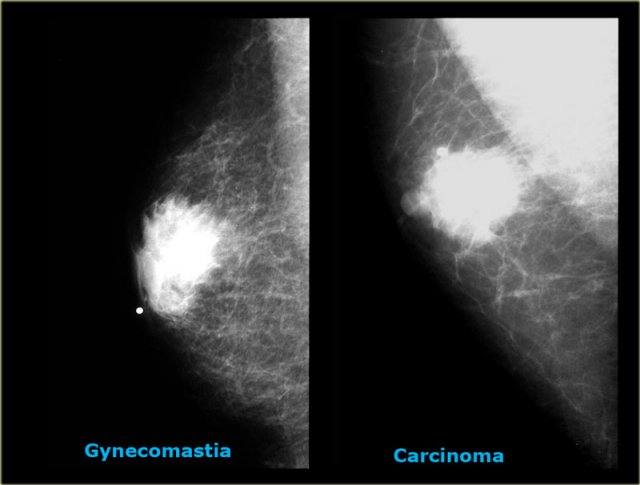
The last cases on the left look very similar to each other.
Based on the mammogram these two can not be differentiated.
In those rare instances a biopsy is needed.