Pulmonary nodule - Benign versus Malignant
Differentiation with CT and PET-CT
Ann Leung and Robin Smithuis
Department of Radiology, Stanford University Medical Center, Stanford, California and the Department of Radiology, Rijnland Hospital, Leiderdorp, the Netherlands
Publicationdate
A solitary pulmonary nodule is defined as a discrete, well-marginated, rounded opacity less than or equal to 3 cm in diameter that is completely surrounded by lung parenchyma, does not touch the hilum or mediastinum, and is not associated with adenopathy, atelectasis, or pleural effusion.
Lesions larger than 3 cm are considered masses and are treated as malignancies until proven otherwise.
The differential diagnosis of a solitary pulmonary nodule is broad and management depends on whether the lesion is benign or malignant.
In this overview we will discuss some of the new features that can help to differentiate between benign and malignant nodules based upon CT and PET-CT findings.
CT: benign versus malignant
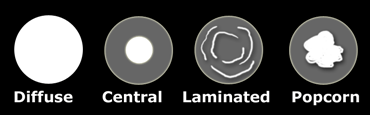
Calcification
Diffuse, central, laminated or popcorn calcifications are benign patterns of calcification.
These types of calcification are seen in granulomatous disease and hamartomas.
All other patterns of calcification should not be regarded as a sign of benignity.
The exception to the rule above is when patients are known to have a primary tumor.
For instance the diffuse calcification pattern can be seen in patients with osteosarcoma or chondrosarcoma.
Similarly the central and popcorn pattern can be seen in patients with GI-tumors and patients who previously had chemotherapy.
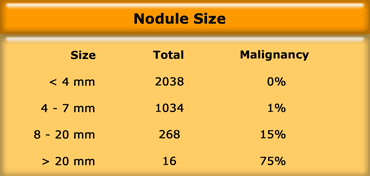
Size
A solitary pulmonary nodule (SPN) is defined as a single intraparenchymal lesion less than 3 cm in size and not associated with atelectasis or lymphadenopathy.
A lesion greater than 3 cm in diameter is called a mass.
This distinction is made, because lesions greater than 3 cm are usually malignant, while smaller lesions can be either benign or malignant.
Swensen et al studied the relationship between the size of a SPN and the chance of malignancy in a cohort at high risk for lung cancer (1).
Their findings are listed in the table on the left.
They concluded that benign nodule detection rate is high, especially if lesions are small.
Of the over 2000 nodules that were less than 4 mm in size, none was malignant.
Growth
Comparison with prior imaging studies is often the most useful procedure to determine the importance of the finding of a SPN, since stability over 2 years is highly associated with benignity.
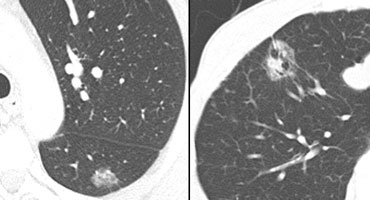
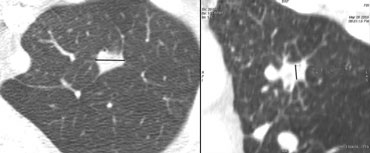 Transverse image (left) and coronal reconstruction (right)Three-dimensional ratio = transverse dimension : vertical dimension
Transverse image (left) and coronal reconstruction (right)Three-dimensional ratio = transverse dimension : vertical dimension
Shape
Japanese screening studies showed that a polygonal shape and a three-dimensional ratio > 1.78 was a sign of benignity (2,3).
A polygonal shape means that the lesion has multiple facets (multi-sided).
A peripheral subpleural location was also a sign of benignity in this study.
The three-dimensional ratio is measured by obtaining the maximal transverse dimension and dividing it by the maximal vertical dimension.
A large three-dimensional ratio indicates that the lesion is relatively flat, which is a benign sign.
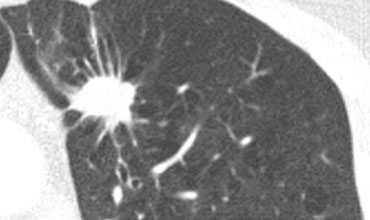
Margin
- Corona radiata sign - highly associated with malignancy (figure)
- Lobulated or scalloped margins - intermediate probability
- Smooth margins - more likely benign unless metastatic in origin
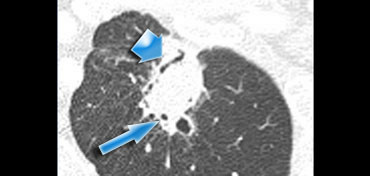
Air Bronchogram sign
Recent studies have showed that an air bronchogram is more commonly seen in malignant pulmonary nodules.
It is most commonly seen in BAC (bronchoalveolar cell carcinoma) and adenocarcinoma.
The case on the left shows an airbronchogram seen as a linear lucency (broad arrow) and as a more cystic lucency (small arrow) due to the fact that the bronchus is seen en face.
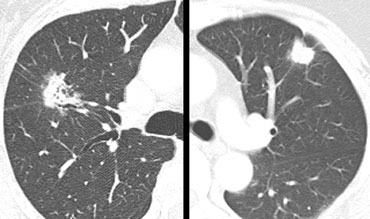
On the left two solitary pulmonary nodules.
Based upon the morphology, which lesion has the most malignant features?
The lesion on the far left has a spicuated margin and has lucencies within it.
The lesion next to it is lobulated in contour and has some spicules radiating to the pleura.
It is however homogeneous in attenuation.
Based on these findings we should be most concerned that the lesion on the far left is malignant.
It proved to be an adenocarninoma, while the other one was a fungal infection.
The lucencies and frank air bronchograms should not mislead you in thinking that it probably is infection.
Solid and Ground-glass components
Another result from screening studies is that nodules containing a ground-glass component are more likely to be malignant (5).
- Partly solid lesions with ground-glass components had a malignancy rate of 63%.
- Nonsolid - only ground-glass lesions had a malignancy rate of 18%.
- Only solid lesions had a malignancy rate of only 7%.
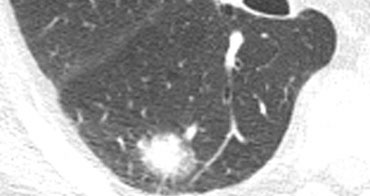
On the far left a lesion that only has a ground-glass appearance and next to it a lesion that has both ground-glass and solid components.
The likelihood of malignancy is 1:5 for the lesion on the far left and 2:3 for the lesion with both ground-glass and solid components.
Contrast enhancement
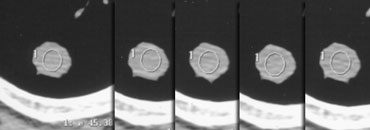
Contrast enhancement less than 15 HU has a very high predictive value for benignity (99%).
After a baseline scan, 4 consecutive scans at 1 minute interval are performed.
This applies only for nodules with the following selection criteria:
- Nodule > 5mm
- Relatively spherical
- Homogeneous, no necrosis, fat or calcification
- No motion or beam hardening artifacts
PET-CT: benign versus malignant
 False negative PET in a patient with adenocarcinoma. Activity is not sufficient for the diagnosis malignancy.
False negative PET in a patient with adenocarcinoma. Activity is not sufficient for the diagnosis malignancy.
PET-CT plays an increasingly important role in the evaluation of solitary nodules.
When you perform PET-CT, you have to realize the following:
- PET has a very high sensitivity 95%, but a lesser specificity of only 81%
- PET is false positive in granulomatous disease
- PET is usually false negative in size
With these specificity numbers, there will be false positives in about 20%, depending on the background prevalence of granulomatous disease.
On the left a patient with an adenocarcinoma, that was not hypermetabolic on the PET, so it is a false negative PET.
Conclusion
In the differentiation of benign versus malignant solitary pulmonary nodules nowadays new imaging features have to be added.
We especially have to look for the presence of areas of ground-glass opacity, air bronchograms or cavities and the three-dimensional ratios of a lesion.
With the increasingly important role of PET-CT, we have to be aware of the accuracy of PET-CT and we should have an idea about the prevalence of infectious and non-infectious granulomatous disease in the area that we practice.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.