Horner syndrome
Reina Sol-Kloet¹ and Sjoert Pegge²
¹University Medical Center Groningen and ²Radboud University Medical Center
Publicationdate
Horner
syndrome is a rare clinical condition presenting with partial ptosis,
miosis and facial anhidrosis described in 1869 by Johann Friedrich Horner.
The
clinical symptoms allow the anatomic location of the underlying pathology
somewhere in the oculosympathetic pathway.
Imaging plays an important role
in the final diagnosis.
Anatomy
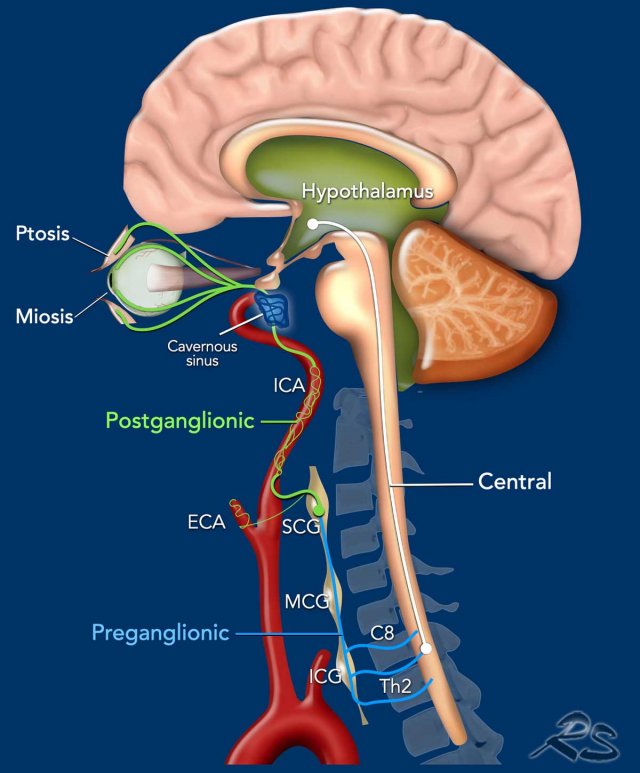
Horner syndrome is the result of an interruption of the oculosympathetic nerve system which starts in the posterolateral part of the hypothalamus and goes all the way through the brainstem and the spinal cord (level C8-Th2), cervicothoracic sympathetic ganglia and along the internal carotid artery (and some fibers along the external carotid artery, maxillary artery) and cavernous sinus to the eye.
Horner
syndrome can be anatomically classified into three types depending on where the
oculosympathetic pathway is interrupted:
- Central (first
order neuron) - in white
Involves the first order neuron that starts in the hypothalamus, runs through the reticular formation in the brainstem and descends to the cervicothoracic level, where the first synapse is located anteromedial in the gray matter of the myelum. - Preganglionic (second
order neuron) - in blue
Involves the second order neurons that pass from the myelum with the ventral rami of C8-Th2 to the inferior (ICG) and middle cervical ganglion (MCG) in the cervicothoracic region to end in the superior cervical ganglion (SCG) in the neck located at the level of the second and third cervical vertebrae. - Postganglionic (third
order neuron) - in green
Involves the third order neuron that ascends along the internal carotid artery to the skull base to enter the cavernous sinus, where it joins the ophthalmic division of the trigeminal nerve to enter the orbit through the superior orbital fissure.
A small portion of the neurons ascend with the external carotid and maxillary artery to the facial sweat glands.
Clinically it can be difficult to
differentiate a central Horner from a pre- or postganglionic Horner.
Pharmacological testing of the eyes
with Apraclonidine or Cocaine can help make the diagnosis.
This means that in patients with a
unilateral Horner all these levels need to be examined unless other symptoms
point to a specific anatomical area.
Only in patients with a bilateral
Horner we can assume, that the pathology is located in the central neuron.
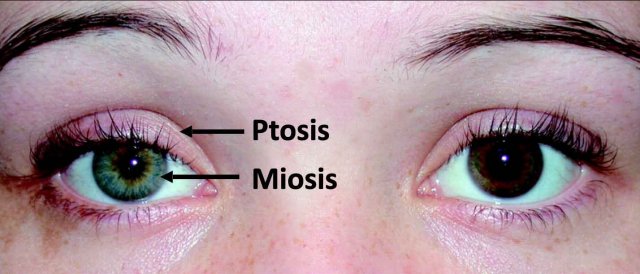
Horner syndrome classically presents with:
- Partial ptosis - drooping of upper eyelid
- Miosis - constricted pupil
- Facial anhidrosis - loss of sweating
Interruption of oculosympathetic pathways leads to inactivation of the superior tarsal muscle resulting in ptosis and inactivation of the dilator muscle producing a miosis.
The ptosis of Horner syndrome may be subtle, often 2 mm or less and has to be distinguished from the severe ptosis in oculomotor (CN III) palsy which supplies the levator palpebrae superior and is accompanied by a dilated pupil due to a loss of innervation to the sphincter pupillae.
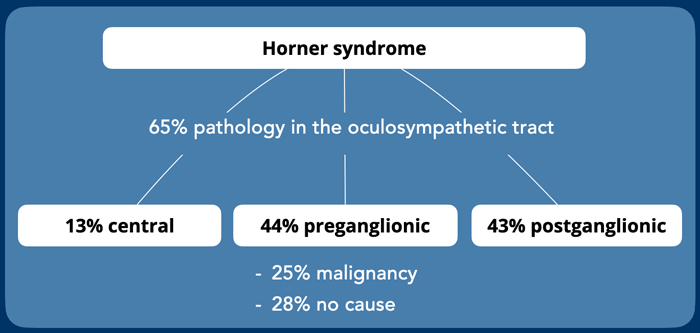
Pre- and postganglionic causes of Horner syndrome are as common.
Central Horner syndrome is uncommon.
Clinically frequently the central Horner syndrome goes unnoticed, because the other symptoms of brain pathology dominate the clinical picture.
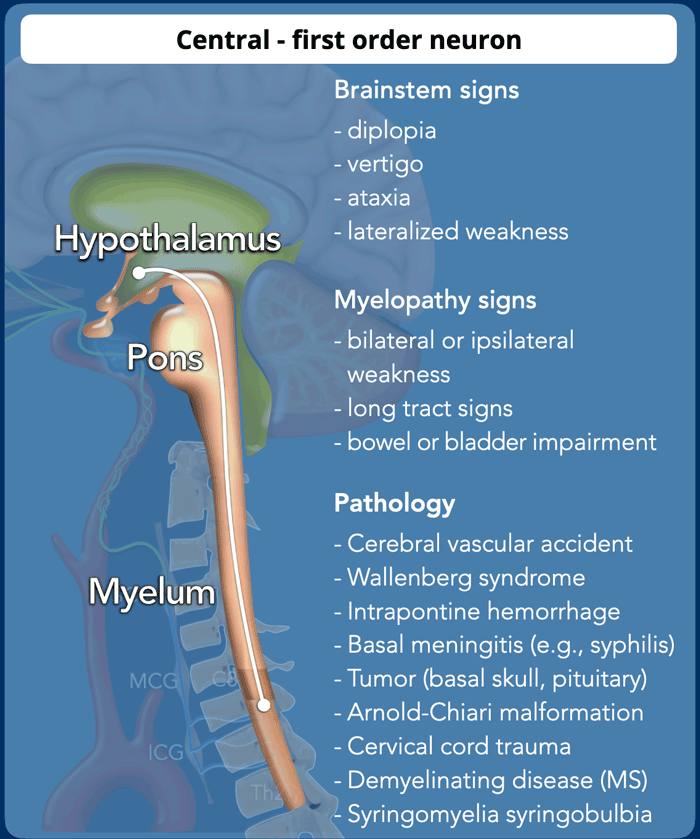
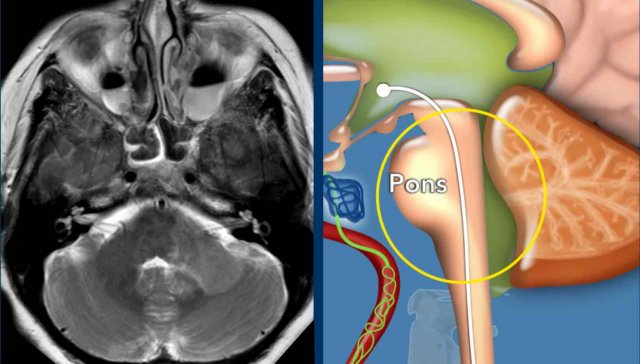
Central - 1st order neuron
The most common cause of a central Horner is infarction of the posterior-inferior cerebellar artery or
of the distal vertebral artery territory and is part of the
lateral medullary syndrome.
Other causes of a central Horner are demyelination, infection or inflammation (rhombencephalitis), hemorrhage and spinal cord lesions (table).
Brainstem signs suggest a brainstem
localization and indicates MRI of the brain.
Myelopathic features suggests
involvement of the cervicothoracic cord and indicates MRI of the cervical spine
and/or brachial plexus.
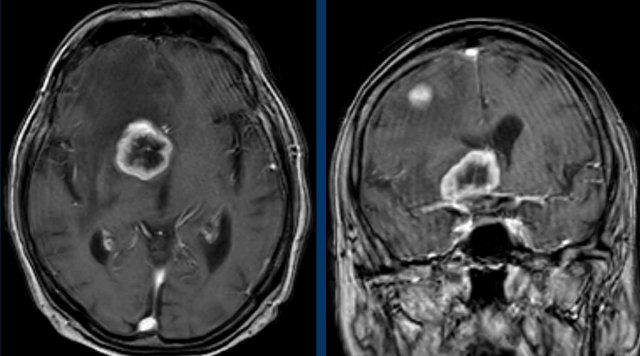
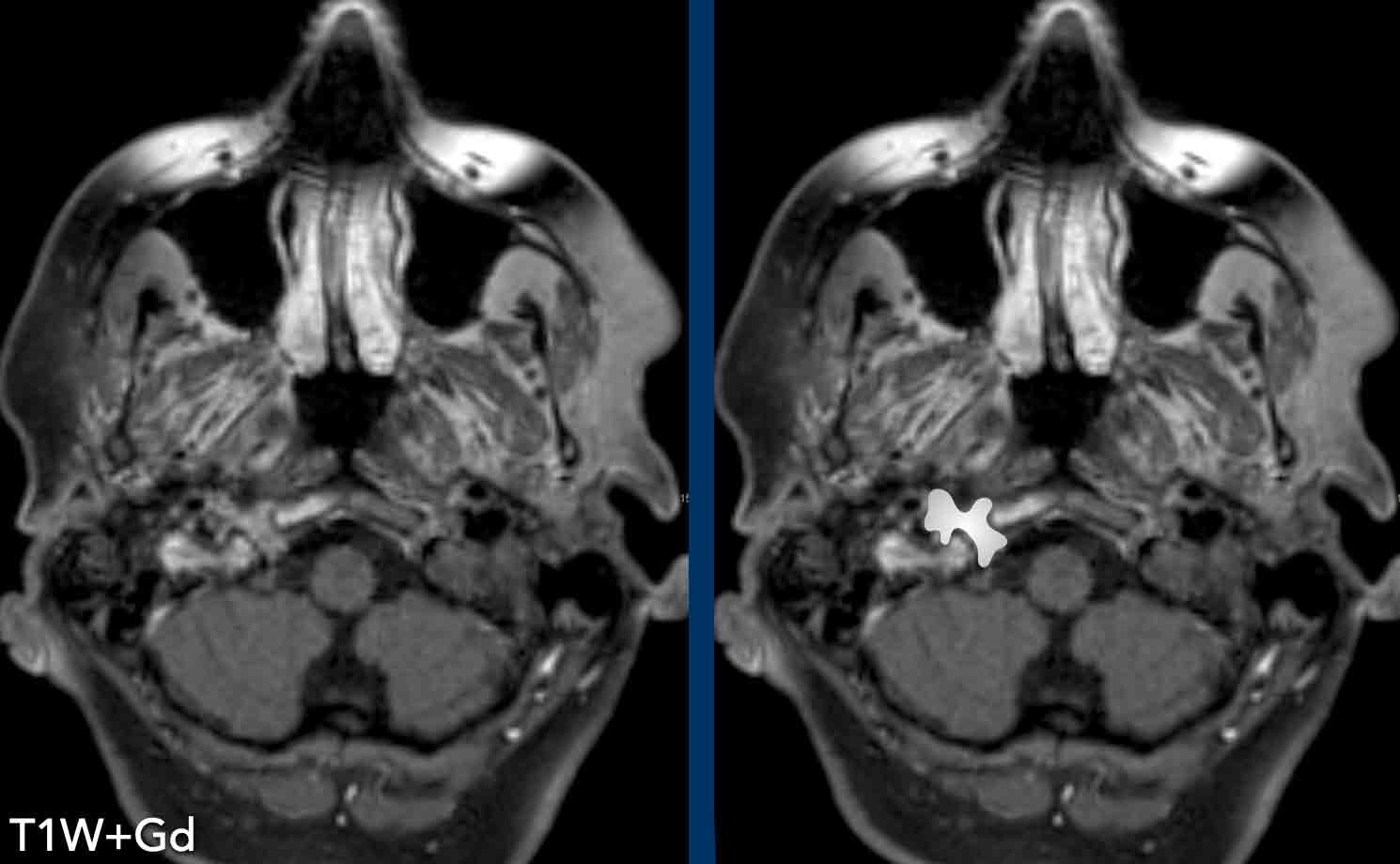
Hypothalamus
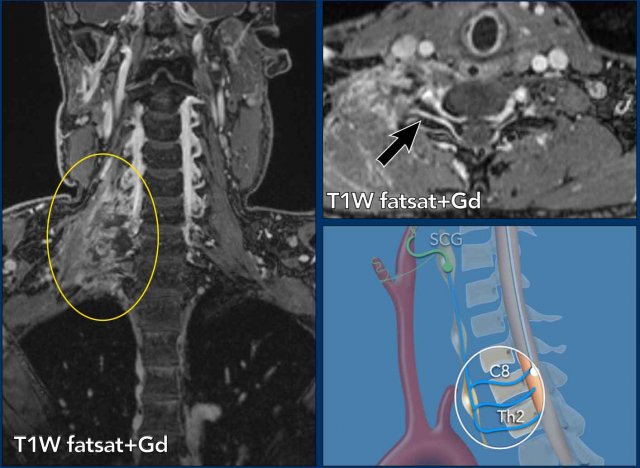
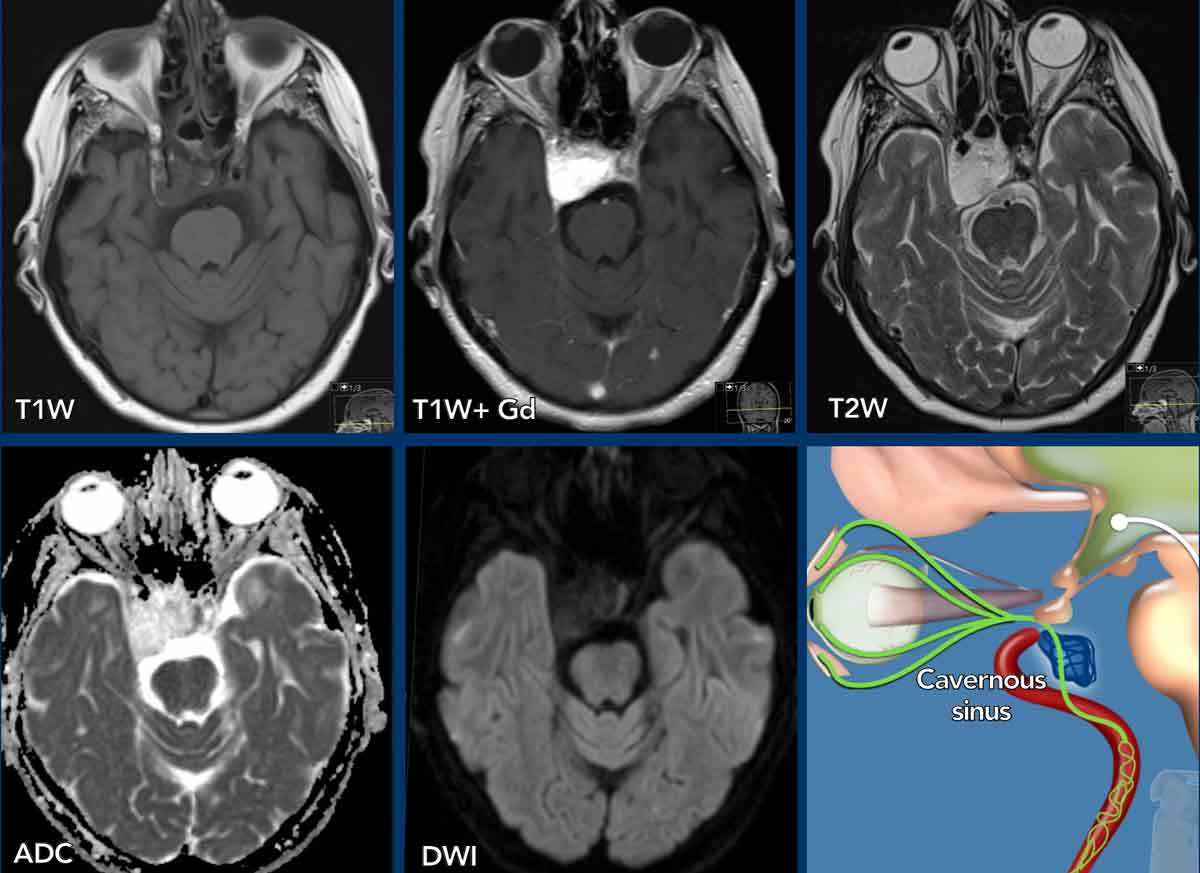
These images are of a 78-year old man
who is known to have a squamous cell carcinoma of the floor of the mouth and complains of double vision.
At physical examination he is desorientated and has
dysarthria and a Horner.
Based on these findings we assume that the Horner is
caused by a central problem.
Images
3D-T1 MPRAGE shows a large ring enhancing lesion at the level
of the hypothalamus on the right and a second lesion in the right
hemisphere.
Conclusion
Metastases of a squamous cell carcinoma.
Usually these carcinomas do not metastasize that easily.
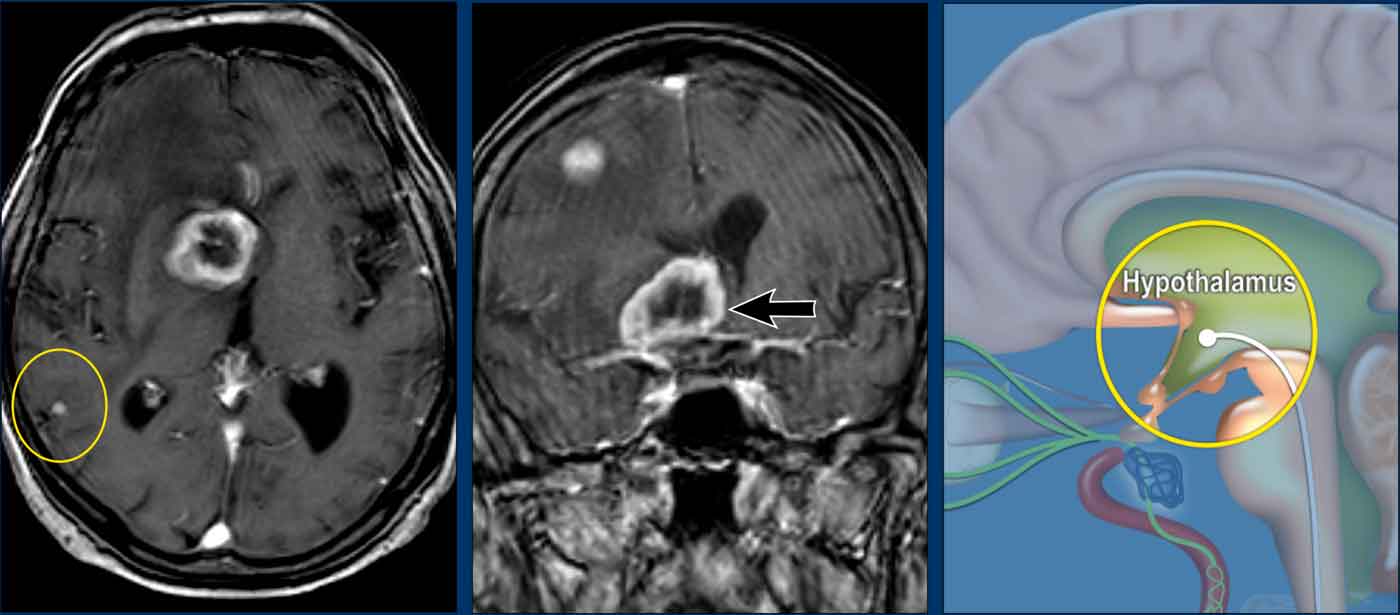
Continue with the next images...
At other levels there were more metastases (circle).
The illustration shows the level of the pathology.
Brainstem
These images are of a 58 year-old women with vague
neurological complains for years for which she was treated by a rehabilitation phycisian.
Images
Axial 3D-FLAIR with fat suppression shows
multiple T2 hyperintens lesions infratentorial in the medulla oblongata on the left and
bilateral cerebellar hemisphere).
Coronal 3D-FLAIR with fat suppression shows confluent white matter lesions periventricular and infratentorial.
Continue with the next images...
Images
MRI of the cervical and thoracic spine show multiple intramedullary
lesions.
Sagittal 3D-FLAIR shows multiple confluent Dawsons fingers and the axial 3D-FLAIR shows multiple T2 lesions in de brainstem.
Conclusion
Radiological consistent with Multiple Sclerosis.
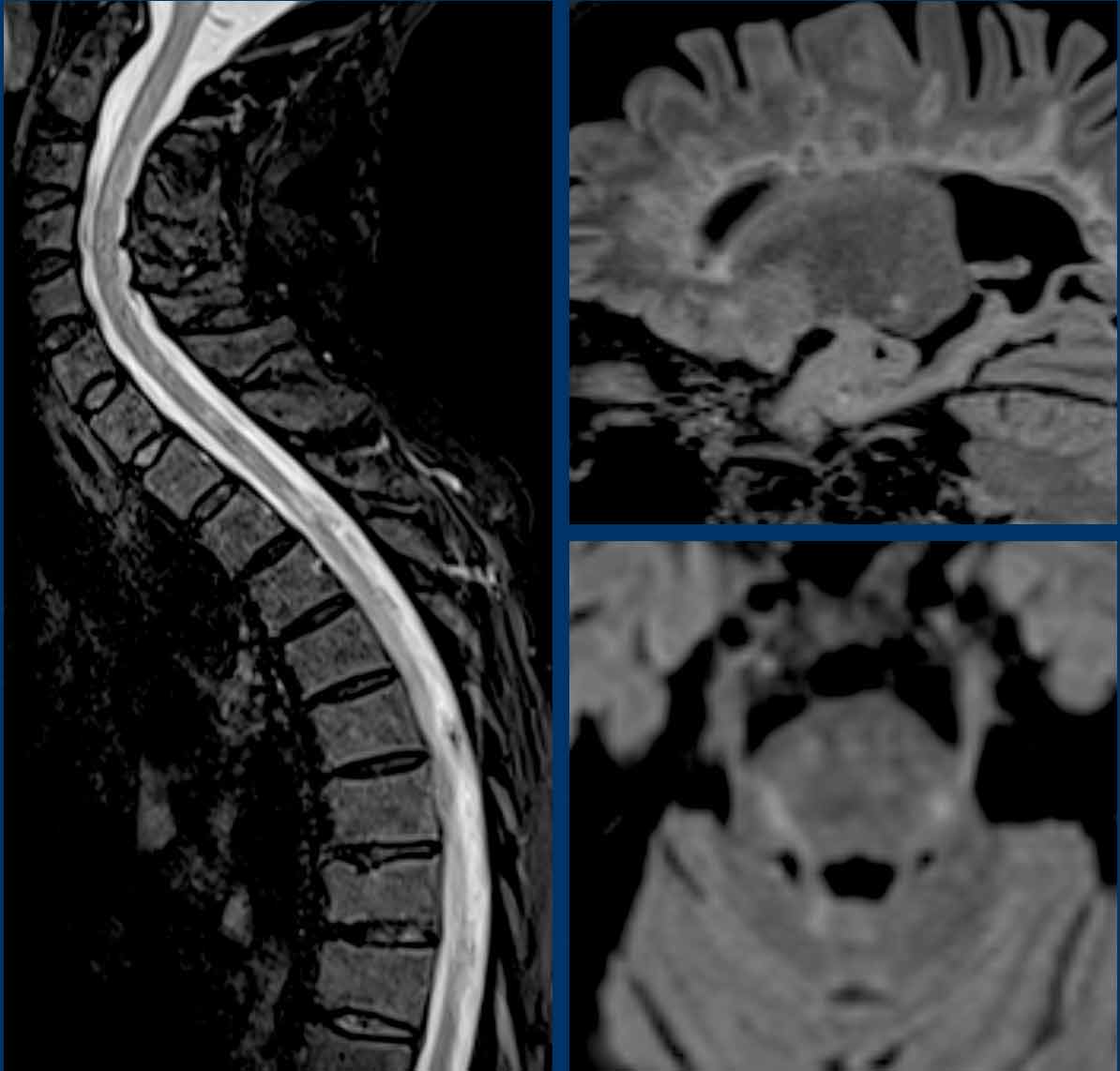
Spinal cord
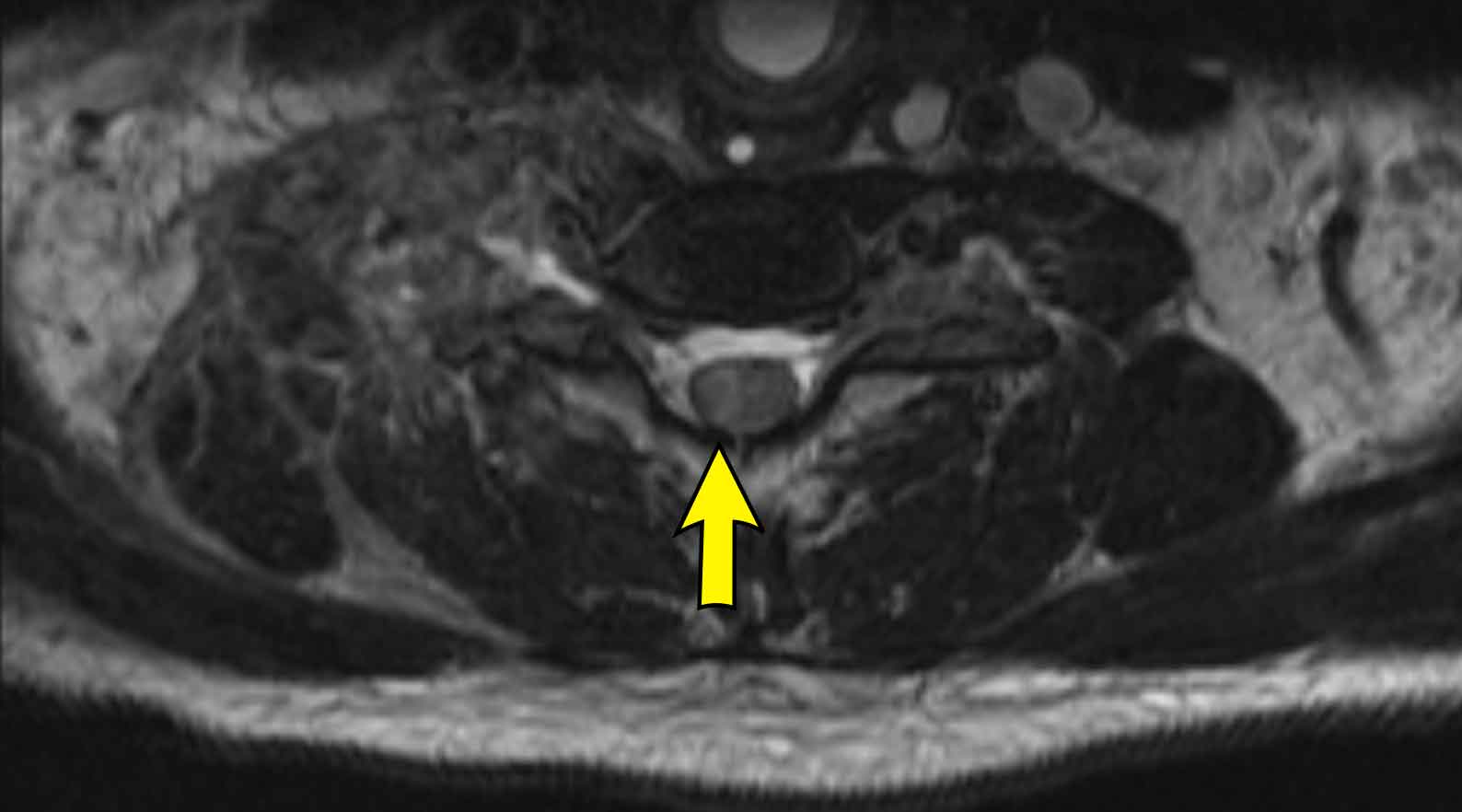
These images are of a 45-year old man who had a traumatic cord injury at the level of T4-5 some years ago.
He now presents with progressive pain in the legs with decreased reflexes in both arms and legs and a bilateral Horner.
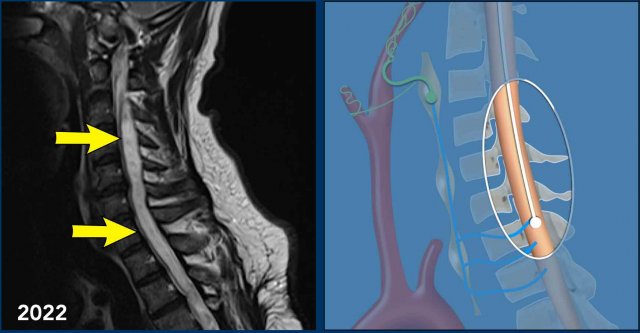
Images
Sagittal T2 TSE weighted images in 2021 of the cervicothoracic spine show loss of height of verterbra T4 with cord dissection and a cystic myelomalacia at this level and surrounding syringohydromyelia.
In 2022 sagittal T2W images
of the cervicothoracal spine show progressive syringohydromyelia.
Continue with the next images...
The Horner syndrome can be explained by the progressive syringohydomyelia at the cervical level with disruption of the first order neurons of the oculosympathetic pathway.
Case
45 year-old man with sudden onset
Horner syndrome, dysphagia, ipsilateral ataxia, nystagmus and sensory
impairment ipsilateral face and contralateral body.
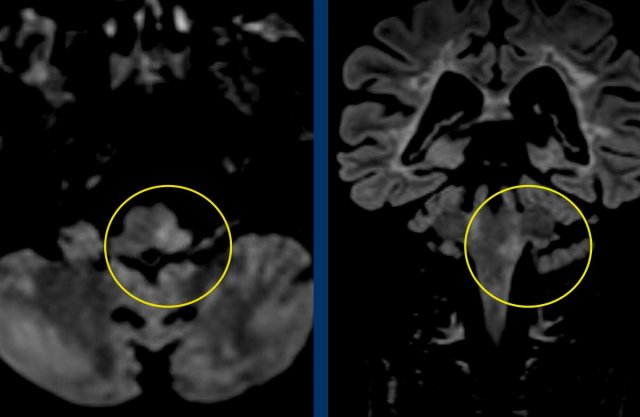
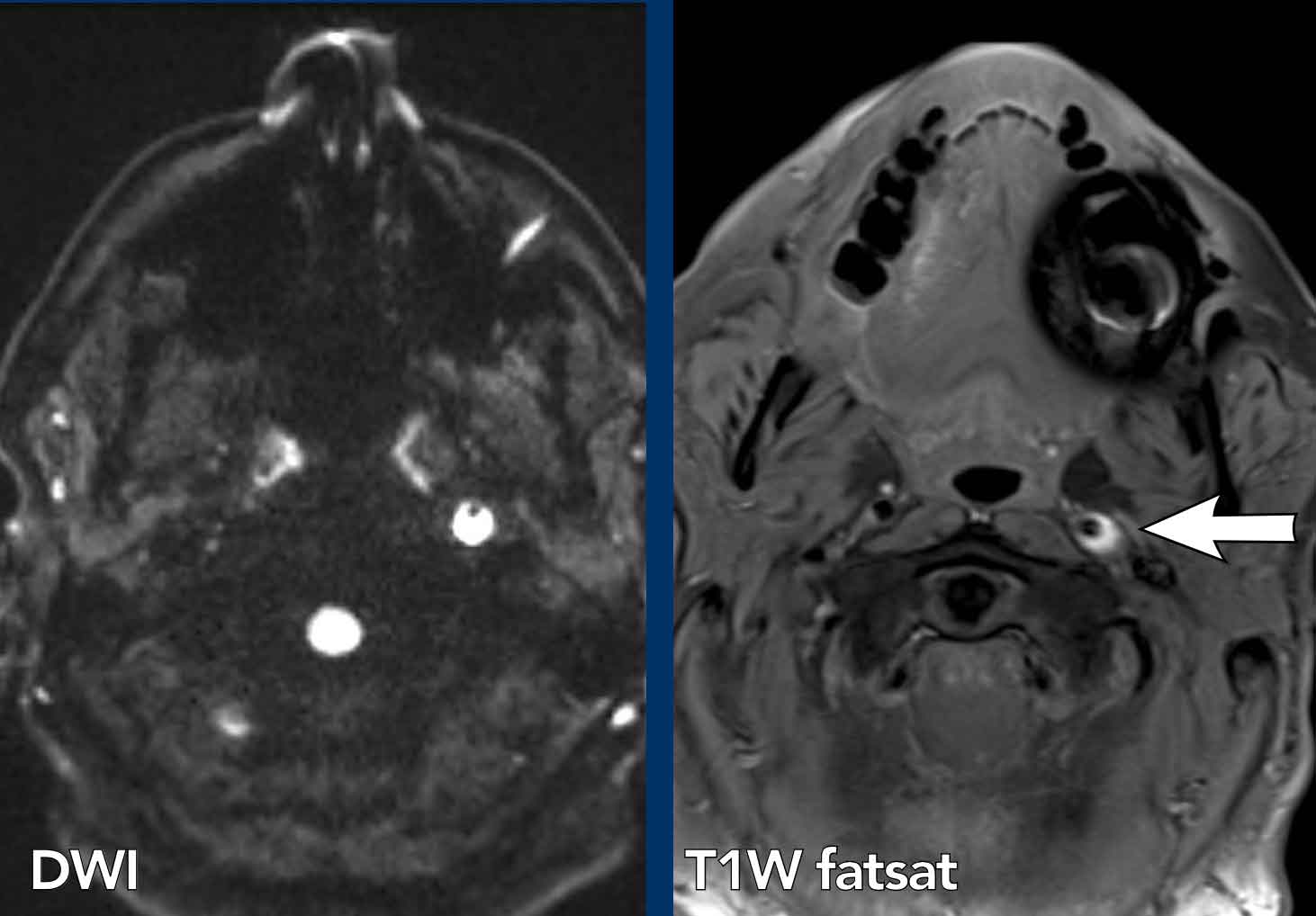
Images
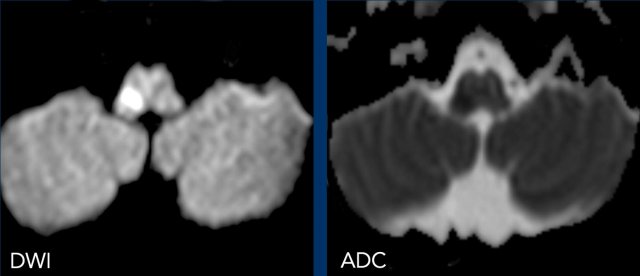
Diffusion weighted images
DWI (B1000) and ADC images show restricted diffusion in the medulla oblongata on right side due to a lateral medullary infarction.
Continue with the MRA of the neck...
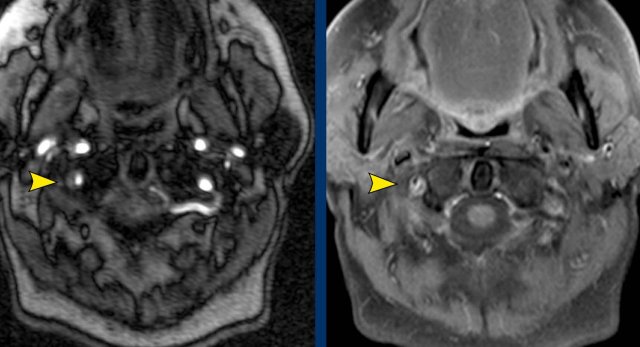
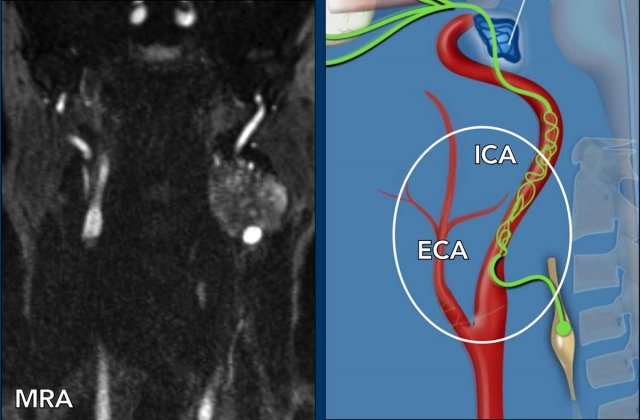
Images
Contrast enhanced MRA of the neck (on the right) shows narrowing of the right vertebral artery .
The T1WFS-image of the neck shows a hyperintense crescent signal intensity in the wall of the right vertebral artery typical of an intramural hematoma.
Conclusion
Dissection of the right vertebral artery resulting in a medullary infarction.
Case
These images are of a patient who was treated with antibiotics for a persistent cough that lasted for three weeks.
She now presented at the ER with a sudden nausea, vomiting, vertigo and diplopia (double vision).
At examination she had a bilateral Horner.
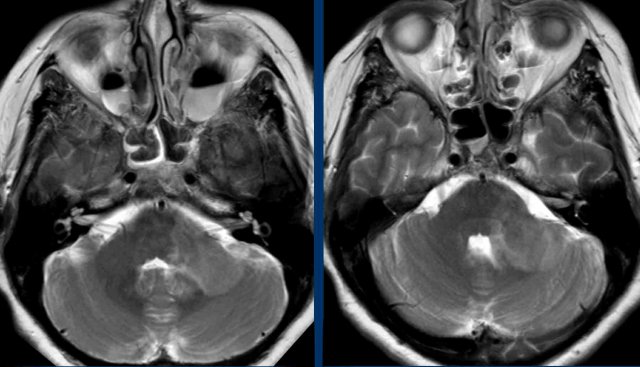
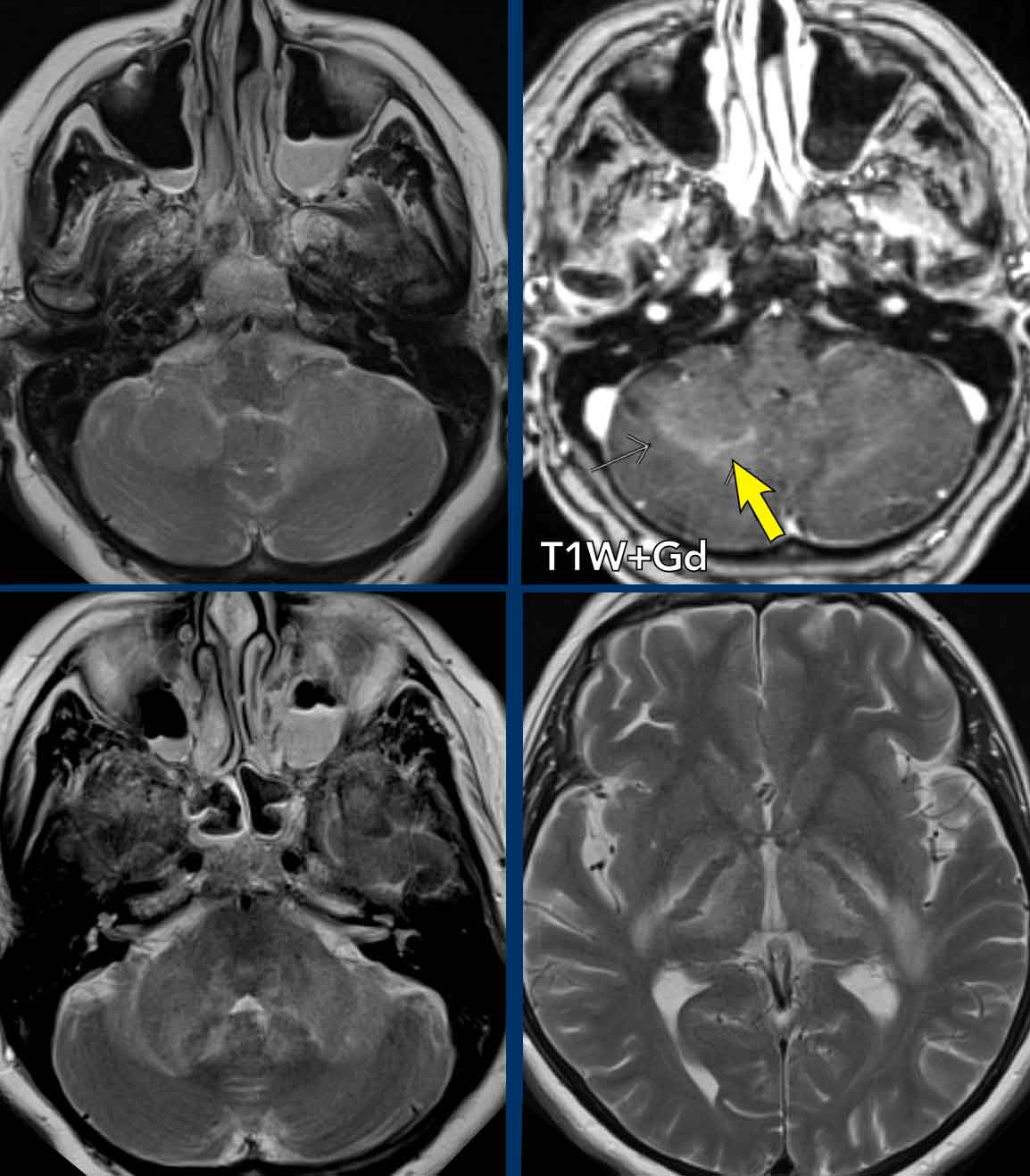
Images
This was a limited scan protocol (T2W and DWI) only to find out if there was any sign of ischemia.
There was no diffusion restriction (not shown) and acute ischemia was ruled out.
There is a large lesion with only limited mass-effect in the left cerebellar peduncle and there are bilateral air-fluid levels in the maxillary sinuses.
Continue with the follow up scan two days later...
First look at the four images.
What are the findings and what is your differential diagnosis?
You can click on the images for an enlarged view.
Images
- Lesions in both cerebellar peduncles, which means enormous progression in two days.
- Peripheral enhancement of the lesion on the right (arrow).
- Lesions in both thalami
- Lesions in the external capsule more on the left (right lower image).
- Diffusion was still normal (not shown).
Discussion
With this kind of fast progression of the disease a tumor can be excluded.
The differential focussed on demyelinization and rhombencephalitis.
Rhombencephalitis is an inflammatory disease affecting the brainstem and cerebellum with a wide variety of etiologies, including infection, autoimmune diseases and paraneoplastic syndromes.
Continue...
Conclusion
Finally the most likely diagnosis was an inflammatory rhombencephalitis.
there was a slow recovery.
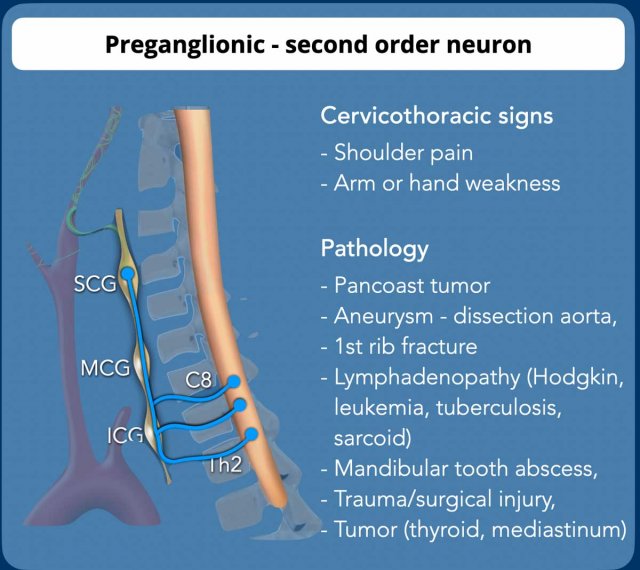
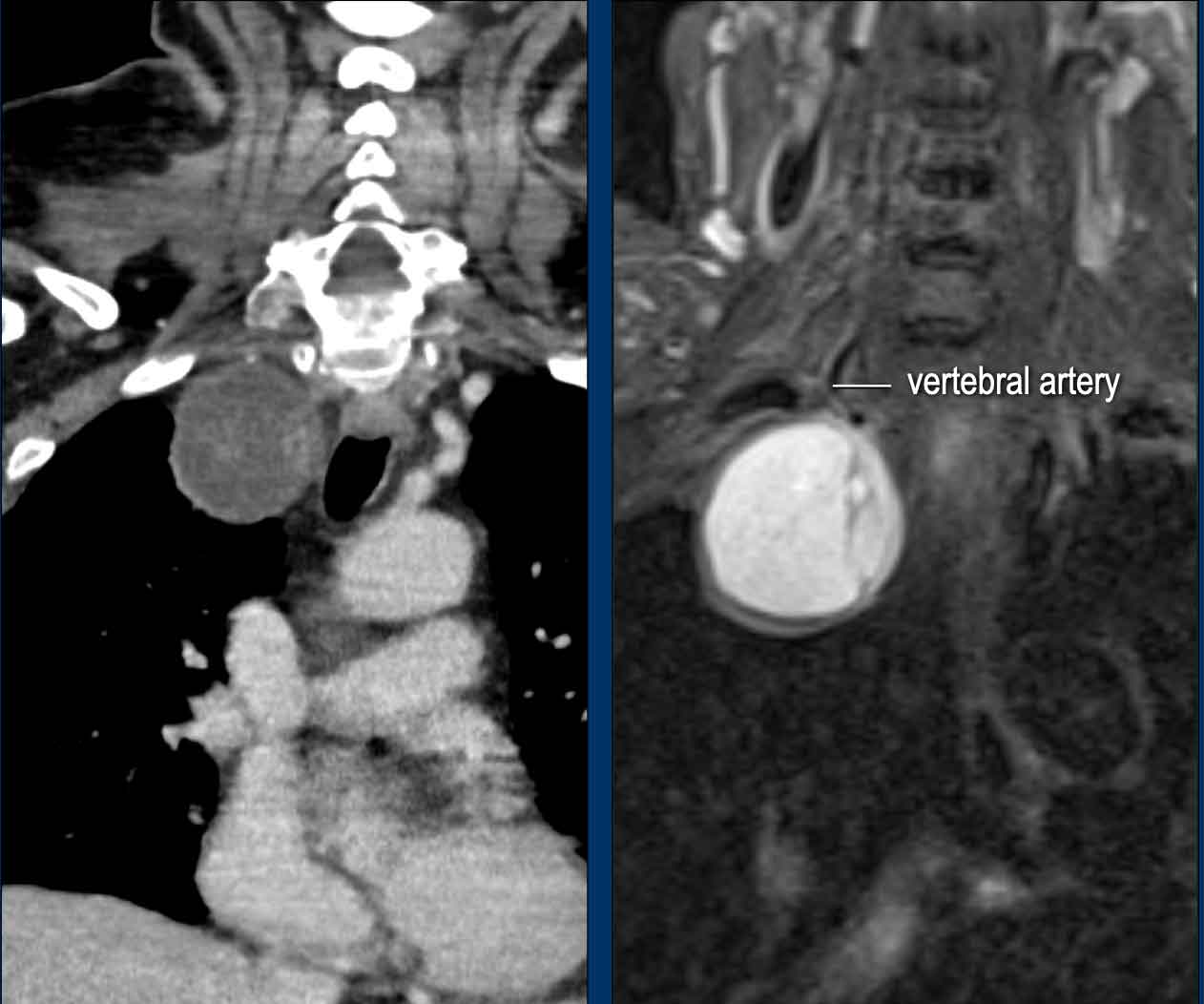
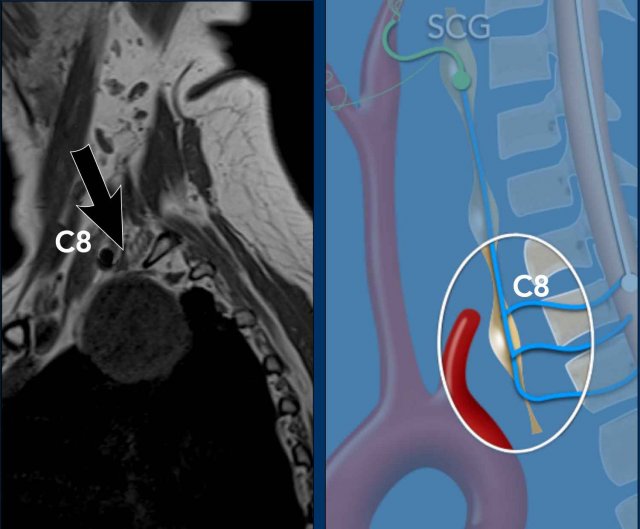
Preganglionic- 2nd order neuron
Preganglionic or second order neuron is
located in the intermediolateral gray substance of the spinal cord (ciliospinal center of Budge-Waller) between
C8 and T2.
Postganglionic fibers exit in the ventral spinal roots C8,
T1, and T2 and pass through the inferior cervical (or stellate ganglion, fusion with
the first thoracic ganglion to form the cervicothoracic ganglion), middle
cervical ganglion thereafter synapse in superior cervical ganglion.
The inferior cervical ganglion (ICG) is
located posterior to the vertebral artery between the transverse process of the C7
vertebra and the first rib.
The middle cervical ganglion (MCG) is
at the level of the cricoid cartilage C6, medial of the carotid tubercle and anterior
- superior to the inferior thyroid artery.
The superior cervical ganglion (SCG)
is located at the level of C2-C3 posterior to the carotid sheath and anterior
to the longus capitis muscle.
Arm pain or hand weakness are typical of brachial plexus lesions and indicates CT of the chest or a dedicated MR study of the brachial plexus.
Preganglionic Horner syndrome is a
common cause of Horner syndrome and most often caused by tumor or trauma.
Patients with preganglionic Horner's syndrome
often present with the classic triad: ptosis, miosis, anhidrosis and sometimes
in combination with brachial plexopathy.
The most common abnormalities that cause preganglionic Horner's syndrome are listed in the table.
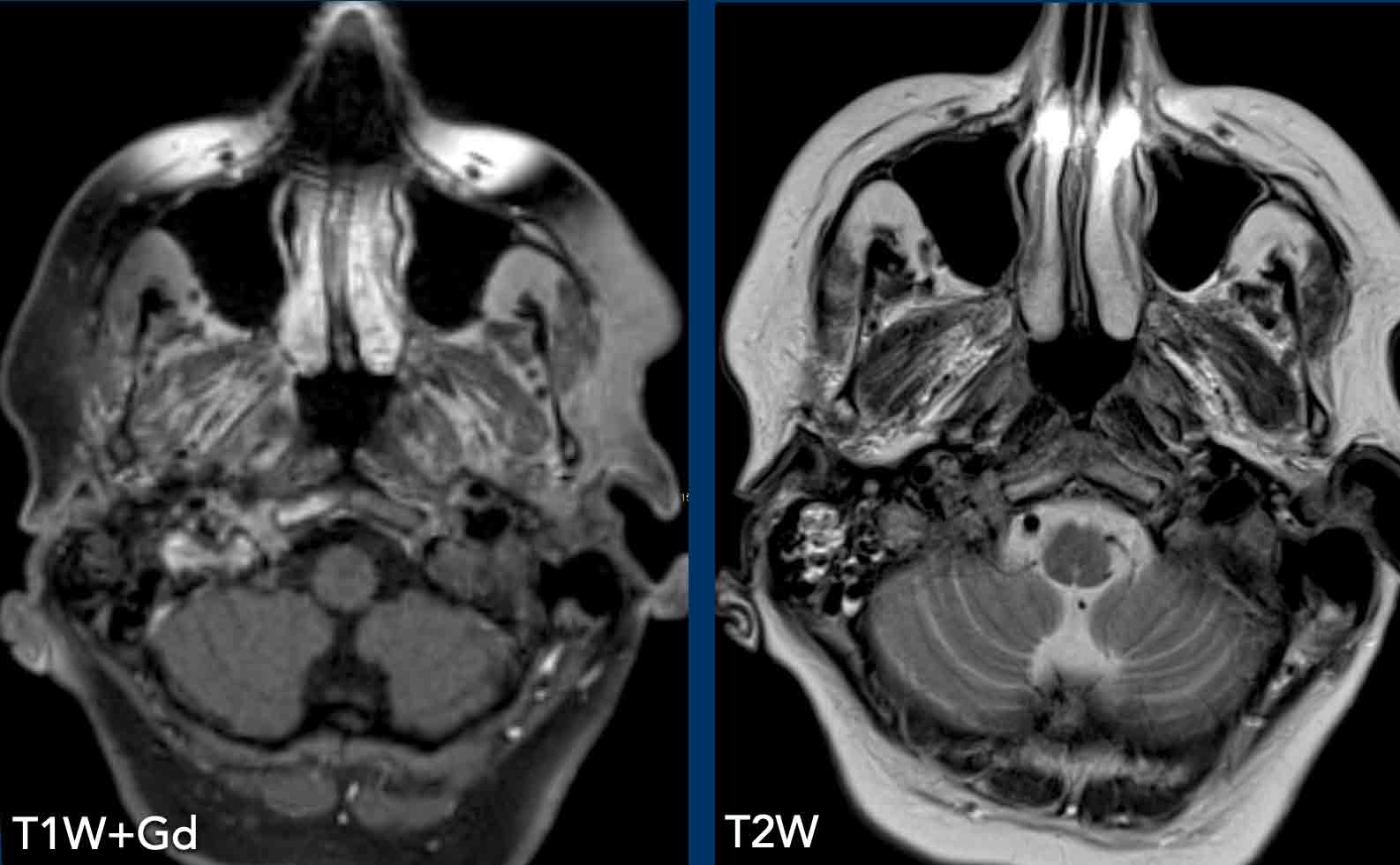
Cervical ganglia
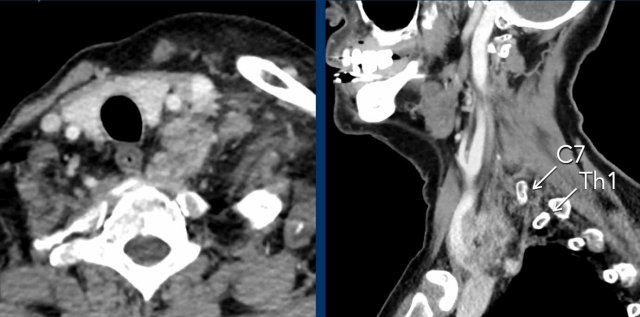
Case
These images are of a patient with a metastatic prostate cancer, who now presents with a paralysis of the hypoglossus on the right and a left-sided Horner.
First look at the images.
Where is the pathology.
Then continue reading.
Images
The left hypoglossus canal is normal.
On the right there is an enhancing mass.
Continue...
The image on the right illustrates the enhancing mass within the hypoglossal canal.
The hypoglossal canal is located between the occipital condyle and jugular tubercle and runs obliquely forwards from posteromedial to anterolateral allowing the hypoglossal nerve to exit the posterior cranial fossa.
In this patient with metastatic prostate cancer we assume that it is a metastasis.
This finding however does not explain the Horner on the left.
Continue...
Subsequently a CT of the neck and chest was performed, which showed a prevertebral mass at the level of C7-Th1.
This is the exact location of the inferior cervical ganglion.
A mass in this location explains the Horner on the left.
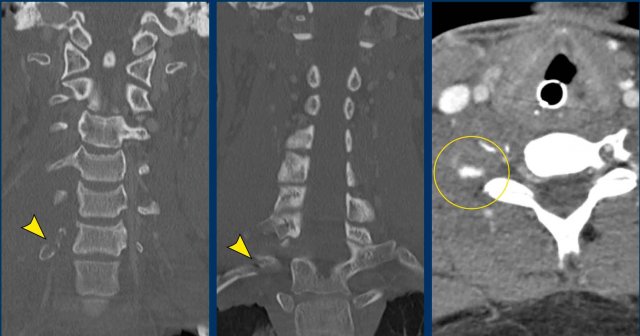
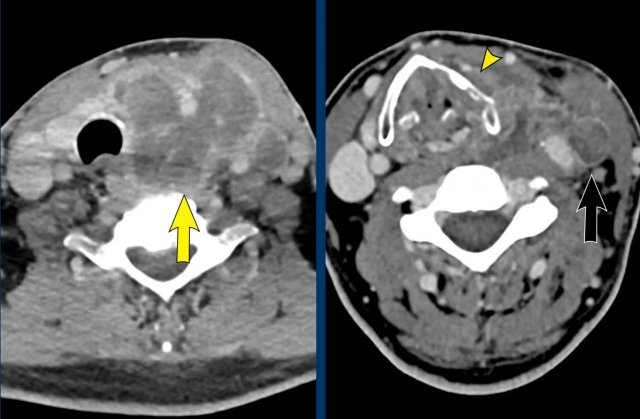
Case
This young man was involved in a motocross accident.
He was admitted to the ICU with multiple injuries.
After three days he regained consciousness and a paresis of his right side was noted, which could not be explained by any cerebral injury.
He also had a Horner on the right side.
Images
The CT at admission showed fractures of the transverse process of C7 and of the first rib (arrowheads).
On the CECT there was contrast extravasation indicating active bleeding (circle).
Continue with the MRI...
First an ultrasound of the neck was performed to look for nerve avulsion, but this examination was limited by traumatic changes in this area.
Subsequently an MRI was performed.
Images
The
axial image shows enhancement of nerve roots indicative of a brachial plexus
injury.
Also note the injury to the right paravertebral soft tissues.
Continue....
Image
In addition the T2W-image shows some subtle high signal in the myelum on the right (arrow).
This was regarded as post traumatic myelopathy and could also be an explanation for the right-sided Horner.
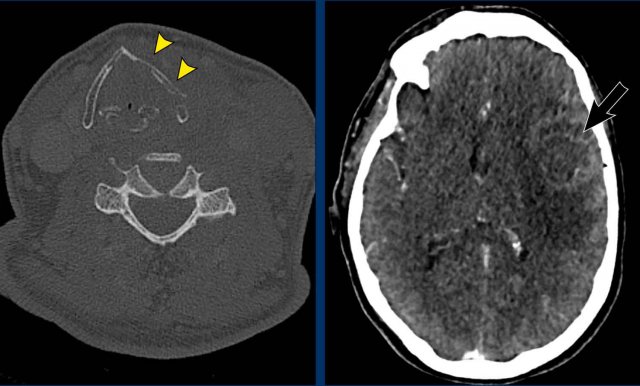
Case
Images of a patient with a rapidly enlarging neck mass, who complaints of swallowing problems and hoarseness.
The physical examination also detected a partial Horner with ptosis and miosis.
Images
CT of the head and neck shows an
invasive thyroid mass with paralaryngeal and prevertebral extension and involvement
of thyroid cartilage (yellow arrowhead).
There is a tumor thrombus in the jugular vein (black arrow).
Continue with the next images...
Images
Notice the invasion of the thyroid cartilage (yellow arrowhead).
On the edge of the scan there was a brain metastasis.
Discusson
The Horner is caused by influencing the preganglionic system.
There are numerous fibers connecting the middle cervical ganglion (MCG) and inferior cervical ganglion (ICG), which are located anterior and posterior to the vertebral artery.
Final diagnosis
Anaplastic thyroid carcinoma.
This cancer is one of the most aggressive tumors and has a bad prognosis.
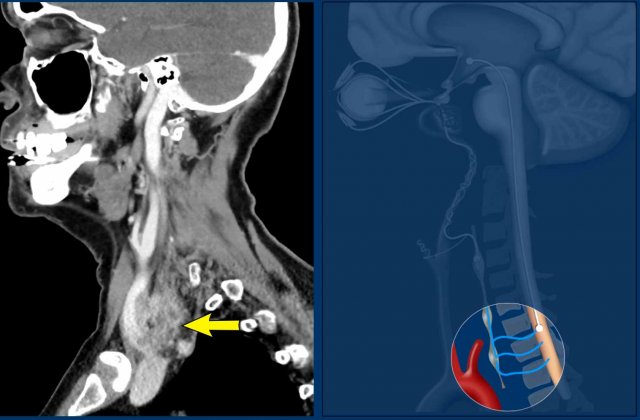
Case
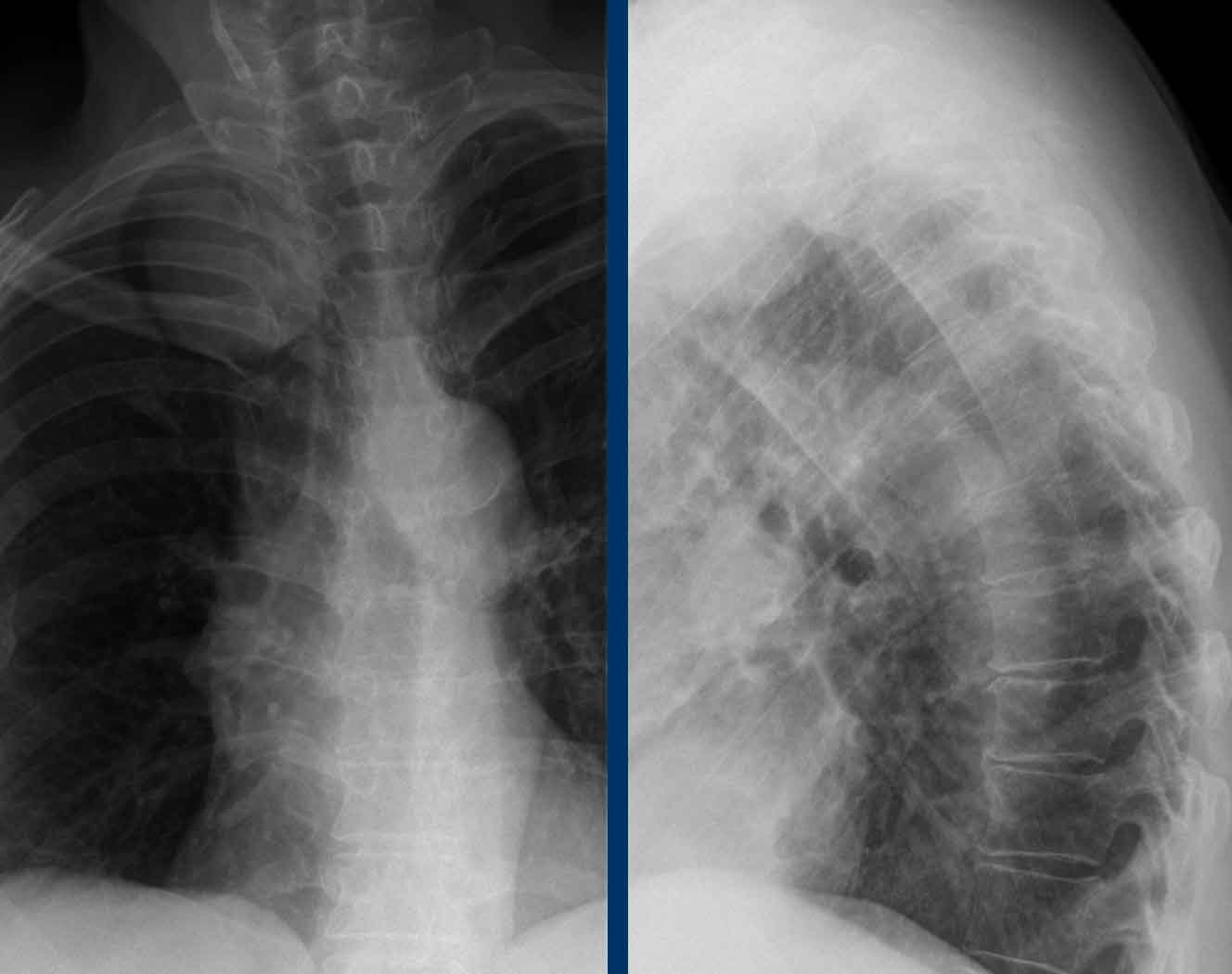
images of a 55 year old women woman with pain in the shoulder and neck.
Images
The X-ray of the cervical
and thoracic spine shows a mass projecting apically
about the right lung.
Given the cervicothoracic sign most likely originating
from the posterior mediastinum.
Differential diagnosis
The most likely diagnosis of a mass in the posterior mediastinum is:
- Neurogenic tumors (schwannoma, neurofibroma).
- Lymphadenopathy.
- Neuroenteric cysts
- Meningoceles
- Extramedullary
hematopoiesis.
Click here for more information on mediastinal masses.
Continue with the next images...
At neurologic examination a Horner syndrome on the rigth side was detected.
First a CT was performed because a possible malignancy was suspected.
Images
The CT shows an encapsulated lesion in the posterior mediastium.
There is no lymphadenopathy.
The MRI shows a well-defined lesion with T2 hyperintense signal indicating cyst or necrosis.
Continue...
Images
The sagittal T1W image shows rim enhancement.
Conclusion
The lesion has a mass effect on the inferior cervical ganglion on the right side and that is the cause of the Horner syndrome.
The most likely diagnosis is an old schwannoma.
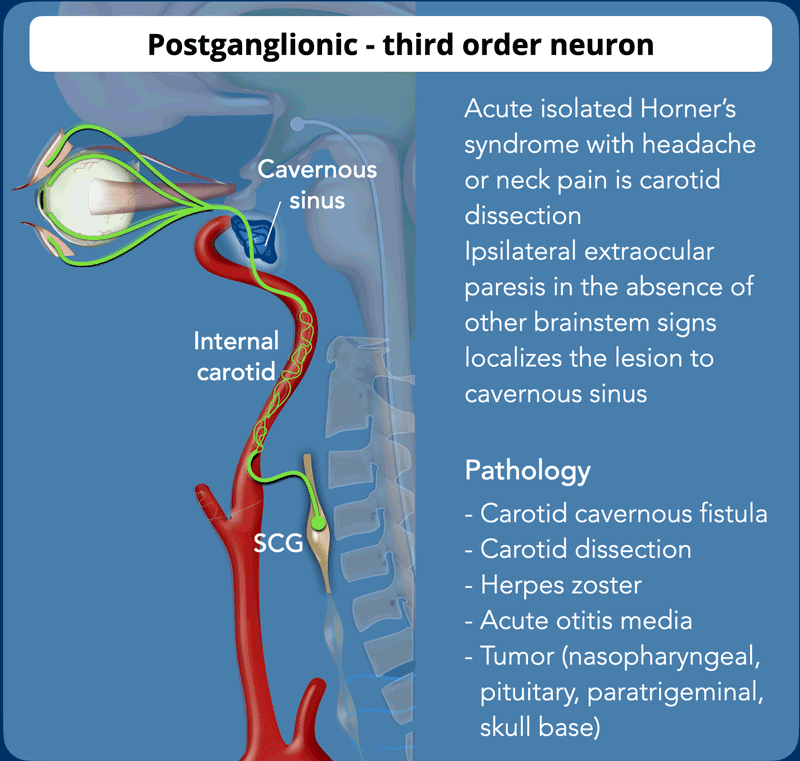
Postganglionic - 3rd order neuron
The postganglionic neuron starts after the synapse of the superior
cervical ganglion at the level C2-3 where the sympathetic plexus passes posterior to the
carotid space and anterior to the longus
colli muscle.
The neuron travels along the internal carotid artery and the cavernous sinus
along the n VI and n V₁ via the superior orbital fissure to the superior
tarsalis muscle, also called Muller's muscle.
Sympathetic fibers traveling with the
external carotid artery follow the internal maxillary artery to the face and innervate the
sweat glands.
Postganglionic causes of Horner are as common compared as preganglionic.
For pathology causing
postganglionic Horner syndrome we have to study the internal and
external carotid artery, skullbase , cavernous sinus, orbital apex and the eye.
- An acute isolated Horner syndrome with headache or neck pain is a carotid dissection until proven otherwise and MRA or CTA of the head and neck is needed.
- An ipsilateral extraocular paresis (nIII, nIV, nVI) in the absence of other brainstem signs localizes the lesion to the cavernous sinus.
- Horner syndrome as a result of a Herpes Zoster infection is extremely uncommon, but the anatomic relationship of the fifth, sixth, and sympathetic nerves in the cavernous sinus may provide a route whereby the varicella-zoster virus can produce a Horner syndrome.
Carotid artery
Case
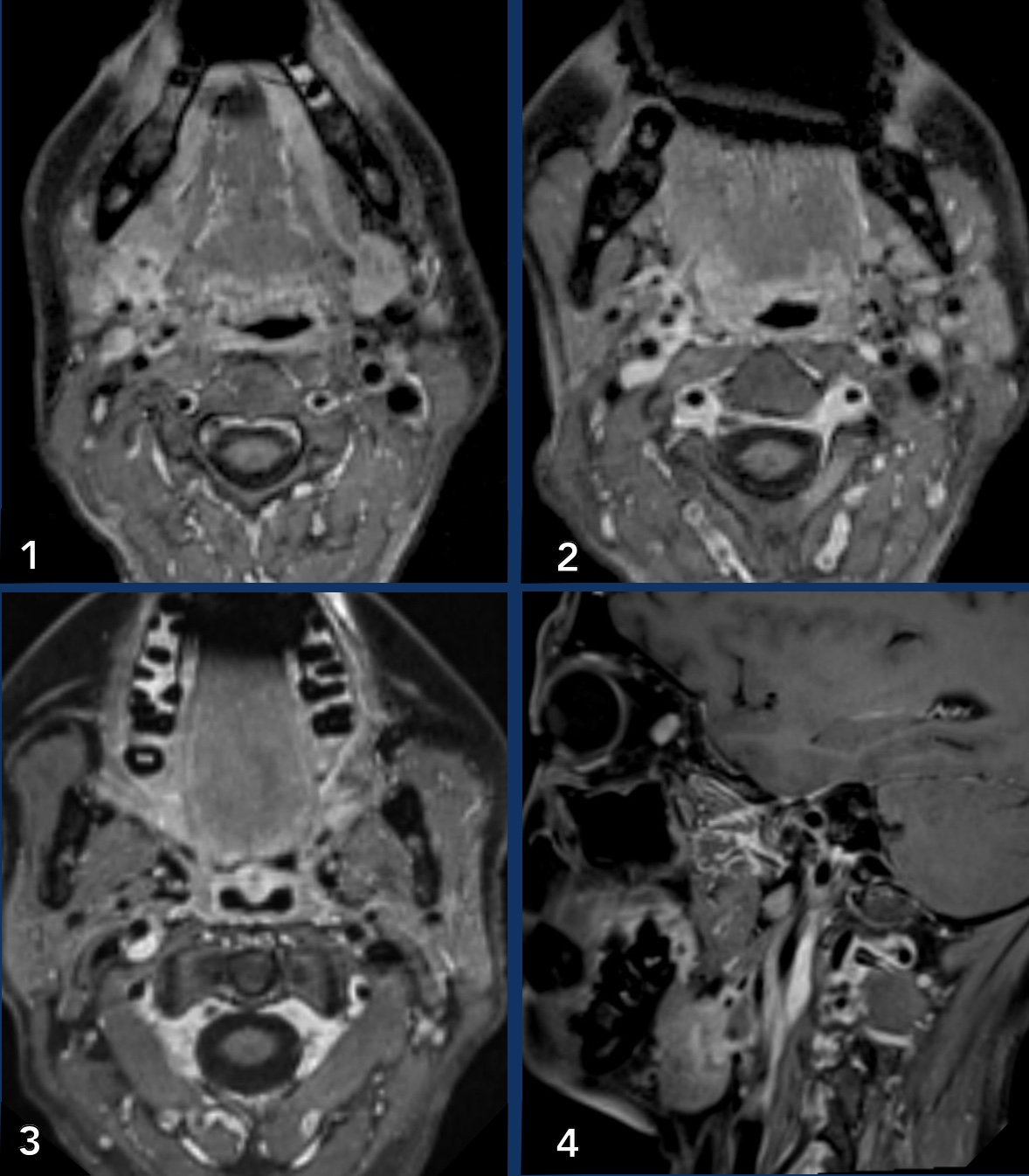
These
images are of a patient who had a swelling in the neck for a couple of years.
Extensive imaging studies followed, but all studies were negative.
She
now presented with and a Horner on the right.
Study the images.
What are the findings?
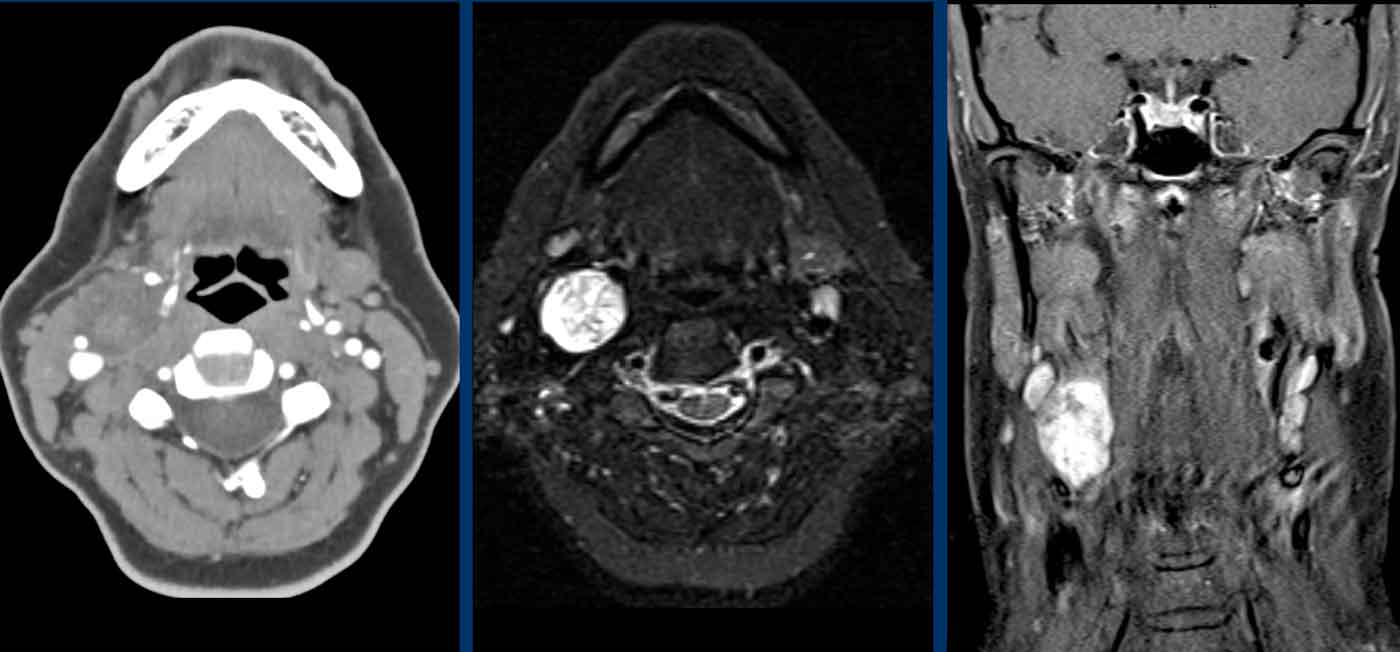
Images
- When you compare the right and left submandibular gland (image 1), you will notice an enhancing mass lesion on the right (arrow on scroll image).
- The enhancement can be followed on image 2 and 3 along the internal and the external carotid
- This can also be appreciated on the sagittal image, where the enlarged gland is seen (*) and streaks of enhancement along the internal carotid artery (arrow heads).
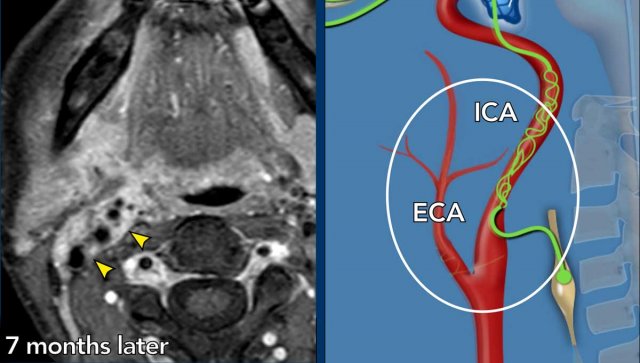
Images
Seven months later the tumor surrounding the ICA and ECA has enlarged.
Conclusion
This turned out to be an adenoid cystic carcinoma with
perineural tumorspread.
Case
These images are of a 73-year old man who presented with a mass in the neck.
Examine the images.
What are the findings and most likely diagnosis?
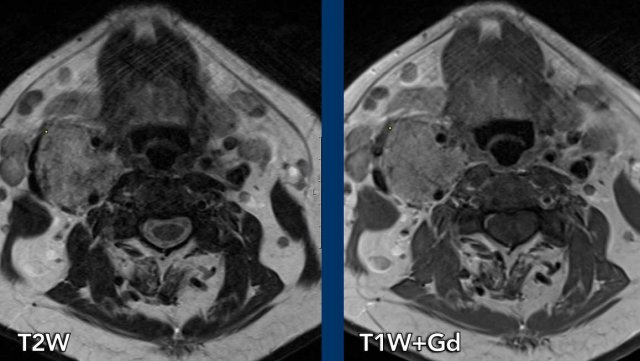
Images
There is a lesion in the carotid space at the bifurcation splaying the internal and external carotid artery.
On T2W the lesion is hyperintens and on T1W isointens with peper and salt appearance.
There was enhancement after contrast (image not shown).
Continue with the Twist-MRA images...
Examine the images.
What are the findings and most likely diagnosis?
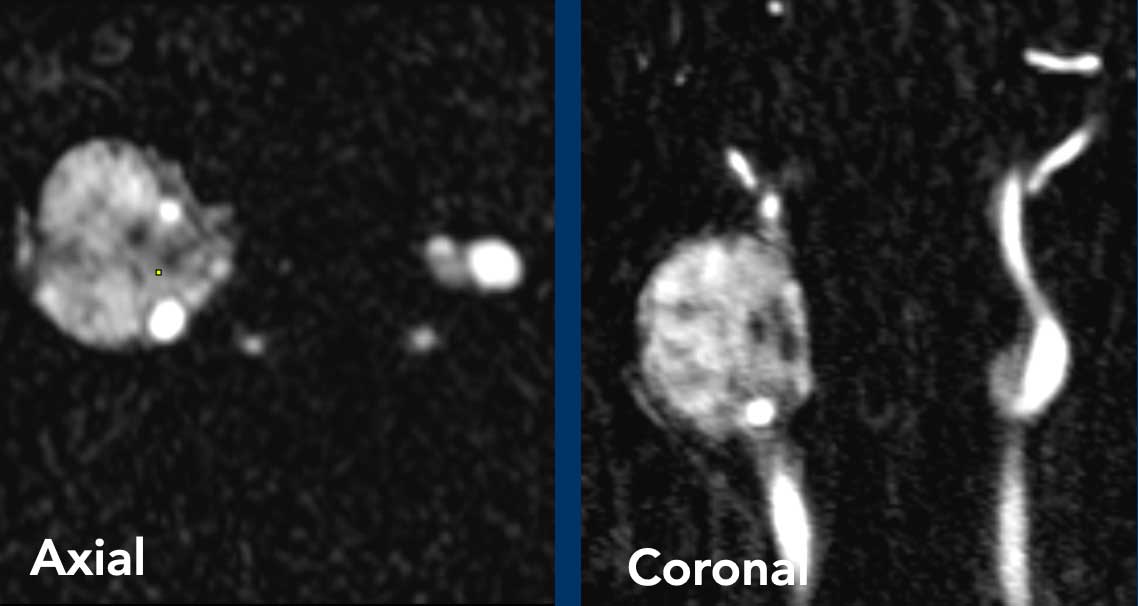
Images
On the TWIST MRA there is early artery enhancement in the large lesion on the right.
Notice that on the left side there is also a early arterial enhancing lesion on the carotid bifurcation.
Conclusion
Bilateral paraganglioma.
Bilateral lesions are common in inherited syndromes like SDH gene mutations.
Here a companion case with a paraganglioma on the left.
Continue with the Twist-MRA images...
Image
3D-TWIST MRA shows intense early arterial enhancement
The illustration shows the level of obstruction of the postganglionic neuron.
Case
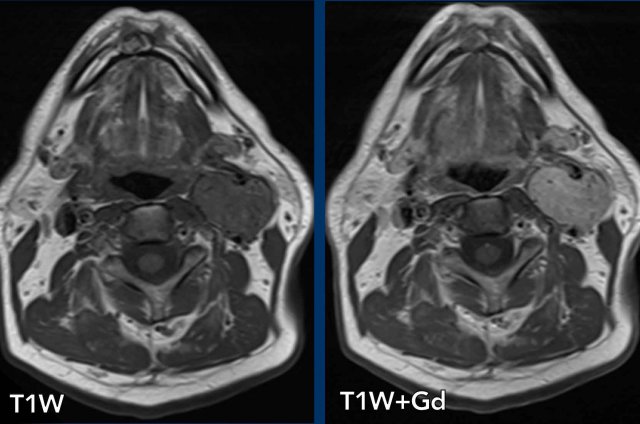
Images of a 45 year old man with an asymptomatic neck mass and a Horner
syndrome at physical examination.
Images
- CTA of the neck shows a mass in the carotid space on the
right side.
There is no real early arterial enhancement.
The internal carotid artery is displaced anteromedially and the jugular vein is displaced posterolateral. - T2WI shows an hyperintens lesion.
On the left side there are some lymph nodes, which are not pathologically enlarged. - Coronal T1W-image shows late contrast enhancement.
Conclusion
This was a schwannoma.
A paraganglioma would have shown early enhancement on the CT image.
Case
These images are of a patient who presented with sudden problems of speaking in a fluid way.
The physiacal examination revealed an unequal size of the eyes' pupils and the impression of a hemianopsia on the right.
The patient was presented to the stroke unit.
The non-enhanced CT was normal, which excluded a hemorrhage.
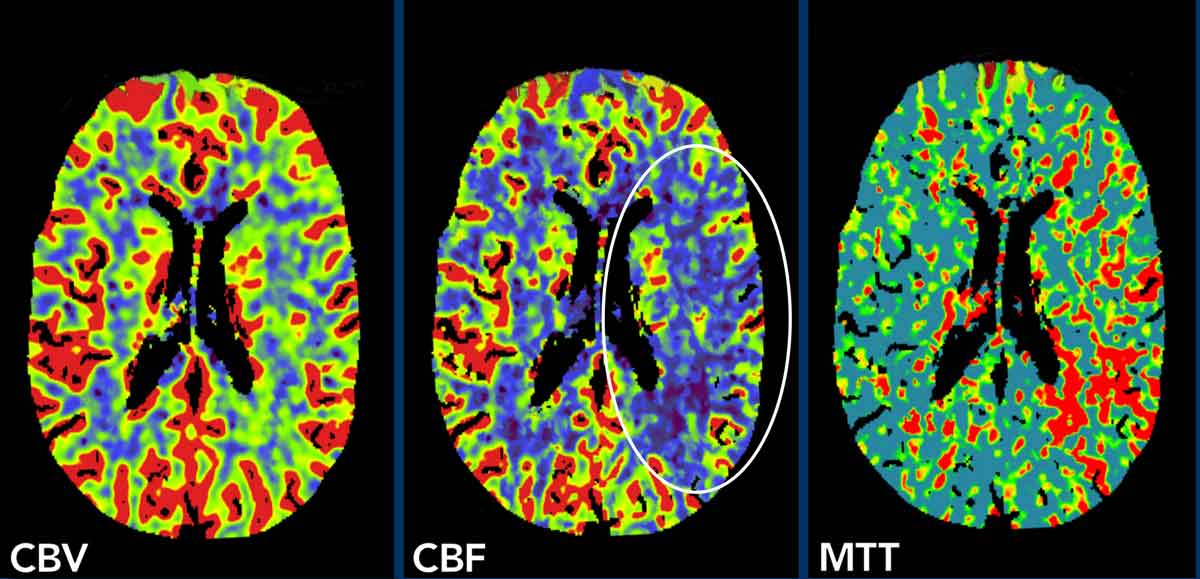
Images
The perfusion images show a slightly decreased cerebral blood volume (CBV) and flow (CBF) in the territory of the middle cerebral artery on the left (circle) and an increased mean transit time (MTT).
This patient had a M3-occlusion, which was visible when we did scroll through the images (not shown)
However a M3-occlusion can only explain a small part of the findings on the perfusion images.
In those cases you always have to study the internal carotid artery.
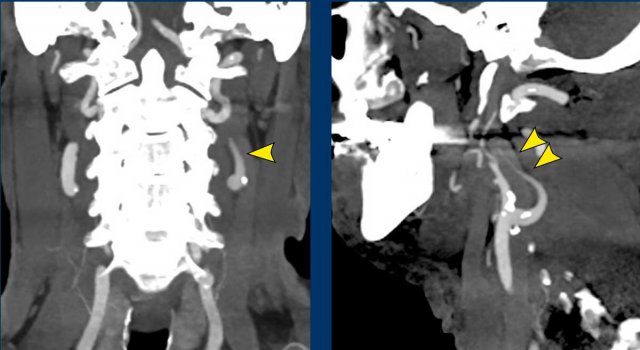
Images
The image on the right shows the typical CTA-appearance of a carotid dissection with the flame shape a couple of centimeters above the bifurcation (arrowheads).
Two weeks later and MRI was performed.
Images
An intramural hematoma of the dissection is nicely shown (arrow).
At that time a Horner on the left was also noted and this can be explained by the pressure by the intramural hematoma of the ICA on the post-ganglionic system (third order neuron) travelling in the adventitia of the internal and external carotid arteries to the cavernous sinus.
In these patients the Horner can resolve when the hematoma minimizes, as was the case in this patient after treatment with antiplatelet agents.
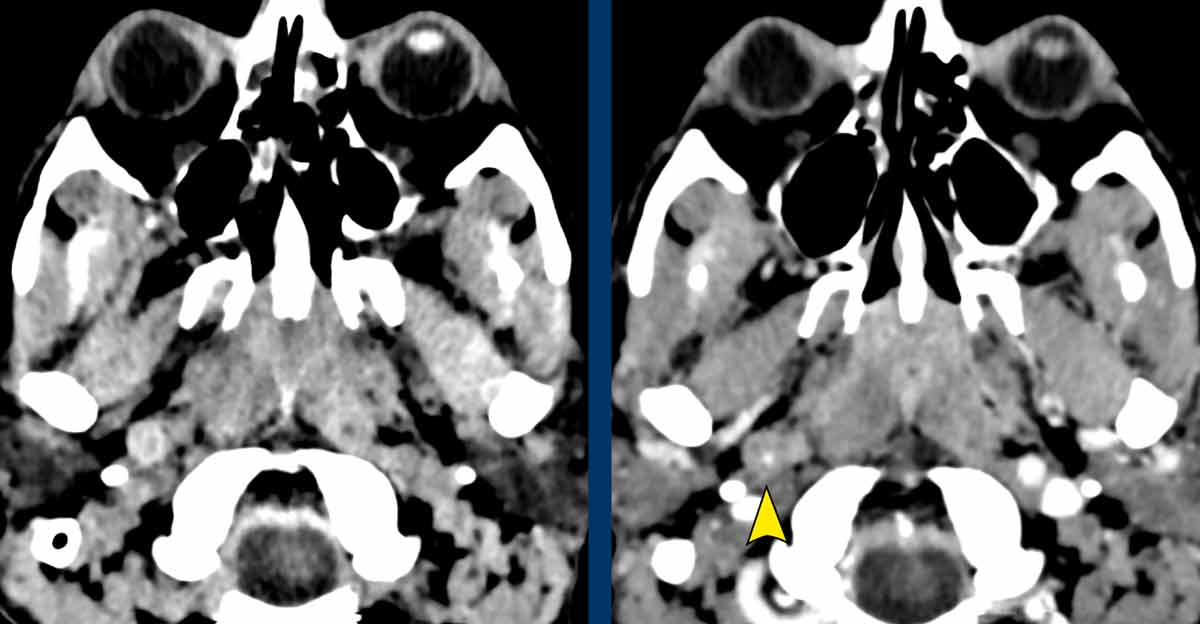
Case 5
This
is a similar case.
Images
Notice
on the non enhanced CT on the left that the internal carotid is larger in
diameter as a result of the hematoma.
On
the enhanced CT on the right the narrowed true lumen is demonstrated
(arrowhead).
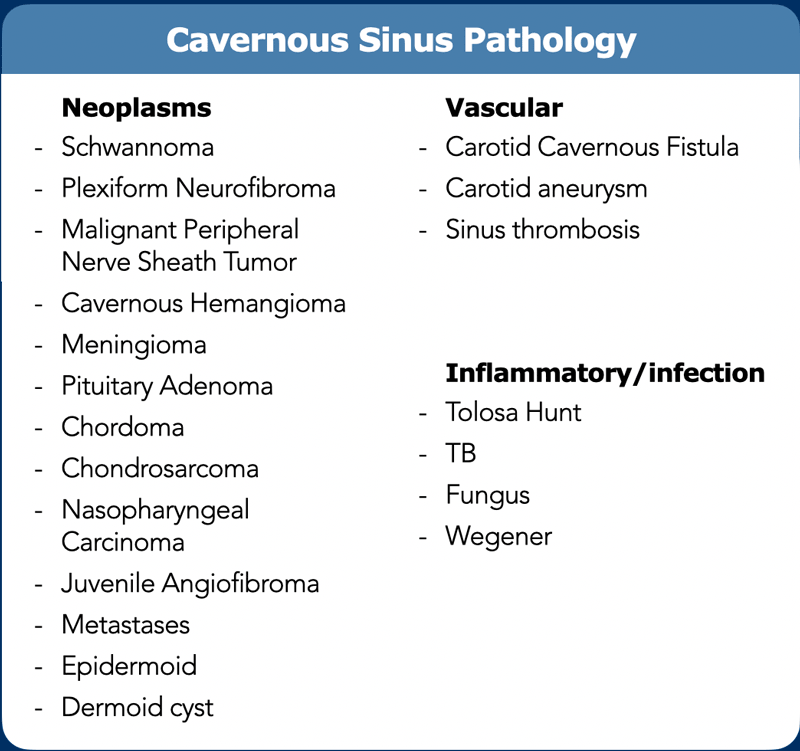
Cavernous sinus
The list of cavernous sinus pathology is extremely long and contains neoplastic, inflammatory and vascular lesions (table).
Case
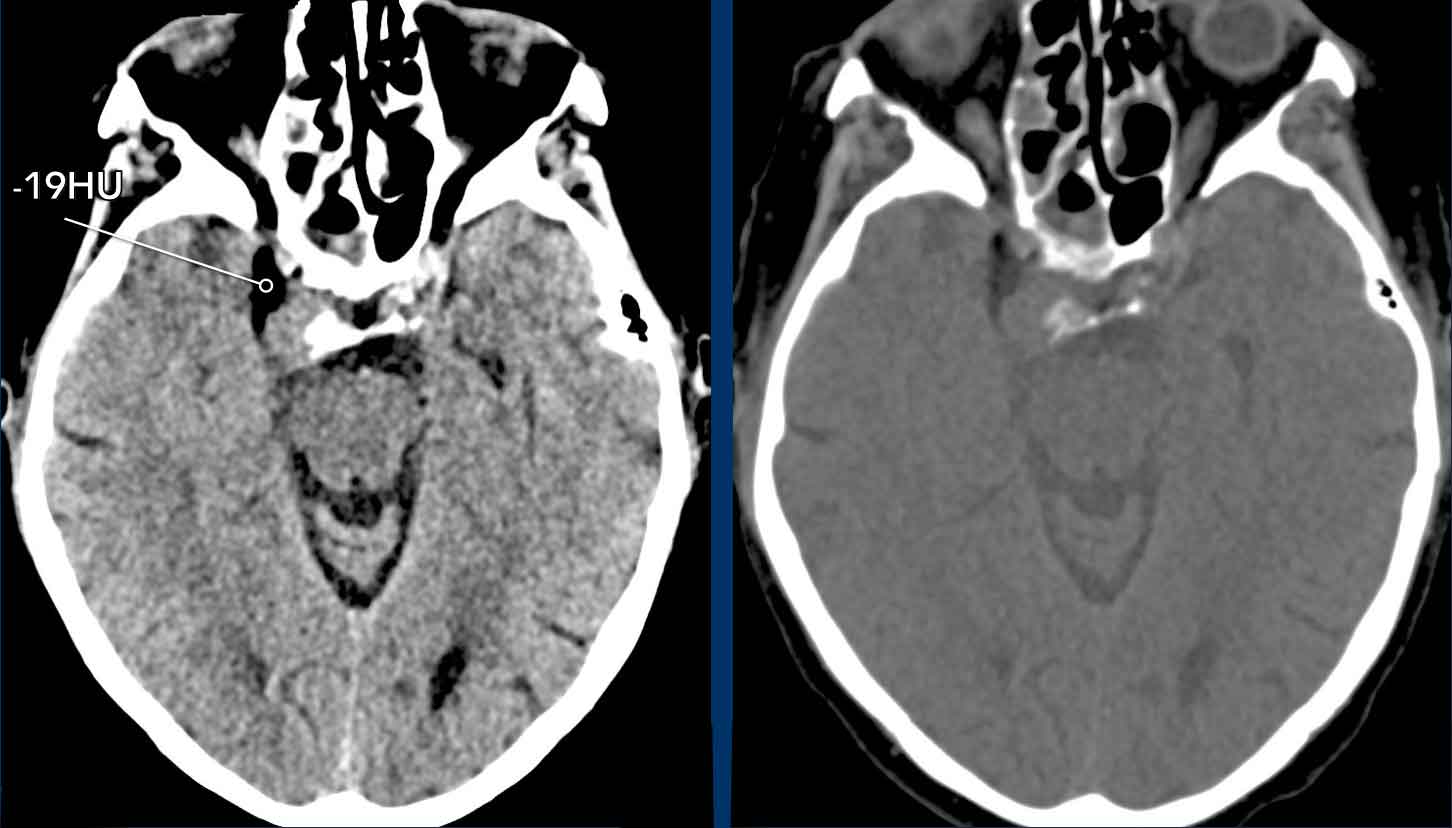
These images are of a 79-year-old woman who could not be examined properly because she was in fetal position and was shivering severely.
She also had a Horner syndrome on the right, but this was diagnosed later, which is not uncommon as we mentioned before.
Because of her clinical condition a CT-scan was preferred over a MRI.
First study the CT.
What are the findings and what is your differential diagnosis?
Images
Mass lesion on the right at the level of the cavernous sinus.
The lesion contains fat
Discussion
Based on the presence of fat within the lesion the differential diagnosis was dermoid cyst and hemangioma.
Continue with the MRI...
Images
The MR-images show fat located within the tumor and this is not the normal fat that we sometimes see surrounding the cavernous sinus.
This patient was operated and the final diagnosis was a hemangioma.
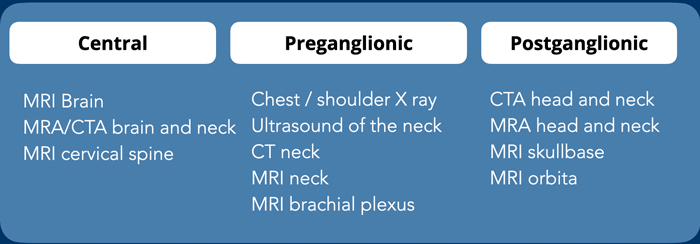
Imaging protocol
CT and MRI can be complementary, but CT is preferred in the acute setting and for evealuation of vascular and osseous injury and pulmonary mass
MRI is preferred for imaging of the brain and spinal cord.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.