Peritoneal Pathology
Angela Levy
Chief Gastrointestinal Radiology, Department of Radiologic Pathology, Armed Forces Institute of Pathology, Washington DC Associate Professor of Radiology, Uniformed Services University of the Health Sciences, Bethesda, MD
Publicationdate
This review is based on a presentation given by Angela Levy and adapted for the Radiology Assistant by Robin Smithuis.
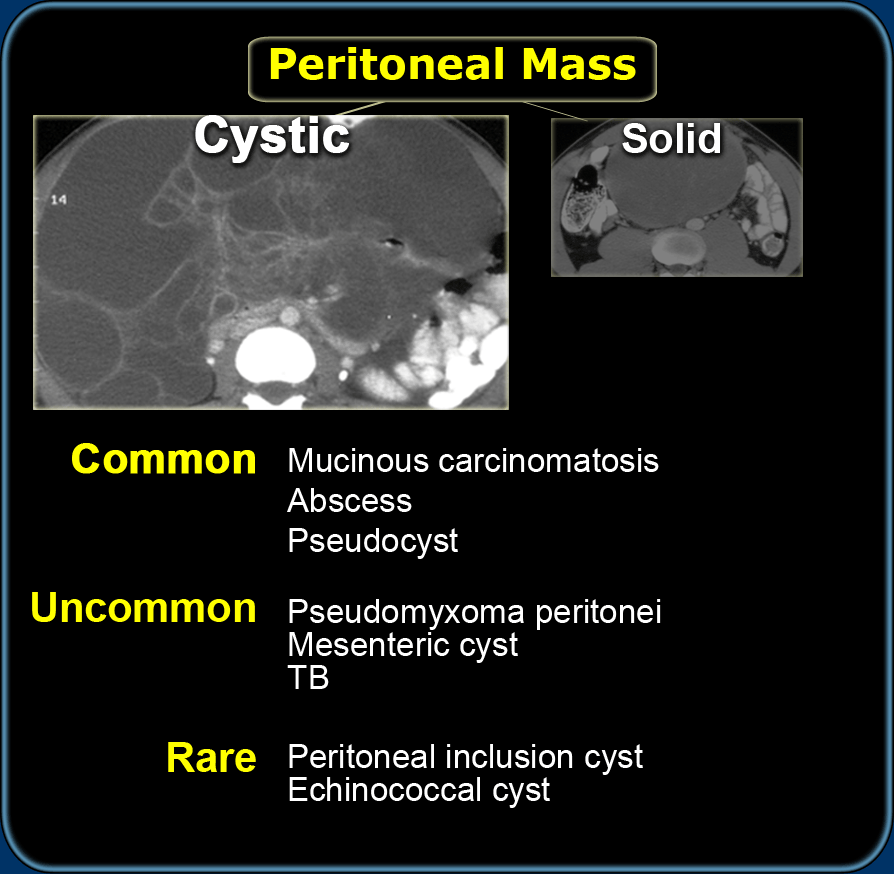
We will discuss the differential diagnosis of cystic and solid peritoneal and mesenteric masses.
In Peritoneum and Mesentery - part I: Anatomy
the normal anatomy and physiology of the peritoneum and peritoneal cavity are discussed.
You can click on images to get an enlarged view.
by Angela Levy
Differential Diagnosis
Cystic masses
The first step when diagnosing peritoneal or mesenteric masses is to separate them into cystic and solid.
Secondly we have to realize that any loculated fluid collection due to infection, i.e. abscess or as a result of pancreatitis, perforation or bile peritonitis can simulate a cystic mass.
Especially fluid collections in the lesser sac can simulate a cystic mass.
Lastly we have to know which cystic masses are common and look for specific features of these masses.
- Mucinous carcinomatosis
is the most likely diagnosis of cystic peritoneal masses. - Pseudomyxoma peritonei
is less common, but looks quite similar to peritoneal carcinomatosis. - Mesenteric cyst
Lymphangioma is the most common mesenteric cyst.
Other mesenteric cysts like enteric duplication cyst, enteric cyst, nonpancreatic pseudocyst and mesothelial cyst are very uncommon and have no specific features. - Peritoneal inclusion cyst
is a less common benign primary peritoneal tumor.
It is also known as benign multicystic mesothelioma.
This name is very confusing since there is no relation with the malignant mesothelioma. It is seen in women with prior gynaecological surgery or infection.
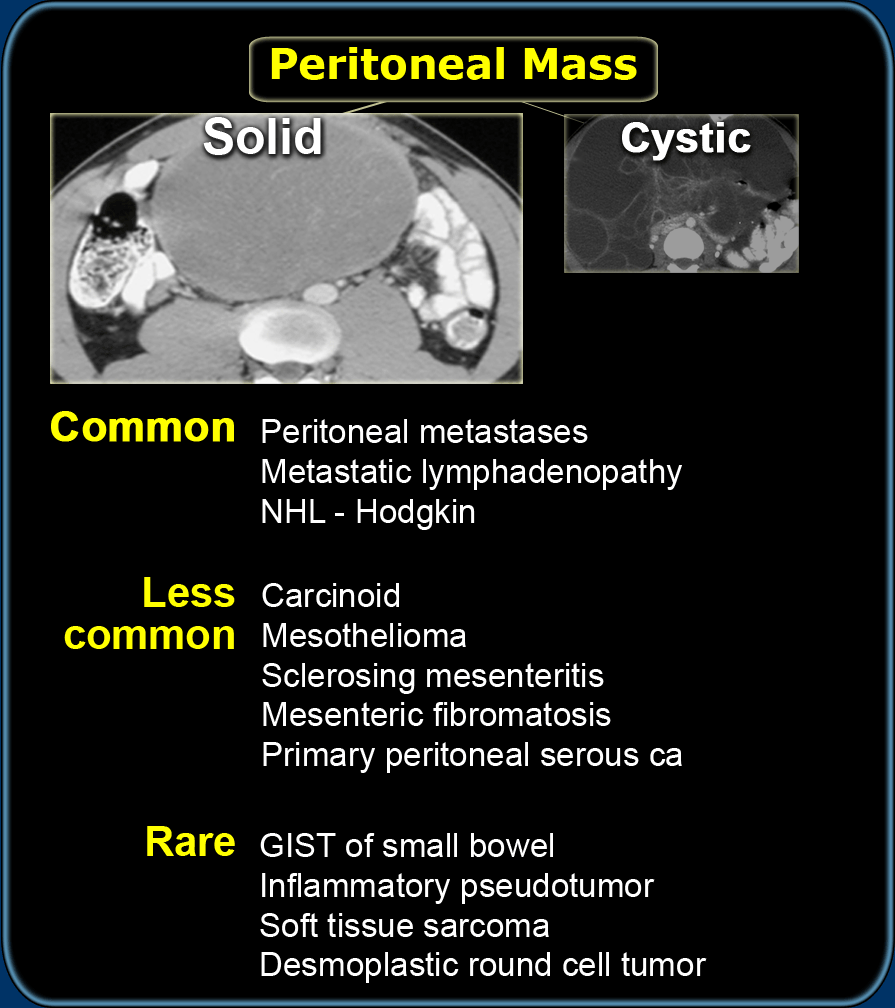
Solid masses
- Peritoneal carcinomatosis
Is the most common peritoneal solid mass resulting from ovarian or gastrointestinal cancer.
Usually there are omental metastases, i.e. omental cake and ascites. - NHL and lymph node metastases
Are the most common diagnoses of a mesenteric mass.
NHL is the most common cause of lymphadenopathy and usually there are other sites with lymphoma. - Carcinoid
Presents as a spiculated mesenteric mass often with a central calcification. It metastasize to the liver.
There is associated bowel wall thickening due to a desmoplastic reaction. - Sclerosing mesenteritis
May look like carcinoid.
There is a wide spectrum of presentations ranging from an infiltrative solid mass to the more common accidental finding also known as mesenteric panniculitis, which presents as a lipomatous mass, usually with no clinical implication. - Mesenteric fibromatosis
Is also known as intraabdominal fibromatosis, abdominal desmoid or desmoid tumor.
It is a locally aggressive tumor which often recurs but does not metastasize.
It can have a myxoid stroma resulting in a low attenuation on CT and a high attenuation on T2WI. - Mesothelioma
Accounts for 20% of all mesotheliomas and is associated with asbestos exposure and pleural plaques.
Cystic Masses
Mucinous Carcinomatosis
Mucinous carcinomatosis is the most common cystic tumor to affect the peritoneal cavity.
Usually these metastases arise from mucinous carcinomas of the ovary or of the gastrointestinal tract (stomach, colon, pancreas).
The prognosis is poor.
However, when low-grade mucinous adenocarcinoma of the appendix spreads to the peritoneal cavity, the consequence is typically pseudomyxoma peritonei, which is a distinct tumor with a better prognosis.
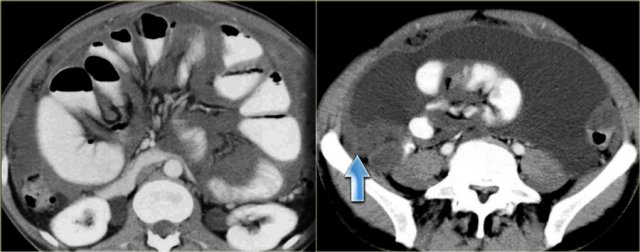
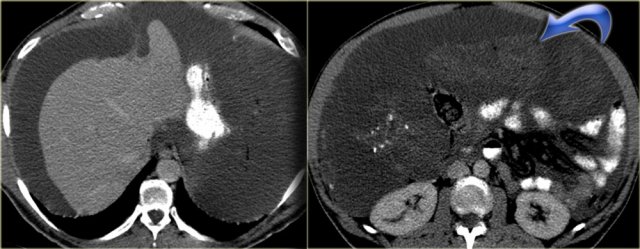
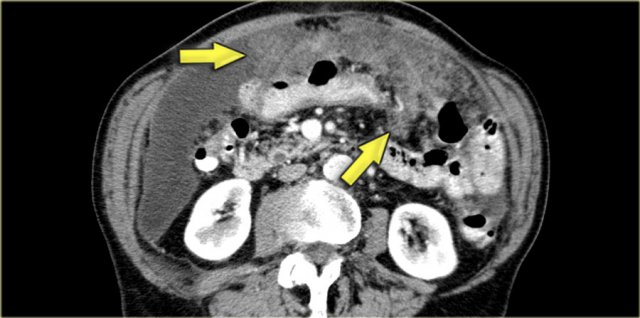
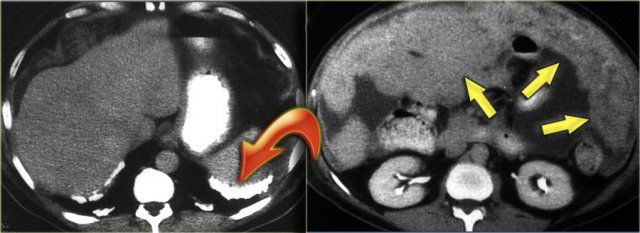
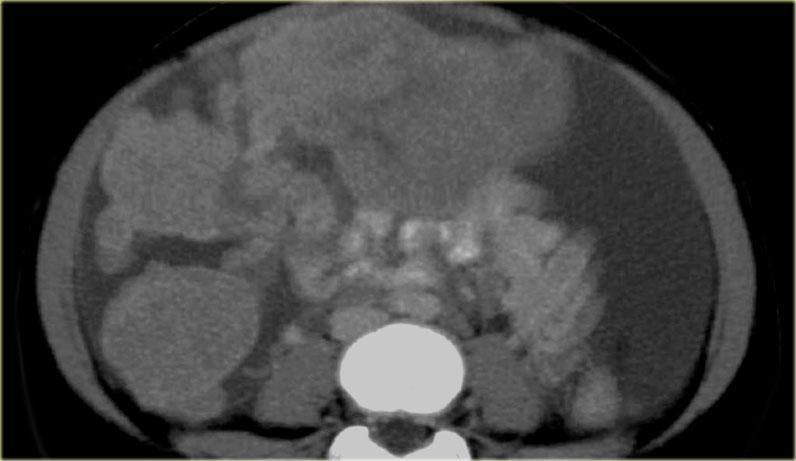
In peritoneal carcinomatosis we see tumor nodules along the peritoneal lining (arrow), omental tumor deposits, and bowel obstruction.
 Pseudomyxoma peritonei with pronounced scalloping of the liver and almost destruction of the spleen. Notice the calcifications
Pseudomyxoma peritonei with pronounced scalloping of the liver and almost destruction of the spleen. Notice the calcifications
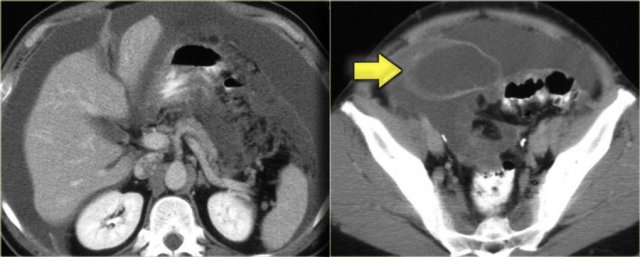
Pseudomyxoma peritonei
Pseudomyxoma peritonei is the result of a mucinous adenocarcinoma of the appendix, which presents as a mucocele and spreads to the peritoneal cavity.
It is a clinical syndrome, characterized by recurrent and recalcitrant voluminous mucinous ascites due to surface growth on the peritoneum without significant invasion of underlying tissues.
A typical feature of pseudomyxoma peritonei is scalloped indentation of the surface of the liver and spleen.
Unlike peritoneal metastases, there are no tumor nodules.
There may be some calcifications.
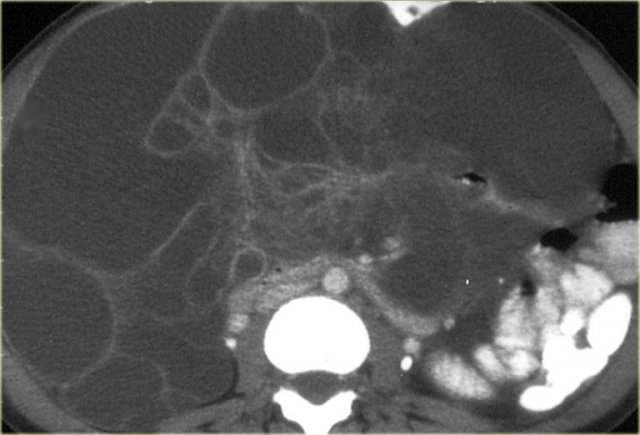
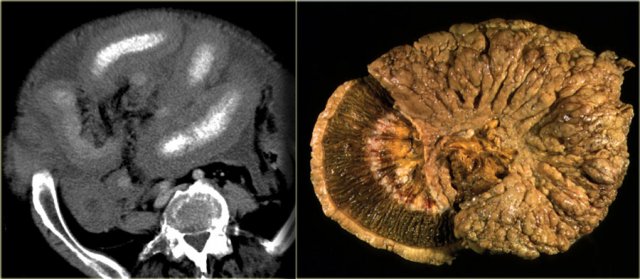
Pseudomyxoma peritonei (2)
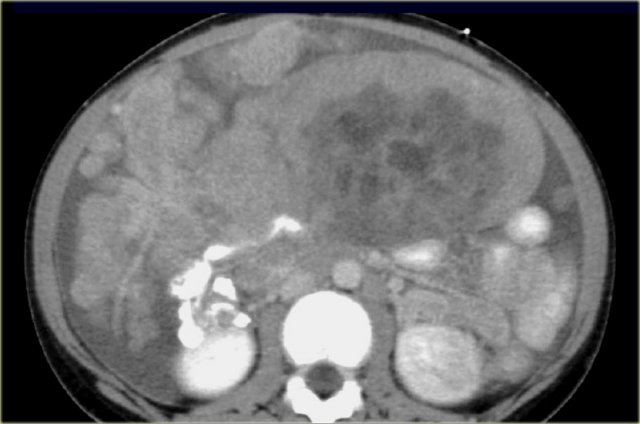
On the left another case of pseudomyxoma peritonei.
There is hardly any scalloping of the liver.
Notice the thickened falciform ligament.
There is a mucocele of the appendix (arrow).
This finding is only rarely seen.
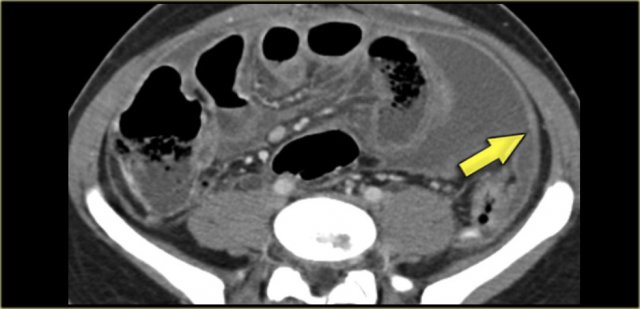
On the left another case of pseudomyxoma peritonei.
There is compression of the mesentery resulting in a thickened cake-like hyperdense mesentery (arrow).
There are also some calcifications.
Pseudomyxoma peritonei is often confused with mucinous carcinomatosis.
Unlike carcinomatosis it does not have true omental tumor deposits presenting as omental cake or peritoneal tumor deposits.
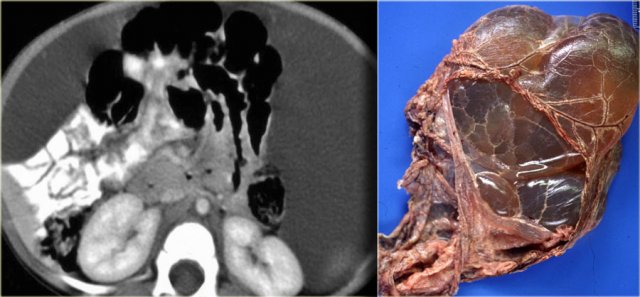
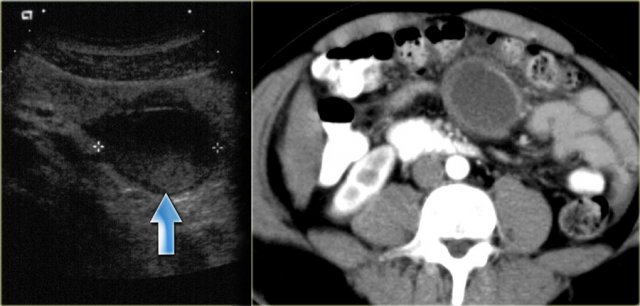
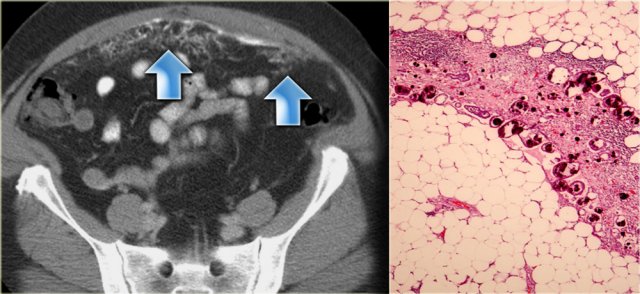
Mesenteric cyst - Lymphangioma
Mesenteric cyst is a descriptive term for any cystic lesion within the mesentery.
Usually it is a lymphangioma.
Other mesenteric cysts like enteric duplication cyst, enteric cyst, nonpancreatic pseudocyst and mesothelial cyst are very uncommon and have no specific features.
Lymphangioma is a benign lesion of vascular origin.
Most lymphangiomas are located in the neck, but 5% of lymphangiomas are abdominal.
Lymphangioma has enhancing septa.
Unlike in cystic peritoneal metastases, ascites is not a feature of lymphangioma.
When you see a septated cystic lesion without ascites the most likely diagnosis is a lymphangioma.
Lymphangioma is often closely associated with the small bowel.
At surgery it is usually very difficult to separate the tumor from the bowel and in many cases the bowel also has to be resected.
The case on the left is also a lymphangioma.
Notice that CT does not always appreciate the septations, although the specimen clearly shows multiple septations.
Ultrasound or MR depict these septations better than CT.
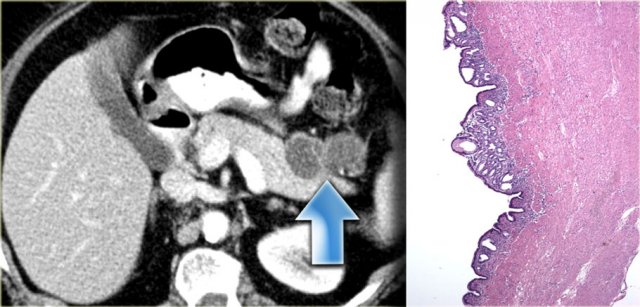
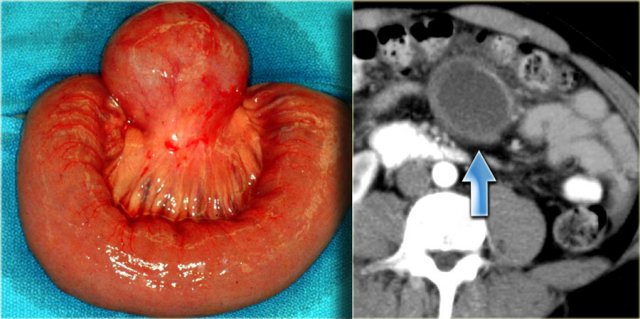
Enteric Duplication Cyst
Enteric duplication cyst is a cyst with a wall that has all three layers of the bowel wall, i.e. mucosa, submucosa and muscularis propria.
Although we commonly think of duplication cysts when we see a cystic mass adjacent to the bowel, we have to realize, that these are rare lesions.
They may occur anywhere in the mesentery, so either adjacent to or away from the bowel.
On the left an enteric duplication cyst.
It is located in the transverse mesocolon.
This patient was suspected of having a cystic pancreatic tumor.
The specimen demonstrates all the bowel wall layers.
Nonpancreatic Pseudocyst
Nonpancreatic pseudocyst is a residual of an old hematoma or infection.
Most of these patients have a history of prior abdominal trauma.
Often there is a thickened wall and there can be some debris within the lesion.
The patient on the left had had a car accident eight months before.
This is probably an old mesenteric hematoma as a result of a lap belt injury.
Notice the thickened wall on the CT and the debris on the ultrasound.
On the left a specimen and CT image of a nonpancreatic pseudocyst.
Notice the thick wall.
Probably this is an old hematoma or abscess.
You can suggest this diagnosis when you have a positive history and you see this thickened wall or debris.
Enteric cyst and mesothelial cyst
These are also mesenteric cysts. They are rare and have nonspecific imaging features. The case on the left was diagnosed as a lymohangioma, simply because a lymphangioma is by far the most common mesenteric cyst. At surgery this was a mesothelial cyst.
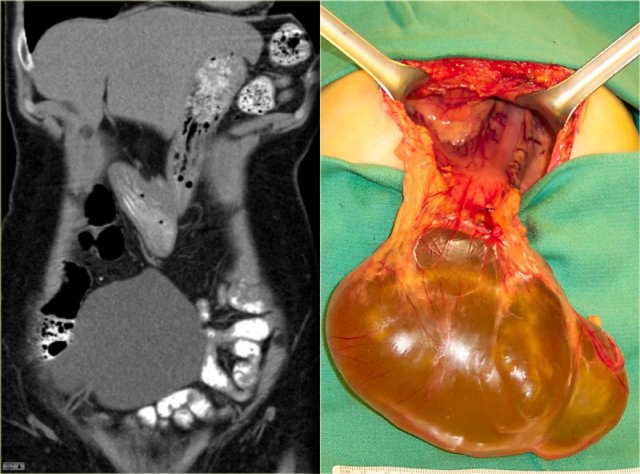
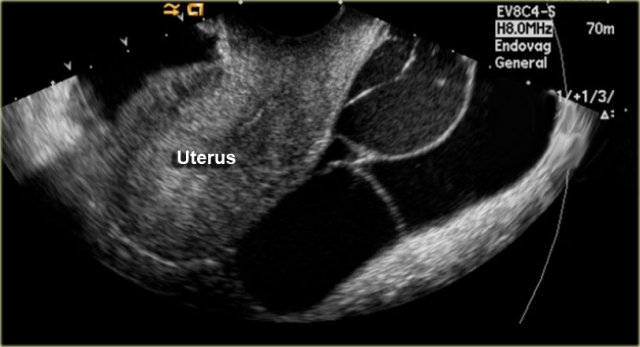
Peritoneal Inclusion Cyst
Also called Multilocular peritoneal inclusion cyst or Benign cystic mesothelioma.
This is an uncommon benign primary peritoneal tumor that has no relation with the malignant mesothelioma.
It occurs in premenopausal women with prior gynaecological surgery or infection that results in peritoneal scarring.
The hormonally active ovaries secrete fluid that becomes loculated in the pelvis.
The imaging features of a peritoneal inclusion cyst are non-specific except that it has to be located in the pelvis:
- Multicystic pelvic mass
- Enhancing septa
- Peritoneal surfaces of uterus, bladder
- May extend into upper abdomen
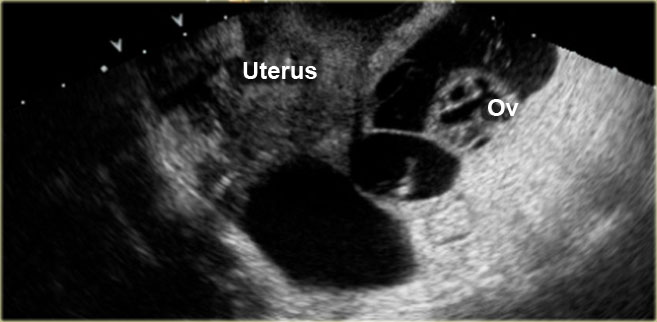
On the left a transvaginal ultrasound demonstrating a multicystic pelvic lesion next to the uterus, which proved to be a peritoneal inclusion cyst.
Sometimes the ovary is seen 'trapped' with the septate fluid collection (figure).
Peritoneal inclusion cyst (2)
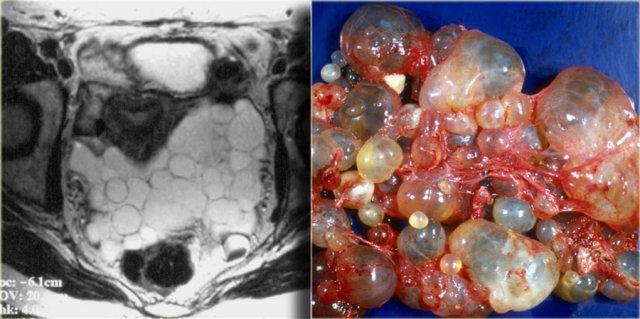
When these peritoneal inclusion cysts become very large, they may extend into the upper abdomen as is seen in the case on the left.
Notice that the left ovary is encircled by the cyst (arrow).
There are also some enhancing septa.
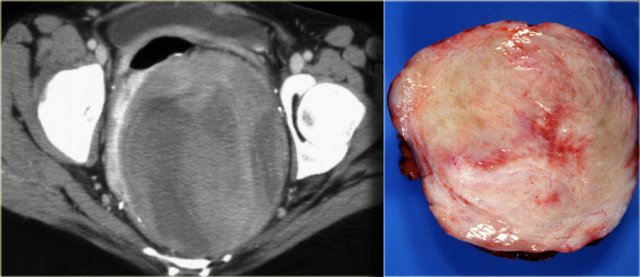
Peritoneal inclusion cyst (3)
On the left another example of a peritoneal inclusion cyst.
There is a nice correlation between the MR and the specimen.
Peritoneal inclusion cyst (4)
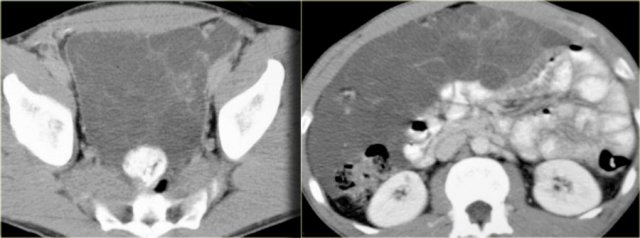
On the left images of a male patient, who presented with a lower abdominal mass.
There is a multi-cystic mass extending from the pelvis along the right paracolic gutter to the upper abdomen.
In a male patient this is a very uncommon diagnosis.
These images look quite similar to images of a pseudomyxoma peritonei which was discussed before.
In peritoneal inclusion cysts however, you will not see scalloping of the surface of the liver.
Tuberculosis
TB can produce very thick ascites, that can be loculated in distribution.
Because of this, it can simulate a cystic lesion..
Usually there is accompanying abnormality of the terminal ileum and lymphadenopathy.
The lymph nodes most often are of low attenuation (caseated).
So these are the things to look for.
On the left another image of the same patient.
In TB the peritoneum is usually very thick (arrow).
Echinococcal Cyst
It is unusual for an echinococcal cyst to be located in the peritoneum.
It favors the liver, the spleen and even the kidney over the peritoneum.
On the left we see cysts in the peritoneum and in the spleen.
Notice the daughter cysts as small dark lesions within the large peritoneal cyst (arrows).
In the pelvis additional echinococcal cysts are seen.
Solid Masses
Peritoneal metastases
Peritoneal metastases are the most common peritoneal solid masses.
Gastrointestinal and ovarian cancers are the most common etiologies.
Usually there are omental metastases, i.e. omental cake and ascites.
On the left a CT demonstrating omental cake in a patient with ovarian cancer.
On the left a patient with a lung carcinoma.
This solitary solid mass was found in the pelvis.
Based on the history this was suspected to be a metastasis.
Other solitary solid tumors like ... can have the same presentation.
Biopsy is needed to make the diagnosis.
This proved to be a metastasis of the lung carcinoma.
Lymphoma
NHL is the most common cause of lymphadenopathy.
Usually there are other sites with lymphoma.
The CT attenuation at diagnosis is very homogeneous in most cases with minimal to no enhancement.
Heterogeneous attenuation is seen only in cases with aggressive histology.
During treatment the attenuation becomes heterogeneous as a result of necrosis and fibrosis.
Calcification may occur.
Carcinoid
Carcinoid is a slow-growing neuroendocrine tumour most commonly found in the small bowel.
Less than 10% of patients with carcinoid will develop the carcinoid syndrome, caused by the overproduction of serotonin, which can lead to symptoms of cutaneous flushing, diarrhea and bronchoconstriction.
Carcinoid metastasizes to the mesentery, which at times is easier to appreciate than the primary tumor in the small bowel.
There is associated bowel wall thickening due to a desmoplastic reaction.
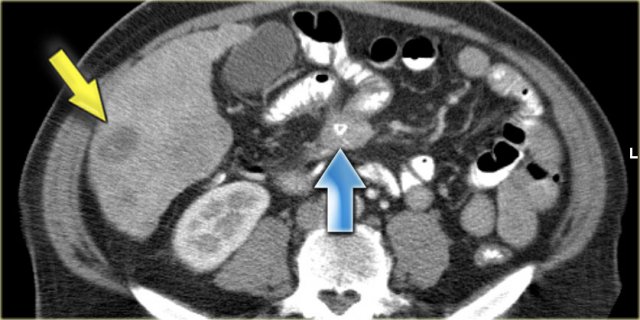
On the left a patient with a typical carcinoid with central calcification (blue arrow).
Notice the bowel retraction and wall thickening.
There is a metastasis in the liver (yellow arrow).
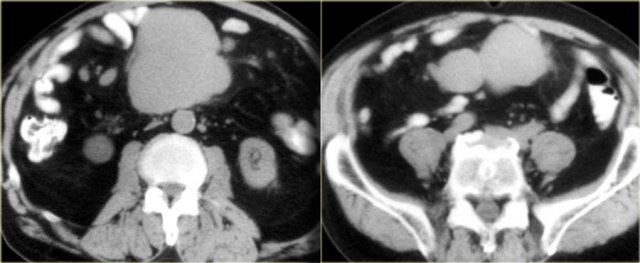
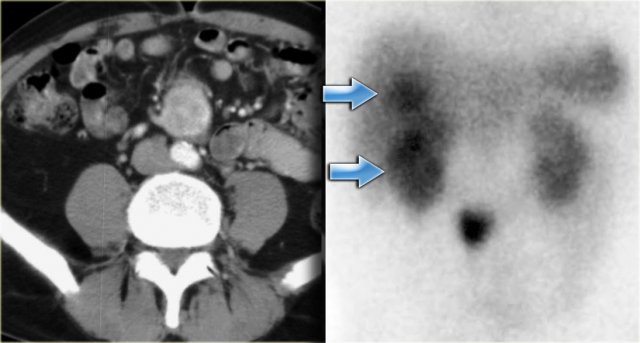
On the left another patient with a carcinoid.
The right image is the octreoscan, which is positive in 85% of carcinoids, so this can be a great help in the differential diagnosis.
In this case we can also detect liver metastases on the scan (blue arrows).
Notice that there is no activity of a primary tumor in the small bowel.
This is often the case because the primary tumor can be quite small.
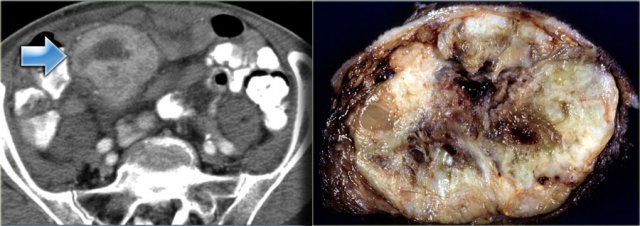
Gastrointestinal Stromal Tumor - GIST
Primary small bowel tumors can extend into the mesentery and the typical example of that is the GIST.
You can have a large mesenteric component and such a small attachment to the bowel, that you may not appreciate it.
On CT they are of mixed density due to necrosis and hemorrhage and they tend to be well vascularized, so they will enhance like the case on the left.
Inflammatory Pseudotumor
This disease can affect lung, orbit and mesentery.
Inflammatory pseudotumor is a diagnosis by exclusion.
Usually the diagnosis is made at surgery or biopsy.
It is the result of chronic inflammation with an unclear pathogenesis.
Probably it is an occult infection due to minor trauma or post surgical.
Mesenteric fibromatosis - Desmoid
Mesenteric fibromatosis is also known as intra-abdominal fibromatosis, abdominal desmoid or desmoid tumor.
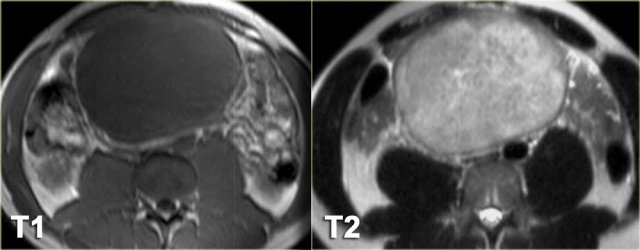
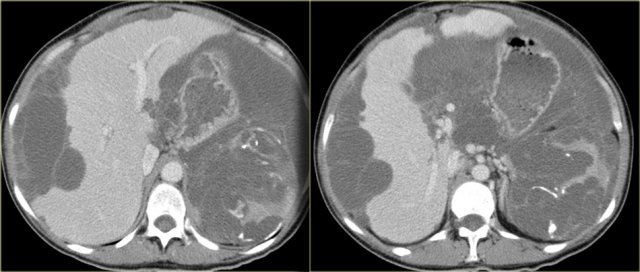
On the left a 33-year-old man who complains of an increasing abdominal girth, abdominal fullness, and a palpable abdominal mass.
First study the images on the left and continue with the MR.
Look for some imaging features that are helpful in the differential diagnosis.
First of all this is a well circumscribed lesion with a low density on CT.
There is some enhancement around the lesion and there are some small strands of enhancement within the lesion.
On MR there is a low signal on T1 as we would expect.
On T2 there is relatively high signal.
In combination with the low density on CT this tells us that there is mucin within the lesion.
This finding is very suggestive of the diagnosis of mesenteric fibromatosis.
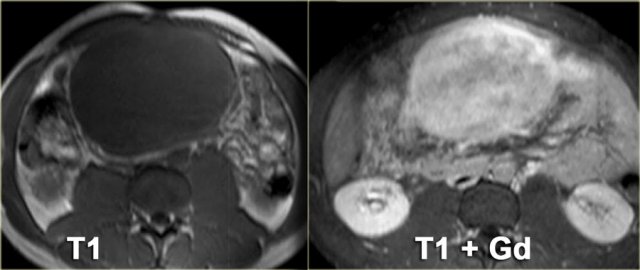
Mesenteric fibromatosis - Desmoid (2)
The enhancement on MR is more intense compared to the enhancement on CT.
On CT the low density of the mucin stands out, but on MR we can appreciate the enhancement better.
It tells us that the lesion is well vascularized.
Mesenteric fibromatosis or desmoid is a benign proliferative process that is locally aggressive and can recur, but it does not metastasize.
The small bowel mesentery is the most common site.
13% of patients have familial adenomatous polyposis (FAP).
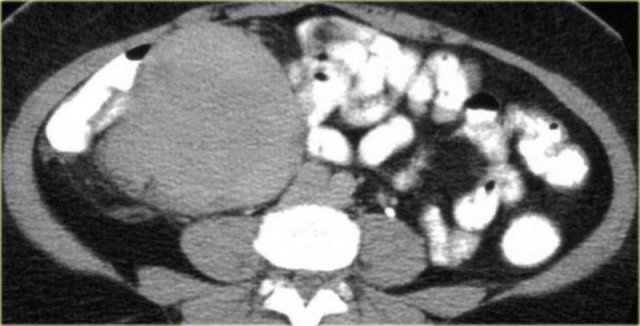
On the left images of another patient with mesenteric fibromatosis.
Notice that this lesion is not of low attenuation.
This lesion has a more collagenous or fibrous stroma.
So there are two distinct patterns.
Mesenteric fibromatosis - Desmoid (3)
On the left again a more typical case with a low density tumor located in the greater omentum (upper image) and the gastrosplenic ligament (lower image).
 Mesenteric fibromatosis arising in the mesentery of a J-pouch in a patient with familial adenomatous polyposis
Mesenteric fibromatosis arising in the mesentery of a J-pouch in a patient with familial adenomatous polyposis
On the left an unusual location, because normally there is no mesentery deep in the pelvis.
This patient had familial adenomatous polyposis.
A total colectomy with J-pouch of the ileum was performed.
Now accompanying that J-pouch is mesentery in which mesenteric fibromatosis has developed.
Notice the low attenuation foci or bands of myxoid stroma within the tumor.
In familial adenomatous polyposis the mesenteric fibromatosis is almost always post operative and occurs at the operative sites.
It frequently occurs at multiple sites including abdominal wall fibromatosis.
These cases can be very aggressive.
It usually comes back and when it does, it comes back as a more aggressive tumor.
Therfore these patients are treated as conservatively as possible.
Sclerosing Mesenteritis
This disease has multiple synonyms reflecting the wide histologic spectrum: mesenteric panniculitis, fibrosing mesenteritis and mesenteric lipodystrophy.
Pathologically it is a chronic inflammation of unknown etiology.
This entity is more common than previously thought.
The signs and symptoms are variable.
Patients present with pain, a palpable mass or bowel complications, but in many cases it is an incidental finding on CT made for other reasons.
The image on the left is the form that we most frequently see in patients that are screened for other reasons.
This form is mostly named panniculitis mesenterialis.
In a more advanced stage you can have significant fibrosis resulting in retraction of the small bowel.
Within these masses dystrophic calcifications can be seen as well as lucent areas of fat (arrow)
Sclerosing mesenteritis (2)
On the left a nice radiological pathological correlation.
Notice the retraction of the bowel and also notice the resemblance to carcinoid.
In these cases the octreoscan can be a great help in the differential diagnosis.
These lesions are situated in the root of the mesentery and this makes a surgical procedure extremely difficult.
These lesions are treated conservatively with immunosuppressiva, anti inflammatory drugs and sometimes anti-estrogens as long as possible.
Malignant mesothelioma
Malignant mesothelioma is one of the primary peritoneal malignancies (Table on the left).
Suggestive features are a sheet-like peritoneal thickening and absence of lymphadenopathy.
Just like pleural mesothelioma, it is associated with asbestos exposure.
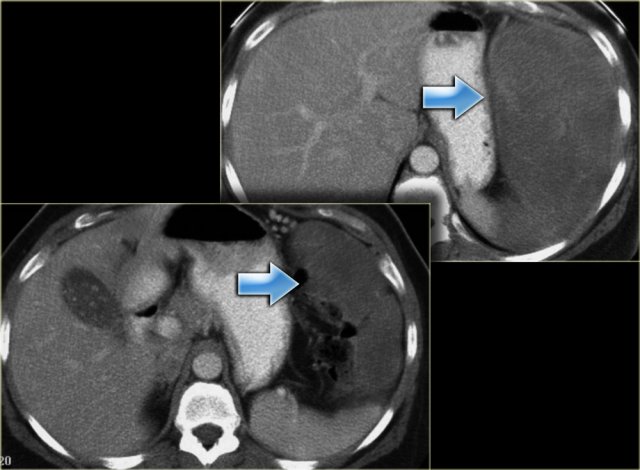
On the left a patient with malignant mesothelioma.
Notice the sheet-like thickening of the peritoneum.
The diagnosis was suggested because of the pleural calcifications.
Malignant mesothelioma (2)
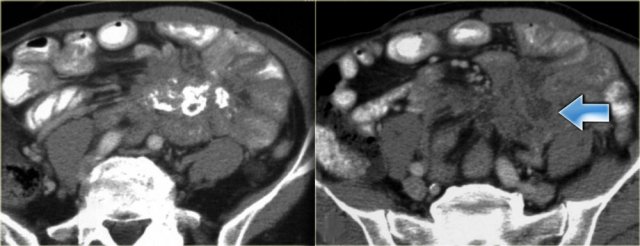
In advanced cases you will see encasement of the intra-peritoneal structures.
In the case on the left there is besides encasement of the bowel and the liver, also encasement of the mesentery.
On the left a rad-path correlation of the same case.
Primary Peritoneal Serous Carcinoma
This tumor is also one of the primary peritoneal malignancies.
It occurs exclusively in women.
This tumor is histologically identical to malignant ovarian surface epithelial tumors.
It was once thought to be very rare, but now almost one third of tumors previously diagnosed as ovarian cancer are diagnosed as primary peritoneal serous carcinoma.
Consider this diagnosis when:
- Ovaries are normal or
- Involvement of extraovarian sites is greater than that of the ovarian surface or
- If ovaries are involved, yet disease is confined to the surface epithelium
As a radiologist you should consider this diagnosis if you think of metastatic ovarian cancer but the ovaries are normal.
On the left a typical case.
There is ascites and omental involvement, so your first thought is ovarian cancer, but the ovaries were normal.
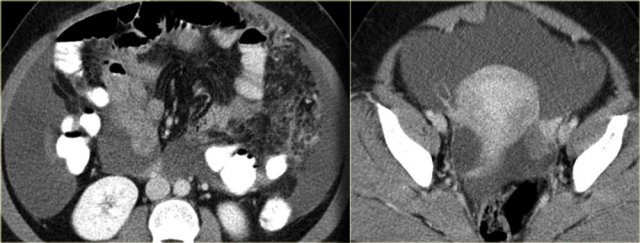
Desmoplastic Small Round Cell Tumor
This tumor is also one of the primary peritoneal malignancies.
It is a rare malignancy of uncertain origin.
It occurs primarily in young men with a mean age of 19 years.
Consider this diagnosis if you see something that looks like peritoneal carcinomatosis in a young man that has no history of a primary malignancy.
It is a very aggressive tumor with a poor prognosis.
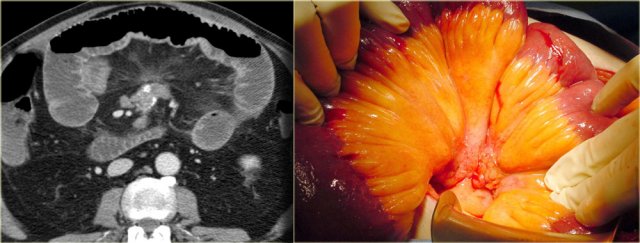
Desmoplastic small round cell tumor begins as a dominant mass and then multiple masses occur within the peritoneum (figure).
At this stage it is no different upon imaging to other tumors, however, the age of the patient provides the clue to the diagnosis.
NHL would be number one in the differential diagnosis of these images.