Biliary duct pathology
Angela D. Levy MD
Chief Gastrointestinal Radiology, University Department of Radiologic Pathology, Armed Forces Institute of Pathology, Washington DC
Publicationdate
This review is based on a presentation given by Angela Levy and adapted for the Radiology Assistant by Robin Smithuis.
We will discuss:
- Nonobstructive biliary disorders
- Obstructive biliary neoplasms
by Angela D. Levy
Introduction
Differential Diagnosis of bile duct dilatation
Whenever there is bile duct dilatation, the first priority is to look for obstruction.
Obstruction
If there is an obstruction, we first look for gallstones in the bile duct.
If there are no gallstones involved, we then look for strictures.
The differential diagnosis for a stricture is based on the location.
- A distal stricture is most likely the result of a distal cholangiocarcinoma, pancreatic carcinoma or pancreatitis.
- A stricture within the liver is likely due to gallbladder carcinoma or inflammatory strictures like PSC (Primary Sclerosing Cholangitis) or AIDS cholangiopathy.
- Metastatic disease can occur anywhere within the bilairy system.
No Obstruction
Once we have excluded obstruction, we have to think about nonobstructive biliary diseases like:
- Caroli disease
- Choledochal cyst
- Recurrent pyogenic cholangitis
- Primary sclerosing cholangitis
Caroli Disease
Caroli disease is an autosomal recessive disease secondary to the ductal plate malformation.
It is associated with polycystic kidney disease, medullary sponge kidney and medullary cystic disease.
So looking at the kidneys can sometimes help you make this diagnosis.
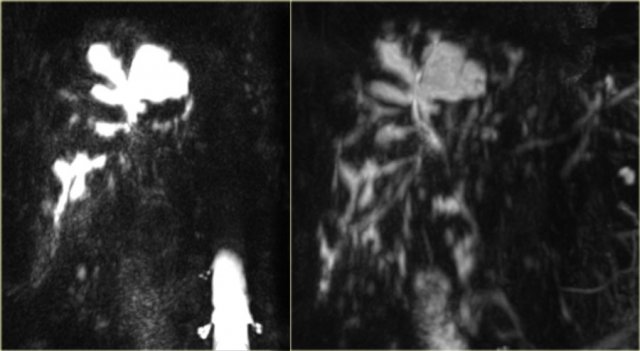
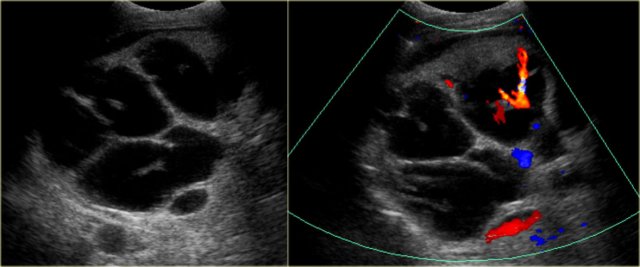
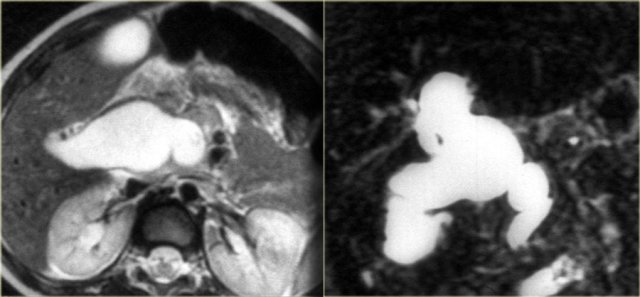
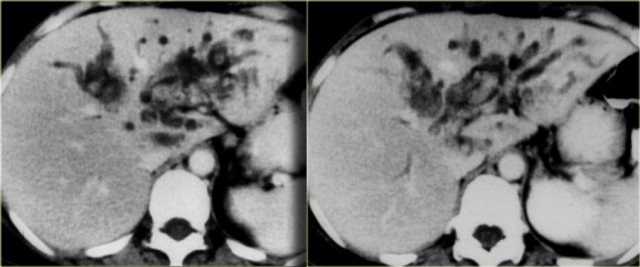
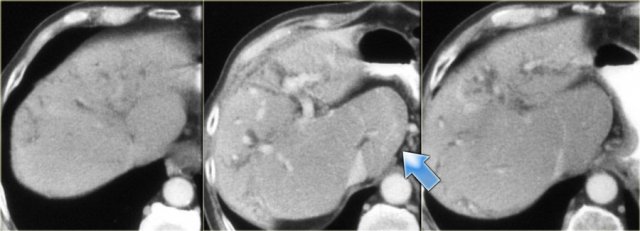
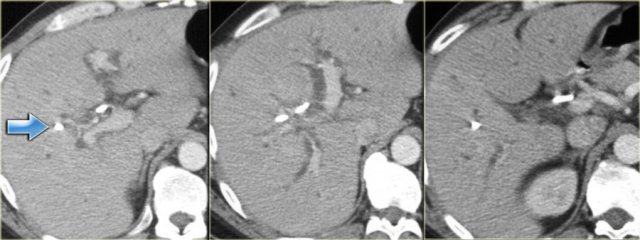
On the left we see images of a patient with Caroli disease.
Notice the intrahepatic duct dilatation and the normal caliber of the choledochal duct (extrahepatic bile duct).
The hallmark of Caroli disease is intrahepatic duct dilatation.
The dilatation can be very large and saccular as seen in the case on the left or it can be very linear.
Caroli Disease (2)
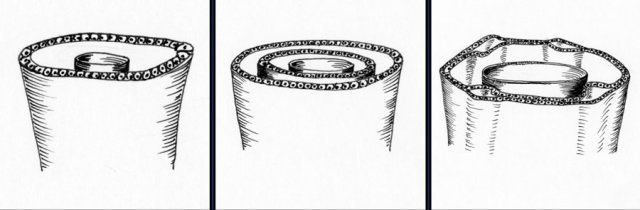
The duct dilatation in Caroli disease is due to a congenital malformation of the ductal plate, which is the precursor of the intrahepatic bile ducts.
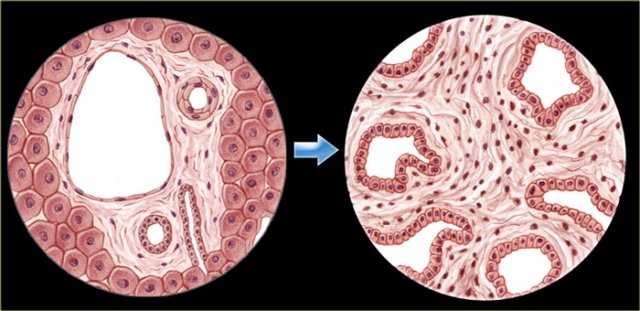
On the left we see the normal development of the ductal plate.
Embryologically each bile duct begins as a single layer of cells that surrounds a portal vein.
This layer then duplicates.
Portions of this double layer fuse and resorb leaving unfused portions that become the bile ducts.
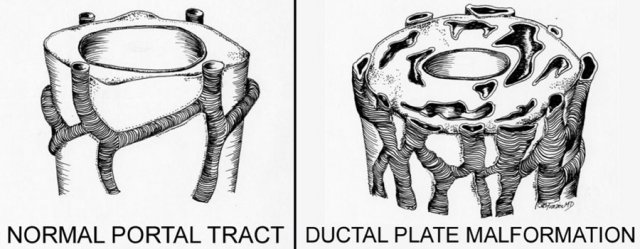
So in the normal situation each portal vein is surrounded by interconnecting bile ducts (left image).
However if the patient has ductal plate malformation, the bile ducts are too numerous and they are ectatic (right image).
Whether or not we see this on imaging depends on which portion of the bile ducts is affected.
If the large ducts are involved, we see this as Caroli disease.
However if only the very small ducts are involved, the result is congenital hepatic fibrosis.
If all ducts are involved, then there is a combination of fibrosis and Caroli disease, which is also known as the Caroli syndrome.
Central dot sign
Most commonly the intrahepatic duct dilatation is segmental (83%) in distribution.
The diffuse form is less common (17%).
The shape of the dilatation is saccular in 76% or fusiform in 24% of the cases.
A very important sign is the central dot sign.
The central dot corresponds to the portal vein that is surrounded by dilated bile ducts.
On the left we see a dot within the dilated ducts.
When we put on the color doppler, we will notice that these structures contain blood flow and represent portal veins.
Caroli Disease (3)
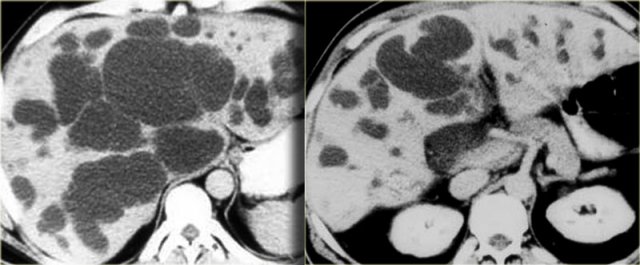
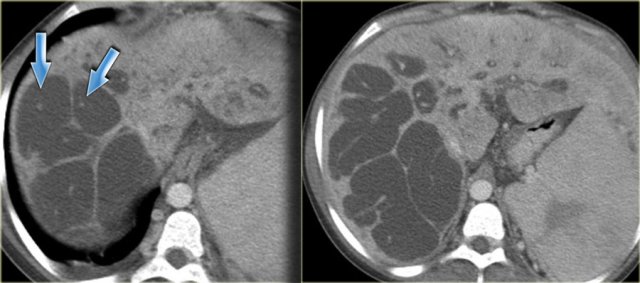
On the left CT-images of the same patient.
Notice the central dot sign and the segmental involvement.
This patient has cirrhosis with splenomegaly due to portal hypertension.
Extrahepatic duct dilatation is present in 53% of cases, secondary to cholangitis and stone or sludge passage.
These are secondary findings, that are not part of the primary disease.
When there is extensive fibrosis, these patients can develop cirrhosis over time.
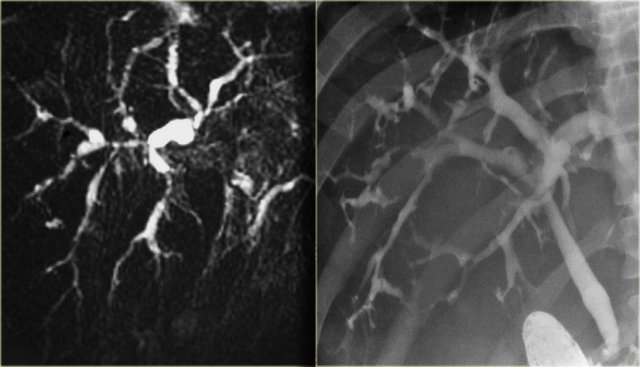
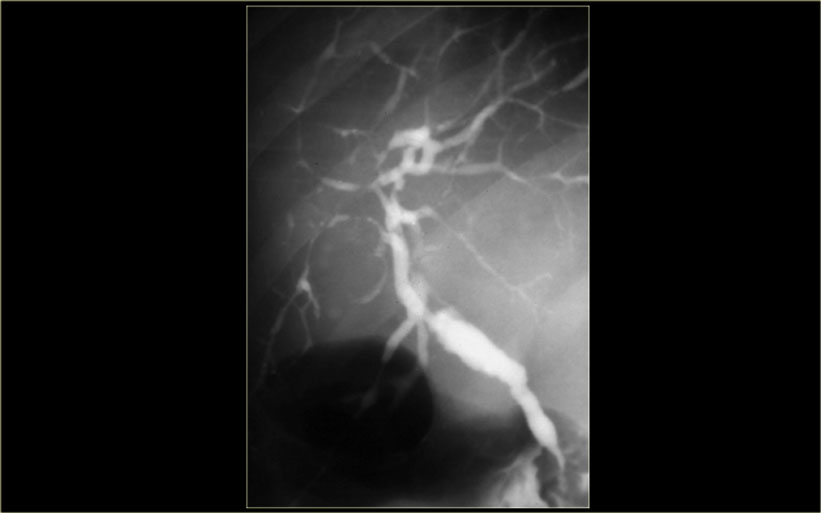
 ERCP: Caroli disease with severe intrahepatic duct dilatation. No obstruction. Mild dilatation of the choledochal duct due to cholangitis
ERCP: Caroli disease with severe intrahepatic duct dilatation. No obstruction. Mild dilatation of the choledochal duct due to cholangitis
Caroli Disease (4)
The cholangiogram is important in the work up of these patients, because obstruction has to be excluded.
This can be done with MRCP or ERCP, as is shown on the left.
There was no sign of obstruction.
The mild dilatation of the choledochal duct was the result of cholangitis.
Study the image on the left.
Then continue reading.
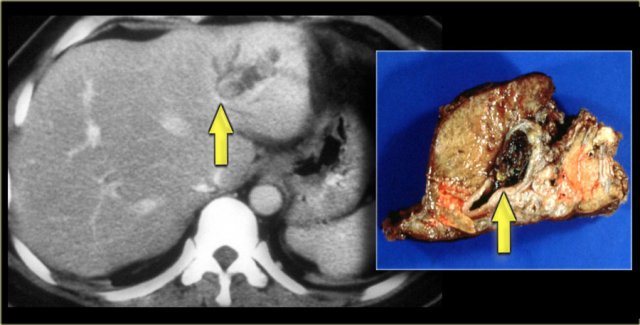
There is focal dilatation with intermixing strictures of the bile ducts in segment IV (arrow).
The other bile ducts and the choledochal duct are normal.
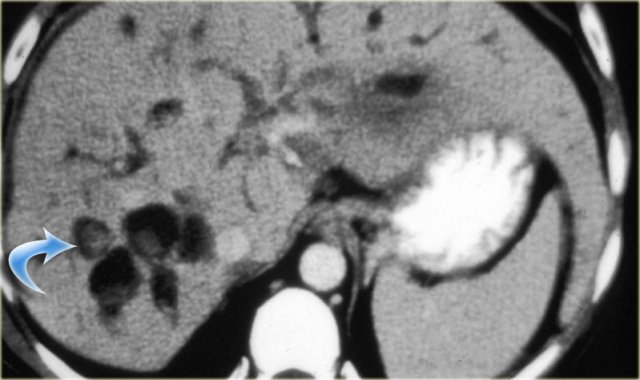
In some of the cases of Caroli disease the imaging findings may simulate a cystic neoplasm as is seen in the case on the left.
This case was originally diagnosed as a biliary cystadenoma.
However, the gross specimen demonstrates dilated bile ducts and ductal plate malformation was present microscopically.
Caroli Disease (5): Complications
Patient with Caroli disease are usually brought to our attention, when they develop complications.
These complications are commonly the result of biliary stasis, which leads to stone formation and infection.
Complications:
- Intraductal stones
- Cholangitis and Abscess
- Livercirrhosis
- Cholangiocarcinoma
On the left a patient with dilated bile ducts with intraductal stones (arrow)
Study the image on the left.
Then continue reading.
The findings are:
- Medullary sponge kidney with stone formation (red arrow)
- Mild bile duct dilatation (blue arrow)
- Round hypoattenuating mass in the right liver lobe
The mass in the right lobe of the liver turned out to be an abscess.
Remember that liver abscesses in the early phase can look quite solid.
In the differential diagnosis we would also have to include a neoplasm, because patients with Caroli disease have an increased risk of developing a cholangiocarcinoma.
Ultimately if there is substantial fibrosis and the entire liver is involved, these patients develop cirrhosis.
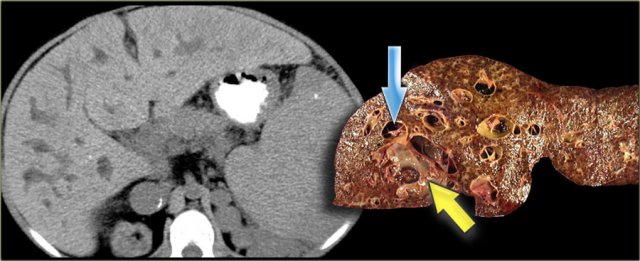
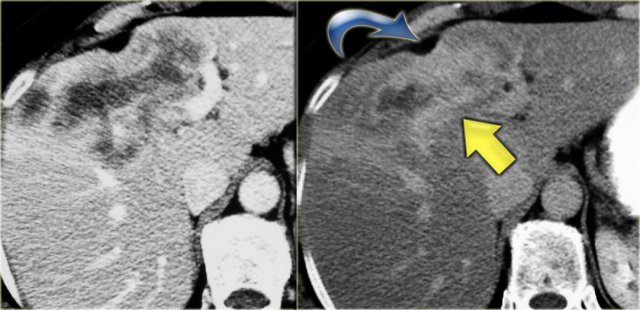
The patient on the left developed severe liver failure and a resection was performed.
Notice the intrahepatic bile duct dilatation, splenomegaly and dilated venous collaterals.
In the resected specimen there is a central dot sign (blue arrow) and a small pus collection (yellow arrow).
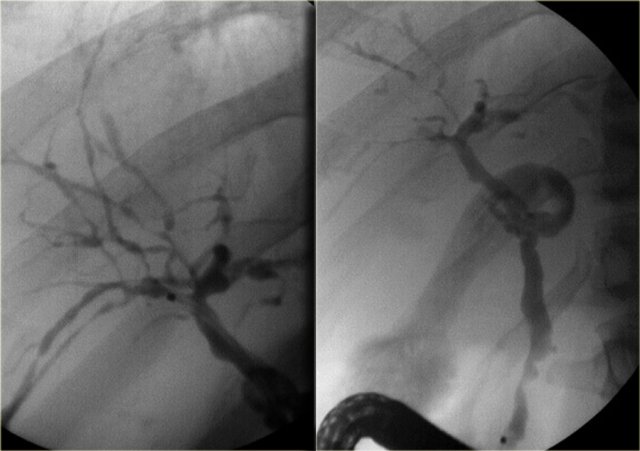
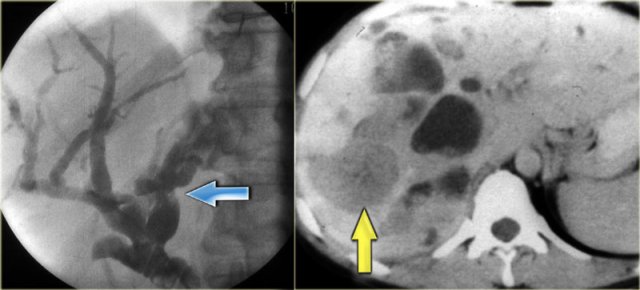 LEFT: Infiltrating cholangiocarcinoma with stricture in a patient with Caroli disease RIGHT: Intraductal cholangiocarcinoma
LEFT: Infiltrating cholangiocarcinoma with stricture in a patient with Caroli disease RIGHT: Intraductal cholangiocarcinoma
Cholangiocarcinoma can take on many forms in patients with Caroli disease.
The cholangiogram on the left demonstrates a focal stricture (blue arrow), which turned out to be a infiltrating cholangiocarcinoma.
The patient on the right has a cholangiocarcinoma in which the tumor was filling up the dilated ducts (yellow arrow).
Choledochal cyst
A choledochal cyst is a congenital dilatation of the extrahepatic bile duct.
These patients do not have a ductal plate abnormality.
The most common theory for the development of a choledochal cyst is that the dilatation is due to an underlying anomalous pancreatico-biliary junction.
In the anomalous junction the biliary and pancreatic duct join proximal to the sphincter of Oddi.
In these patients there is a long common channel.
The theory is that when the sphincter of Oddi contracts, pancreatic enzymes will flow into the bile duct and causing dilatation and in some cases, narrowing of the distal duct.
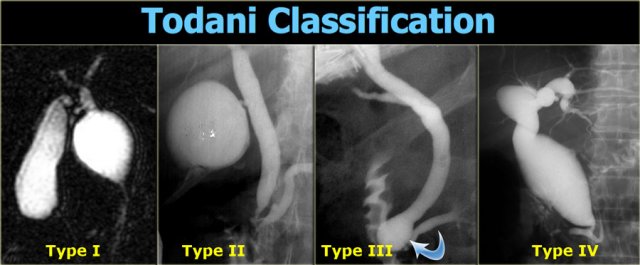
Todani Classification
This classification classifies the choledochal cysts into 5 cathegories.
Type V, which is not shown on the left is Caroli disease.
We now know, that Caroli is a different disease.
Type I is a true choledichal cyst with focal dilatation of the extrahepatic duct.
This is the most frequent type (90-95% of the cases).
Type IV is also a true choledichal cyst with dilatation of the entire extrahepatic duct with involvement of portions of the intrahepatic ducts.
The intrahepatic ducts taper normally to the periphery, indicating that there is no obstruction.
Type II and III are extremely rare and it is debatable whether or not these are true choledochal cysts.
Type II is a diverticulum of the extrahepatic duct and many believe that this entity is not related to an anomalous pancreatico-biliary junction.
Type III is a choledochocele, where there is dilatation of the distal part of the bile duct.
These patients also have a normal pancreaticobiliary junction.
Choledochal cyst (2)
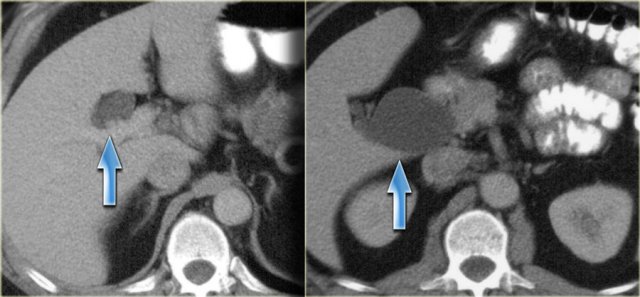
On the left a patient with dilatation of both the extrahepatic duct and part of the intrahepatic ducts.
So this is a type IV.
Notice that the peripheral ducts are normal, so this is not an obstructive pattern.
On the left another type IV choledochal cyst.
There is dilatation of the extrahepatic duct, cystic duct and a small portion of the left hepatic duct.
There is no intrahepatic dilatation.
Choledochal cyst (3)
There is an association of bile duct adenocarcinoma and choledochal cysts.
These carcinomas can occur within the choledochal cyst, like the case on the left, or in the gallbladder or anywhere else in the biliary ducts.
In the bile ducts they can present as classic peripheral cholangiocarcinoma, Klatskin tumor or distal cholangiocarcinoma.
Recurrent Pyogenic Cholangitis (RPC)
Recurrent pyogenic cholangitis is an uncommon disease in the western world.
Most of these cases are seen in Asian countries.
The etiology is unknown, although some of these patients have biliary parasites.
The disease is characterized by the presence of intrahepatic pigmented stones and recurrent infection.
These patients are also at risk of developing biliary cirrhosis and cholangiocarcinoma.
The left lobe is the most common location of the disease due to the delayed drainage of the left system.
On the left a typical case.
There is focal dilatation of the bile ducts in the left lobe with stones.
Recurrent pyogenic cholangitis (2)
On the left another example of recurrent pyogenic cholangitis.
There is intrahepatic lithiasis with focal diatation.
A case like this is indistinguishable from focal Caroli disease with secundary stone formation.
Primary Sclerosing Cholangitis
When we see intrahepatic bile duct dilatation with strictures and only mild dilatation, the first diagnosis we think of is primary sclerosing cholangitis (PSC).
We know however that there is a long differential diagnistic list which includes:
- Cholangiocarcinoma
- Metastatic disease (especially breast cancer)
- Iatrogenic bile duct strictures
- Unusual biliary tumors (granular cell tumor)
-
Secondary sclerosing cholangitis due to:
- Ischemia, for example post -Chemoembolisation
- AIDS related cholangiopathy
The case on the left nicely demonstrates the bile duct strictures.
Notice that there is only mild dilatation, which is common in PSC.
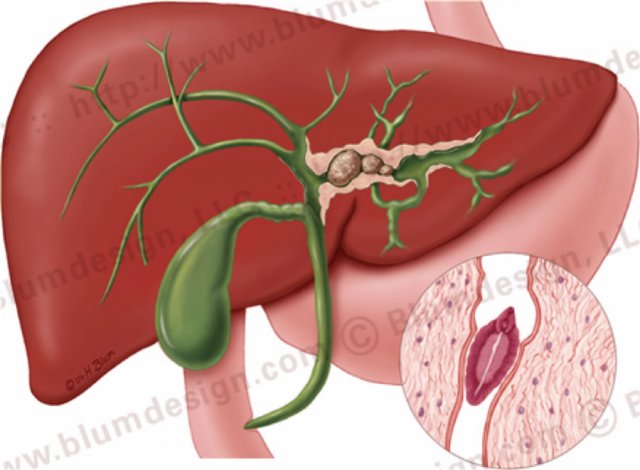
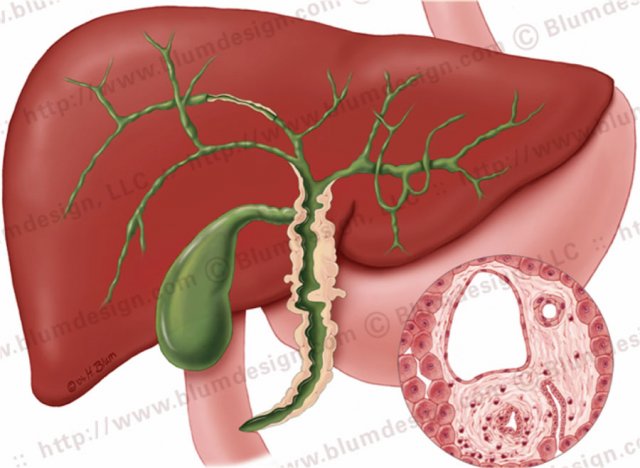 Primary sclerosing cholangitis with strictures both in the intra- and extrahepatic bile ducts. Illustration by Heike Blum
Primary sclerosing cholangitis with strictures both in the intra- and extrahepatic bile ducts. Illustration by Heike Blum
The hallmark of PSC is strictures, but early on in the disease the strictures can be difficult to appreciate.
The underlying abnormality in PSC is fibrosis, which is of unknown etiology.
PSC is strongly associated with ulcerative colitis in up to 70% of patients, but it can also be associated with Crohn's disease of the large intestine.
The reason for the association with IBD is unknown, but it is thought to be the result of an immune response.
Primary sclerosing cholangitis (2)
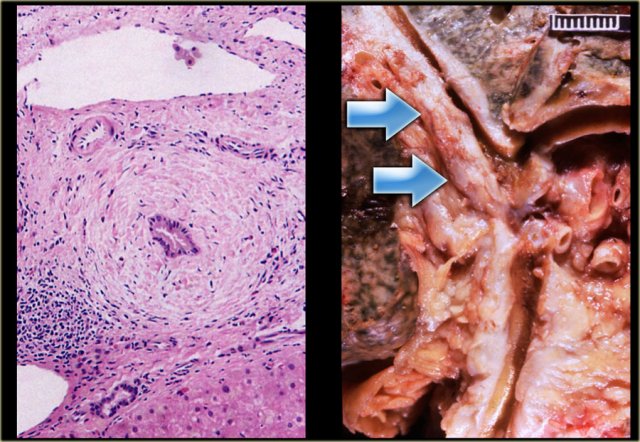
On the far left a histologic specimen demonstrating chronic inflammation surrounding the bile duct.
The gross specimen demonstrates the thickening of the wall of the bile duct (arrow) causing many strictures.
The strictures in PSC are short in the order of 3-5 mm in length, which is helpful to remember because if you are looking for cholangiocarcinoma, the malignant strictures usually exceed 10 mm in length.
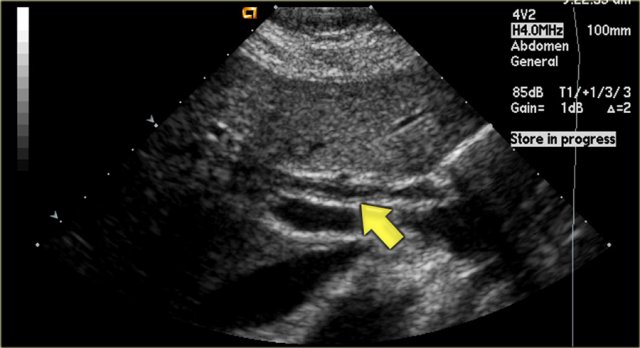
Ultrasound findings
One of the earliest features in PSC is on sonography where we see thickening of the wall of the bile duct as is seen in the image on the left.
This patient came for an ultrasound examination to rule out gallstones.
Notice that the intrahepatic ducts are normal.
The differential diagnosis would include PSC, AIDS-cholangitis and cholangiocarcinoma.
A cholangiocarcinoma would be rather unlikely, because there is no obstruction.
Continue with the CT.
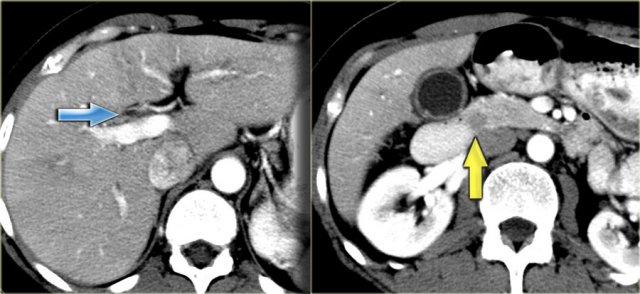
CT findings
On the CT the liver looks quite normal.
However if you look at the common bile duct in the pancreatic head you will notice the soft tissue density.
The differential diagnosis would include an impacted stone or cholangiocarcinoma, but since this patient had no obstruction, it was thought to be the result of bile wall thickening.
The gallbladder wall is also thickened.
Primary sclerosing cholangitis (3)
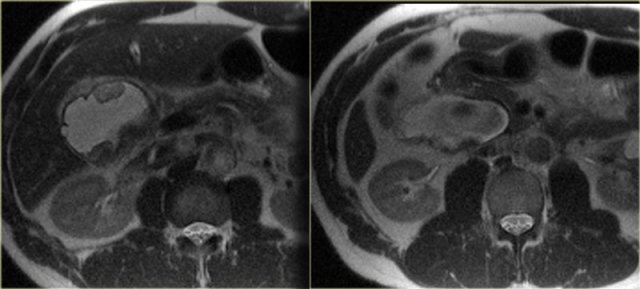
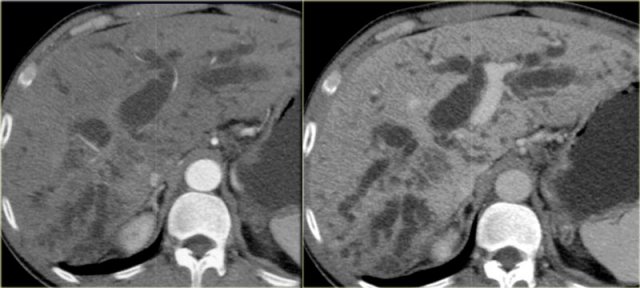
On the left a patient with more severe disease.
We can see mild bile duct dilatation with a discontinuous pattern.
On the left a patient with more pronounced CT findings.
Study the image and then continue reading.
The findings are:
- Discontinuous dilatation
- Bile wall thickening at the level of the porta hepatis
- Lymphadenopathy
Primary sclerosing cholangitis (4)
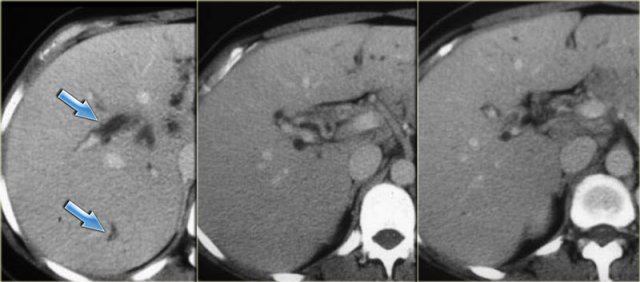
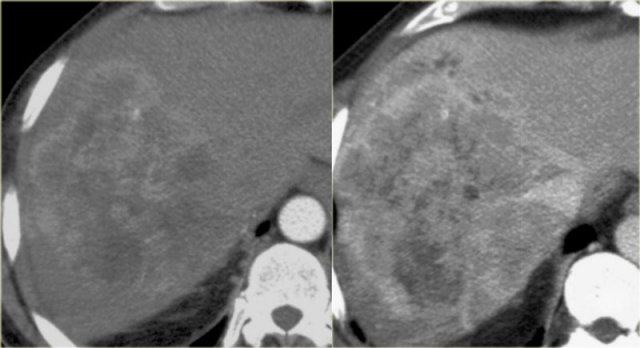
Late CT features are seen on the images on the left.
Study the images and then continue reading.
The findings are:
- Morphologic changes of cirrhosis (volume loss in the right lobe and a large caudate lobe (arrow)
- More pronounced dilatation of the bile ducts
Cholangiography is used in the initial diagnosis of the disease, when there are only subtle strictures and in patients known with PSC to look for new strictures that are suspicious for carcinoma.
On cholangiography we can see:
- Beading: alternating pattern of strictures and normal or slightly dilated ducts
- Pruned-tree: distal bile ducts are narrowed and difficult to see
- Mural irregularity: irregular luminal margin (best seen on the left in the extrahepatic duct)
- Diverticula: best seen in the next patient
On the left the typical findings in PSC.
Notice the diverticula on the image on the right.
Diverticula are very specific for the diagnosis PSC.
So when you see these diverticula, you should immediately search for subtle strictures in the intrahepatic ducts.
Primary sclerosing cholangitis (5)
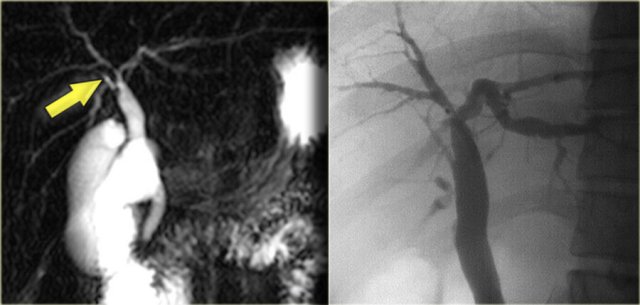
On the left a MRCP in a pateint with PSC.
Notice the large stricture, which is quite worriesome for cholagiocarcinoma (arrow).
The strictures in PSC show an abrupt transission, while here we see 'shouldering', which indicates mass-efect.
In addition there is intrahepatic dilatation proximal to this stenotic area.
On the left a MRCP in a patient demonstrating a stricture at the level of the hilum.
On MRCP this stricture looked long and worriesome for cholangiocarcinoma.
However, on the ERCP, the ducts have been distended with contrast and we can see that this is a short stricture compatible with the diagnosis of PSC.
During follow up this proved to be just PSC.
Cholangiocarcinoma
Cholangiocarcinoma (i.e., adenocarcinoma of the bile duct) arises from the columnar epithelium of the bile duct.
It is characterized by malignant glands within a desmoplastic stroma.
These tumors have an infiltrative growth pattern and do not have a capsule.
There are four basic patterns of chlangiocarcinoma: (illustration on the left).
Cholangiocarcinoma is an uncommon tumor, that is mostly seen in patients with underlying benign bilairy disease.
The incidence in the U.S. is 2000 to 2500 cases per year (coloncancer 150.000 per year).
In Asian countries the incidence is ten times greater due to more chronic biliary infection.
High risk groups are patients with:
-
Autoimmune diseases
- PSC, ulcerative colitis, primary biliary cirrhosis
-
Congenital anatomic anomalies
- Caroli, choledochal cyst, anomalous pancreaticobiliary junction
- Abnormal tumor suppressor genes, FAP, NF1
-
Infection
- Biliary parasites, recurrent pyogenic cholangitis
Clinical presentation:
- Jaundice
- Pain
- Fever if secondary cholangitis
Intrahepatic cholangiocarcinoma
These arise in the very small peripheral ducts.
These tumors have abundant fibrous stroma that can cause retraction of the liver capsule.
The tumor typically enhances in the equilibrium and delayed phases (5-10 minutes).
Read more about intrahepatic cholangiocarcinoma in Liver : Masses Part II : common liver tumors
Although these tumors are usually quite heterogeneous because the contrast uptake is delayed and can be irregular.
The key findings to look for are:
- Delayed enhancement
- Peripheral biliary dilatation
- Capsular contraction
On the left a typical case.
Notice the capsular retraction (blue arrow) and the late enhancement (yellow arrow).
Intraductal Cholangiocarcinoma
These are very rare tumors.
They present as a intrabiliary mass with biliary dilatation peripheral to the mass.
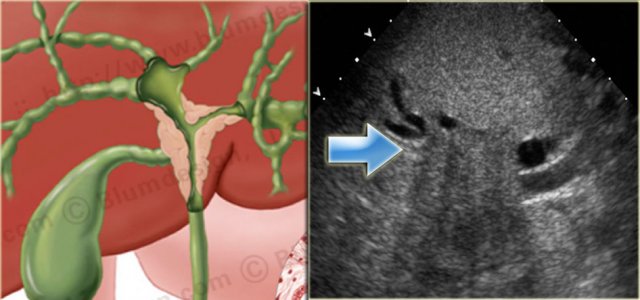 Klatskin Tumor with dilatation of bile ducts in the right and left lobe of the liver Illustration by Heike Blum
Klatskin Tumor with dilatation of bile ducts in the right and left lobe of the liver Illustration by Heike Blum
Klatskin Tumor - Hilar Cholangiocarcinoma
The most common site of biliary adenocarcinoma is at or near the confluence of the right and left hepatic ducts.
These tumors are also known as Klatskin tumors.
Klatskin tumors have an aggressive biologic behavior.
Imaging features:
- Duct dilatation
- Ill-defined mass
- Lobar atrophy
- Vascular invasion
On the left a nice correlation between an illustration and a sonographic image of a Klatskin tumor.
Notice how ill-defined the tumor is.
On CT these tumors can be very difficult to visualize.
Many of these patients already have a stent in place when they first come to CT which makes it even harder (figure).
Klatskin Tumor (2)
In the case on the left we can identify the tumor at the confluens of the left and right hepatic duct.
The margins of the tumor however are imperceptible because of the infiltrative growth.
Based on the CT it is not possible to stage the tumor correctly.
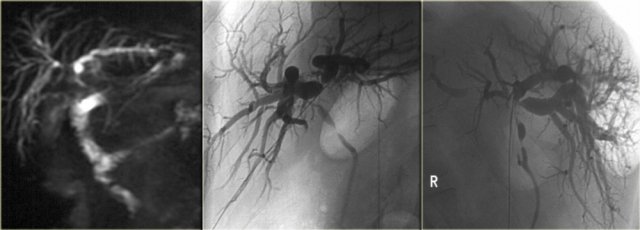 Hiar Cholagiocarcinoma. Notice the superiority of ERCP to MRCP. The image on the right nicely demonstrates the shouldering at the hilum and the multiple strictures.
Hiar Cholagiocarcinoma. Notice the superiority of ERCP to MRCP. The image on the right nicely demonstrates the shouldering at the hilum and the multiple strictures.
In these tumors it may be difficult to get a definitive diagnosis pre-operatively.
Biopsy is almost impossible and results of endoscopic brushing are commonly negative.
The staging is done with cholangiography and is based on the finding of mass effect (shouldering), irregular margins and abrupt tapering at the obstruction.
The limitations of MRCP in staging are the spatial resolution and the inability in the evaluation of the secondary ducts.
ERCP is superior to MRCP (figure)
Klatskin Tumor (3) : Resectability
These tumors are unresectable when:
-
Bilateral tumor extension
- Into secondary ducts
- Into hepatic parenchyma
- Hepatic artery or portal vein
- Occlusion main portal vein
- N2 nodes (nodes around the pancreas)
- Distant metastases
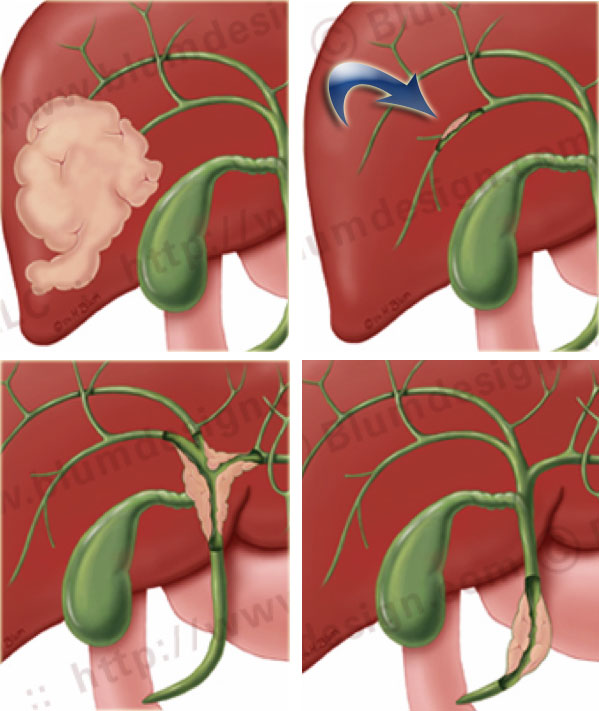
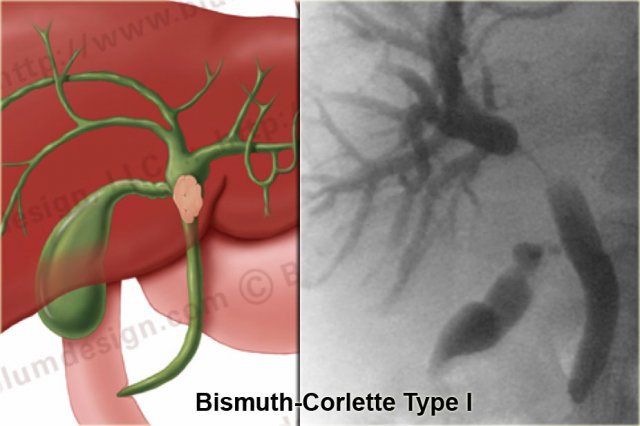
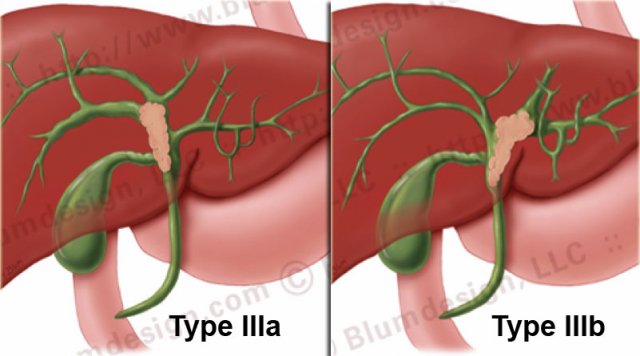
Klatskin Tumor - Bismuth-classification
Bismuth-Corlette type I
A type I tumor is a lesion limited of the common hepatic duct, i.e. below the confluence.
These patients can undergo resection with bile duct recontruction because the confluence is normal.
Bismuth-Corlette type II
A type II tumor is a lesion that extends to the confluence.
These tumors are potentially resectable
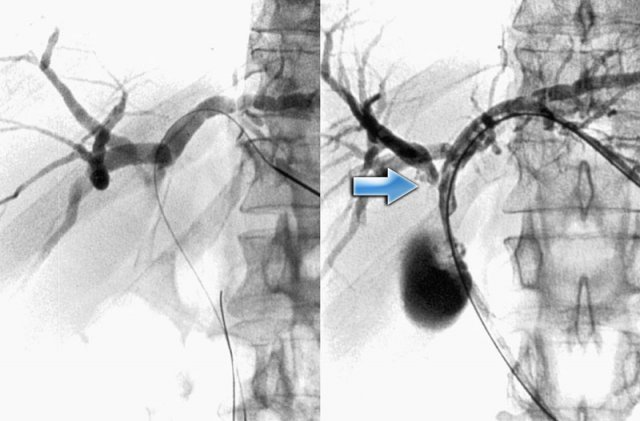
Bismuth-Corlette type IIIa and IIIb
A IIIa-tumor extends into the right and a IIIb-tumor extends into the left hepatic duct.
On the left PTC-images of a type IIIa-tumor.
The arrow indicates the extention into the right hepatic duct.
The left duct is normal.
This patient can undergo a resection of the right lobe of the liver.
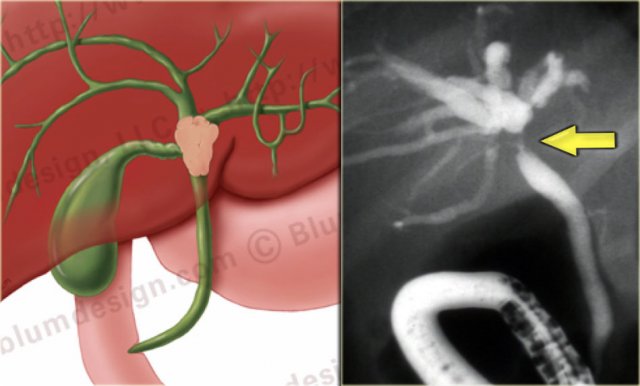
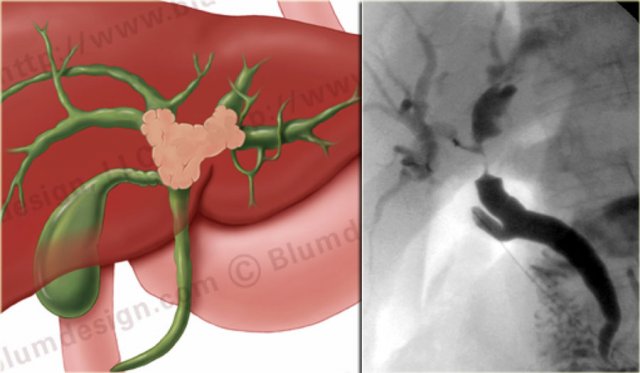
Bismuth-Corlette type IV
On the left an illustration and ERCP of a type IV-tumor with extention into the right and left duct.
A type IV tumor is unresectable.