TLICS Classification of fractures
Thoraco-Lumbar Injury Classification and Severity score
by Clark West, Stefan Roosendaal, Joost Bot and Frank Smithuis
Department of Radiology and Regional Spinal Cord Injury Center of the Delaware Valley, Thomas Jefferson University Hospital, Philadelphia and the Radiology Department of the Free University Medical Center and the Academical Medical Center, Amsterdam
Publicationdate
The Thoraco-Lumbar Injury Classification and Severity score (TLICS) is a classification system for thoracolumbar spine injuries, designed to assist in clinical management.
Unlike other classifications, the TLICS is an easy scoring system that depicts the features important in predicting spinal stability, future deformity, and progressive neurologic compromise.
TLICS also facilitates appropriate treatment recommendations.
Introduction
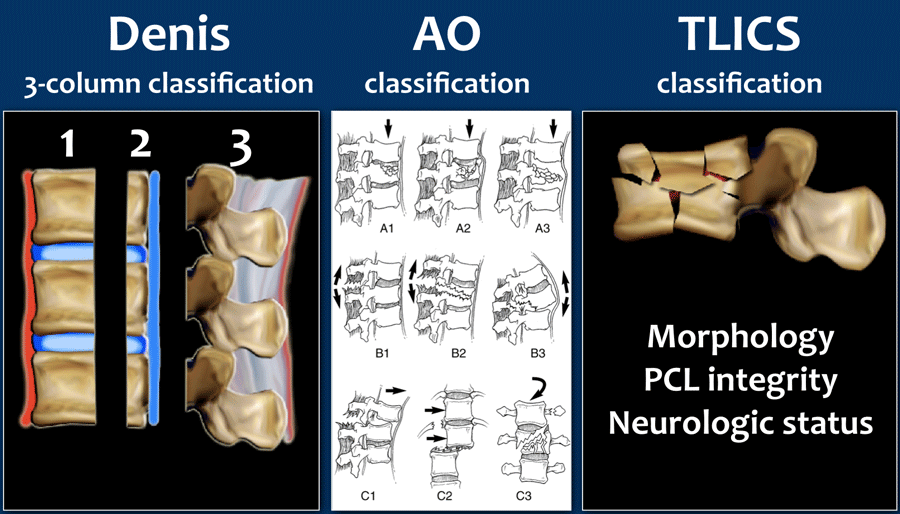
Most classification systems of spine injuries are based on injury mechanisms and describe how the injury occurred.
This is all based on the premise that a fracture caused by forward flexion should be treated by undoing the flexion by positioning the patient in an extension brace, or by surgical intervention correcting the spinal column in extension.
Some of the injuries thought to be due to extension mechanisms, however, turn out to be due to flexion and vice versa. These descriptions may thus be misleading.
A problem with classifications such as the AO-classification is that they are usually complex, leading to high inter-reader variability.
Using the popular Denis three-column classification may lead to another situation since it uses the terms stable and unstable. In many cases, however, there is no good correlation with the necessity for surgery.
Furthermore, the word stability itself is ambiguous and may refer to direct osseous stability; it may refer to neurological stability and finally, to long-term (ligamentous) stability.
Both of these commonly used systems fail to systematically take into account the neurological status of the patient and the indication for MRI to determine the integrity of the posterior ligamentous complex.
For these reasons the Spine Trauma Study Group introduced in 2005 the Thoracolumbar Injury Classification and Severity Scale (1), with intention to be a reliable, ease-to-use tool to facilitate clinical decision making and as a practical alternative to cumbersome classification systems already in use.
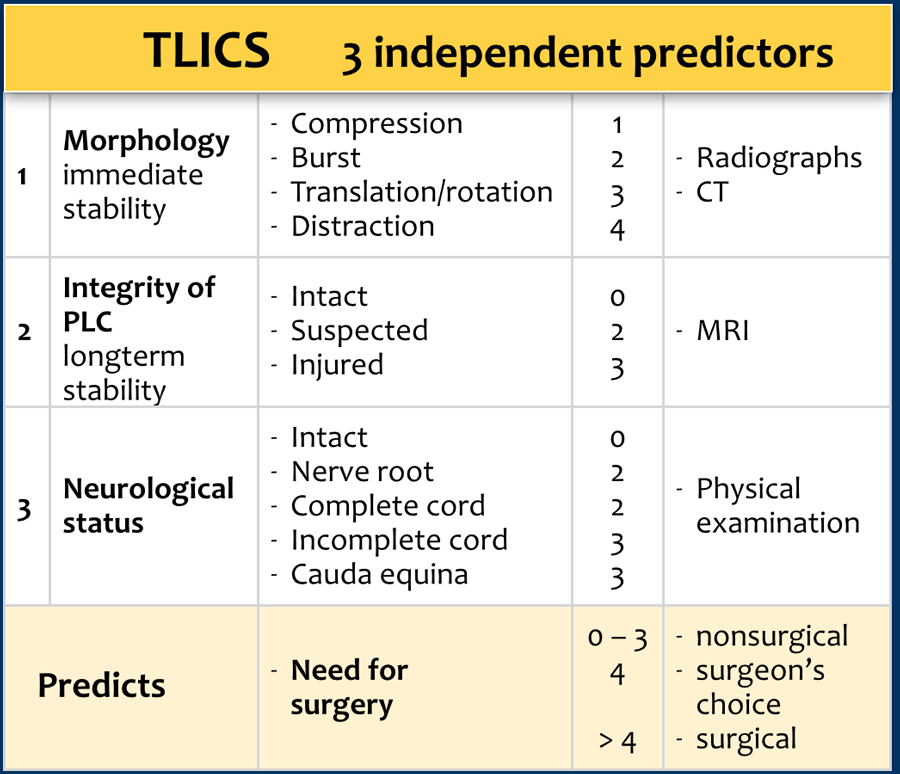
The TLICS consists of three independent parameters:
- Injury Morphology
- Integrity of the Posterior Ligamentous Complex
- Neurologic status.
A parameter can be scored 0-4 points and the total score is the sum of these parameters with a maximum of 10 points.
The total score predicts the need for surgery as is shown in the TLICS algorithm. A total of more than 4 points indicates surgical treatment.
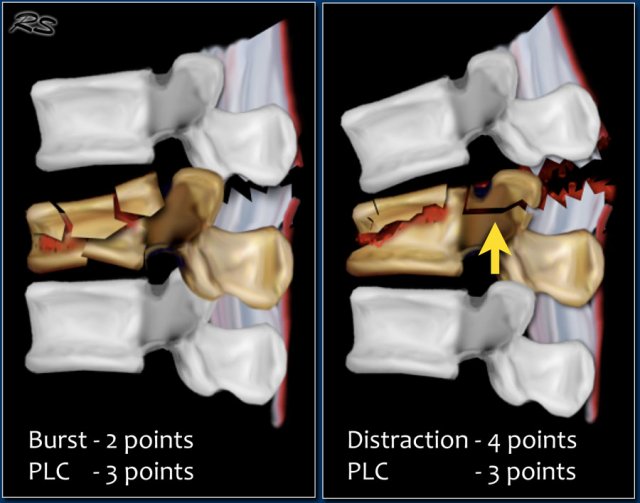
A compression fracture gets 1 point. When it is complicated by a burst, it gets an additional 1 point, resulting in 2 points.
The integrity of the posterior ligamentous complex plays an important role in the TLICS. Sometimes it will be possible to determine PLC injury on CT, but MRI may be necessary.
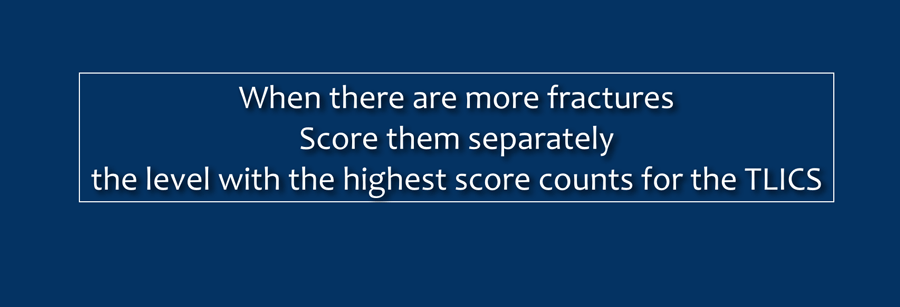
When there are several fractures, each level has to be scored separately. The level with the highest TLICS score will determine the type of treatment.
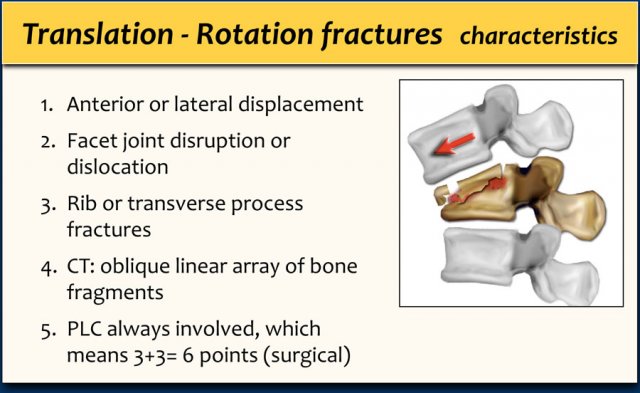
Morphology and PLC are scored separately. For example, in a translation/rotation injury, the PLC is always involved, making a total of 3+3=6 points. When there is a distraction on the posterior side, the PLC is always involved, making a total of 4+3=7 points.
In case of a distraction on the anterior side, however, the PLC may or may not be involved, i.e. it will be either 4 or 4+3= 7 points.
Morphology
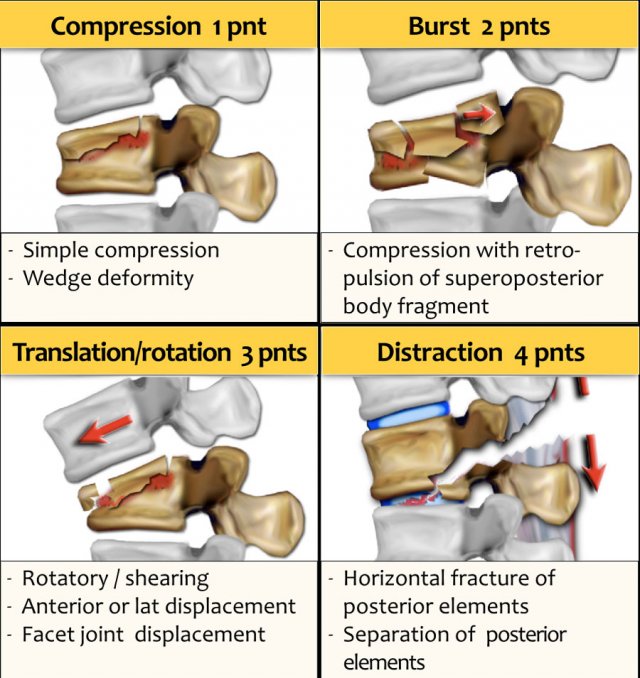
The TLICS describes injury morphology as a pattern; it is not a mechanism of injury.
Usually the morphology matches the injury mechanism, but sometimes it does not. Once you realize that, it should not confuse you.
- Compression is usually the result of axial force with flexion.
- Burst is the result of compression with severe axial loading.
- Translation/rotation is the result of displacement in the horizontal plane.
- Distraction is the result of displacement in the vertical plane.
The different morphology patterns will be discussed more in detail in the following chapter.
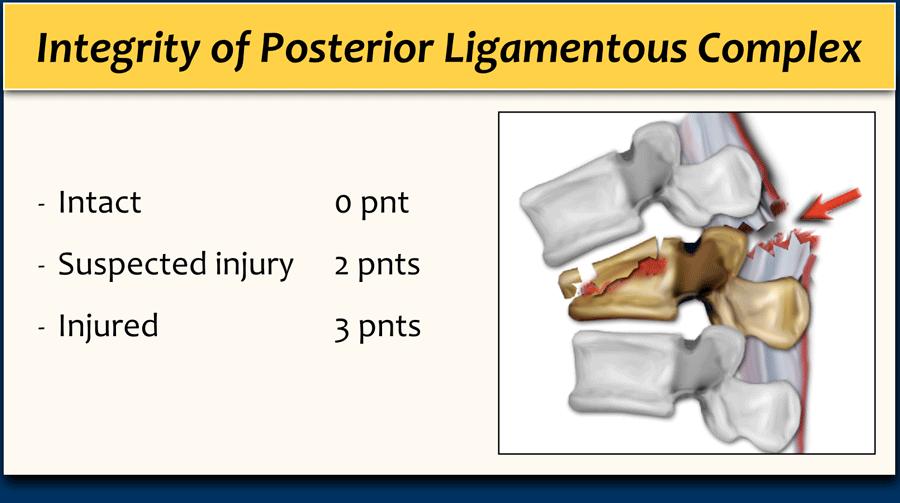
Posterior Ligamentous Complex
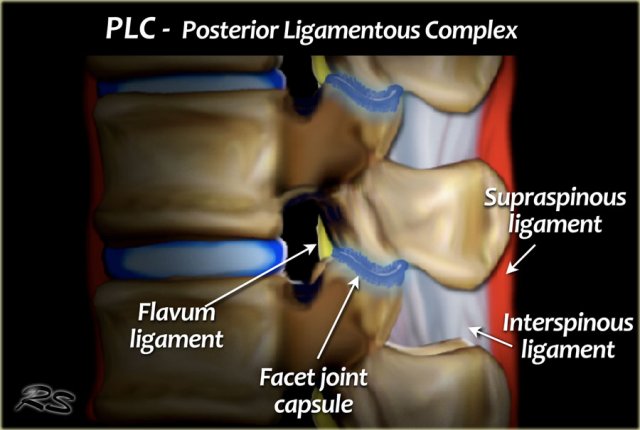
The PLC serves as a posterior "tension band" of the spinal column and plays an important role in the stability of the spine (3).
A torn PLC has a tendency not to heal and can lead to progressive kyphosis and collapse.
The PLC is composed of the supraspinous ligaments, interspinous ligaments, articular facet capsules, and ligamenta flava (figure).
The supraspinous ligament is a strong, cordlike ligament which connects the tips of the spinous processes from C7 to the sacrum.
The interspinous ligaments are weak, thin, membranous structures connecting the adjacent spinous processes.
The contractile force of the ligamenta flava presses the vertebrae together and keeps them aligned.
The facet joints act against rotational forces.
CT features of PLC pathology are:
- Widening of the interspinous space.
- Avulsion fractures or transverse fractures of spinous processes or articular facets.
- Widening or dislocation of facet joints.
- Vertebral body translation or rotation.
When the PLC is definitely injured on CT, it can already be scored as 3.
Since the integrity of the PLC depends mostly on ligamentous structures, MR is sometimes needed to adequately diagnose pathology of the PLC, especially when there is no dislocation or disruption on CT.
MRI features of PLC pathology are:
- Definite: 3 points
- Loss of normal low signal intensity of the ligamenta flava or supraspinous ligaments on T1 and T2.
- Indeterminate: 2 points
- Edema without clear rupture; high signal intensity of the interspinous ligaments or along the facet joints on T2 SPIR or STIR.
MRI has a tendency to overdiagnose PLC injury (4).
In some cases it can be difficult to decide whether there is a burst fracture with a torn PLC or distraction with a torn PLC and a compression fracture (figure).
You have to decide what you think is the main issue: the collapse of the vertebral body or the distraction.
Since in both cases the TLICS score based on imaging will be high, there is usually an indication for surgical treatment.
TLICS score
In case of multiple fractures, you have to score each level separately.
The level with the highest TLICS score usually will be decisive for the therapy of choice.
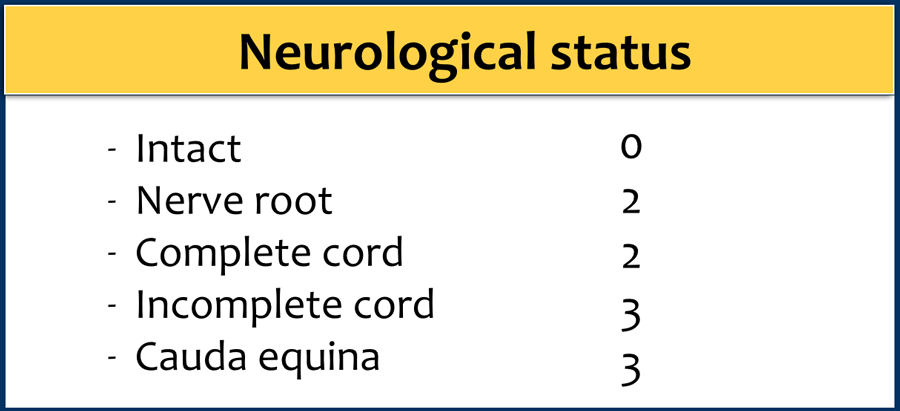
Neurological status
The third category is the neurological status as determined by the neurologist or spine surgeon.
The role of the radiologist is to report the following:
- Myelopathy or nerve compression.
- Retropulsion of a body fragment and the percentage of narrowing of the spinal canal.
- Epidural hematoma.
One of the key points here is that an incomplete cord lesion will likely benefit more from surgery than a complete lesion; therefore a complete cord injury is scored as only 2 points, while an incomplete cord injury gets 3 points.
Modifiers
- Modifiers are other factors which can affect the decision of appropriate treatment:
- Sternum fracture
- Rigid spine
- Multiple rib fractures at the same levels
- Non braceable
- Wounds
- Pre-existing deformities
Sternum fracture
The image shows a vertebral fracture with a transverse fracture of the spinous process, but also a fracture of the sternum.
Analogous to the 3-column classification of Denis, some investigators consider the sternum as the fourth column in upper thoracic spinal fractures and recognize it as an independent variable in the assessment and treatment of these patients (5).
Rigid spine
Patients with a rigid spine (such as in ankylosing spondylitis, DISH and rheumatoid arthritis) are more susceptible to spinal fractures, even after minimal trauma (6).
Ossification of the spinal ligaments and calcification of the annulus fibrosus alter the biomechanics of the spine, creating long lever arms and limiting the ability to absorb even minor impacts.
The bone is usually very osteoporotic.
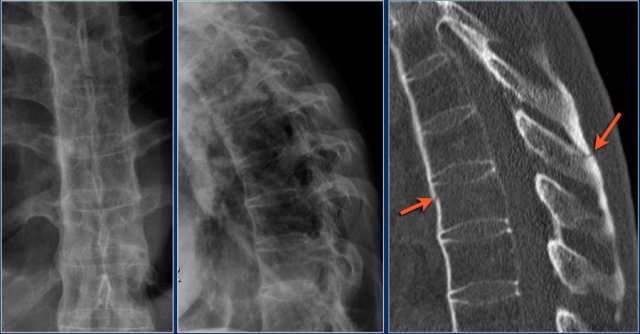
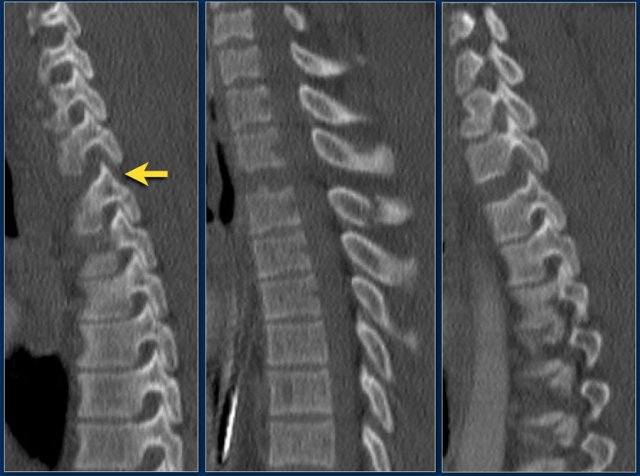
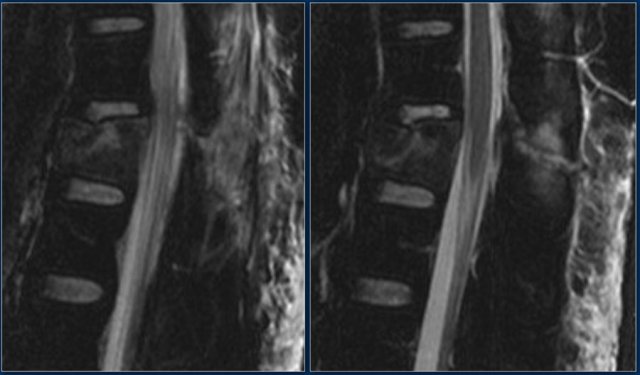
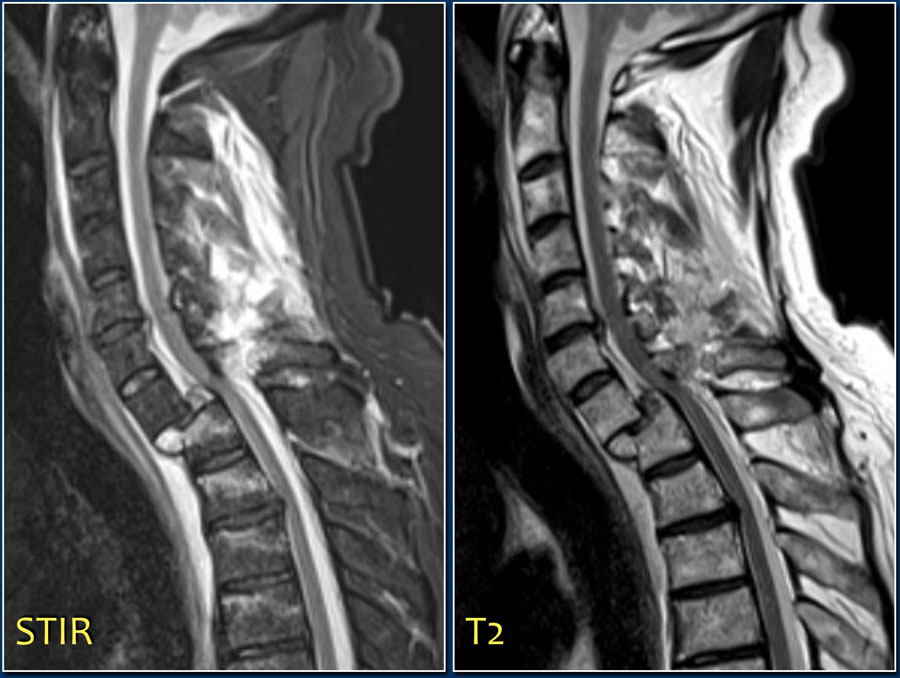
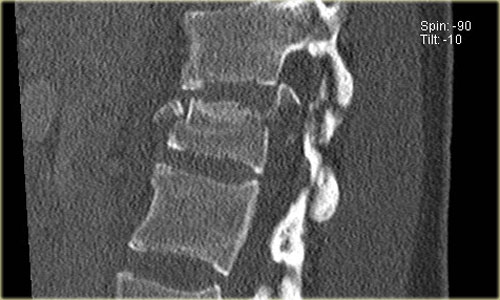
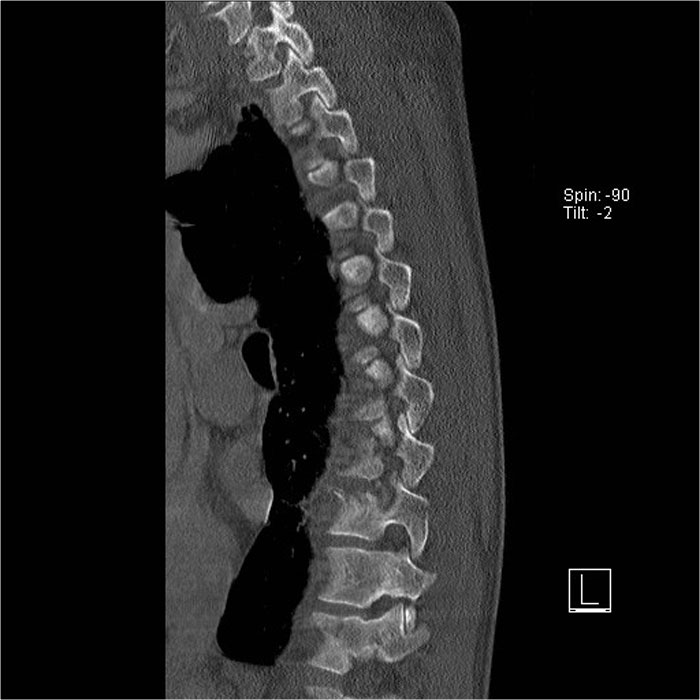
The images are of a patient with a typical bamboo spine as a result of ankylosing spondylitis.
After a fall on his back no fracture was seen on the x-rays.
However the CT shows a thin fracture line through the anterior side of the vertebral body and also through the spinous process.
Continue with the MR-images.

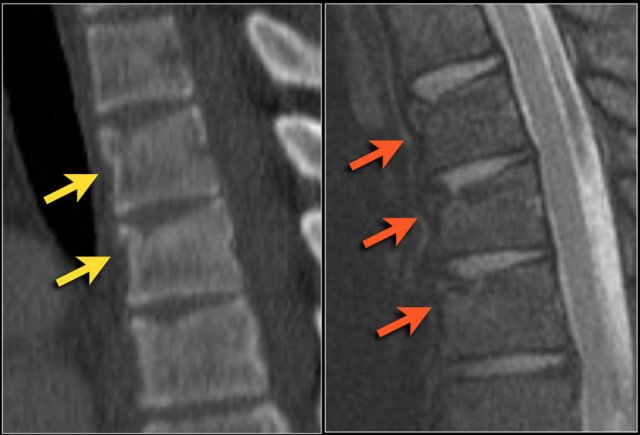
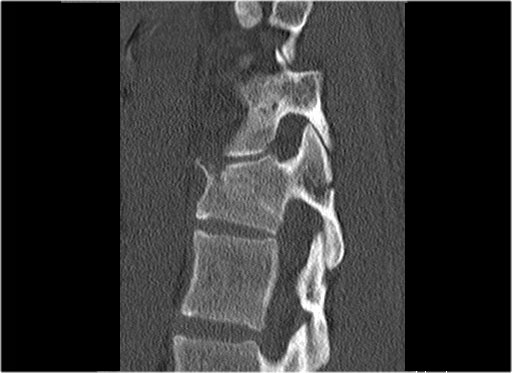
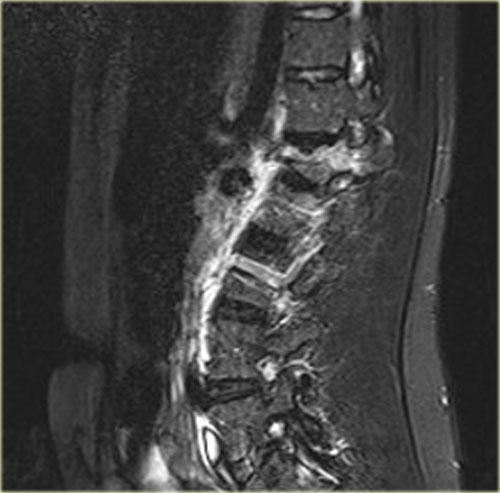
Look at the images.
What are the findings?
Then scroll to the next images.
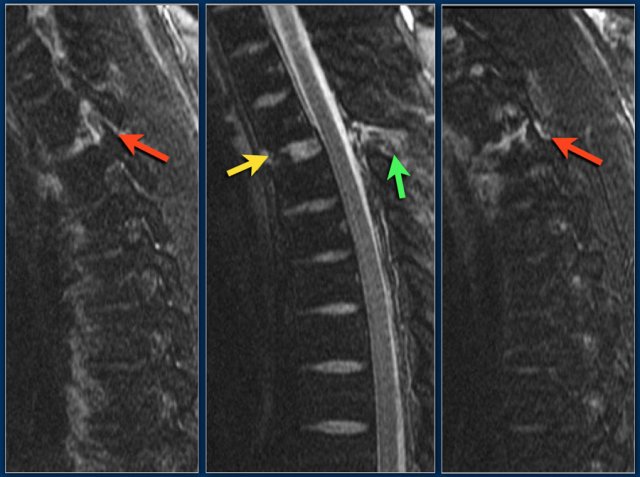
The findings are:
- Vertebral bodies show marrow edema as a result of a fracture.
- Torn flaval ligament (yellow arrow).
- Fractures through the posterior elements (red arrows).
The TLICS-score is high, because there is distraction and injury to the PLC.
Morphology
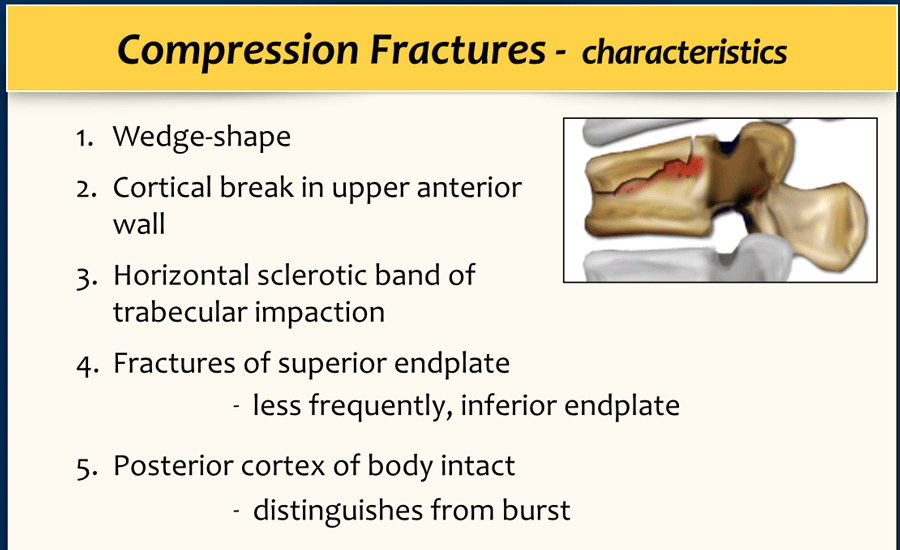
Simple compression
A simple compression fracture is the most common form of injury and is seen in 90% of cases.
It is either loss of height of the anterior part of the vertebral body or disruption of the vertebral endplate.
The posterior cortex of the vertebral body has to be intact and this feature differentiates a simple compression fracture from the more severe burst fracture.
The posterior cortex may bulge slightly posteriorly in a simple compression fracture. As long as there is no free fragment with posterior displacement, it is a wedge compression fracture and not a burst fracture.
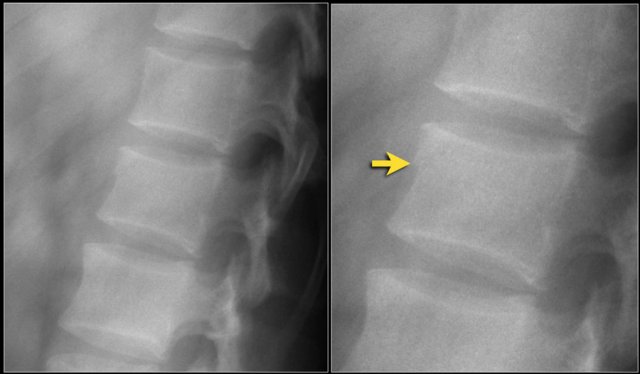
The images show a compression fracture.
All we see is a cortical disruption in the upper anterior wall of the vertebral body and slight loss of height ventrally.
The posterior vertebral cortex is intact.
The sagittal reformatted image also shows the cortical disruption.
Notice that on a 2.5mm axial slice you can miss these fractures.
You have to look at the thin slices to detect such a subtle fracture.
Scroll through the images.
Notice the horizontal band of density, which is often described as sclerosis.
This density does not mean that it involves an older fracture that is already healing with sclerosis.
This is merely a sign of trabecular impaction in an acute fracture.
It is very common to see more fractures on imaging with CT and MRI than on the radiographs.
In this case the CT shows 2 fractures and the MRI shows 3 fractures.
Pitfalls in diagnosing a compression fracture are:
- Congenital anomalies
- Osteochondrosis with irregular endplates
- Limbus vertebrae
The images show two cases of osteochondrosis.
On the right with kyphosis.
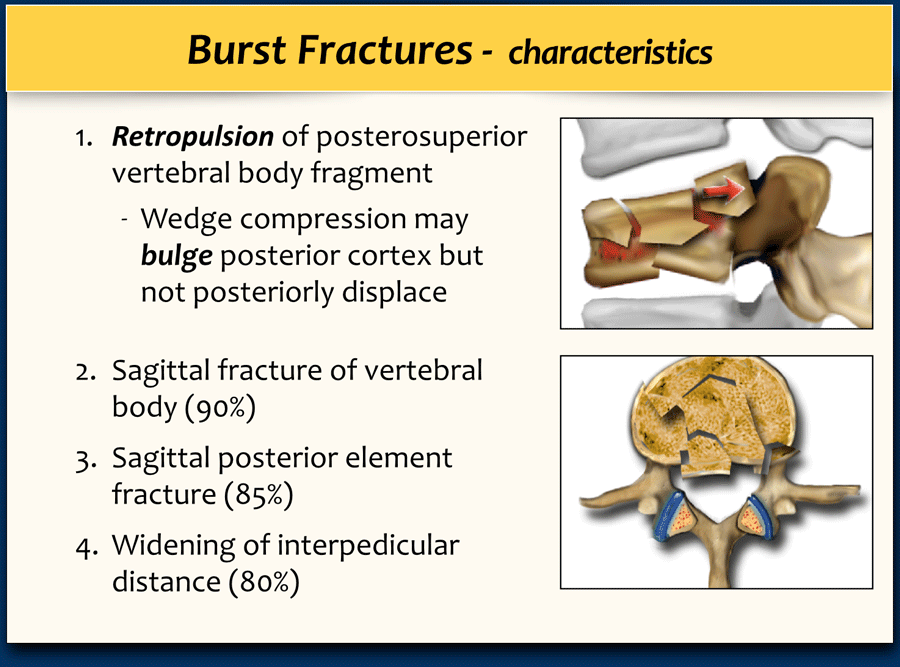
Burst fracture
This is the severe variant of a compression fracture with higher risk of neurologic deficits.
The name is derived from the typical fracture following a fall from height and landing on the feet.
A burst fracture gets 2 points for morphology in the TLICS.
This means that a patient can be treated non-surgically.
In the absence of a neurologic deficit, PLC integrity should be confirmed at MR imaging, especially if conservative management of a burst fracture is planned (3).
In the Denis classification a burst fracture is classified as a two-column injury, calling it unstable and requiring surgical stabilization.
Subsequent modifications of the Denis classification have recognized that with an intact posterior ligamentous complex (PLC), two-column unstable injuries can be successfully treated non-surgically (3).

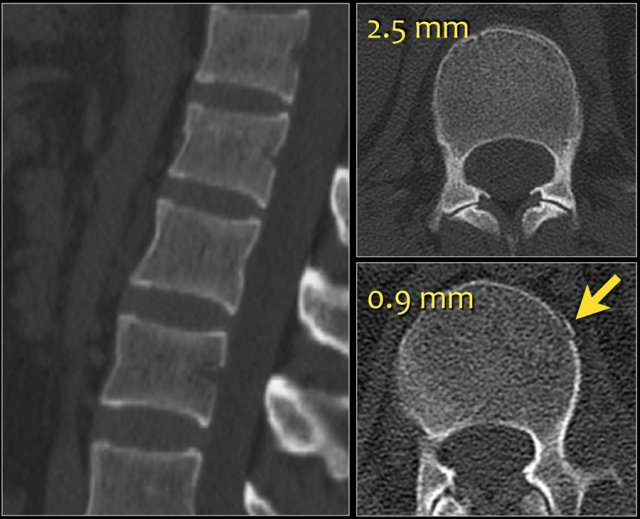
Retropulsion of posterosuperior vertebral body fragment
Retropulsion of a fragment is the typical feature of a burst fracture and distinguishes it clearly from a simple compression fracture.
Scroll through the images.
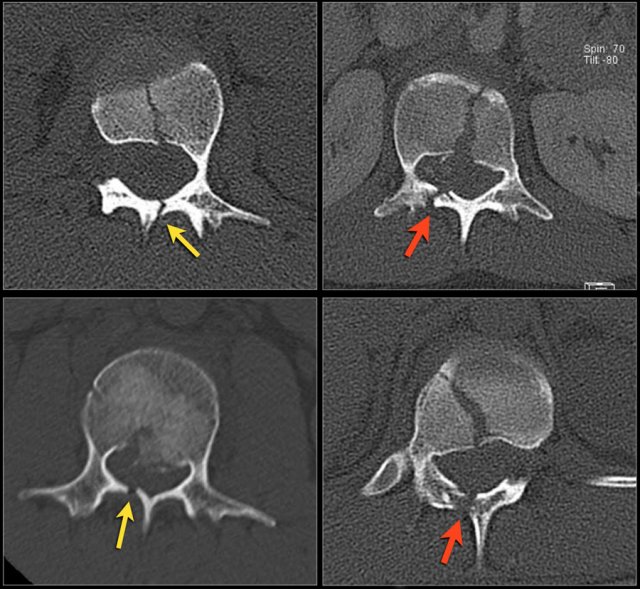
Sagittal fracture of vertebral body and posterior element
A sagittal fracture of the vertebral body and a sagittal posterior element fracture is seen in respectively 90% and 85% of cases of burst fracture cases.
Here are four examples.
In the Denis classification this would be a three column fracture -anterior/middle/posterior - indicating a very unstable fracture.
In the TLICS classification however this is a burst fracture, i.e. 2 points for morphology.
The treatment will depend on the PLC integrity and the neurological status.
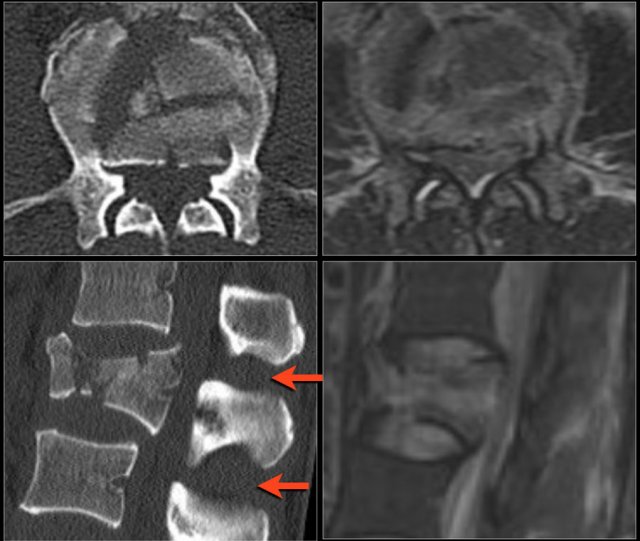
Widening of the interpedicular distance
Widening of the interpedicular distance, often a result of the sagittal fracture, is seen in 80% of burst fractures.
The lateral view shows the typical features of a burst fracture.
On the AP-view notice the subtle widening of the interpedicular distance compared to the levels above and below.
The axial CT and MRI in the same patient show the displaced fragment pressing on the thecal sac.
On the sagittal CT and MRI there are no signs of posterior ligamentous injury.
The anterior longitudinal ligament is disrupted.
The right facet joint looks a bit widened on the CT and there is some fluid in the joint on the MRI.
If there was a lot of fluid in the joint, we should call this indeterminate.
In this case we are not sure.

Scroll through the images.
How would you describe the morphology and the PLC?
The findings are:
- The morphology is burst (2 points)
- The PLC is injured with a fracture through the adjacent spinous processes. One of the fractures is a typical avulsion.
- TLICS score: 5 points
You could argue that these fractures of the spinous processes indicate distraction, i.e. 4 points for morphology.
However in this case the compression is the most prominent finding.
Translation - Rotation
This type of fracture includes all fractures that are the result of displacement in the horizontal plane: side-to-side motion, either left-to-right or anterior-to-posterior or side-to-side rotary motion of one vertebral body with respect to another.
Often unilateral or bilateral facet dislocation is seen in rotational fractures.
It is a severe type of injury, which always involves the PLC.
In the TLICS this means 3 points for the morphology and 3 points for the PLC, which makes a total of 6 points indicating the need for surgical stabilization.

Here a typical case of translation.
The x-ray of the C-spine in this patient was normal and did not show the fracture.
First look at the first CT-images and decide what is going on.
Then scroll to the next images.
In this case of translation there is bilateral facet dislocation and also a horizontal fracture of the spinous process.
There is severe narrowing of the spinal canal.
Continue with the MRI-images.
Again look at the first MR-images and decide what is going on.
Then scroll to the next images.
The findings are:
- Anterior displacement of C7 to Th1.
- Protrusion of the disc.
- Compression of the spinal cord.
- Bone marrow edema in several vertebral bodies, either due to contusion or fracture.
- Interspinous edema and disruption of the ligamenta flava C7-Th1 and supraspinous ligament Th1-Th2.
In some cases it can be difficult to decide whether there is a translation or distraction injury and we have to assume that the traumtic mechanism is a combination of forces.
Scroll through the images.
What are the findings?
At first glance this looks just like another burst fracture.
However notice the following:
- Minimal anterior displacement of the upper vertebral body.
- Kyphosis.
- Facet fracture.
Even though there is not much displacement at this moment, we should probably call this translation injury.
Continue with the axial images.

On the axial images we see:
- Transverse process fractures
- A rib fracture
These are typical findings in translation-rotation fractures.
So we should call this a translation fracture with anterior displacement.
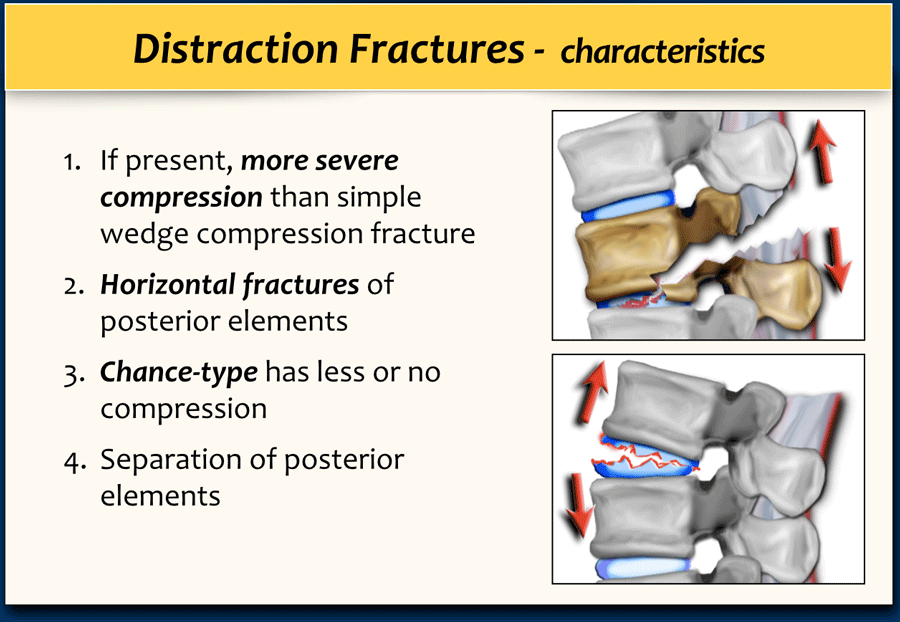
Distraction
A distraction injury is separation or pulling apart of two adjacent vertebrae.
It is a severe injury since there is a high chance of cord injury when its osseous and ligamentous supporting structures are pulled apart.
A distraction injury on the posterior side can lead to a compression fracture on the anterior side.
So be sure not to underestimate the injury by only looking at the compression fracture and overlooking the distraction injury.
In some cases it is difficult to decide whether you are dealing with distraction combined with a compression fracture or with a compression fracture with PLC-injury.
If the distraction is the main feature, then the morphology is distraction, i.e. 4 points.
In these cases the PLC is always involved, resulting in a total of 7 points for the TLICS-score.
If compression is the main feature, then the morphology is burst, i.e. 2 points combined with the PLC injury making a total of 5 points.
In both cases the patient is a surgical candidate.
Scroll through the images.
What are the findings?
In this case the main findings are the horizontal fractures of the posterior elements.
The vertebral body fractures show hardly any compression.
Notice that there are 3 vertebrae involved.
Only the level with the highest score counts.
TLICS score based on imaging is 7 points:
- Distraction: 4 points
- PLC involvement: 3 points
In this case there is severe compression of the vertebral body.
However the most important findings are the horizontal fractures of the posterior elements.
TLICS score based on imaging is 7 points.
Scroll through the images.
What are the findings?
The findings are:
- The main feature is posterior distraction with horizontal fractures of posterior elements (red arrow)
- Avulsion of a spinous process (yellow arrow)
- Widening of facet joint (green arrow)
- Burst-type fracture
In this case some would call this a burst fracture with PLC-injury i.e. 2+3 points.
However the distraction is the most important finding, i.e. distraction and PLC injury, i.e. 4+3 points.
So here is a typical case of distraction.
The primary feature is pulling apart.
There is not much else happening here.
The disc space is markedly widened about four times the normal level.
The facet joints are separated on both sides.
There is a spinous process fracture, which is not a key element but a frequently associated injury.
Continue with the MR.
The MRI shows exactly the same things.
Frequently when you have a good CT, you have most of the anatomic information.
The MRI also shows disruption of the ligamentum flavum and a partial disruption of the interspinous ligament.
TLICS score:
- Morphology: distraction - 4 points
- PLC injury - 3 points
This patient is at high risk of developing a spinal cord injury.
Here a fracture that just looks like another compression fracture on the lateral view.
At first glance the AP-view doesn't look very odd. That is until we zoom in and look at the distance between the spinous processes.
Now when you look carefully at the lateral view, you will notice that the facets are separated.
The MRI tells us the whole story.
You can see the edema related to the fracture of the vertebral body and the massive edema in the paraspinous muscles.
There is major disruption of the PLC of both the ligamenta flava and the interspinous ligament.
TLICS: distraction injury + PLC disruption.
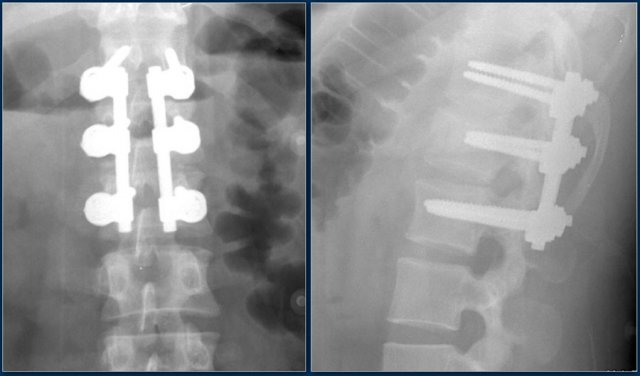
This is an interesting case since non-surgical management was initially attempted in this patient.
However when we classify according to the TLICS-score, we give 4 points for the morphology and 3 points for the PLC.
Assuming the neurological exam was normal, this patient would still get 7 points.
Unfortunately, but not unexpectedly, conservative management failed with near-dislocation.
Finally a posterior spondylodesis was performed.
Here's another example.
You could call these compression fractures.
There is loss of height with a dense band of impaction and there is an anterosuperior corner fracture on both levels.
But look at the spinous processes.
One of the spinous processes is in two pieces and the two pieces are widely separated.
So this is a distraction fracture, also known as Chance fracture.
Now when you describe such a fracture the first word in your report should be distraction, i.e. morphology: 4 points.
This next case has a great teaching point.
There is widening between the spinous processes.
But there are also little pieces ofbone, that have avulsed at least 10mm away.
At first we thought that little pieces of bone didn't matter, but they may be the most important sign of a major injury on a CT-scan.
The fact that these little pieces of bone have been so severely displaced means there has to be a major injury.
Now in this case there are lots of other things going on, but sometimes these little pieces of bone are all you get.
If you look back, see how nicely it correlates with the PLC-injury on the MRI.
The teaching point is: pay careful attention to little pieces of bone.
Patients with a rigid spine are more at risk for translation or distraction.
Here is a patient with distraction on the anterior side.
Notice the rigid spine and how easily this major injury can be overlooked.
This patient had a motorcycle accident.
The MRI demonstrates rupture of the flava ligaments, interspinous and supraspinous ligaments as well as fracture of the posterior elements and compression of the vertebral body.
A posterior spondylodesis was performed.
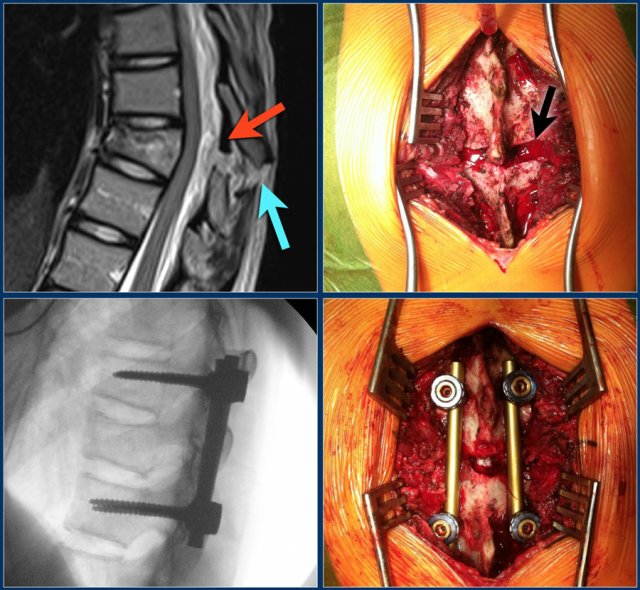
Here another distraction injury.
At surgery the rupture of the supraspinous ligament was confirmed (red and black arrows)
Additional Cases
Case 1
Scroll through the images.
How would you describe the morphology and the PLC?
The findings are:
- The morphology is of a vertebral fracture with retropulsion of a fragment, i.e. burst (2 points)
- The PLC is injured with edema of the interspinous ligament and a torn flaval ligament (3 points).
Based on imaging alone, the TLICS score is 5 points and this patient is a surgical candidate.

Case 2
Look at the images.
How would you describe the morphology and the PLC?
Then scroll to the next images.
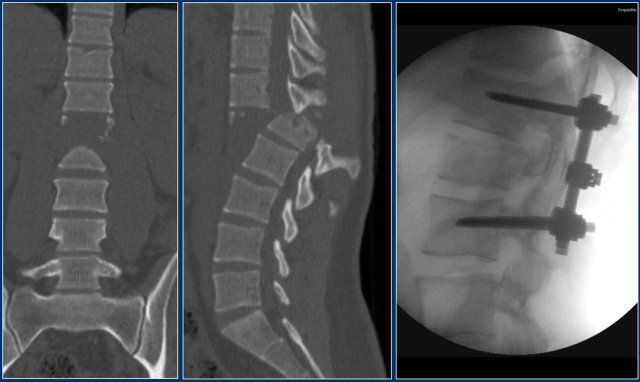
The findings are:
- Morphology: Burst - 2 points
- PLC: very subtle widening of right facet joint - 2 or 3 points
- TLICS based on imaging: 4 or 5 points
A spondylodesis was performed.
Case 3
Look at the images.
How would you describe the morphology and the PLC?
The findings are:
- Morphology: Translation - 3 points
- PLC: always disrupted in translation - 3 points
- TLICS: 6 points
Case 4
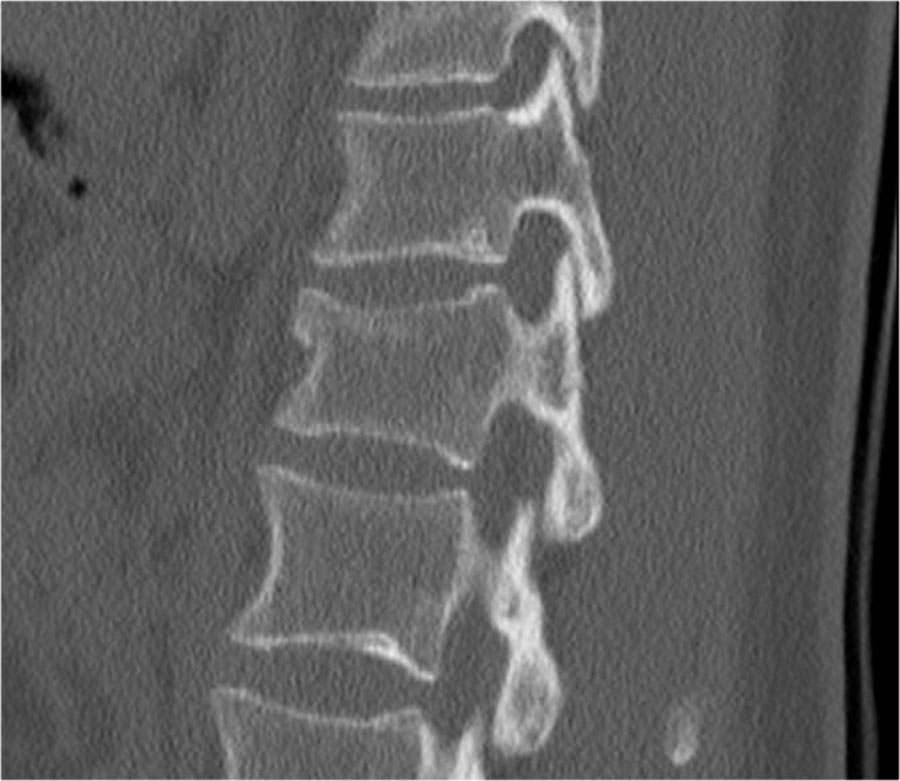
Look at the images.
How would you describe the morphology and the PLC?
The findings are:
- Morphology: Distraction- 4 points
- PLC: always disrupted in distraction on posterior side - 3 points
- TLICS: 7 points
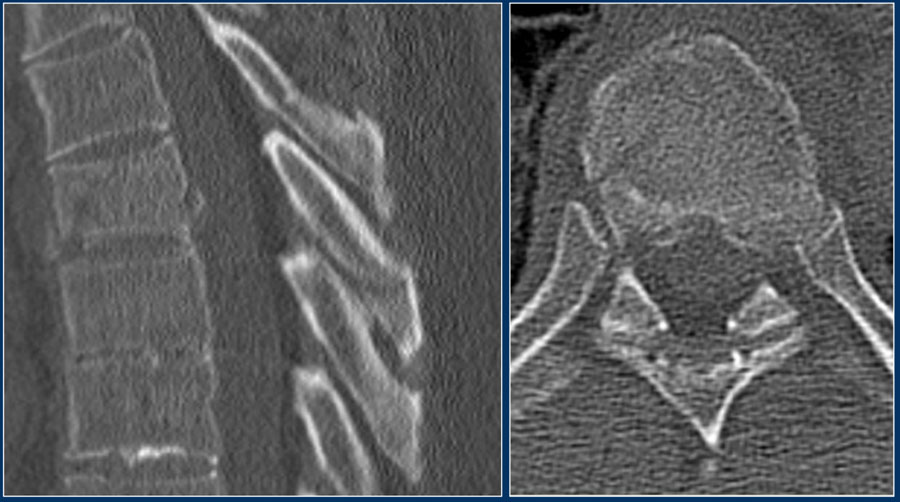
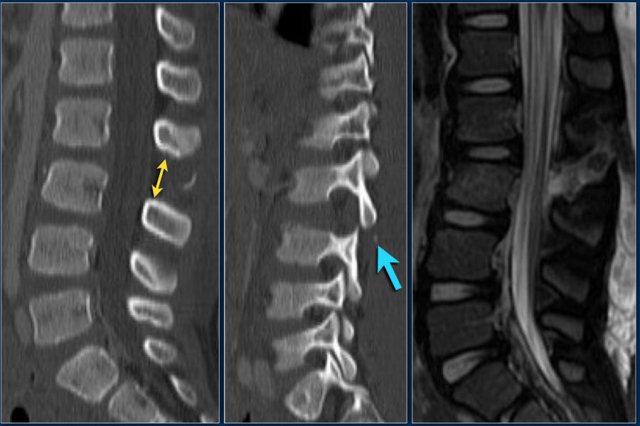
Case 5
Look at the images.
How would you describe the morphology and the PLC?
Then scroll to the next images.
The findings are:
- Morphology: Burst - 2 points
There is retropulsion of a body fragment (black arrow) - PLC: widening of both facet joints (yellow arrow) and a fracture of spinous process (blue arrow) - 3 points
- TLICS based on imaging: 5 points
Discussion: based on only these two images it is hard to say whether this is burst with PLC-injury or maybe distraction on the posterior side.
In either case the TLICS-score is high and this patient is a surgical candidate.

Case 6
Look at the images.
How would you describe the morphology and the PLC?
Then scroll to the next images.
The findings are:
- Morphology: Distraction - 4 points
- PLC: always torn in posterior distraction - 3 points
- TLICS based on imaging: 7 points
The key point in this case is that you should not describe this morphology as burst - 2 points.
The horizontal fractures on the posterior side and the increased interspinous distance indicate distraction, which means a higher score for morphology.
Always go for the highest possible score in TLICS.