Enhancement Patterns in CNS disease
Linda Jacobi-Postma and Debbie Duyndam
Maastricht University Medical Center and Onze Lieve Vrouwe Gasthuis in the Netherlands
Publicationdate
Under normal conditions there will be no enhancement of
the brain parenchyma in the central nervous system, because the brain is the only organ with a barrier for proteins, inflammatory cells and also for contrast medium.
This barrier is called the Blood-Brain Barrier.
The Blood-Brain Barrier can be damaged by various diseases like:
- Inflammation or infection (abscess)
- Demyelinization
- Ischemia
- Tumors like gliomas, lymphomas and metastases.
Understanding the patterns of enhancement in CNS disease will improve image assessment and differential diagnosis.
In this article eleven patterns will be discussed with many examples.
We want to honour James Smirniotopoulos, who teached us thinking in patterns, not just enhancement.
His article in 2007 in Radiographics and his animated lectures inspired us writing this article.
He was so kind to review this article.
Introduction
Pattern approach
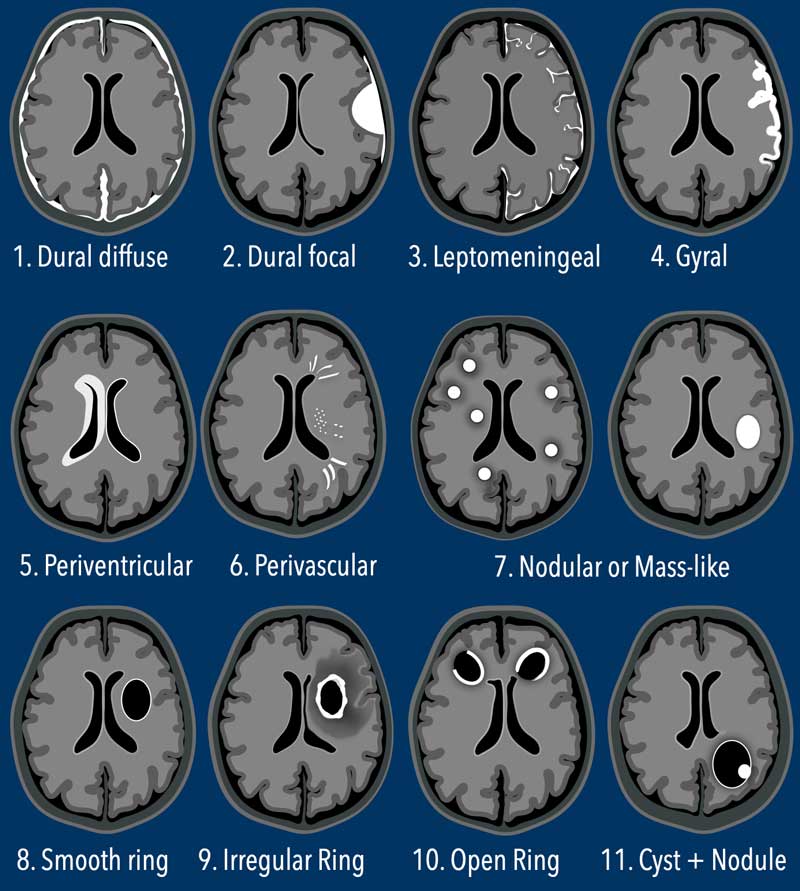
In this table the most common patterns of enhancement in CNS diseases are illustrated.
The first three are extra-axial (diffuse and focal dural and leptomeningeal), while the others are all intra-axial patterns.
You can click on the links below to go directly to examples of a specific pattern.
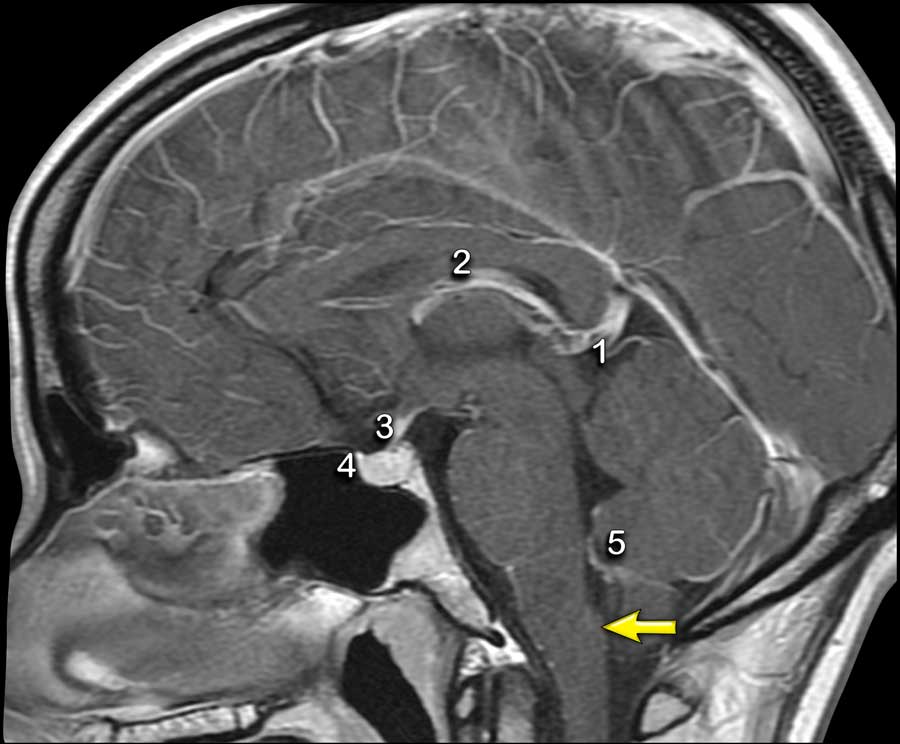
Normal enhancement
Structures in the brain, that do not have a blood-brain barrier or structures that are extra-axial will show normal enhancement.
These structures are the dura, the pineal gland (1), vessels (2), the pituitary stalk (3) and pituitary gland (4), the choroid plexus (5) and the area postrema (arrow).
The area postrema is a highly vascular paired structure in the medulla oblongata in the brainstem and is located just inferoposterior of the floor of the fourth ventricule.
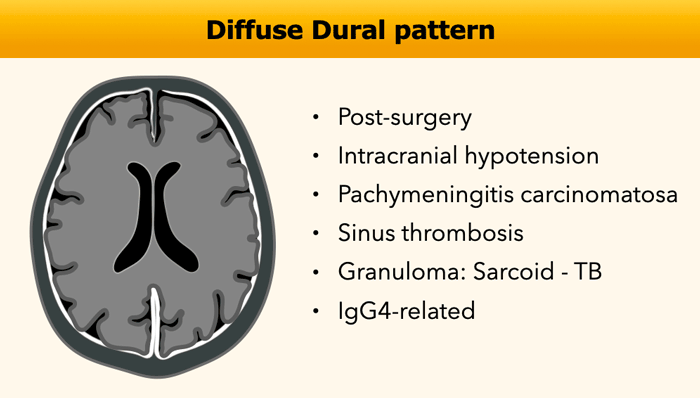
Diffuse Dural pattern
The diffuse dural pattern of enhancement is a common finding in MR examinations.
It is most commonly seen in post-surgery and intracranial hypotension.
Normal dural enhancement
The dura mater is an extra-axial structure and therefore does
not have a blood-brain barrier.
In half of the population enhancement can be seen on a
contrast-enhanced MRI as a thin, smooth and discontinuous layer as seen in
these images.
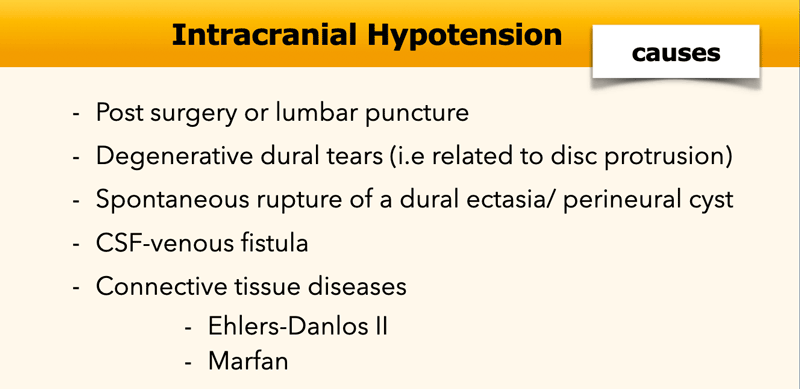
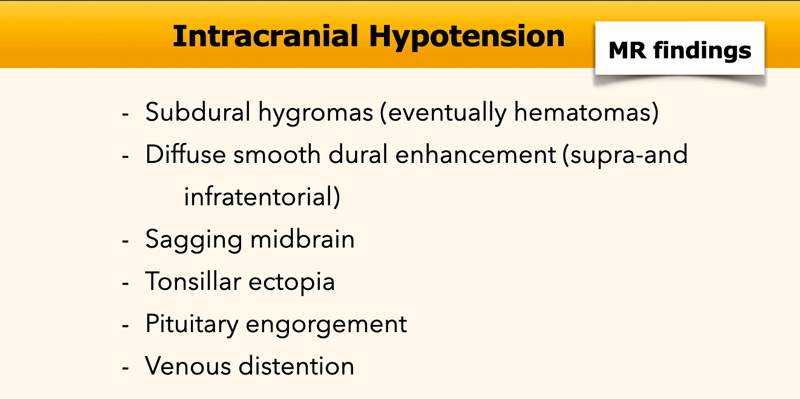
Intracranial hypotension
Intracranial hypotension is a condition in which there
is abnormally low pressure or volume within the skull due to a reduction in
cerebrospinal fluid (CSF).
The classical presentation is a persistent orthostatic
headache.
Intracranial hypotension can be caused by surgery, lumbar puncture, ventricular drains and “spontaneous”
CSF leakage.
Spontaneous CSF leakage is seen in an anterior dural tear (type 1), a leaking nerve root diverticulum (type 2) or a CSF-venous fistula (type 3).
Further
work-up to find the cause for CSF leakage requires spinal imaging, either with
MRI of CT-myelography.
The CSF leakage can be treated by placing an epidural bloodpatch.
MRI findings include small ventricles, subdural hygromas and eventually hematomas, diffuse (supra-and infratentorial) smooth dural enhancement, sagging of the midbrain and acquired tonsillar ectopia, pituitary engorgement and distention of the dural venous sinuses.
When the CSF pressure drops, the volume of the veins in the subarachnoid space increases, ultimately leading to vasocongestion and interstitial edema in the dura.
Imaging findings can be normal in 10% of cases.
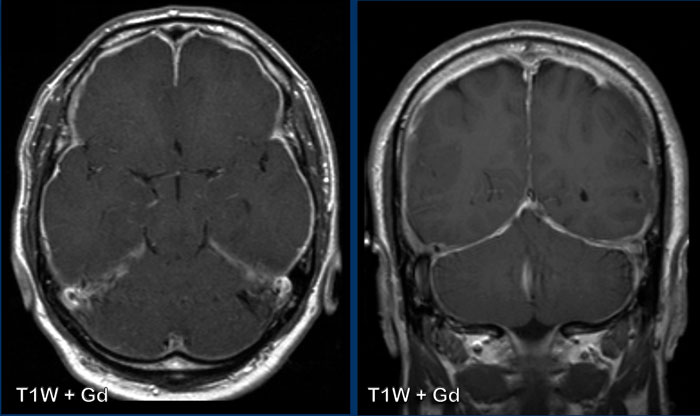
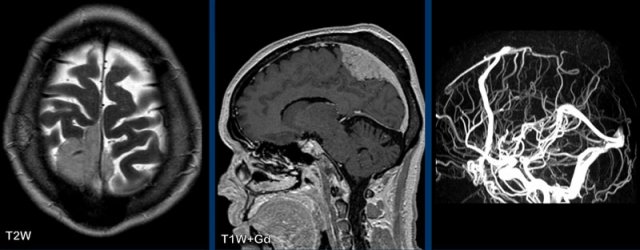
These images are of a 58 year-old male who presented with headache in the sitting and standing position.
Images
A
smooth dural enhancement is present in both the supratentorial and the infratentorial compartment.
Notice the small ventricles.
Continue with the sagittal images...
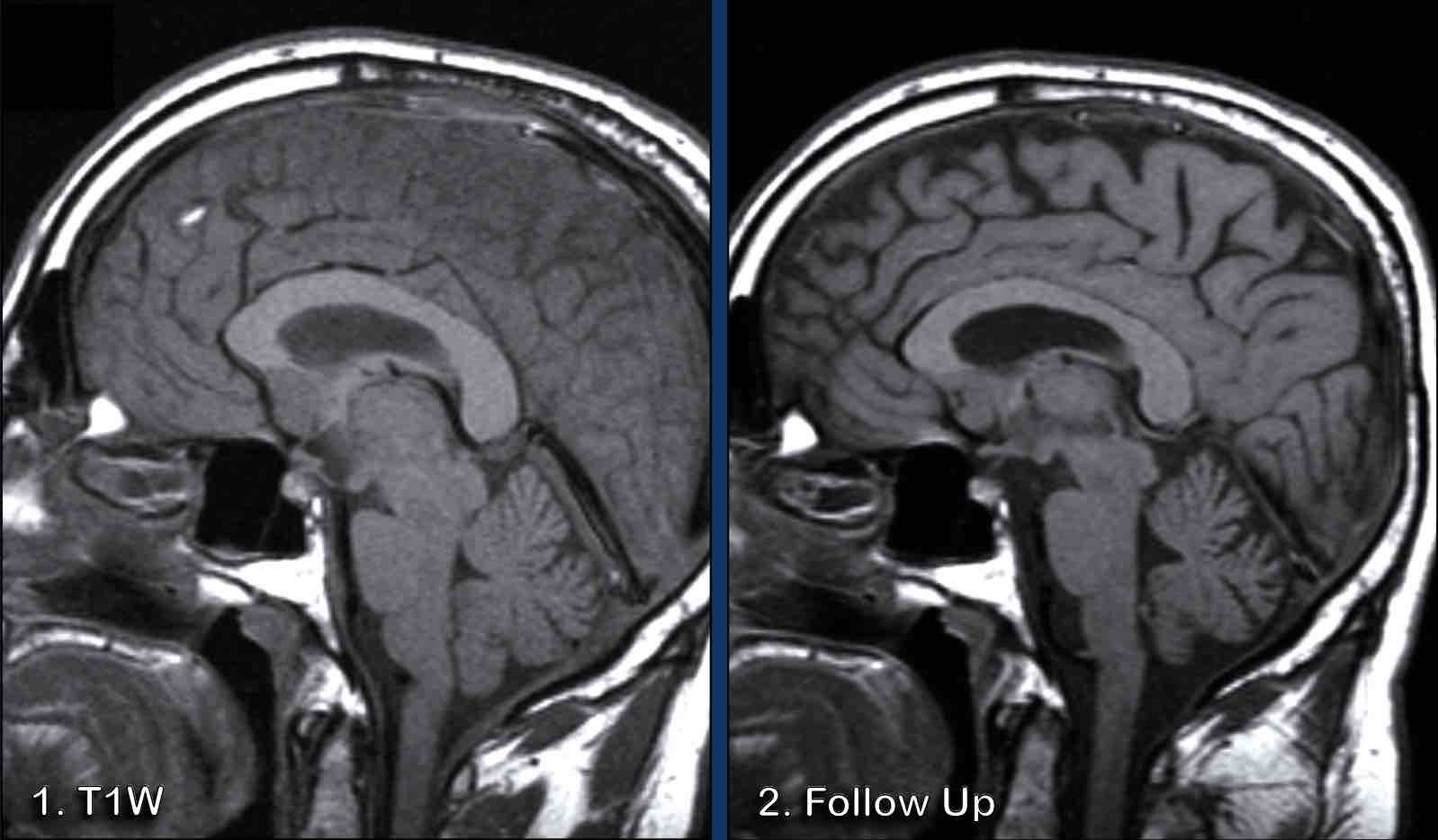
Image 1
The findings are rather subtle, but there is:
- Sagging of the midbrain with decreased pontomamillary distance, effacement of the suprasellar cistern, flattening of the anterior pons and kinking at the craniocervical junction.
- The hypothalamus is folding over the dorsum of the sella, the pituitary gland is somewhat enlarged (white circle).
- The interthalamic substance is lowered; the posterior part of the corpus callosum is lowered (‘drooping penis sign”). Note the flattening of the supracerebellar cistern.
- In this case the tonsils are in a normal position and there is no herniation (yellow circle).
Conclusion: findings
typical for intracranial hypotension.
Image 2
After therapy, which was a non-targeted epidural bloodpatch, the brain and brainstem have returned to their normal position with normalization of the cisterns and fourth ventricle configurations.
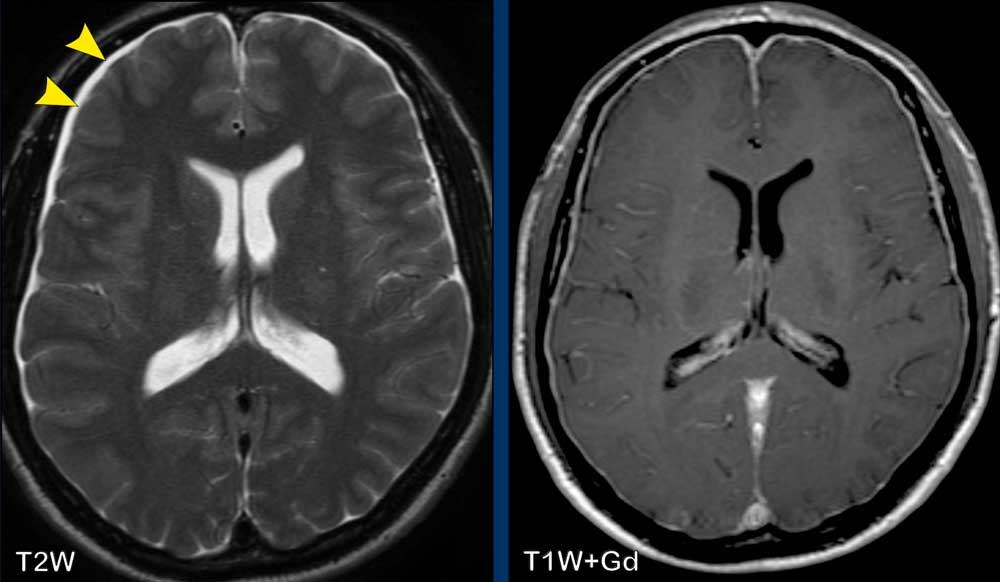
These images are of a 44-year old male, who presents with longstanding headache, which increases with forward bending.
Images
T2W-image demonstrates small bilateral subdural hygromas (arrowheads).
After gadolinium there is
smooth dural enhancement.
Continue with the sagittal images...
Images
There is engorgement of the venous structures, as is depicted in the superior sagittal sinus (arrow heads), the straight sinus and confluens.
There is downward placement of the brainstem with shortening of the pontomammilary distance, flattening of the pons and kinking of the brainstem at the craniocervical junction.
The venous plexus in the cervical anterior epidural space is widened.
Conclusion
These findings are typical for intracranial hypotension.
The patient was later diagnosed with a connective tissue disorder.
These images are of a male with a history of left-sided middle cerebral artery infarction, who presented with headache, worsening on standing and forward bending and tinnitus.
Images
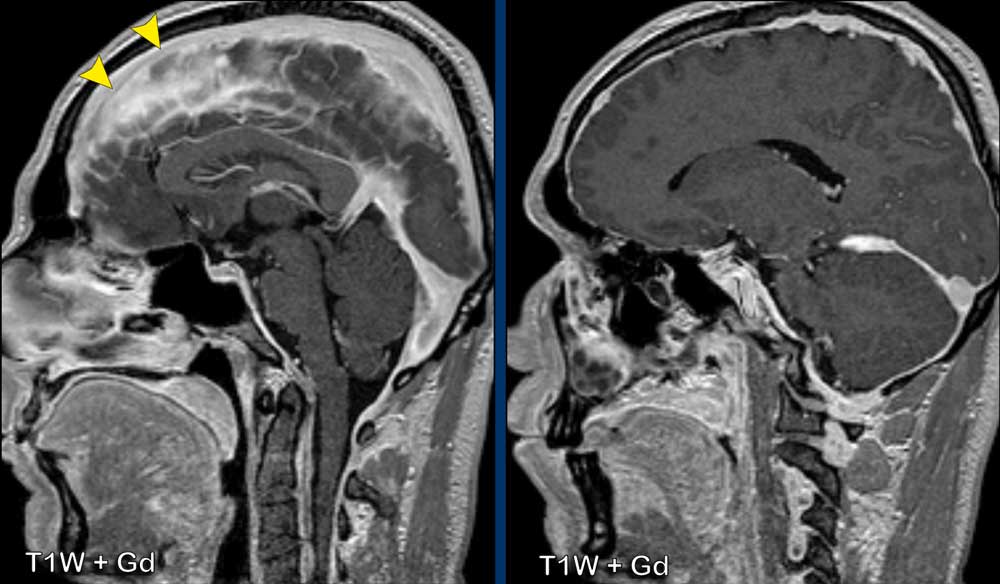
There is thick and somewhat irregularenhancement of the dura, with thicker apposition
over the tentorium, left temporal and left
frontoparietal dura.
Conclusion
Idiopathic
hypertrophic pachymeningitis.
This turned out to be a biopsy proven IgG4-related disease.
Continue with the post-treatment images...
After treatment with corticosteroids there is resolvement of the dural thickening and enhancement.
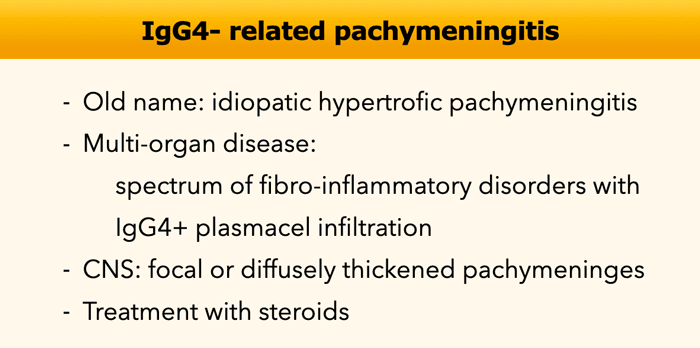
IgG4-related pachymeningitis
It has now become clear that many of the cases, that we used to call idiopathic hypertrophic pachymeningitis are actually IgG4-related.
IgG4-related disease is an auto-immune disease that can affect many organs of which the pancreas is the most common.
In the brain the meninges can be involved.
It is important to suggest this diagnosis as it is a treatable disease.
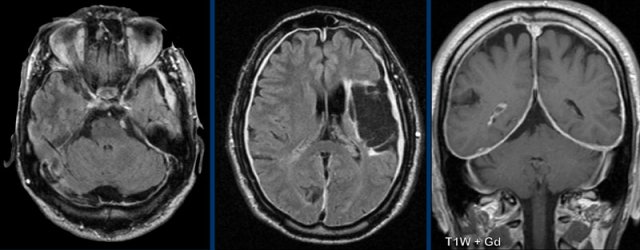
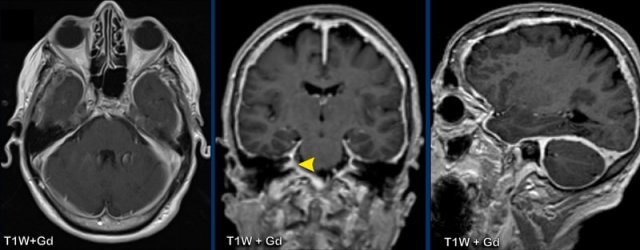
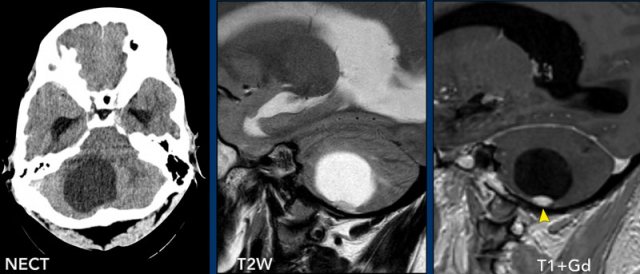
This is a companion case of a patient with headache and bilateral hearing loss.
Images
There
is thickening of the dura with enhancement with a slight irregular aspect.
there is no
engorgment of the veins
The enhancement extends into
the internal acoustic meatus (yellow arrowhead).
Continue with the images post-treatment...
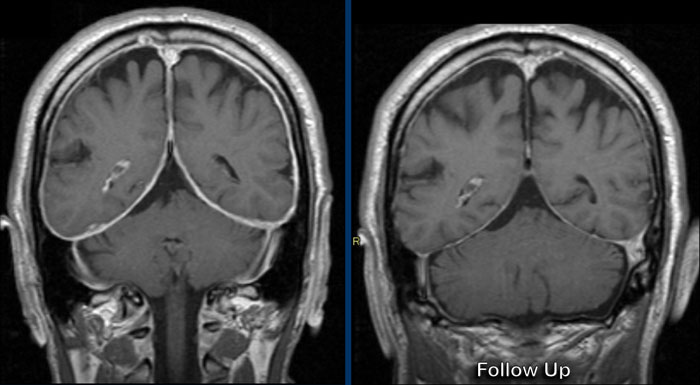
Same patient before and 6 months after steroid therapy with resolution of the abnormalities .
This patient had a craniectomy for surgical evacuation of a left-sided subdural hematoma.
Images
A thin linear enhancement of the left parietal dura is shown,
demonstrating postsurgical dural enhancement.
(PS you might also call a focal dural pattern).
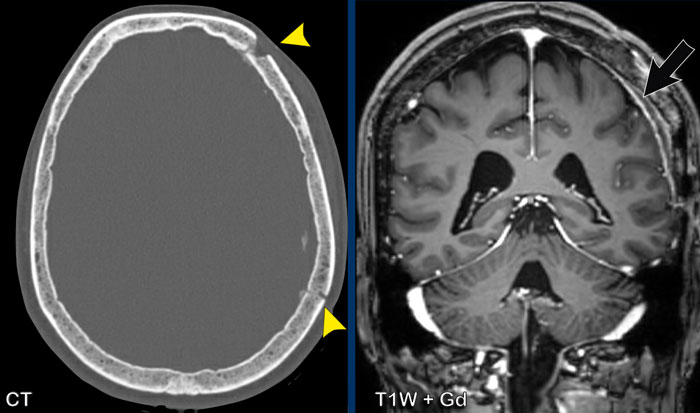
Focal Dural pattern
The most common tumor that presents with a focal dural pattern is a meningioma, which is an extra-axial lesion.
Lymphoproliferative disorders comprise a heterogeneous group of diseases characterized by uncontrolled production of lymphocytes, including lymphomas, lymphocytic leukemia, multiple myeloma, LIP and many others.
Lymphomas that present as a dural tumor are secondary CNS lymphomas, i.e. the lymphoma starts elsewhere in the body and spreads to the brain.
Most intra-axial CNS lymphomas however are primary.
They start in the brain and are not located in other organs.
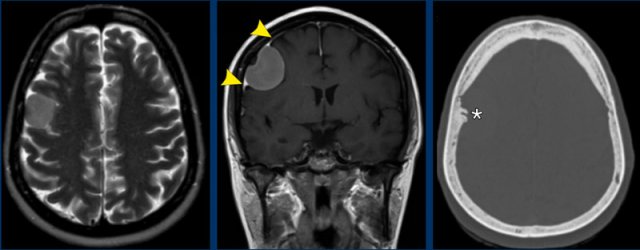
Meningioma
Which findings are typical for the diagnosis meningioma?
Findings:
- The tumor is extra-axial as can be seen on the T2W-image. There is CSF between the tumor and the brain parenchyma, this is called a CSF-cleft
- On T2W image the tumor has a relative low signal intensity
- There is homogeneous enhancement.
- Dural tail (arrowheads)
- Hyperostosis of the skull (asterix).
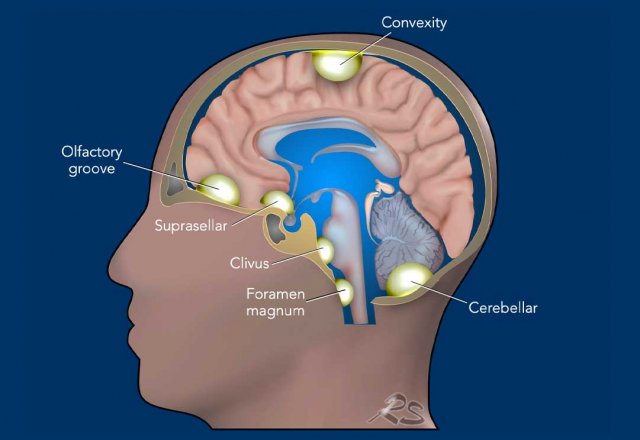
The illustration shows favorite locations of meningiomas: at the skull base, the falx, tentorium and convexity.
Most meningiomas are WHO grade 1.
An atypical meningioma is grade 2 and an anaplastic
meningioma is grade 3.
The meningo-endothelial cells arise from the arachnoid cap cells, which
is the inner most layer of the dura.
On CT a meningioma is relatively hyperdense and may contain
calcium.
When they contain calcium, they usually grow very slowly.
On MRI a meningioma is iso-intense to the grey matter on T1-
and T2W-images.
There is vivid enhancement due to the fact that the
extra-axial dural capillairies do not have a blood-brain barrier.
A dural tail is a common finding.
It is caused by vasocongestion and interstitial edema of the
nearby dura and mostly not caused by tumorcells.
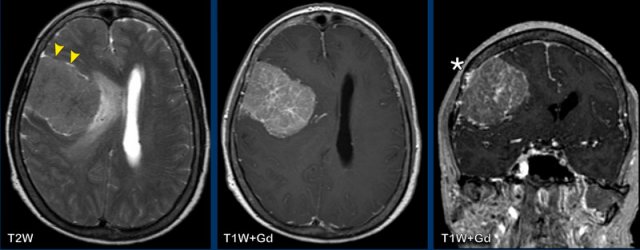
The images show a more aggressive looking lesion with edema
and midline shift.
Which findings favor the diagnosis of a
meningioma?
Findings:
- The tumor has a flat dural base.
- Most important finding is the CSF between the tumor and the surrounding brain tissue (arrow heads). This finding definitely makes this an extra-axial tumor.
- Low signal on T2W
- Reactive changes in the skull (asterix) There is osseous involvement of the lesion. Not typical but frequently seen in a meningioma
The intraparenchymal
extension suggests a higher grade meningioma, while the presence of
edema is not a reliable sign of a higher grade.
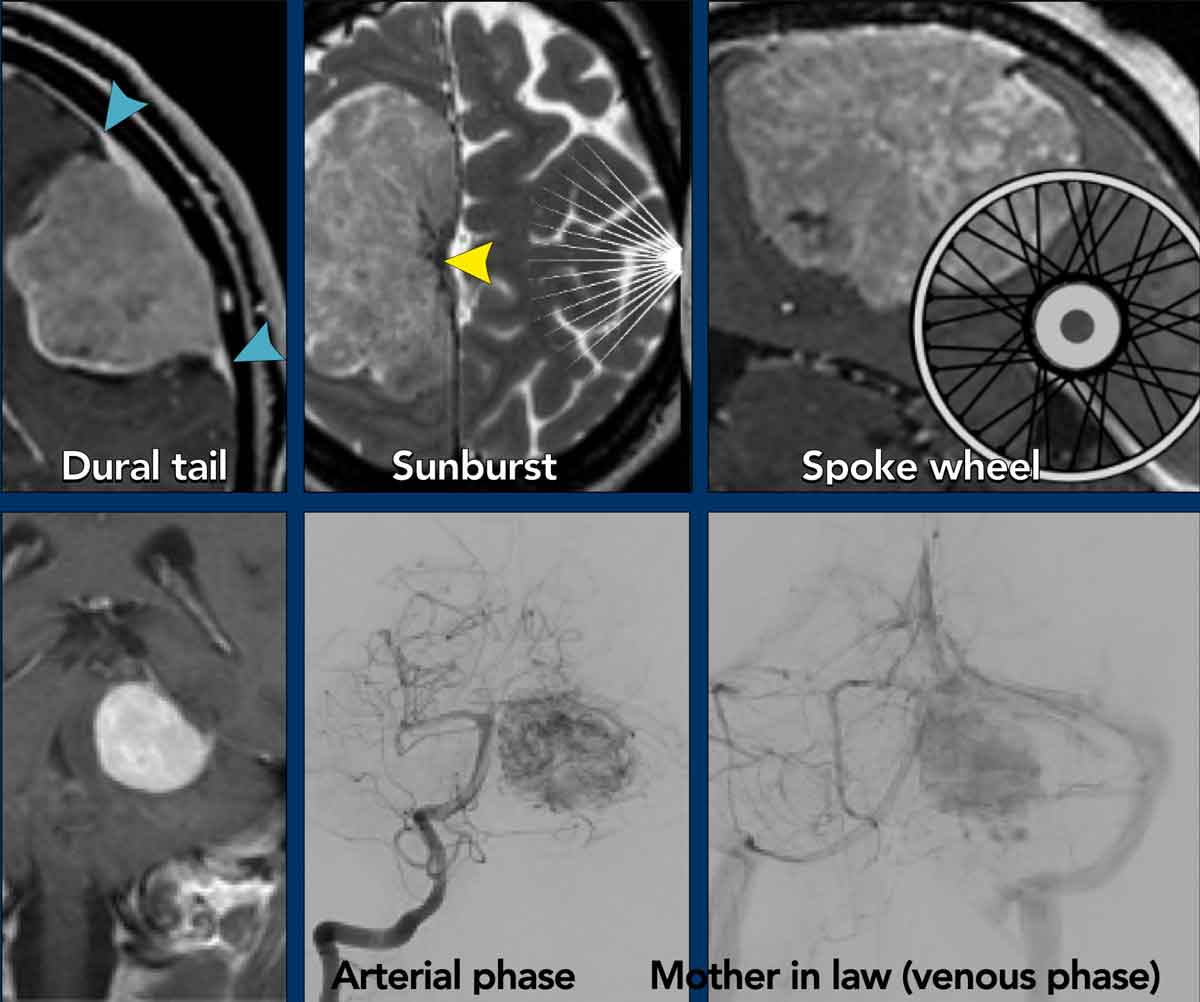
The following signs are described in meningiomas:
- Dural tail sign (blue arrowheads)
- Sunburst sign (yellow arrowhead)
- Spokewheel sign
This is the same as the sunburst but seen in a perpendicular direction.
It refers to the characteristic vascular supply seen in some meningiomas when seen from the side. - Mother-in-law
sign
This is an angiographic sign as demonstrated in this tentorial meningioma. A mother-in-law comes early (arterial phase) and stays late (venous phase). A meningioma shows early enhancement and the enhancement stays for a long time.
The sunburst sign can give the appearance of a flower like in this anterior skull base meningioma’s
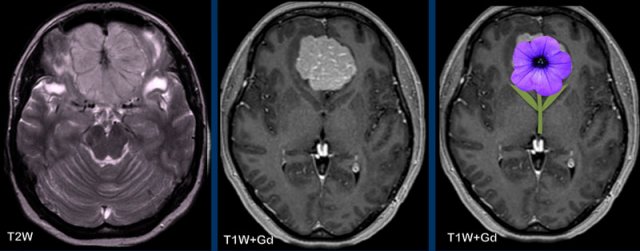
These
images are of a 56-year old woman with breast cancer.
She had a skull lesion at a bone scan nine years earlier
which was thought to be a metastasis.
Now she presented with vomiting and headache.
Images
There is a a large extra-axial lesion compatible with a meningioma.
There is profound hyperostosis of the skull and invasion of the superior sagittal sinus.
This is not a bone metastasis because of these findings and the fact that the lesion is present for nine years.
Metastases
Although meningioma is the most common dural tumor, which is regularly seen as an incidental finding on brain imaging, there are many other dural masses which can mimic the appearance of a meningioma, including primary neoplasms, lymphoma, metastases, granulomatous diseases and infection.
Although not pathognomonic, key features which increases the probability of a lesion being a meningioma include intralesional calcifications, skull hyperostosis, focal dural enhancement and increased perfusion.
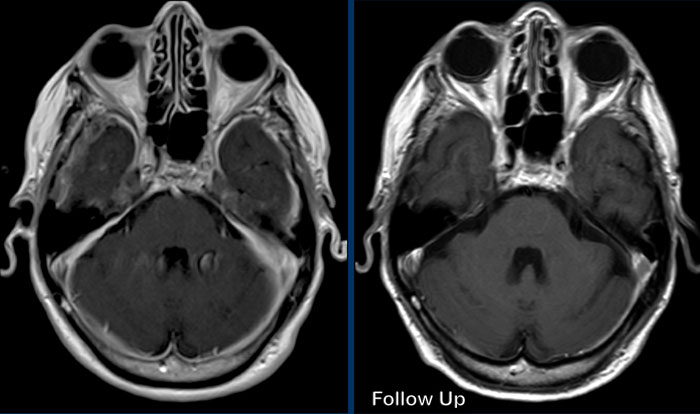
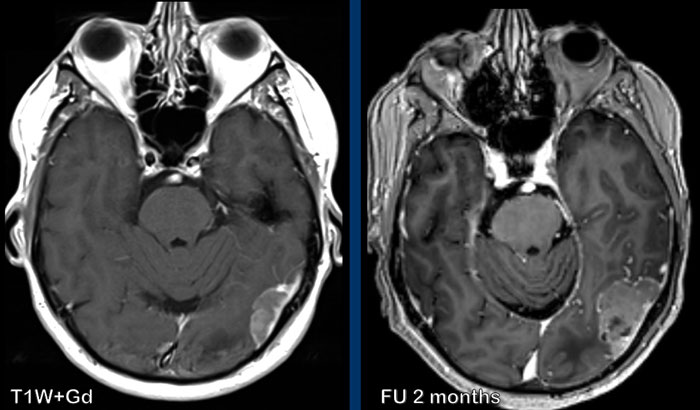
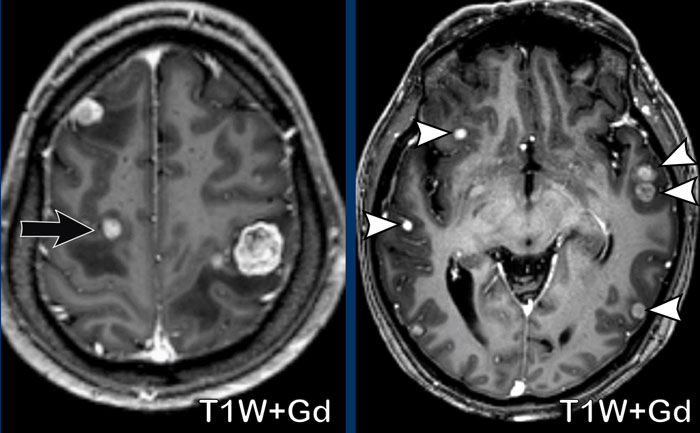
Images
These images are of a 58-year old man with lung cancer.
There are two lesions, that mimic the appearance of meningioma.
Continue with the follow up images...
On the 2 month follow-up image there is significant growth of the lesion.
Now the borders are irregular.
This turned out to be a dural metastasis.
These images are of a woman with cervical cancer.
There is an extremely large bone metastasis with involvement
of the dura and extracranial extension.
Notice a parenchymal metastasis in the posterior fossa (arrowhead).
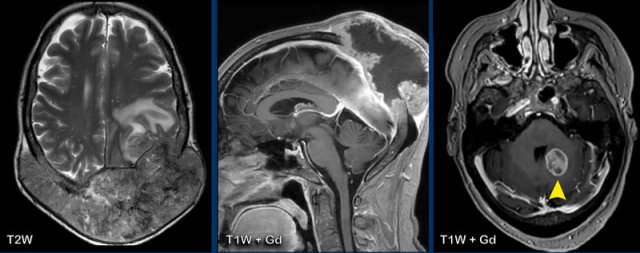
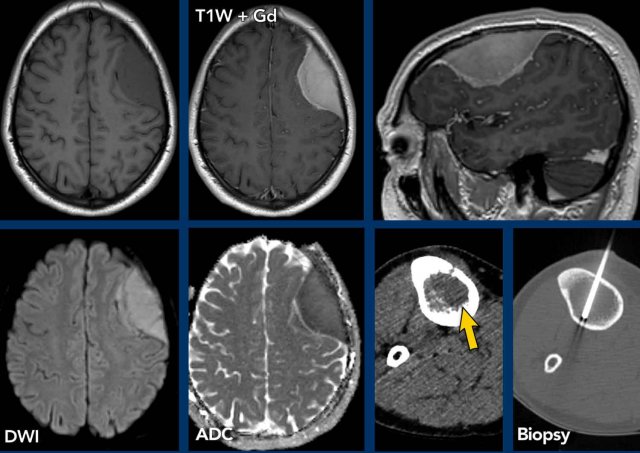
Lymphoma
This
patient had multiple osseous FDG-PET positive lesions.
A
biopsy of a tibial lesion demonstrated a malignant lymphoma.
He also presented with a dural based mass with additional subtle leptomeningeal involvement.
The lesion demonstrates homogeneous enhancement and restricted diffusion.
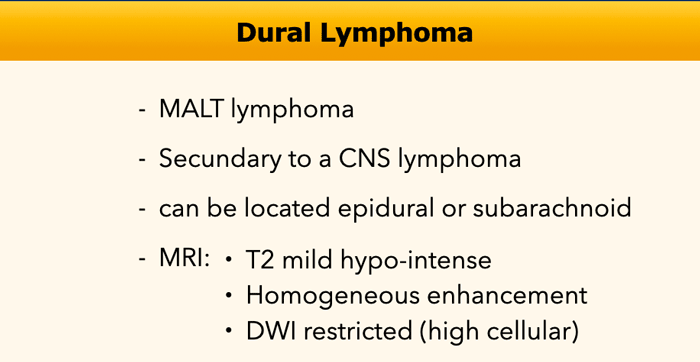
Primary dural lymphoma is an extranodal non-Hodgkin
lymphoma that accounts for less than 1% of all central nervous system
lymphomas.
It can mimic the appearance of a meningioma and
meningiomas can sometimes show restricted diffusion, especially when it is an atypical or malignant meningioma.
In this patient, a multifocal dural lymphoma was diagnosed.
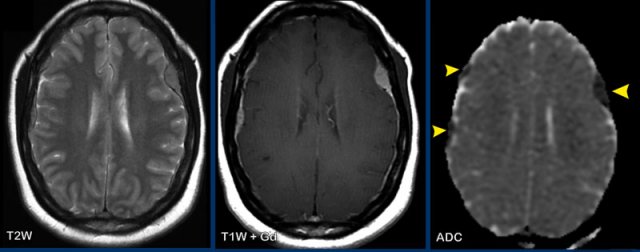
Images
Multiple enhancing extra-axial located dural based lesions with restricted diffusion.
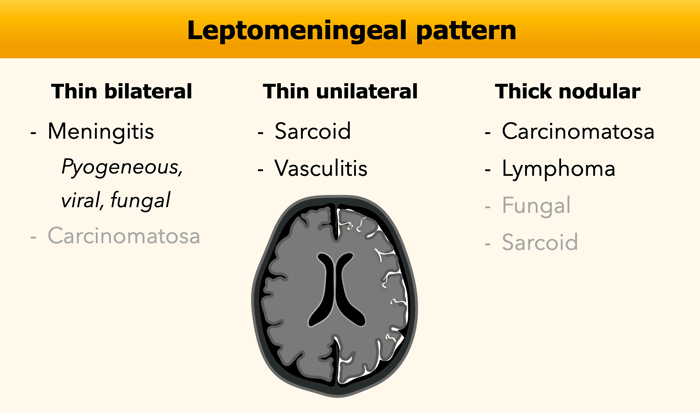
Leptomeningeal
The leptomeningeal enhancement follows along the pial surface of the brain and fills the subarachnoid spaces of the sulci and cisterns.
The most common cause is infectious meningitis followed by meningeal carcinomatosis.
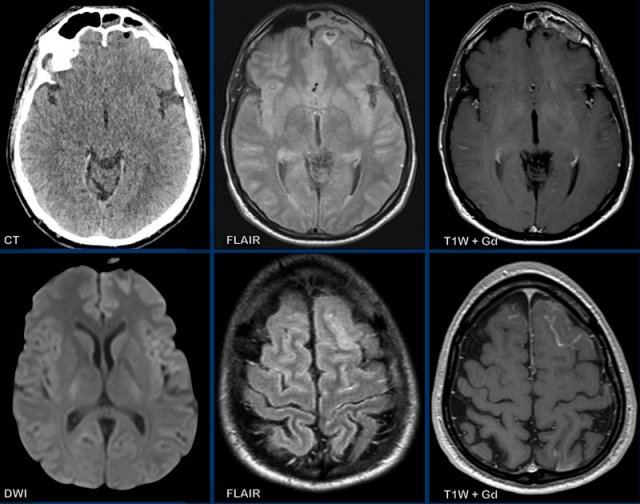
This patient presented with headache.
Images
- CT: notice a small air focus at the left on the left side, with only minor sinus secretions in the left frontal sinus.
- FLAIR: a small hyperintense lesion with a central hypo-intens focus.
- T1W+Gd: no enhancement of the lesion, but only faint leptomeningeal enhancement.
- DWI: no restricted diffusion.
- FLAIR image at a higher level shows hyperintensity in the left frontal subarachnoid space and at the frontal cortex, which is compatible with meningitis.
- T1W+Gd: enhancement in the left frontal subarachnoid space
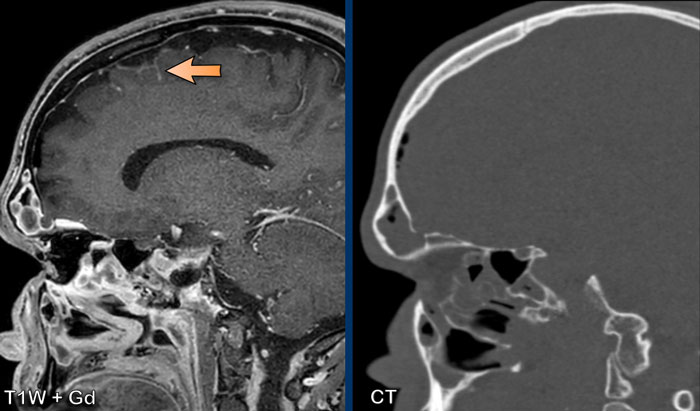
Images
Sagittal images demonstrate a small osseous defect at the posterior border of the frontal sinus with a small frontal cerebral encephalocele (black arrowhead).
There is leptomeningeal enhancement (arrow).
Conclusion
The
presence of a frontal encephocele lead to opacification of the frontal sinus and meningitis due to direct communication
via the osseous defect.
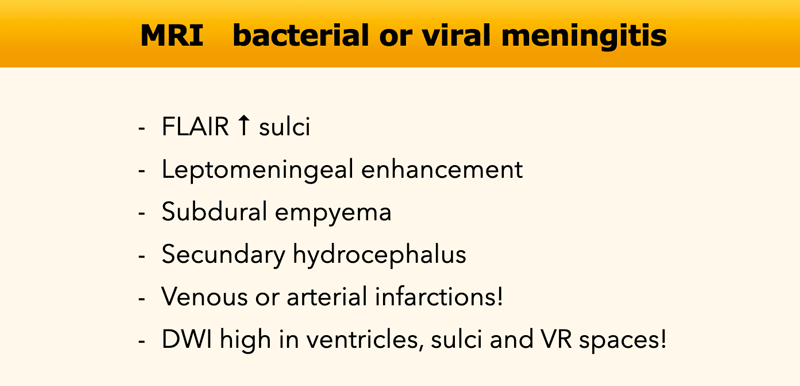
Leptomeningitis represents inflammation of the subarachnoid space.
MRI demonstrates FLAIR hyperintensity in the CSF space, especially in the sulci, and leptomeningeal enhancement. Possible complications of leptomeningitis are subdural empyema, secondary communicating hydrocephalus, infarction and ventriculitis.
Diffusion restriction can be seen in the ventricles, sulci and VR spaces.
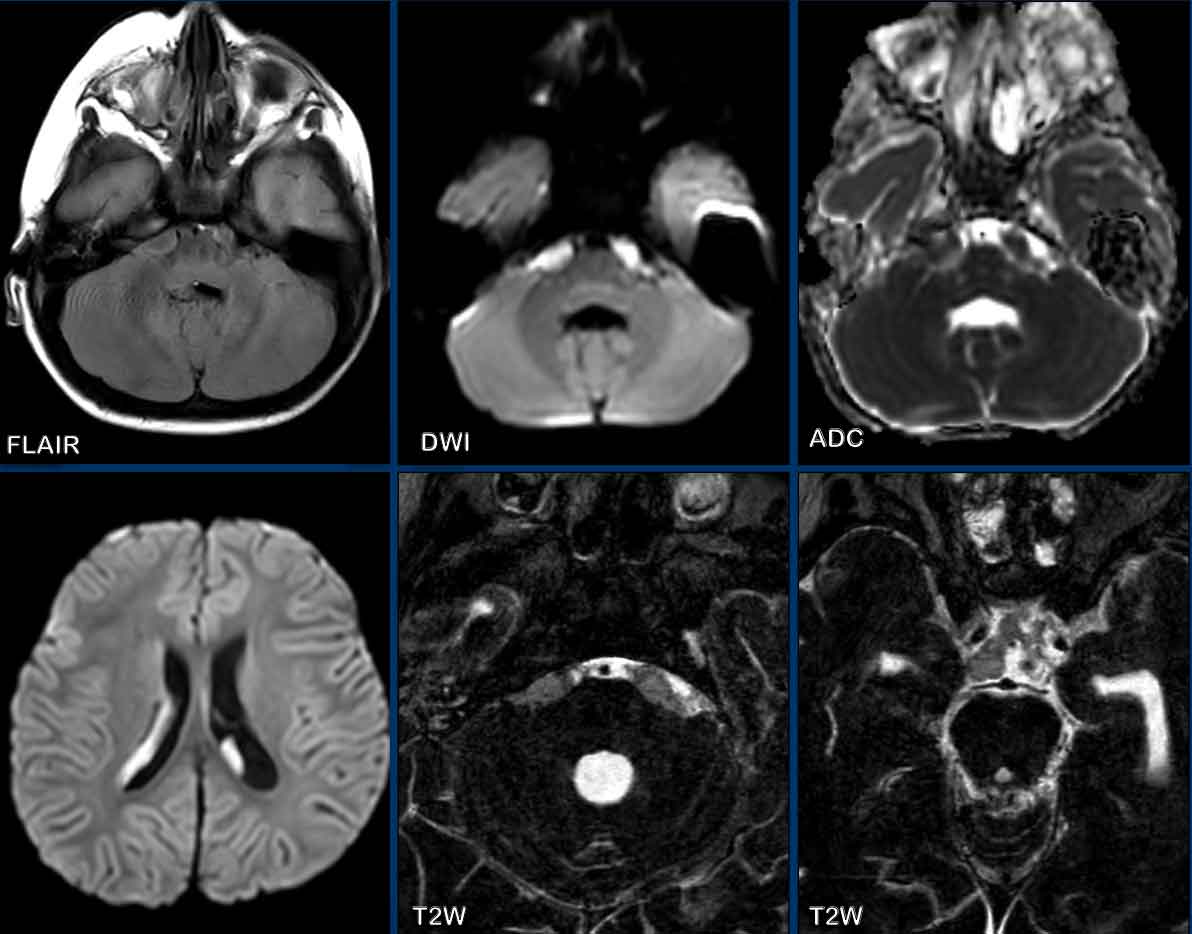
these images are of a 2 year old child, who presented with fever, abducens paresis and eventually loss of consciousness.
Images
There is obliteration of the prepontine cistern on FLAIR with
restrictive diffusion.
There is hyperintense signal on DWI in the
bilateral ventricles, consistent with pus.
High-resolution T2W-images demonstrate loss of hyperintense signal in the cisterns and subarachnoid space, based on thick
pus.
Final diagnosis
Haemophilus influenzae type B meningitis and ventriculitis.
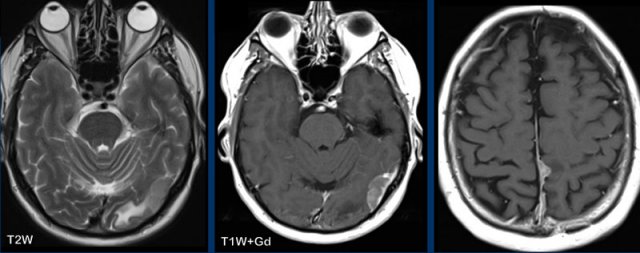
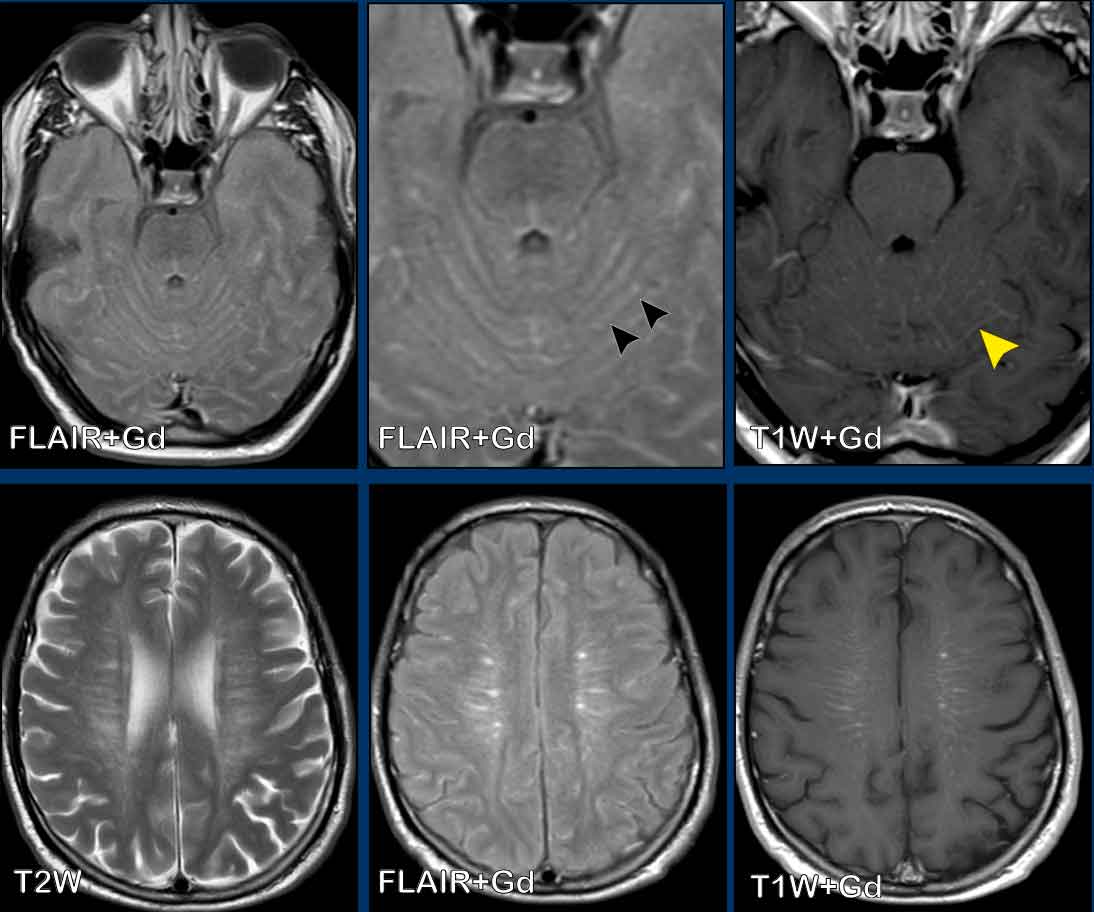
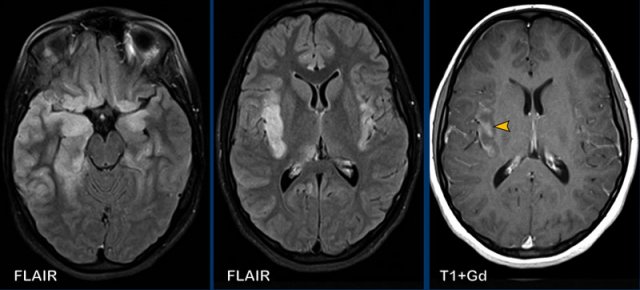
These images are of a 55-year old immunocompromised patient, who presented with cognitive complaints and headache.
Images
FLAIR shows non-supressed enhancing CSF in the subarachnoid
space.
Look along the cerebellar foliae, these are hyperintense on FLAIR (black arrowheads).
There is faint leptomeningeal enhancement (yellow arrowhead).
Furthermore there is high FLAIR signal at the
perivascular spaces in the semioval centre with enhancement.
Conclusion
This turned
out to be cryptococcal meningitis.
The spread
along the perivascular spaces in an immunocompromised patient is suggestive.
Sometimes in these patients there are also pseudocysts.
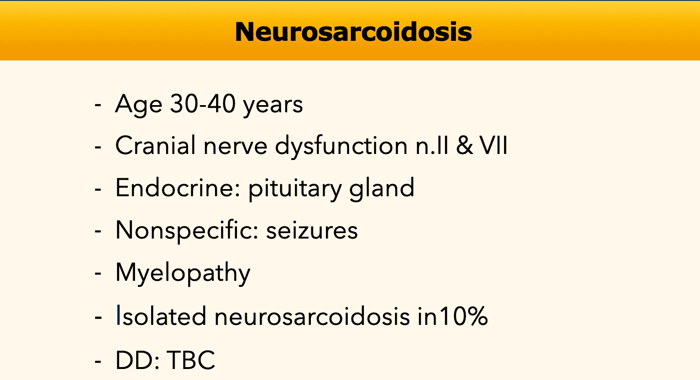
Neurosarcoidosis
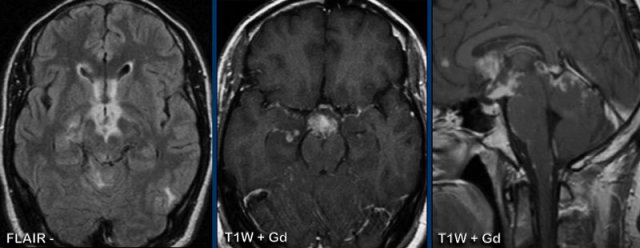
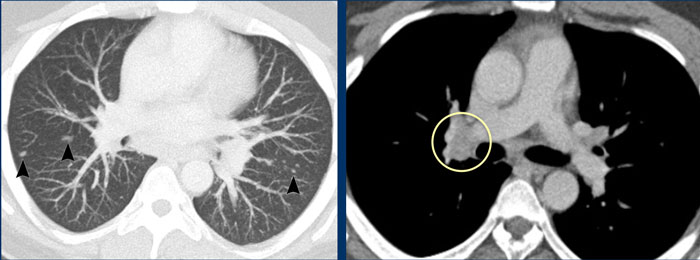
These images are of a 31-year old male, who presented with headache and hemihypesthesia.
Images
FLAIR demonstrates high signal at the basal structures, with enhancement at and around
the basal cisterns and vallecular cisterns.
These findings are compatible with the diagnosis of basal meningitis.
Meningitis at the base of the brain is usually caused by sarcoid, tuberculosis, syphilis, or any other low-grade chronic granulomatous process.
For this reason a chest CT was performed.
Continue with the CT-images...
The chest CT shows the typical findings of sarcoid.
There are small nodules along the fissures in a perilymphatic distribution and enlarged hilar nodes.
Sarcoid
can have different neurological and radiological presentations.
The cranial nerve symptoms are the result of basal meningitis.
In most cases there are also abnormal chest findings.
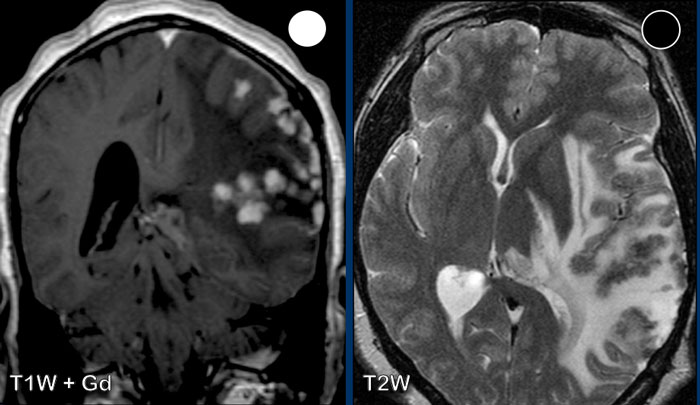
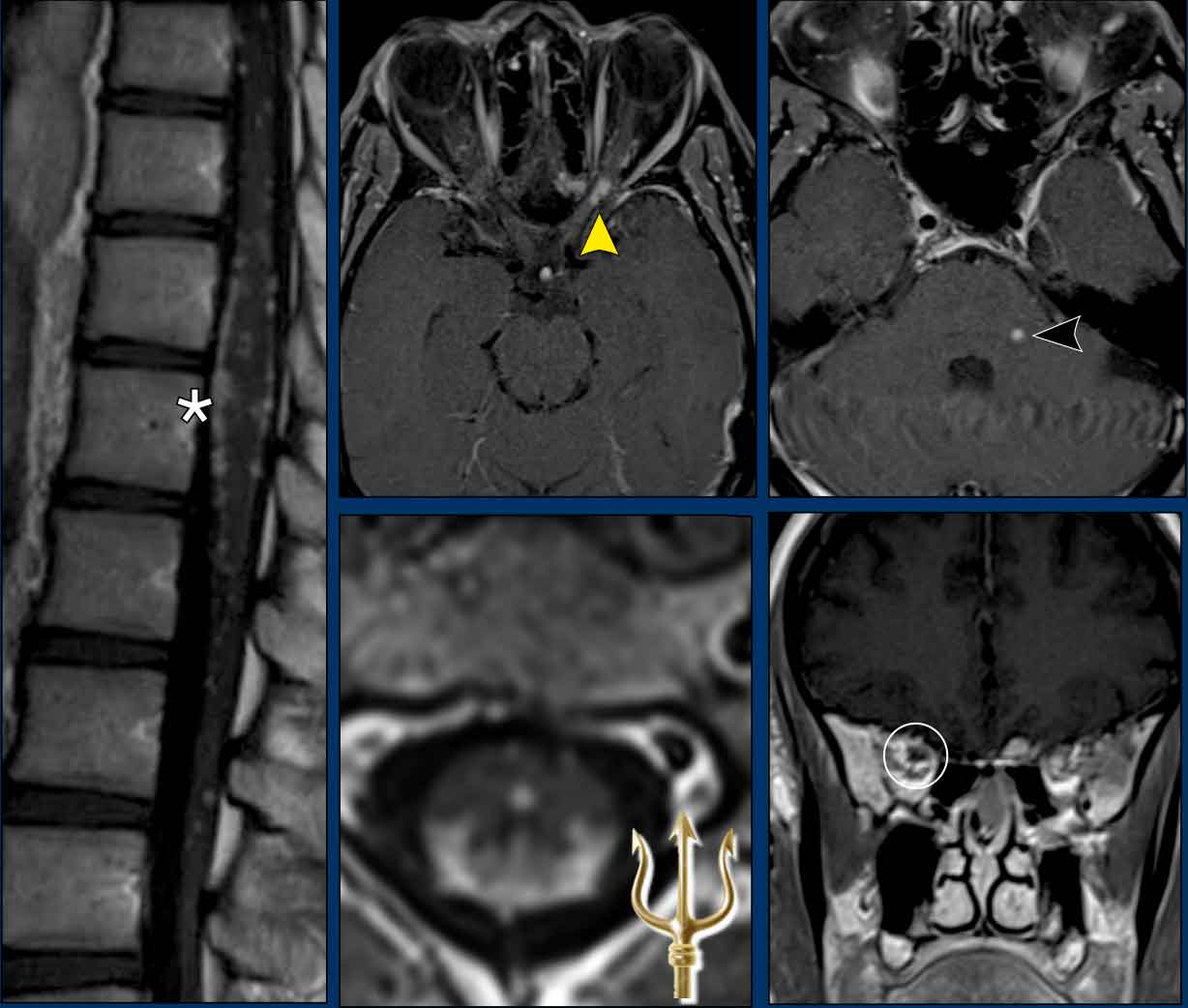
This patient has mutiple leptomeningeal nodules
They have high signal post contrast and relatively low signal on T2-weighted images, compatible with granulomatous
nodules.
This proved to be neurosarcoidosis.
Classical spinal neurosarcoidosis may present with the ‘trident’ sign, where there is enhancement of the leptomeninges and peripheral white matter (*) and central canal of the spinal cord.
In this patient there was also enhancement of the trigeminal nucleus (black arrowhead), the dura and both optic nerves.
The enhancement around the left optic nerve is best seen on the axial image (yellow arrowhead), while the enhancement on the right is best seen on the coronal image (white circle).
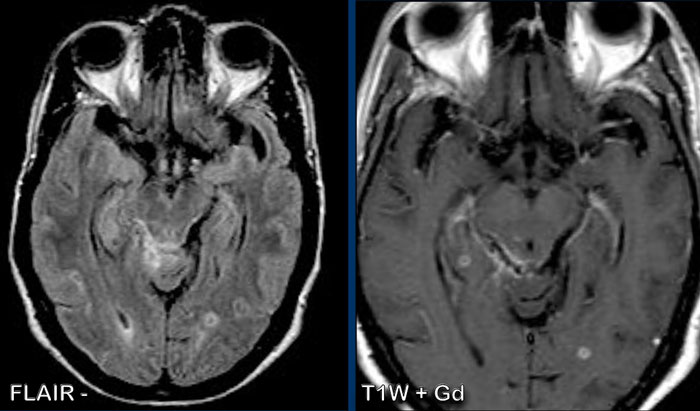
In this companion case there is high
signal intensity along the basal cisterns on FLAIR-images and leptomeningeal
enhancement along the ambiens cistern and tegmentum.
Note the small enhancing foci in the right hippocampus and left occipital lobe.
This turned out to be a tuberculous meningitis.
Meningeal carcinomatosis
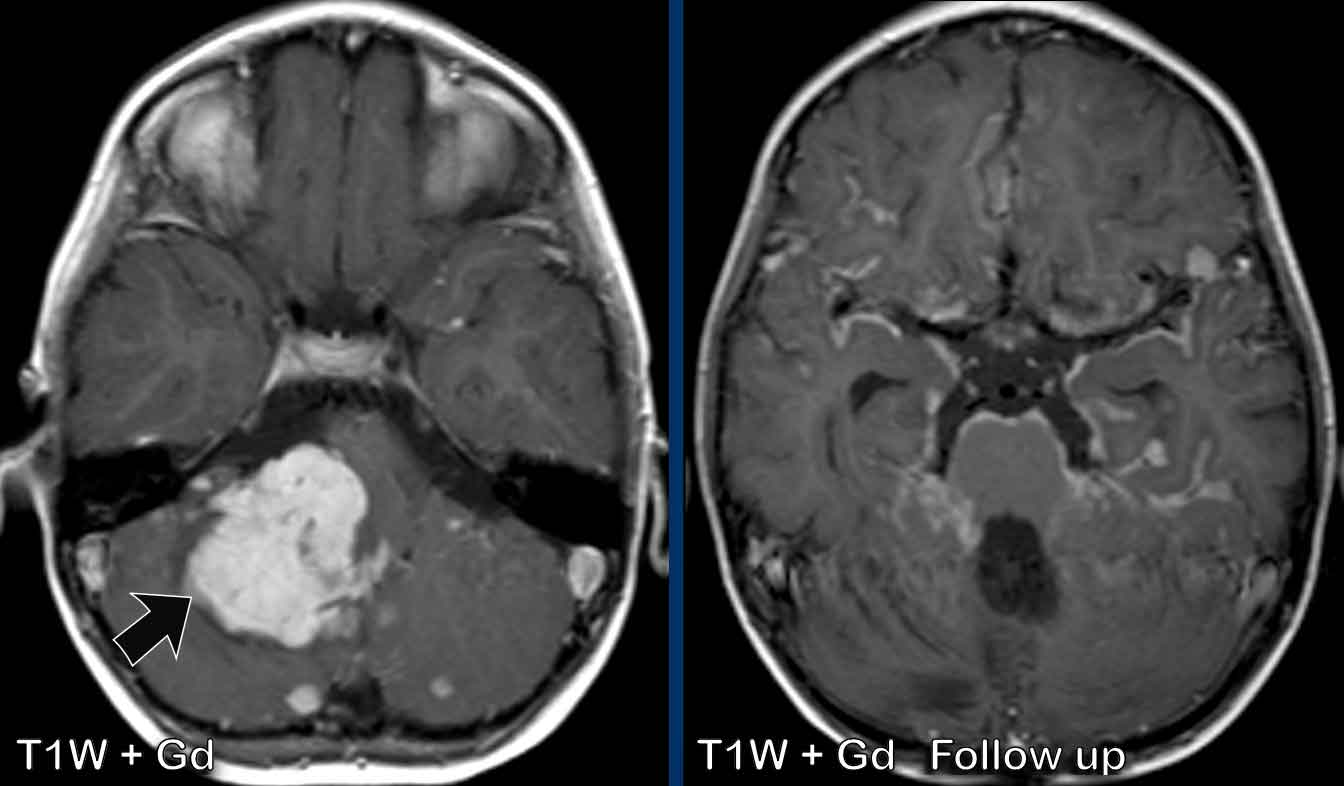
These images are of a 9-year old boy who is known with a posterior fossa medulloblastoma.
Images
The medulloblastoma presents as a large enhancing mass (arrow).
There are many small enhancing foci as sign of leptomeningeal metastases.
At follow-up after surgery and
radiotherapy there is irregular and nodular leptomeningeal enhancement.
This
“sugarcoating” enhancement is well demonstrated at the pons and the lining of
the vallecular cisterns.
Depiction
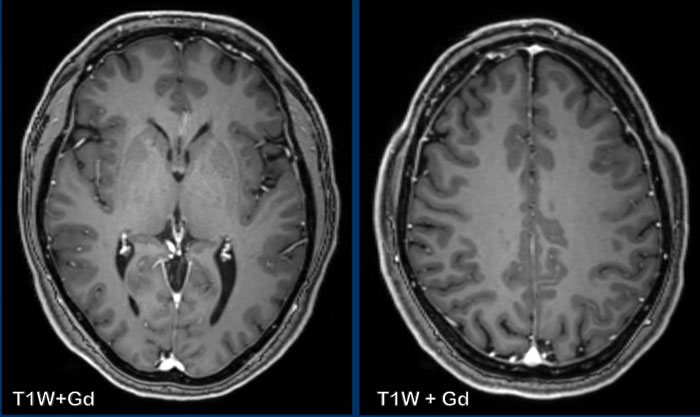
of leptomeningeal foci and enhancement can be improved by using contrast-enhanced
FLAIR.
As with meningitis also look at the subarachnoid space at non-contrast FLAIR.
Normally on these images the CSF is suppressed, but in case of pathology the CSF appears more
hyperintense.
A helpful clue for metastasis as differential for meningitis is
the appearance of thick nodular enhancement and the presence of intracerebral
and dural metastases.
Always check the cranial nerves for enhancement.
The clinical signs and history of the patient can be a helpful clue.
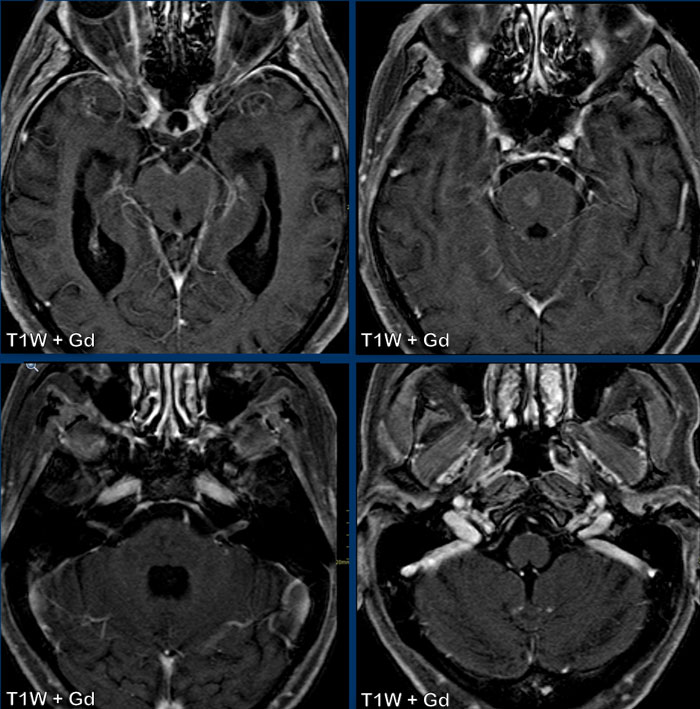
This is a patient with lungcancer which was complicated by carcinomatous meningitis.
Can you tell which cranial nerves are involved?
Now on these images it is very difficult to see, but if you were able to scroll through the enhanced MRI, you would notice that the following cranial nerves show pathologic enhancement:
- N.III (yellow arrow)
- N.V & n.VI (orange arrows)
- N.VII & n.VIII (blue arrow)
- N.IX t/m XI (white arrow)
Also note the pontine metastasis.
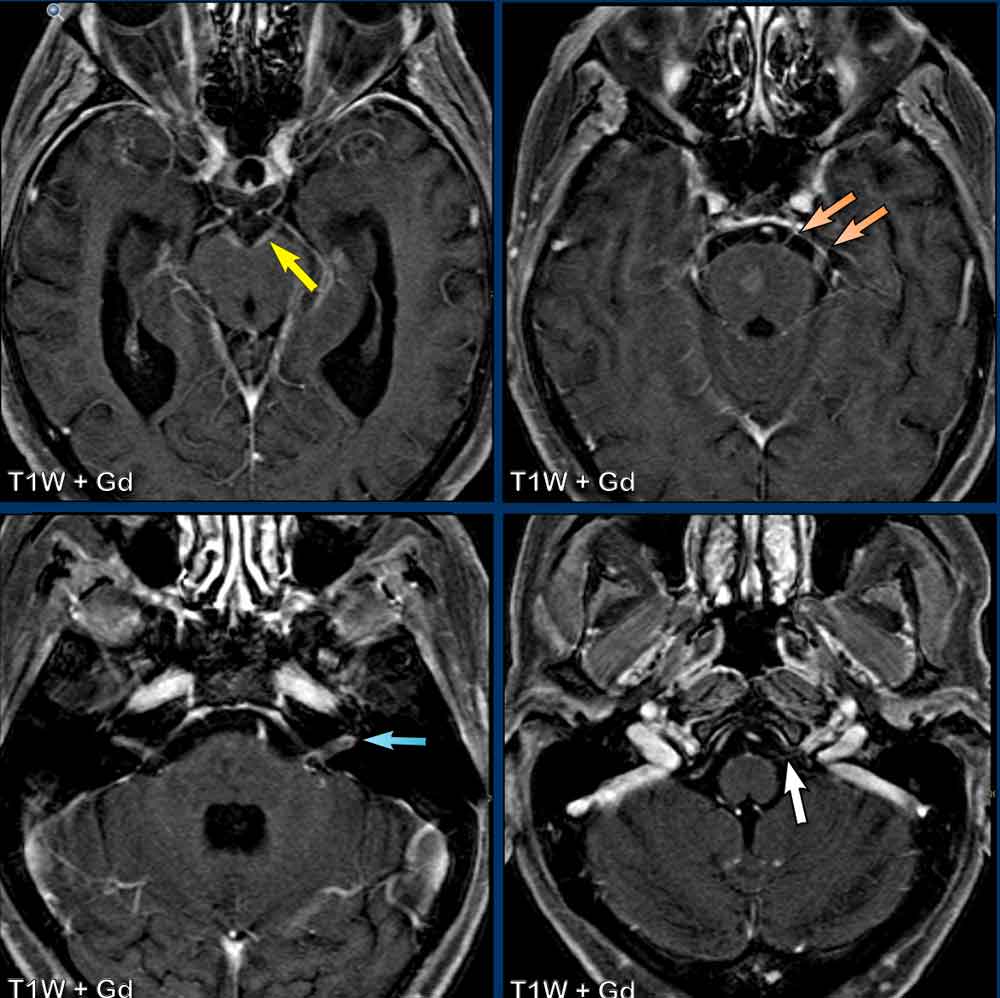
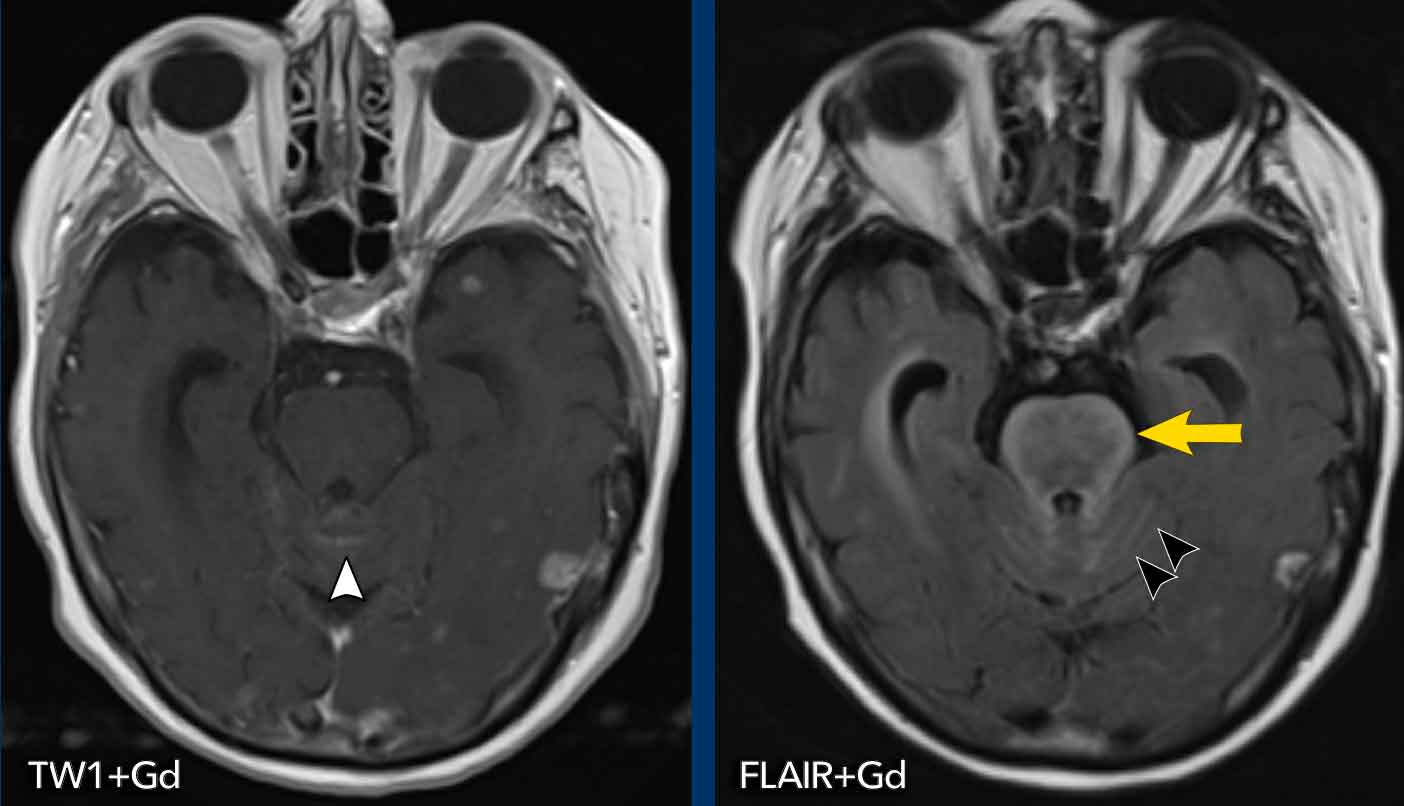
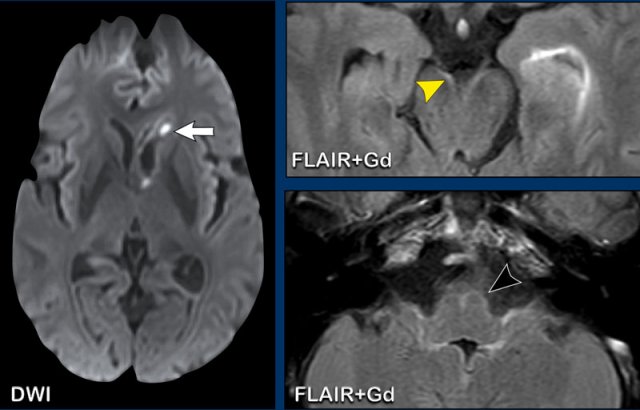
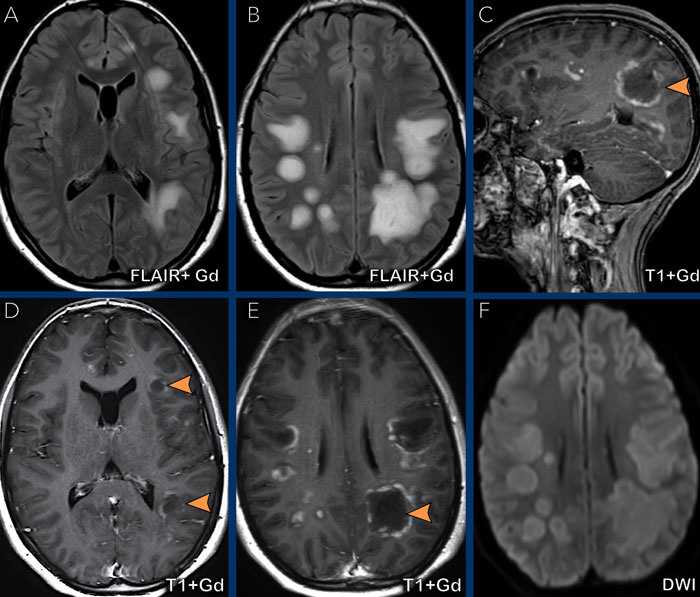
These examples show the advantage of FLAIR+Gd over T1W+Gd in a patient with lung cancer with cerebral metastases and carcinomatous meningitis.
Images
The FLAIR-image better shows the leptomeningeal enhancement around the pons (yellow arrow) and in the cerebellar foliae (black arrowheads).
Gyral pattern
The gyral pattern of enhancement is enhancement of the
cortex, most frequently seen in ischemia as a result of reperfusion during the healing
phase in subacute and acute ischemia
This can be caused by
luxury perfusion and/or cortical laminar necrosis.
Another cause of gyral enhancement is the vasodilatation phase of migraine headache and posterior reversible encephalopathy syndrome (PRES).
SMART is Stroke-Like Migraine Attacks After Radiation Therapy, which is an uncommon delayed complication of cerebral radiotherapy.
Subacute infarction
These images are of a 86-year old man who has a wobbling walk since a couple of weeks.
Study the images and then continue reading.
What are typical findings in this case?
Typical findings:
- Both grey and white matter are involved which is typical for infarction
- The involved area has a wedge shape
This type of gyral enhancement is the result of luxury perfusion with a disturbance of the blood-brain barrier and some neovascularization.
Continue with more images of this patient..
Question: what is the hyperintensity on the non-contrast T1W-image?
Images
The FLAIR shows an infarction with cytotoxic edema and
swelling of the gyri.
The hyperintensity on the non-contrast T1W-image is called laminar necrosis and although first described
as anoxic encephalopathy, it represents cytotoxic oedema with degradation of
proteins within the metabolic active cortex.
It is a poor prognostic
indicator.
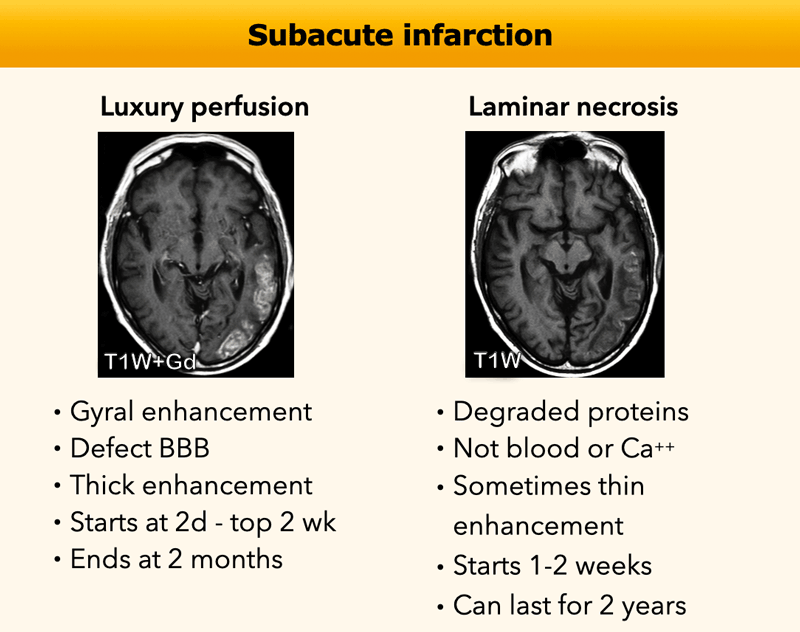
In this table the findings in luxury perfusion and laminar necrosis are summarized.
In patients who are treated with intra-arterial thrombectomy, the gyral enhancement can start earlier.
Sometimes it can be difficult.
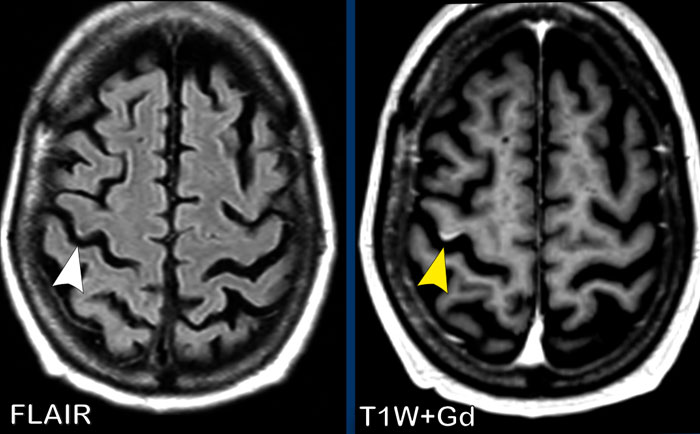
This patient had a history of breast cancer.
An MRI was done because she had some neurological failure.
On the FLAIR image there is a tiny hyperintense spot (white arrow).
Now this could have been diagnosed as a possible metastasis, but on the T1W-image with Gd there is definitely linear gyral enhancement.
This makes a small subcortical infarction the most likely diagnosis.
A follow up scan (not shown) was performed and definitely excluded the possibility of a metastasis.
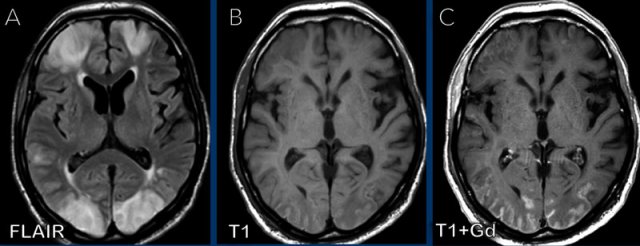
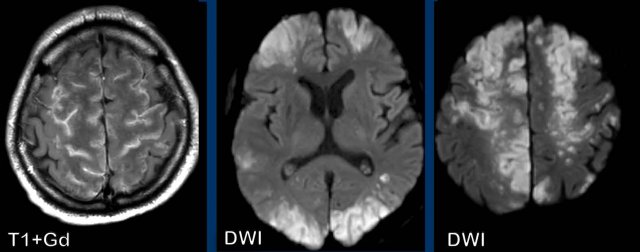
This is a patient with COVID infection, which was complicated by clotting problems and this resulted in multiple infarctions.
Notice the gyral pattern of the enhancement.
Continue with more images of this patient...
Again notice the gyral enhancement on the T1W+Gd images as a result of luxury perfusion and notice the widespread diffusion restriction on the DWI-images.
Can you tell which vascular areas are involved?
These areas are called the watershed or border zone areas.
A border zone area receives a dual blood supply from the most distal branches of two large arteries.
In times of systemic hypoperfusion, such as in disseminated intravascular coagulation or heart failure, these regions are particularly vulnerable to ischemia because they are supplied by the most distal branches of their arteries, and thus the least likely to receive sufficient blood.
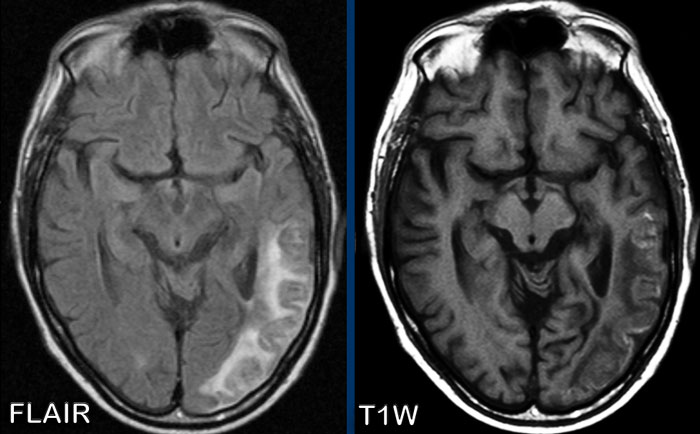
SMART
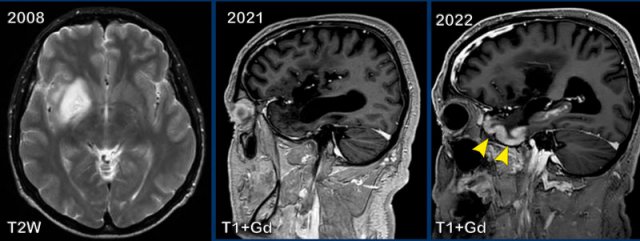
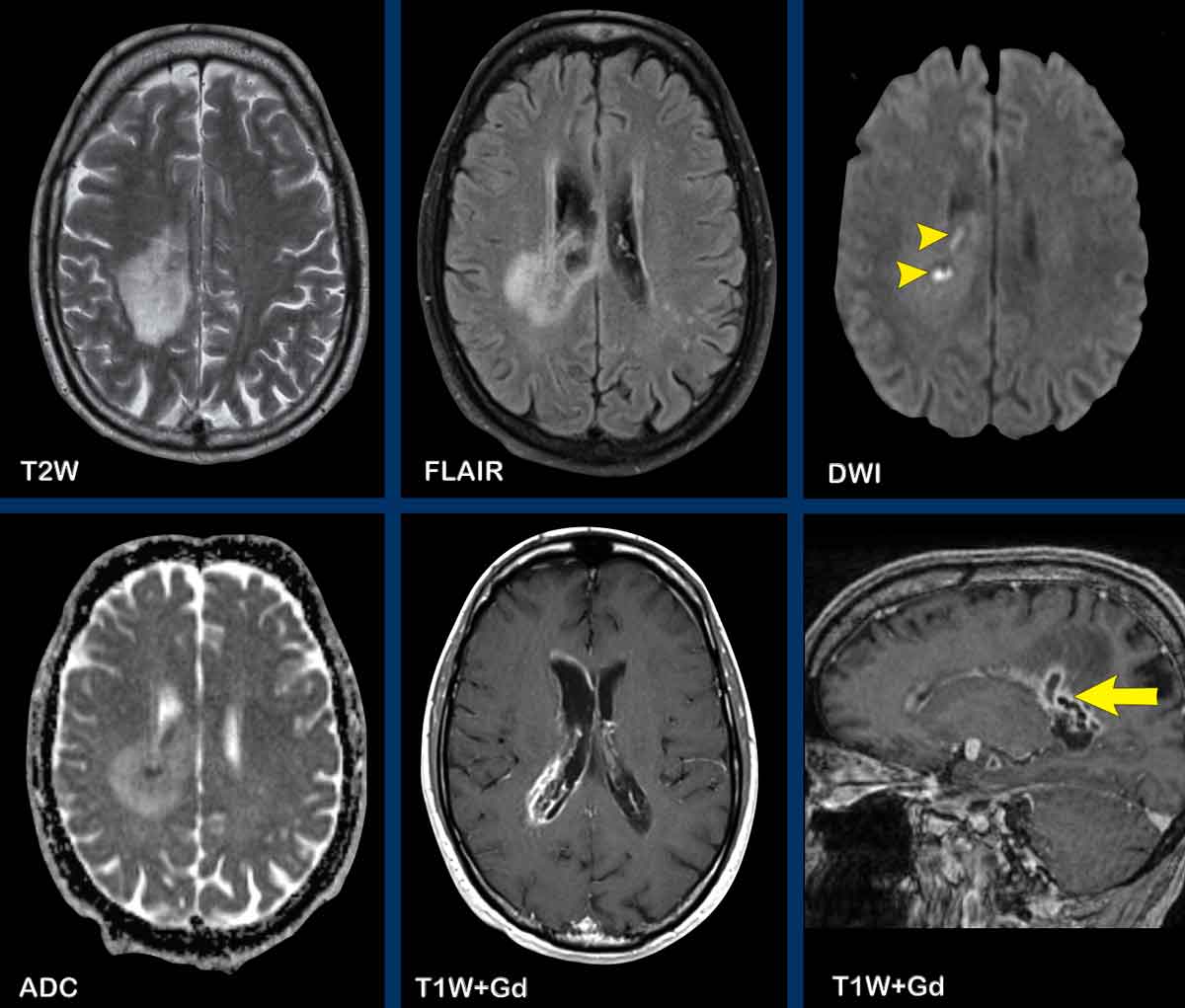
These images are of a 59-year old man, who had a partial resection of a glioma in 2008.
In 2016 there was progression of the tumor which was treated with radiotherapy followed by chemotherapy.
In 2021 there was no sign of residual tumor and in 2022 this patient presented with migraine.
Images
In 2008 a tumor is seen as a lesion with high signal on T2W
at the right basal ganglia and insular region.
In 2021 everything is stable, but in 2022 there is gyral
enhancement of the grey matter of the temporal lobe (arrowheads).
Continue with two more images of this patient...
Images
DWI shows cortical diffusion restriction in the right temporal lobe.
The sagittal T1W+Gd-image at a different level again shows the gyral enhancement pattern.
This is called SMART (Stroke-like Migraine Attacks after Radiation Therapy).
It is an uncommon delayed complication of cerebral radiation therapy characterized by cortical swelling and gyral enhancement.
These patients usually present with migraine, but seizure and hemiparesis is also a possible presentation.
In the context of prior brain radiotherapy this should raise the suspicion of SMART syndrome.
Prompt diagnosis is essential to avoid unnecessary invasive investigations.
It is a self limiting disease.
It is a diagnosis per exclusionem and you have to rule out ischemia, PRES and seizures.
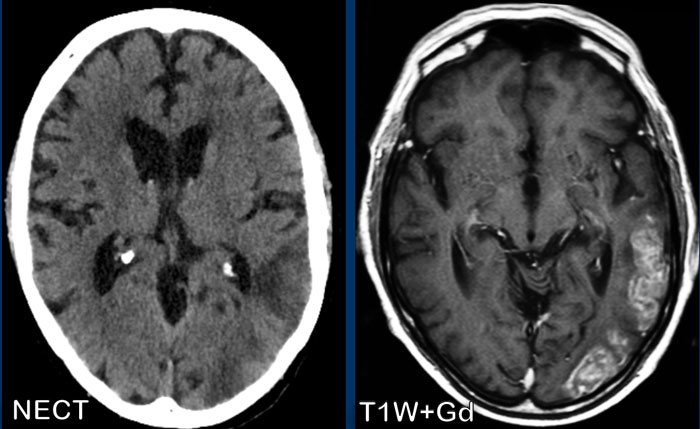
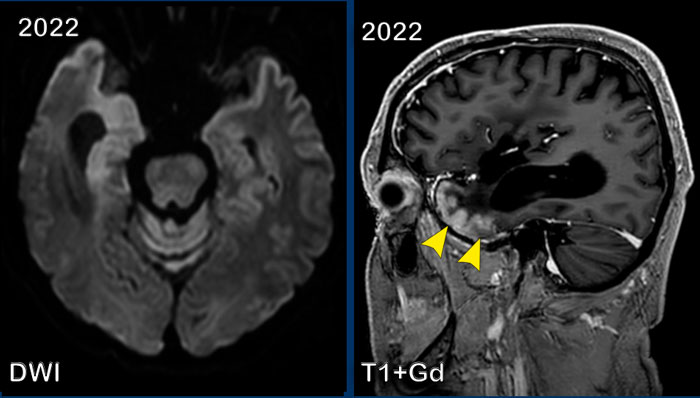
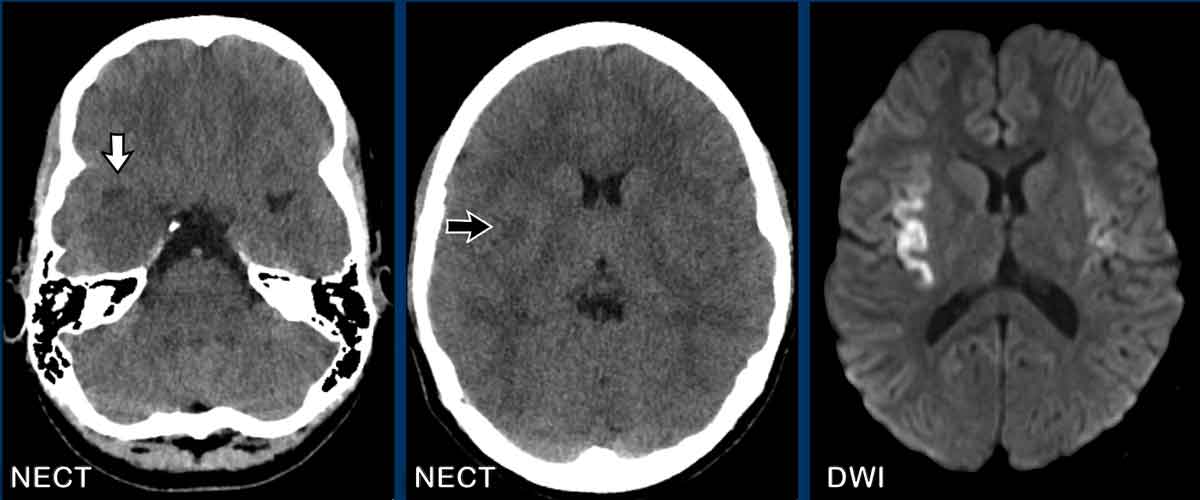
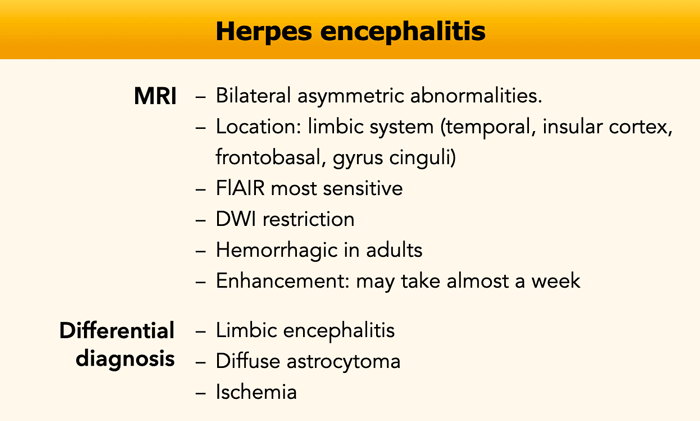
Herpes encephalitis
A 13-year old girl was admitted to the hospital with acute headache and confusion.
Images
FLAIR images show widespread hyperintense areas in both temporal lobes and insula.
This is more pronounced on the right side where the T1W+Gd
shows gyral enhancement of the insular cortex.
This is a typical case of Herpes encephalitis.
Continue with more images of this patient...
Notice how subtle the abnormalities are on the NECT compard to the findings on MR.
The right temporal lobe is more hypodense compared to the
left with some compression of the right temporal horn (white arrow).
Note also
the small hypodensity at the insular ribbon (black arrow).
CT is less sensitive than MRI and can detect abnormalities
only in half to two-thirds of the patients.
It may take 3-4 days to manifest
the changes in the temporal or frontal lobes.
Hypodensities, hemorrhage and
edema are often noted, while contrast enhancement may take almost a week.
The DWI
shows diffusion restriction on both sides.
MRI
is more sensitive and subtle abnormalities as diffusion restriction can be
present at an early stage.
In case of suspicion a lumbar puncture is warranted
and prompt treatment should be started.
Herpes encephalitis
Herpes encephalitis is a reactivation of the HSV-1 virus which is located in the trigeminal ganglion.
Herpes encephalitis has a bimodal spread.
It is seen in young children and in patients over fifty.
Limbic encephalitis
Limbic encephalitis can present with similar imaging findings, but usually has a more indolente course, whereas herpes encephalitis
presents more acutely.
It is a paraneoplastic or auto-immune disease where neuronal antibodies attack the cells in the limbic system.
Antibodies can sometimes be found in the CSF, but a normal CSF and brain imaging does not exclude the diagnosis.
Patients are treated with immune therapy.
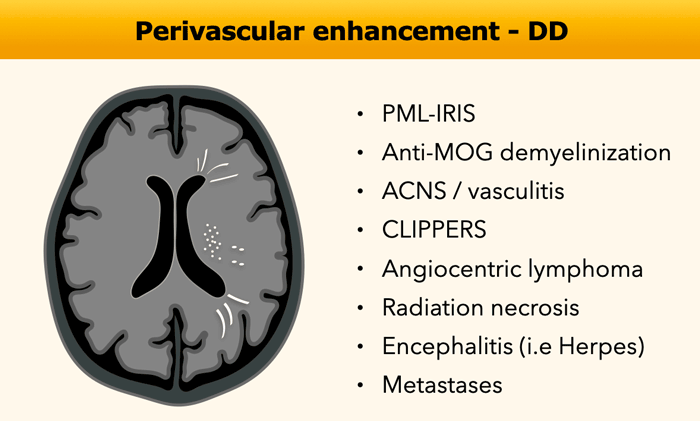
Vascular / Perivascular
Perivascular enhancement is a linear type of enhancement
along the smaller vessels and in the perivascular space.
On axial images this type of enhancement can present as small
dots (see figure) or stripes in the distribution of the perivascular spaces.
The differential diagnosis of perivascular enhancement contains many rare diseases, which makes it difficult.
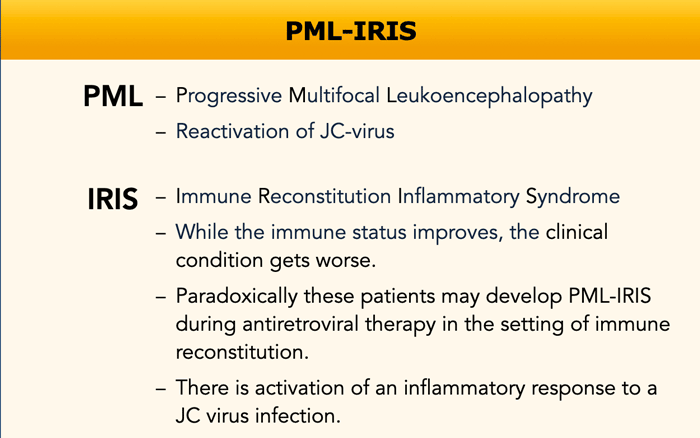
PML-IRIS
PML-IRIS is a paradoxical deterioration of the patient
following abrupt improvement of the patients immune function.
The improvement of the immune system results in an activation
of the inflammatory response to a JC virus infection.
It is seen in HIV patients following initiation of
antiretroviral therapy (HAART).
The same mechanism with development of PML-IRIS, that we see in these HIV patients, can be seen in MS patients who are treated with Natalizumab.
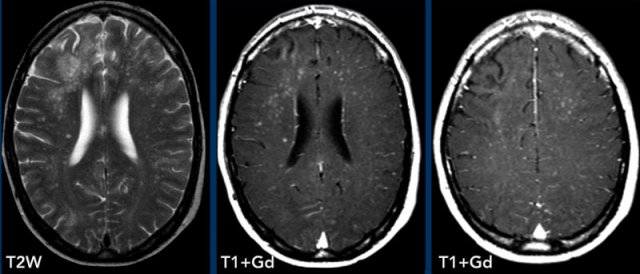
These images are of a HIV-patient who had started HAART therapy 2 weeks earlier and presented with behaviour disturbances.
Images
On the T2W-image there is hyperintensity of the right frontal white
matter.
Notice the punctate enhancement on the axial images, which is actually
linear on coronal or sagittal images (not shown).
This is a perivascular pattern and combined with the history the diagnosis is PML-IRIS.
Here another patient with HIV, who had started HAART two
months ago.
The CD4-count is good.
However, there is a progressive paresis and the patient is experiencing
more seizures.
Large bilateral white matter lesions are shown with punctuate
enhancement on the post-contrast T1W-Image.
The diagnosis PML-IRIS was made and the patient was treated with steroids.
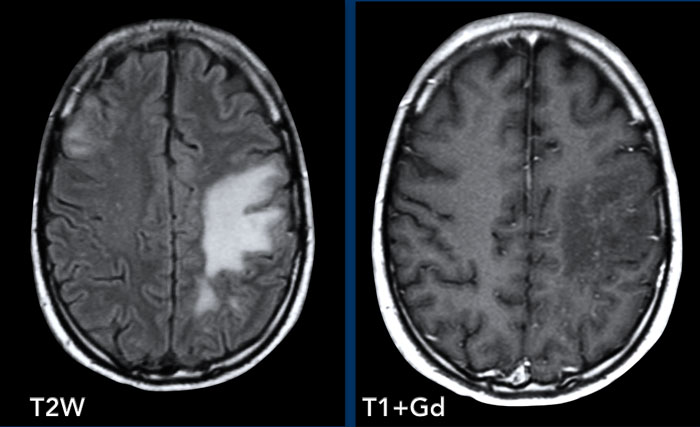
CLIPPERS
CLIPPERS is a Chronic Lymfocytic Inflammation with Pontine Perivascular Enhancement Responsive to Steroids.
It can be difficult to differentiate this lymphocytic inflammation from lymphoma and that is why some cases that were first diagnosed as CLIPPERS turned out to be lymphoma.
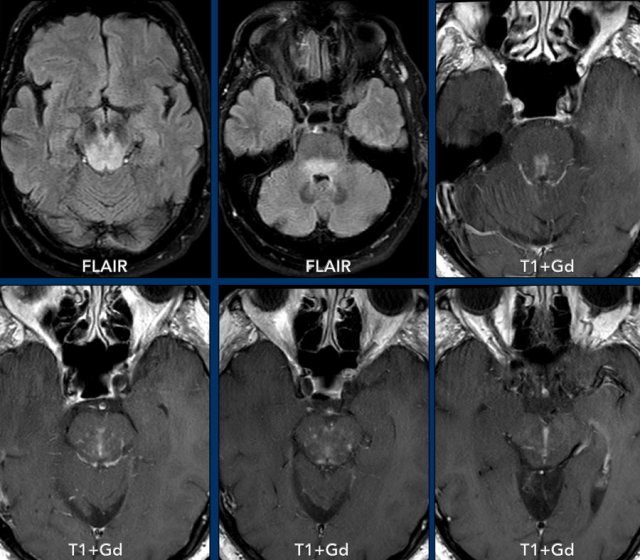
These images are of a 62-year old man who presented with loss of function of the oculomotor nerve on the left side.
Images
FLAIR images show widespread hyperintensity in the pons and
mesencephalon.
There is punctate and linear enhancement.
When we combine the punctate enhancement of different levels,
we can imagine that it actually is part of a linear or perivascular
enhancement.
Differential diagnosis:
- These findings are suggestive of CLIPPERS, although steroid response can only be evaluated after therapy.
- Pontine osmotic demyelination syndrome most often is more centrally located
- Ischemia shows restricted diffusion and no perivascular enhancement.
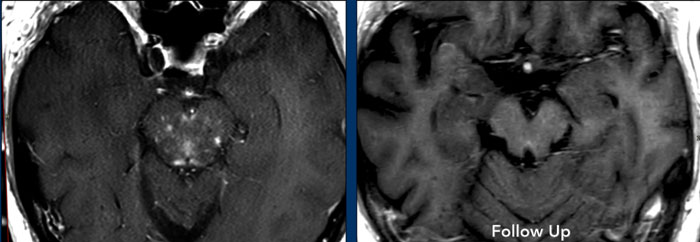
Continue with post-treatment images of this patient...
This patient was treated with steroids and the perivascular enhancement is not anymore seen on the follow up exam.
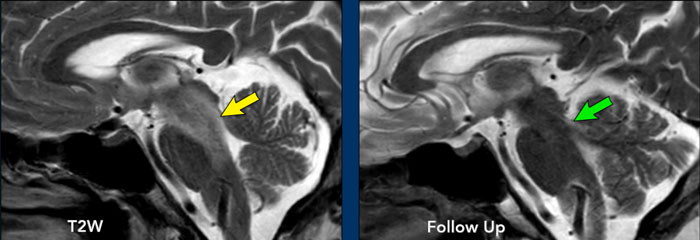
Continue with the sagittal images...
Also on the sagittal T2W-images the hyperintensity (yellow arrow) is gone on the follow up image (green arrow).
These images are of a patient with stage IV lungcancer who was on immune therapy.
She presented with nausea, vomiting and confusion.
Initially it was thought that this was PML-IRIS.
The treatment was stopped.
Tests however didn't find any sign of a JC-virus infection and the patient got worse.
Finally this proved to be metastases as a result of tumor emboli, that got stuck in the small vessels in the watershed areas.
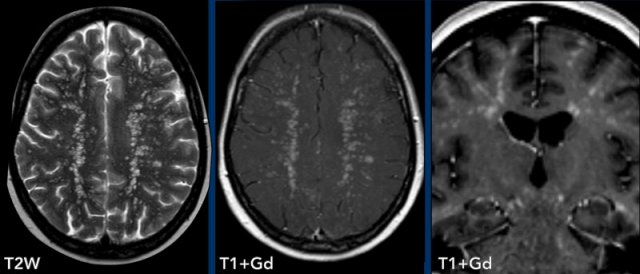
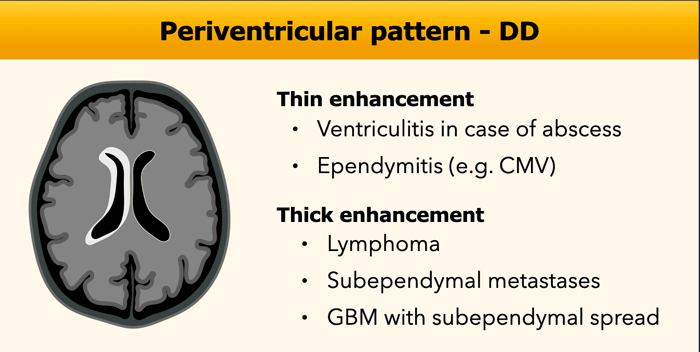
Periventricular
Periventricular enhancement follows the subependymal lining of the ventricles.
In case of thin enhancement this is most often caused by an infection, whereas one should think of tumor in case of thick periventricular enhancement.
Ventriculitis
These images are of a 62-year old male, who presented with headache, fever and lethargy.
Images
On the contrast-enhanced FLAIR-images there is a hyperintense lining of the left lateral ventricle representing thin enhancement, better
visible than on the contrast-enhanced T1 W images.
This proved to be a Lyme meningitis, which was complicated by ventriculitis.
Continue with some additional images...
There is restricted
diffusion in the left ventricle.
The leptomeningeal enhancement is well appreciated on the contrast-enhanced FLAIR-images (arrowheads).
This finding is not specific for lyme meningitis, also other infectious causes should be considered in the differential diagnosis.
When bilateral enhancement of the facial nerve is present, always consider lyme meningitis.
These images are of a patient with a parietal abscess.
Images
The abscess shows central diffusion restriction with a relatively thick enhancing wall.
The yellow arrowheads points towards the thin enhancement of the ventricular wall.
Conclusion
Intraventricular
extension of the abscess, which resulted in ventriculitis.
These images are of a 63-year old male, who presented with a small cerebral abscess (yellow
arrow) in the right semioval centre.
Notice that there is significant ventricular
involvement.
Next to the ventricular enhancement, there is diffusion
restriction in the abscess and the ventricle (arrowheads)
Lymphoma
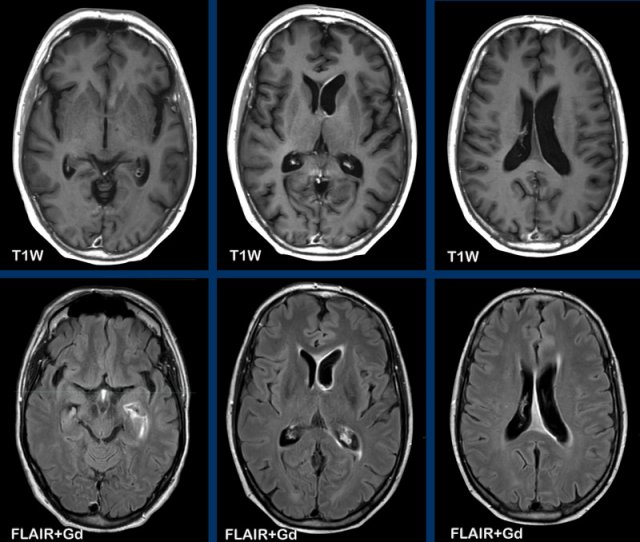
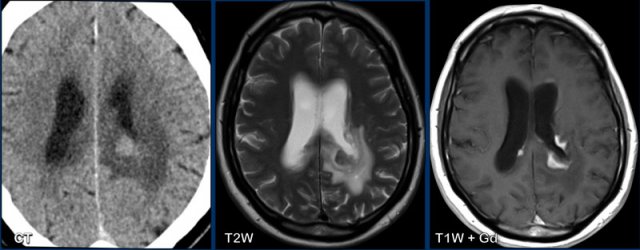
These images are of a 63-year old patient.
Images
CT shows a dense periventricular
lesion with surrounding edema.
On the T2W-image the lesion has a relatively low density. There is homogeneous enhancement of the lesion with multiple periventricular enhancing
lesions.
The density on the CT and the distribution are highly suggestive of lymphoma.
GBM subependymal spread
This patient was previously treated for a GBM and now has a recurrence in the left frontal lobe.
Images
There is thick enhancement along the left
lateral ventricle, which is subependymal tumor spread.
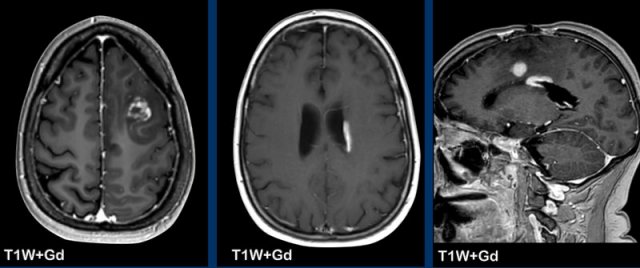
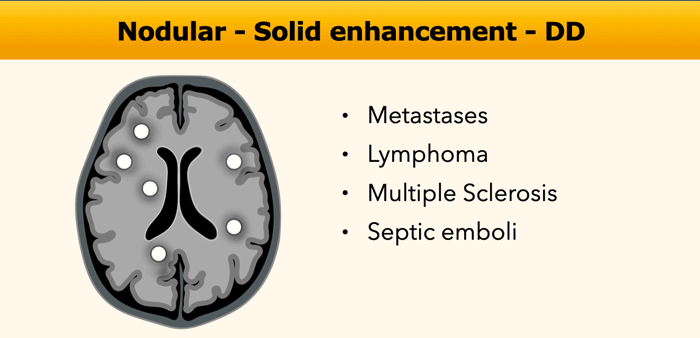
Nodular pattern
Solid nodular enhancement can be solitary or multiple, ranging from minuscule to larger lesions, with a wide differential diagnosis.
Always take a close look to the location of the lesions as this can aid in differential diagnosis.
On axial images normal vessels can mimic small nodular enhancement.
Metastases
First look at the images and then continue reading.
Question:
- What is the most likely diagnosis?
- Which findings are typical for this diagnosis?
The findings are:
- Multiple small enhancing nodules.
- Their location at the gray/white matter interface and in the watershed area is very typical for metastases as the tumor emboli get stuck in the areas where the caliber of the vessels is very small.
In 25-45% of the cases metastases can be solitary.
 Metastases in the watershed area (black arrow) and at the gray/white matter interface (white arrowheads)
Metastases in the watershed area (black arrow) and at the gray/white matter interface (white arrowheads)
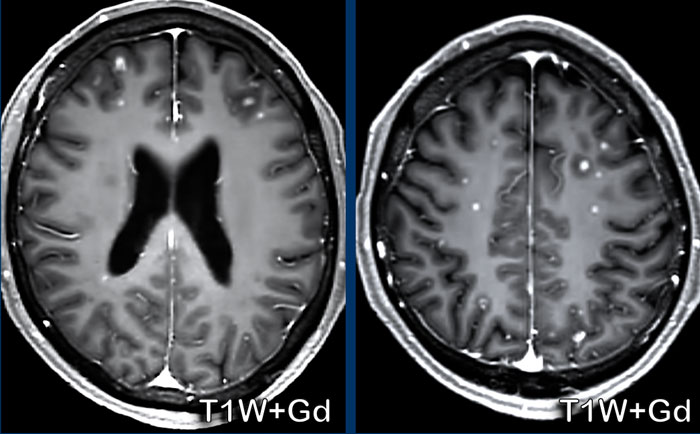
Here another patient with metastases.
Again notice the location in the watershed area (black arrow) and at the gray/white matter interface (white arrowheads)
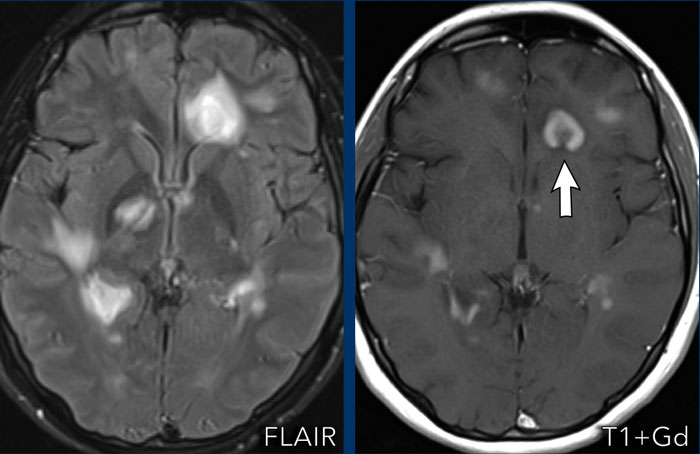
Lymphoma
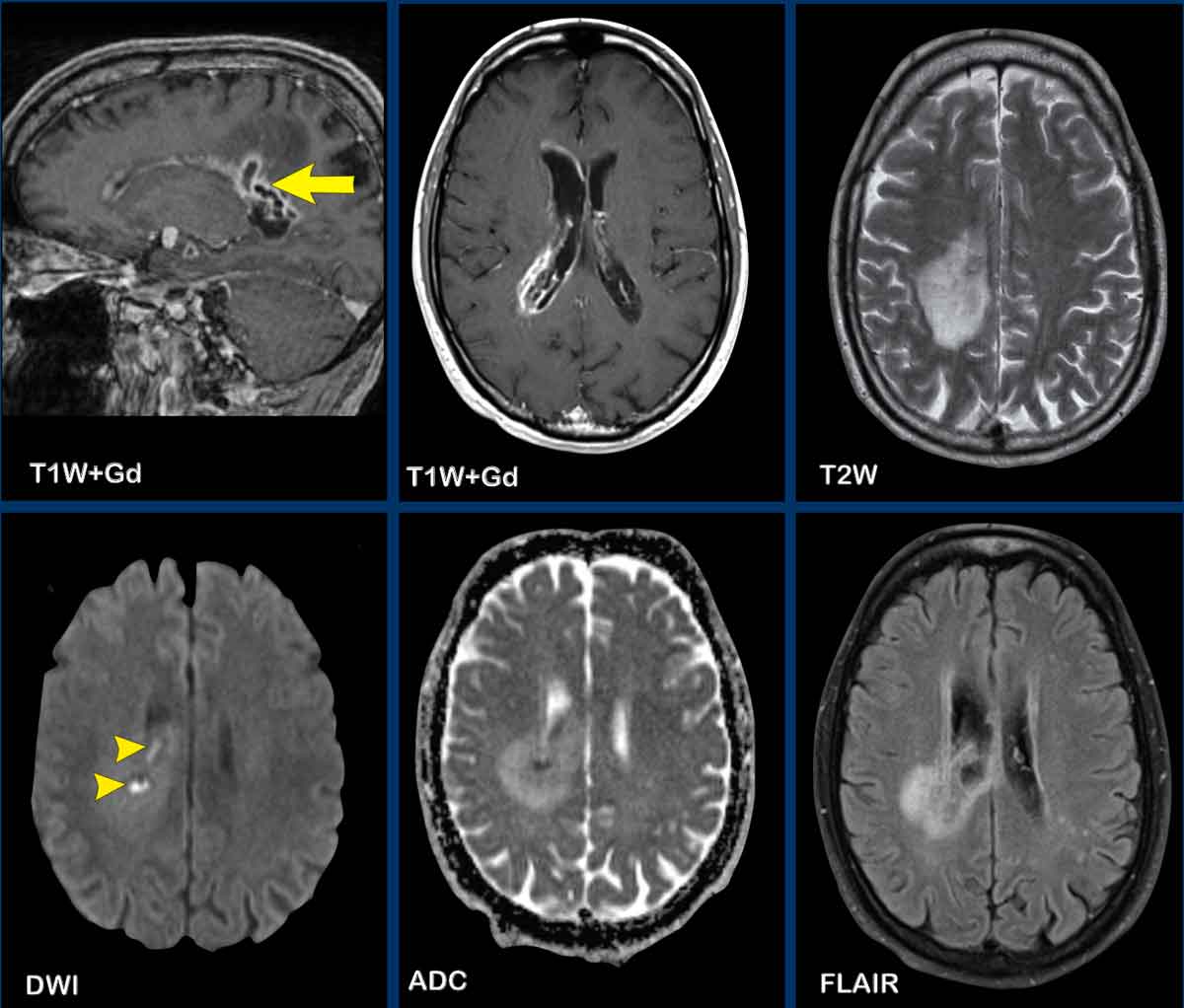
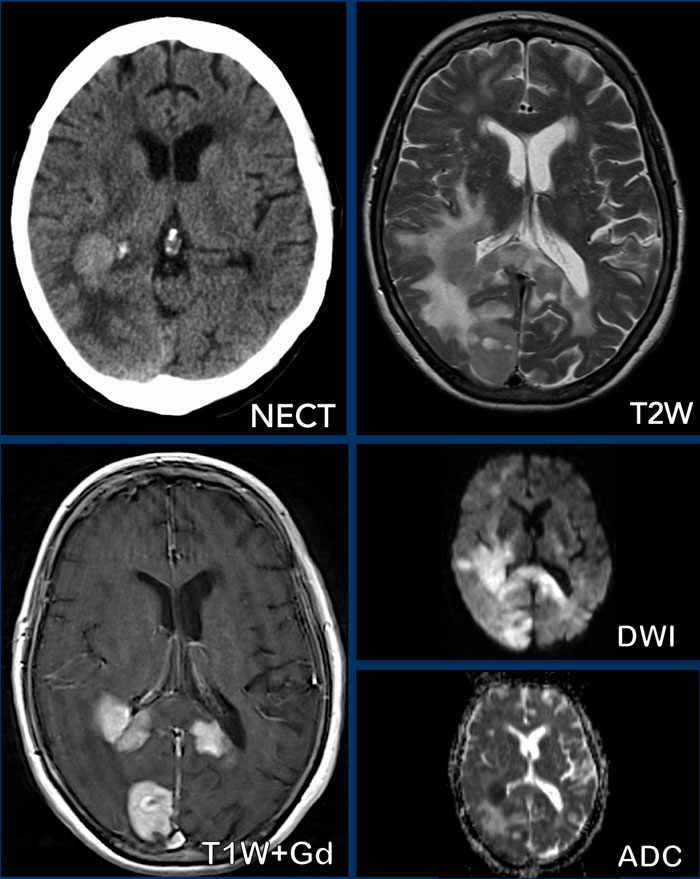
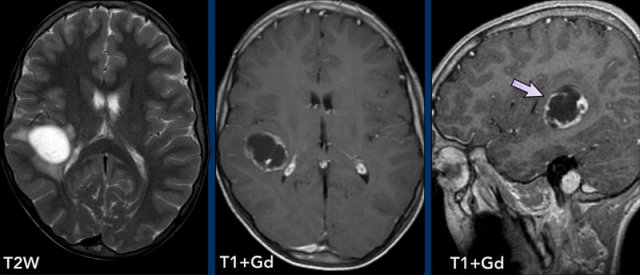
These images are of a 76-year old woman, who was confused after a fall.
First look at the images and then continue reading.
Question:
- What is the most likely diagnosis?
- Which findings are typical for this diagnosis?
The findings are:
- Hyperdense lesion on the NECT with some vasogenic edema.
- MR shows multiple lesions with solid enhancement and diffusion restriction.
- On T2W the lesions show a low signal intensity
- One lesion is located in the corpus callosum and another one is periventricular.
All these findings are typical for a primary CNS lymphoma, which is different from a systemic lymphoma.
These tumors make up for 6-7% of all CNS tumors and the histology is a B-cel NHL.
They are mostly located periventricular subependymal, in the corpus callosum and in the basal ganglia.
Always think lymphoma in a solid enhancing lesion which is located near the ventricles.
The hyperdense appearance on CT and the slight hypointensity on T2W-imaging, as well as the restricted diffusion are attributed to the dense cellularity of the lymphomatous tissue.
In immuno-compromised patients the enhancement can be ring-like.
This patient has a lot of edema, but in many cases the edema is very limited.
This is a 81-year old man with Waldenstrom disease.
A rare manifestation of Waldenstrom is CNS infiltration by lymphoplasmocytoid cells. This is called Bing-Neel syndrome.
Notice in this patient multiple solid enhancing lesions, which are all located in the periventricular area.
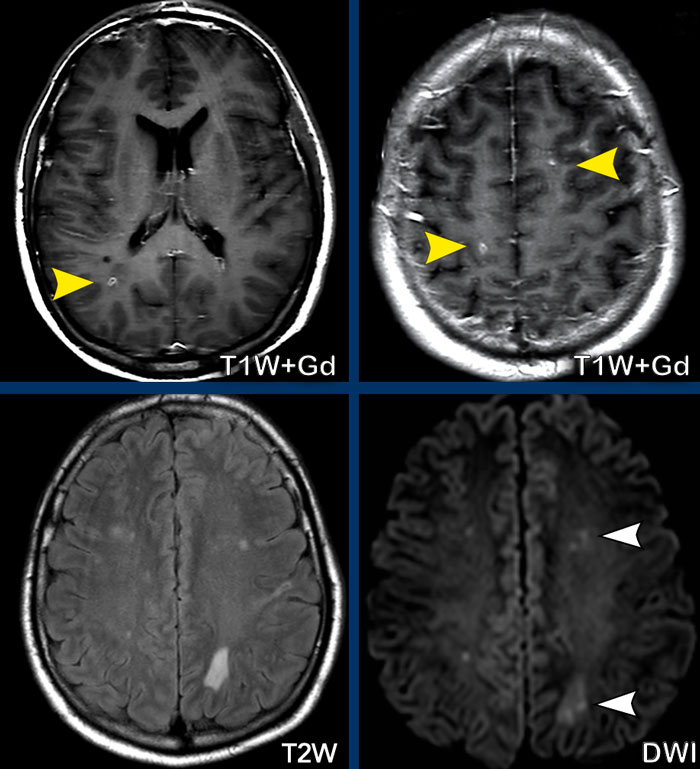
Septic emboli
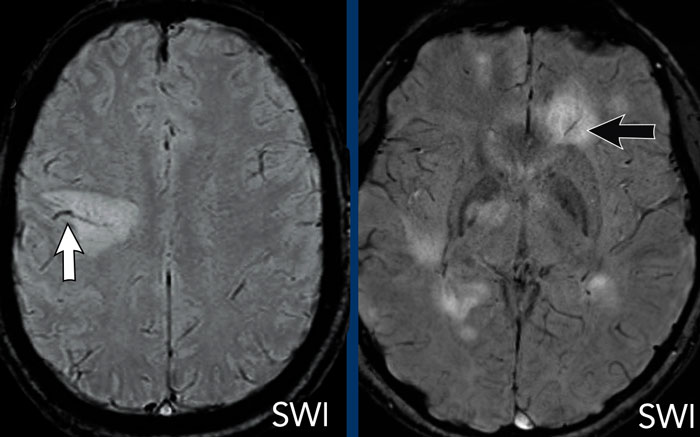
These four images are of a young patient with a pneumococal sepsis who deteriorated and became comatous.
Images
There are small enhancing nodules (yellow arrowheads) in the watershed areas and at the gray/white matter interface.
There is diffusion restriction (white arrowheads).
This pattern is identical to the previous cases.
Conclusion
This was regarded as septic emboli.
Multiple sclerosis
This patient is known with MS.
Notice that some of the hyperintense lesions, that are seen on the FLAIR
image, show enhancement on the T1W+Gd image. which is a sign of active disease.
The enhancing lesions
show different patterns of enhancement: nodular and (incomplete) ring.
The
lesions are also located in the corpus callosum.
This
is not a frequent location for metastases or ischemia, but commonly seen in MS.
The location of the
FLAIR abnormalities perpendicular to the ventricles (Dawson fingers), the
juxtacortical location of the white matter lesions and the incomplete
enhancement make the diagnosis of a d emyelinating disease, i.e. MS most likely.
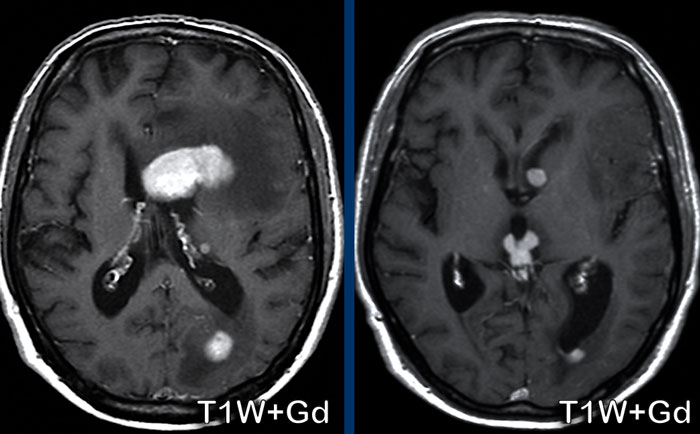
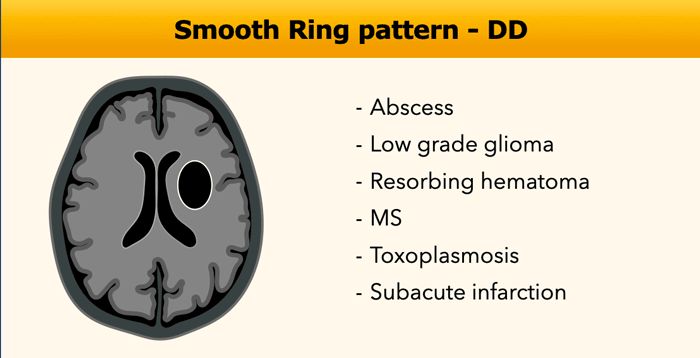
Smooth Ring
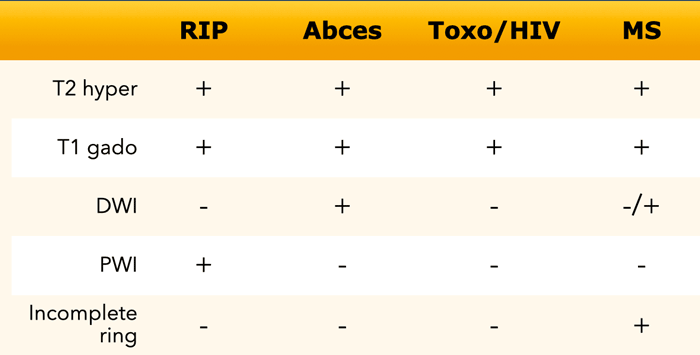
The differential diagnosis of ring enhancing lesions is shown in the table.
In this table some findings, that can help to differentiate between various ring-enhancing entities.
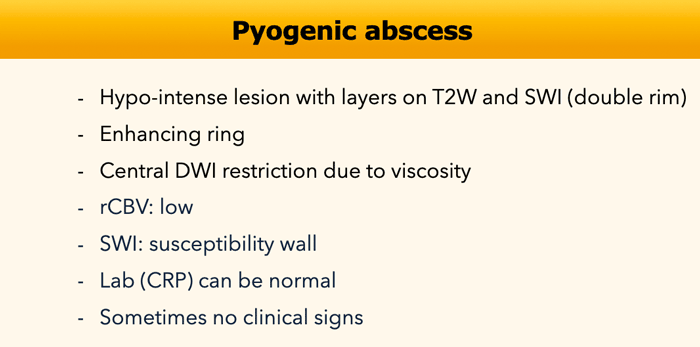
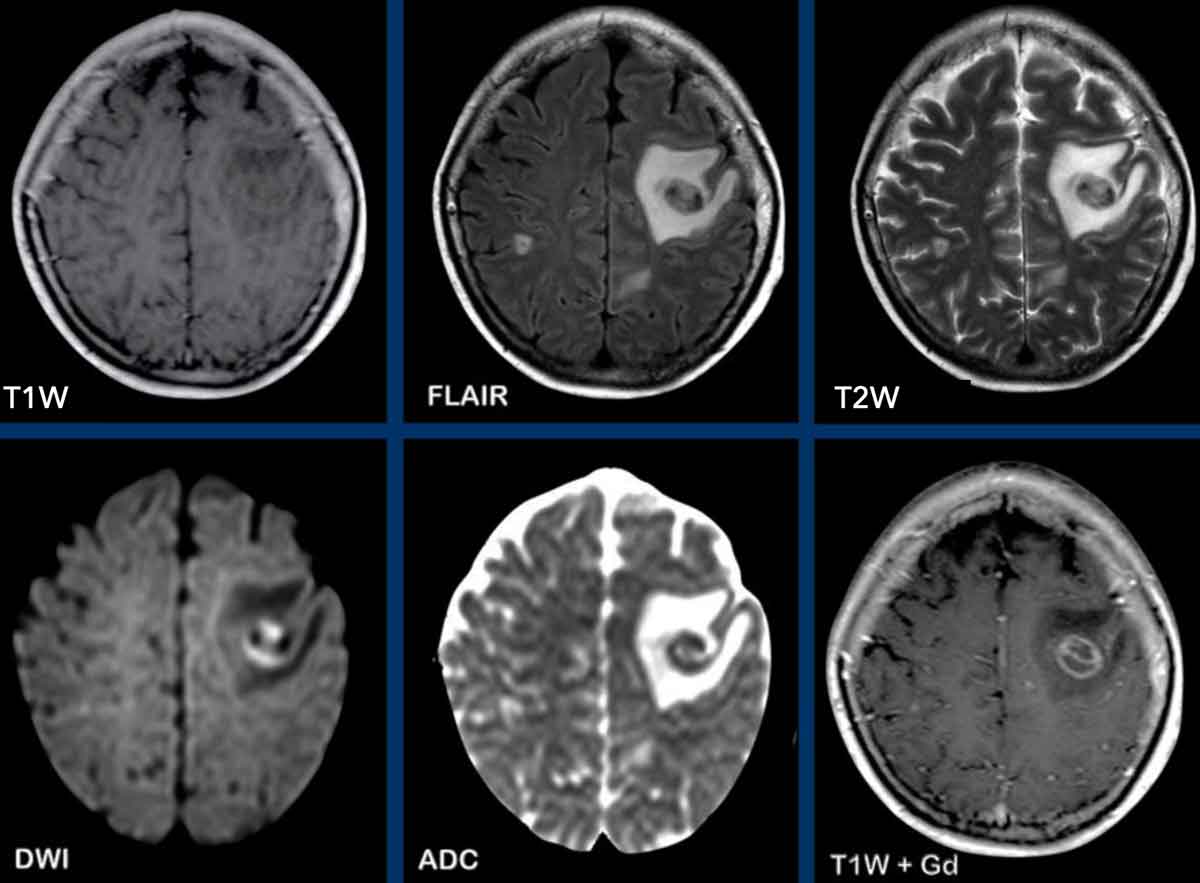
Pyogenic Abscess
The various MR-findings of a pyogenic abscess are shown in the table.
The most typical finding is a peripherally-enhancing lesion with central diffusion restriction.
The MR-findings can be false negative when there is bleeding into the abscess and it can be false positive when there is a tumor with infected central necrosis.
These images are of a 55-year old male with headache.
First look at the images and then continue reading.
Question:
- What is the most likely diagnosis?
- Which findings
are typical for this diagnosis?
The findings are:
- There are two ring enhancing lesions surrounded by edema
- On the T2W-image a double rim sign is present in the left frontal lesion.
- There is central diffusion restriction.
- There is smooth enhancement.
All these findings are
consistent with the diagnosis of cerebral abscesses.
A double rim on T2W-images can be seen in up to 75% of cases.
Classically there is a complete rim
enhancement and diffusion restriction, but sometimes there is incomplete enhancement as the abscess points
towards the ventricle, ready to empty the pus into the ventricular system.
You
can see the beginning of that process in the right frontal abscess.
When this abscess ruptures into the ventricle the rim will be interrupted and there will be
diffusion restriction within the ventricle.
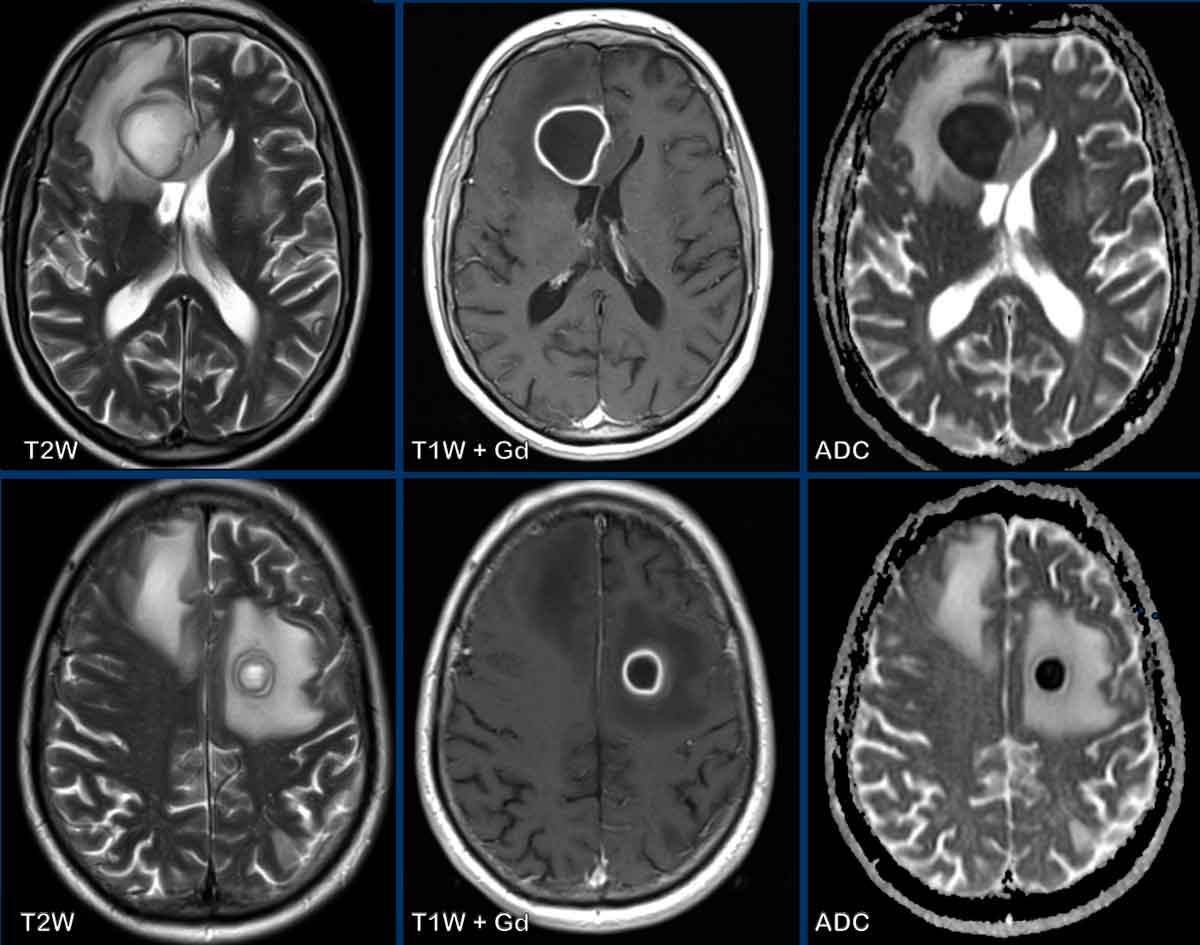
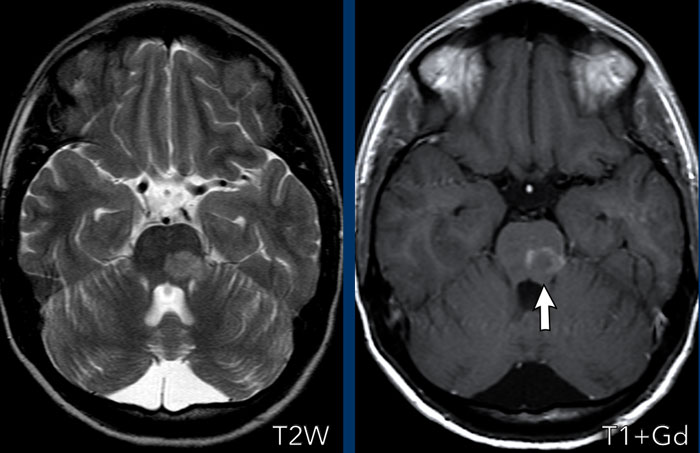
These images are of a patient, who presented with headache.
Images
There is a right parietal lesion, with rim enhancement and central diffusion
restriction.
SWI shows susceptibility at the rim, this is thought to be due to
paramagnetic free radicals, produced by macrophages.
There is also a
hemorrhagic spot at the ventral side, where diffusion is not restricted.
The faint enhancement
outside the inner rim, due to blood-brain-barriere leakage, can make
differentiation from a tumor difficult, but the restricted diffusion,
together with a low rCBV (not shown) makes the diagnosis of an abscess the most likely
Here a more difficult case.
This is a patient, who presented with acute cerebellar
signs.
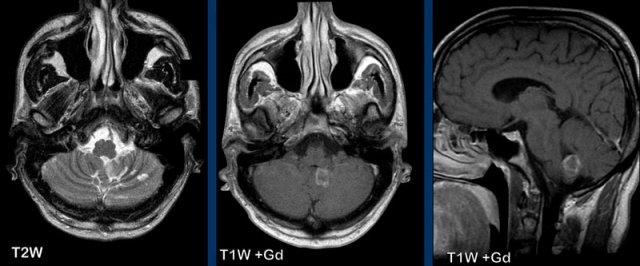
Images
On the T2W-image there is a hyperintense lesion, which shows rim enhancing after contrast
administration.
This is luxury perfusion in an enhancing subacute infarction.
Note also the older infarctions in the left cerebellar hemisphere.
When in doubt, follow-up imaging can help.
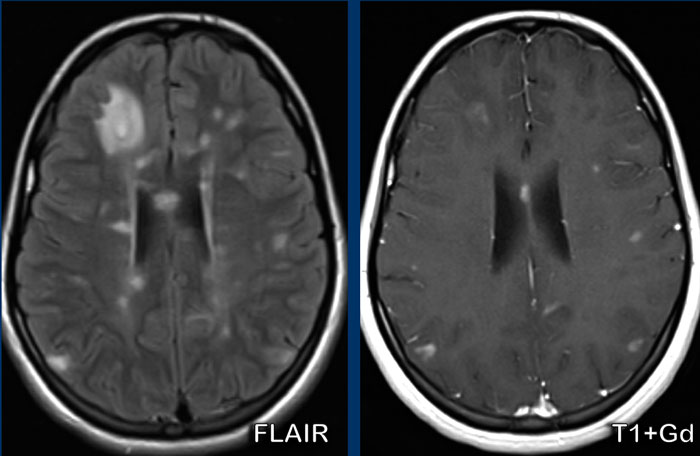
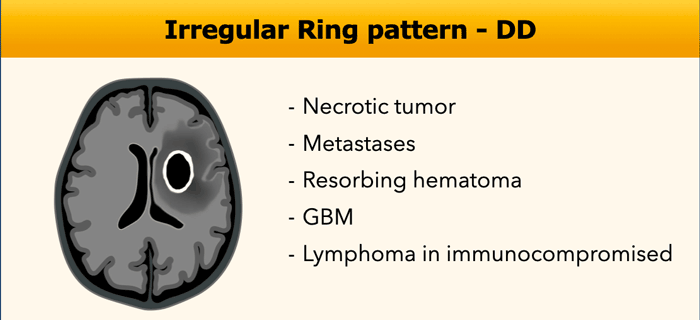
Irregular Ring
In the table the various causes of an irregular ring enhancement.
There is some overlap with smooth ring enhancement.
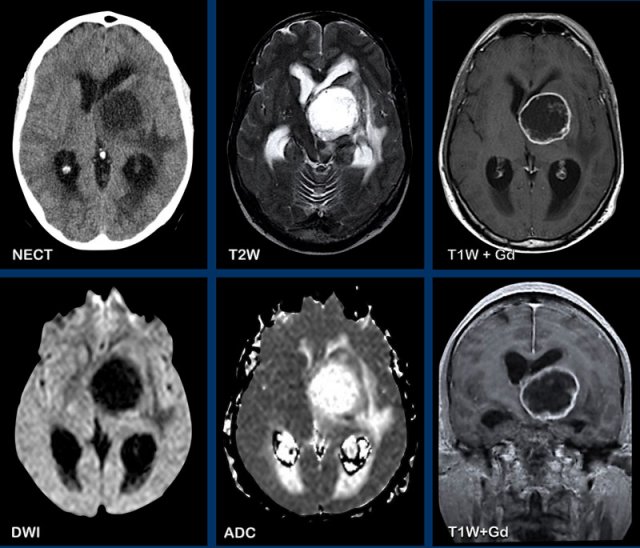
These images are of a 47-year old male, who presented with headache, vomiting and a right-sided hemiparesis.
Images
A ring enhancing lesion is present in the left basal ganglia.
Note the enhancing structures within the inner border of the
enhancement.
There is no diffusion restriction, which makes the diagnosis of an abscess unlikely.
This is a pathologically proven GBM.
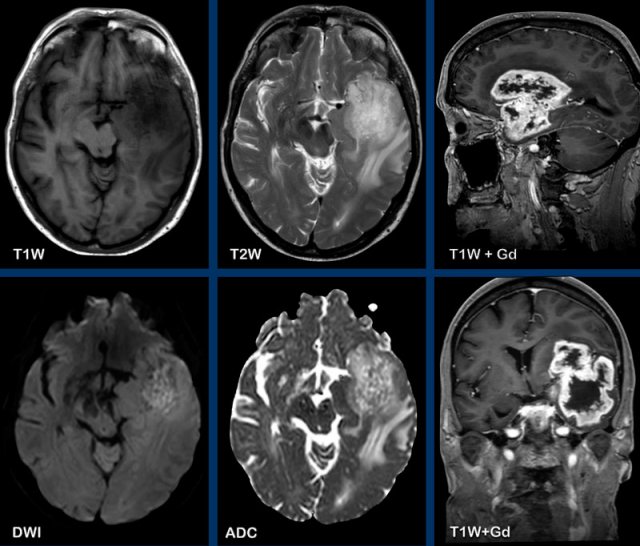
These images are of a 55-year old patient, who presented with headache and aphasia.
First look at the images and then continue reading.
- What are the findings?
- What is the most likely diagnosis?
Images
There is a left
frontotemporal lesion, which is bright on T2W, with thick and irregular ring enhancement.
The lesion follows - and extents into the white matter like
the uncinate fasciculus and the u-fibers.
The centre of the lesion shows no diffusion restriction and no enhancement and is most likely necrosis.
The most likely diagnosis is a GMB.
Glial
tumors originate from glial cells in the central nervous system and are
infiltrative tumors.
GBM’s are the most malignant primary brain
tumors.
They diffusely infiltrate along the white matter tracts, as e.g. the
corpus callosum.
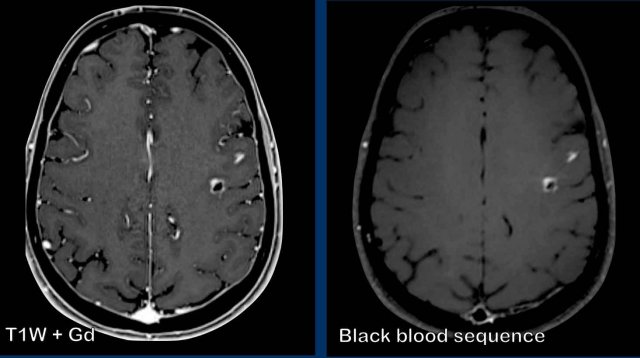
These images are of a patient with metastatic lung carcer. There are two enhancing
metastatic lesions in the left hemisphere.
On the T1W-image with Gadolinium there is also
extensive enhancement of the vessels making it difficult to detect the metastases.
On the black blood sequence the signal of the blood in the
vessels is suppressed making the recognition of the enhancing metastases easier.
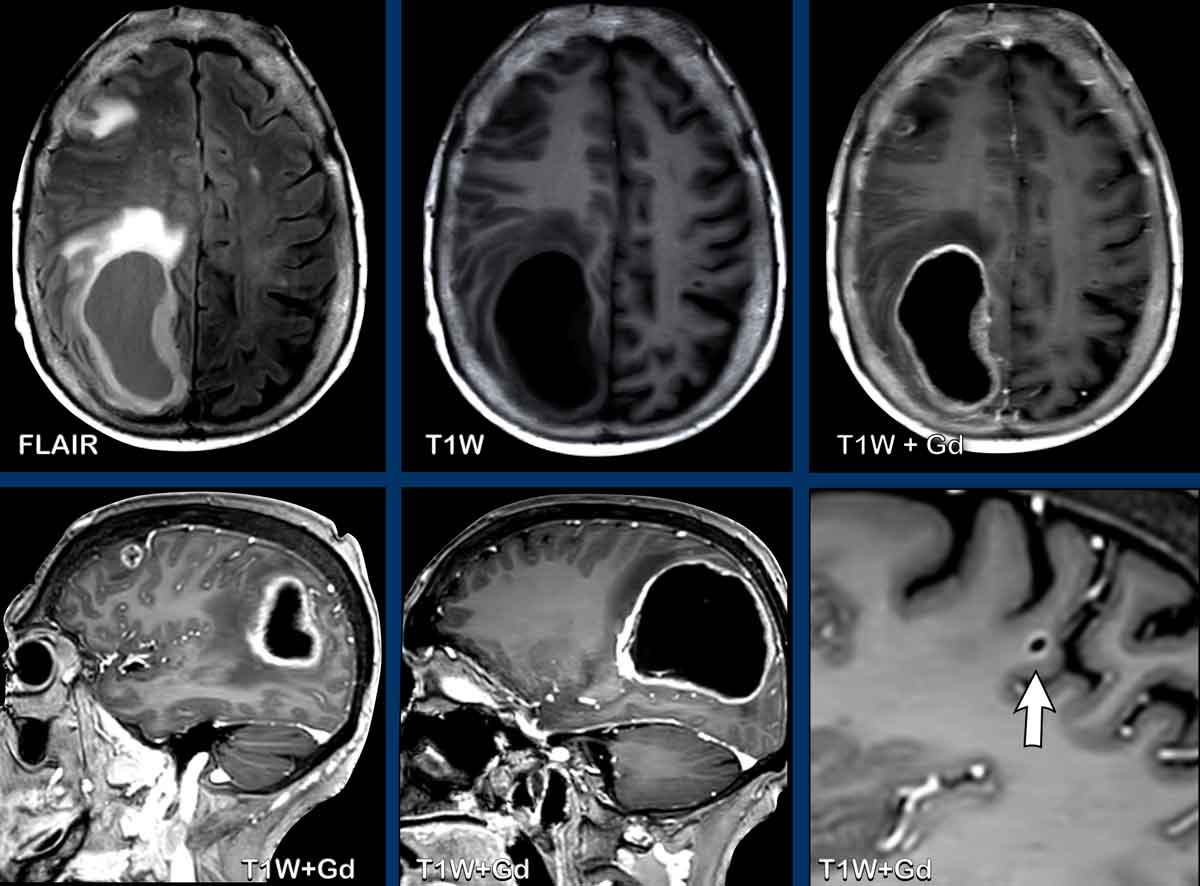
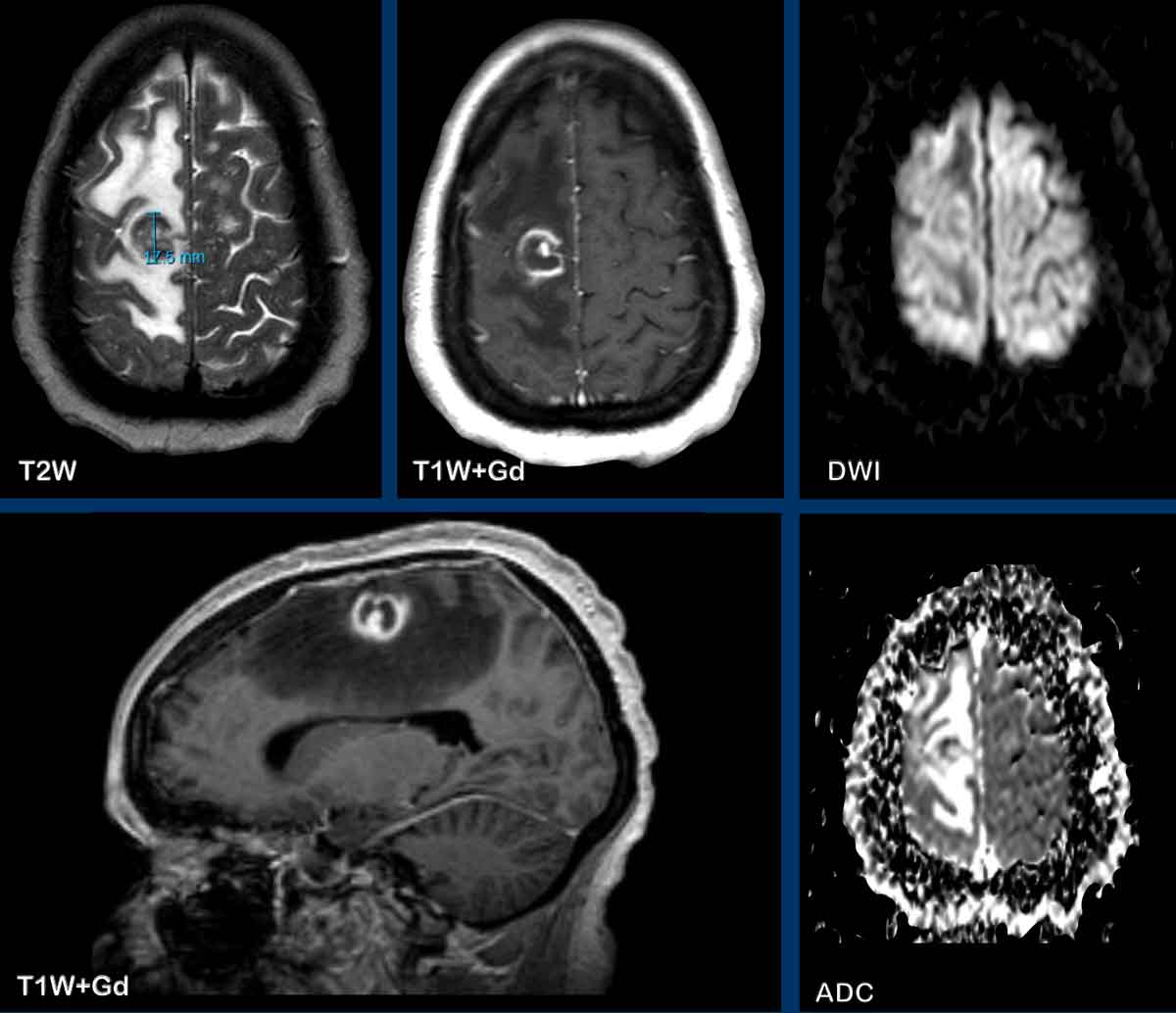
In this patient your eye is attracted to a large cystic
lesion in the right parietal lobe with irregular and partially thick enhancement .
There is mass effect and surrounding edema, without restricted diffusion.
One could think of a glioma.
However, there are several other
lesions far apart.
One of them with a characteristic location at the gray-white matter
interface (arrow).
These turned out to be metastases
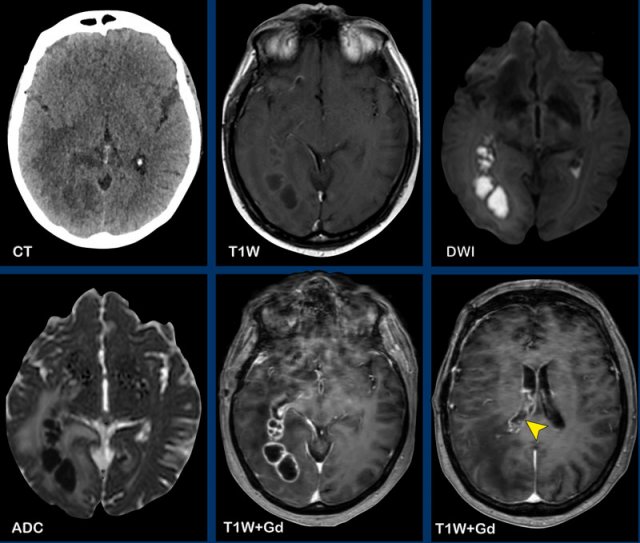
This patient has a history of lungcarcinoma and presented with headache and mental slowness.
Take a look at the images and then continue reading.
Question:
- What are the findings?
- What is the most likely diagnosis?
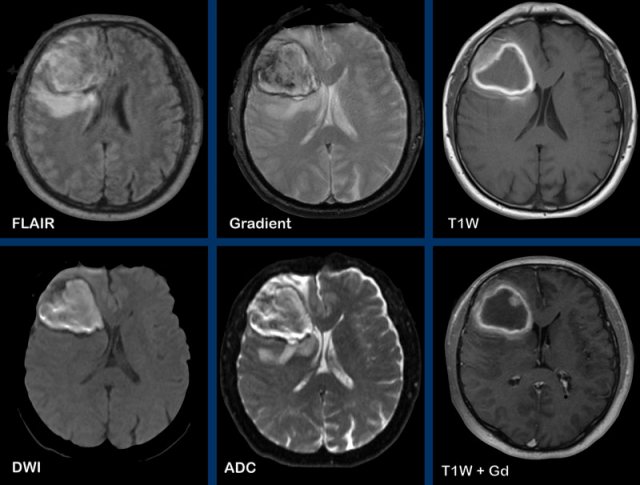
Images
There
are multiple connected ring enhancing lesions with surrounding edema in the right hemisphere.
The
lining is relatively thin and smooth with central diffusion restriction.
There
is extension to the right lateral ventricle with enhancement of the ventricular
lining (arrow).
Note also the diffusion restriction at the trigonum of the left lateral
ventricle.
Many thought that this was metastatic disease because of the history, but the findings are more typical for abscesses with ventriculitis, which turned out to be the right diagnosis.
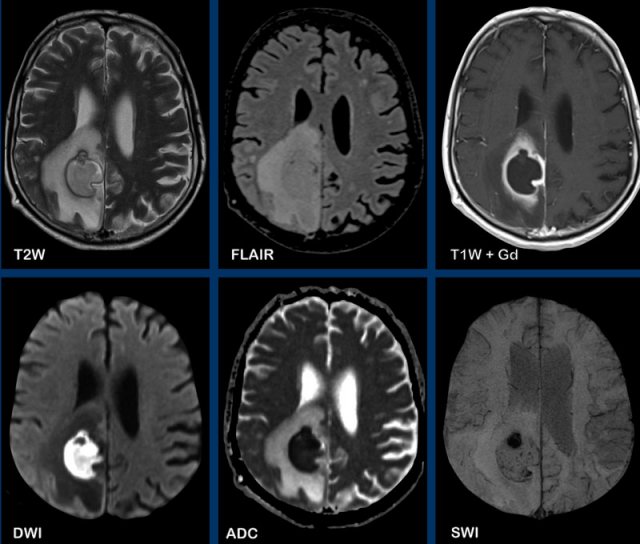
Toxoplasmosis
These images are of a 50-year old female, who presented with a left-sided
hemiparesis.
Her medical history was unremarkable.
Images
There is a rim-enhancing lesion in the right frontal lobe.
There is no central diffusion restriction, but with an eccentric target sign.
This
target sign is highly suggestive of cerebral toxoplasmosis.
This sign is thought to represent enhancing inflamed vessels within the abscess cavity.
This is a companion case of a 34-year old female, who presented with seizures.
Images
There is a rim-enhancing lesion in the
left frontal lobe with a target sign and rim-like diffusion
restriction.
Note also the low signal intensity on T2W and FLAIR
Final diagnosis: toxoplasmosis.
As classical bacterial causative agents of abscesses
demonstrate central diffusion restriction, atypical causative agents like fungi
and toxoplasmosis do not, making the diagnosis of a cerebral abscess more
challenging.
An eccentric target sign as in this case is very helpful for the
diagnosis.
This is a challenging case of a 60-year old patient, who presented with headache.
Images
There is a right frontal lesion with a thick hyperintense rim, which is already visible on the T1W-image without contrast. After gadolinium a nodule is suggested at the ventral part,
could this be a tumor?
Let’s take a look at the other sequences.
On the FLAIR-image the lesion is relatively hypointense.
On the gradient echo there are susceptibility artefacts at the rim and centrally constistent with hemosiderine.
There is central diffusion restriction due
to clot formation and the T1W hyperintensity is due to methemoglobine.
Findings are consistent with an intraparenchymatous
hemorrhage.
Because of the suggestion of an underlying lesion, the patient was
operated, but no tumor was found.
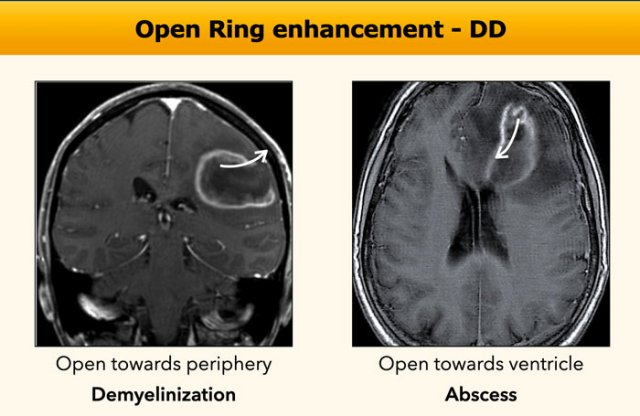
Open ring enhancement
The pattern of an open ring usually suggests a demyelinating disease, but is less frequently seen in an abscess.
In demyelinization the ring is mostly open towards the periphery, while an abscess wants to get rid of the pus centrally into the ventricles, just like an intracerebral hematoma, that leaks into the ventricular system.
Tumefactive MS
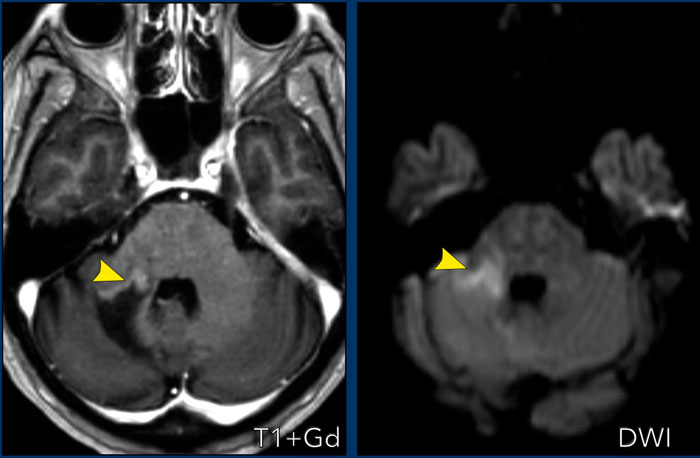
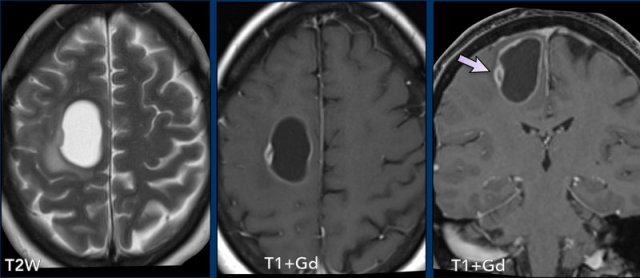
These images are of a 50-year old woman, who presented with a
hemiparesis of the left arm and leg. No previous history.
First look at the images. What are the findings?
Images
- Multiple high intensity areas on the FLAIR images.
- Multiple ring enhancing lesions. The ring is open towards the periphery.
- On the DWI no sign of central diffusion restriction in the content of the lesion making an abscess highly unlikely. There is some peripheral diffusion restriction
- Although these lesions are quite large, there is no sign of mass effect and this is typical for a demyelinating disease as is e.g. multiple sclerosis.
These findings are typical for tumefactive MS.
Dilated central vein
Here another tumefactive MS-case.
Notice the dilated vein in the centre of the lesion.
Most MS lesions in the cerebral white matter expand outward from small inflamed veins.
This is called a perivenular
distribution.
Continue with more images of this patient...
There is an incomplete ring enhancement.
Notice that the open ring points towards the ventricle (arrow), which would favor the diagnosis of an abscess.
However, there is a central vein on SWI and on the DWI (not shown) there was no diffusion restriction
In this case the open ring does not follow the rule.
Here another example of open ring enhancement located in the pons in a patient with demyelinization.
These images are of a 52-year old woman who was treated for AML and now presented with paresis of the right arm and difficulty finding the right words.
Images
On
the contrast-enhanced
T1W-image
there is a hypointense lesion without any mass effect, with incomplete enhancement
of
the wall.
Only
this enhancing part of
the lesion shows diffusion restriction (arrowheads).
Conclusion
We regarded this as demyelinization with open ring enhancement.
This proved to be progressive multifocal leukoencephalopathy (PML), which is a demyelinating disorder caused by opportunistic infection of JC virus in patients with severe immunodeficiency.
Abscess
Although abscesses classically present with a complete ring, they sometimes present with open ring enhancement like in this case.
Images
In the left frontal lobe is a lesion with open ring enhancement next to the frontal sinus.
There is a small defect in the wall of the sinus (arrowhead).
The central part of the lesion shows diffusion restriction.
Conclusion
Intracerebral abscess as a complication of a frontal sinusitis.
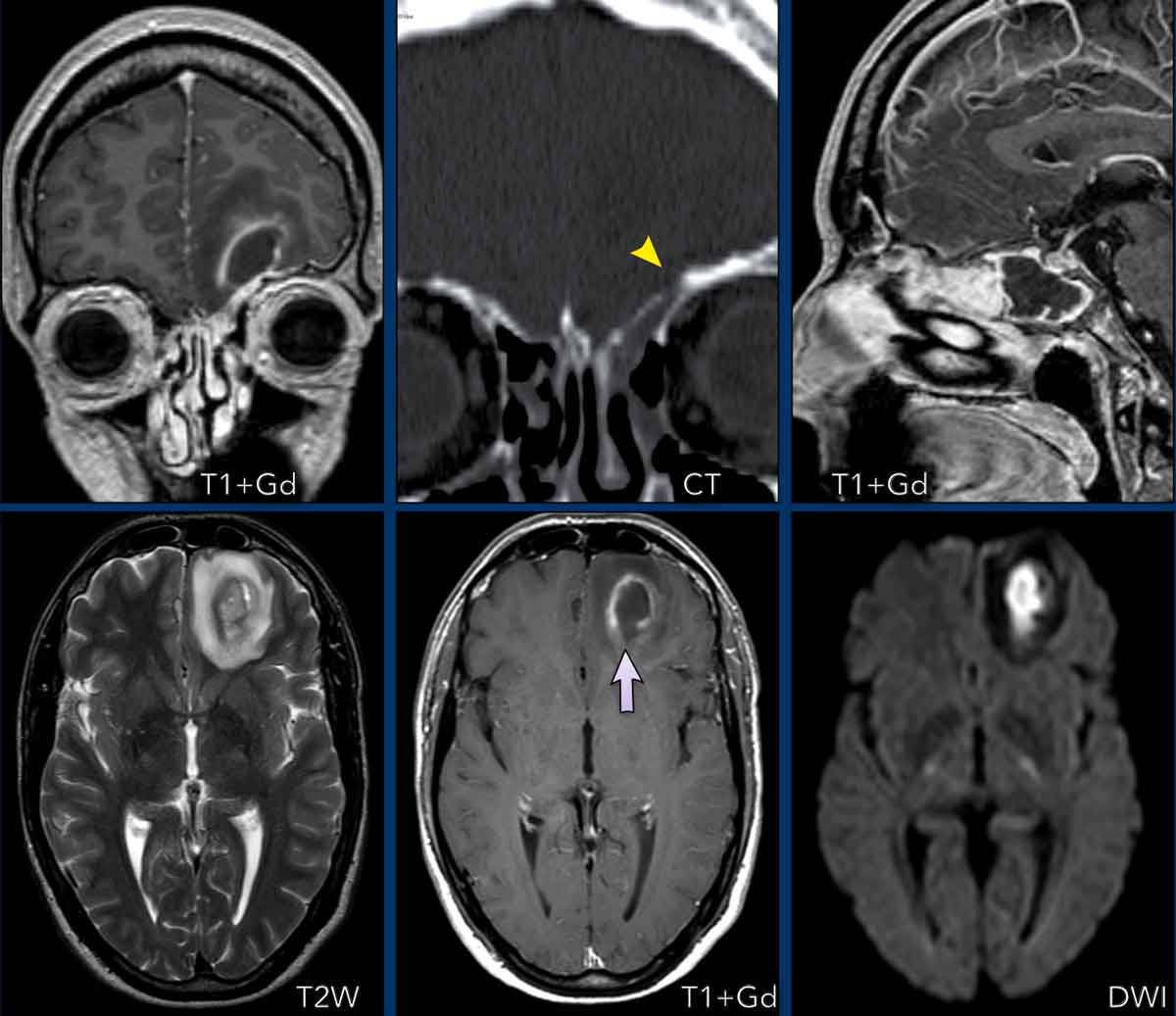
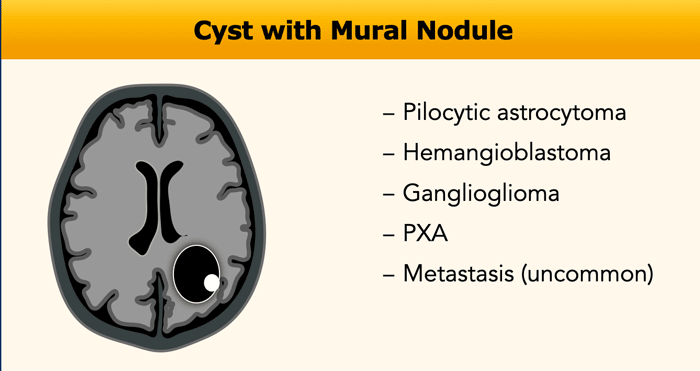
Cyst with Nodule
In this enhancement pattern, the age of the patient is important for your differential diagnosis.
In children the differential diagnosis is Pilocytic astrocytoma, Ganglioglioma and Pleomorphic xanthoastrocytoma (PXA).
In adults hemangioblastoma is more
likely.
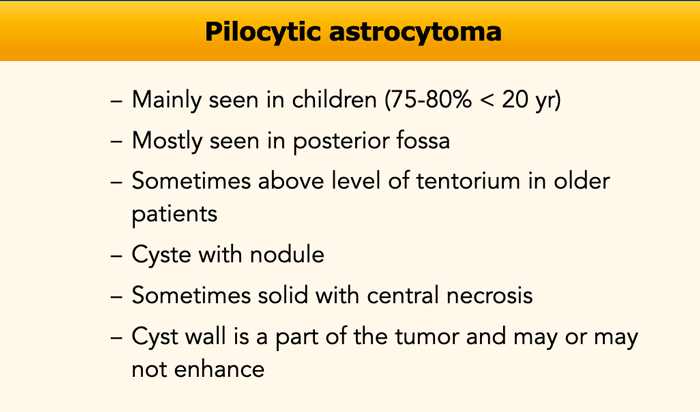
Pilocytic astrocytoma
Pilocytic astrocytoma is the most common childhood brain tumor and most often found in the posterior fossa.
Complete resection usually cures the patient.
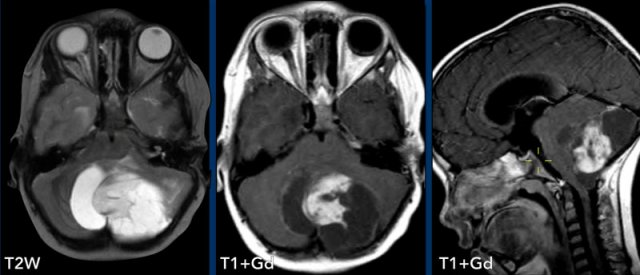
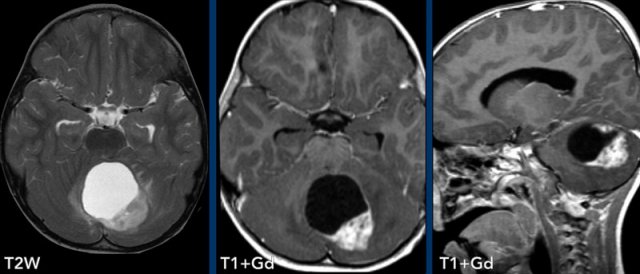
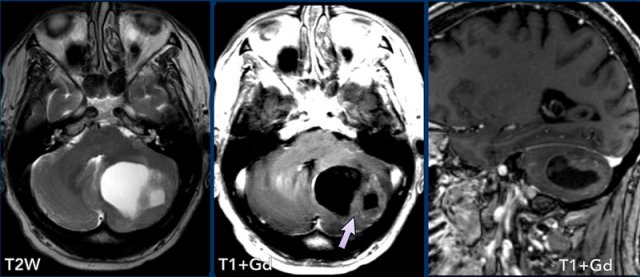
These images are of a 9-year old child who presented with headache.
Images
there is a large cystic posterior fossa mass with compression and
obstruction of the fourth ventricle and brainstem.
A solid contrast enhancing
nodule is present, as well as enhancement of the cyst wall.
Conclusion
Most likely diagnosis at this age is a pilocytic astrocytoma
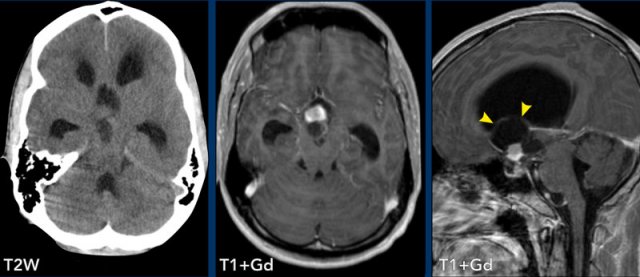
These images are of a 3-year old child who also presented with headache.
There are two important findings.
Take a closer look at the images and then continue reading.
Images
Large cyst with enhancing nodule in the posterior fossa..
Notice that the wall of the cyst enhances.
The nodule is not located on the pial side (inner part of the meninges) unlike in a hemangioblastoma.
Conclusion
Most likely diagnosis at this age is a pilocytic astrocytoma.
The enhancing wall is part of the tumor and needs to be resected.
These images are of a 25-year old man.
What are the findings.
Take a closer look at the images and then continue reading.
Images
Cystic lesion in the suprasellar region with a solid enhancing nodule complicated by an obstruction hydrocephalus.
Conclusion
For
suprasellar lesions, a large differential diagnosis is present (mnemonic
SATCHMO).
On the NECT
there is no calcium in the tumor, which makes a craniopharyngioma unlikely.
In this location the most likely diagnosis is an optic pathway glioma.
Most of them are
pilocytic astrocytoma.
In older patients a pilocytic astrocytoma can be located above the level of the tentorium.
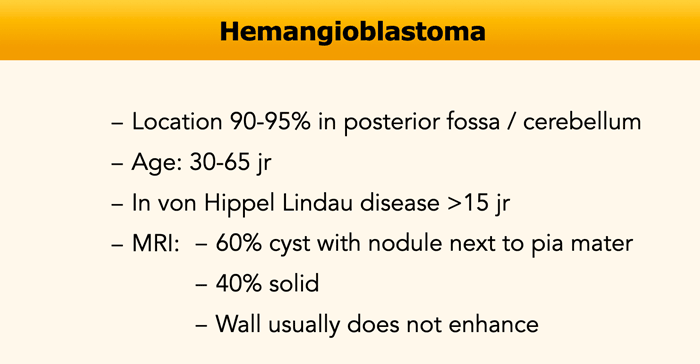
Hemangioblastoma
Hemangioblastoma occurs most often in the cerebellum, where it is the most common primary neoplasm in adults.
It is less commonly seen in the spinal cord.
They start as a solid nodule and gradually develop a cyst.
The nodule is located on the pial side (inner part of the meninges).
The wall of the cyst is not a part of the tumor and normally they do not enhance, unless in cases when there has been a bleeding within the cyst.
Since the wall is not tumor, it is not necessary to resect the whole cyst.
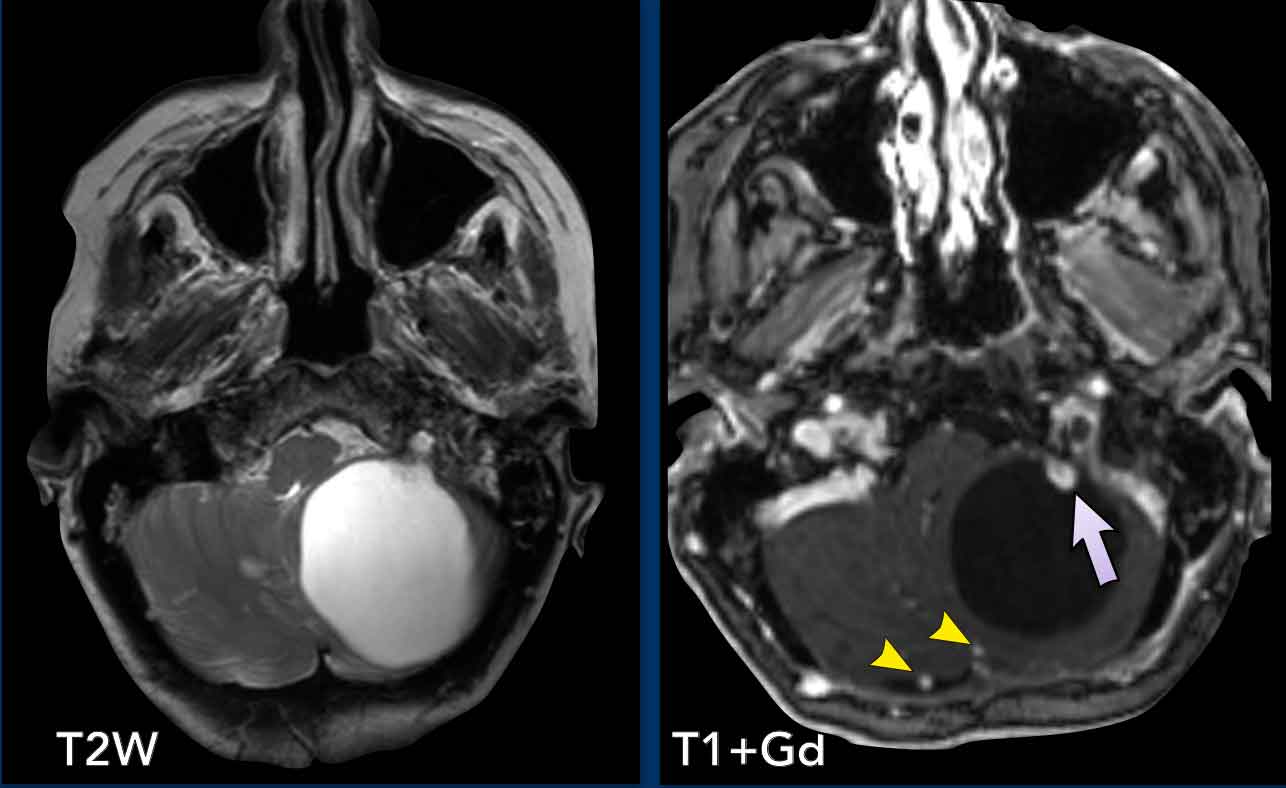
These images are of a 63-year old woman who has von Hippel Lindau disease.
Take a closer look. What is barely visible?
Images
There is a large cyst with a small enhancing nodule in the right cerebellar hemisphere.
The wall of the cyst does not enhance.
Notice that the tumor nodule is located on the pial side (arrow).
There are two more enhancing small nodules on the posterior side of the cerebellum.
Multiple tumors are almost always associated with von Hippel-Lindau disease.
These images are of a 29-year old man.
Images
Cystic lesion with a non-enhancing wall and an enhancing nodule on the pial side.
Conclusion
Typical hemangioblastoma.
When this tumor is going to be resected, they only have to remove the nodule.
Ganglioglioma
These images are of a 13-year old child who presented with seizures.
Images
There is a cystic lesion in the right hemisphere.
Notice the location in the grey matter best appreciated on sagittal images (arrow).
Although you could call this pattern ring enhancement, we prefer to call this pattern "cyst with mural nodule".
Conclusion
The
most likely diagnosis is a ganglioglioma.
Differential
diagnosis: PXA, DNET, desmoplastic infantile astrocytoma
(younger age) and the cystic part pilocytic astrocytoma (non-cortical).
This case just looks like a benign cystic tumor with a nodule.
Most likely a ganglioglioma.
However much to anyone's surprise at resection this proved to be a glioblastoma (GBM).
These images are of a 58-year old woman.
In older patients the differential diagnosis of a cyst with
tumor nodule is mainly hemangioblastoma and metastasis.
The nodule is not on the pial surface and the enhancement is less pronounced compared to previous cases
shown.
This proved to be a metastasis of a neuroendocrine neoplasm.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.