Bone tumor H-O
Bone tumors and tumor-like lesions in alphabethic order
Henk Jan van de Woude and Robin Smithuis
Radiology department of the Onze Lieve Vrouwe Gasthuis, Amsterdam and the Rijnland hospital, Leiderdorp, the Netherlands
Publicationdate
In Bone Tumors - Differential diagnosis we discuss a systematic approach to the differential diagnosis of bone tumors and tumor-like lesions. .
Here we continue with the most common bone tumors and tumor-like lesions in alphabethic order.
HPT - Brown tumor
key facts:
- Hyperparathyroidism typically presents in a patient with renal disease, which leads to secondary HPT.
- Bone changes in hyperparathyroidism are generally diffuse including subperiosteal resorption or generalized demineralization.
- Subperiosteal bone resorption is pathognomonic.
- Brown tumor is the result of a more extreme focal bone resorption.
It resembles a primary bone tumor or metastatic lesion. - May occur in any bone, most frequently centrally in the diaphysis.
- Not seen before the age of 30.
- Borders are usually sharp on plain radiographs, though non-sclerotic.
- May be confused with giant cell tumor when located in the epiphysis or metaphysis.
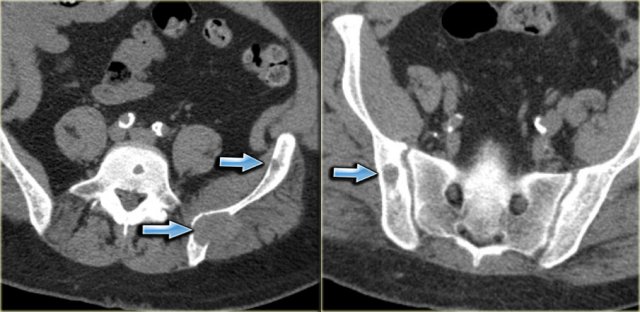
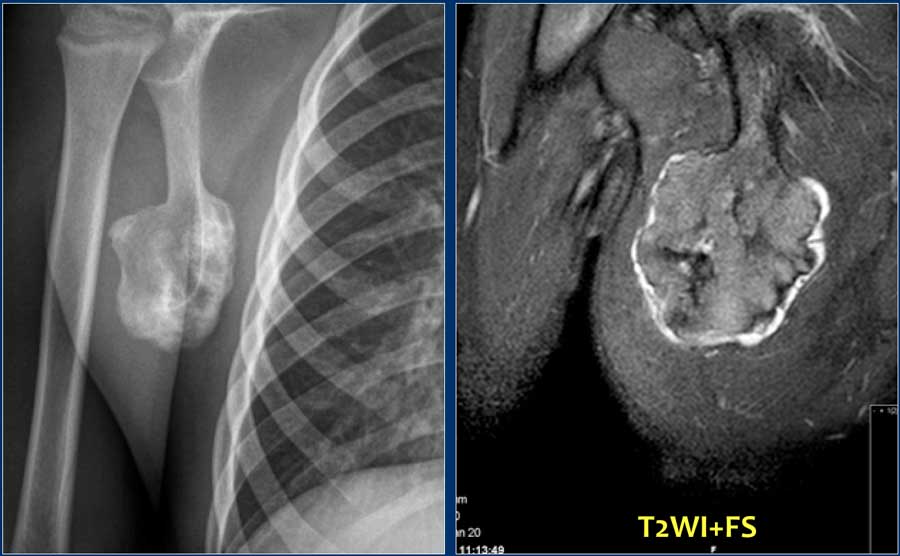
Here CT-images of a patient with renal failure and multiple well-defined osteolytic lesions.
The differential diagnosis included metastases, multiple myeloma and Brown tumors in hyperparathyroidism.
Biopsy revealed Brown tumor.
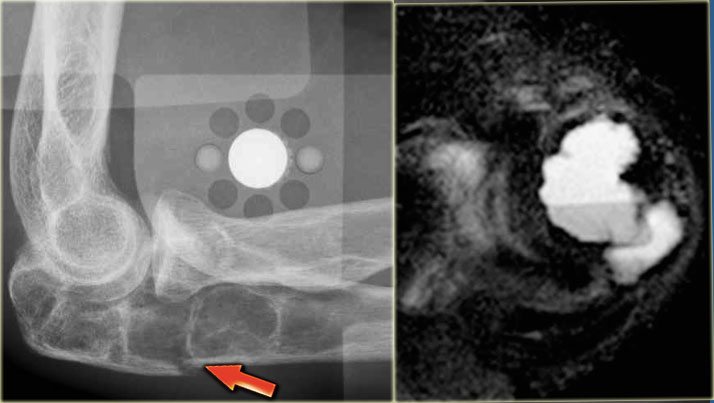
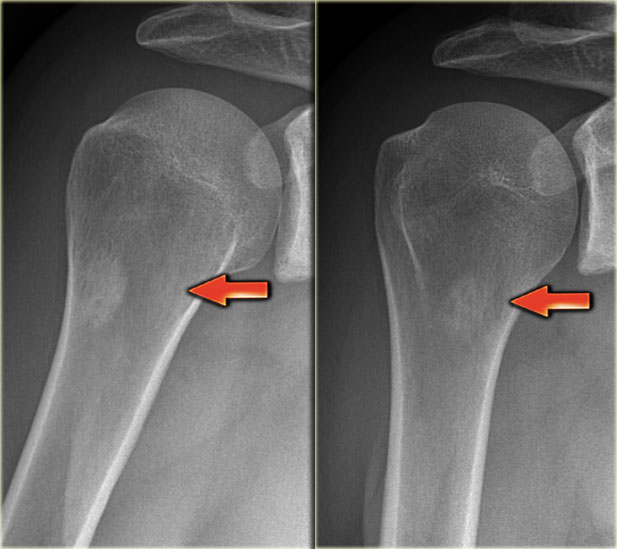
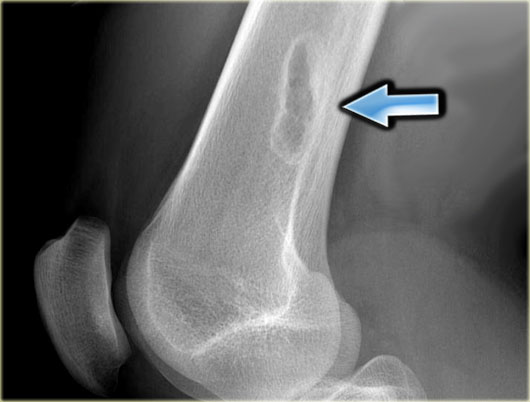
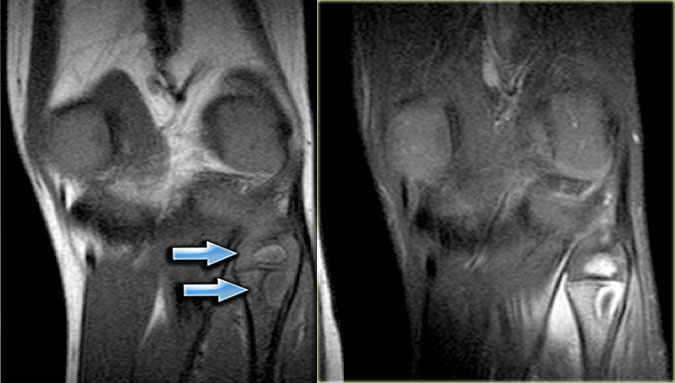
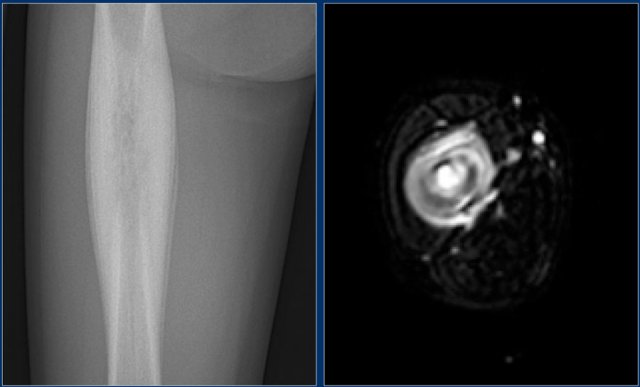
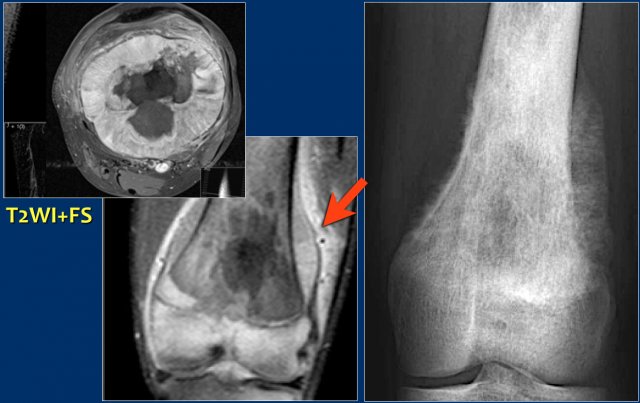
Here images of a 30-year-old male.
There is a wel-defined lytic lesion of the olecranon with several ridges and a pathologic fracture.
The differential diagnosis includes giant cell tumor and ABC.
The T2WI+FS shows fluid-levels due to sedimentation making ABC the most likely diagnosis.
Biopsy however revealed Brown tumor.
Lymphoma
key facts:
- Affects adults.
- May arise in any bone, but most commonly in femur and pelvis.
- Mostly central in diaphysis, but may occur eccentrally in metaphysis
- Usually bone involvement in known NHL, but may uncommonly arise as an isolated primary bone tumor.
- Advanced lesion: highly permeative, often large soft tissue mass.
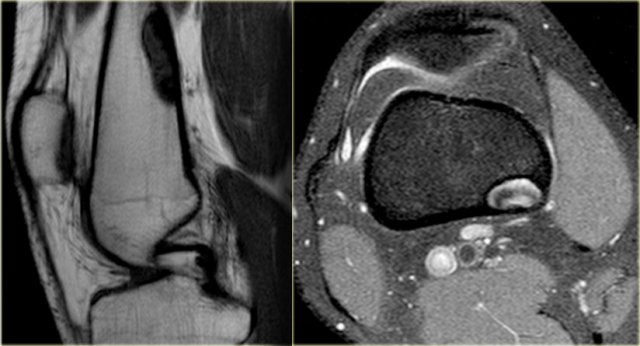
Here a NHL presenting as a non-specific ill-defined mixed osteolytic-sclerotic lesion in the proximal tibia.
Here a bone lesion in a patient with known NHL.
The imaging findings are non specific.
Melorrheostosis
key facts:
- Uncommon idiopathic disorder.
- Thickened cortical new bone with dripping candle wax-appearance.
- May be symptomatic
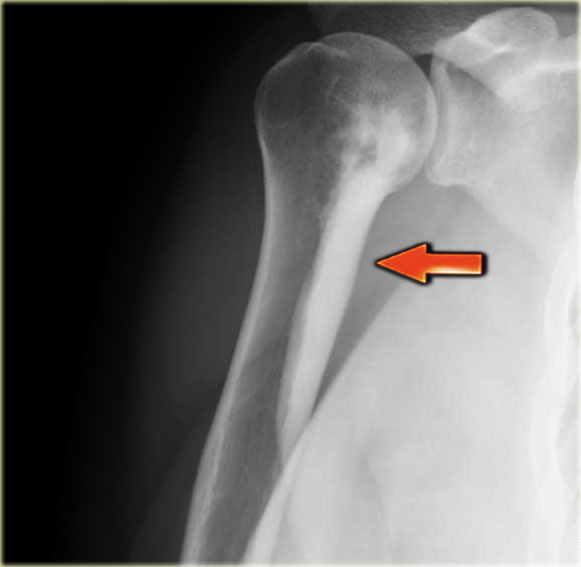
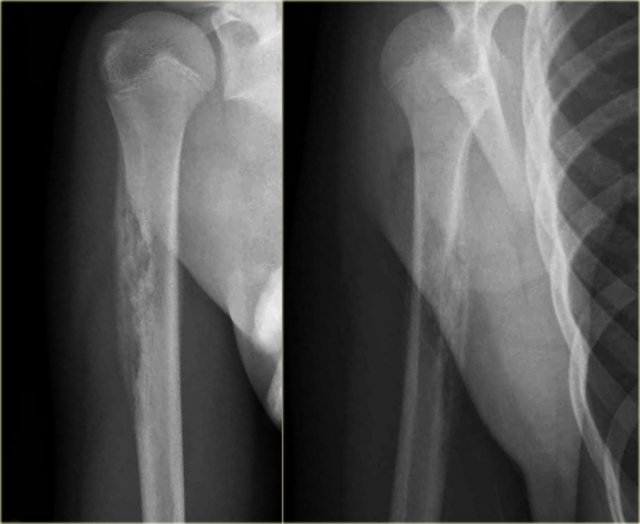
Melorrheostosis of proximal humerus.
Metastases
key facts:
- In adults, especially those over age 40, metastatic tumors are about 100 times more common than primary malignant tumors.
- Usually multifocal, occasionally solitary.
- Benign appearance does not exclude a metastasis.
- Predilection for hematopoietic marrow sites and proximal long bones, vertebrae, pelvis, ribs, cranium.
- 75% of bone metastases originate from prostate, breast, kidney or lung cancer
- Pediatric metastases: neuroblastoma, rhabdomyosarcoma, retinoblastoma
The x-rays show a sclerotic lesion in a patient with breast cancer.
This is an osteoblastic metastasis.
Osteolytic metastases
Most metastases are osteolytic.
They originate mostly from kidney, lung, colon and melanoma.
Here a subtle osteolytic metastasis in the distal femur.
Sclerotic metastases
Sclerotic metastases are osteoblastic.
In patients over the age of 40 with a sclerotic lesion, your first thought is metastatic disease.
In a patient younger than 40 years a sclerotic lesion is usually an incidental benign finding like an ossified NOF, bone island, osteoid osteoma or infection.
Here a patient with both sclerotic and osteolytic metastases.
It is a male patient, so your first thought is prostate cancer, which this patient had.
Multiple myeloma
key facts:
- Most common primary malignant bone tumor
- Older adults
- Imaging: sharply circumscribed lytic lesions or diffuse demineralization.
- Isolated myeloma lesion without systemic marrow involvement is called a plasmacytoma.
Multiple punched-out lesions in the skull.
This pattern is very characteristic fot multiple myeloma.
Also known as Swiss cheese-pattern.
Multiple small osteolytic lesions in a patient with multiple myeloma.
Non-ossifying fibroma
key facts:
- Eccentric well-defined lytic lesion with sclerotic lobulated margin.
- Usually located around the knee in diaphysis or meta/diaphysis and does not occur in hands, feet, spine and flat bones.
- Found as incidental finding or presents with a fracture.
- The natural course is a sclerotic filling over time.
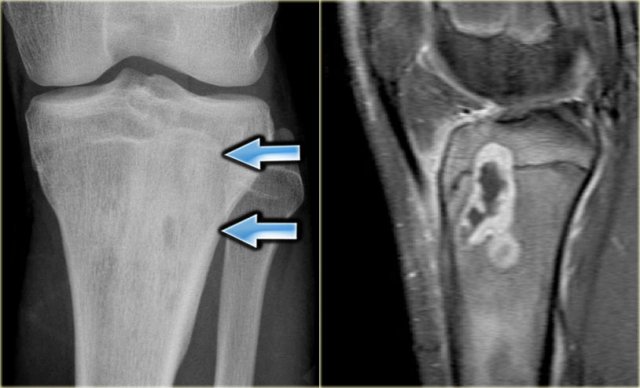
Typical case of non-ossifying fibroma.
Notice the sclerotic borders in this well-defined eccentric lytic lesion.
Same patient on MRI: eccentric well-defined lesion with intermediate to low SI on T1-WI and low to high SI on T2-WI; sclerotic margin, no surrounding edema.
More examples of NOF.
The lesion may become quite large and may then mimic fibrous dysplasia or ABC.
First presentation with a fracture is frequently seen.
Eccentric well-demarcated lesion with lucent areas, thin ridges and groundglass attenuation.
Differential diagnosis: fibrous dysplasia, giant NOF.
MRI in the same patient: well-defined, eccentric somewhat lobulated lesion with heterogeneous SI on T1-and T2-weighted fatsuppressed sequences.
On the left an incidental finding in a young adult without any symptoms of the upper leg.
There are eccentric well-defined sclerotic lesions.
This is typical for multiple non-ossifying fibromas with sclerotic fill-in.
No further imaging is required and no biopsy.
Osteoblastoma
key facts:
- Very rare lesion.
- Think of osteoblastoma when a lesion looks like a large osteoid osteoma or an ABC.
- Most common location: posterior arch of vertebral body.
Osteoblastomas are lytic lesions.
Frequently however there is associated reactive sclerosis and varying amounts of ossifications .
Therefore these lesions are discussed in the chapter of sclerotic lesions, as well as in the chapter of well-defined osteolytic lesions
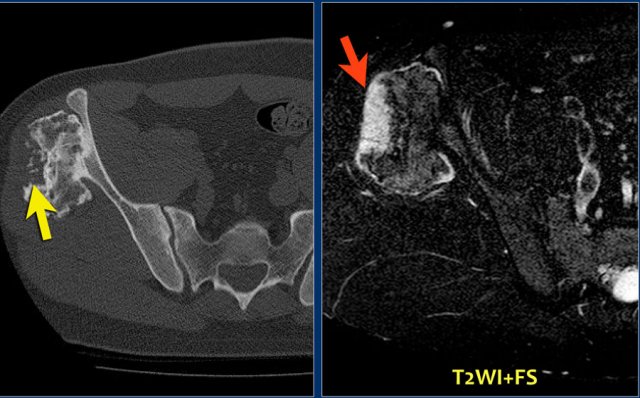
CT image of lytic lesion with central mineralisation in the right acetabulum.
T2-weighted coronal MR image shows abundant osseous edema surrounding the lesion: osteoblastoma.
The differential diagnosis includes a chondroblastoma.
Osteochondroma
key facts:
- Bony protrusion covered by a cartilaginous cap.
- Growth in childhood takes place in the cap, corresponding to normal enchondral growth at the growth plates.
- A thick cartilaginous cap in an adult is suspicious of chondrosarcoma.
Here a patient with a broad-based osteochondroma.
Notice that the cortical bone extends into the lesion.
This feature differentiates it from a juxtacortical tumor.
Here a bony protrusion arising from the scapula with the cortex extending in a mixed sclerotic mass.
The MR image shows a thin peripheral cartilage cap.
The osteochondroma consists for the larger part of bone marrow with focal sclerosis
Osteochondroma usually presents as an incidental finding, or in the form of a syndrome with multiple osteochondromas.
Radiographically, osteochondromas usually are located at the metaphysis of long bones and directed away from the joint, or arise from flat bones like the scapula or pelvis.
Typically, the underlying cortical bone extends into the stalk of the lesion, which can be thin or broad-based.
On MR imaging, the central part of a mature osteochondroma consists of fatty bone marrow, continuously with the marrow cavity of the underlying bone.
On the outside a thin cartilaginous cap may be present and focal areas of enchondral ossification, just beneath the cartilage cap.
In the mature phase, the osteochondroma is typically homogeneously sclerotic and well-defined.
Malignant transformation
Radiographic features that should raise the suspicion of malignant transformation on plain radiographs or CT include:
- Growth of osteochondroma in skeletally mature patient
- Irregular or indistinct surface of lesions
- focal lucent regions in interior of lesions
- erosion or destruction of adjacent bone
- presence of soft tissue mass with scattered or irregular calcifications
Here a patient with multiple osteochondromas.
Follow up is necessary because of an increased risk of malignant degeneration.
Continue with CT and MR.
CT:
- Large osteochondroma arising from the iliac bone.
- The central defect and punctate calcifications are highly suspicious for malignant progression to a peripheral chondrosarcoma.
MRI:
- The defect is filled with a large cartilage cap with high SI.
- This is diagnostic for the diagnosis chondrosarcoma
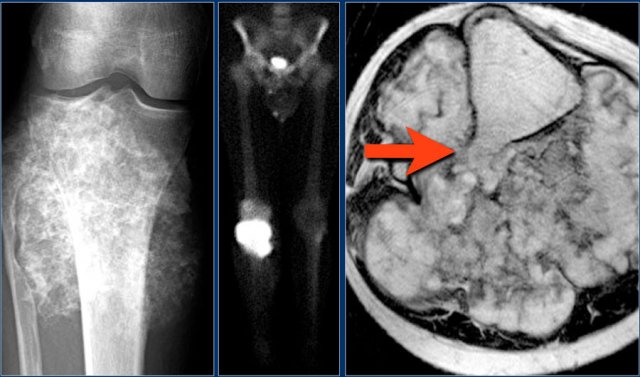
Here a patient with a large calcified mass arising from the proximal fibula.
There is high uptake on a bone scan.
The axial T1-weighted MR image demonstrates a large lobulated mass enveloping the fibula and the stalk of a previous osteochondroma in continuity with the bone marrow compartment.
All these findings indicate chondrasarcoma arising from an osteochondroma.
Osteoid osteoma
key facts:
- Typical: lucent nidus with central small sclerotic focus
- Femur, tibia, hands and feet, spine (arch).
- Usually prominent periosteal and endosteal reaction (may obscure nidus)
- Axial imaging for differentiation from Brodie abscess, osteoblastoma, stress fracture
The x-ray demonstrates an eccentric lytic lesion in the proximal femur in a child.
There is surrounding reactive sclerosis.
Histology revealed osteoid osteoma.
Osteoid osteoma may present as a lytic lesion.
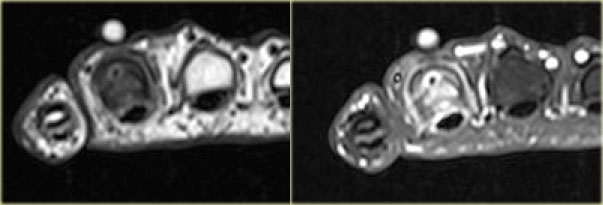
Here images of a male patient, 18 years of age, with complaints of pain, particularly at night in the fourth digit.
Plain radiograph shows extensive sclerosis and broadening of the proximal phalanx.
CT shows a small lucency with central calcification and extensive sclerosis of the bone marrow.
Scintigraphy reveals intense focal activity.
The CT findings are pathognomonic for an osteoid osteoma.
Axial T1 weighted TSE images before and after Gd-DTPA of the same patient.
The nidus with the central calcification is well seen.
Notice the enhancement of the nidus and surrounding bone marrow due to edema, which almost always present.
Here a typical osteoid osteoma in the femur.
Notice the extensive cortical broadening.
Here a typical osteoid osteoma in the radius.
CT nicely shows the nidus.
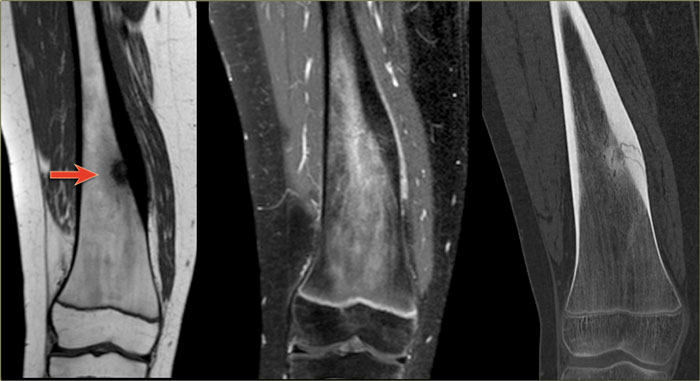
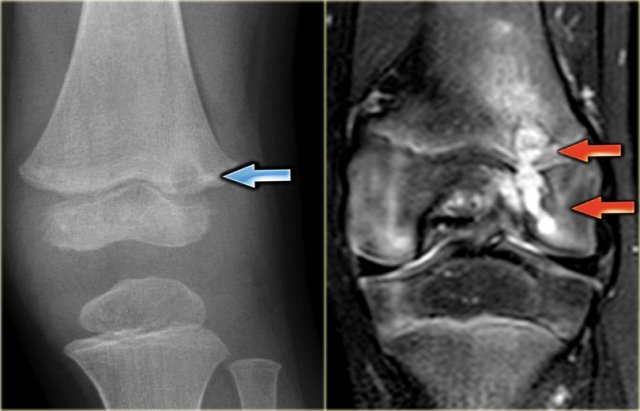
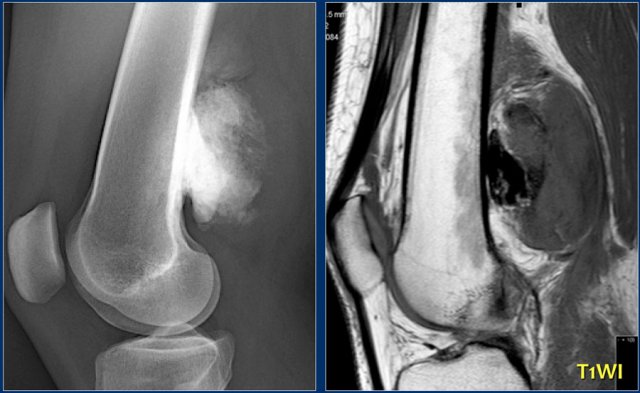
Here a typical osteoid osteoma in the tibia.
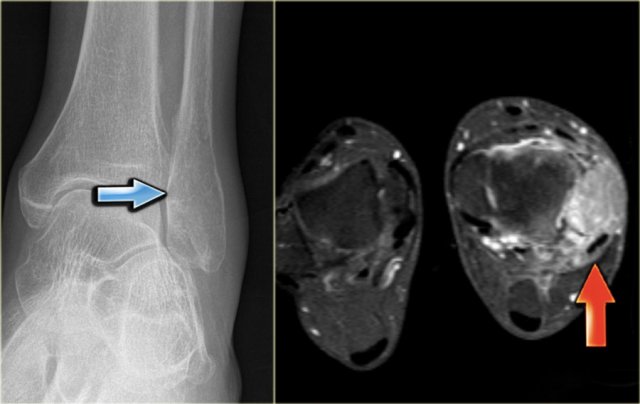
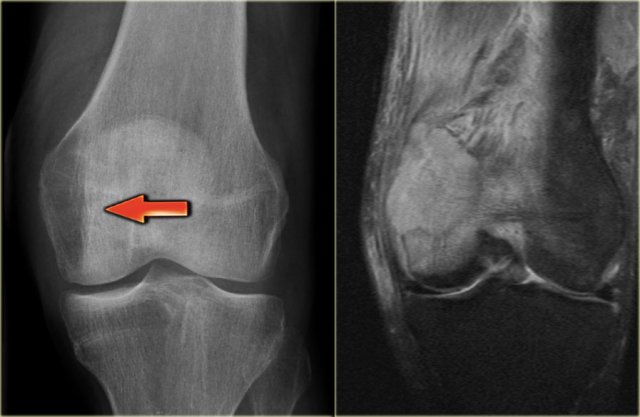
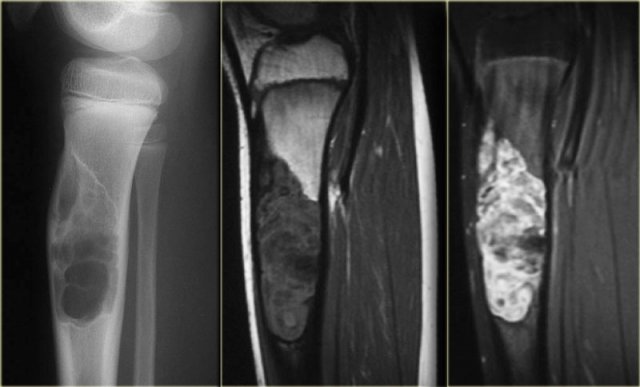
X-ray an CT-image of a typical osteoid osteoma in the proximal tibia.
Notice the sclerotic center within the osteolytic lesion (red arrow).
MR-images of the same patient demonstrate cortical thickening and extensive edema.
Osteomyelitis
key facts
- Osteomyelitis should be included in the differential diagnosis of any lytic lesion in any location in any age-group.
- May appear highly aggressive with permeative change, periosteal reaction and abscesses
- Often reactive sclerosis
- Bone defect can be found on both sides of the growth plate.
- MR: cortical breakthrough with abscesses, fascial fluid
- May not be able to differentiate from aggressive tumor
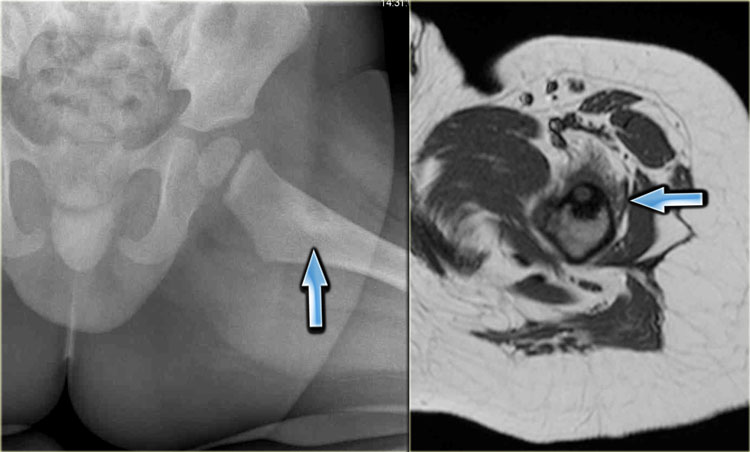
Here a patient with an eccentric lytic lesion in the metaphysis of the proximal fibula.
Coronal T1WI and T1WI with Gd and fatsat demonstrate the extension of the lesion on both sides of the physeal plate.
There is rim enhancement and edema in the bone marrow and soft tissues.
Brodie abscess
A Brodie abscess is a subacute osteomyelitis, which may persist for years before converting to a frank osteomyelitis. Brodie abscess present as an osteolytic bone defect with sharp borders surrounded by extensive reactive sclerosis.
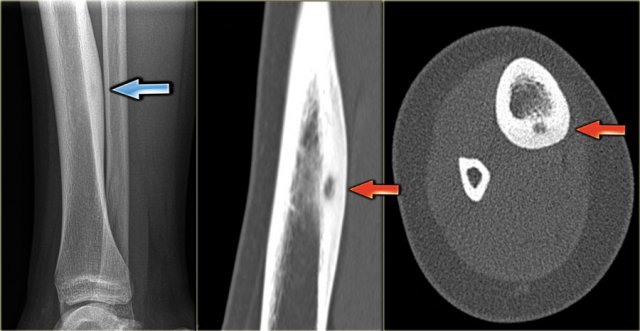
The radiograph demonstrates an ill-defined osteolytic lesion in the tibia with extensive reactive sclerosis and solid periosteal reaction.
The T1WI+Gd+FS shows that the lesion extends through the physeal plate into the epiphysis.
There is a thick rim of enhancement and extensive reactive edema.
Final diagnosis: Brodies abscess.
The radiograph shows a well-defined osteolytic lesion in the distal metaphysis of the tibia with surrounding reactive sclerosis.
The coronal T1-weighted Gd-enhanced image with fat-suppression shows a central hypointense focus with thick enhancing zone and peripheral low-intensity rim.
There is extensive bone marrow edema, which enhances.
On the sagittal T1-weighted image notice the low signal intensity rim edging the infectious foci and the low SI of the bone marrow due to edema.
Final diagnosis: Brodies abscess.
Another patient with a subacute osteomyelitis or Brodie's abscess.
On the x-ray there is an ill-defined lucent lesion on both sides of the growth plate of the femur.
The coronal T2-weighted image with fat-suppression reveals the high intensity of the abscess in the epiphysis and metaphysis and the high signal intensity of the surrounding marrow edema.
Differential diagnosis
Since osteomyelitis can mimic almost any bone tumor or tumor-like lesion in all age groups, the differential diagnosis is very large.
Differential diagnosis:
- Bone tumors:
- Ewing
- Osteosarcoma
- Lymphoma
- Osteoid osteoma
- Chondroblastoma
- Leukemia
- Tumor-like lesions or reactive processes
- Eosinophilic granuloma
- Intraosseous ganglion and synovial cyst
- Stress fracture
- Tug lesion
- Bone infarct
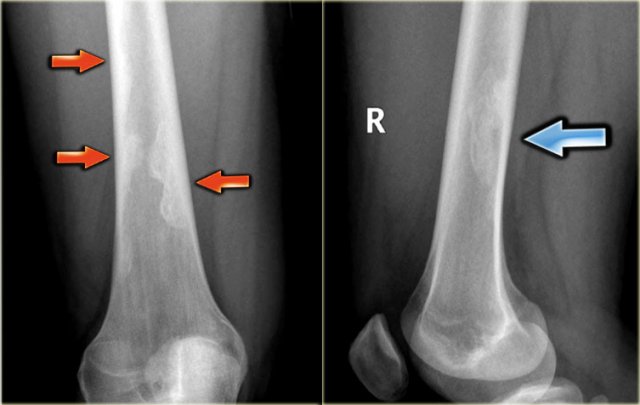
The images show another case of osteomyelitis.
Notice the ill-defined osteolysis with a permeative pattern of destruction of the cortex and an interrupted periosteal reaction.
In a child the differential diagnosis includes a Ewing sarcoma and an eosinophilic granuloma.
Here another patient with osteomyelitis.
The radiograph shows thickening of the cortical bone and an ovoid central lucency.
T1WI+Gd+FS also demonstrates cortical thickening with extensive enhancement of the bone marrow and rim-enhanced fluid collection centrally consistent with an abscess.
Here another case of osteomyelitis.
There is cortical thickening, sclerosis and a layered periosteal reaction.
Axial T2-weighted fat-suppressed image shows high signal of the bone marrow, cortex and surrounding periosteum.
Differential diagnosis:
- Eosinophilic granuloma in a young patient.
- Ewing sarcoma especially if there was an interrupted periosteal reaction and a more extensive soft tissue mass.
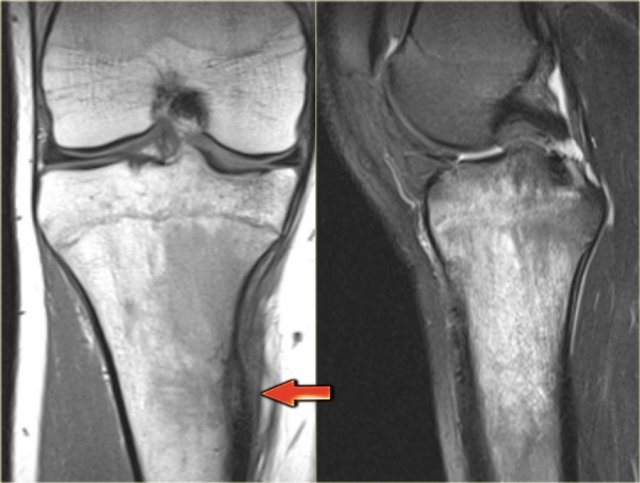
Here two patients with quite similsr findings on the radiographs.
Both have small osteolytic areas surrounded by sclerosis.
Osteosarcoma
key facts:
- Most common primary malignant bone tumor.
- Typical presentation - metaphyseal bone-forming lesion around the knee in a patient 10-25 years of age, who presents with a painful mass.
- Small second peak in > 60 years.
Study the images of a 14-year old boy and then continue reading.
The findings are:
- Radiograph.
Mixed lytic-sclerotic lesion in distal femur metaphysis and diaphysis with possible extension to the epiphysis.
The matrix of the tumor is bone.
Diagnosis: osteosarcoma. - MRI.
Coronal image confirms the epiphyseal involvement with reactive edema.
Axial image shows the circumferential soft tissue extension and relationship to the neurovascular structures.
Here another young patient with an osteosarcoma.
There is homogeneous sclerosis of a large part of the right hemipelvis with intense uptake on the bone scintigraphy.
Parosteal Osteosarcoma
key facts
- Parosteal osteosarcoma is a sarcoma that has its origin on the surface of the bone.
- Grows primarily into the surrounding soft tissues, but may also infiltrate into the bone marrow.
- Most commonly located on the posterior side of the distal femur.
- Ossification in a parosteal osteosaroma is usually more mature in the center than at the periphery. This is opposed to myositis ossificans which also may present close to the cortical bone, but maturation develops from the periphery to the center.
Study the images and then continue reading.
The findings are:
- Radiograph.
Homogeneous ossified mass adjacent to the cortical bone of the distal femur. Typical location and appearance of parosteal osteosarcoma. - MRI
Sagittal T1-weighted MR image shows partial very low signal intensity due to the ossified matrix and the cortical bone which is unimpaired.
Study the images of another 14-year old patient and then continue reading.
The findings are:
- Radiograph.
Small homogeneous mass adjacent to the cortex of the diaphysis of the femur - MRI
Juxtacortical mass with enhancement of the periphery.
Bone marrow and cortiical bone are otherwise normal.
Notice absence of reactive changes around the lesion.
Differential diagnosis:
- Organized reactive post-traumatic mass like myositis ossificans.
- Juxtacortical or Parosteal osteosarcoma, because of the homogeneity of the lesion.
Final diagnosis: parosteal osteosarcoma
Study the image and then continue reading.
The findings are:
- A well-defined and homogeneous sclerotic mass with a broad base to the underlying diaphysis of the fibula.
A juxtacortical or parosteal osteosarcoma should be considered, particularly when a history of trauma is lacking.
Final diagnosis: parosteal osteosarcoma
Paget's disease
key facts
- Paget disease is a chronic disorder of unknown origin with increased breakdown of bone and formation of disorganized new bone.
- The osteolysis can result in osteoporosis circumscripta in the skull and deformity and wedge fractures in long bones.
- There is always enlargement of bone with coarse appearance of trabeculae.
- Usually a mixed lytic-sclerotic appearance.
- Second most common bone disorder after osteoporosis.
- 70-90% of persons with Paget disease are asymptomatic.
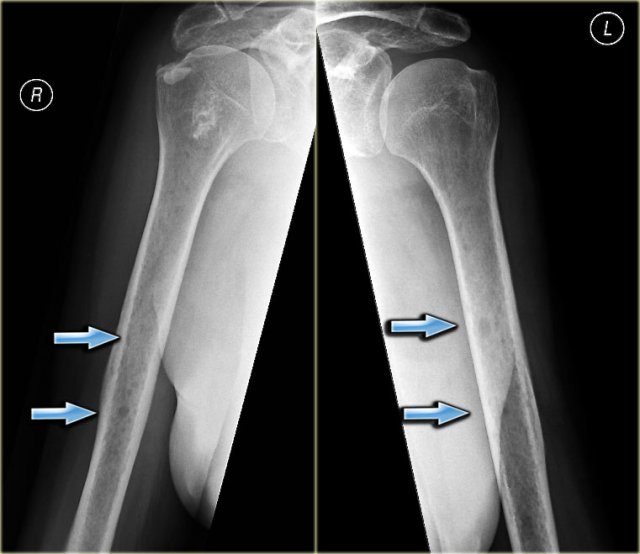
Study the images and then continue reading.
The findings are:
- Pathognomonic triad of bone expansion, cortical thickening and trabecular bone thickening.
- This is the mixed lytic and sclerotic phase of Paget.
- Positive bone scan.
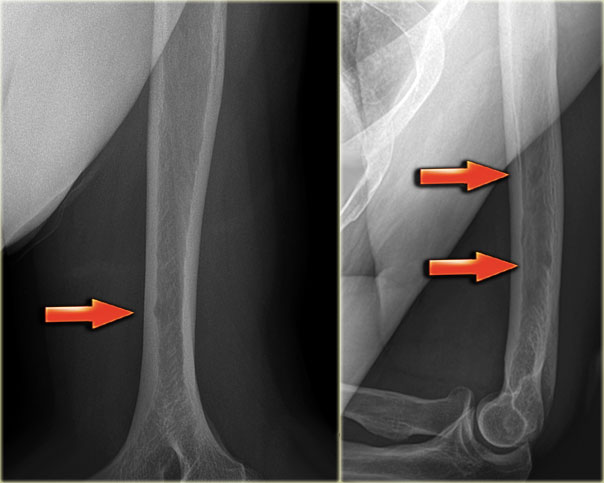
Here we see broadening of the ulna shaft is seen with a mixed lytic-sclerotic appearance and coarse trabeculation.
Differential diagnosis based on the radiograph:
- Paget's disease
- Fibrous dysplasia
The intense uptake of the tracer on the bone scintigraphy makes the diagnosis of Paget's disease the most likely.