Bone tumor P-Z
Bone tumors and tumor-like lesions in alphabethic order
Henk Jan van de Woude and Robin Smithuis
Radiology department of the Onze Lieve Vrouwe Gasthuis, Amsterdam and the Rijnland hospital, Leiderdorp, the Netherlands
Publicationdate
In the article Bone Tumors - Differential diagnosis we discussed a systematic approach to the differential diagnosis of bone tumors and tumor-like lesions.
The differential diagnosis mostly depends on the age of the patient and the findings on the conventional radiographs, i.e. is it a sclerotic lesion or an osteolytic lesion with either well-defined or ill-defined borders.
In this article we will discuss the most common bone tumors and tumor-like lesions in alphabethic order.
Paget's disease
key facts
- Paget disease is a chronic disorder of unknown origin with increased breakdown of bone and formation of disorganized new bone.
- The osteolysis can result in osteoporosis circumscripta in the skull and deformity and wedge fractures in long bones.
- There is always enlargement of bone with coarse appearance of trabeculae.
- Usually a mixed lytic-sclerotic appearance.
- Second most common bone disorder after osteoporosis.
- 70-90% of persons with Paget disease are asymptomatic.
Study the images and then continue reading.
The findings are:
- Pathognomonic triad of bone expansion, cortical thickening and trabecular bone thickening.
- This is the mixed lytic and sclerotic phase of Paget.
- Positive bone scan.
Here we see broadening of the ulna shaft is seen with a mixed lytic-sclerotic appearance and coarse trabeculation.
Differential diagnosis based on the radiograph:
- Paget's disease
- Fibrous dysplasia
The intense uptake of the tracer on the bone scintigraphy makes the diagnosis of Paget's disease the most likely.
Here we see the pathognomonic triad of :
- Bone expansion
- Cortical thickening
- Trabecular bone thickening
This is the mixed lytic and sclerotic phase of Paget's disease
Here the typical 'cotton wool' appearance of the skull based on a mixed lytic and sclerotic pattern of Paget's disease.
Parosteal osteosarcoma.
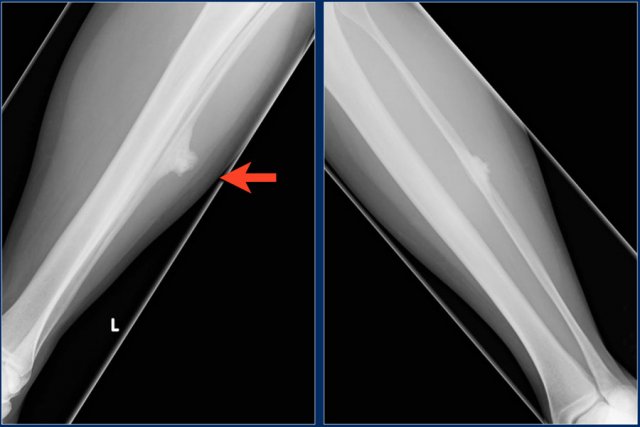
Broad-based solid sclerotic mass, adjacent to the diaphyseal cortical bone of the fibula shaft.
This lesion can easily be misdiagnosed as a reactive post-traumatic mass, like an ossified hematoma.
Biopsy revealed parosteal osteosarcoma.
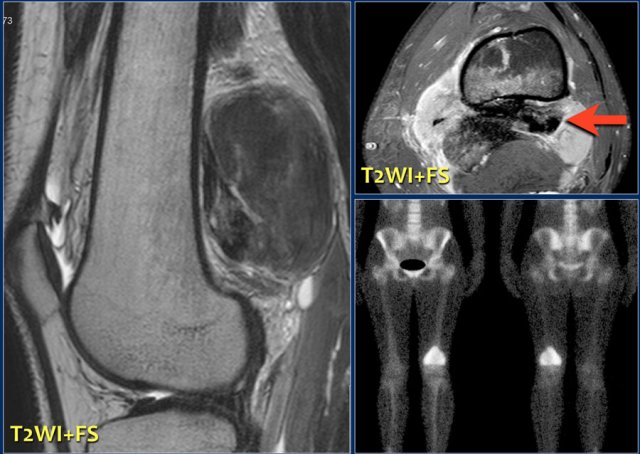
sclerotic mass, partially ill-defined posteriorly to the distal femur in a 20-year-old patient.
This is a rather typical location and presentation of an osteosarcoma, of the parosteal / juxtacortical subtype.
Continue with the MR-images...
The tumor shows intense activity on the body scintigram.
Sagittal and axial T2 weighted images demonstrate low signal parts of the bony matrix and some areas of high Si.
Parosteal or juctacortical osteosarcoma in different patient with secondary invasion of the distal femur.
Here images of a young female patient with painful swelling of the humerus.
Study the images and then continue reading.
The findings are:
- Plain radiograph: heterogeneous sclerotic mass against the shaft of the humerus.
- MR: partial enhancement of the bone marrow, which is also of importance for the surgical strategy.
Notice the lucency on the radiograph due to a biopsy.
This should be avoided when a parosteal osteosarcomais in the differential diagnosis.
The narrow relation to the cortical surface, the irregular contours, the more or less homogeneous sclerosis and the lack of perilesional edema make a diagnosis of a reactive process less likely.
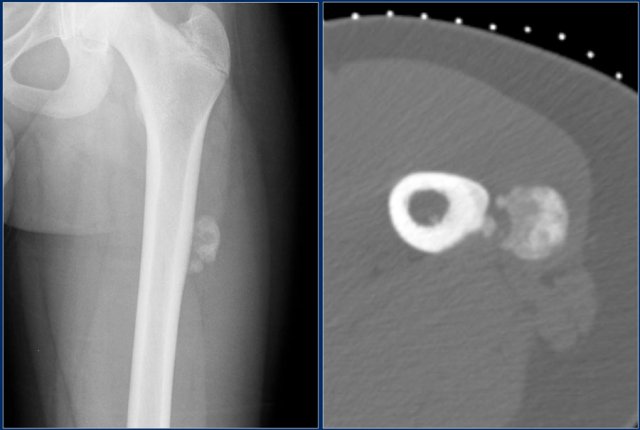
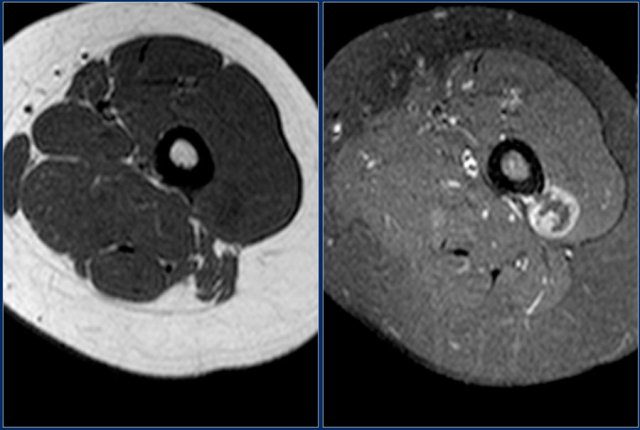
Here a similar case of a 15-year old female with swelling of the left thigh without a previous trauma.
Plain film and CT show a rather homogeneous sclerotic mass adjacent to the cortical bone.
there is no periosteal rection.
Because of hte history and because the sclerosis develops from the periphery to the center, this lesion is very suspicious to be a parosteal sarcoma.
Biopsy: parosteal osteosarcoma.
Continue with the MR...
Axial T1WI before and after contrast administration.
Notice lack of peripheral reactive edema which is usually present in a reactive process or post-traumatic myositis ossificans.
Periosteal chondroma
Periosteal or juxtacortical chondroma arises at the surface of the bone.
Scalloping of cortical bone is possible, but there is no marrow involvement.
It may be difficult to differentiate from a periosteal chondrosarcoma.
The size of the lesion is the most important factor.
It may also be difficult to differentiate a periosteal chondroma from a periosteal osteosarcoma, however periosteal chondroma is much more common.
Pigmented Villonodular Synovitis
key facts:
- Synovial proliferation with hemosiderin deposition.
- Hemosiderin results in areas of low signal intensity on Gradient- and T2W-images.
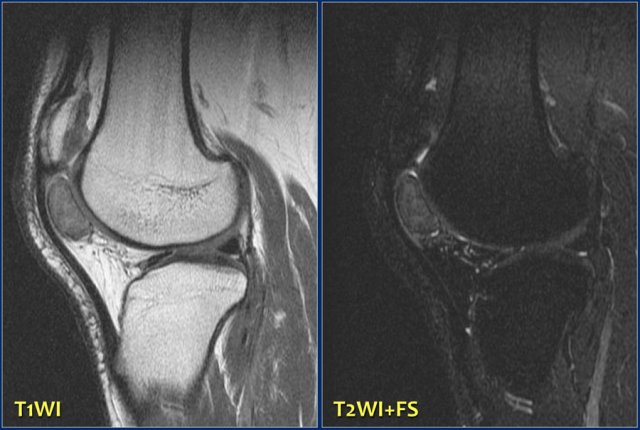
Study the images and then continue reading.
The findings are:
- Solitary well-defined soft tissue lesion in the superior part of Hoffa's fat pad
- Relatively low signal intensity on T2-weighted fat-suppressed image
These findings are consistent with the diagnosis Pigmented Villonodular Synovitis, which is a localized form of diffuse tenosynovial giant cell tumor.
Plasmocytoma
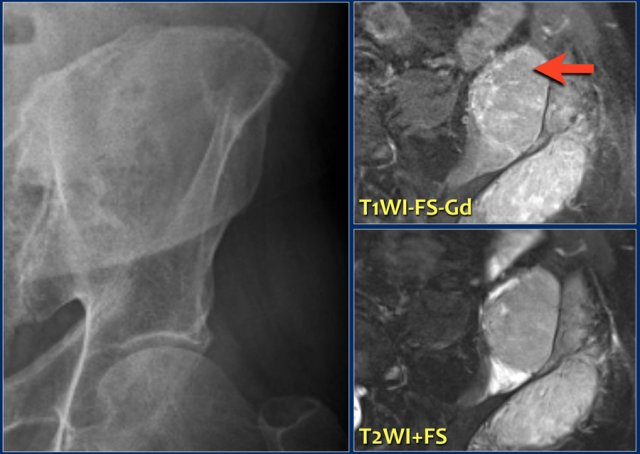
Here a 67-year old male with pain in the left buttock area.
There is an unsharp lytic lesion in the iliac wing.
Axial MR images (T2 FD and T1 CE fat suppressed) demonstrate a tumor with a large associated soft tissue mass.
Differential diagnosis:
- Metastasis
- Myeloma
- Lymphoma.
Biopsy revealed plasmacytoma
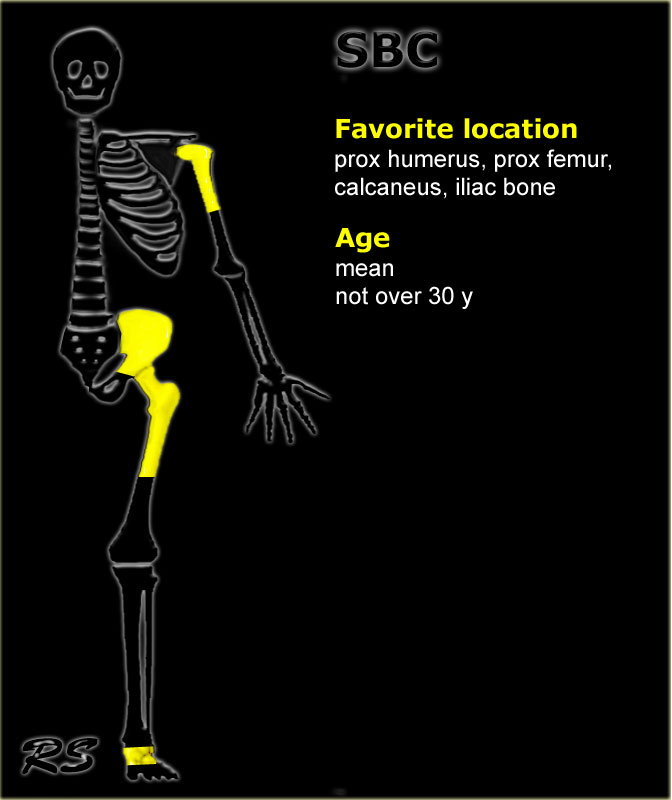
Solitary bone cyst
key facts:
- Well-defined osteolytic lesion most frequently seen in the proximal humerus (55%) or proximal femur (20%)
- Tendency to migrate from the metaphysis to the diaphysis during growth
- Centrally located with minor or mild expansion only
- May present with a fracture after a minor trauma.
- So called fallen fragment may be found
- DD: ABC or fibrous dysplasia
Left:
Young patient with well-defined diaphyseal lucent lesion, with some expansion and cortical thinning.
Diagnosis: SBC, differential diagnosis: ABC usually more expansion or fibrous dysplasia.
Middle:
Another young patient with well-defined expansile lucent lesion in the proximal meta-diaphysis of the fibula.
Because of the expansion, ABC should be considered.
Histology revealed SBC.
SBC may migrate from metaphysis to diaphysis during growth.
Right:
A well-defined lytic lesion with sclerotic margin in the right iliac wing of an adult.
Benign characteristics. Diagnosis is SBC. SBC can be encountered as an asymptomatic coincidental finding in the pelvis.
Here a well defined lytic lesion of the proximal humerus in a 11-year old boy.
Minimal expansion and some ridges and no fluid sedimentation levels on T1- and T2-weighted MR images.
First diagnosis should be solitary bone cyst.
Differential diagnosis:
- Fibrous dysplasia with secondary cyst formation.
- Aneurysmal bone cyst (less likely).
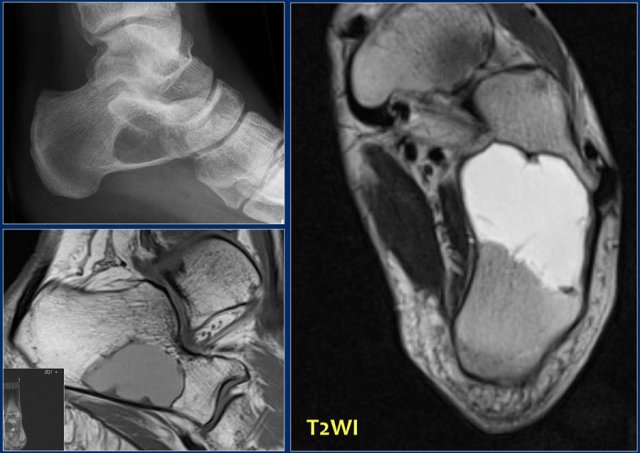
Sharply-defined lytic lesion of the calcaneal bone.
Differential diagnosis based on x-ray:
- Intraosseous lipoma
- Intraosseous ganglion.
- Solitary bone cyst.
- Aneurysmal bone cyst.
- Fibrous dysplasia.
MR doesn't show signal intensity of fat or blood (sedimentation).
Histology showed solitary bone cyst
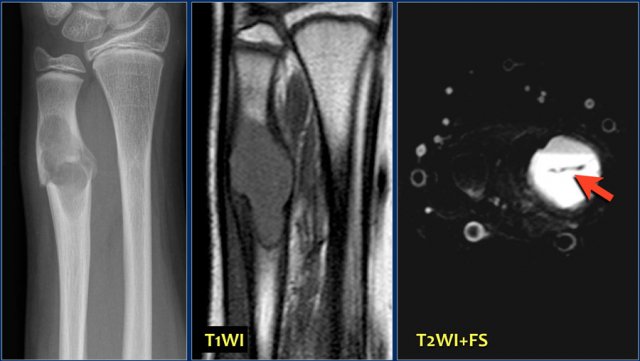
Here a well-defined lytic lesion in the distal metaphysis of ulna with a fracture.
T1-weighted MR image reveals some expansion.
Axial fat-suppressed T2-weighted image demonstrates a single fluid level with linear fallen fragment (arrow), highly suggestive for traumatized solitary bone cyst.
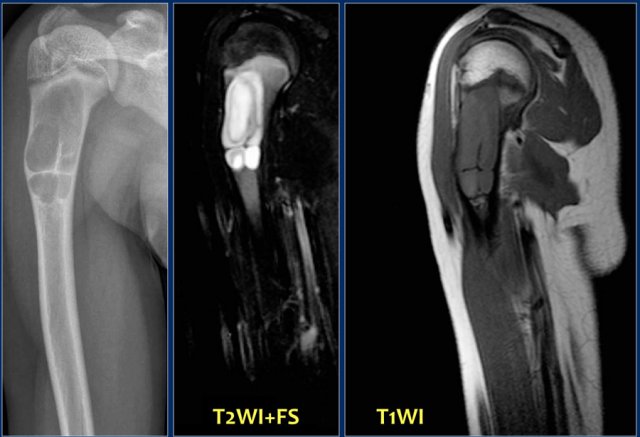
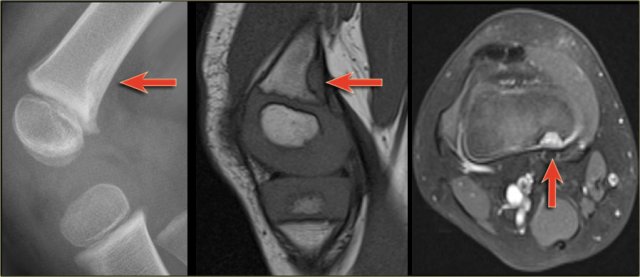
Here another well-defined lytic lesion in proximal humerus of a young boy.
There is endosteal scalloping and a fracture.
T2-weighted MR image shows homogeneous high SI of the lesion with rim enhancement on T1-weighted fat-suppressed image.
Differential diagnosis on plain film:
- SBC
- Fibrous dysplasia
- Aneurysmal bone cyst (usually more expansile)
- Chondroid lesion
Final diagnosis: solitary bone cyst.
Here another young patient with a typical SBC.
Another typical centrally located SBC presenting with a fracture.
SBC in fibula.
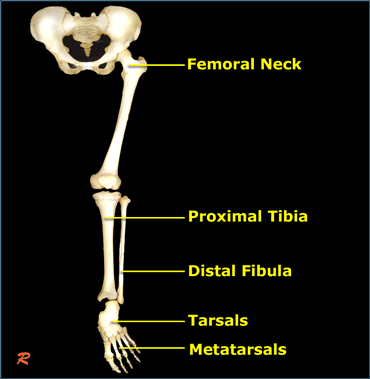
Stress fracture
key facts:
- Typical location in long bones - subcapital femur, proximal tibia metaphysis, distal tibia metaphysis
- Linear sclerosis is diagnostic
- In uncertain cases: MRI is diagnostic
Typical stress fracture of medial side of the femoral neck
Typical stress fractures in medial tibia and metatarsals.
Tug lesion
key facts:
- Tendinous insertion may 'tug' its attachment: surface mass, sometimes with reactive calcification.
- Also called cortical desmoid.
- Underlying cortex may resorb ('tendonoperiostitis')
- Best known site: 'cortical desmoid' at posteromedial corner distal femoral metaphysis
- Also known as Cortical Desmoid