BTS guideline of pulmonary nodules
Guideline of the British Thoracic Society
Onno Mets and Robin Smithuis
the Academical Medical Centre, Amsterdam and the Alrijne Hospital, Leiderdorp, the Netherlands
Publicationdate
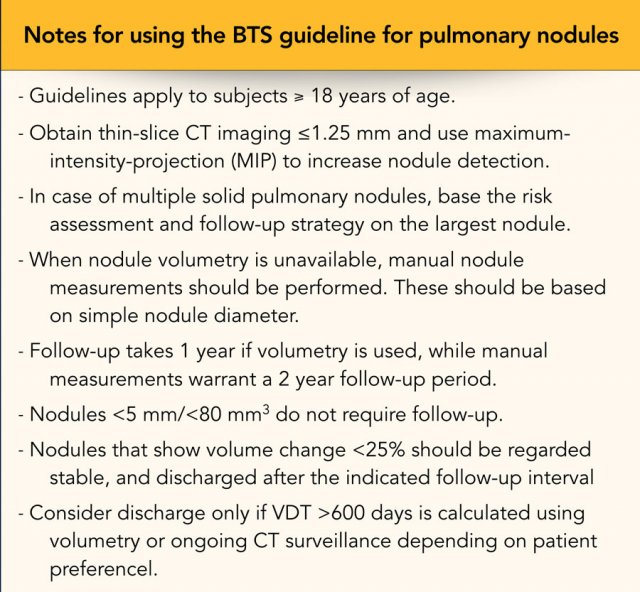
This article presents the 2015 guidelines of the British Thoracic Society (BTS) for the management of pulmonary nodules [1].
Important issues in these guidelines are:
- Higher nodule size threshold for follow up ⩾ 5mm or ⩾ 80mm3
- Reduction of the follow-up period to one year for solid nodules.
- Use of two malignancy risk prediction models to better characterize pulmonary nodules.
- The same approach for nodules detected incidentally as for those detected through screening.
Introduction
BTS guideline
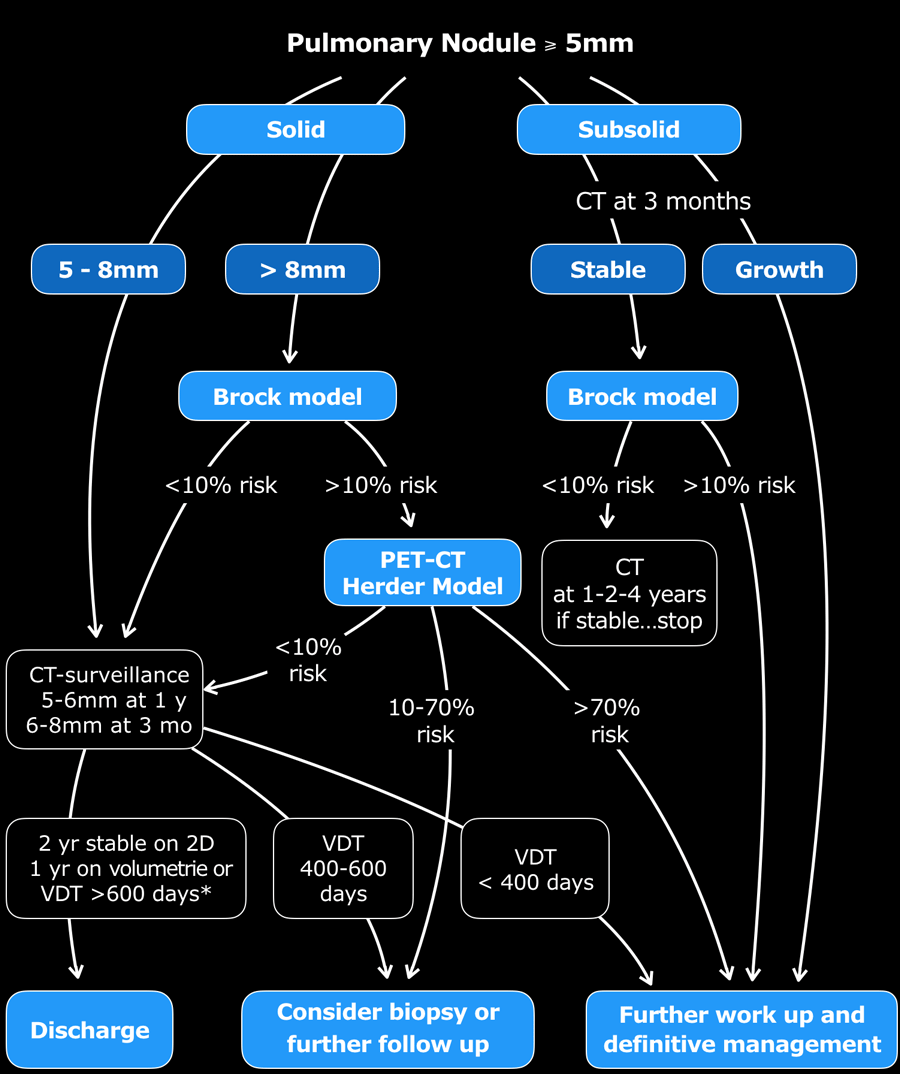
The figure shows a comprehensive version of the BTS-algorithms.
- Step 1
No follow up for nodules < 5mm and typically benign lesions with benign calcifications like hamartomas and perifissural nodules. - Step 2
Only lesions of 5mm or more require follow up. Divide lesions into solid and subsolid (groundglass or part solid) - Step 3
Use the Brock Model application to assess the risk of malignancy for solid lesions >8mm and subsolid lesions that are stable during 3 month follow up. - Step 4
Use the Herder model when you perform a PET-CT.
Follow-up takes 1 year if volumetry is used, while manual 2D-measurements warrant a 2 year follow-up period.
Nodules that show volume change less than 25% should be regarded stable and discharged after the indicated follow-up interval.
Consider discharge only if VDT >600 days is calculated using volumetry.
When there is previous imaging, determine the risk of lung cancer based on the volume doubling time.
Example 1
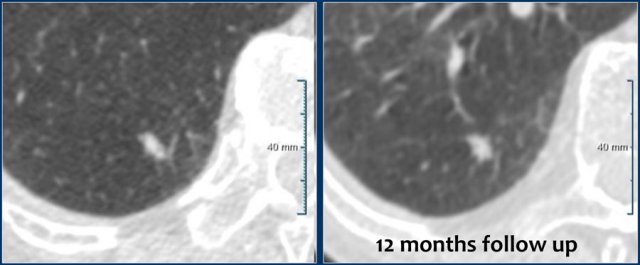
A solitary non-spiculated solid nodule of 7 mm (162 mm3) is shown in the RLL of a 55 year old male without a positive family history, but with some emphysema.
Follow-up showed long term stability with 7 mm (146 mm3) at 12 months.
Patient was discharged from further CT surveillance.
Example 2
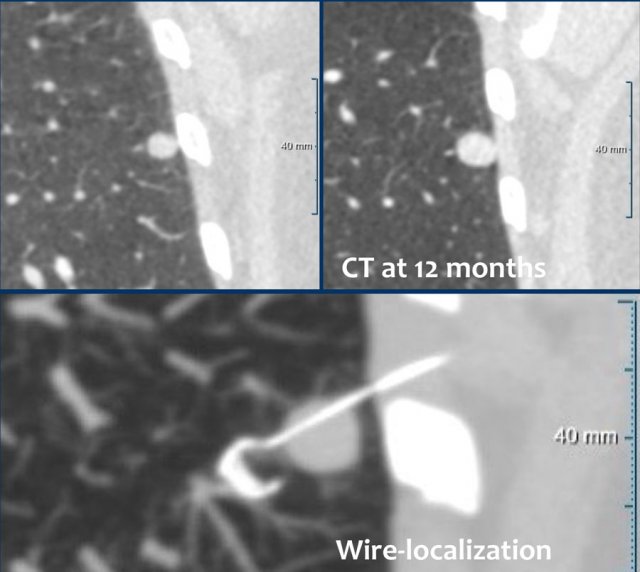
A solitary non-spiculated solid nodule of 9 mm (362 mm3) is shown in the LLL of a 75 year old female without a positive family history or emphysema.
Risk prediction by the Brock model equalled 6.3%, indicating surveillance with CT at 3 months.
This showed borderline stability, but CT at 12 months showed evident growth with a VDT <400 days.
Wedge resection after wire-localization was performed, diagnosing a pulmonary carcinoid.
BTS Pulmonary Nodule Risk Prediction Calculator
Click here to use the calculator for the Brock model, Herder model and the volume doubling time calculator after checking the box to accept the conditions of use.
With this calculator you can calculate:
- Probability of malignancy following CT (Brock Model)
- Probability of malignancy following PET-CT (Herder Model)
- Volume Doubling Time
You can also download the calculator-app on your iPhone or Android phone.
Click here to see the app in the App Store.
The BTS guidelines allow both measurements obtained using a 2D caliper technique and 3D nodule volumetry.
Note that the 2D measurement is the single maximal diameter and not the average of short- and long-axis diameters, as in the Fleischner method.
In case of multiple pulmonary nodules, the risk assessment and follow-up strategy is based on the largest nodule.
Nodule growth is defined as an volume increase ≥25%.
When the volume increase is less than 25%, the lesion is called stable.
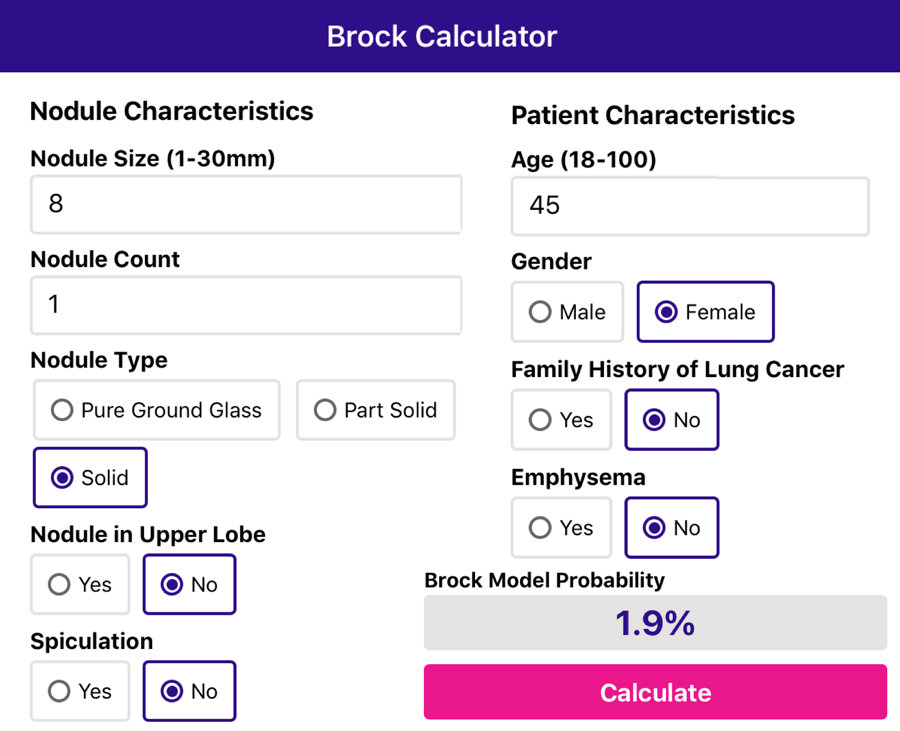
Brock Model
McWilliams and colleagues developed the Brock model for pulmonary nodule malignancy risk prediction [2].
Use the app to fill in the nodule and patient characteristics and it will calculate the malignancy risk.
Here we see an example of a 45 year old woman with an 8 mm solid nodule not located in the upper lobe and without spiculation.
There is no family history of lung cancer and there is no emphysema.
The app calculates a malignancy risk of 1.9%.
Here another example of a 65 year old man with an 26 mm solid nodule located in the upper lobe with spiculation.
There is a family history of lung cancer and there is emphysema.
The app calculates a malignancy risk of 67.7%.
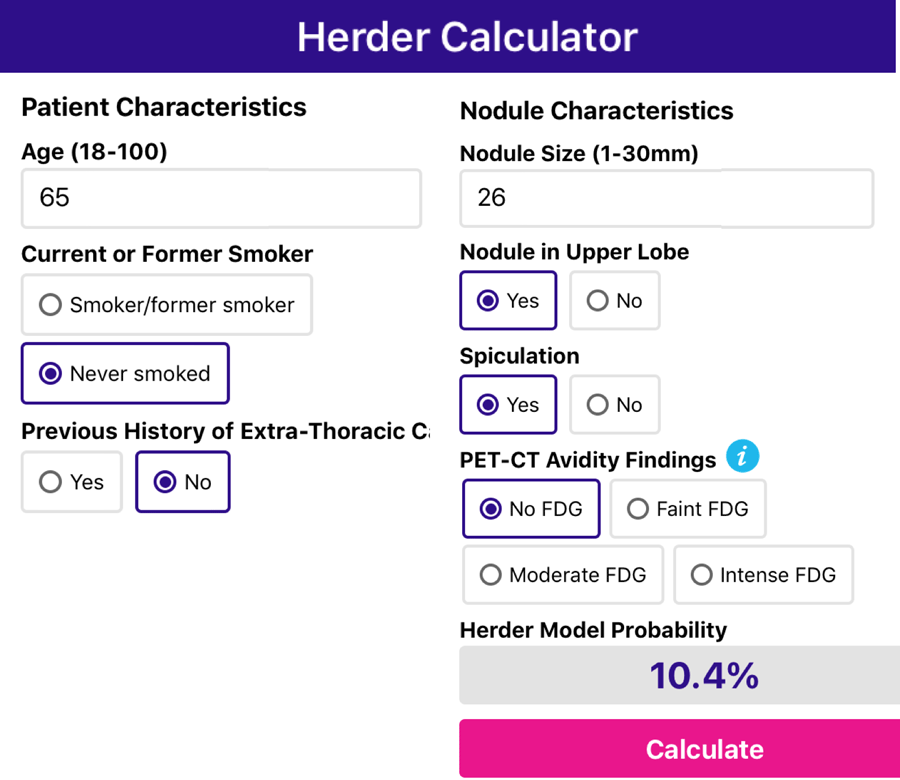
Herder model
The BTS guideline applies the Herder model to reassess the malignancy risk in nodules that are evaluated with PET-CT after a prior increased risk for malignancy, defined as a Brock score ≥10%.
It calculates the risk that a nodule will be diagnosed as cancer using :
- Patient characteristics:
age, smoking status, history of extra-thoracic cancer - Nodule characteristics:
size, upper lobe location, spiculation. - FDG-avidity: no - faint - moderate - intense.
This model showed excellent performance [3], although the performance is limited for subcentimeter nodules due to PET-CT resolution.
An example of the Herder model in the app is seen here.
It is the same 65-year old man as in the example of the Brock model.
Notice that the probability of lung cancer dropped from 67.7% to 10.4% based on the fact that there was no FDG-uptake in the lesion.
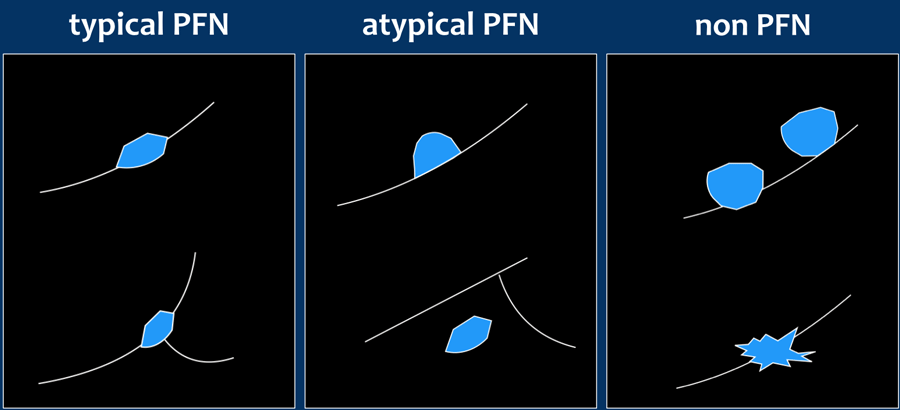
Perifissural nodules
Perifissural nodules are a separate and benign entity.
A typical PFN is attached to a pulmonary fissure, is homogeneous, and solid with smooth margins.
The shape is oval, lentiform or triangular (Figure).
A nodule with these specific characteristics needs no follow-up and is probably an intrapulmonary lymph node.
In a study by de Hoop none of the 919 typical and atypical PFNs were found to be malignant in 5.5 year follow-up.
Thus, follow-up of a perifissural nodule is indicated only when a non-PFN lesion is found.
Typical or atypical PFNs should be left alone.
Typical PFNs can show significant growth rates on serial imaging comparable to malignant nodules.
This is not a sign of malignancy, but merely a result of their lymphatic origin.
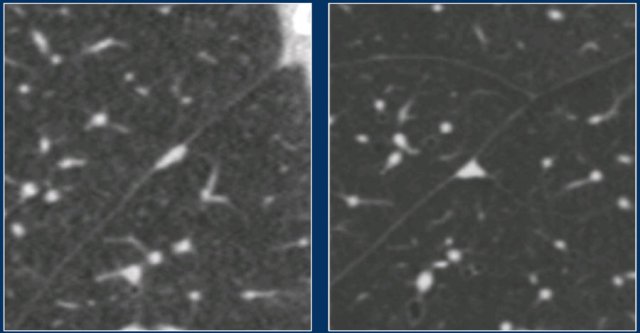
Here are two examples of typical PFNs.
No follow-up is needed.
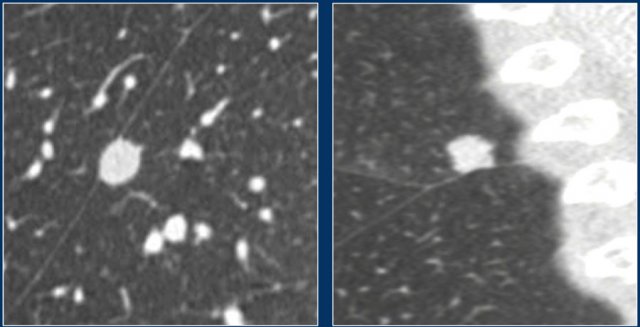
The images show lesions that do not fulfill the criteria for PFNs.
These non-PFN lesions proved to be an HCC metastasis (left) and an adenocarcinoma (right).
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.