Differential of Breast Calcifications
Robin Smithuis and Ruud Pijnappel
Radiology department, Rijnland Hospital, Leiderdorp and Martini Ziekenhuis, Groningen, the Netherlands.
Publicationdate
Ductal carcinoma-in-situ (DCIS) represents 25-30% of all reported breast cancers.
Approximately 95% of all DCIS is diagnosed because of mammographically detected microcalcifications.
In this review we will focus on:
- Description of breast calcifications
- Differential diagnosis
- BIRADS classification
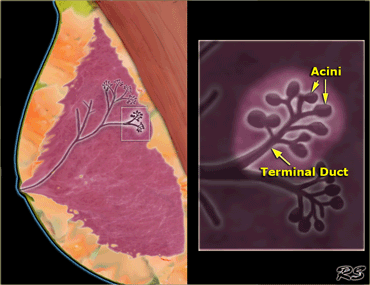
Anatomy
Terminal ductal lobular unit
The basic functional unit in the breast is the lobule, also called the terminal ductal lobular unit (TDLU).
The TDLU consists of 10-100 acini, that drain into the terminal duct.
The terminal duct drains into larger ducts and finally into the main duct of the lobe (or segment), that drains into the nipple.
The breast contains 15-18 lobes, that each contain 20-40 lobules.
The terminal ductal lobular unit is an important structure because most invasive cancers arise from the TDLU.
It also is the site of origin of ductal carcinoma in situ (DCIS), lobular carcinoma in situ, fibroadenoma and fibrocystic disease, like cysts, apocine metaplasia, adenosis and epitheliosis.
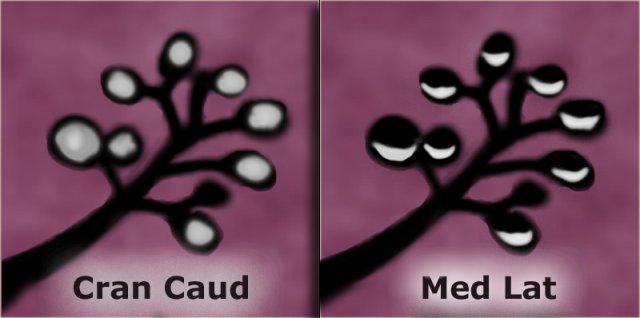
Most calcifications in the breast form either within the terminal ducts (intraductal calcifications) or within the acini (lobular calcifications).
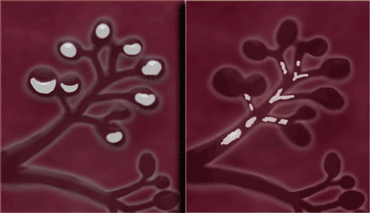 LEFT: Lobular calcifications: punctate, round or 'milk of calcium' RIGHT: Intraductal calcifications: pleomorph and form casts in a linear or branching distribution.
LEFT: Lobular calcifications: punctate, round or 'milk of calcium' RIGHT: Intraductal calcifications: pleomorph and form casts in a linear or branching distribution.
Lobular calcifications
These calcifications fill the acini, which are often dilated.
This results in uniform, homogeneous and sharply outlined calcifications, that are often punctate or round.
When the acini become very large, as in cystic hyperplasia, 'milk of calcium' may fill these cavities.
However when there is more fibrosis, as in sclerosing adenosis, the calcifications are usually smaller and less uniform.
In these cases it can be difficult to differentiate them from intraductal calcifications.
Lobular calcifications usually have a diffuse or scattered distribution, since most of the breast is involved in the process that forms the calcifications.
Lobular calcifications are almost always benign.
Intraductal calcifications
These calcifications are calcified cellular debris or secretions within the intraductal lumen.
The uneven calcification of the cellular debris explains the fragmentation and irregular contours of the calcifications.
These calcifications are extremely variable in size, density and form (i.e. pleomorphic from the Greek pleion 'more' and morphe 'form').
Sometimes they form a complete cast of the ductal lumen.
This explains why they often have a fine linear or branching form and distribution.
Intraductal calcifications are suspicious of malignancy and are classified as BI-RADS 4 or 5.
Diagnostic Approach
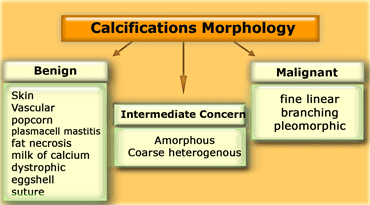
The diagnostic approach to breast calcifications is to analyze the morphology, distribution and sometimes change over time.
The form or morphology of calcifications is the most important factor in deciding whether calcifications are typically benign or not.
If not, they are either suspicious (intermediate concern) or of a high probability of malignancy.
Usually biopsy in these cases is needed to determine the etiology of these calcifications.
Morphology
The form of calcifications is the most important factor in the differentiation between benign and malignant.
If calcifications cannot be readily identified as typically benign or as 'high probability of malignancy', they are termed of 'intermediate concern or suspicious'.
If a specific etiology cannot be given, a description of the calcifications should include their morphology and distribution using the descriptions given in the BI-RADS atlas (1).
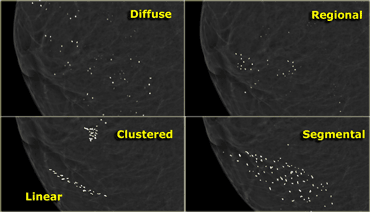
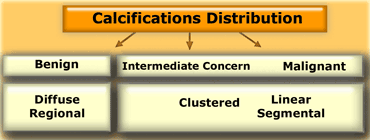
Distribution
In the BI-RADS atlas the following descriptions are given for the distribution of calcifications (1) :
- Diffuse or Scattered: diffuse calcifications may be scattered calcifications or multiple similar appearing clusters of calcifications throughout the whole breast.
- Regional: scattered in a larger volume (> 2 cc) of breast tissue and not in the expected ductal distribution.
- Clustered : at least 5 calcifications occupy a small volume of tissue (Linear: calcifications arrayed in a line, which suggests deposits in a duct.
- Segmental: calcium deposits in ducts and branches of a segment or lobe.
Diffuse or scattered distribution is typically seen in benign entities.
Even when clusters of calcifications are scattered throughout the breast, this favors a benign entity.
Regional distribution according to the BI-RADS atlas would favor a non-ductal distribution (i.e. benignity), while
Segmental distribution would favor a ductal distribution (i.e. malignancy).
Sometimes this differentiation can be made, but in many cases the differentiation between 'regional' and 'segmental' is problematic, because it is not clear on a mammogram or MRI where the bounderies of a segment (or a lobe) exactly are.
Clustered calcifications are both seen in benign and malignant disease and are of intermediate concern.
When clusters are scattered througout the breast, this favors a benign entity.
A single cluster of calcification favors a malignant entity.
Linear distribution is typically seen when DCIS fills the entire duct and its branches with calcifications.
Change over time
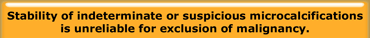
There are conflicting data concerning the value of absence of change over time.
It is said that the absence of interval change in microcalcifications that are probably benign on the basis of morphologic criteria is a reassuring sign and an indication for continued mammographic follow-up (2).
On the other hand in a retrospective study that included indeterminate and suspicious clusters of microcalcifications, stability could not be relied on as a reassuring sign of benignancy (3).
In this group of patients with biopsy proven malignancy, 25% of patients had stable microcalcifications for 8-63 months.
It seems that the morphology of calcifications is far more important than stability and stability can only be relied on if the calcifications have a probably benign form.
In the same study it was shown that the odds for invasive carcinoma versus DCIS are statistically significantly higher among patients with increasing or new microcalcifications.
The likelihood that carcinoma will be invasive increases significantly when a suspicious or indeterminate cluster of calcifications is new or increasing.
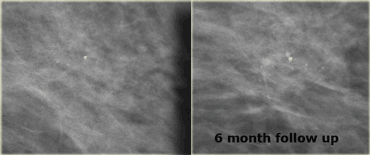
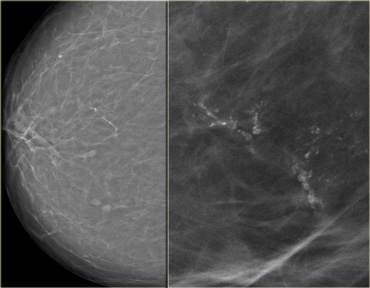
On the left a patient with a few heterogeneous coarse calcifications.
They were classified as BIRADS 3 (probably benign with a likelihood of malignancy less than 3%).
At six month follow up they had increased in number and DCIS was found at biopsy.
Benign Calcifications
Skin Calcifications - Tatoo sign
Many calcifications can be classified as typically benign and need no follow up (i.e. BI-RADS 1 or 2).
Many of these are skin calcifications. These are usually lucent-centered deposits.
Atypical forms may be confirmed by tangential views to be in the skin.
Usually they are located along the inframammary fold parasternally and in the axilla and areola.
When you consider the possibility of dermal calcifications, always study the portion of the skin that is seen en face to look for similar calcifications (arrow).
Tatoo sign
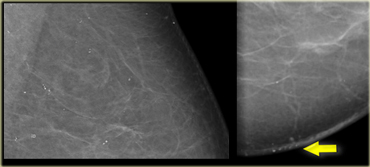
Skin calcifications may simulate parenchymal breast calcifications and may look like malignant-type calcifications.
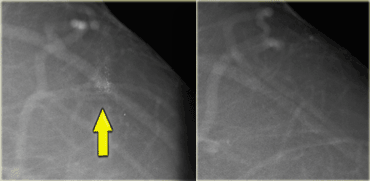
The cluster calcifications on the left was presented for biopsy.
During the vacuum assisted biopsy procedure it was not possible to biopsy these calcifications, because they were out of range.
When you look at the oblique and craniocaudal view, notice that the calcifications look exactly the same in configuration.
This is called the tattoo sign .
Spot views subsequently prooved that these were dermal calcifications.
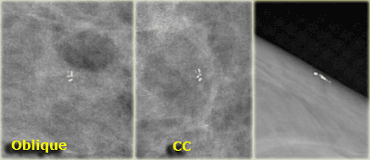
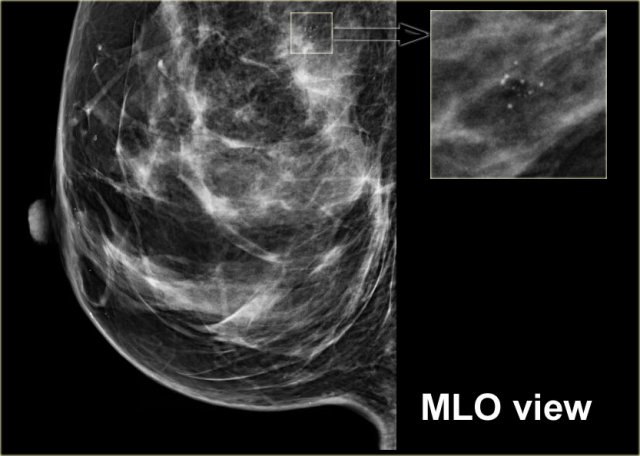
Here another example of the tatoo-sign.
First notice that there are some calcifications that are clearly located within the skin (arrows).
The cluster calcifications on the MLO-view has the exact configuration as the cluster on the CC-view (next image).
On the CC-view the configuration of the microcalcifications is exactly the same.
If these calcifications were located in the centre of the breast they should have a different configuration, because the projection is different.
Only when calcifications are located within the skin their configuration stays the same.
Tatoo sign video
Here two cases of skin calcifications presenting as tatoo sign (courtesy Roel Mus).
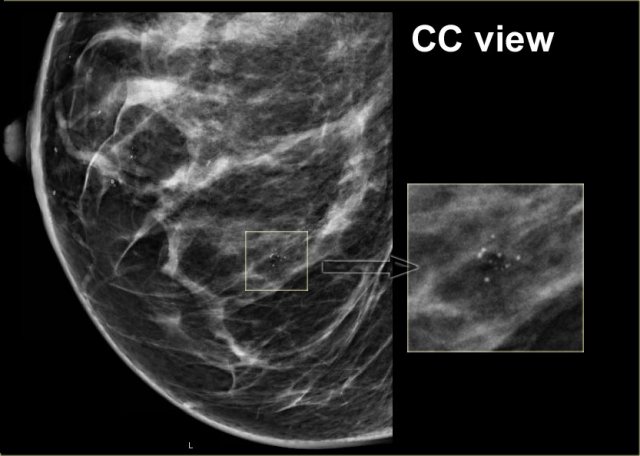
Vascular Calcifications
These are linear or form parallel tracks, that are usually clearly associated with blood vessels.
Vascular calcifications noted in women
On the left typical vascular calcifications.
If only one side of a vessel is calcified (arrow), the calcification may simulate intraductal calcification, but usually the diagnosis is straight forward.
Coarse or 'Popcorn-like'
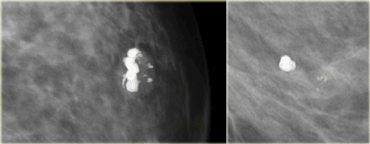
The classic large 'popcorn-like' calcifications are produced by involuting fibroadenomas.
These calcifications usually do not cause a diagnostic problem.
When the calcifications in an fibroadenoma are small and numerous, they may resemble malignant-type calcifications and need a biopsy.
Large Rod-like, Plasma cell mastitis
These are formed within ectatic ducts.
These benign calcifications form continuous rods that may occasionally be branching.
They are different from malignant-type fine branching calcifications, because they are usually > 1 mm in diameter.
They may have lucent centers if the calcium is in the wall of the duct.
These calcifications follow a ductal distribution, radiating toward the nipple and are usually bilateral.
These secretory calcifications are most often seen in women older than 60 years.
Sometimes it is difficult to differentiate these from lineair calcifications as seen in DCIS.
Round and punctate calcifications
Round calcifications are 0.5-1 mm in size and frequently form in the acini of the terminal duct lobular unit.
When smaller than 0.5 mm, the term 'punctate' is used.
Round and punctate calcifications can be seen in fibrocystic changes or adenosis, skin calcifications, skin talc and rarely in DCIS.
Suspect DCIS when the calcifications are small, i.e. punctate , and show some heterogeneity especially when in cluster, linear or segmental distribution.
Round and punctate calcifications are classified as:
- Bi-RADS 2: when scattered round calcifications.
- Bi-RADS 3 or 4: when in isolated cluster or if new or ipsilateral to a cancer.
Lucent-Centered
These are round or oval calcifications that range from under 1 mm to over a centimeter.
They are the result of fat necrosis, calcified debris in ducts, and occasional fibroadenomas.
Eggshell or Rim Calcifications
These are very thin benign calcifications that appear as calcium is deposited on the surface of a sphere.
These deposits are usually under 1 mm in thickness when viewed on edge.
Although fat necrosis can produce these thin deposits, calcifications in the wall of cysts are the most common 'rim' calcifications.
On the left a sharply defined lesion.
The low density indicates the presence of fat.
This is a typical oil cyst.
On a follow up mamogram the wall has calcified resulting in eggshel calcifications.
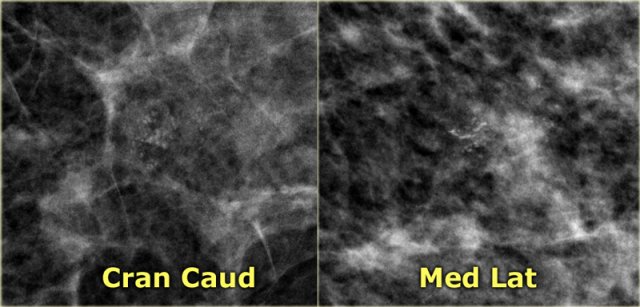
Milk of Calcium
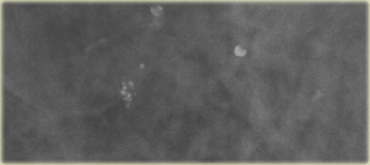
These are benign sedimented calcifications in macro- or microcysts.
On craniocaudad views they appear as fuzzy, round or amorphous.
Consider magnification spot film with horizontal beam when you think of the possibility of milk of calcium, because on a 90? lateral view they may appear as semilunar, crescent shaped tea cups.
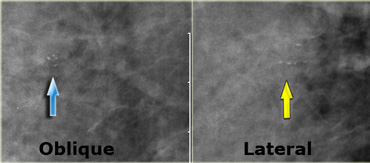 LEFT: cluster of pleiomorphic calcifications on oblique viewRIGHT: milk of calcium (teacups) on lateral view with horizontal beam
LEFT: cluster of pleiomorphic calcifications on oblique viewRIGHT: milk of calcium (teacups) on lateral view with horizontal beam
Many calcifications representing milk of calcium within microcysts however do not layer on horizontal beam radiographs.
The most important feature of these calcifications is the apparent change in shape of the calcific particles on different mammographic projections (craniocaudal versus oblique or 90? lateral).
The images show a different shape on the oblique view compared to the mediolateral view.
On the mediolateral view there is layering of the calcium.
On the craniocaudal image the calcifications are round, fuzzy and ill-defined.
On the mediolateral view the calcifications appear as semilunar, crescent shaped tea cups.
Click on the image for an enlarged view.
Suture calcifications
They represent calcium deposit on suture material.
They are typically linear or tubular in appearance and knots are sometimes visible.
Dystrophic calcifications
These are coarse irregular 'lava-shaped' calcifications.
These calcifications are larger than 0.5 mm and often have a lucent center.
They are seen in irradiated breast or following trauma.
They develop 3-5 years after treatment in about 30% of women.
These calcifications are also described as fat necrosis.
It is important to differentiate them from a recurrent malignancy.
On the left more extensive dystrophic calcifications.
Suspicious Calcifications
If calcifications are not typically benign, they are either called 'Suspicious or of Intermediate Concern'
or they are called 'High Probability of Malignancy'.
We will first discuss suspicious calcifications.
These calcifications have either an amorphous or coarse heterogeneous form.
Usually these calcifications are biopsied to determine their exact nature.
Amorphous calcifications
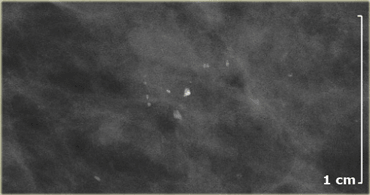
Amorphous or indistinct calcifications are defined as 'without a clearly defined shape or form'.
These calcifications are usually so small or hazy in appearance, that a more specific morphologic classification cannot be determined.
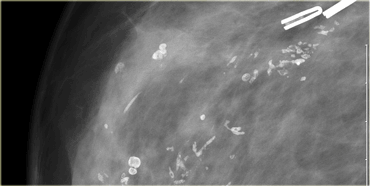
On the left amorphous and pleomorphic calcifications.
Based on the morphology these calcifications were classified as BI-RADS 4.
Biopsy revealed fibrocystic changes (FCC)
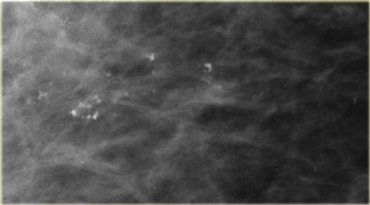
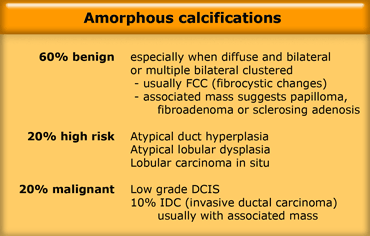
Amorphous calcifications (2)
Many benign and malignant breast diseases may present with amorphous calcifications (Table).
About 20% of amorphous calcifications turn out to be malignant.
Usually it is low grade DCIS.
Amorphous calcifications (3)
- BI-RADS 2: when diffuse and bilateral
- BI-RADS 3: when multiple bilateral clustered
- BI-RADS 4: when unilateral clustered or new on follow up or in a patient with a cancer in the contralateral breast
On the left amorphous calcifications within a denser area of the breast.
This was classified as Bi-RADS 4 (3-95% chance of malignancy).
Biopsy revealed DCIS with invasive ductal carcinoma.
Coarse Heterogeneous
Coarse heterogeneous microcalcifications, formerly called coarse granular, are irregular, conspicuous calcifications that are generally larger than 0.5 mm.
They are considered to be of intermediate concern, along with amorphous microcalcifications.
They have to be differentiated from fine pleomorphic microcalcifications, formerly called fine granular, that vary in size and shape, are usually less than 0.5 mm in diameter and are considered to be of higher probability of malignancy, along with the fine linear microcalcifications (1).
Coarse heterogeneous microcalcifications tend to coalesce but are not the size of the larger irregular dystrophic calcifications.
On the left coarse heterogeneous calcifications
They were classified as Bi-RADS 4.
Biopsy revealed DCIS.
The differential diagnosis of coarse heterogeneous calcifications includes:
- Fibroadenoma
- Fibrosis
- Post-traumic representing evolving dystrophic calcifications (fat necrosis)
- DCIS.
Multiplicity and bilaterality of such calcifications favors a benign etiology.
DCIS is considered when these calcifications have a clustered, linear or segmental distribution.
On the left a patient in whom new calcifications were detected during follow up for breastcancer in the contralateral breast.
There are coarse heterogeneous calcifications in a segmented distribution.
These calcifications were classified as Bi-RADS 4.
Biopsy showed calcifications within fibrous stroma.
There was no sign of malignancy.
High Probability of Malignancy
Calcifications with a higher probability of malignancy are:
- fine pleomorphic
- fine linear
- fine linear branching
Fine Pleomorphic
These calcifications vary in size and shapes and are usually.
They are more conspicuous than the amorphic calcifications.
There is a 25-40% risk of malignancy.
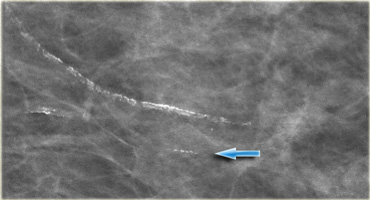
On the left fine pleomorphic calcifications in a segmental and linear distribution.
These were classified as BI-RADS 4B.
Biopsy revealed high grade DCIS.
 Fine pleomorphic calcifications in a segmental distribution in combination with an irregular mass (Bi-RADS 5)
Fine pleomorphic calcifications in a segmental distribution in combination with an irregular mass (Bi-RADS 5)
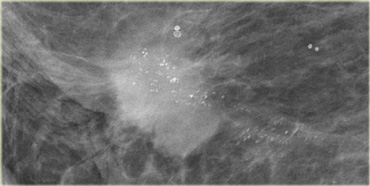
On the left a mammogram demonstrating two forms of calcifications.
There are some round typically benign calcifications.
The most conspicious calcifications however are the fine pleomorphic calcifications.
They have a segmental distribution.
In the presence of the mass these calcifications were classified as Bi-RADS 5.
Biopsy demonstrated an extensive high grade DCIS with an invasive carcinoma.
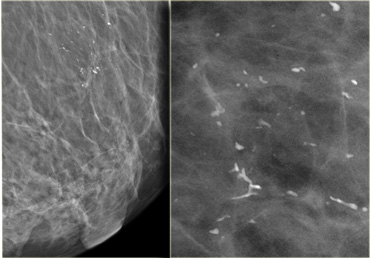
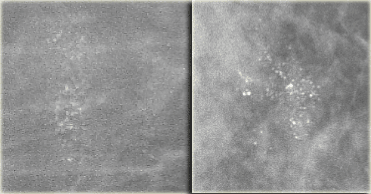
The calcifications on the left were detected on the first mammogram in a screening program.
There is a cluster of amorphous and fine pleomorphic calcifications.
These calcifications were classified as BI-RADS 4B.
A biopsy was performed and only fibrocystic changes were found.
On the left a case that looks quite similar to the one above.
New calcifications were detected during follow up in a screening program.
These are fine pleomorphic calcifications in a cluster.
These calcifications were classified as Bi-RADS 4.
This proved to be DCIS.
The message is that with these calcifications you cannot tell whether they are malignant or not and they have to be biopsied.
Fine Linear or Fine Linear Branching
These are thin, linear or curvilinear irregular calcifications.
They may be discontinuous.
Usually they are
Their appearance suggests filling of the lumen of a duct, i.e. 'casting' calcifications.
These calcifications are classified as Bi-RADS 4C.
On the left calcifications in a segmental distribution.
Some have a linear distribution and some have a branching morphology.
This is highly suggestive of malignancy (Bi-RADS 4C).
On the left fine linear and branching calcifications in a segmental distribution highly suggestive of malignancy (Bi-RADS 4C).
Extensive high grade DCIS was found at biopsy.
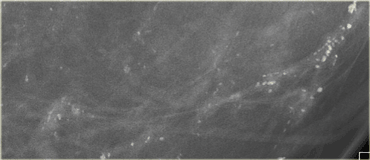
On the left a patient with new calcifications detected in a screening program.
These are fine pleomorphic and fine linear calcifications.
The distribution is linear.
On the basis of the morphology and distribution these calcifications were classified as BI-RADS 4C.
At biopsy this was high grade DCIS.
Artifacts
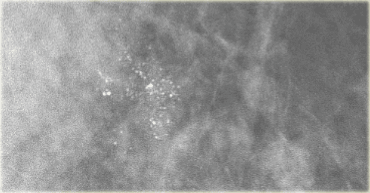
On the left artifacts within a cassette that simulate fine pleomorphic calcifications.
A repeat exam with a different cassette did not show any calcifications.
Image of the cassette.
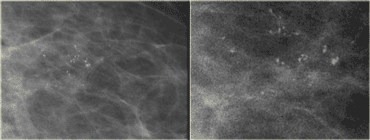
The image on the left shows the same artifacts.
On the image on the right DCIS.