Closed Loop Obstruction with video
Robin Smithuis
the Alrijne Hospital, Leiderdorp, the Netherlands
Publicationdate
The most important diagnosis an abdominal radiologist can make is 'Closed Loop Obstruction'.
Making this diagnosis can sometimes save the patient's life.
Preferably, the radiologist should state in every CT-report of a patient with small bowel obstruction whether it is a simple obstruction - which usually has a good prognosis - or a closed loop obstruction, in which case emergency surgery is necessary.
In this video article, we will combine text and videos to illustrate the findings of closed loop obstruction on CT and in the OR.
Introduction
Small Bowel Obstruction and Closed Loop
Ileus is usually the result of a small bowel obstruction (SBO).
In most cases this caused by adhesions, even in patients without prior surgery.
An adhesion can cause a simple obstruction; in these cases, we see a change in caliber of the bowel and both the dilated bowel and the collapsed bowel have a normal vascularization.
In closed loop obstruction, the small bowel is obstructed at two points along its course, thus forming a closed loop.
These patients have a high risk of bowel ischemia due to venous infarction, which will result in perforation, septic shock and other complications with a high mortality rate.
In this video, we have two patients with a small bowel obstruction.
The patient on the left has a simple obstruction at only one point.
The patient on the right however, has a second obstruction caused by the same adhesion.
This second obstruction is more proximal and usually difficult to detect, because both the closed loop as well as the small bowel proximal to this second obstruction are dilated.
Why is closed loop a difficult diagnosis?
This video taken in the OR demonstrates how difficult it is for the surgeon to inspect the abdomen in a patient with a closed loop obstruction.
In many cases the surgeon will not make the diagnosis of closed loop obstruction.
So, if you as a radiologist do not make the diagnosis, and the surgeon doesn't make the diagnosis, you will both not know what you have missed.
When the radiologist tells the surgeon that there is a small bowel obstruction, probably due to an adhesion, and misses the diagnosis of a closed loop obstruction, there is a good chance that the surgeon - after resecting 2 meters of necrotic bowel two days later - will say to the radiologist.... 'yeah, you were right'.
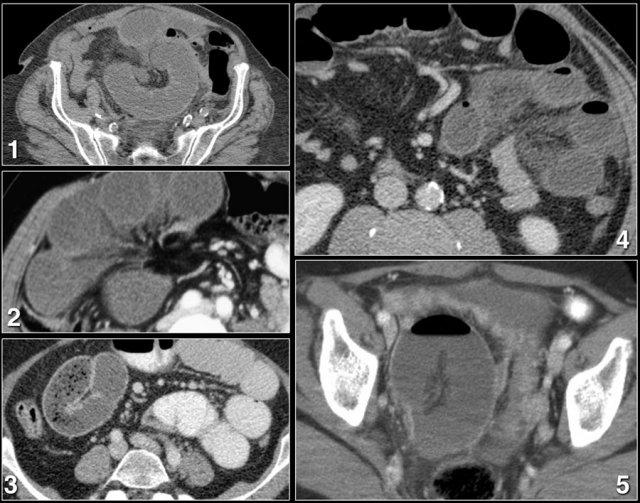
Here the axial and coronal CT images.
Closed loop obstruction is hard to diagnose on CT because it looks like a simple obstruction caused by an adhesion.
You look for a change in caliber of the bowel and once you have found it, you think that the job is done.
Look for an odd position of a group of small bowel loops with mesenteric edema and go for the second obstruction.
The video of the coronal reconstructions better shows the closed loop as well as the two points of obstruction in one plane.
Radiological signs of Closed loop obstruction
The most important signs of a closed loop obstruction on CT are:
- Odd configuration of small bowel loops
The bowel loops have a strange arrangement. In most cases, this is due to adhesions, but sometimes due to internal herniation. - Mesenteric edema
This is edema only on the mesenteric side of the bowel, the result of venous obstruction. Some call this 'wet ischemia' (unlike dry ischemia, which is seen in arterial ischemia). - Two points of obstruction
This is the ultimate proof of a closed loop obstruction.
Other signs that can be seen in patients with closed loop obstruction are:
- Dilatation of bowel loops is seen in most cases. However, in early cases the bowel has not had time to dilate (see later case)
- Bowel wall thickening
- High density of the bowel wall on the unenhanced CT as a result of hemorrhage.
- Poor enhancement of the bowel wall (uncommon finding only seen in the late arterial phase).
- Dilatation of veins
- Kinking of veins
- Ascites
- Perforation
Odd configuration of small bowel loops
Look for a strange configuration of small bowel loops clumped together.
Sometimes it looks like a volvulus.
This is not that strange, since actually a volvulus is a closed loop obstruction of the large bowel.
In the large bowel this hardly ever leads to ischemia; unlike a closed loop obstruction of the small bowel.
Mesenteric edema
Mesenteric edema is the result of venous obstruction due to strangulation.
It is only seen on the mesenteric side of the bowel, unlike the circumferential edema in enteritis or Crohn's disease.
Here is a video of a patient with closed loop obstruction demonstrating mesenteric edema.
Try to find the mesenteric edema before the green arrow does.
Two points of obstruction
Although an odd configuration of bowel loops and mesenteric edema in a patient with a small bowel obstruction are probably a good indication for surgery, finding two points of obstruction will give you 100% confidence in diagnosing a closed loop obstruction.
The two points of obstruction are always within 2 cm of each other so you don't have to look far, but they can be in any plane, so you need reconstructions.
The video shows you the images without comment first.
Try to find the closed loop with the two points of obstruction.
Then continue the video with commentary.
CT protocol
i.v. contrast
Good enhancement of the bowel wall will help you to track the bowel and to find the two stenoses.
Sometimes it even helps you to make the diagnosis of ischemia when there is a difference in enhancement.
Optimal enhancement of the bowel is in the late arterial phase and starts at about 15-20 seconds after enhancement of the abdominal aorta.
A flow of 5cc/sec will give a good peak of enhancement in the aorta and thus also in the bowel (see figure).
Do not scan in the portal venous phase, because most of the contrast will be gone.
Unfortunately, some of the patients with a closed loop obstruction are dehydrated.
Need for reconstructions
In order to find the two stenoses you need reconstructions.
Some closed loops are obvious on axial images, but sometimes reconstructions in multiple planes are necessary.
In this video, we demonstrate the importance of reconstructions.
Oral contrast
There are two main reasons to not give oral contrast:
- You cannot see the enhancement of the bowel wall
- You have to wait a while before you can start scanning and valuable time is lost, because the sooner the patient goes to surgery, the greater the chance of saving the bowel.
- The oral contrast will probably not reach the point of the first stenosis and certainly not the second stenosis.
In my opinion there is almost never a reason to give a patient oral contrast for CT scanning.
Adhesions at surgery
Most closed loop obstructions are the result of adhesions - even in patients without a history of prior abdominal surgery.
Is there always dilatation of bowel?
Of course, the answer to this question is no.
The dilatation of the small bowel proximal to the closed loop and the dilatation within the closed loop depend on the amount of obstruction at the two stenoses and the time before the patient gets to CT and surgery.
In most cases both the proximal bowel and the closed loop are dilated, but sometimes there is only dilatation of the proximal bowel or only of the closed loop.
When the obstruction is very acute and there is no time delay, the bowel may not be dilated at all, which can make the diagnosis difficult.
Watch the next video...
This is a patient without prior surgery who presented at the ER with acute abdominal pain for two hours.
This patient has a closed loop obstruction.
Notice that there is no dilatation of the small bowel, both on CT and at surgery.
After cleavage of the adhesion the bowel was placed back into the abdomen and re-inspected after 10 minutes.
The 1.5 meter of ischemic bowel had regained a normal color.
This patient left the hospital the following day, in good condition.