Spontaneous Intracranial Hypotension
Stefan Roosendaal¹ and Jeroen Markenstein²
¹Amsterdam University Medical Center in the Netherlands and ²Algemeen Ziekenhuis Turnhout in Belgium
Publicationdate
Intracranial hypotension as a result of CSF leakage can be seen in patients who had a lumbar puncture, placement of tubes for epidural anesthesia or after spinal trauma and surgery.
CSF leaks can also occur without an obvious cause in the history of the patient.
Then it is called spontaneous intracranial hypotension (SIH).
Leakage of CSF at the spinal level is usually the cause of SIH and imaging plays an important role in identifying these patients with SIH and finding the cause of the leakage.
Introduction
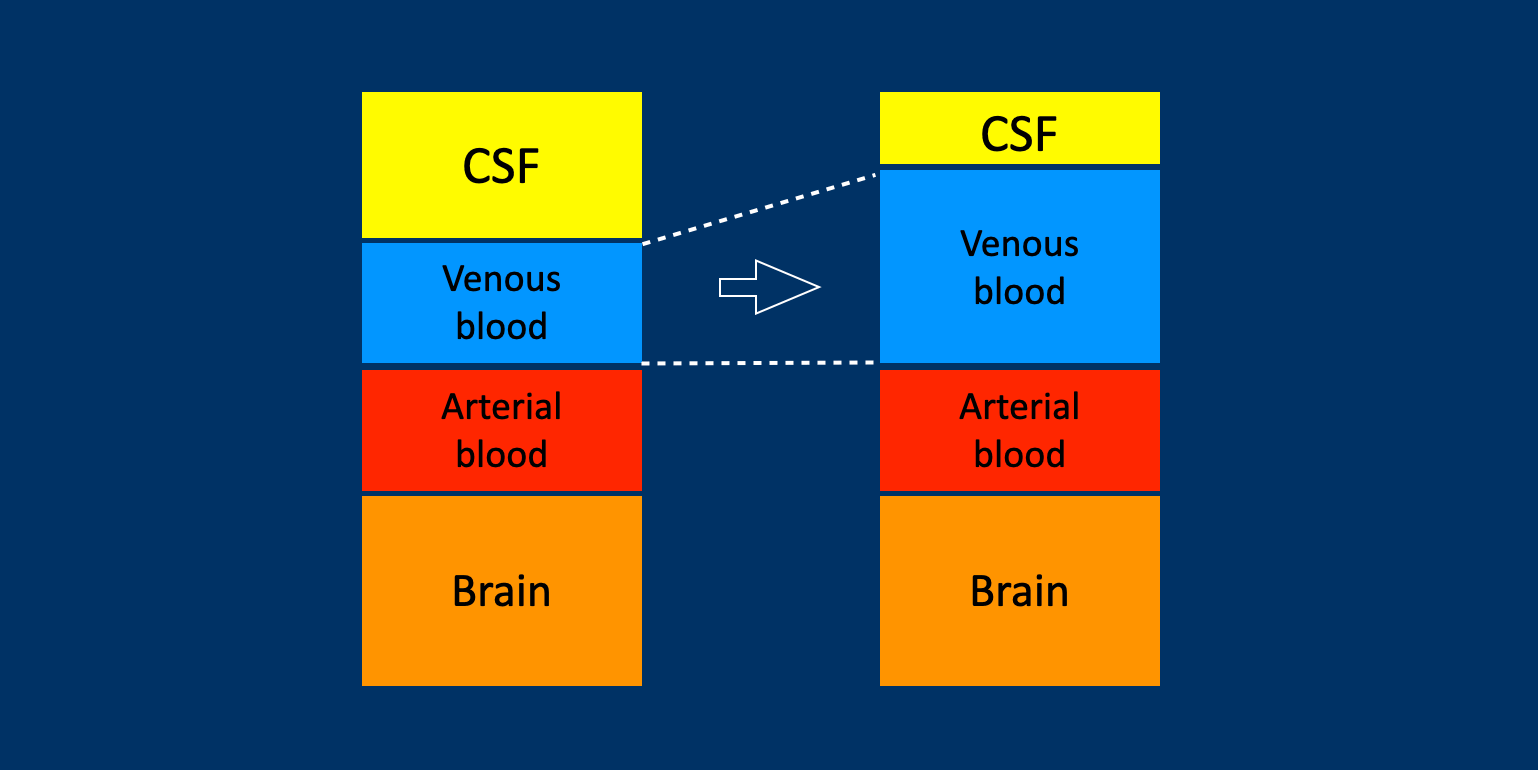
The brain is surrounded by the meninges that form a bag filled with cerebrospinal fluid (CSF).
The CSF provides cushioning and supports the brain as a result of the buoyancy provided by the fluid.
Normally, the weight of the brain is nearly 1500 grams in air.
However within the pool of CSF, the apparent weight of the brain is about
50 grams decreased due to the buoyancy, resulting in the tendency of the brain to float or to rise within the CSF.
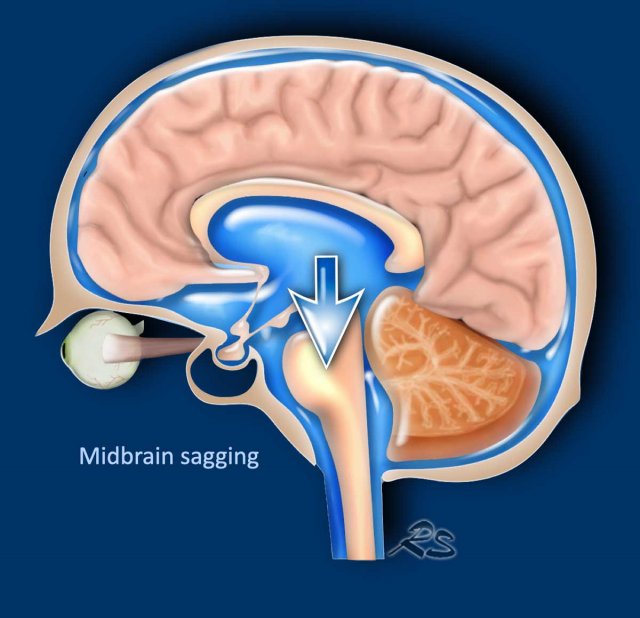
When the pressure of the CSF is too low or when there is less CSF due to a leak somewhere in the meninges, the brain may sag downward (fig).
This sagging causes traction on the sensory nerves of the meninges and the bridging veins, leading to headaches.
The traction on the meninges is increased in the upright position leading to increased intensity of headache when standing.
This is called postural headaches.
Leakage of CSF from the spinal thecal sac is increasingly recognized as the cause of spontaneous intracranial hypotension.
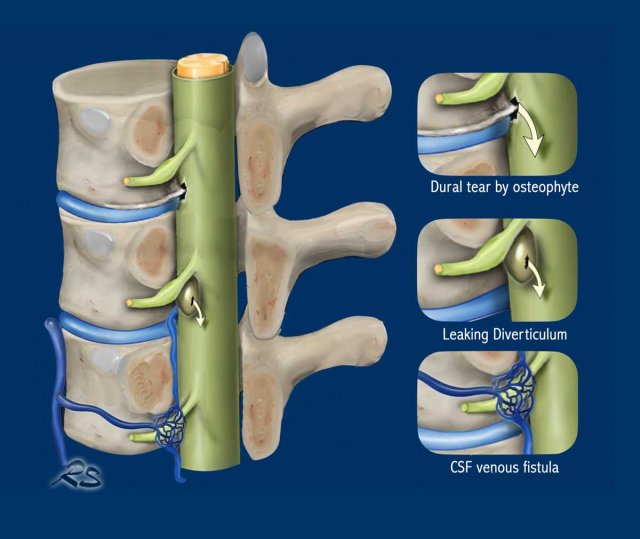
Leakage of CSF can result from:
- Dural tear caused by an osteophyte.
- Ruptured meningeal diverticulum
- CSF venous fistula.
Underlying weakness of the spinal dura can be present in many cases of spontaneous intracranial hypotension.
Several genetic disorders have been associated with a thin or weak dura that may predispose to CSF leaks.
These include:
- Ehlers-Danlos syndrome
- Marfan syndrome
- Autosomal dominant polycystic kidney disease
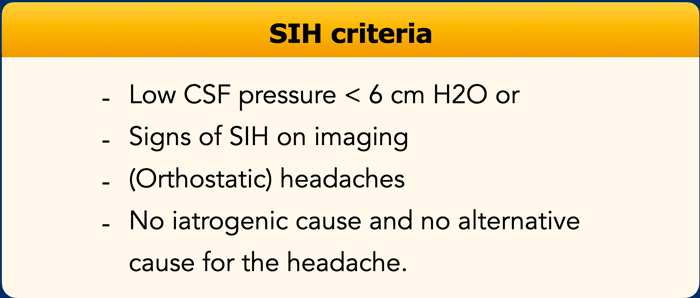
Criteria for SIH
Criteria for the diagnosis of SIH are:
- Low CSF pressure < 6 cm H2O or
Signs of SIH on imaging. - (Orthostatic) headaches.
- No iatrogenic cause like lumbar puncture, epidural anesthesia etc.
- No alternative cause for the headache.
It is estimated that intracranial hypotension affects about 5 per 100.000 people, but it is thought to be underdiagnosed.
The problem is that many patients do not have the typical symptoms and most of them do not have an abnormal low CSF pressure when measured by liquor puncture (LP).
The normal range of intracranial pressure measured by LP in adults is quite broad (6 to 25 cm H₂O) with a mean value of 18 cm H₂O.
Although most patients with SIH have a relatively low CSF pressure, only 34% of patients have an abnormal low pressure (0-6 cm H₂O).
This means that 66% of patients with SIH have an intracranial pressure within the normal range.
Therefore imaging plays an important role in the diagnosis of SIH.
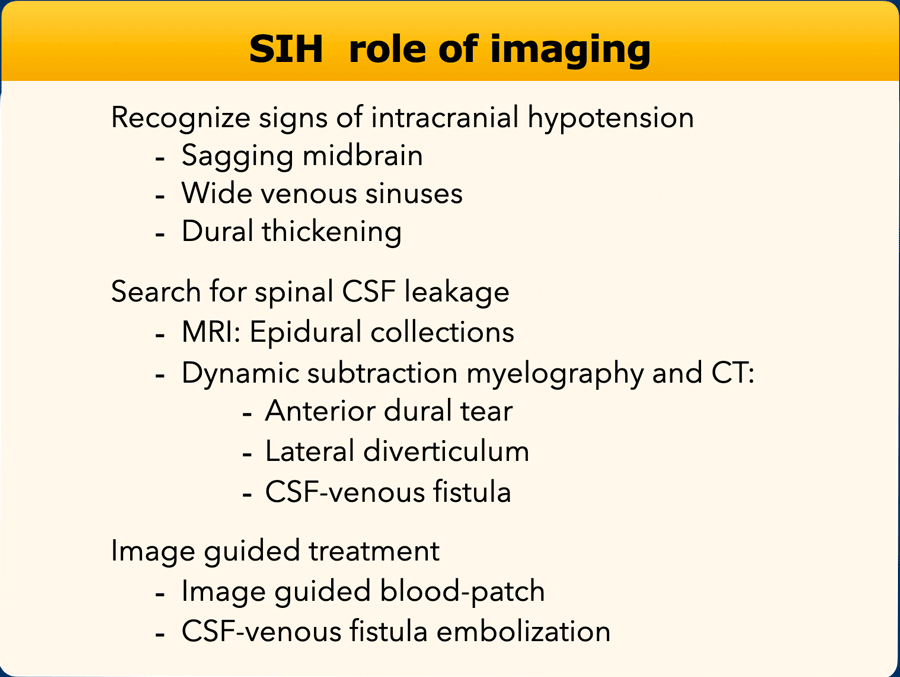
Role of Imaging
The role of imaging is:
- Diagnosing SIH: Sagging midbrain, wide venous sinuses and dural thickening.
- Finding the spinal CSF leakage: Epidural collections on MRI and with Subtraction myelography and CT finding an anterior dural tear, a lateral diverticulum or a CSF-venous fistula.
- Image guided treatment of the leak with a blood patch or embolization of a CSF-venous fistula.
We will discuss all these subjects in more detail.
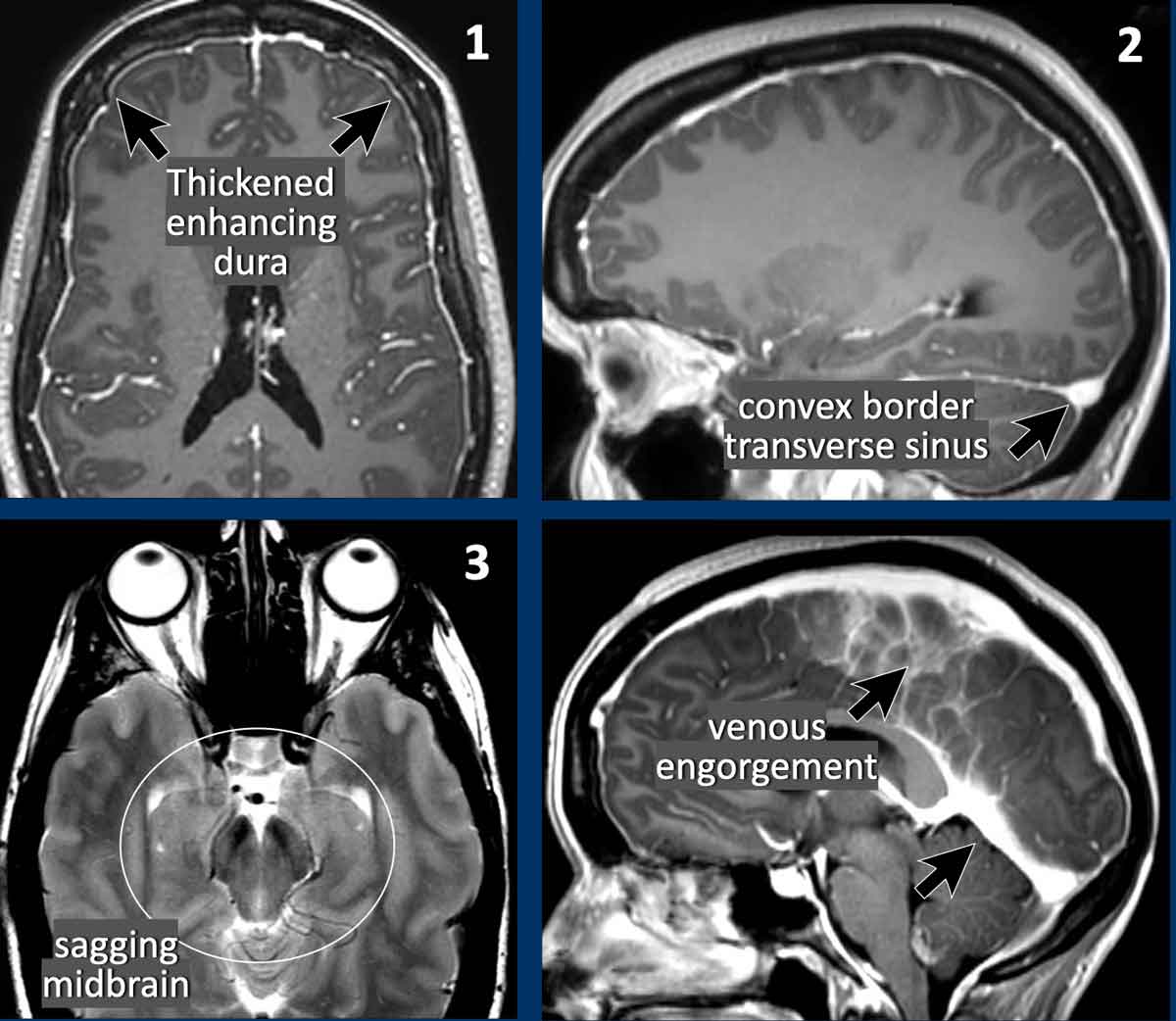
Imaging Findings in SIH
The most sensitive finding for the diagnosis of SIH in order of frequency is:
- Dural thickening with enhancement (83%).
- Convexity of the transverse sinus (75%).
- Brainstem sagging (61%).
As mentioned before there is a poor correlation between these imaging findings and the measurements of the CSF pressure.
On the other hand 10% of the patients with SIH have no imaging abnormalities and consequently a normal MRI does not excludes a SIH.
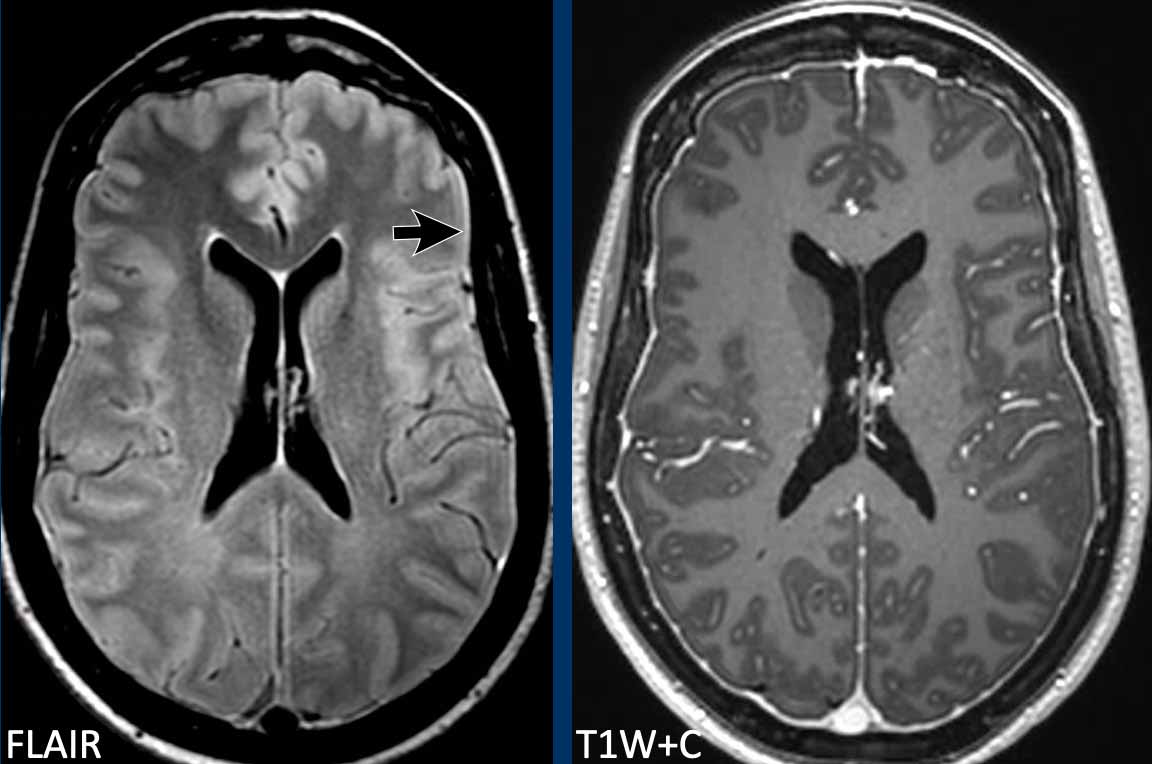
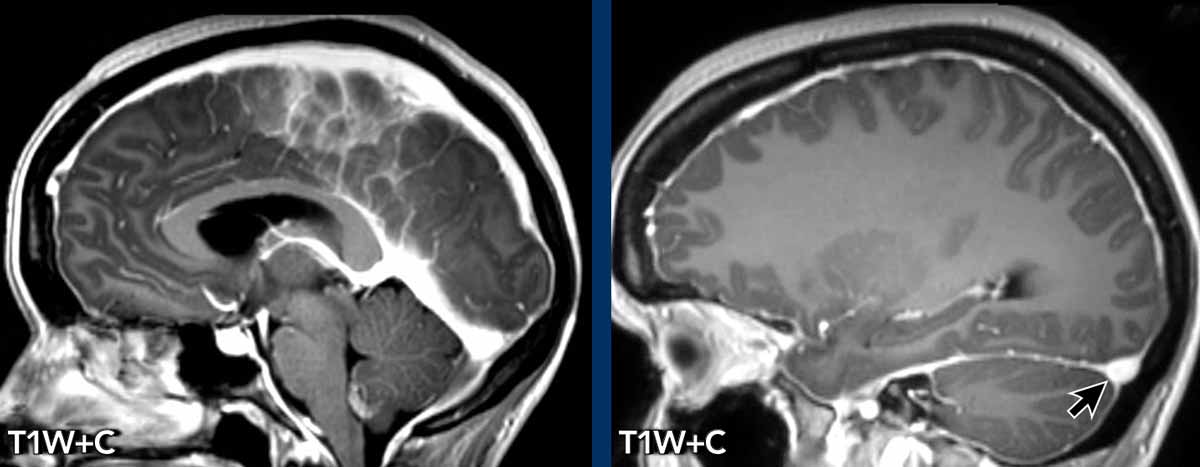
Dural thickening
Diffuse smooth dural thickening is sometimes visible on FLAIR images (arrow) but is more easily seen on post-contrast T1W-images.
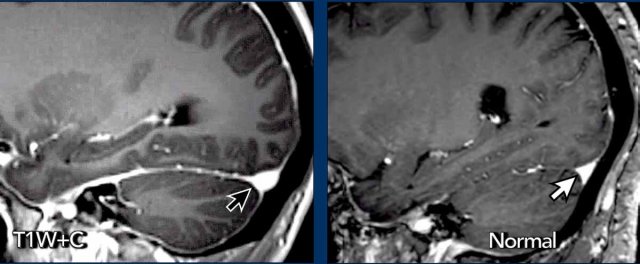
Convex border transverse sinus
In SIH the lower border of the transverse sinus can be convex (black arrow).
In normal conditions the transverse sinus usually has concave borders (white arrow).
The explanation for the venous engorgement and the concave borders of the transverse sinus is that the low volume of CSF in the cranial vault in patients with SIH is compensated by an increase in volume of the cerebral veins.
Obviously the brain and the arteries cannot compensate for the volume loss, while the total amount of tissue and fluid has to remain the same.
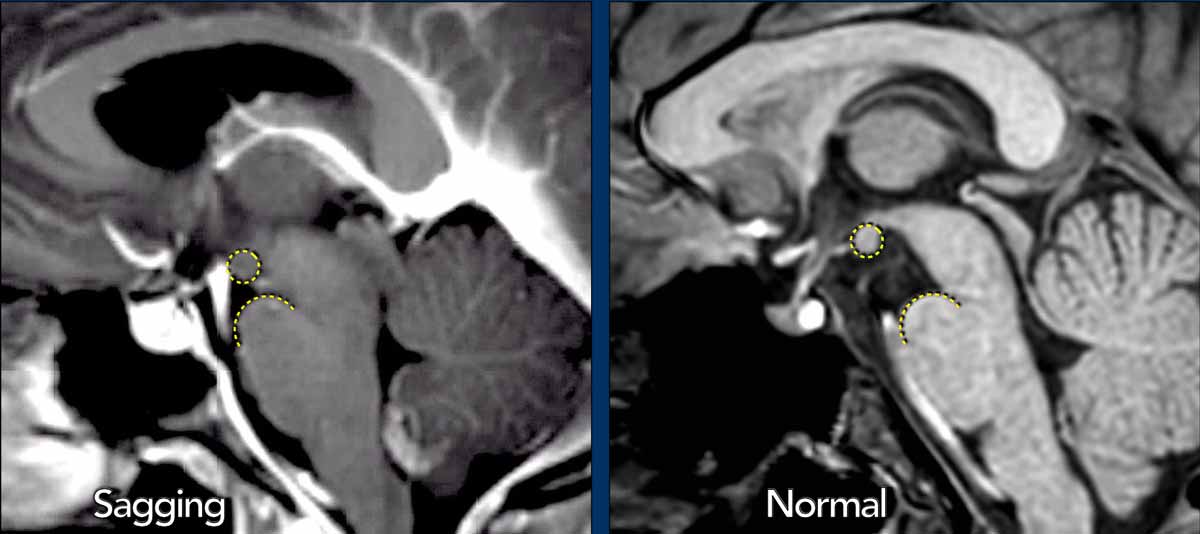
Midbrain sagging
In more severe cases of SIH, the brain is displaced downwards, leading to compression of the brainstem against the skull base.
This finding is referred as “brainstem slumping” or “midbrain sagging” and is considered specific for intracranial hypotension.
In normal conditions the mamillary bodies are cranially to the dorsum sellae and the distance to the pons is at least 5.5 mm.
In midbrain sagging the distance to the pons is less than 5.5 mm.
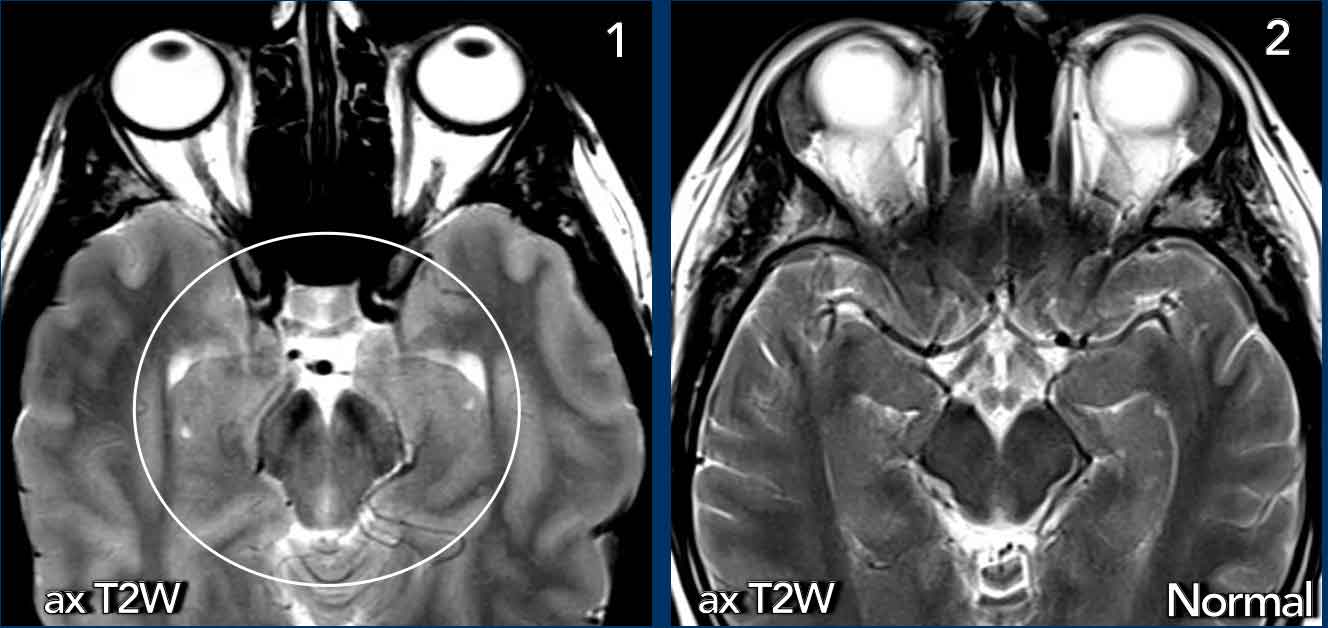
On axial images the downward displacement of the brain leads to compression of the midbrain.
Images
- Sagging with compression of the midbrain from either side (circle).
- Normal midbrain for comparison.
In this patient with SIH all the veins are dilated and the borders of the transverse sinus are convex.
Notice also the thickened enhancing dura.
Anterior dural tear
An anterior dural tear is often the result from a calcified ventral osteophyte leading to an extradural CSF collection.
The CSF collection can present as a spinal longitudinal epidural collection (SLEC) as seen on a MRI.
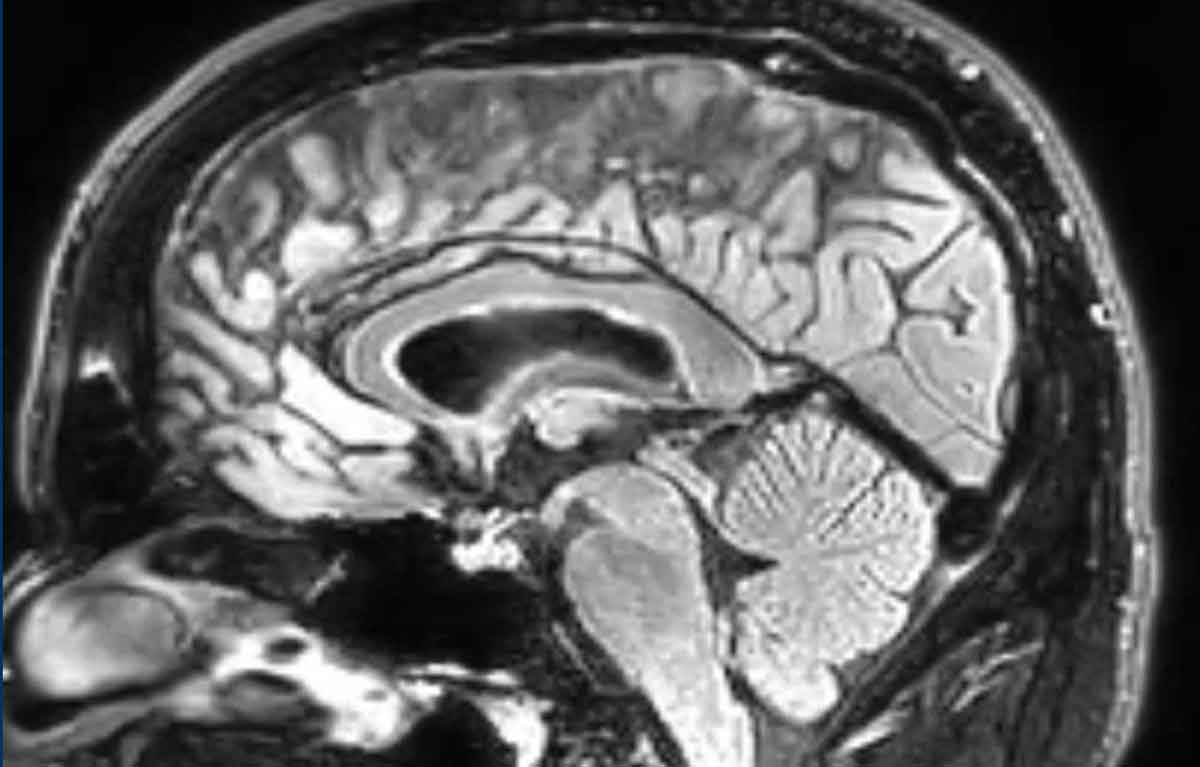
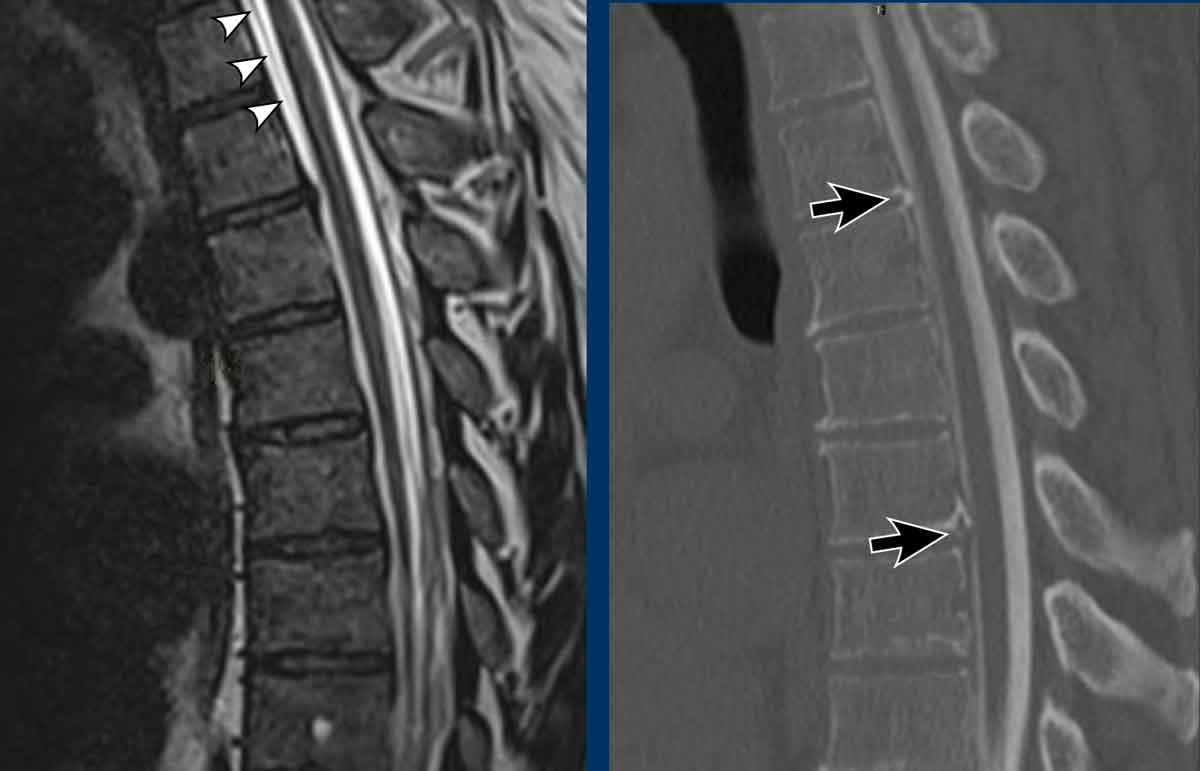
This image is of a patient with headaches.
The FLAIR image shows typical features of spontaneous intracranial hypotension:
- dilated veins and dural sinus
- mild midbrain sagging
- decreased mammillary pontine distance
Continue with the MRI and CT myelography...
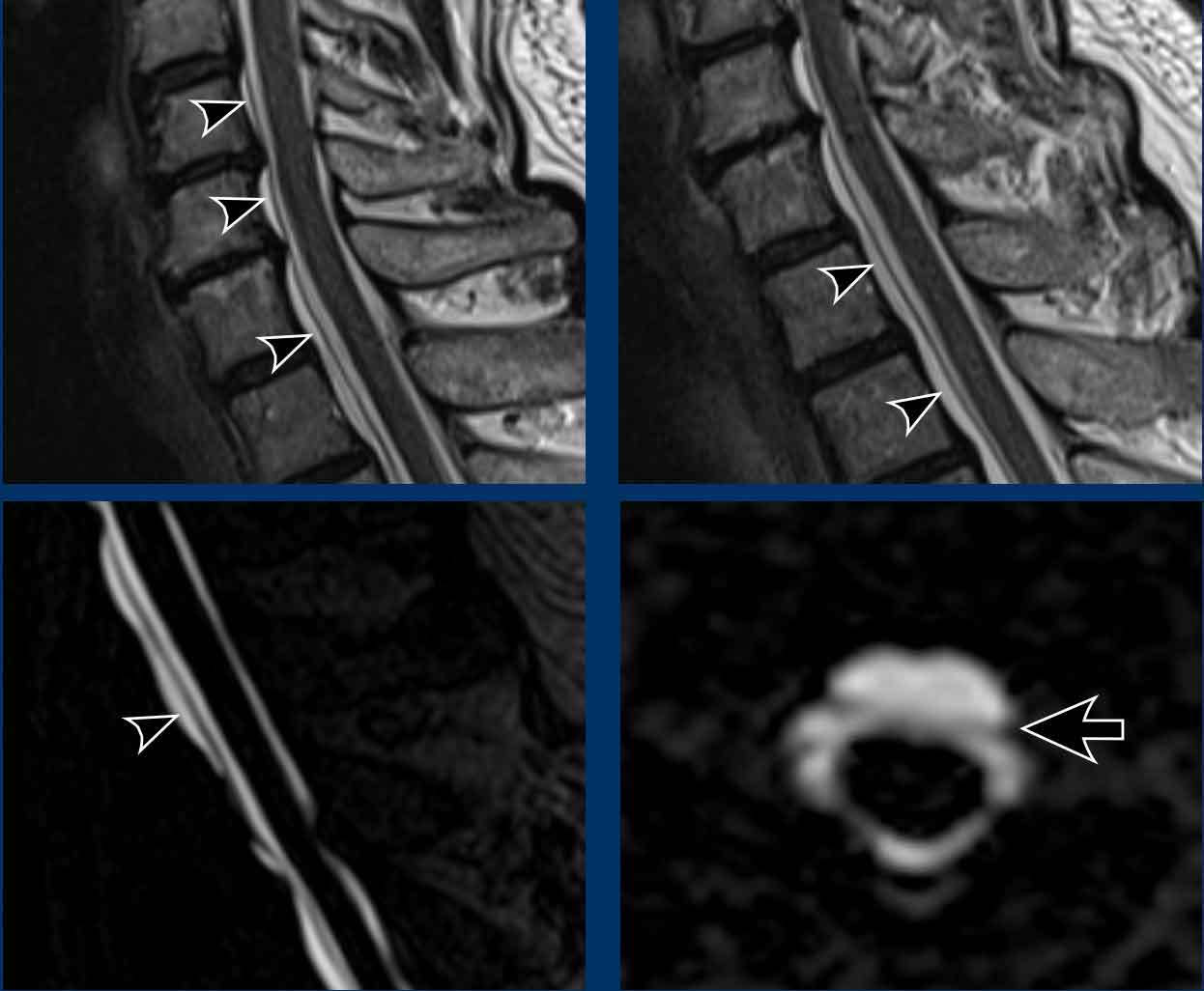
Images
- The sagittal T2W image of the spine shows a spinal longitudinal anterior collection (SLEC), which is located just anterior to the anterior dura (black linear structure indicated with arrowheads).
- Conventional CT myelography (acquired after dynamic myelography) shows two partially calcified hernias in the upper thoracic spine (arrows).
Continue with the axial reconstructions of the CT myelography...
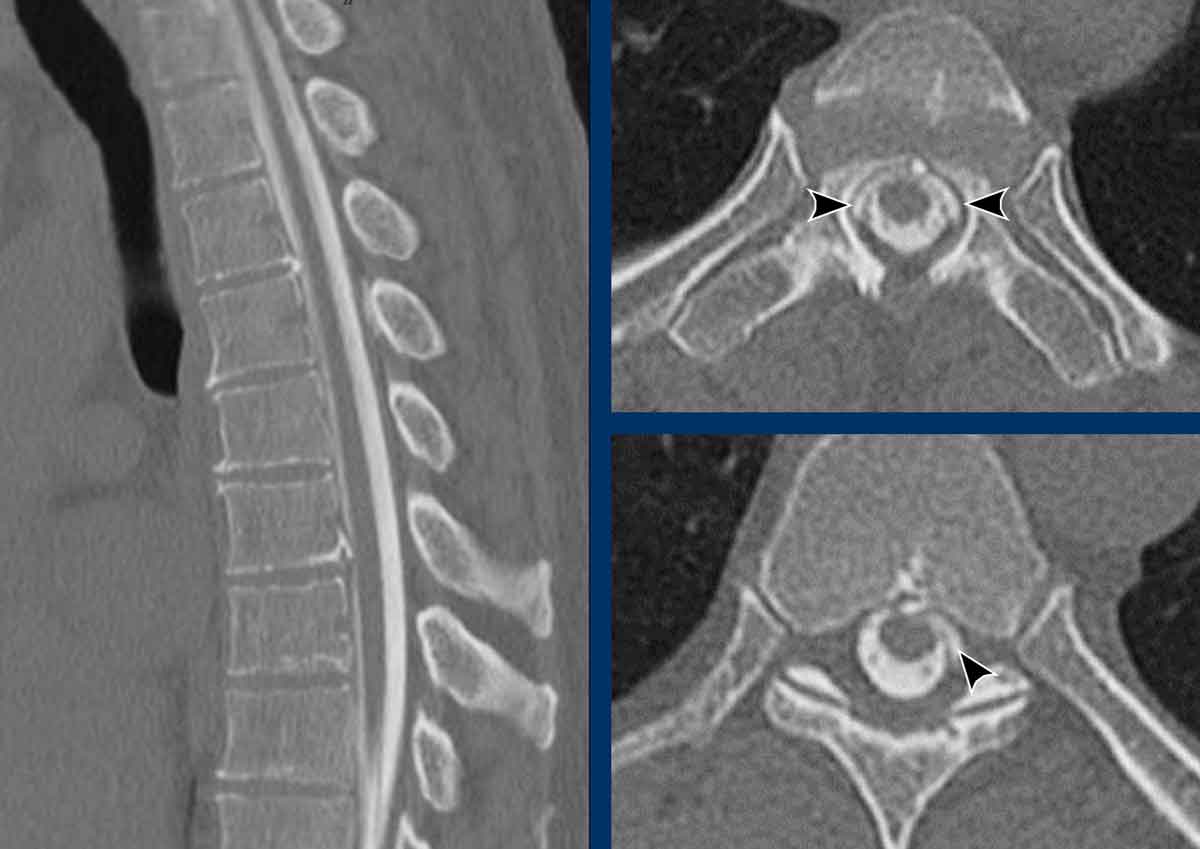
Images
On the conventional CT myelography there is leakage of iodine contrast to the anterior epidural space.
Notice that this is only visible on the axial reconstructions (arrowheads).
On the sagittal images you will miss this subtle finding.
Continue with the video of the dynamic myelography...
A dynamic myelography is the best technique for localizing subtle or high-flow spinal CSF leaks.
Because the leakage was suspected to be on the anterior side, the patient was examined in the prone position.
Video
In this case there is contrast leaking outside the thecal sac locating the level of the anterior dural tear (arrow).
Leaking diverticulum
Leaking nerve root diverticula will result in an extradural fluid collection.
Depending on the precise location of the diverticulum, these patients can present with or without a spinal longitudinal epidural collection (SLEC).
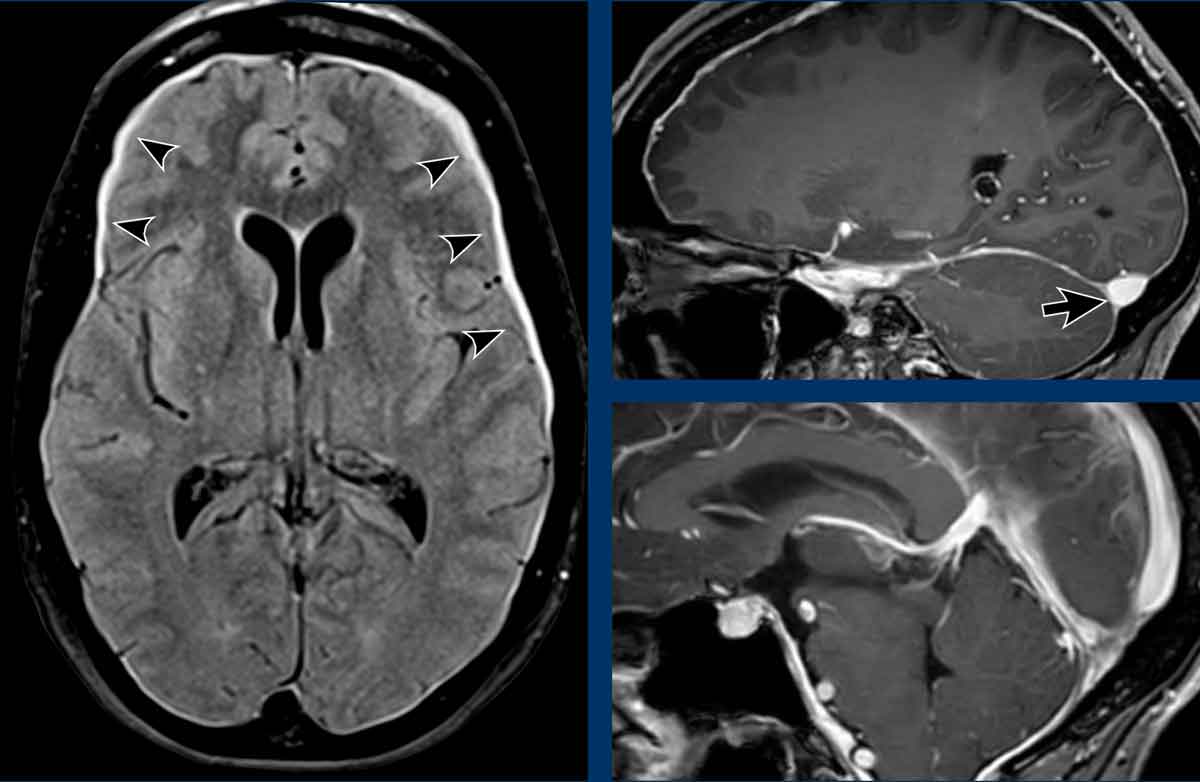
Post-contrast 3DT1 and axial FLAIR These images are of a patient with headaches and cognitive complaints with SIH.
First look at the images and then continue reading.
Images
- Bilateral subdural effusions on the axial FLAIR (arrowheads).
- Dilated veins and dural sinus with a convex lower border of the transverse sinus (black arrow).
- Midbrain sagging and a decreased mammilary – pontine interval.
Continue with the spinal imaging...
Images
Spinal imaging did not show a longitudinal epidural collection.
However at the level of L1 slight asymmetry was noted (arrow).
This was suspect for a small lateral epidural fluid collection on the right side.
Continue with the dynamic spinal myelography..
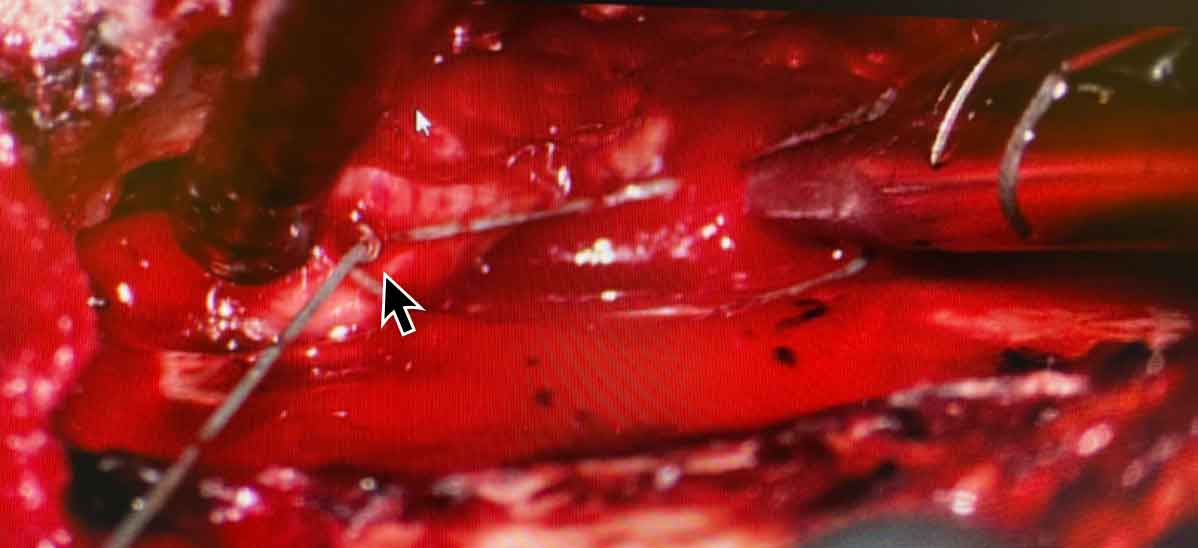
On the dynamic spinal myelography there is leakage of contrast on the right side from a lateral diverticulum.
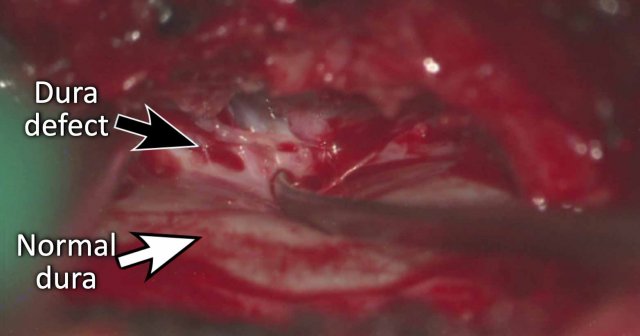
Continue with the image during surgery...
During spinal surgery a small defect was noted (black arrow).
The normal dura is indicated with the white arrow.
The defect was closed.
After closure of the defect the patient experienced no more headaches.
However it took a long time to regain a normal cognitive function.
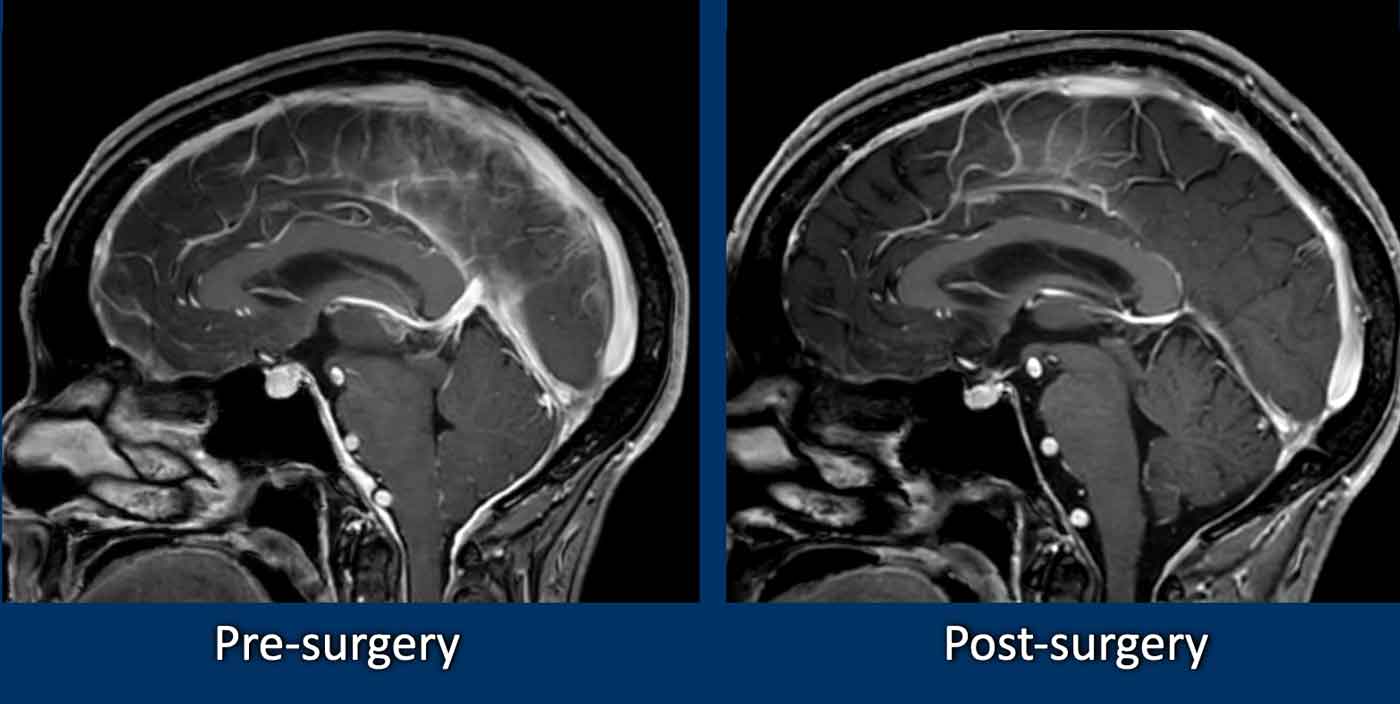
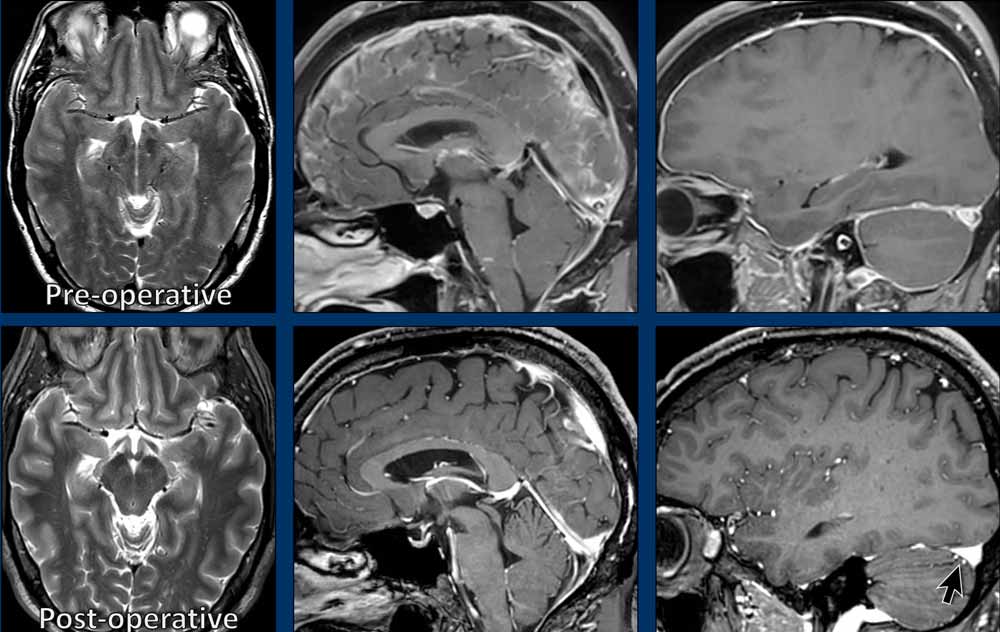
Continue with the post-surgery MRI...
On the post-surgery MRI there is almost complete normalization.
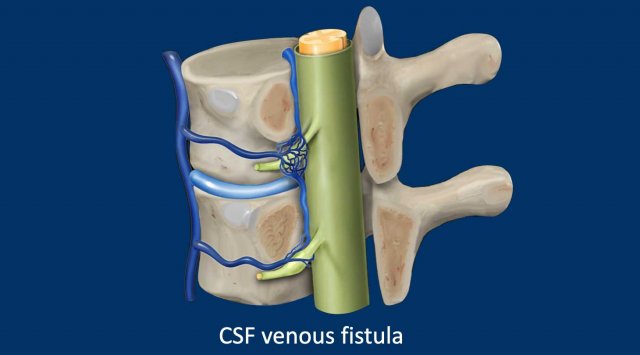
CSF venous fistula
These are direct CSF-venous fistulae without an extradural fluid collection, i.e. SLEC negative.
These fistulae tend to be found in the lower thoracic spine, usually originating from nerve root sleeve diverticula.
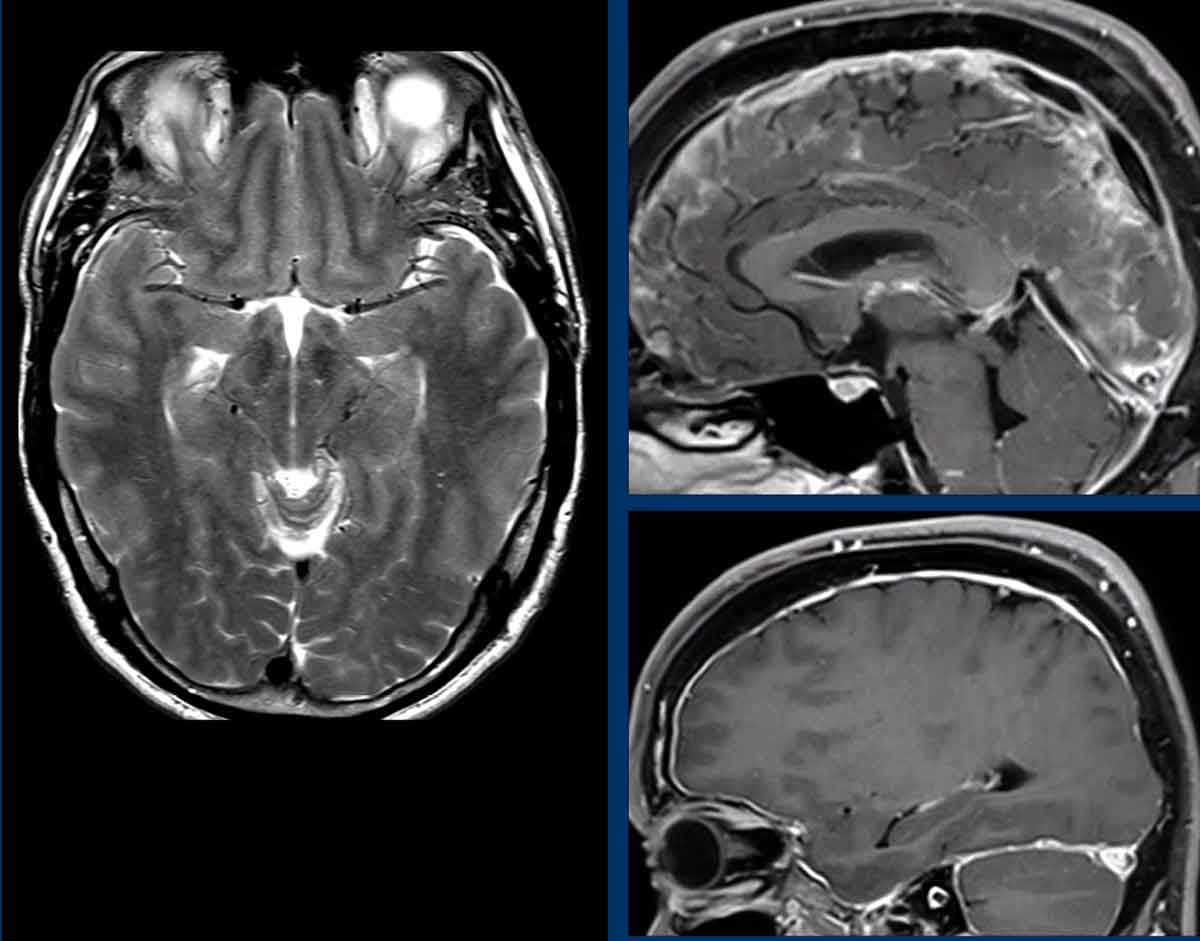
These images are of a 49-year-old male, who complained of headaches during coughing and when he bended down.
Study the images.
What are the findings?
Then continue reading.
Findings
- Midbrain sagging on the axial T2W.
- Venous engorgement with a convex lower border of the transverse sinus.
- Thickened enhancing dura.
- Decreased mammillary-pontine distance.
Conclusion
Spontaneous intracranial hypotension.
Continue with the next images...
The patient was treated with blood patches, but this only had a temporary effect.
Subsequently a total spine MRI was made, which showed a few meningeal diverticula, but no epidural fluid collections.
Continue....
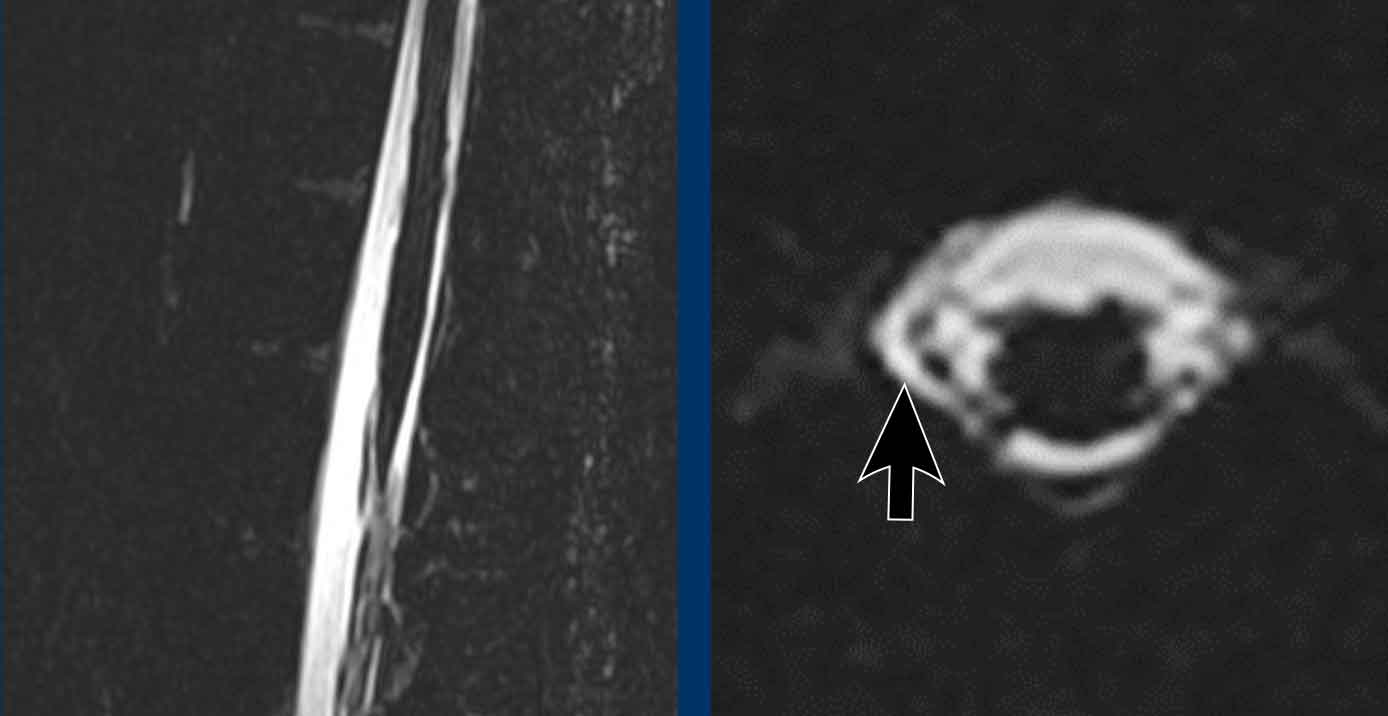
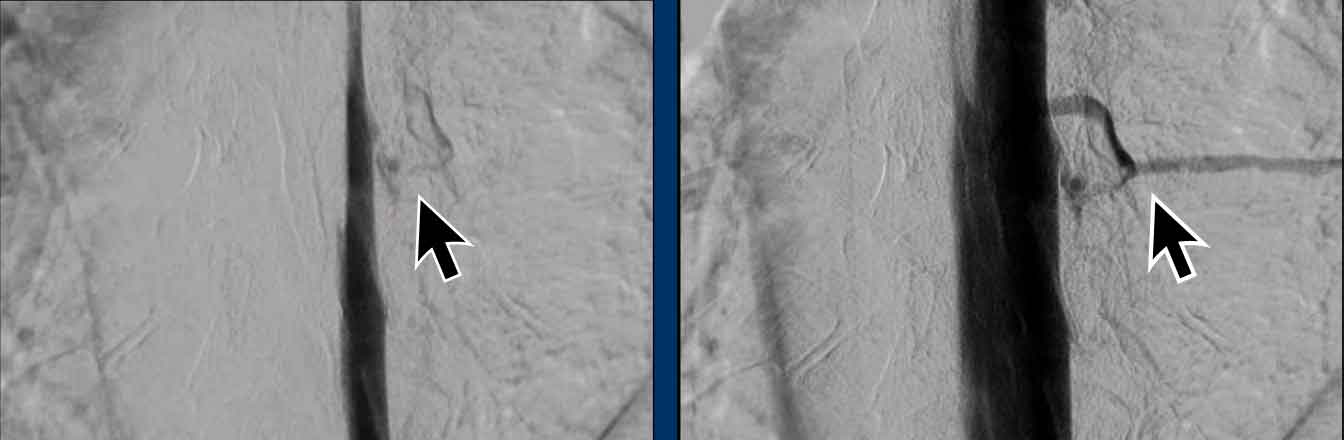
Finally a digital subtraction myelography was performed (Courtesy René van den Berg).
First a lumbar puncture is performed.
Then the patient is positioned on one side and images are made with a horizontal beam while the contrast is injected and flows in a cranial direction (see video).
When the patient was lying on his left side no abnormalities were seen.
This video was taken with the patient lying on his right side.
Question
Do you see any CSF leakage?
Continue with the next images...
At a low thoracic level there is leakage of contrast via a CSF venous fistula.
During the operation prominent venous convolutes were coagulated and the root Th8 was ligated.
Compare the pre-operative images with the post-operative ones.
Notice the normalization of the imaging findings.
Most importantly, the headaches were gone.
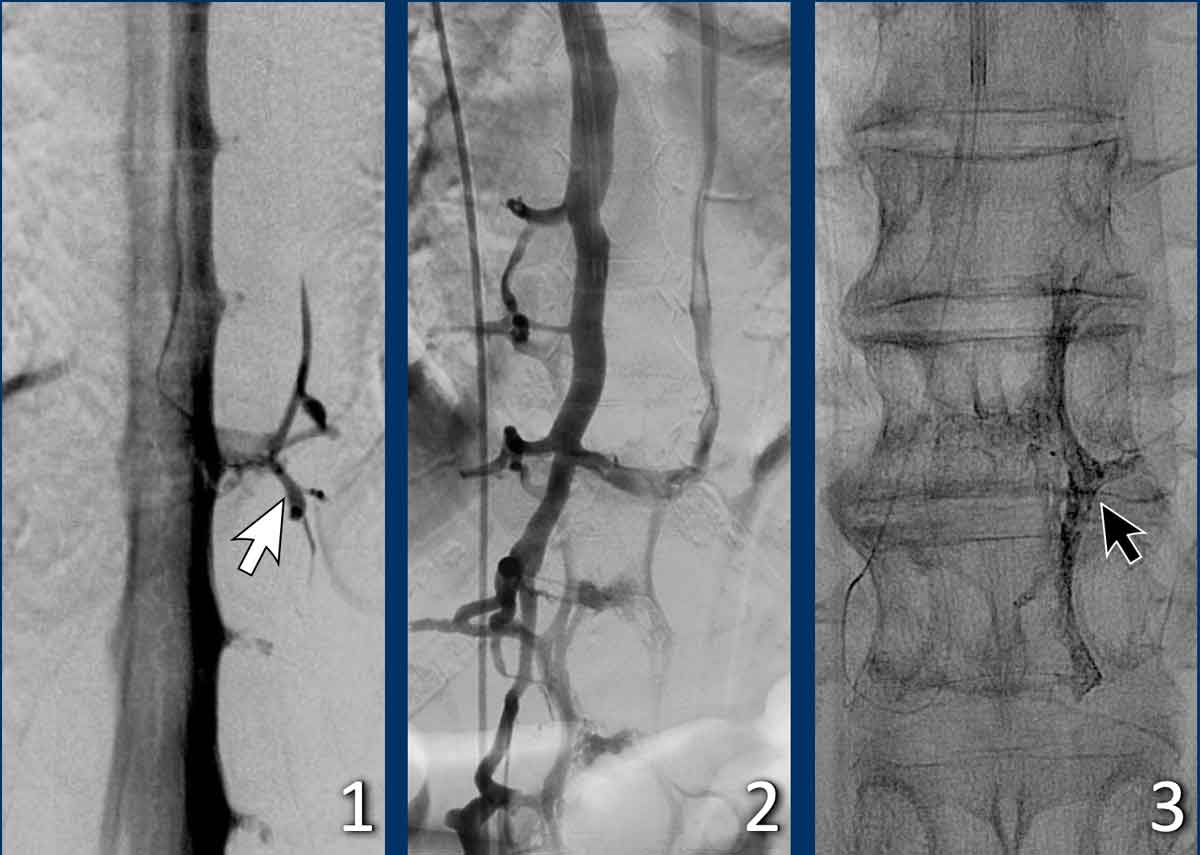 Treatment of a CSF-venous fistula through a venous route. Courtesy René van den Berg and Olvert Berkhemer
Treatment of a CSF-venous fistula through a venous route. Courtesy René van den Berg and Olvert Berkhemer
These images are of a patient with spontaneous intracranial hypotension, who has a CSF-venous fistula which was treated through a venous route.
Images
- CSF-venous fistula (arrow).
- Treatment by an endovascular approach and embolization through a venous route.
- The cast of embolization material is visible on the right non-subtracted image.
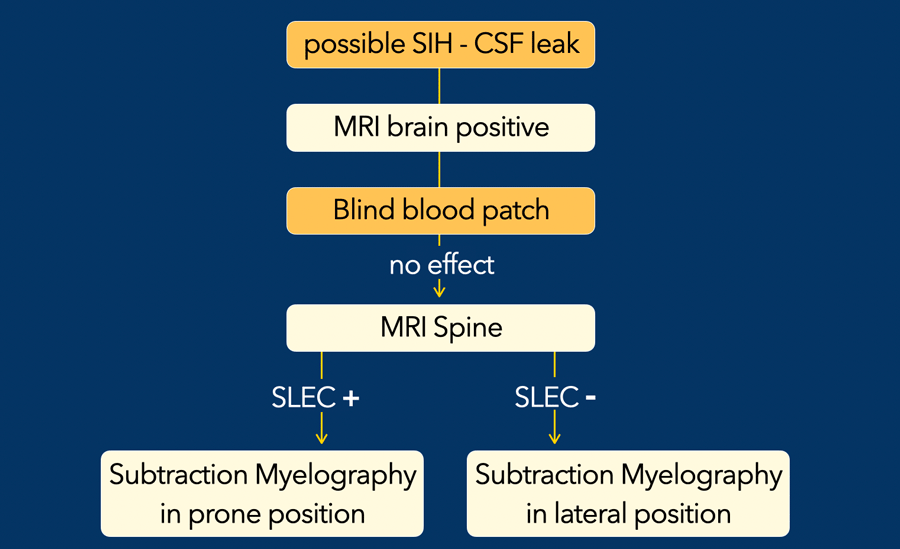
Roadmap for possible CSF leak
In patients who are suspected of having SIH, the first step is to do a MRI brain to look for typical imaging findings of SIH.
If the brain MRI is positive, the treatment starts with a "blind" epidural blood patch in order to seal off the CSF leak.
If this is not successful a MRI of the whole spine is performed to look for a dural tear, meningeal diverticulum or CSF venous fistula.
Some of these patients may have a spinal longitudinal epidural collection (SLEC) on the MRI as a result of a CSF leak due to an anterior dural tear.
Depending on the precise
location a patient with a lateral diverticulum can present with or without
SLEC.
Patients with a CSF-venous fistula usually are SLEC negative.
SLEC positive patients are best positioned prone for digital subtraction myelography and may warrant additional attempts with a directed epidural blood patch.
SLEC negative patients are best evaluated in the decubitus positions because they more frequently have a lateral leaking diverticulum or a CSF-venous fistula.
Patients with a CSF-venous fistula may forgo further epidural blood patch treatment and proceed with surgical repair. (3).
Images
Notice the longitudinal spinal fluid collections (arrowheads).
This is called SLEC-positive.
MR protocol
Often sagittal T1, T2 and CISS/FIESTA with axial reconstructions will be sufficient to diagnose a SLEC.
Sometimes additional sagittal STIR and cine flow images may be beneficial.
SIH and Pseudo-SAB
Sometimes the differential diagnosis between SIH and a subarachnoid hemorrhage can be challiging.
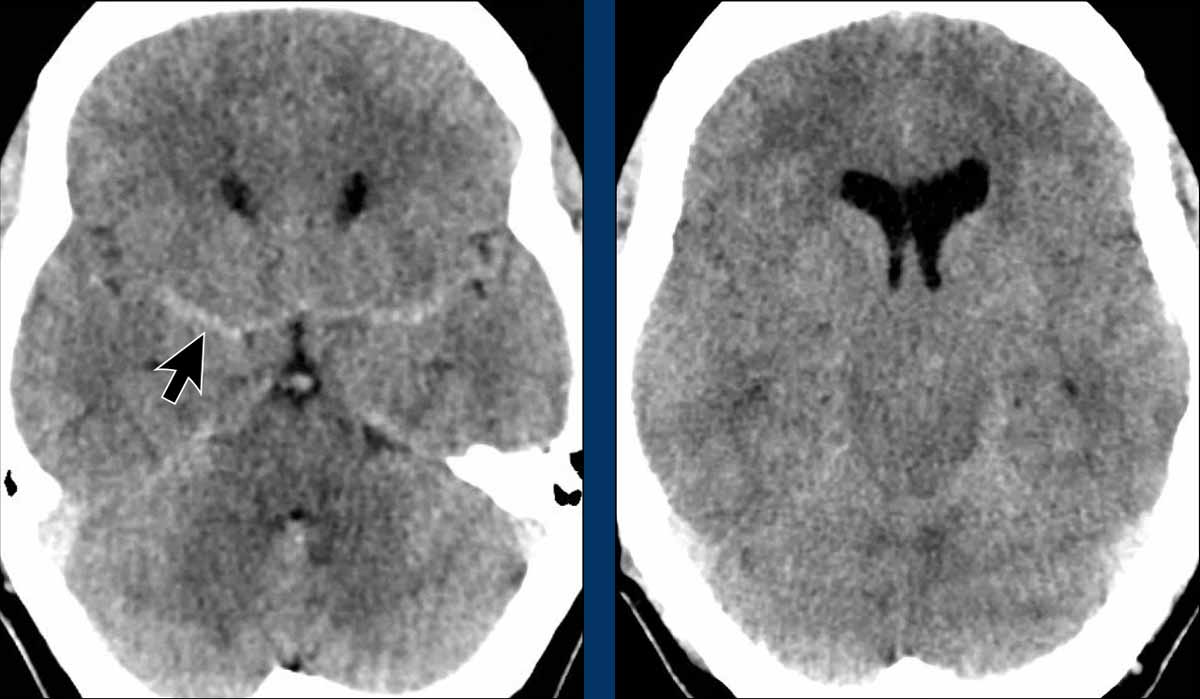
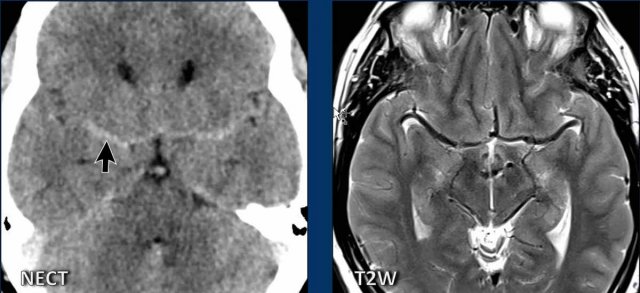
These images are of a 57-year-old male , who presented with headaches and vomiting.
He was alert and there were no abnormalities at neurologic examination.
First look at the images.
What is your opinion?
Images
The symmetrical density in the subarachnoid space was first regarded as sign of a subarachnoid hemorrhage, which seems a reasonable idea.
There is obliteration of the basal cisterns indicative of a descending transtentorial herniation.
CTA was performed, but did not show any aneurysm.
The following options were considered:
- Lumbar puncture to prove that it really was a SAB.
- DSA to look for an aneurysm, DSA being more sensitive than a CTA.
- MRI brain to get more information
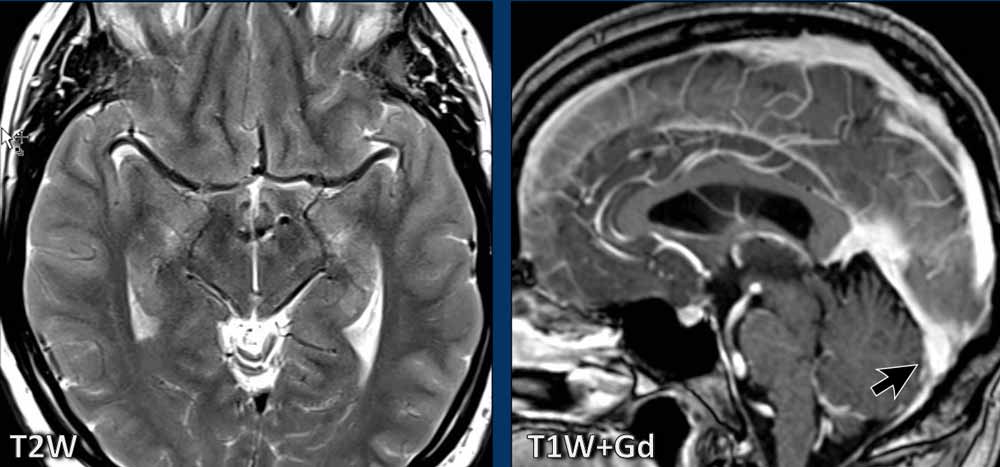
Continue with the MRI...
First look at the images.
What is your opinion?
Images
On the MRI it becomes clear, that the bilateral dense structures, that were seen on the CT, are the middle cerebral arteries.
On a CT due to the lack of
surrounding CSF they appear more dense than usual.
The MRI also shows midbrain sagging, seen on the axial image as as an abnormal shape and on the sagittal image as a short distance between the mamillary bodies and the pons.
There is a convex undersurface of the transverse sinus.
We can conclude that this is a case of SIH.
Pseudo-SAB differential diagnosis
The differential diagnosis of this pseudo-SAB sign on a NECT is:
- Intracranial hypotension (SIH).
- Purulent meningitis - a bacterial infection of the subarachnoid space.
- Polycythemia - due to the high density of the middle cerebral artery.
- Diffuse cerebral edema - due to the relative hyperdensity of the cerebral arteries compared to the hypodensity of the edematous cerebrum.
SIH and Chiari type I
Although SIH and Chiari malformation type I (CM1) are very different conditions, they both can present with chronic headaches and low-lying cerebellar tonsils.
In patients with SIH this can lead to a misdiagnosis of a CM1.
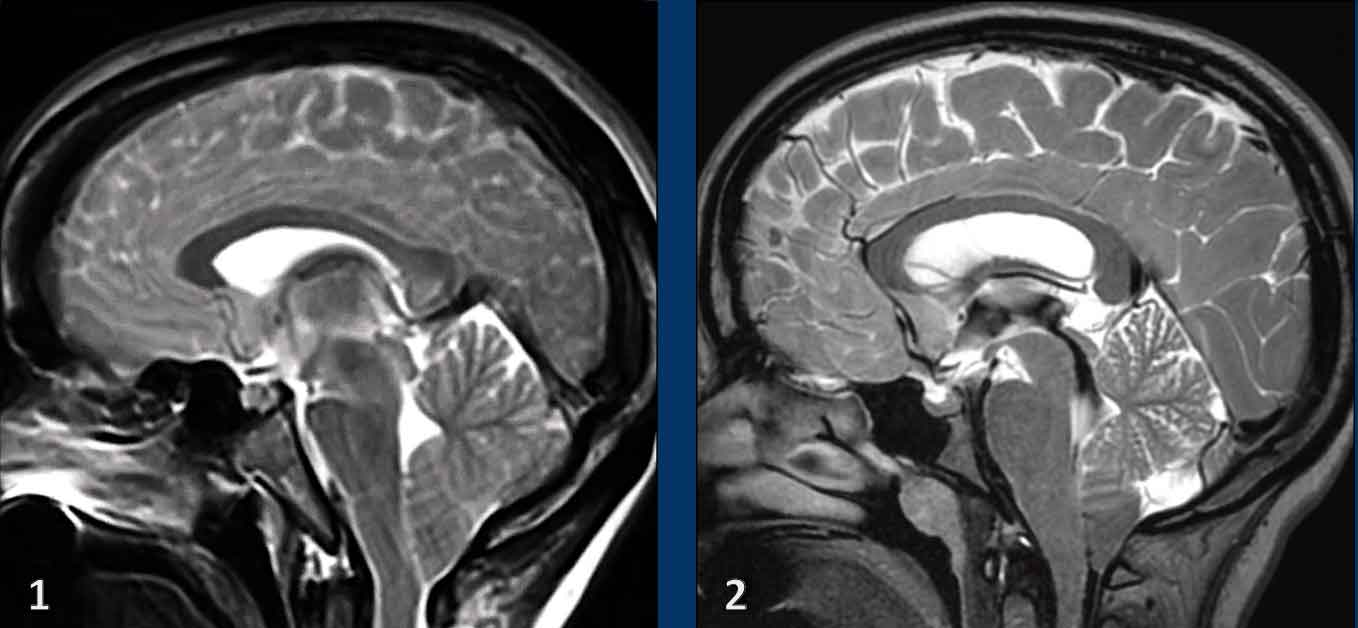
First study the images.
Both patients are young women with chronic headaches.
Which one has SIH and which one has CM1?
Images
- Low-lying cerebellar tonsils
It is not very obvious also due to some movement artefacts, but the shape of the brainstem is not normal and there seems to be a short distance between the pons and the mamillary bodies.
Maybe there is also some venous congestion. - Besides low-lying cerebellar tonsils, the image looks normal.
Continue with additional images ......
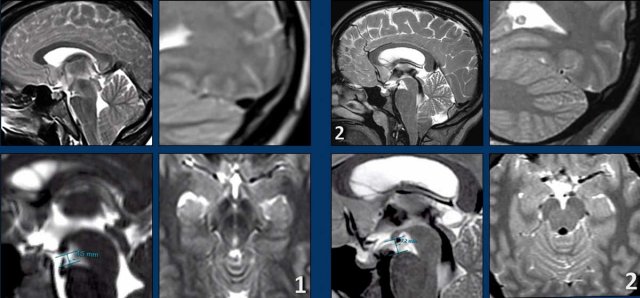
Images
- The four images on the left show the typical findings of SIH with a convex border of the transverse sinus, a short distance between the mamillary bodies and the pons and midbrain sagging.
- The images on the right do not show these findings.
The patient with SIH was treated four times with a blind blood patch, which was succesful.
The patient with the Chiari type 1 had a craniocervical decompression with a good result.
It is our duty as radiologist to save patients with SIH from being treated as Chiari 1 patients.