Cartilage tumors
with special attention to Atypical Cartilaginous Tumors
Kirsten van Langevelde and Robin Smithuis
Leiden University Medical Center and the Alrijne hospital in Leiden, the Netherlands
Publicationdate
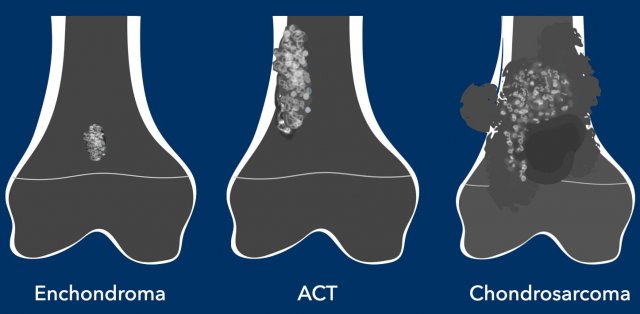
Cartilage or chondroid tumors are a heterogeneous group of bone
tumors that all share a chondroid matrix.
They range from benign enchondromas
to highly malignant chondrosarcomas.
Low-grade chondrosarcomas of the long
bones have been classified as an
intermediate group and are
now called atypical cartilaginous tumor (ACT), because these
tumors rarely metastasize and have a better
clinical outcome compared to the same tumor in the axial skeleton.
The recommended treatment of ACT has
changed over the years from resection to curettage
and even "watchful waiting" with MRI follow-up [1].
Due to these changes in management, imaging plays a
major role in the diagnosis and follow up of ACT.
In this article we will discuss:
- How to make the diagnosis of a chondroid tumor.
- How to differentiate ACT from enchondromas and from high grade chondrosarcomas.
- Follow up of ACT.
Introduction
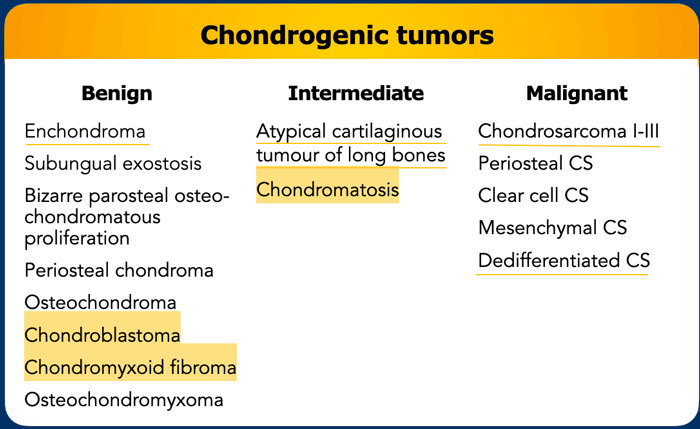
Cartilage tumors share the characteristic production of a chondroid matrix with frequently typical matrix calcifications.
They vary in severity from benign enchondromas and locally aggressive atypical cartilaginous tumors (ACT) to malignant chondrosarcomas.
About 10% of chondrosarcomas are dedifferentiated, which is a highly malignant variant of chondrosarcoma.
Atypical cartilaginous tumors (ACT)
have been classified as intermediate grade chondroid tumors by the World Health
Organization in 2013.
“Intermediate”
means that these tumors may behave locally aggressive but rarely
metastasize (< 2%).
Since 2020 intermediate lesions in the appendicular skeleton are called ACT, while the same lesions
located in the axial skeleton are called chondrosarcoma grade I (CS-I) because they have a poorer outcome.
The term CS-I is therefore reserved for these tumors in the
axial skeleton, meaning the spine,
pelvis, ribs, sternum, scapula and
skull base.
Task of the radiologist
Enchondromas are benign and do not need follow up.
High grade chondrosarcomas are treated with wide resection, since they are insensitive to chemotherapy and radiation.
For ACTs watchful waiting
with MRI follow up is replacing surgical intervention in many centers.
Given these developments,
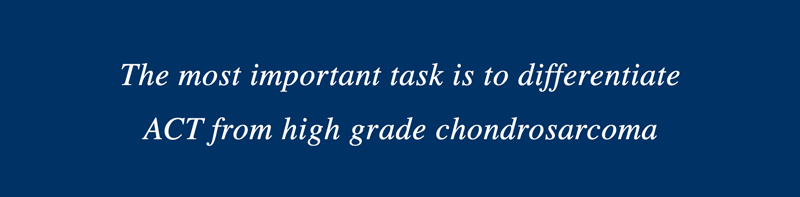
the most important task for the musculoskeletal radiologist is to differentiate
ACTs from high grade chondrosarcomas.
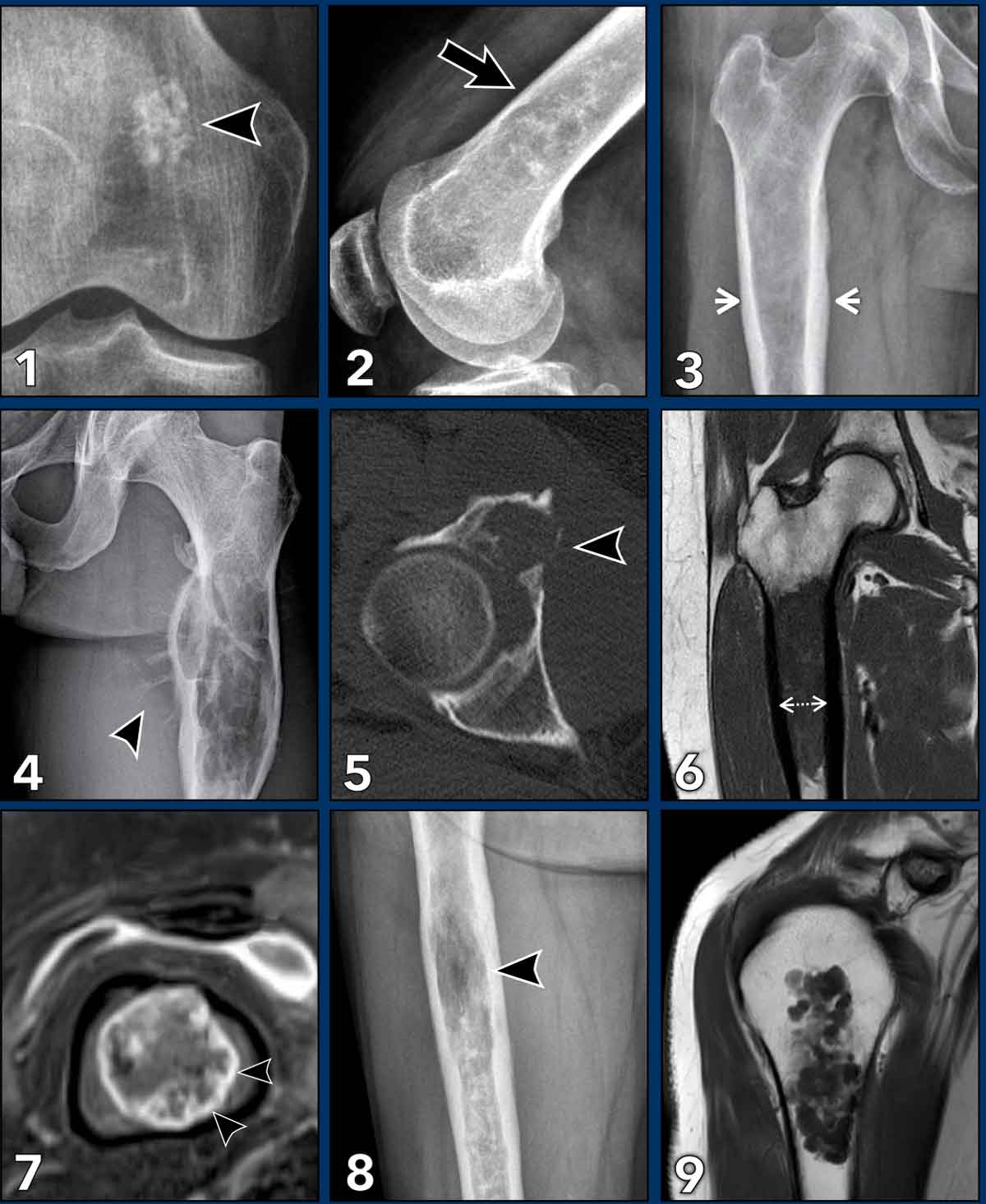
Terminology in Chondroid tumors
This figure demonstrates
examples to explain the terminology used to describe chondroid tumors.
In some examples there can
be more than one typical finding.
- Popcorn calcifications typically seen in cartilaginous tumors.
- Scalloping refers to resorption of the inner layer of the cortex by a slow growing lesion. Most commonly seen in ACT, but may also be present in fibrous dysplasia, giant cell tumors of bone or Langerhans cell histiocytosis.
- Expansion means widening of the bone, this may occur in ACT but is a worrisome feature for higher grade chondrosarcoma.
- Periostitis or periosteal reaction is a typical finding in high grade chondrosarcoma, however it may be present after a fracture in enchondroma or ACT. Sometimes the periostitis is only visible on MRI by a rim of T2 hyperintense signal and enhancement around the cortex.
- Cortical destruction means that a tumor focally grows through the cortex. A typical finding in high grade chondrosarcoma
- Wall to wall filling means that a lesion extends from the anterior to posterior or medial to lateral cortex. Also note the cortical thickening.
- Septonodular or rings-and-arcs enhancement is the typical enhancement pattern for chondroid tumors, which helps the radiologist to make the right diagnosis.
- Osteolysis means that within a chondroid tumor there is a lucent area without matrix calcifications. This can be due to a mucoid component in high grade CS. It is hyperintense on fluid sensitive sequences with fat suppression and shows no contrast enhancement.
- Interspersed or entrapped fat is often present in ACTs between the cartilage nodules. Over time, cartilage nodules may decrease as the amount of interspersed fat increases.
How to diagnose a Chondroid tumor
X-ray
On radiographs, chondroid tumors show
foci of nodular, popcorn-like matrix mineralization.
These calcifications may be present within the entire spectrum of
chondroid tumors.
Often the tumor
size is underestimated on a radiograph, as frequently only the mineralized part of the
tumor is visible.
In the phalanges, enchondromas may present as purely osteolytic tumors, not necessarily containing matrix calcifications.
Image
There is a small area of 1.5 cm with popcorn calcifications in the distal metaphysis of the femur without extension to the cortex.
This is an enchondroma.
Images
The radiograph demonstrates an
osteolytic lesion in the distal femur containing typical popcorn calcifications
and showing anterior cortical scalloping (arrowhead).
On the sagittal MRI we can appreciate
that the tumor is larger than the area of calcifications on the radiograph,
measuring 8 cm.
The tumor is hyperintense on T2 STIR and contains multiple foci
of low signal intensity, corresponding to the chondroid matrix calcifications
on the radiograph.
Conclusion
Since there is no periosteal reaction or soft tissue mass, these findings fit with the diagnosis of ACT.
The patient remains in follow-up.
CT
CT is not part of the routine imaging work-up in chondroid tumors,
however it may aid in the detection of subtle matrix mineralization in case
there is doubt about the diagnosis.
CT can also be helpful in axial
lesions where radiographs are not sufficient - such as the skull base or pelvis
- to quantify bone destruction and the extent of the tumor.
If there is doubt about cortical
destruction in an expansile lesion on MR, CT will usually clearly demonstrate
the presence or absence of a cortex.
Finally,
CT is useful to assess pathological fractures and for example to assess whether
these extend into a joint.
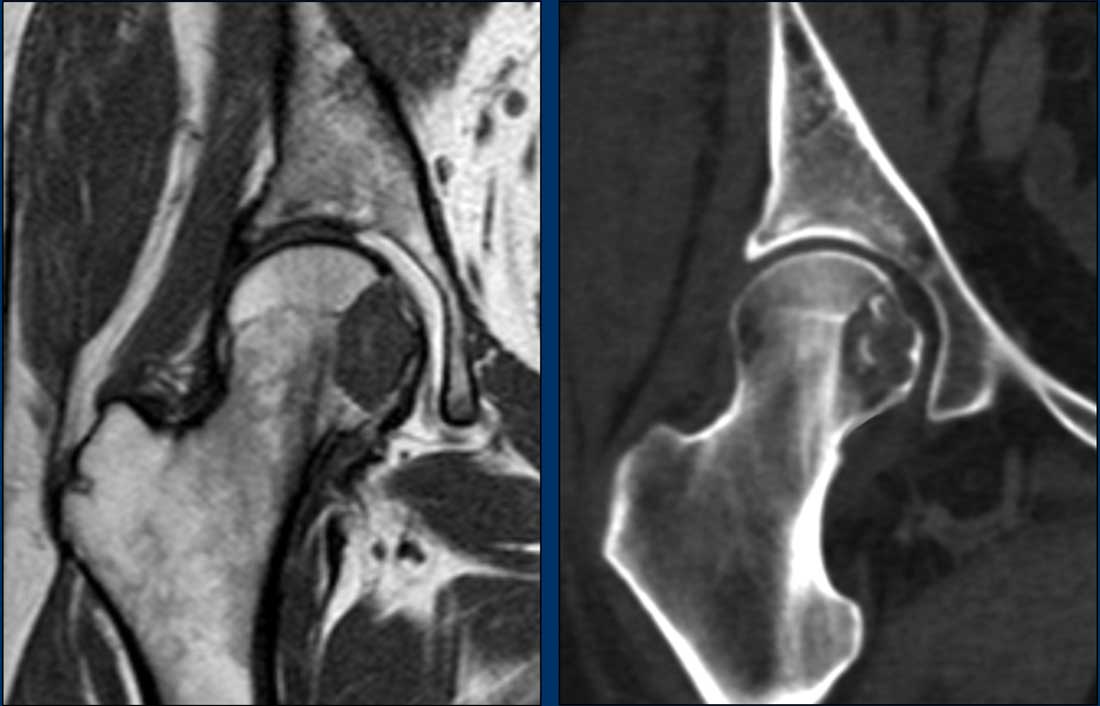
Images
MRI cor T1W-image shows an eccentric,
slightly expansile lesion in the caput and collum of the right femur.
It is difficult to appreciate whether
the medial cortex is only thinned or destructed.
Therefore an unenhanced CT was done
in addition.
Unenhanced CT demonstrates a lytic
lesion containing chondroid matrix calcifications.
There is cortical scalloping
medially, but no cortical destruction.
Curettage was performed to exclude a clear cell chondrosarcoma. This is a rare subtype of chondrosarcoma which occurs in the epiphysis of long bones in young adults.
Pathology diagnosis: ACT.
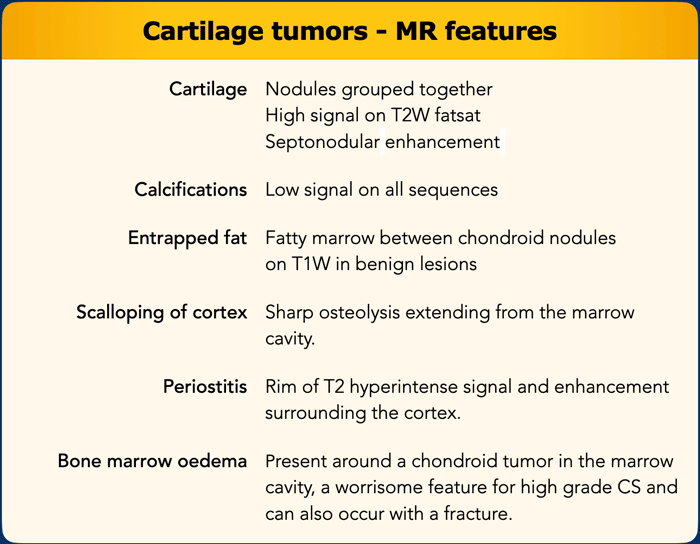
MR
On fluid sensitive sequences - preferably T2W with fat suppression - cartilage nodules are hyperintense and grouped together.
After gadolinium contrast administration, cartilage tumors enhance with a typical septonodular enhancement.
This feature is helpful in distinguishing cartilage tumors from other bone tumors.
Calcifications can be visible on MRI and show low signal intensity on all sequences.
Unfortunately, diffusion weighted
imaging has been shown not to be of use in differentiating low grade from high
grade cartilage tumors.
Interspersed fat
Chondroid nodules may have
fatty marrow between them, also called interspersed or entrapped fat.
This is best assessed on
T1-weighted images and is present in lesions at the benign side of the
spectrum, so in ACTs.
For example, during follow
up of ACTs, the amount of interspersed fat and calcifications may increase,
which can be interpreted as “maturation” of a lesion.
This may
even cause decrease in size of the tumor over time.
Both fatty maturation and
increased calcification of a chondroid tumor over time are signs of benignity.
Scalloping
Cartilage tumors may cause scalloping
of the cortex, which appears as sharp osteolysis extending from the marrow
cavity.
The Birmingham group proposed the
BACTIP criteria for MRI assessment of chondroid tumors and guidance towards referral to a
tertiary center or end of follow up.
BACTIP defined scalloping as
localized if less than 10% of the lesion circumference was involved, measured
on an axial slice with the largest tumor diameter.
Whereas scalloping of more than 10%
of the lesion circumference was defined as extensive.
Relevance of the depth of cortical
scalloping remains unclear.
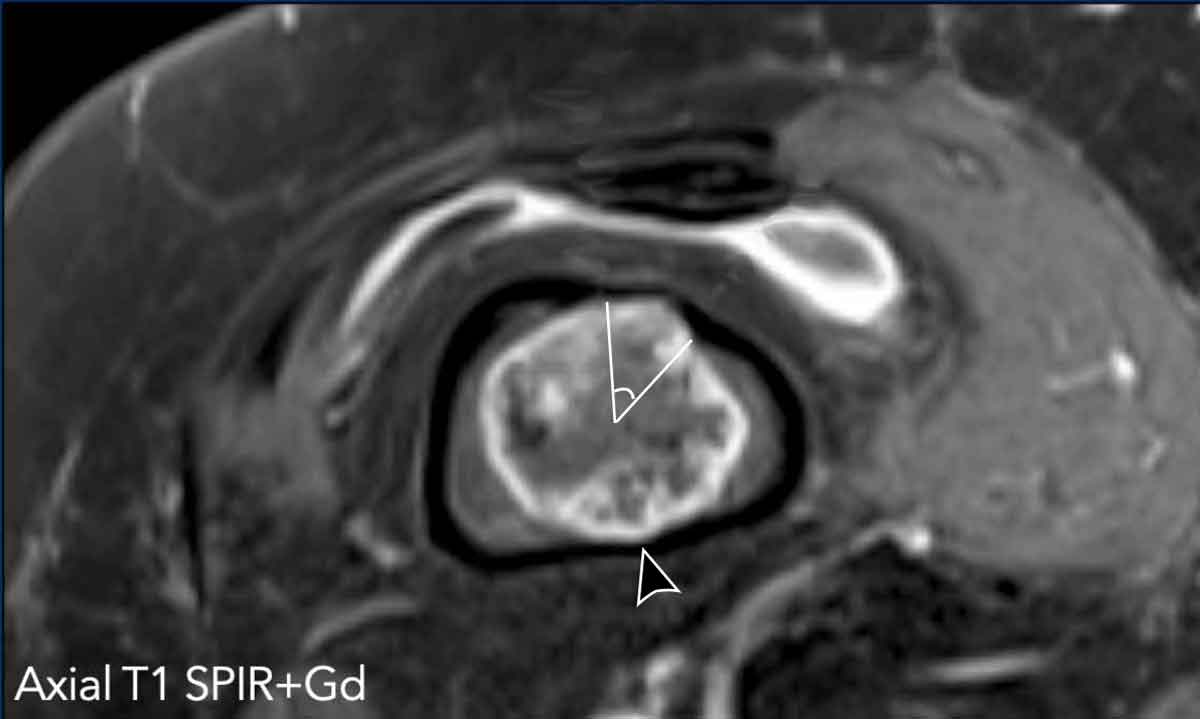
Image
The axial T1 SPIR post contrast shows cortical scalloping anteriorly over approximately 43/360 degrees.
This means scalloping of 12% of the tumor circumference (extensive).
Also note more subtle posterior cortical scalloping (arrowhead).
This tumor shows septonodular, peripheral enhancement.
Note the low signal intensity foci in keeping with calcifications.
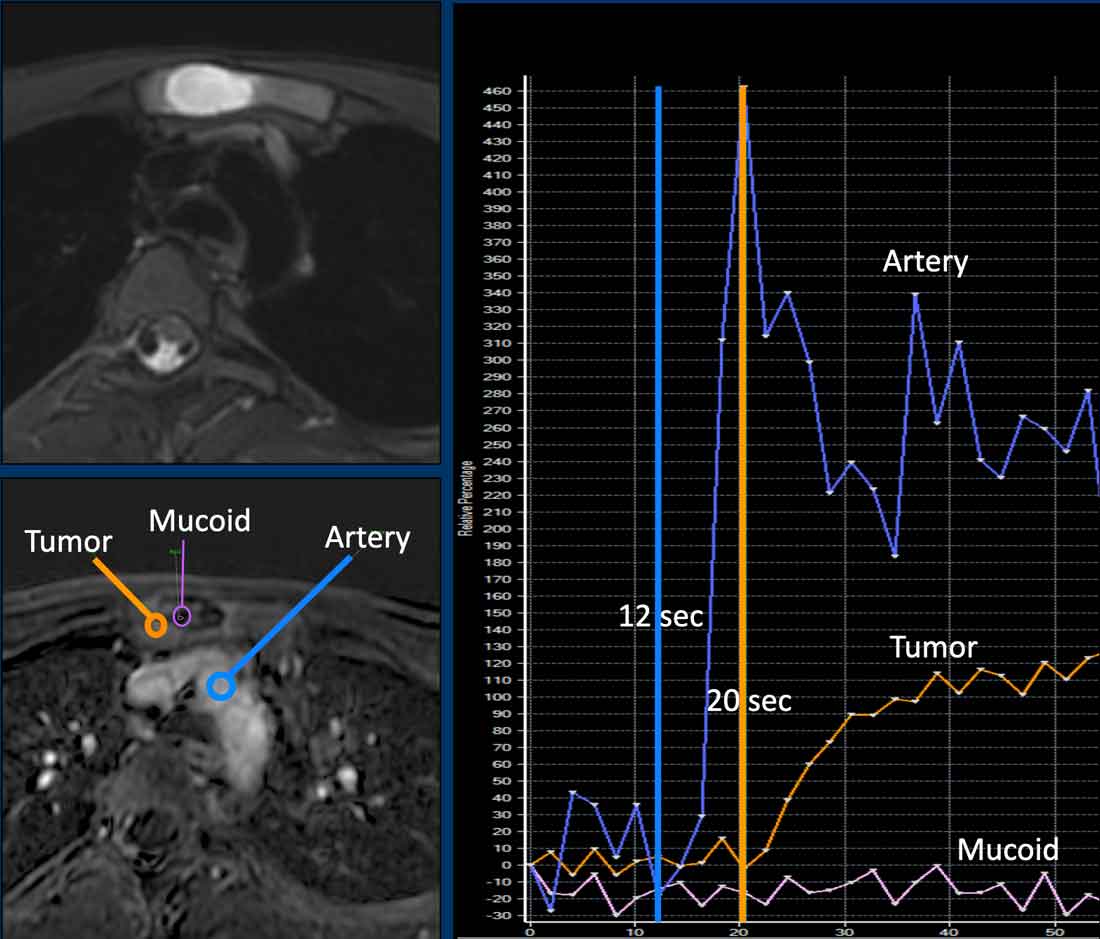
MR perfusion
Perfusion or dynamic contrast
enhanced MRI is a functional imaging technique in which early enhancement of
the tumor is monitored after an intravenous gadolinium bolus injection.
In cartilage tumors, perfusion has been used to differentiate
enchondroma from chondrosarcomas.
A cut off of 10 seconds is used for fast versus slow enhancement. However, overlap in early enhancement patterns of chondroid tumors may occur, for example: fast enhancing enchondromas exist, but also slow enhancing ACTs.
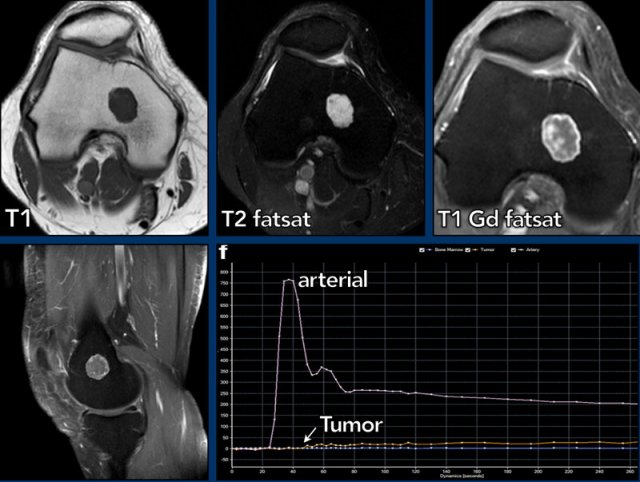
Images
There is a tumor of less than 2 cm in the distal femur metaphysis.
The lesion is hyperintense on T2, iso-intense on T1 and shows septonodular enhancement. There is no relation with the cortex. On the perfusion images (time intensity curve) the tumor shows slow enhancement, starting approximately 20 seconds post arterial enhancement.
This is an enchondroma and needs no follow up.
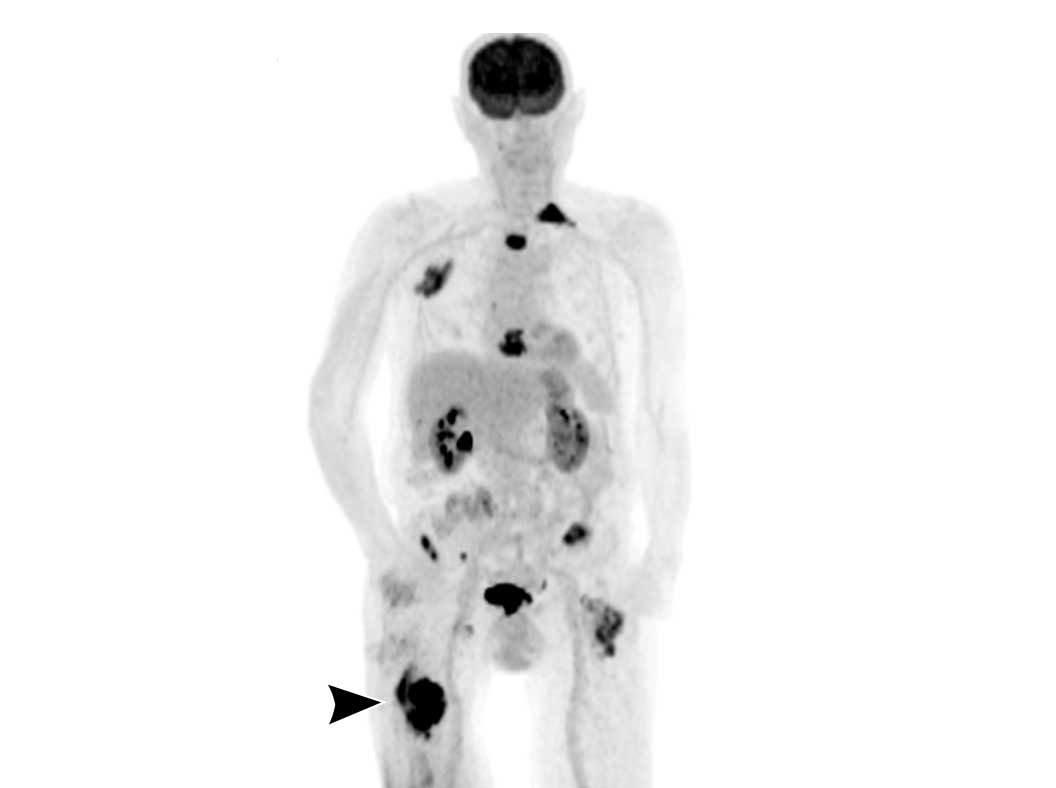
PET-CT
As for 18F-FDG-PET-CT, SUVmax was shown to correlate with
histologic grade in chondroid tumors.
SUVmax < 2 supports the diagnosis of a benign
tumor, while SUVmax > 4.5 is suggestive of higher grade
chondrosarcoma.
However, as the majority of ACT/grade
I lesions ends up in an intermediate category with overlapping values (SUVmax 2- 4.5), PET CT is not recommended
to differentiate cartilage tumors.
Whole body PET CT may be useful in detecting metastases in dedifferentiated chondrosarcoma.
Image
Dedifferentiated chondrosarcoma in the right femur (arrowhead) with multiple metastases.
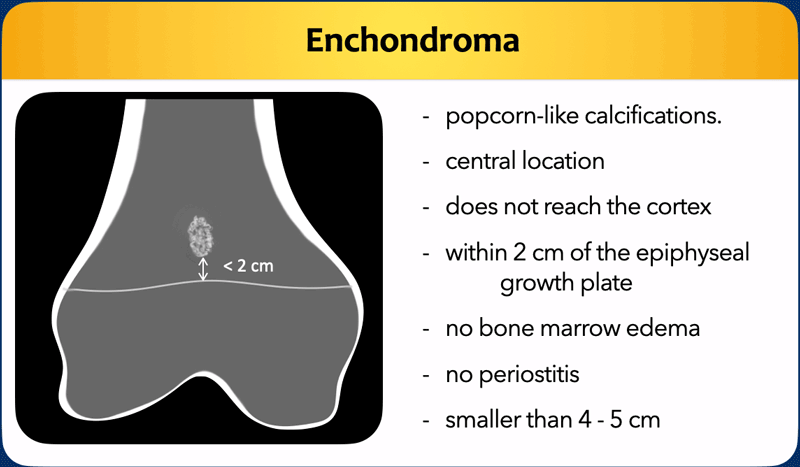
Enchondroma
Enchondromas are considered a “cartilage rest”.
Hence the close relation to the epiphyseal growth plate, often within 2 cm.
Enchondromas are mostly found in the proximal humerus, distal femur or proximal tibia metaphyses.
These benign lesions occur as incidental findings in 3% of all knee MRIs and need no follow up.
Enchondromas may slowly grow over time or even regress in size.
Growth itself is not a sign that the lesion has become malignant.
Enchondromas are typically smaller than 5 cm and 80% of enchondromas in the long bones is smaller than 2 cm.
Variable size cut offs are proposed to differentiate enchondroma from ACT and chondrosarcomas.
In the BACTIP-criteria a cut off of 4 cm is used to decide whether a lesion should be followed up or not.
In our institution we use 5 cm as a cut off, however keep in mind that there is no definitive size cutoff value and you should always rule out aggressive features, since there can be high grade chondrosarcomas smaller than 5 cm that grow through the cortex and have an accompanying soft tissue mass.
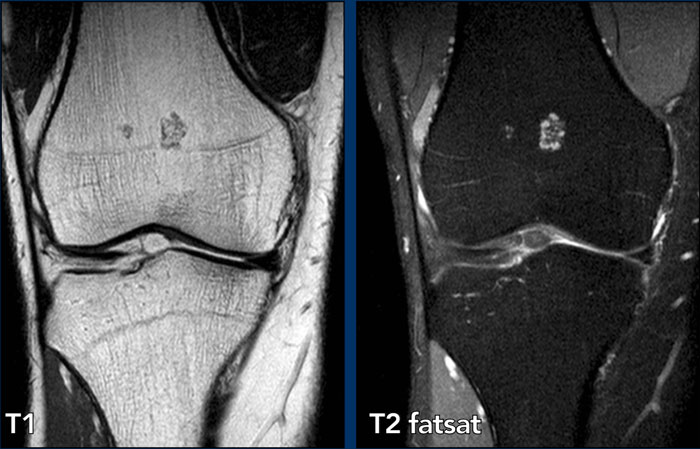
Typical
enchondroma
The images show two small lesions adjacent to the physis in the distal femur metaphysis, representing small cartilage rests without
relation to the cortex or perilesional bone marrow edema.
No follow up is
needed.
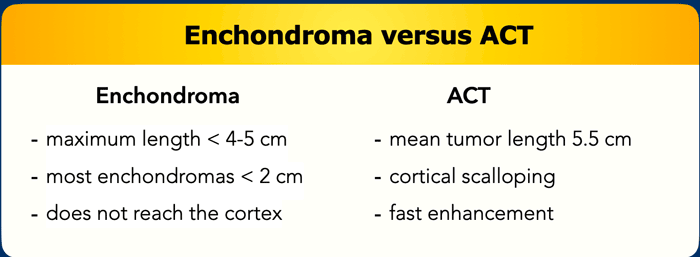
Enchondroma versus ACT
Over time, treatment of ACT has
shifted towards the conservative side, i.e. watchful waiting or “wait and scan” by
MRI instead of curettage.
This has implications for
radiologists too, as the main task is now to decide which lesions we want to
follow up.
In our tertiary referral centre, we
follow up lesions that extend up to the cortex.
This means that independent of size,
we consider possible growth through the cortex in the future an indication for follow up.
See the table with our follow op schedule for ACT below.
Case
First look at the images.
What are the findings?
Then continue reading.
Images
X-ray: An area of chondroid calcifications is present in the distal femur
diaphysis without cortical scalloping.
MRI: Sag T1W-image shows the multinodular
cartilage tumor without contact with the anterior or posterior cortex. The
lesion measures 38 mm.
The axial T1 shows no cortical
scalloping.
Conclusion
Enchondroma.
Pearl
For lesions < 5 cm, as long as the cartilage lesion does not reach the cortex,
and there is no surrounding bone marrow oedema or periostitis, we consider it
an enchondroma. No follow up is needed.
Case
First look at the images.
What are the findings?
Then continue reading.
Images
The X-ray shows shows a small area of
popcorn calcifications in the distal diaphysis.
The MR-images show a 4.6 cm lesion in the distal femur diaphysis with extension up to the
cortex (wall- to-wall filling).
Note that the lesion appears smaller
on the radiograph due to limited calcifications.
The calcifications and septonodular enhancement confirm the
chondroid nature of the tumor.
No cortical scalloping is present on
the axial T1W-image.
Conclusion
The lesion is quite large for the
diagnosis enchondroma.
As mentioned before we use a cutoff
of 5 cm. There is wall-to-wall filling, but no scalloping. No aggressive
features are present (such as periosteal reaction, bone marrow oedema).
It was diagnosed as ACT and follow up
was performed by wait-and-scan.
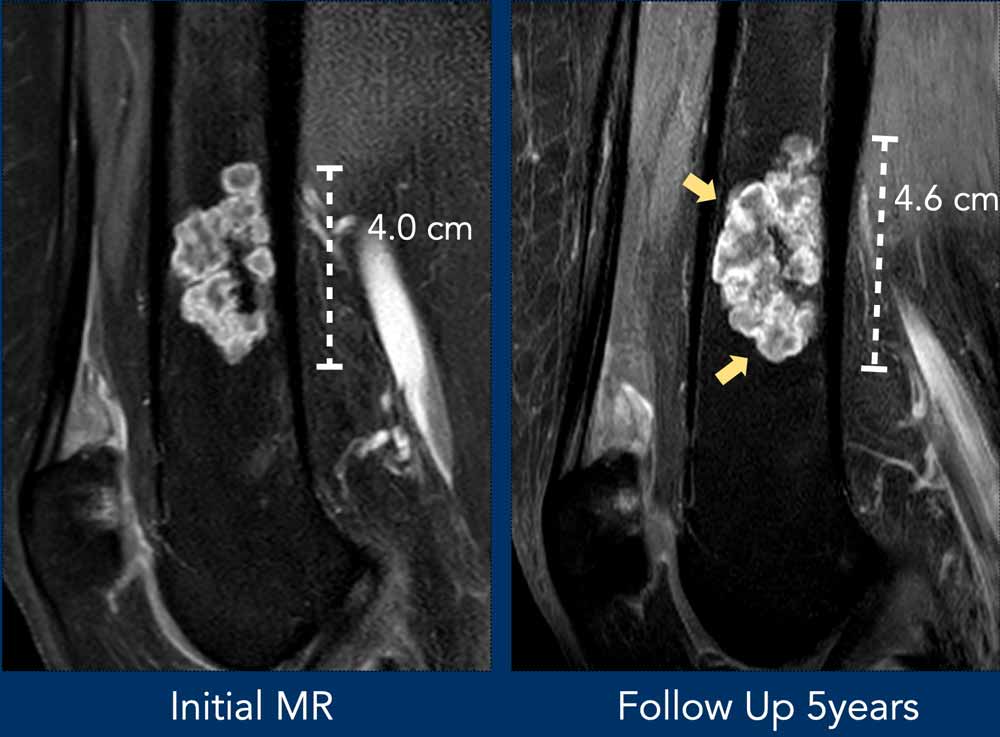
After 5 years of follow up, the
craniocaudal diameter increased 6 mm.
There were no other worrisome
features and the patient remained in follow up.
Case
First look at the images.
What are the findings?
Then continue reading.
Images
X-rays: there is an area with chondroid
matrix calcifications and some osteolysis of less than 2 cm adjacent to the
closed physis in the distal femur.
No relation with the cortex was seen.
MRI was done to assess the true size and decide whether the lesion needed follow-up.
MRI: on the sagittal T1W-image the
lesion measures maximum 2.8 cm and there is a close relation to the posterior
cortex at the intercondylar notch.
Conclusion
Because of the extent to the posterior cortex,
the lesion was called ACT and remained in follow up.
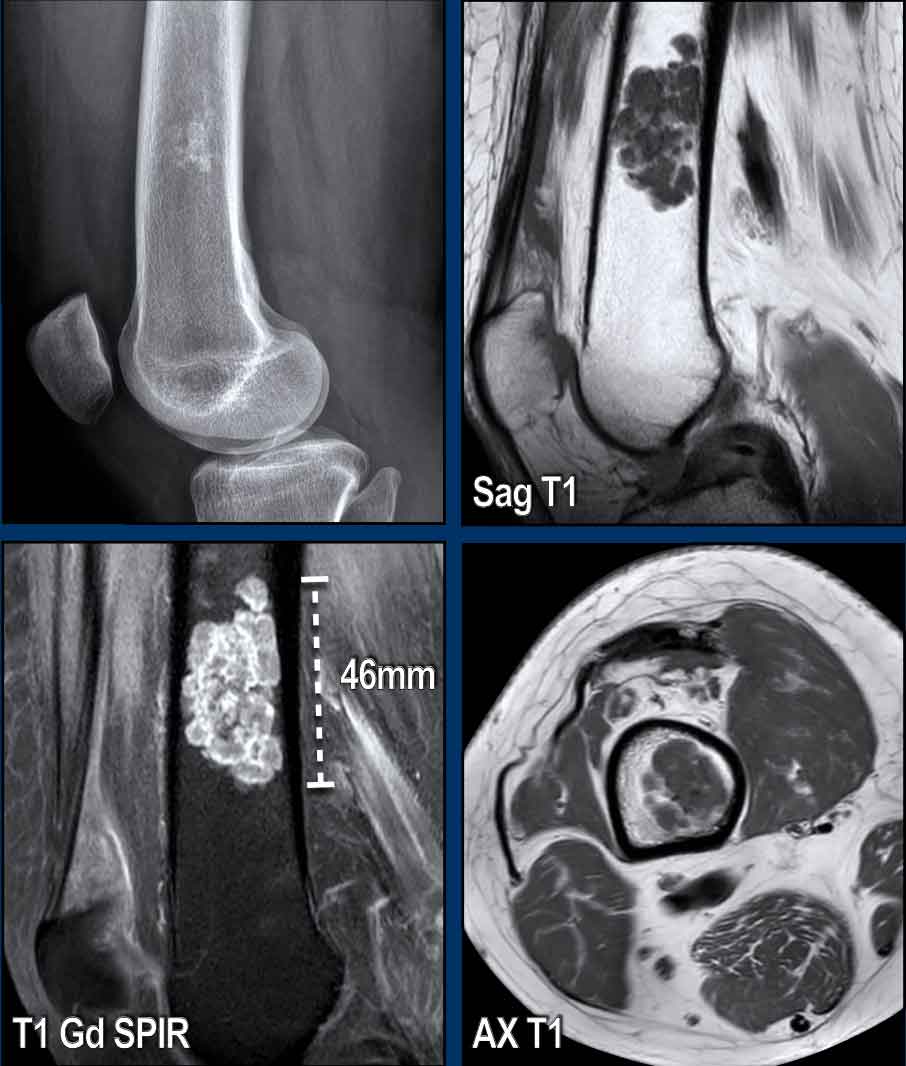
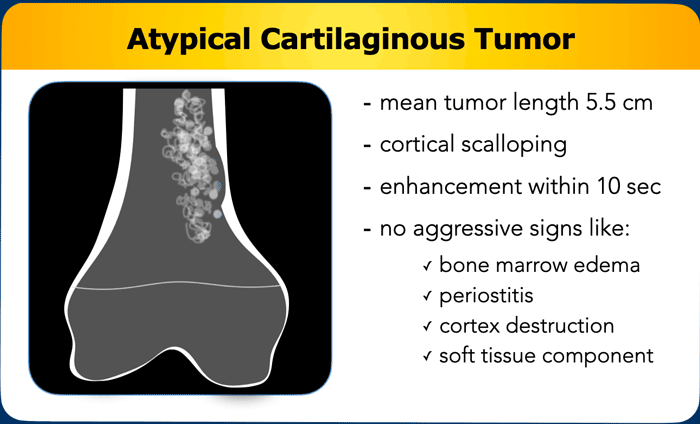
Atypical Cartilaginous Tumor
ACTs are intermediate grade chondroid tumors.
They are often larger than
5 cm, extend up to the cortex and show cortical scalloping.
They may have
interspersed fatty marrow.
On MR perfusion, fast enhancement (within 10
seconds) can be present.
Keep in mind that growth itself does not imply malignant transformation,
and some of these lesions regress in size over time.
ACTs do not show
periostitis unless there is a fracture.
No cortex destruction or soft tissue
mass is allowed for the diagnosis ACT.
In that case we should call it a chondrosarcoma of higher
grade.
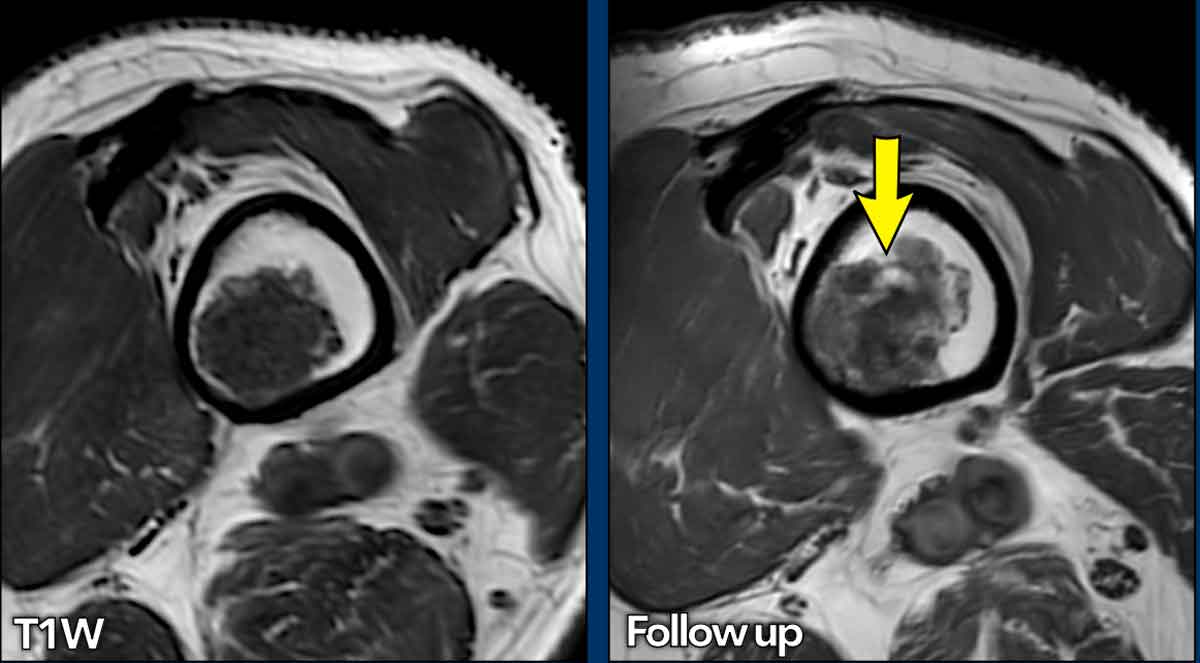
This case was shown before.
Looking back to the previous
MRI performed 5 years before, 6 mm growth occurred in the craniocaudal
dimension.
Also note some expansion
of the lesion anteriorly (yellow arrows).
No cortical thinning,
bone marrow oedema or periostitis are present.
This lesion is an ACT and remains in follow-up.
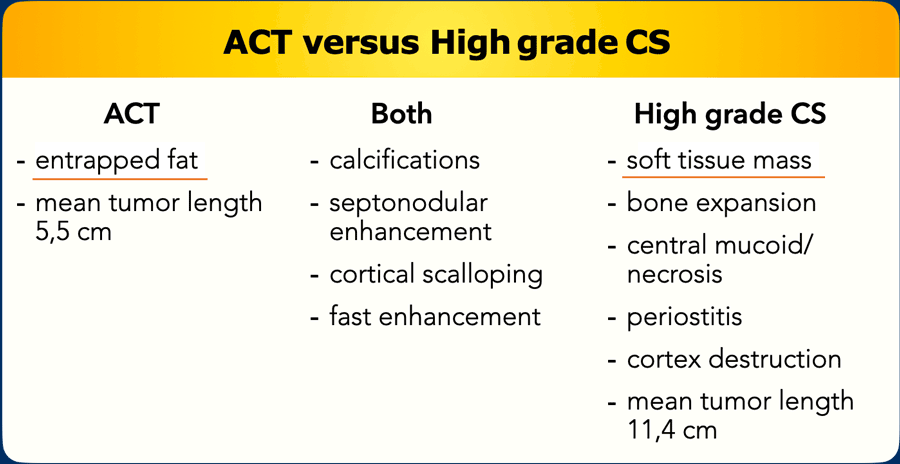
ACT versus high grade CS
Differentiation between ACT and high grade CS is the most important task for a radiologist, as the high grade tumors need wide resection. Since the paradigm has shifted, more and more centers treat ACTs with watchful waiting and no operation.
Actively look for features such as perilesional bone marrow oedema, periosteal reaction, cortical destruction and a soft tissue mass to call a tumor high grade CS. Bone expansion may be seen in ACT but is more common in high grade CS.
Mucoid components are a sign of higher grade and are also present for example in dedifferentiated CS.
Fast dynamic contrast enhancement, cortical scalloping and matrix calcifications can be present in both ACTs and high grade CS so these features do not differentiate the two.
Size matters but is not a key feature to differentiate ACT from high grade CS.
In case of a pathological fracture in ACT, surrounding oedema and periostitis may be present. Always correlate the images with the clinical history of a trauma and recommend follow up MRI after 3-6 months to assure that these findings resolve.
We will now show you some cases, where you have to differentiate between ACT and chondrosarcoma.
Case
First look at the images and decide whether you are dealing with an ACT or CS.
Then continue reading.
Images
There is a lesion measuring
more than 20 cm in the diaphysis of the femur.
Note the popcorn matrix
calcifications.
There
is one focal nodule (within the yellow circle) causing cortical scalloping and
there is mild extension of the marrow cavity.
Continue with the MR...
First look at the images.
Then continue reading.
Images
MR-images show interspersed fat between the cartilage nodules.
It has a high signal on the sagittal T1W-image and low signal on the fat suppressed image (arrows).
There is one focal nodule causing cortical scalloping (<10%) and there is mild extension of the marrow cavity.
Conclusion
The lesion was diagnosed as ACT and remained
stable during follow up.
Case
First look at the images and decide whether you are dealing with an ACT or CS.
Then continue reading.
Images
There is a well defined
osteolytic lesion >10 cm in the proximal femur diaphysis with popcorn i.e.
chondroid matrix calcifications.
There is expansion of the bone, however no frank cortical scalloping or periostitis.
Conclusion
Based on the radiograph alone, this tumor could be an ACT or a chondrosarcoma of higher grade. The next step is to perform MRI for further characterization.
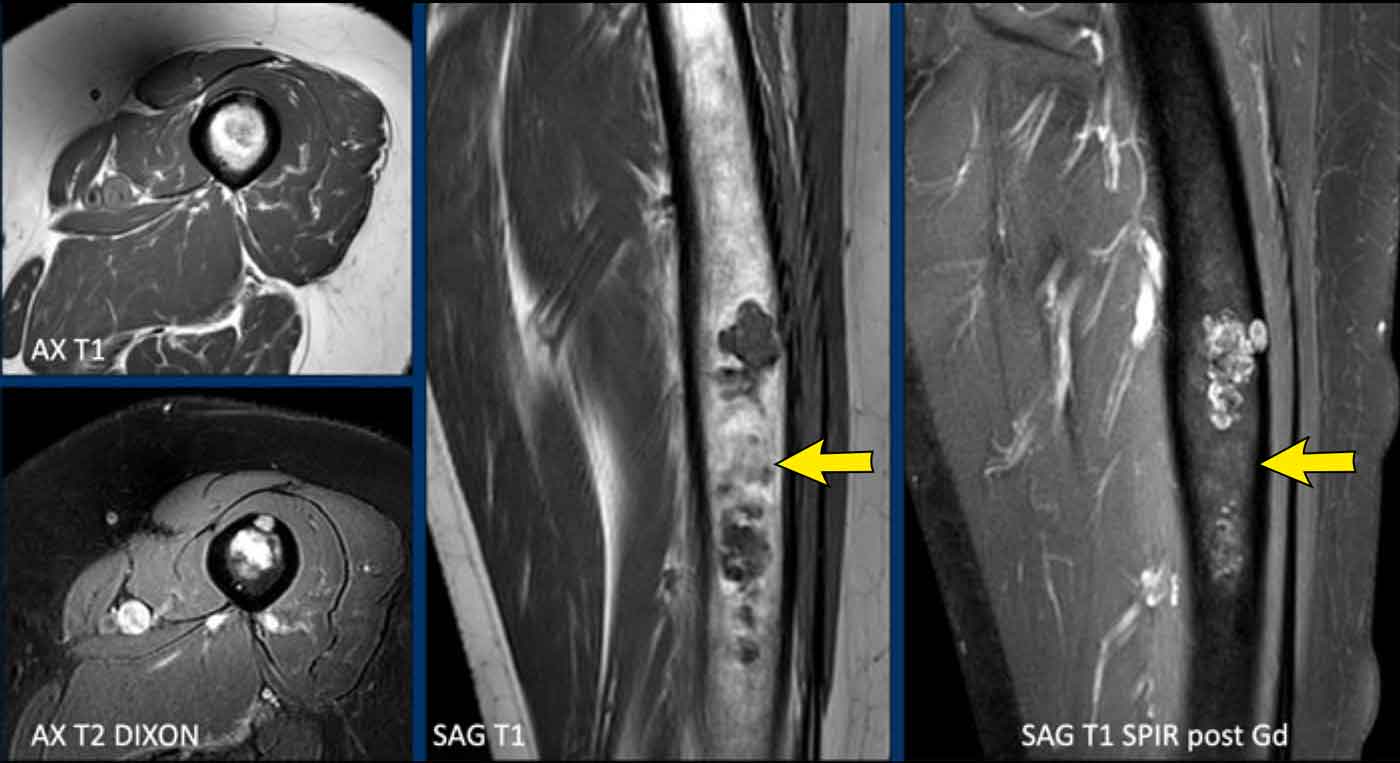
Case
First look at the images.
Then continue reading.
Images
MRI confirms the chondroid nature of the tumor with hyperintense
cartilage nodules on T2 DIXON that show septonodular enhancement after
contrast.
However, there is also marked bone marrow oedema proximally (black arrow) and a periosteal reaction with enhancement (white arrow).
Conclusion
These features are very suspicious for the diagnosis of a high
grade chondrosarcoma.
Images
Axial T1 weighted image confirms deep
anterior cortical scalloping over approximately 1/3 of the cortex, i.e. extensive scalloping ( > 10% of tumor circumference).
A proximal femur resection
was performed.
Final diagnosis: chondrosarcoma grade II
Case
First look at the images.
Then continue reading.
Images
Radiograph shows small areas of chondroid matrix mineralization.
COR T2W FS illustrates how the size of the lesion is underestimated on plain film.
Note the hyperintense cartilage nodules in combination with low SI areas in keeping with the calcifications on X ray.
After contrast typical rings-and-arcs enhancement is seen.
Conclusion
Due to the size of 5.7 cm and the extent to the cortex, this was called an ACT and the lesion will be followed up with MRI.
Case
First look at the images.
Then continue reading.
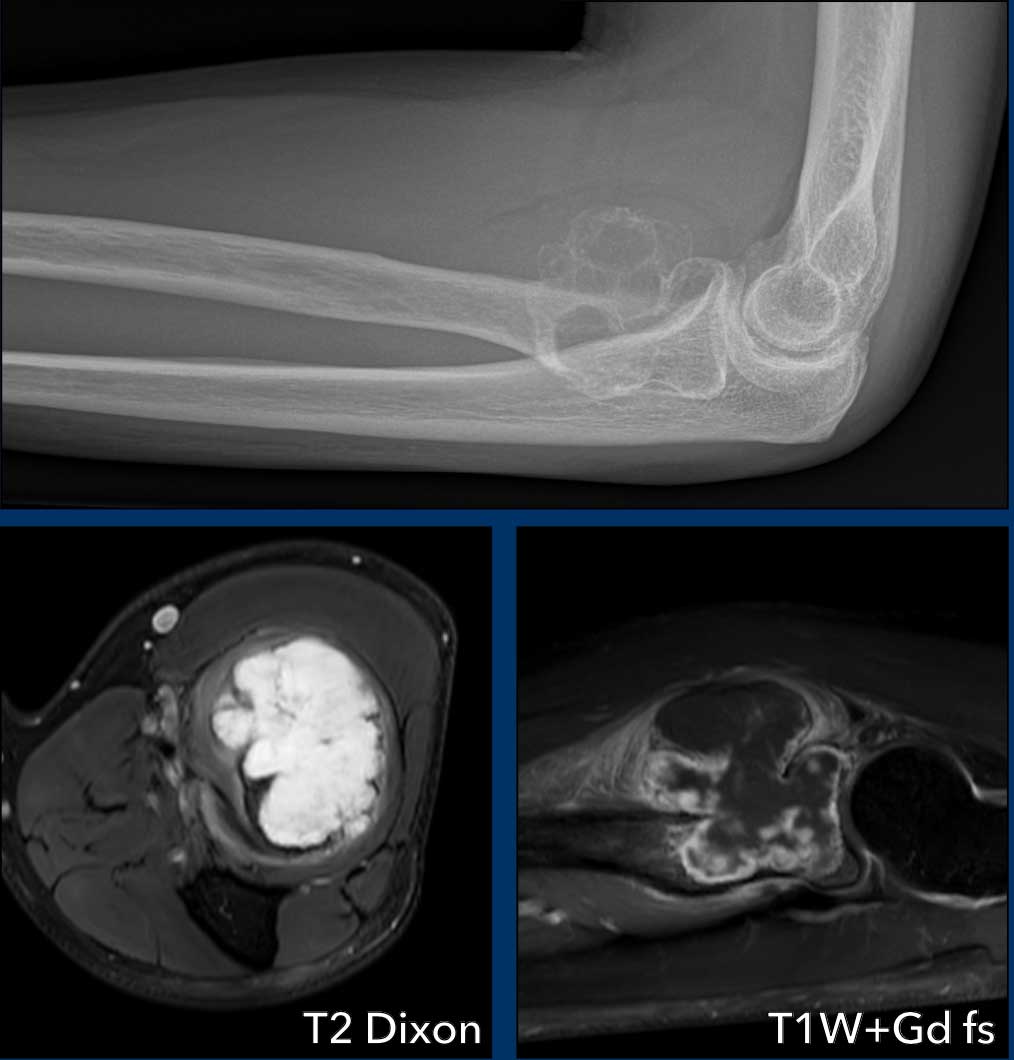
Images
The radiograph shows an expansile multilocular osteolytic lesion in the proximal radius metaphysis.
Some small specs of calcification are visible within the lesion.
The tumor is hyperintense on T2 DIXON and there are areas of cortex destruction.
After contrast, typical septonodular enhancement is present and areas of mucoid without enhancement, also in the soft tissue component.
Around the tumor we see soft tissue oedema.
These findings help us to make the diagnosis of a high grade chondrosarcoma.
Pathology after wide resection came back as grade II chondrosarcoma.
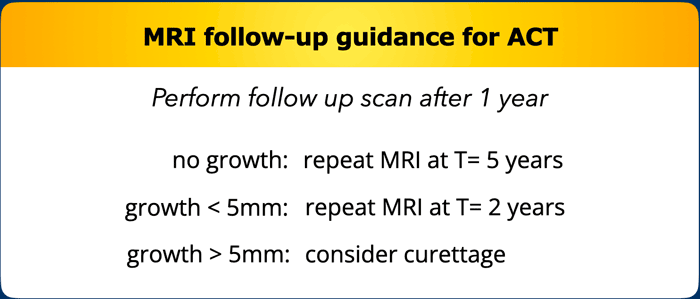
MRI follow-up guidance for ACT
In our centre, ACTs are followed up by MRI as shown in the table [1].
This may provide some clinical guidance, however solid long term (>10 years follow up) data is needed to further define a good follow up interval and final duration, as MRI scans come with a burden of costs and may cause worry for the patient.
If aggressive features occur during follow-up that are worrisome for chondrosarcoma, the patient is discussed in the multidisciplinary tumor board and surgical treatment may be considered.
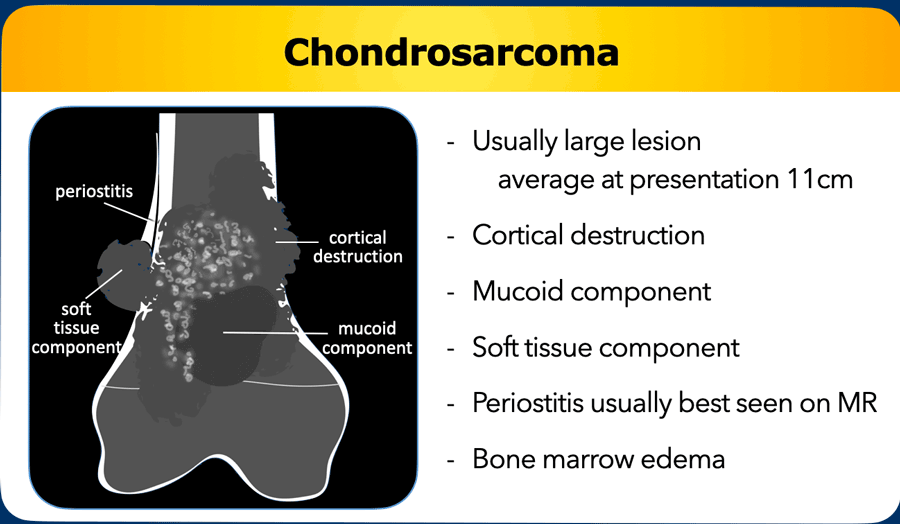
Chondrosarcoma
Chondrosarcomas are on average more than 10 cm
at presentation, show cortical destruction and often have an accompanying soft
tissue mass.
However, smaller chondrosarcomas of high grade occur, therefore
size is not the best criterium.
Periostitis on MRI is shown as a
T2 hyperintense rim surrounding the cortex, enhancing after contrast.
A mucoid
component may be present within the marrow cavity or in the soft tissue mass.
These
lesions are high grade meaning they are at risk to metastasize (primarily to
the lungs).
Treatment is wide resection and in addition to the MRI, a CT may be done for preoperative planning, as radical resection is the only good treatment option.
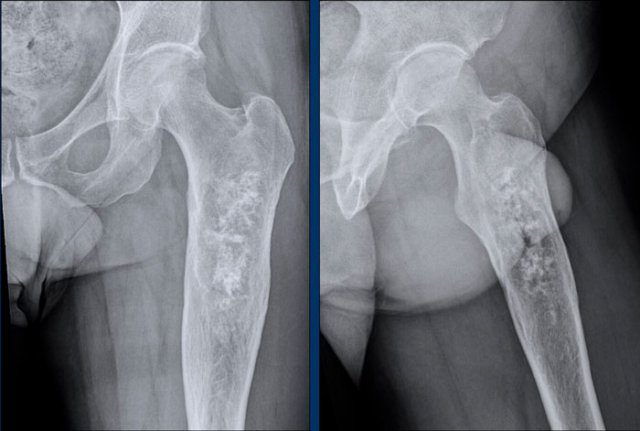
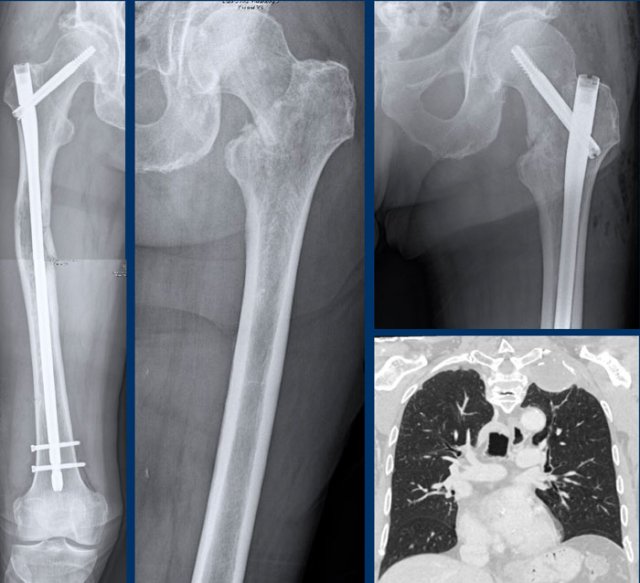
Case
First look at the images.
Then continue reading.
Images
There is an osteolytic, expansile
lesion in the right proximal femur diaphysis.
Adjacent subtle cortical
thickening is present without periosteal reaction.
No frank chondroid matrix is
appreciated on this radiograph.
Conclusion
The differential diagnosis would include chondrosarcoma,
fibrous dysplasia, lymphoma, metastasis and plasmacytoma.
An unenhanced CT could help in
detection of subtle chondroid matrix calcifications in this case. However, we
went straight for MRI.
Continue with the MRI...
First look at the images.
Then continue reading.
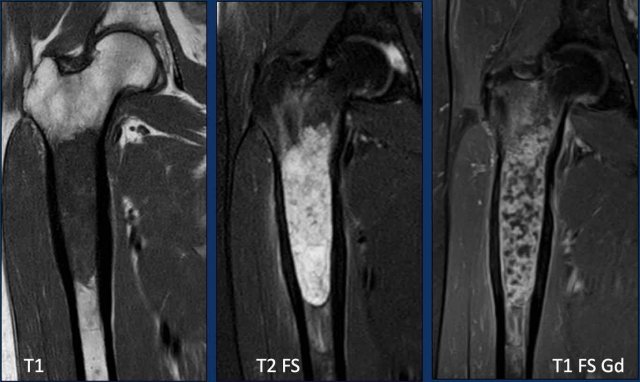
Images
T1W-image shows marrow replacement.
T2W-image shows periosteal reaction
and perilesional bone marrow edema.
The tumor itself is hyperintense and
nodular.
T1W FS post Gd-image shows rings-and-arcs
enhancement pattern.
Conclusion
All these findings are in keeping
with a chondroid tumor, and very suspicious of a chondrosarcoma of grade II or
higher.
In our tertiary referral center for
bone sarcomas we perform no biopsy in these chondroid tumors, as this may cause
sampling error due to heterogeneity within the tumor.
You may erroneously biopsy the
friendlier part of the tumor and underestimate the grade.
Chondroid tumors are known for their seeding along the biopsy tract.
Continue with the postoperative X-rays.....
Treatment consisted of en bloc resection of the proximal femur and reconstruction with an endoprosthesis.
Pathology confirmed a chondrosarcoma grade II.
Chondrosarcomas grade II and III cannot be differentiated based on imaging.
This is a diagnosis made on histopathology.
Therefore, we refer to such lesions as “grade II or higher” in our radiology report.
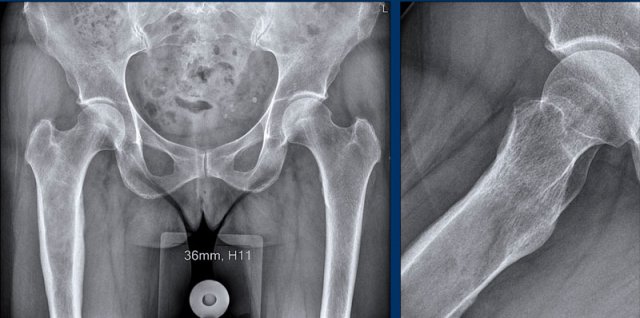
Case
First look at the images.
Then continue reading.
Images
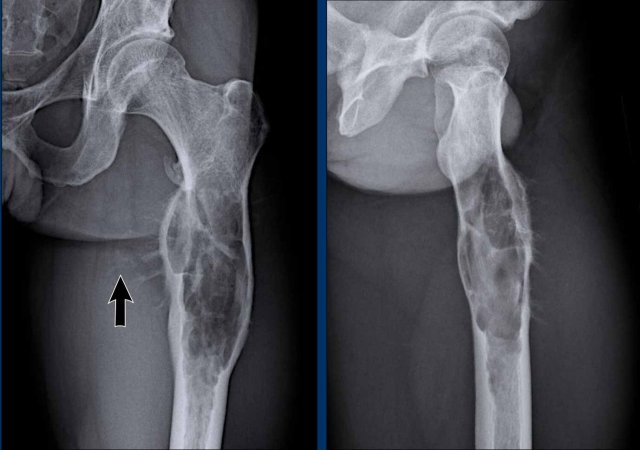
Radiographs demonstrate an
aggressive expansile osteolytic lesion in the proximal femur diaphysis of a 30-year-old patient.
There
is extensive cortical scalloping and a spiculated, hair-on-end periosteal
reaction.
Note the pathological fracture of the trochanter minor.
There is subtle mineralization in the soft
tissues medially (arrow).
Conclusion
All these findings are pointing
towards a malignant bone tumor.
In the differential diagnosis (taking
into account the age and diaphyseal location) we would include a Ewing sarcoma,
but also a high grade chondrosarcoma.
Although Langerhans cell
histiocytosis may also present in the diaphysis of a long bone in this age
group, this tumor is very large and the periosteal reaction is too
aggressive.
Continue with the MRI…
First look at the images.
Is this a chondroid tumor or something else?
What is the best
treatment, follow up or resection?
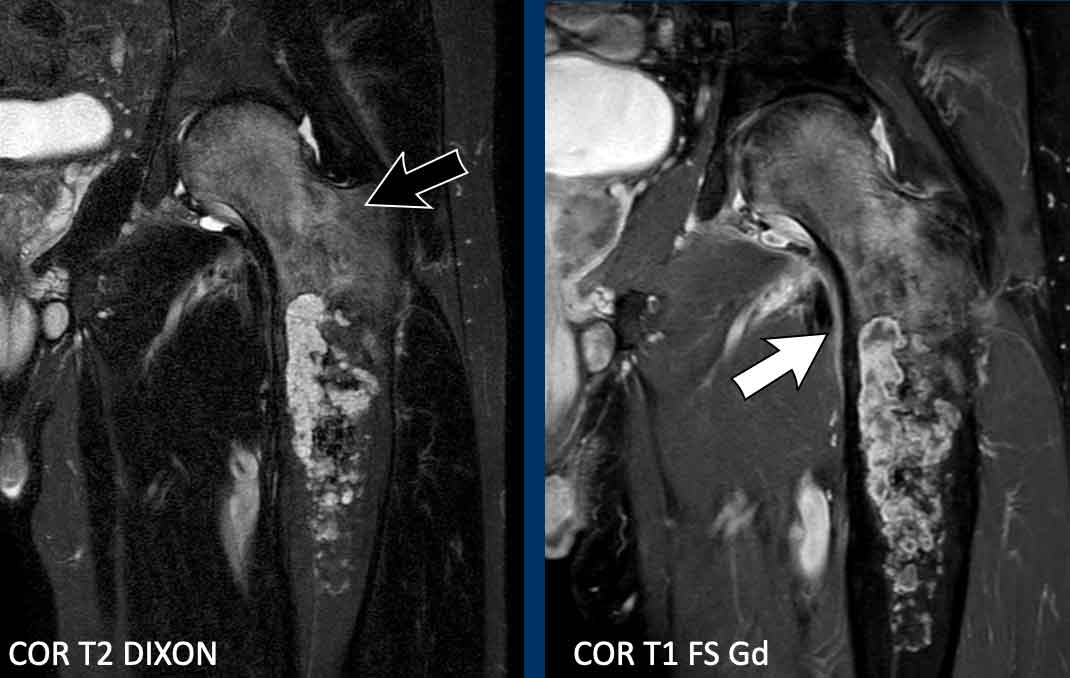
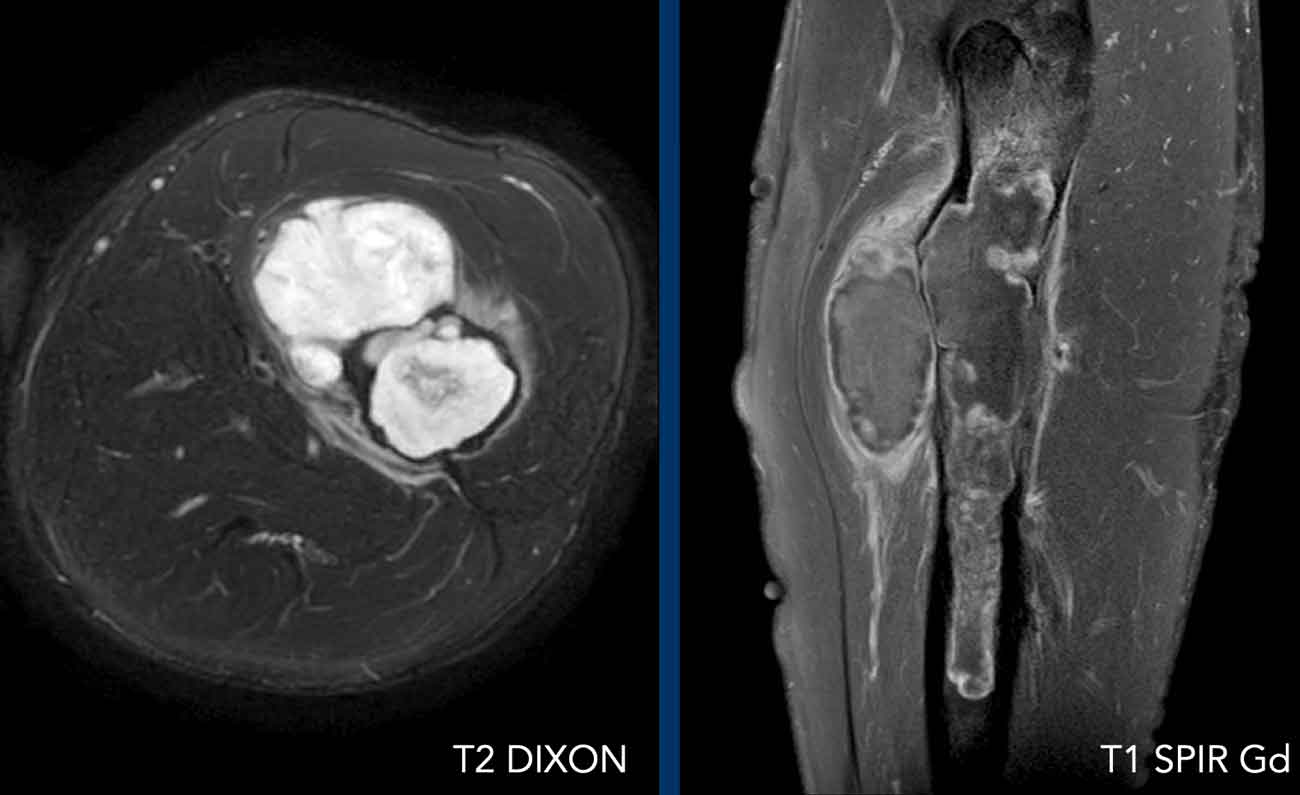
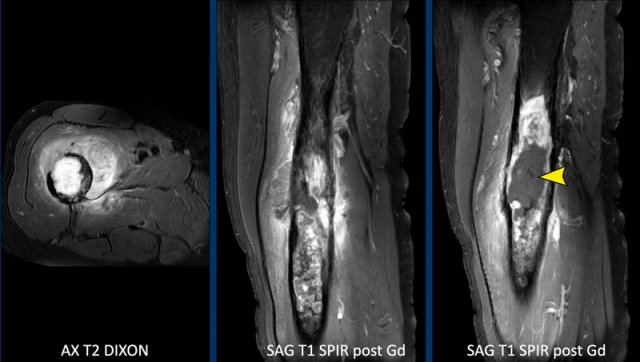
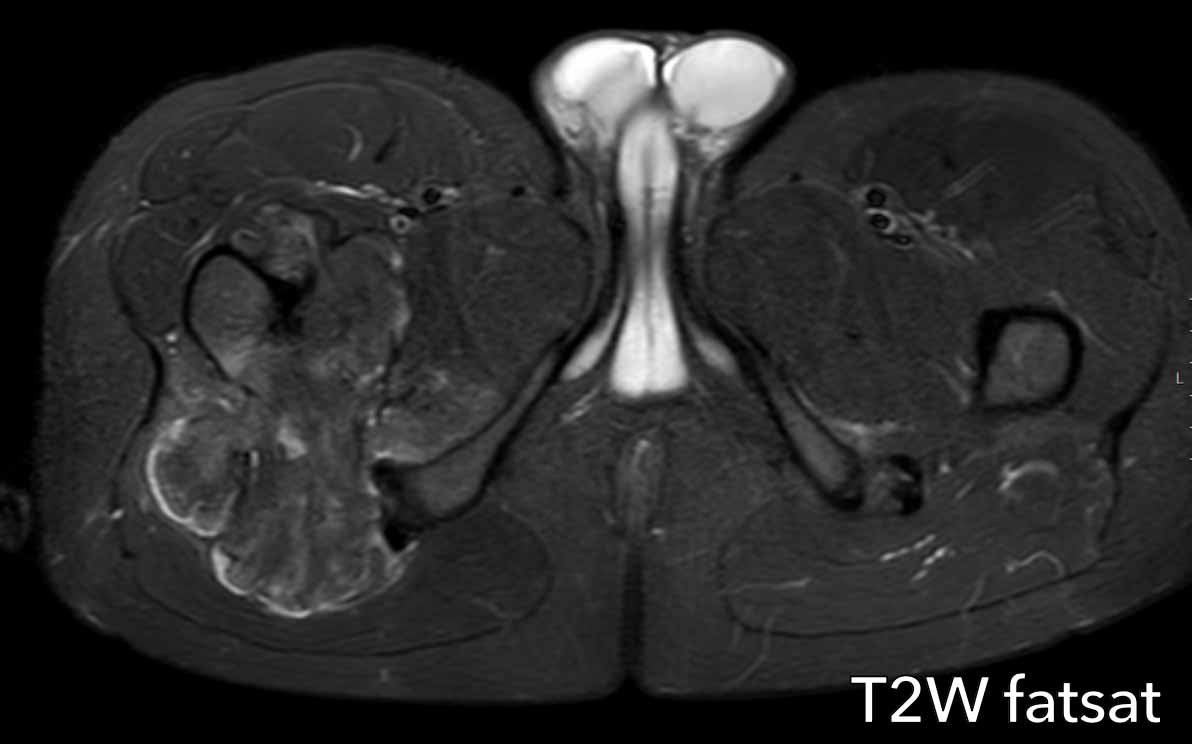
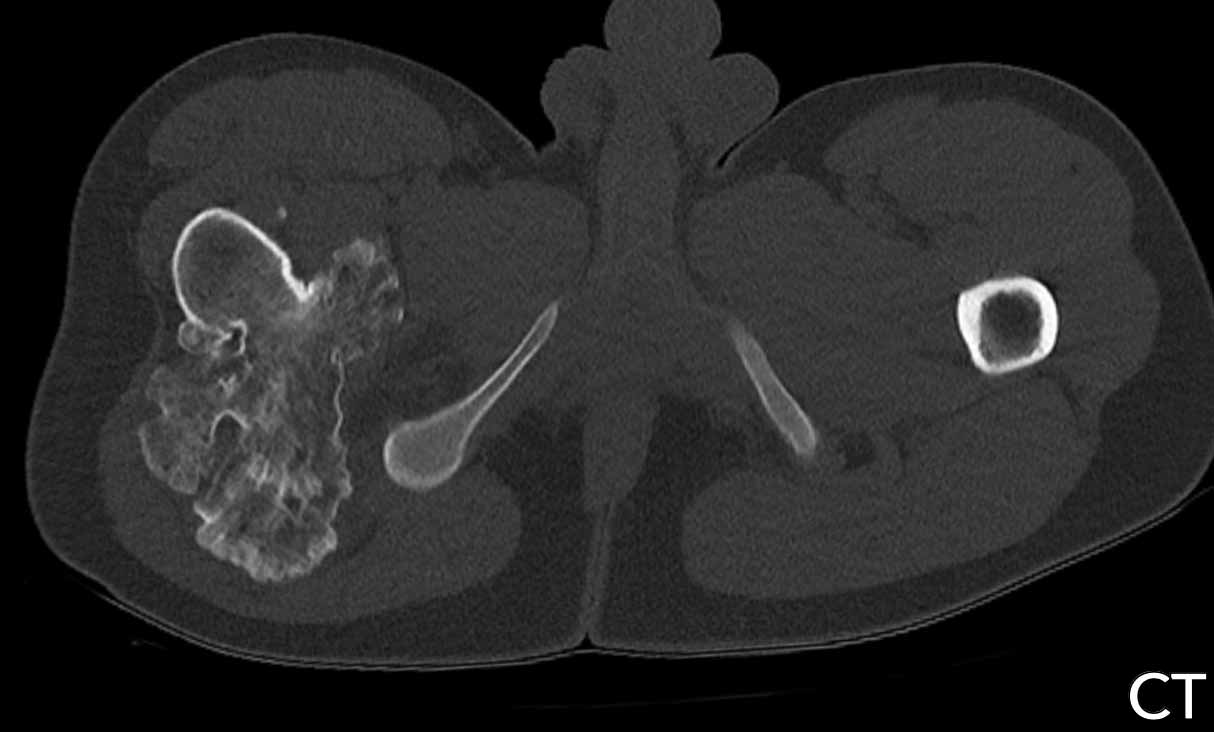
Images
MRI confirms the T2
hyperintense multinodular aspect of a chondroid tumor.
There is a large soft
tissue mass present anteromedially. There is marked periostitis on MRI, bone
marrow oedema proximally and surrounding oedema in the soft tissues.
Note the septonodular
enhancement pattern.
There is no enhancement
cranially in the tumor and in the soft tissue mass. This is regarded as a mucoid
component.
Conclusion
Based on the MRI findings, we should make the diagnosis of a chondrosarcoma grade II or higher.
Treatment was wide resection.
Pathology diagnosis: Chondrosarcoma grade III
A mucoid component is one feature of a high grade chondrosarcoma, visible for both radiologist and pathologist.
The pathologist also assesses cellularity, nuclear atypia and mitoses in the tumor, which are higher than in ACT or grade I chondrosarcoma.
Case
Let’s continue with a chondroid tumor in the axial skeleton. We have to shift gears as there is a different approach than for lesions in the appendicular skeleton.
First look at the images.
Then continue reading.
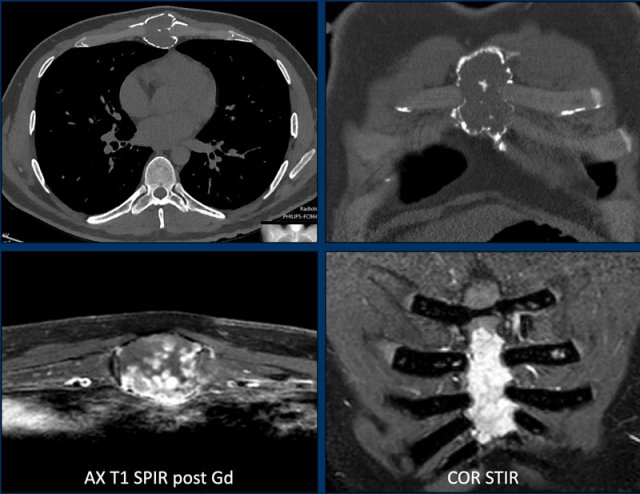
Images
Axial CT shows an expansile
osteolytic tumor in the corpus of the sternum.
There are multiple foci of cortical
destruction.
Popcorn calcifications are present centrally.
MRI confirms the chondroid nature of
this tumor with hyperintense signal on the STIR-image and septonodular contrast
enhancement.
Conclusion
Although there is no soft
tissue component, due to the expansion and multiple foci of cortex destruction this tumor should be called a chondrosarcoma of grade II or higher and en bloc resection
is the correct treatment.
Pathology showed a grade II chondrosarcoma.
In the axial skeleton chondroid tumors have a worse outcome.
This implies, that they are resected even if they are grade I as opposed to the same tumor in the appendicular skeleton, which is called an ACT and will receive follow up.
Do not call axial tumors enchondromas if they show cortical scalloping or cortical destruction, as this would lead to undertreatment.
Case
First look at the images.
Then continue reading.
Images
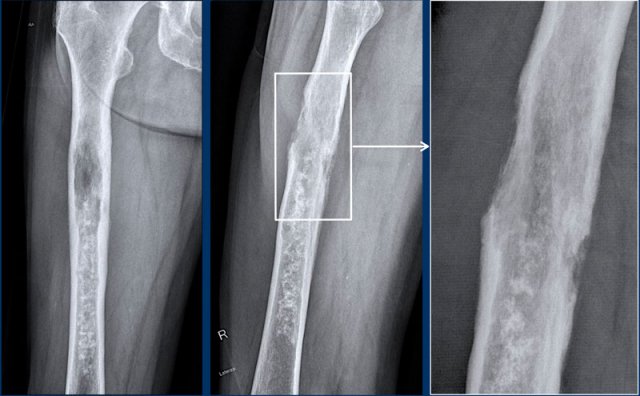
On the radiograph, there is a permeative osteolytic lesion with aggressive periosteal reaction, cortical scalloping and expansion.
Axial T2 DIXON shows multiple soft tissue masses along the humerus.
The post contrast sequence demonstrates septonodular enhancement, aggressive periostitis and mucoid areas within the tumor without enhancement both proximally in the medulla and in the soft tissue mass medially.
Conclusion
High grade CS.
Dedifferentiated chondrosarcoma
First look at the images of a 79-year-old patient with a bone tumor.
Then continue reading.
Images
Radiographs show a large tumor in the femoral diaphysis with typical popcorn calcifications distally and a
more osteolytic component proximally.
Detailed magnified window of the
lateral view shows cortical permeation by the tumor and a high risk for a
pathological fracture.
The caudal part of the tumor appears
like an ACT with focal cortical scalloping, while the cranial part looks like a high grade CS.
Conclusion
This is the typical
presentation of a dedifferentiated chondrosarcoma, with one part behaving like a
low to intermediate grade cartilage tumor with abrupt transition to a
high-grade (sometimes non-cartilaginous) sarcomatous component.
This subtype
usually presents in older adults.
Overall survival of a dedifferentiated
chondrosarcoma is poor as compared to chondrosarcomas grade II and III, as
patients often present with pulmonary and bone metastases at the time of
diagnosis.
Continue with the next images...
Images
Note the cortical defect on the axial
T2 DIXON and the surrounding soft tissue mass.
Part of the tumor does not enhance
and this area of mucoid indicates a high grade chondrosarcoma.
As on the radiographs, this
case is a typical dedifferentiated
chondrosarcoma, where the lower part behaves
like an ACT and the proximal part as a high grade sarcoma.
Frequently they present as a large tumor in an elderly patient.
Perfusion images demonstrate
heterogeneous enhancement within this dedifferentiated chondrosarcoma.
The mucoid part (blue line)
shows no enhancement.
Continue with the PET-CT...
We discussed before that 18F-FDG PET-CT is not recommended for chondrosarcoma to differentiate between ACT and high grade tumors.
However, in dedifferentiated
chondrosarcoma, PET CT combined with a diagnostic CT of the chest may be
performed to look for metastatic disease.
The dedifferentiated chondrosarcoma in
the right femur shows high FDG captation and the whole body image demonstrates multiple bone metastases in the left femur, left clavicle, cranial ribs on the
right and in the sternum.
Para-iliac lymph node metastases are
present bilaterally.
As chondrosarcomas are insensitive to radiotherapy and chemotherapy, the patient received palliative care, including nailing of the right femur to prevent a fracture.
Unfortunately, he developed a pathological fracture in the left femur which was subsequently treated.
Coronal CT image of the chest demonstrates the soft tissue mass around
a metastasis in the left clavicle.
No pulmonary metastases were found.
The prognosis of dedifferentiated chondrosarcoma is poor with a 5-year overall survival of about 18%.
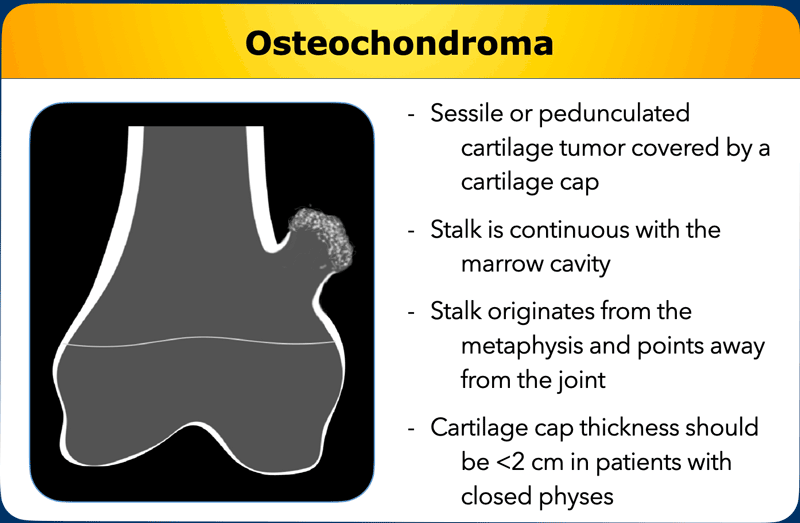
Osteochondromas
Osteochondromas
are peripheral chondroid tumors, meaning they are not located in the medullary
cavity.
Two morphological subtypes exist: sessile (broad based) or pedunculated
lesions (with a stalk) covered by a cartilage cap.
The
stalk of an osteochondroma is continuous with the marrow cavity, originates
from the metaphysis and points away from the joint.
The cartilage
cap thickness should be less than 2 cm in patients with closed physes according
to the WHO criteria defined in 2020.
If the cap measures more than 2 cm, this
is worrisome for ACT or even chondrosarcoma, and these lesions are resected.
In children, the cartilage cap of an osteochondroma may be thicker than 2 cm as their skeleton is still developing.
This radiograph is of a 17-year-old patient presenting with pain in the shoulder since 2 months.
Image
There is a pedunculated lesion originating from the proximal
humerus metaphysis.
The stalk shows continuity of the bone marrow and an
overlying cap containing chondroid matrix calcifications.
These findings are typical for an
osteochondroma.
On the radiograph, the mineralized and thereby visible part of the cartilage cap is large, which is why a MRI was performed to adequately measure the thickness of the cap.
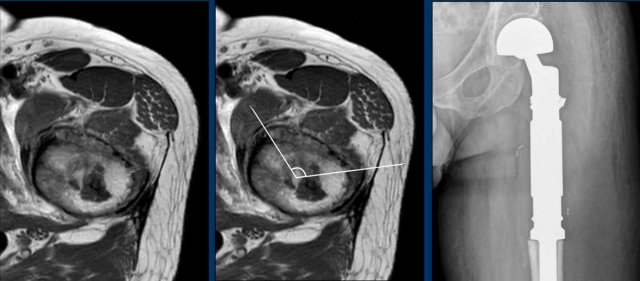
Continue with the MR-images...
The thickness of the cartilage cap is measured perpendicular to the cortex on a T2 weighted sequence.
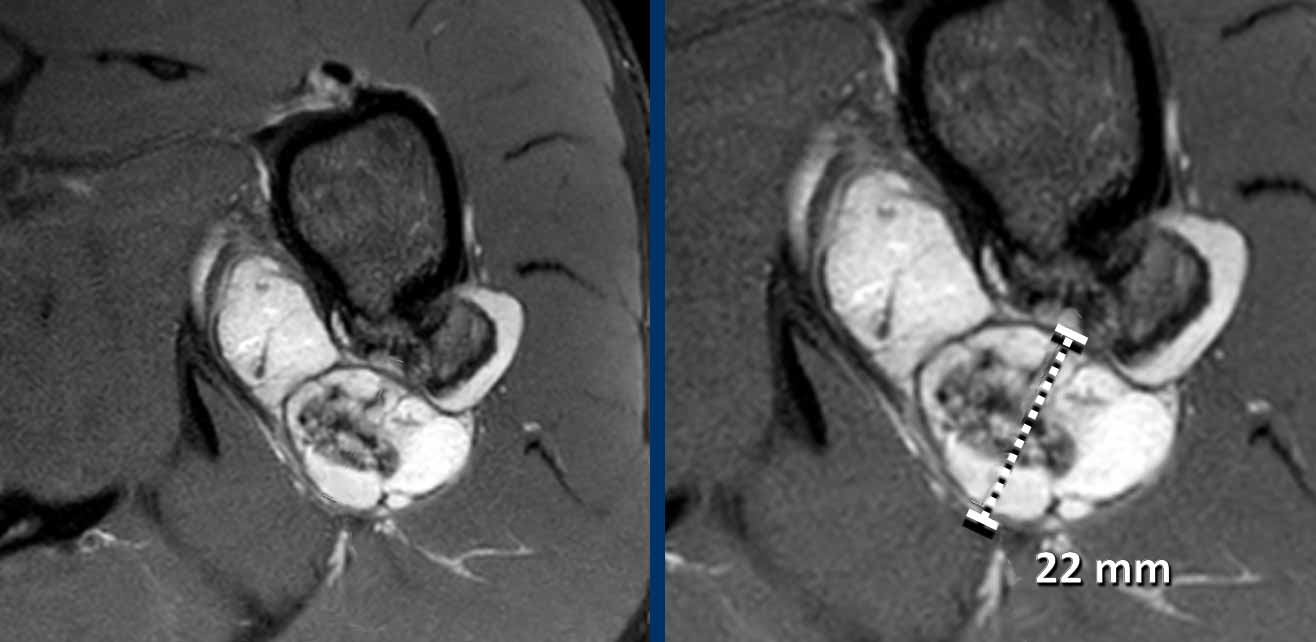
Image
Axial T2W-image with fatsat
shows the osteochondroma on the posterior aspect of the left proximal humerus
with a cartilage cap thickness of 22 mm.
In lesions with a cartilage cap > 2 cm, resection is performed to exclude a chondrosarcoma.
The tumor was removed and pathology was in keeping with a peripheral ACT.
Image
Radiographs show an expansile lesion
with cartilage matrix mineralization originating from the right femur at the
level of the lesser trochanter.
The cartilage cap seems well demarcated and
matured.
MRI was performed to assess the cartilage thickness of the cap.
Continue with the MRI...
T2W-image with fat saturation demonstrates a thin overlying
cartilage cap of only 3 millimeters.
The rest of the lesion is matured, which means that it contains bone marrow with suppressed signal on the fat saturated sequence
Continue with the CT....
In addition, see the complete bony maturation
of the cartilage cap on the unenhanced CT.
The rim of the lesion is well defined.
This lesion was called an osteochondroma as there are no signs of malignancy, it is not suspicious of ACT or chondrosarcoma.
Sometimes these osteochondromas are resected due to mechanical complaints or after a fracture, and they may give rise to an overlying bursa.
Differential diagnosis of Chondroid tumors
The
differential diagnosis of chondroid tumors depends on the age, location and whether
there are single or multiple lesions.
Several examples of differential diagnoses are given in the table.
Bone infarctions and polyostotic fibrous dysplasia are “do not touch lesions”.
This means that these lesions have such a typical appearance that they can be characterized based on radiographs alone without the need for a biopsy.
However if there is only a single lesion and the diagnosis of fibrous dysplasia is uncertain, CT guided biopsy may be performed.
In case of highly aggressive tumors, other primary bone tumors such as Ewing sarcoma and osteosarcoma may enter the differential diagnosis.
Especially the rare subtype osteolytic osteosarcoma or chondroblastic osteosarcoma can be difficult to distinguish from chondroid tumors.
In case of doubt, a biopsy for pathology diagnosis needs to be obtained, as there are important consequences for treatment (such as chemotherapy in osteosarcoma patients).
In patients over 50 years of age, the differential diagnosis includes metastasis and plasmacytoma.
Bone infarction
The most common differential diagnosis for matrix mineralization in the metaphysis of a long bone is a bone infarction.
These calcifications appear more squared than rounded such as in cartilage tumors.
In addition, bone infarctions are often multifocal and may occur bilaterally.
Image
Radiograph demonstrates multiple serpiginous sclerotic lesions in the distal femur and proximal tibia, centered on the metaphysis.
This image is typical for bone infarctions and occurred due to longstanding steroid use in a patient with SLE.
Note the absence of stippled chondroid calcifications.
Fibrous dysplasia
In the differential diagnosis we can consider fibrous dysplasia, which often contains a cartilage component.
In most cases the ground glass appearance on radiographs helps to differentiate.
First look at the images of a 23-year-old male with a history of pubertas praecox (early puberty). Then continue reading.
Hip
There is expansion of the proximal femur with widening of the metaphysis and a ground glass osteolytic lesion with sclerotic margins in the medullary cavity. Note the secondary osteoarthritis of the hip.
Wrist
The distal radius shows the same appearance with a changed bone structure due to ground glass osteolytic lesions with expansion. Also the first and second metacarpals are affected.
Conclusion
The multiple bone involvement together with the age, history of pubertas praecox and the radiographical appearance make this pathognomonic for FD.
No biopsy should be done.
This patient is known with polyostotic fibrous dysplasia as a part of the McCune Albright syndrome.
Images
Radiograph of the right humerus in a 26 year old patient shows a large lesion filling the medullary cavity of the proximal humerus metaphysis and diaphysis, with osteolytic and groundglass appearance and more sclerotic components distally.
There are no periosteal reaction or other aggressive features.
Given the age and this appearance, FD would be a likely diagnosis.
MRI was performed for further characterisation in this case.
Coronal T1 and STIR images demonstrate cystic components within the lesion, which are hypo-intense on T1W and hyperintense on STIR (arrows). These are typical for FD.
In between the cystic areas there is fat, which is hyperintense on T1W and signal is suppressed on STIR (asterix).
Note the distal part of the lesion contains very low signal intensity corresponding to the sclerosis on X-ray.
FD can appear heterogeneous and contain cartilage components adjacent to cystic areas or sclerosis.
No biopsy is needed as these findings are in keeping with mono-ostotic FD.
Langerhans cell histiocytosis
In the ribs Langerhans cell histiocytosis may mimic a chondroid tumor.
Images
- Incidental finding on a CT of the chest with an expansile osteolytic lesion at the costo-chondral junction on the left. The lesion shows scalloping and focal destruction of the cortex, no chondroid matrix was found.
- T2W-image with fatsat demonstrates a hyperintense lesion with a sclerotic rim.
- After contrast the lesion enhances homogeneously without septonodular enhancement.
Conclusion
The differential diagnosis includes a cartilage tumor (CS-I because ribs are part of the axial skeleton), Langerhans cell histiocytosis (typical location, young patient), and in patients over 50 years think of multiple myeloma (typical location).
A biopsy was performed under CT guidance and LCH was the final diagnosis.
The lesion was followed up and resolved without treatment.
In case of highly aggressive tumors (high grade CS), other primary bone tumors such as Ewing sarcoma and osteosarcoma may enter the differential diagnosis.
Especially in the more rare osteolytic osteosarcoma cases this can be difficult to distinguish from chondroid tumors.
In patients over 50 years of age, a metastasis can be a mimicker of a chondroid tumor.
WHO classification of chondroid tumors
In the 2013 WHO classification,
the term atypical cartilaginous tumor (ACT) was introduced as a synonym for
chondrosarcoma grade 1 (CS1) and classified as intermediate (locally
aggressive) to reflect
the clinical behavior of these well-differentiated low-grade lesions.
The argument was that such lesions,
especially in the long bones, behave in a locally aggressive manner and do not
metastasize. Therefore, they should not be classified as having full malignant potential
(1).
In the 2020 WHO edition the term ACT
is only reserved for low-grade chondrosarcomas located within the long bones of
the appendicular skeleton.
The term “CS1”should be reserved for tumors of the
axial skeleton, including the pelvis, ribs, scapula and skull base (flat
bones), reflecting
the poorer clinical outcome of these tumors at these sites.
Primary central ACTs arise in the medulla of long bones without a benign
precursor.
Secondary central ACTs arise centrally in bone in association with a
preexisting enchondroma.
Peripheral ACTs in long bones arise secondary within the cartilaginous
cap of a preexisting osteochondroma.
The WHO 2020 defined a cut-off of 2 cm
for the cartilage cap thickness.
Other changes in the 2020 WHO classification
are:
- Chondroblastoma and chondromyxoid fibroma (previously classified as an intermediate locally aggressive tumor) are now classified as benign.
- Synovial chondromatosis (previously classified as benign tumor) has now been classified as an intermediate locally aggressive tumor category because of its locally aggressive behavior, which is characterized by a high incidence of local recurrence.
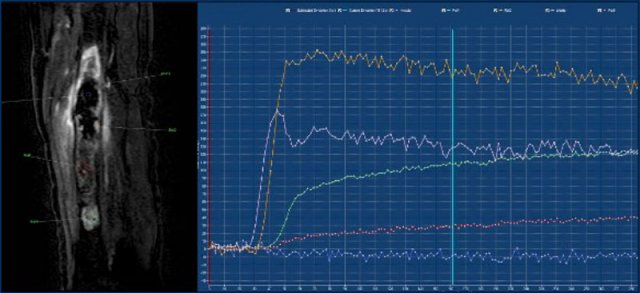
MR perfusion
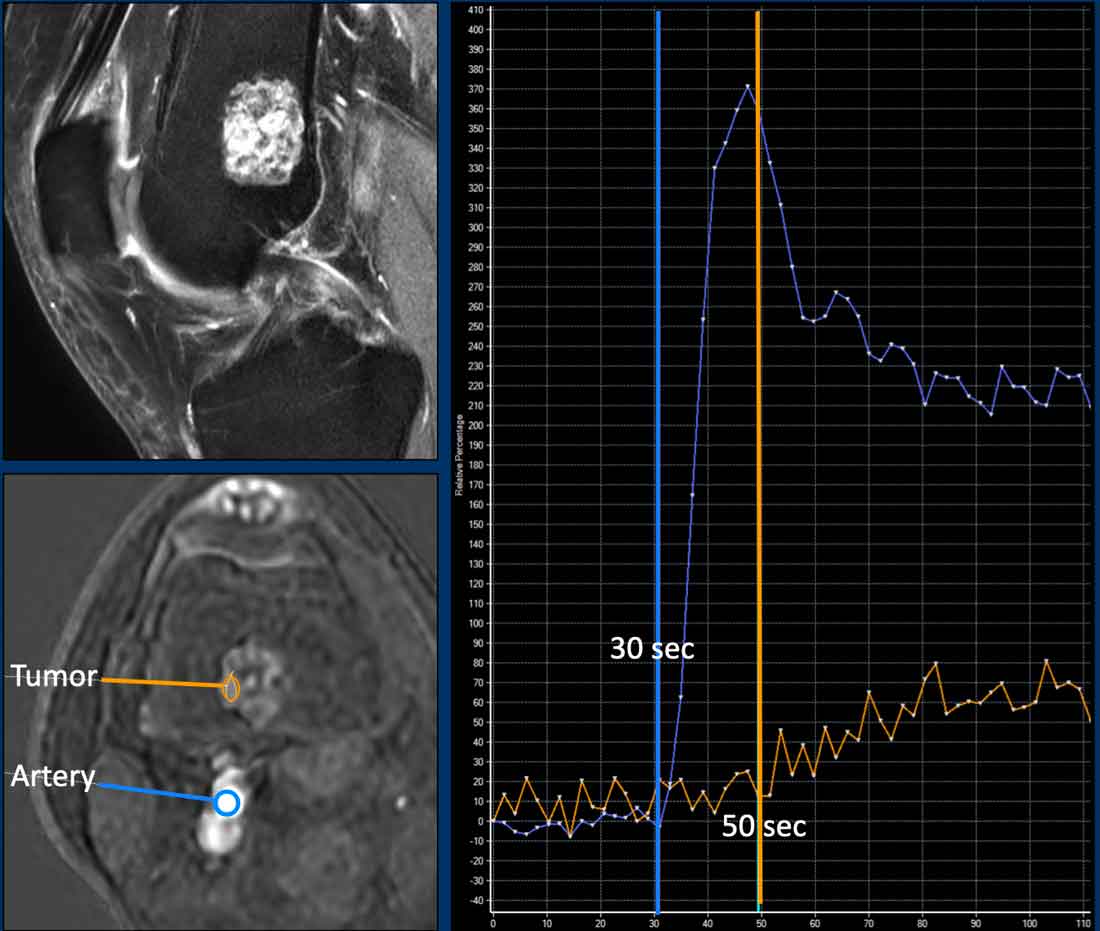 ACT along the posterior cortex in the distal femur showing septonodular enhancement after contrast. Two ROIs were placed, one in the tumor (orange) and one in the popliteal artery (blue).
ACT along the posterior cortex in the distal femur showing septonodular enhancement after contrast. Two ROIs were placed, one in the tumor (orange) and one in the popliteal artery (blue).
Perfusion MRI is a functional imaging technique in which early enhancement of the tumor is monitored after an intravenous gadolinium bolus injection.
This technique provides information on vascularisation and perfusion, capillary permeability, and interstitial compartment volume.
The technique is used for soft tissue and bone tumors (mostly in dedicated tumor centers) all over the world, and may aid for example in selecting a non-necrotic area for biopsy, or for differentiation of a local recurrence versus granulation tissue. Perfusion may help to characterize lesions and to differentiate benign from malignant lesions.
Perfusion MR practically means that you assess the arrival and clearance of gadolinium contrast within a tumor over time.
For this, very fast images need to be obtained with a high temporal resolution (every 2 or 3 seconds), while the contrast washes in and out of the tumor over a total time period of 3 to 5 minutes.
After the dynamic images are obtained, the protocol is usually completed with static post contrast sequences in 2 different planes.
Using a post processing software program, a region of interest (ROI) is drawn within an artery close to the tumor. Next, one or more ROIs are drawn within the tumor and in a healthy muscle for reference.
These different ROIs are then plotted on a time intensity curve (TIC).
In cartilage tumors, perfusion has been used to differentiate enchondroma from chondrosarcomas.
A cut off of 10 seconds is used for fast versus slow enhancement. However, overlap in early enhancement patterns of CS and enchondroma may occur, for example: fast enhancing enchondromas exist, but also slow enhancing ACTs.
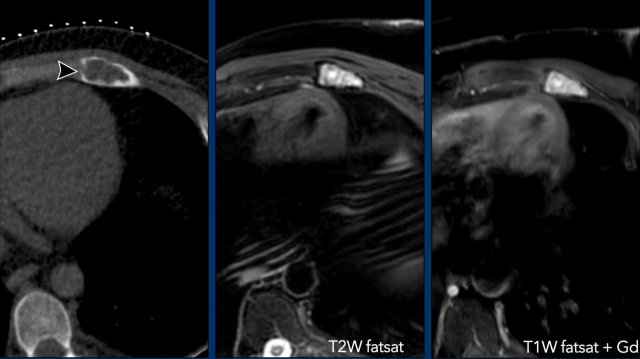
Images
Example of a slow enhancing ACT (orange line), more than 10 seconds after the artery (blue line).
Images
A chondroid tumor in the sternum with perilesional oedema and septonodular enhancement.
The perfusion images show fast enhancement of the tumor (orange ROI and curve) , within 8 seconds after the aorta (blue ROI and curve).
The pink ROI and curve represent mucoid which does not enhance.
This lesion was resected.
Final diagnosis: CS-I in the sternum
Various enhancement patterns exist, and these have been defined to help radiologists characterize different tumor types.
For example, fast enhancement (within 10 seconds after the artery) followed by wash-out is typical in the nidus of an osteoid osteoma or in a giant cell tumor of bone and is called a type IV curve.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here or on the image below to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.