Shoulder Ultrasound 2.0
Mohamed Salah Ayyad, Alrawy Ali Mohammad and Khaled Taha
Radiology department of the faculty of Medicine - Mansoura University, Egypt.
This article is an introduction to ultrasound of the shoulder.
Ultrasound is a simple and readily available imaging modality to examine the shoulder and it also allows a dynamic examination in patients with impingement.
We will discuss the sonographic anatomy of the shoulder, the examination protocol with patient positioning and common pathology.
Anatomy
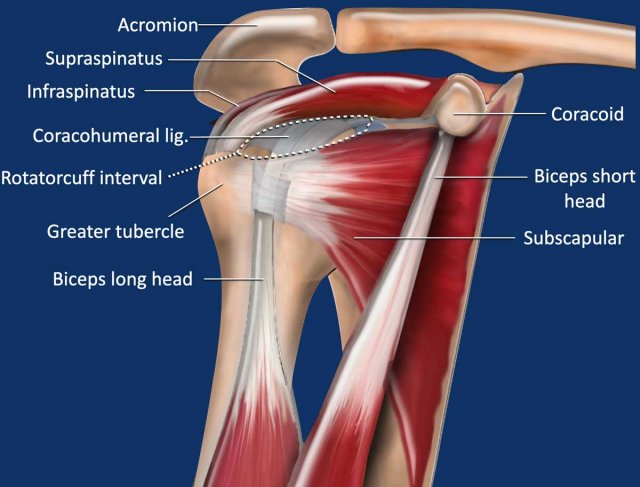
An important stabilizer of the glenohumeral joint is the rotator cuff formed by the subscapular tendon anteriorly, the supraspinatus tendon superiorly and the infraspinatus and teres minor tendon posteriorly.
Of these latter two tendons, only the infraspinatus tendon is partly shown in this illustration.
The rotator cuff interval is the gap in the rotator cuff between the subscapular and supraspinatus tendon.
Here the humeral head is not covered by the rotator cuff, but by the intra-articular portion of the long head of the biceps tendon, which is covered by the coracohumeral ligament.
The normal anatomy is also discussed here.
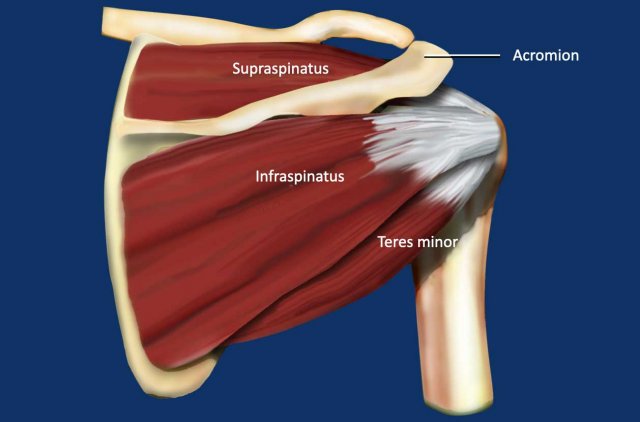
This is a posterior view of the shoulder demonstrating the supraspinatus, infraspinatus and teres minor muscle and tendon.
Standard Ultrasound Examination
A high-resolution linear probe (≥10 MHZ) is used.
In addition sometimes a curvilinear probe (3.5 MHZ) is used to examine the glenohumeral joint as a whole.
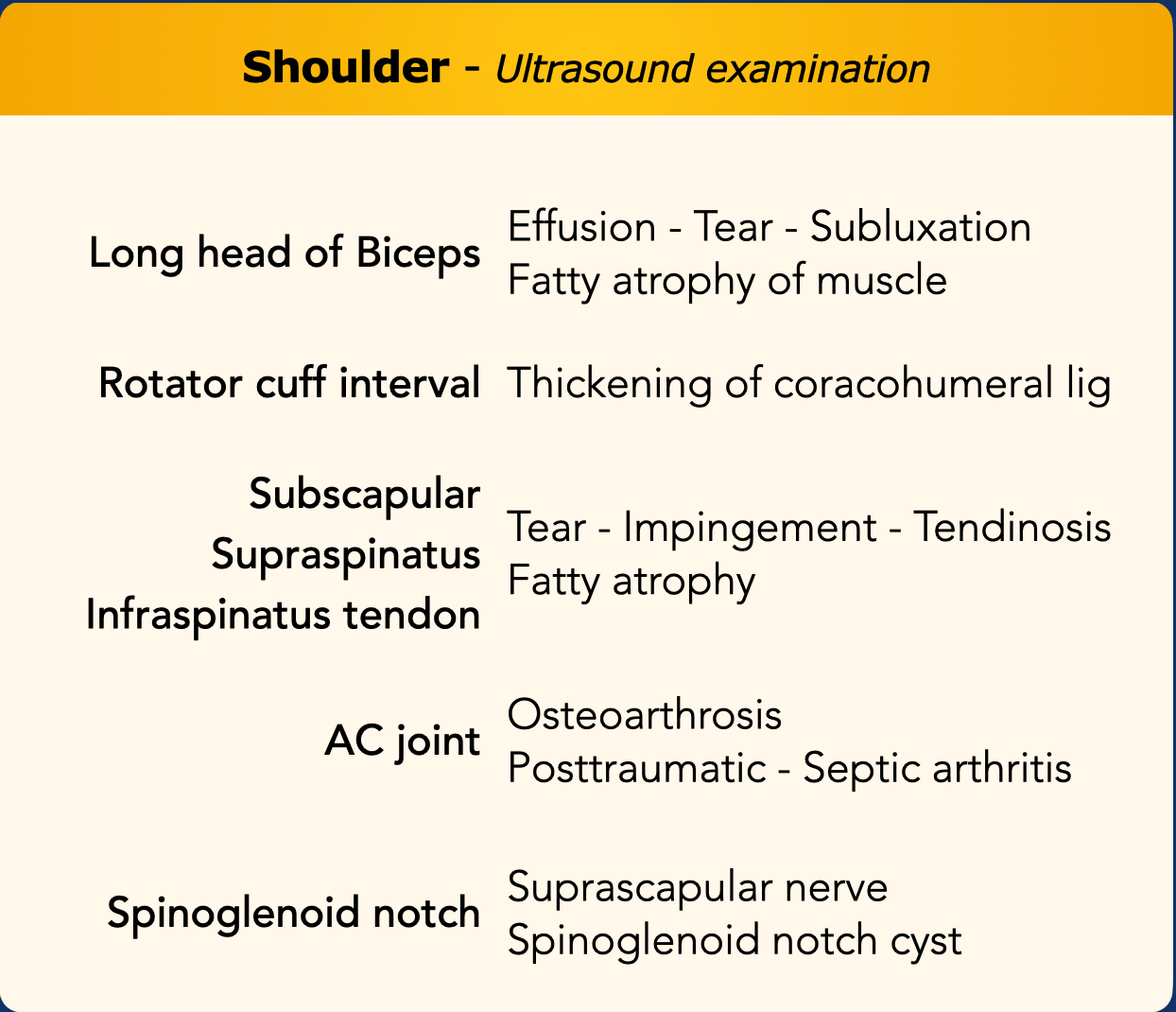
The usual order of examination is first to look at the tendon of the long head of the biceps to look for effuson, a tear or subluxation of the tendon.
Sometimes fatty atrophy can be seen of the muscle or at the myotendinous junction.
Then study the tendons of the subscapular, supra- and infraspinatus muscle and especially look for tears.
You can expand the examination with a study of the AC-joint, spinoglenoid notch, posterior labrum and glenohumeral joint.
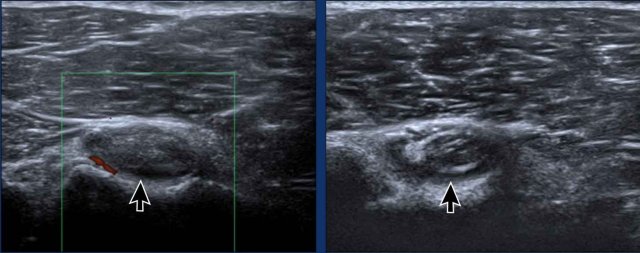
Anisotropy
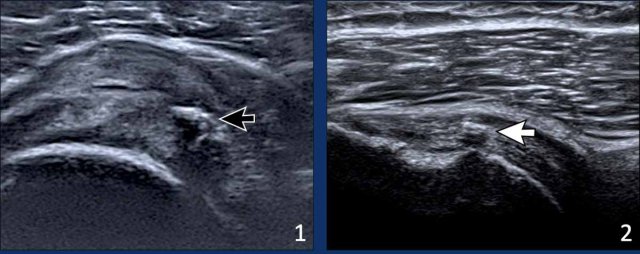
When the direction of the ultrasound beam is not perpendicular to the LHB, you will get less reflection of sound waves.
This can result in anisotropy.
This artifact refers to a darkening and loss of resolution of the structure, that you are examining (black arrow).
You may even get the impression, that the LHB is not within the groove and maybe dislocated.
By repositioning the transducer to perpendicular the normal echogenic LHB will appear (white arrow).
Notice that in this image the subscapular tendon also appears anechoic due to this effect.
Rotator cuff interval
The rotator cuff interval is the area where the humeral head is not covered by the rotator cuff.
It is located between the anterior edge of the supraspinatus tendon and the superior edge of the subscapularis tendon and the main structure in this area is the long head of the biceps.
The biceps tendon is stabilized by a capsuloligamentous complex, which is called the biceps pulley.
It is composed of the superior glenohumeral ligament, the coracohumeral ligament and the distal attachment of the subscapularis tendon (figure).
Normal Subscapular movement
During internal and external rotation of the forearm, the whole tendon should be seen sliding under the coracoid (see video).
Impingement is noted when there is incomplete or delayed passage of the tendon underneath the coracoid (see impingement).
Acromioclavicular joint
The acromioclavicular joint is easily appreciated by palpating the bony projection and then placing the probe over it.
The articulation should be uniform with no cortical irregularity and no bulging cartilages above the articulation between the two bony structures (Figure).
A normal acromioclavicular joint shows a smooth contour of the bony articular surfaces.
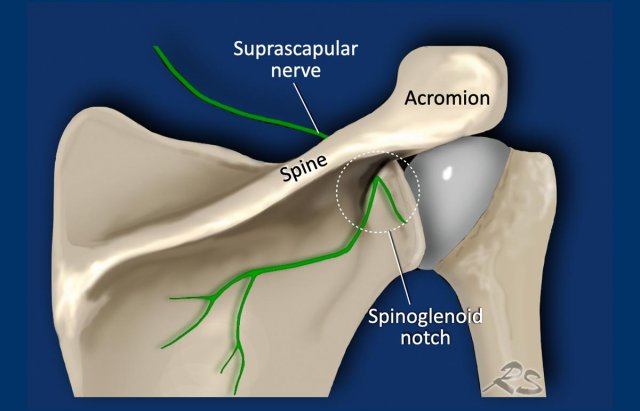
Spinoglenoid notch
The spinoglenoid notch is the area located between the lateral base of the scapular spine and the glenoid process of the scapula.
It connects the supraspinatus fossa with the infraspinatus fossa and allows passage for the suprascapular nerve and artery.
In this area ganglion cysts can arise compressing the nerve resulting in shoulder pain and infraspinatus atrophy.
These cysts are caused by tears in the posterosuperior glenoid labrum.
Pathology
Biceps tendinopathy
Images
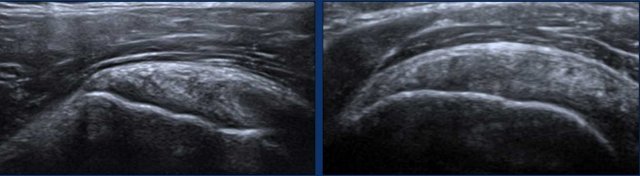
Two examples of a thickened long head of the biceps tendon.
Notice the irregular echo-pattern especially on the image on the right.
There is hypervascularity and some surrounding fluid (arrows).
Tear of the long head of the biceps (LHB)
The most common site of LHB injury is the myotendinous junction and
the adjacent part of the tendon.
The
LHB tears are easily appreciated as anechoic fluid interrupting the muscle fibres.
The echogenicity varies with the age of the injury.
Acute tears are usually
anechoic, while chronic tears may show reflective echoes within the fluid.
Images
Two examples of tears at the myotendinous junction of the LHB.
The tear is
completely anechoic suggesting an acute tear.
Biceps (sub)luxation
The LHB tendon should be centralized within
the bicipital groove.
Eccentric location denotes laxity or rupture of the biceps pulley.
Rotator cuff tears
Partial thickness tears involve only a part of the tendon and do not involve the full thickness.
It can be located on the articular or on the bursal side (figure).
An intrasubstance tear is also a partial thickness tear.
Full thickness tears can be complete or may involve only a part of a tendon.
This is called an incomplete full-thickness tear and is just like a hole in a tendon (figure).
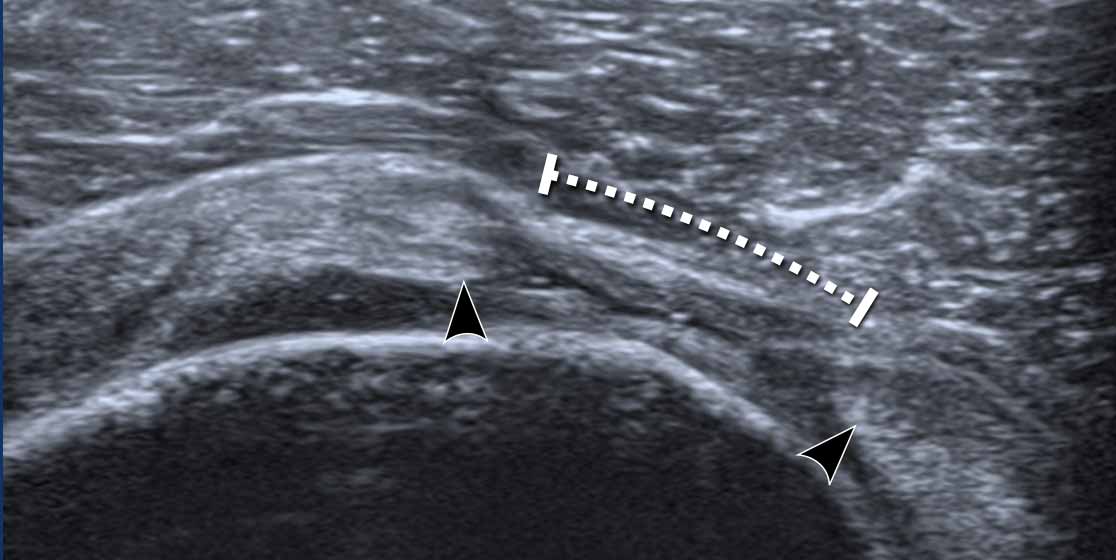
Full thickness tears
This image shows a complete full thickness tear of the supraspinatus tendon.
There is a small hypoechoic fluid collection.
Both tendon edges are blunt and retracted (arrowheads).
Here another example of a ful thickness tears of the supraspinatus tendon.
The gap is filled with some fluid from the glenohumeral joint (arrow)
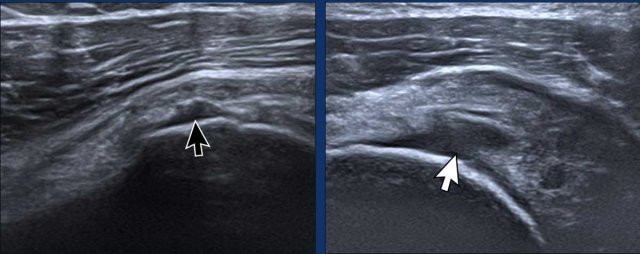
Partial thickness tears
Here two examples of a partial tear on the articular side.
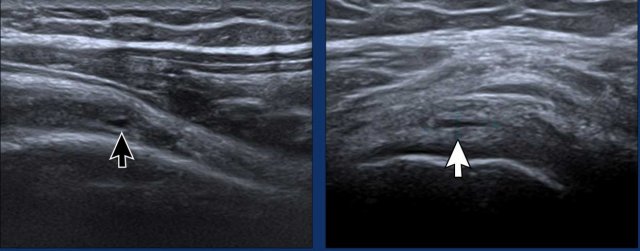
Intrasubstance tears
Intrasubstance tears are partial tears that do not extend to the articular or bursal surface of the tendon.
The images show two examples of a small intrasubstance tear.
Impingement
Subscapular impingement
During endorotation a normal subscapular tendon should show almost complete passage underneath the coracoid process.
Impingement is suspected when a residual portion of the tendon is still visible during maximum endorotation.
Images
During endorotation there is incomplete passage under the coracoid and buckling of the subscapular tendon.
A dynamic scan of the subscapularis also gives an idea of the intimate relation with the coracohumeral and glenohumeral ligaments which stabilize the long head of the biceps.
Supraspinatus impingement
This is usually a result of acromion pathology and chronic muscle insult.
Impingement can be suspected when there is a residual portion of the tendon, that does not slide under the acromion during maximum abduction.
Tendinosis
The term tendinosis is used rather than tendinitis because there is no active inflammation, but instead it is a degenerative process with mucoid degeneration.
The tendon is frequently thickened and may show hypoechoic striated areas.
Images
Calcific tendinopathy
Calcific tendinopathy develops when calcium deposits build up in the tendons.
It most commonly affects the tendons of the rotator cuff of the shoulder.
These deposits can become inflamed and cause pain.
Images
- Markedly thickened supraspinatus tendon with chunky calcifications casting extensive posterior shadow.
- Small calcification in the supraspinatus tendon.
Bursitis
Normally the bursal space is collapsed and barely distinguishable by ultrasound (arrows)
Acute bursitis appears sonographically as
distension of the bursa (yellow arrow).
Chronic bursitis may
show a thick wall (white arrow).
AC pathology
Osteoarthrosis
Recognizing symptomatic
osteoarthrosis of the AC joint is challenging, as the radiographic and ultrasound findings of joint degeneration are ubiquitous in adults and correlate poorly with symptoms.
Images
Osteoarthrosis of the AC joint with cortical irregularity and bulging of the capsule.
AC-arthritis
This image is of a 19-year-old male athlete who sustained an injury during a wrestling match.
There were no signs of septic arthritis and he was diagnosed with post-traumatic arthritis.
He improved with anti-inflammatory medication and rest.