Bone tumor A-G
Bone tumors and tumor-like lesions in alphabethic order
Henk Jan van de Woude and Robin Smithuis
Radiology department of the Onze Lieve Vrouwe Gasthuis, Amsterdam and the Rijnland hospital, Leiderdorp, the Netherlands
Publicationdate
In the article Bone Tumors - Differential diagnosis we discussed a systematic approach to the differential diagnosis of bone tumors and tumor-like lesions.
In this article, which is the first in a series of three, we will discuss the most common bone tumors and tumor-like lesions in alphabethic order.
Our goal is to show many cases in order to make you familiar with the images of these tumors.
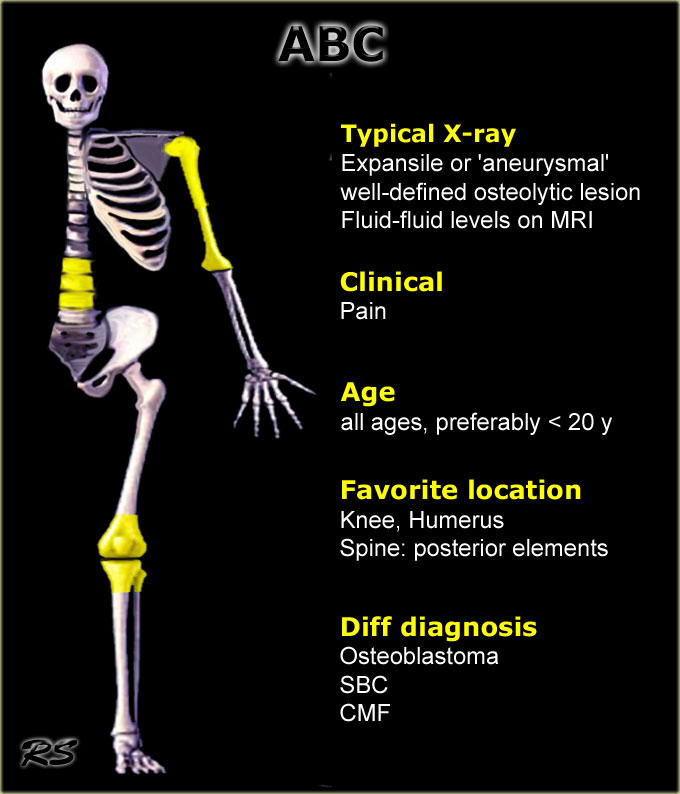
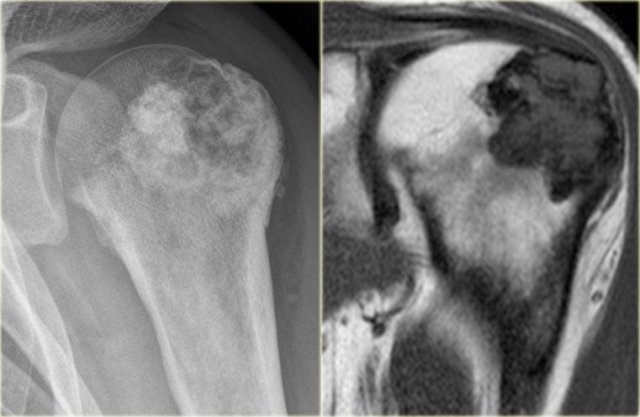
ABC
key facts:
- Aneurysmal bone cyst typically presents as a painful expansile or 'aneurysmal' well-defined osteolytic lesion in a patient younger than 30 years.
- On plain radiographs often ballooning with very thin peripheral bone shell and frequently internal thin bony ridges.
- Central or eccentric origin in the metaphysis or diaphysis of a long bone.
- In the spine located in the body or in both body and arch.
- Characteristic appearance on MR with fluid-fluid levels due to blood sedimentation.
- Peripheral enhancement of multiple small chambers is typical.
- ABC most frequently presents around the knee.
Other locations include the proximal humerus or spine, but many other bones are possible.
In the spine osteoblastoma may mimic ABC.
In the proximal humerus or femur of young children there is frequently a differential diagnosis of ABC, SBC and fibrous dysplasia.
Cavities filled with blood can also be found in giant cell tumor, osteoblastoma and chondroblastoma (i.e with secondary ABC).
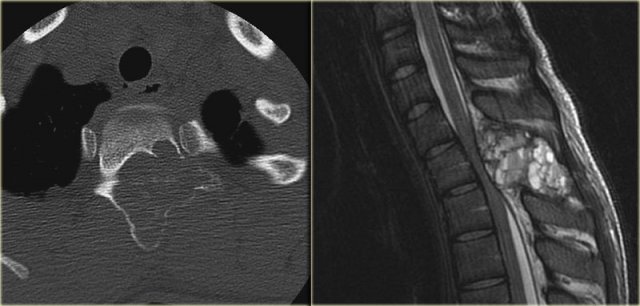
ABC (2)
On the left a typical location for an ABC in the posterior elements of the spine.
Notice the well-defined osteolytic presentation with multiple fluid-fluid levels on MR with the patient in supine position.
The differential diagnosis based on the CT is:
ABC, Osteoblastoma and Tuberculosis (1).
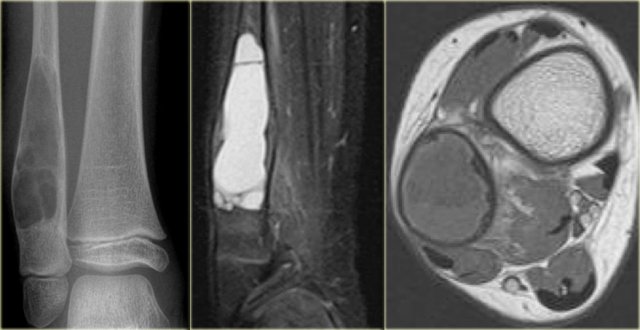
ABC (3)
On the left images of an aneurysmal or expansile well-defined osteolytic bone lesion in the fibula.
The T2-weighted MR-image shows the fluid content and on the T1-weighted image there is a subtle fluid-fluid level.
Differential diagnosis:
SBC or fibrous dysplasia with cystic changes
ABC (4)
On the left images of an aneurysmal or expansile well-defined osteolytic bone lesion in the proximal phalanx.
Notice the expansion and the enhancing rim.
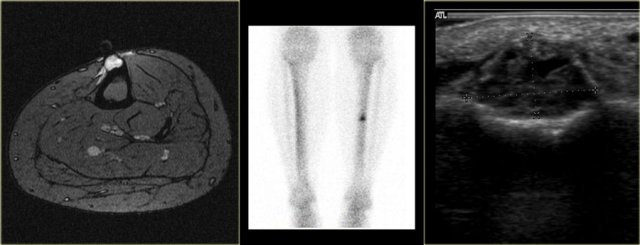
ABC (5)
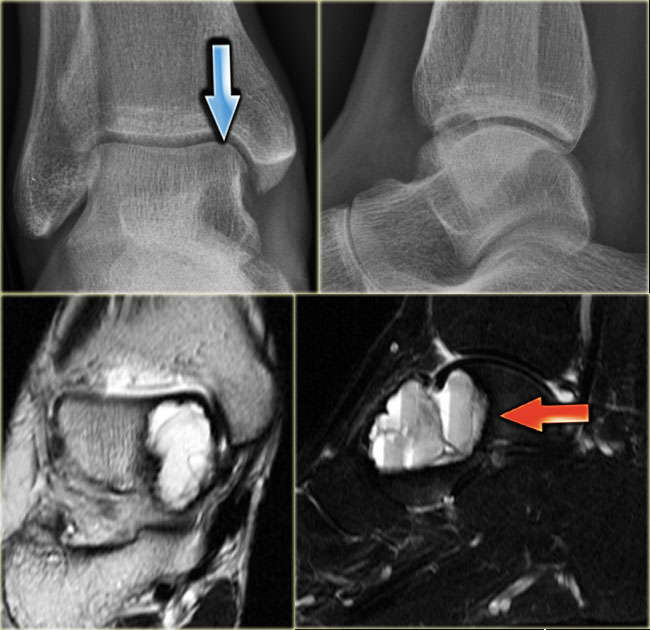
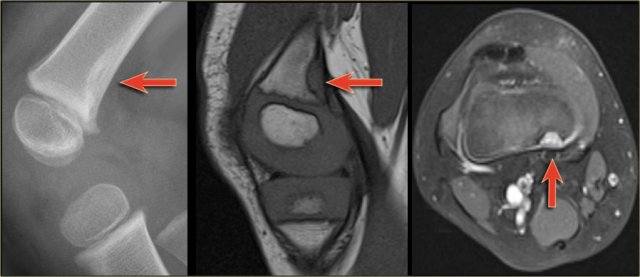
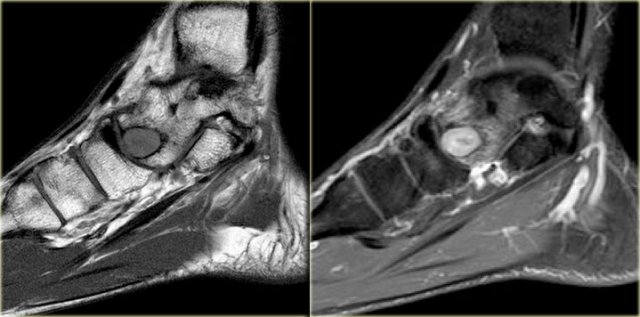
On the left an expansile well-defined osteolytic lesion with a sclerotic margin in the talus.
Axial PD-weighted image shows lobulated contours and cystic appearance with fluid-fluid level (arrow).
Most likely diagnosis: ABC.
Differential diagnosis:
chondroblastoma with secondary ABC.
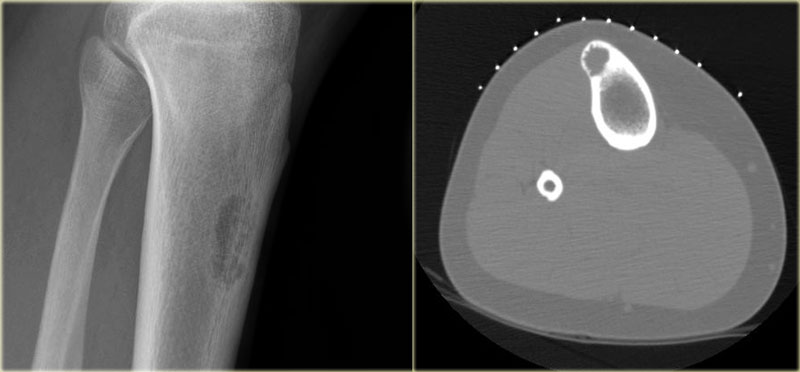
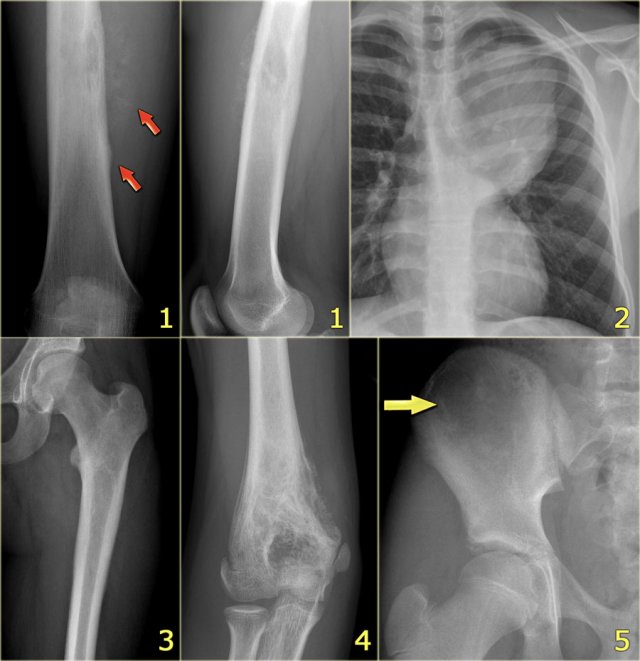
 ABC versus Adamantinoma. Notice resemblance between intracortical ABC in tibia (left) and Adamantinoma (right).
ABC versus Adamantinoma. Notice resemblance between intracortical ABC in tibia (left) and Adamantinoma (right).
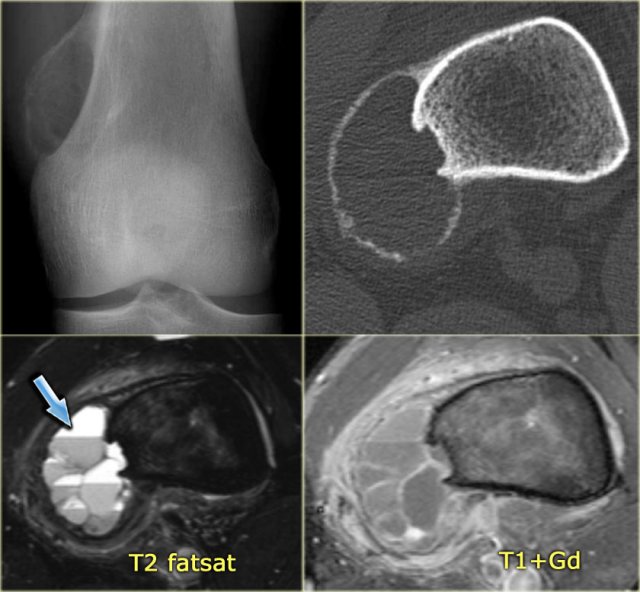
ABC (6) - atypical case
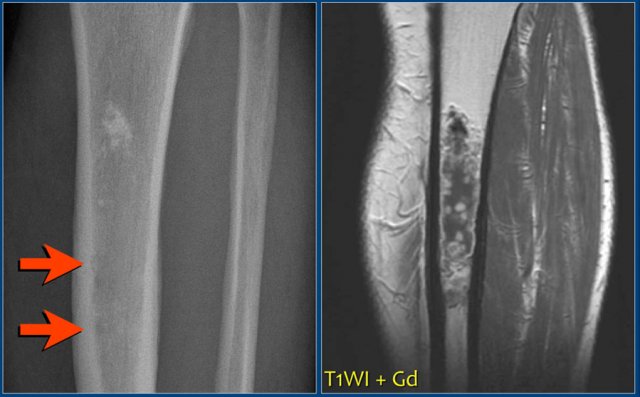
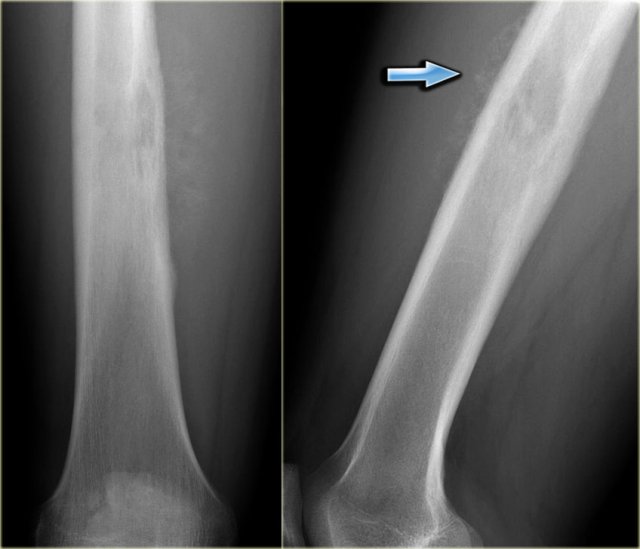
On the left two different patients with an intracortical or subperosteal osteolytic well-defined lesion in the tibia.
The lesion on the far left was thought to be an adamantinoma because of the localisation in the anterior tibial cortex.
At biopsy it proved to be an ABC.
The image on the right is an adamantinoma.
Continue with the additional examinations in this ABC.
Here the MR, bone scan and the sonogram of the same patient with ABC.
On the axial T2WI with fat saturation subtle sedimentation is seen.
The bone marrow is completely normal.
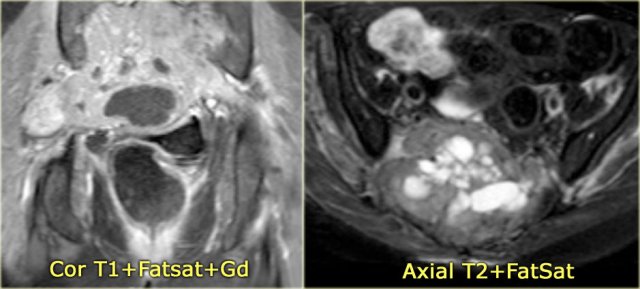
ABC (7)
Here another ABC in the talus.
It is barely visible on the X-rays and was initially missed.
MR shows typical fluid-fluid levels.
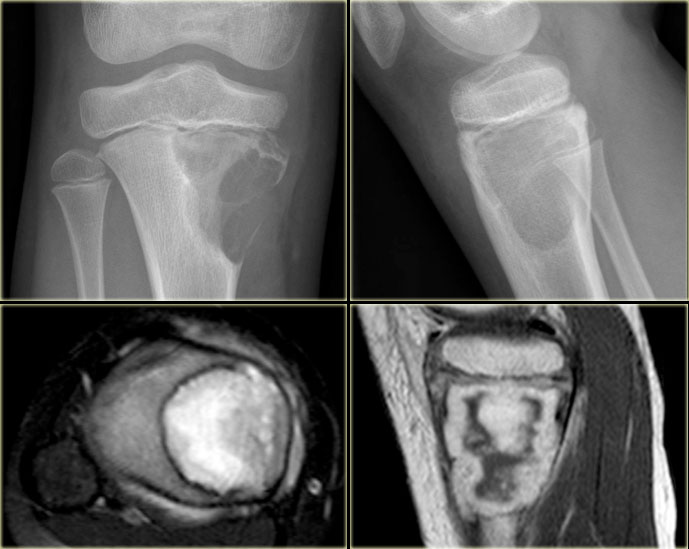
ABC (8)
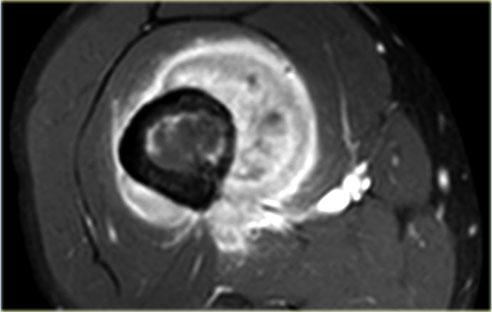
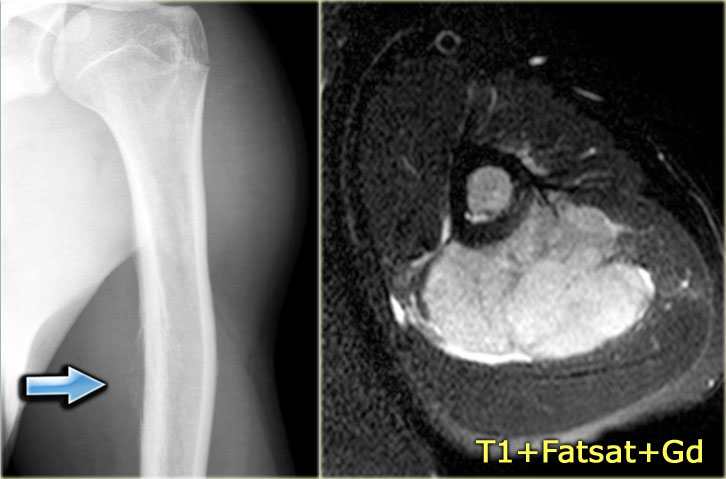
On the left another ABC, located in the distal femur.
The plain radiograph shows a layered periosteal reaction and Codman triangle in direct relationship to an expansile lytic lesion with a thin peripheral bone shell.
CT also reveals the subperiosteal origin of the lesion with secondary involvement of the cortical bone.
Axial T2-weighted image with fatsat and contrast enhanced T1-weighted image with fat sat show multiple fluid-fluid levels with rim enhancement of the cavities filled with blood.
This is typical for an aneurysmal bone cyst.
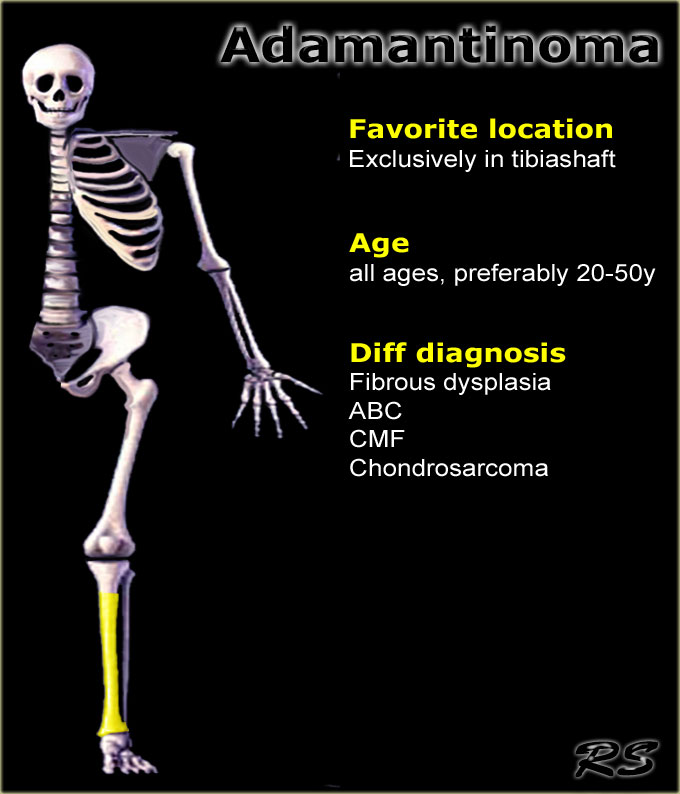
Adamantinoma
key facts:
- Rare low-grade malignant lesion, exclusively found in the diaphysis of the anterior cortex of the tibia.
- Adamantinoma may present as a solitary focus or multicentric lucencies
- May extend into the marrow cavity.
- Plain radiographs and CT show cortical lucencies combined with sclerosis.
- On MRI, the lesion is lobulated with high signal intensity on T2-weighted images and strong enhancement after Gd-DTPA.
- Main differential diagnosis: fibrous dysplasia.
Adamantinoma (2)
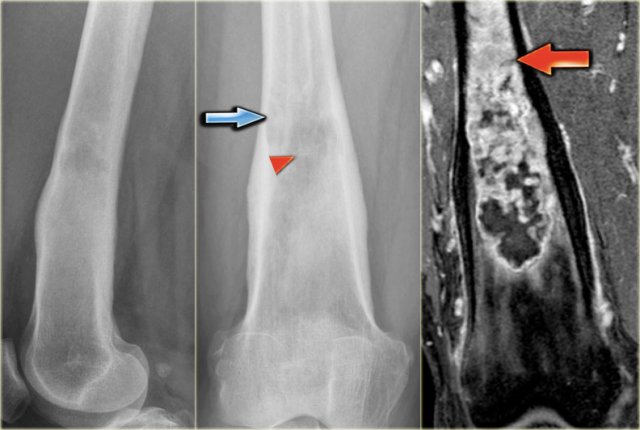
Young patient with a lobulated lytic lesion within the anterior cortical bone of the proximal tibia.
There is a second lucency separately more proximal within the cortical bone.
Axail CT image prior to biopsy demonstrates the lytic appearance of the lesion within the thickened cortical bone.
In the differential diagnosis could have been chondromyxoid fibroma or fibro-osseous lesion, however, the separate cortical lesion strongly suggests adamantinoma, which is almost exclusively found in the tibia and often multicentric.
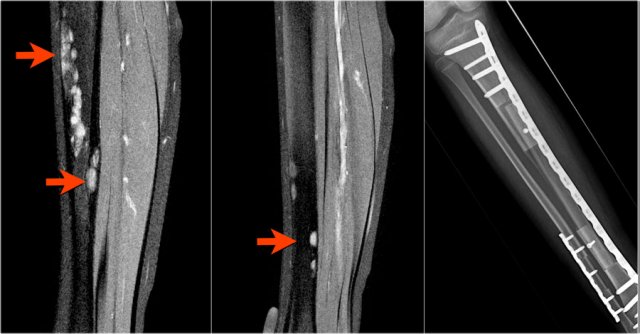
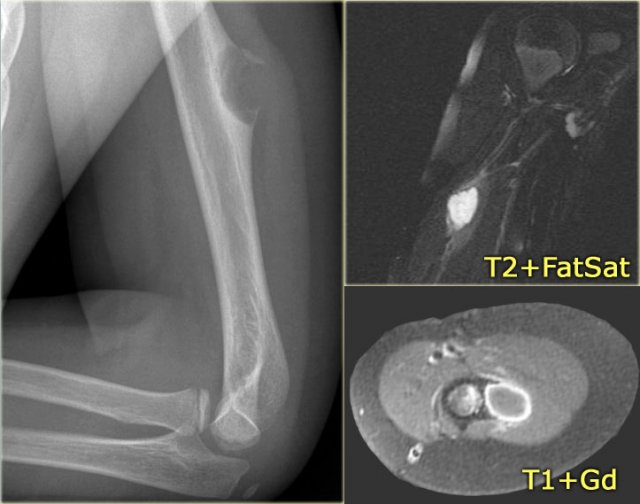
Adamantinoma (3)
Adamantinoma of the tibia in another patient.
There is an ovoid osteolytic lesion within the anterior cortical bone.
Lobulated high signal intensity on axial T2-weighted image.
There is no extension into the bone marrow.
Homogeneous enhancement on T1-weighted image after Gd-DTPA.
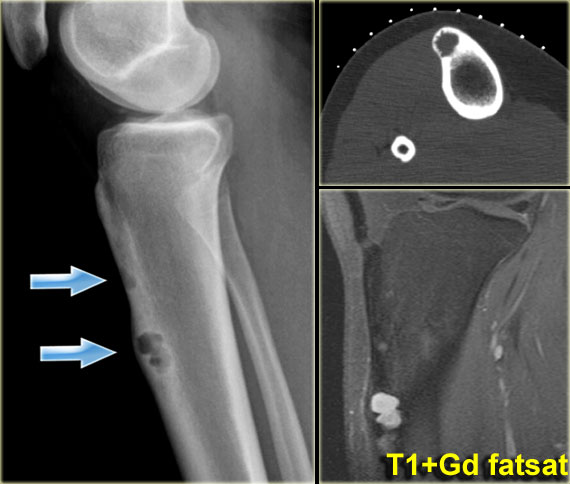
Adamantinoma (4)
On the left a radiograph and CT-image of another typical adamantinoma.
CT was performed prior to biopsy.
Here a mixed sclerotic-lytic lesion, cortically based in the tibia shaft in a 12-year old boy.
There is also a lucent lesion in the cortex of the fibula.
Differential diagnosis includes adamantinoma or osteofibrous dysplasia, based on the typical location, age (2nd-3rd decade) and radiographic appearance.
Biopsy showed adamantinoma.
Continue with the MR.
Same patient.
Sagittal T2-weighted fat-suppressed images demonstrate multiple foci of high SI within the cortices of tibia and fibula.
Post-operative situation on the right.
Care should be taken that each focus is entirely removed.
MRI is pivotal for demonstrating the intramedullary and soft tissue extension.
Adamantinoma (5)
Here another patient with an adamantinoma.
MR reveals also extension within the bone marrow compartment.
Bone infarction
Key facts
- Typical presentation: central lesion in metaphysis or diaphysis with a well defined serpentiginous border.
- May resemble cartilaginous tumors.
- Causes: corticosteroid use, sickle cell disease, trauma, Gaucher's disease, renal transplantation.
The term bone infarction is used for osteonecrosis within the diaphysis or metaphysis.
If the osteonecrosis is located in the epiphysis, the term avascular osteonecrosis is used.
The radiograph shows typical bone infarcts in diaphysis and metaphysis of femur and tibia.
On MR imaging bone infarcts are characterized by irregulair serpentiginous margins with low signal intensity on both T1 and T2 WI and with intermediate to high fat signal in the center part.
Enhancement after i.v. Gadolinium is usually minimal or absent (see right image).
At the periphery of the infarct a zone of relative high signal intensity on T2WI may be found.
Here an almost identical case.
Typical MR pattern of bone infarctions with peripheral serpentiginous zones of low SI and central area of fat. Some enhacement may be encountered surrounding the infarction.
Differentiating a bone infarct from an enchondroma or low-grade chondrosarcoma on plain films can be difficult or even impossible.
Cartilaginous tumors in particular chondrosarcoma may show endosteal scalloping, while a bone infarct does not.
Chrondroid tumors are more frequently encountered than bone infarcts.
Bone island
A bone island consists of well-differentiated mature bone tissue within the marrow, also referred to as enostosis.
Usually it is seen as a coincidental finding.
In patients with breast- or prostate cancer a bone island can be mistaken for an osteoblastic metastasis.
A bone island normally does not show increased uptake on a bone scan.
Bone island (2)
On the left a well-defined compact sclerotic lesion in the proximal humerus.
Most likely diagnosis: bone island or enostosis.
In patient with a known malignancy consider: osteoblastic metastasis.
Brown tumor in Hyperparathyroidism
key facts:
- Bone changes in hyperparathyroidism are generally diffuse including subperiosteal resorption or generalized demineralization.
- More extreme focal bone resorption may result in a lesion which resembles a primary bone tumor or metastatic lesion.
- May occur in any bone, most frequently centrally in the diaphysis.
- Not seen before the age of 30.
- Borders are usually sharp on plain radiographs, though non-sclerotic.
- May be confused with giant cell tumor when located in the epi-metaphysis.
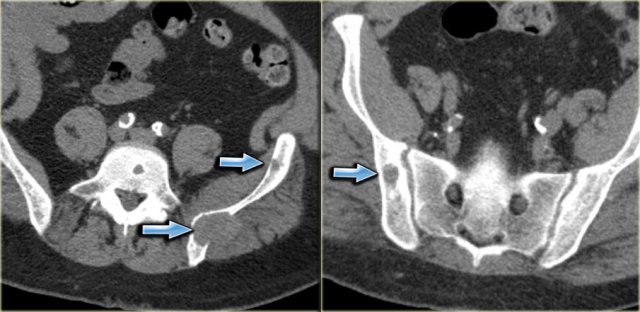
On the left a patient who had a nefrectomy for renal cell carcinoma and who was on dialysis.
Multiple well-defined osteolytic lesions were found on a follow up CT scan.
The differential diagnosis included metastases and Brown tumors in hyperparathyroidism.
Biopsy revealed Brown tumor.
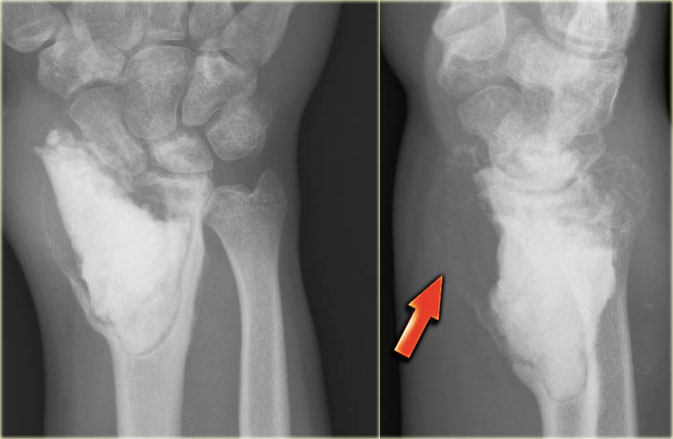
Brown tumor (2)
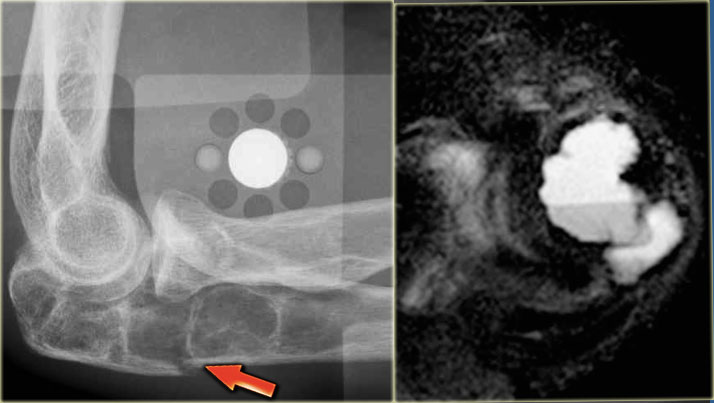
On the left images of a 30-year-old male with well-defined lytic lesion of the olecranon.
On the radiograph several ridges can be seen and a pathologic fracture (arrow).
The T2-weighted image with fat saturation demonstrates fluid-levels due to sedimentation.
Most likely diagnosis: giant cell tumor and ABC.
Biopsy revealed brown tumor.
Here images of a 33-year old male with a diaphyseal eccentric sharply defined lytic lesion predominantly located in the cortical bone.
CT shows the cortical origin with thin peripheral rim in this patients with hyperparathyroidism.
Diagnosis: Brown tumor.
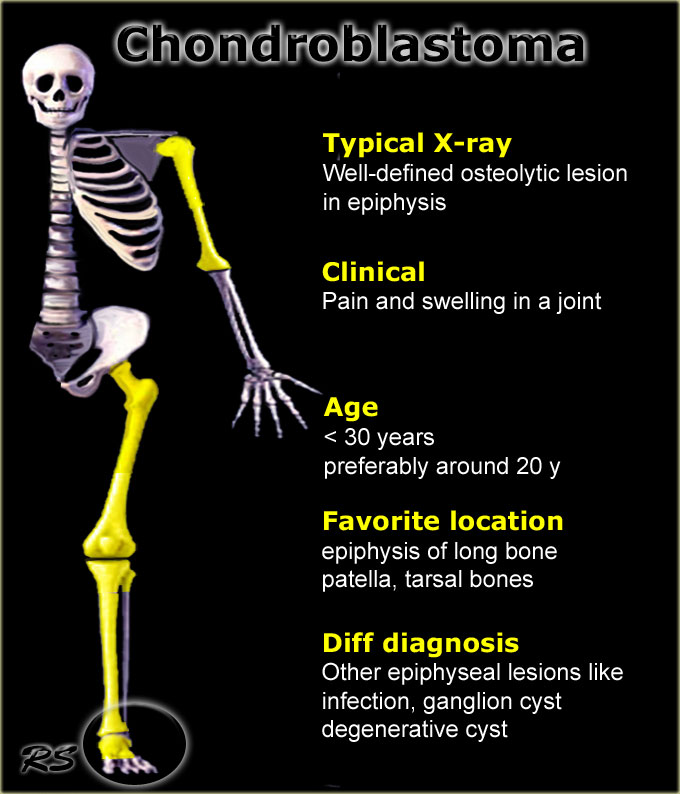
Chondroblastoma
key facts:
- Typical presentation: well-defined osteolytic lesion in tarsal bone, patella or epiphysis of a long bone in a 20-year old with pain and swelling in a joint.
- Abundant edema is almost always present.
- DD: Ganglion cyst, osteomyelitis, GCT, ABC, enchondroma.
The lesion can be lobulated, usually with a sclerotic margin.
Frequently a regular benign periosteal reaction is present.
MR imaging usually shows prominent bone marrow and soft tissue edema.
The differential diagnosis of an epiphyseal lesion in young patients, besides chondroblastoma, includes osteomyelitis and ganglion cyst.
In the foot the differential diagnosis is longer.
Click here for more examples of bone tumors in the foot.
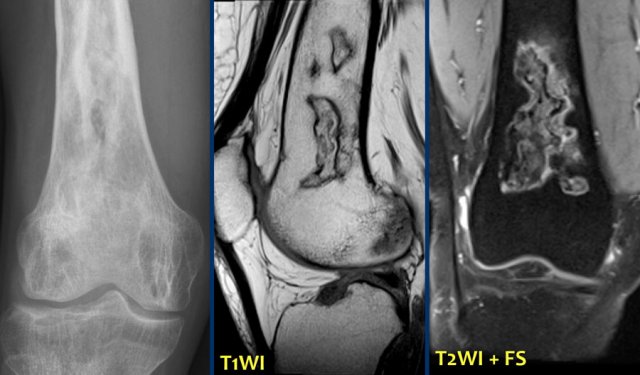
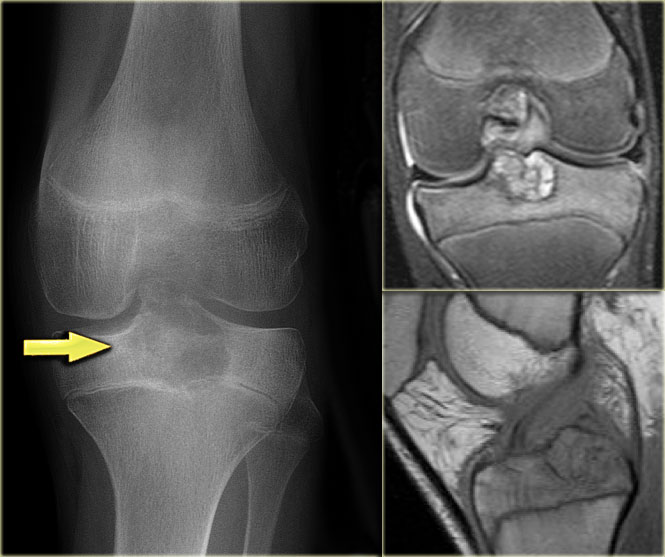
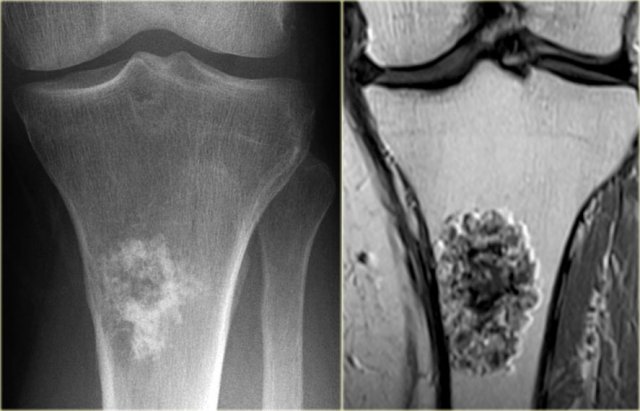
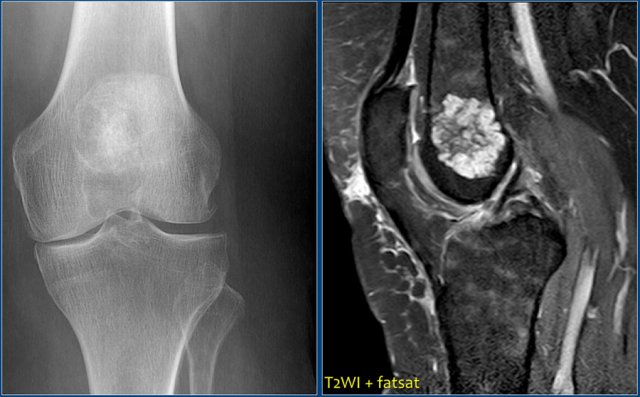
Chondroblastoma (2)
There is a well-defined lytic lesion located posteriorly in the proximal epiphysis of the tibia.
On the radiograph there is some reactive sclerosis surrounding the lesion.
There is no matrix formation.
On the coronal T2-weighted image with fat suppression the lesion has a high SI and subtle internal ridges.
There is edema of the entire epiphysis.
On a sagittal T1-weighted image there is a discrete sclerotic margin.
If there were signs of osteoarthrosis, the differential diagnosis would be a chondroblastoma and a degenerative cyst (or geode).
Click here for comparison to a degenerative cyst in the tibia with similar findings.
 Chondroblastoma. Sagittal T1-weighted image (left) and sagittal T1-weighted image with fatsat after Gd-DTPA (right).
Chondroblastoma. Sagittal T1-weighted image (left) and sagittal T1-weighted image with fatsat after Gd-DTPA (right).
Chondroblastoma (3)
The talar or calcaneal bone is one of the predilectional sites of chondroblastoma.
Note the thin sclerotic margin and surrounding edema.
Other diagnostic possibilities in the young population: SBC (no edema), ABC (fluid levels), or osteoblastoma.
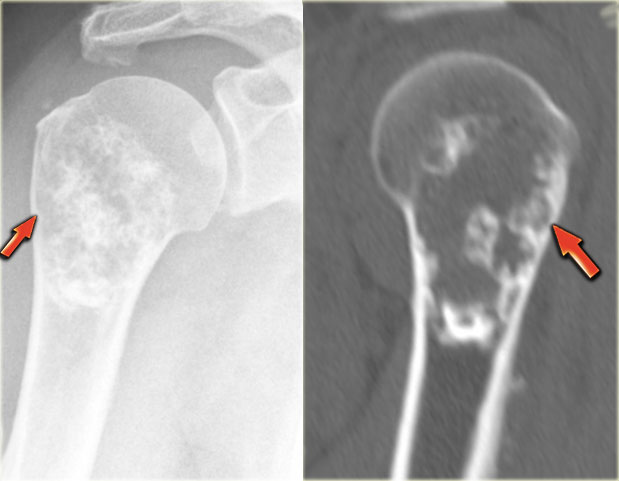
Chondroblastoma (4)
Here a lesion located in the epi- and metaphysis of the proximal humerus.
The lesion is predominantly calcified.
Coronal T1W image shows lobulated margins and peripheral low SI due to the calcifications.
Notice the surrounding decreased signal intensity of the bone marrow, consistent with edema.
Edema almost always accompanies chondroblastoma, but is unusual in other chondroid tumors, like enchondroma or low-grade chondrosarcoma.
Diagnosis: Chondroblastoma.
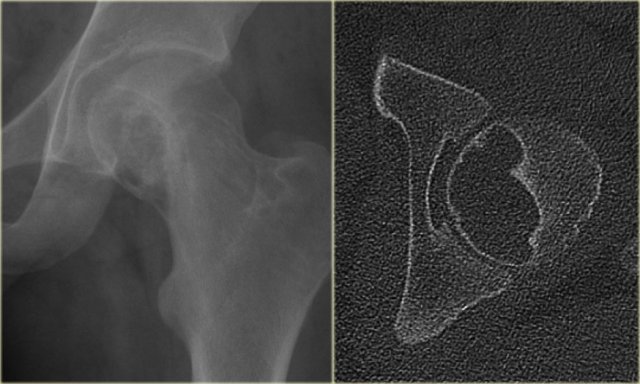
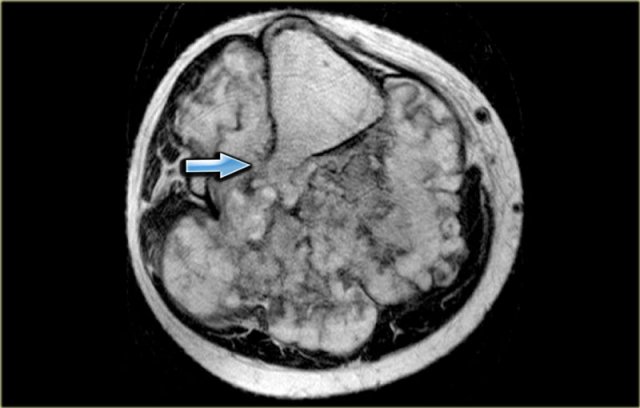
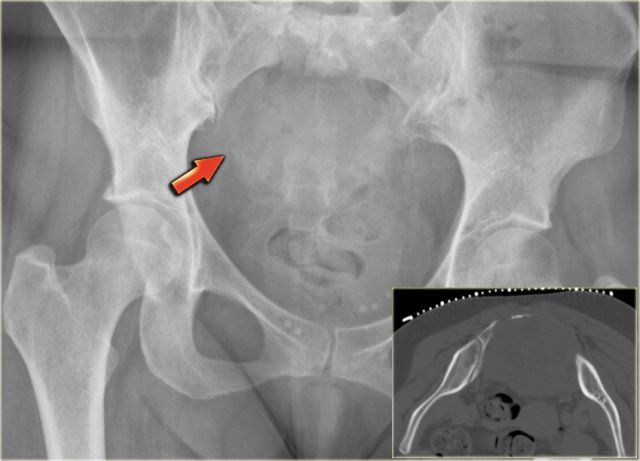
Chondroblastoma (5)
On the left an eccentric well-defined lytic lesion in the proximal femur.
CT image shows a lobulated and sclerotic border.
The location in the epiphysis is typical for a chondroblastoma.
Continue with the MR.
Same patient.
Coronal T2-WI with FS demonstrates high SI of the lesion with a low intensity sclerotic border with perilesional edema.
Chondroblastoma (6)
Edema is almost always present in chondroblastoma.
Here some examples:
- Typical chondroblastoma with epiphyseal localization. Some reactive sclerosis and abundant perilesional edema on T2-weighted image with fat saturation.
- Coronal T2-weighted image with fat saturation demonstratesa chondroblastoma in the femur epiphysis with perilesional edema (same case as above).
- Sagittal T1-weighted MR image of a lytic lesion with peripheral sclerotic rim in the posterior talar bone in a young patient.
The lesion is hypointense, well-defined with a low intensity rim.
The bone marrow has a low signal intensity due to extensive edema (arrow).
Chondroblastoma (7)
The images show a chondroblastoma in the patella.
Notice the extensive edema (blue arrow)
Chondroblastoma (8)
Here lesion in the proximal tibia in a 20 year old.
Key findings:
- Epiphyseal lesion
- Lobulated margins
- Extensive edema
- Young patient.
Diagnosis: Chondroblastoma.
Diff. diagnosis: Osteomyelitis.
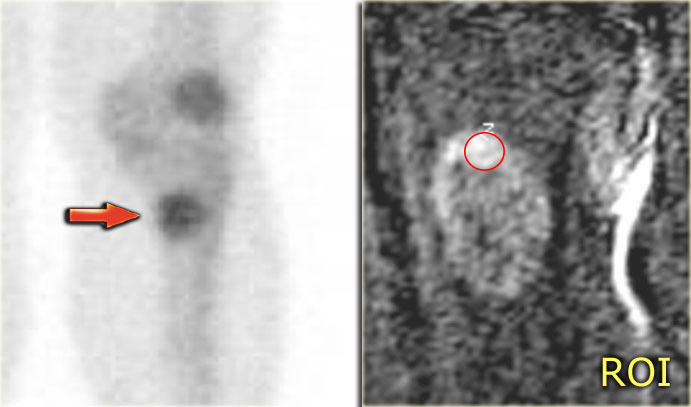
Chondroblastoma (9)
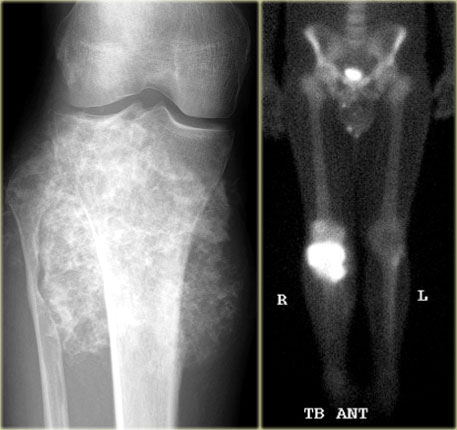
What are the findings:
- Well-defined osteolytic lesion in the talus.
- No matrix formation.
- Subtle reactive sclerosis.
- T2-WI with FS shows typical extensive peritumoral edema in the entire bone.
- High uptake on bone scintigraphy.
Diagnosis: Chondroblastoma.
The talar bone is one of the preferential sites for chondroblastoma.
Chondromyxoid fibroma
key facts:
- CMF is a rare benign osteolytic lobulated lesion preferentially found eccentric in the tibia metaphysis and less common in the femur and foot.
- Mainly found in young adults.
- The lesion may cause cortical expansion.
- Calcifications are usually not present.
- Differential diagnosis: ABC, NOF and fibrous dysplasia.
Chondromyxoid fibroma (2)
Eccentric well-defined lytic lesion in the metaphysis of the proximal tibia in a young child.
Contours are somewhat lobulated, narrow transitional zone.
Differential diagnosis, because of the eccentric manifestation: non-ossifying fibroma or chondromyxoid fibroma.
Axial T2-weighted image nicely shows the low SI sclerotic margin, high SI of the intrinsic part of the lesion, bone marrow edema and some soft tissue reaction.
There is thick peripheral enhancement on sagittal T1-weighted after Gd-DTPA.
The MR features support the diagnosis of CMF
Chondromyxoid fibroma (3)
On the left a well-defined lytic lesion at the base of the 2nd metatarsal bone.
There is no mineralisation.
T1-weighted images before and after Gd-DTPA demonstrate some expansion and lobulation.
On the T1-weighted image before contrast there is a nonspecific intermediate signal intensity.
After the administration of Gadolinium there is thick peripheral enhancement.
Differential diagnosis based on plain radiograph: giant cell tumor or chondroid lesion, i.e. enchondroma, low grade chondrosarcoma or CMF.
Biopsy revealed CMF.
Although this is a rare lesion, the foot is one of the preferential sites of origin.
Chondromyxoid fibroma (4)
On the left a diaphyseal cortically based lytic lesion with expansion and a thin peripheral bone shell.
There is peripheral enhancement on the axial T1-weighted image with fat saturation.
The lobulated morphology with high SI on the T2-weighted image with fat saturation suggests that this is a cartilaginous lesion.
Fianl diagnosis: chondromyxoid fibroma
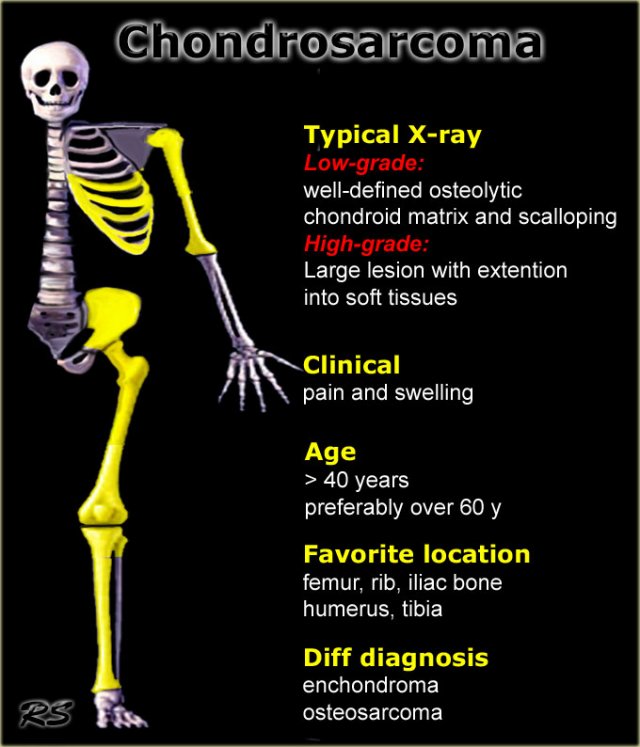
Chondrosarcoma
key facts:
- Malignant bone tumor that produces cartilage.
- Typical presentation: large osteolytic lesion with scalloping of the inner cortex and rings-and-arcs or popcorn calcifications in an elderly person with a painful swelling.
- Secundary chondrosarcoma is most common and arises from enchondroma or osteochondroma.
- Patients with multiple enchondromas like in Ollier's disease and Mafucci's syndrome are at risk.
- Low grade tumor can usually not be differentiated from enchondroma based on imaging findings alone.
- High grade tumor may present as aggressive ill-defined lesion with extention into the soft tissues.
On plain radiographs the differential diagnosis with enchondroma can be difficult.
Think of chondrosarcoma instead of enchondroma if there is one or more of the following features:
- Elderly patient
- Location in long bones
- Size > 5 cm
- Uptake on bone scan
- Endosteal scalloping on MRI
- Cortical involvement
- Early enhancement on dynamic contrast enhanced series
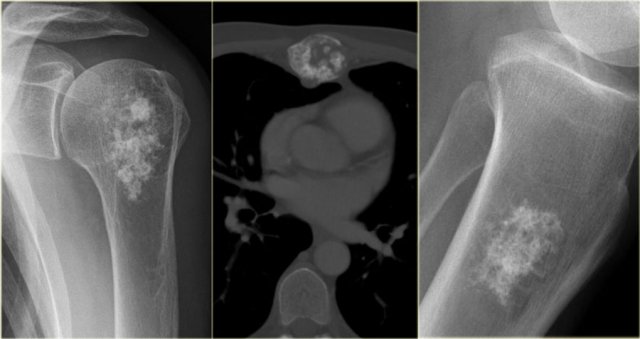
Chondrosarcoma (2)
The differential diagnosis on the plain radiographs in all these three cases is enchondroma.
Additional MR imaging and bone scintigraphy may be helpful to make the diagnosis of chondrosarcoma more or less likely.
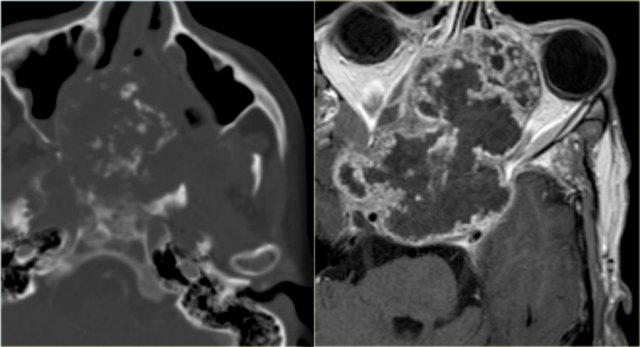
Chondrosarcoma (3)
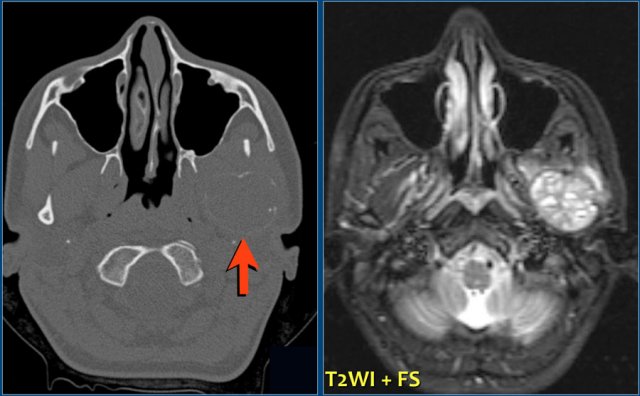
On the left a massive chondrosarcoma of the skull base with extension to the nasal and paranasal cavities and orbita.
CT demonstrates irregular calcifications produced by the tumor.
A T1-weighted image after Gd shows typical septal and nodular enhancement.
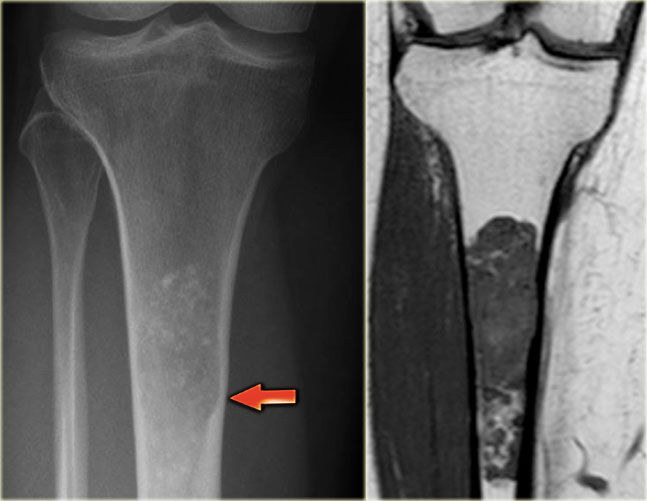
Chondrosarcoma (4)
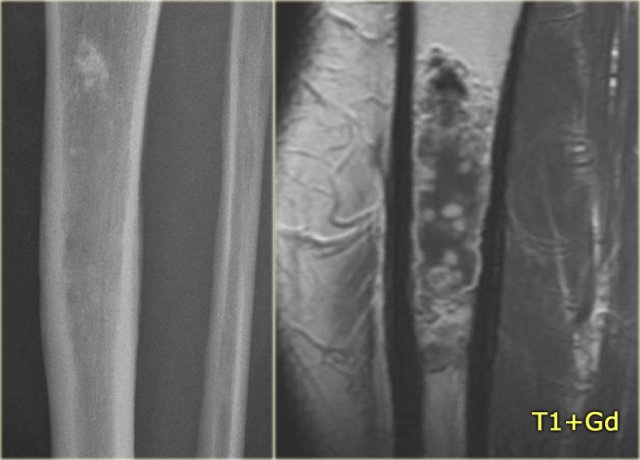
On the left a chondrosarcoma in the proximal tibia diaphysis.
The tumor is recognized by subtle calcifications in the proximal part.
The distal border is not well defined.
Notice endosteal scalloping at the medial side which is a hallmark of chondrosarcoma.
MR better defines the extension of the lesion.
MRI also demonstrates the endosteal scalloping.
Chondrosarcoma (5)
Partially calcified chondroid tumor in the proximal tibia.
Based on the imaging findings it is not possible to differentiate between an enchondroma or a low grade chonrosarcoma.
On the coronal T1-weighted MR the typical chondroid morphology is seen.
There is no evidence of endosteal scalloping.
Continue with bone scan and dynamic MR.
Bone scintigraphy of the same patient shows increased uptake in the lesion.
This increased uptake in a chondroid tumor is in favor of the diagnosis of a low grade (grade I) chondrosarcoma.
The fast dynamic contrast enhanced MR image with subtraction revealed early and progressive enhancement, which is also in favor of the diagnosis of a grade I chondrosarcoma.
Chondrosarcoma (6)
On the left a patient with a calcified lesion in the proximal diaphysis of the tibia.
On the sagittal T1-weighted CE image. The calcifications with low SI are present in the proximal part.
On the MR, the lesion is far more extensive than suspected on the plain radiograph at first glance.
On second inspection you will notice the subtle endoteal scalloping of the tumor on the radiogrph.
The large diameter and the scalloping favor the diagnosis of a chondrosarcoma.
Chondrosarcoma (7)
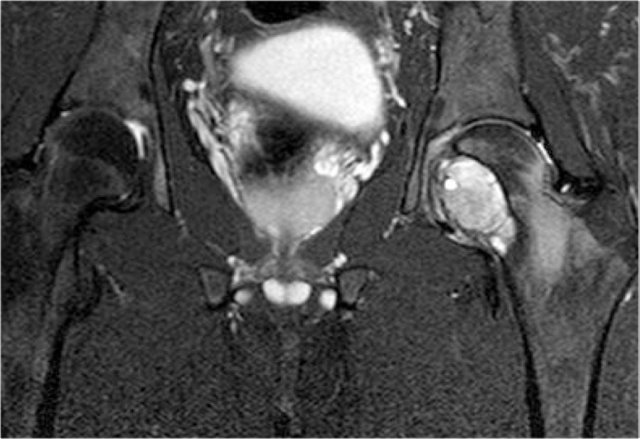
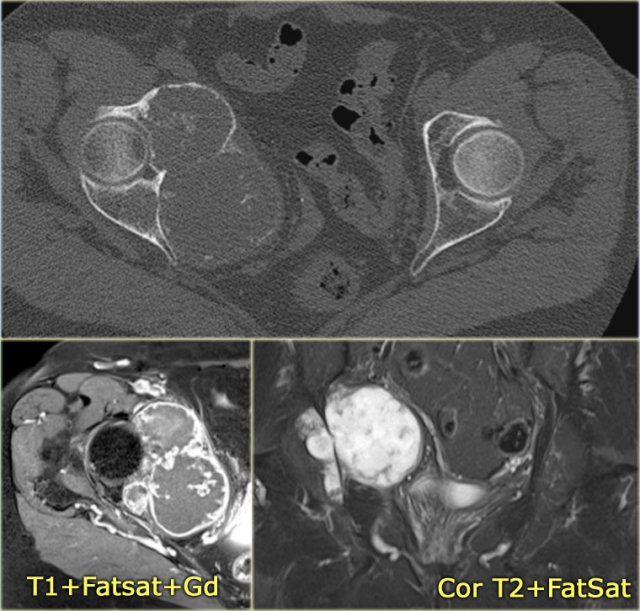
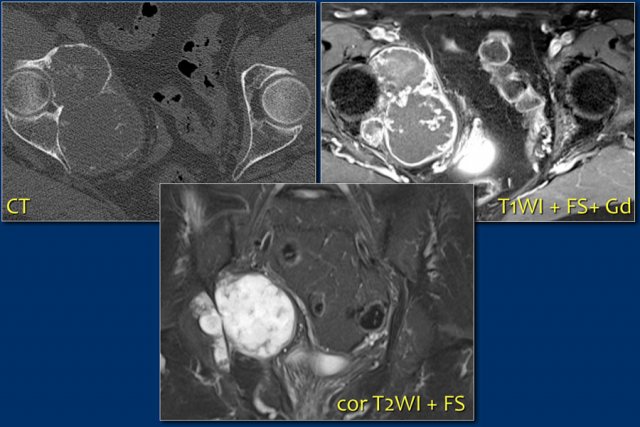
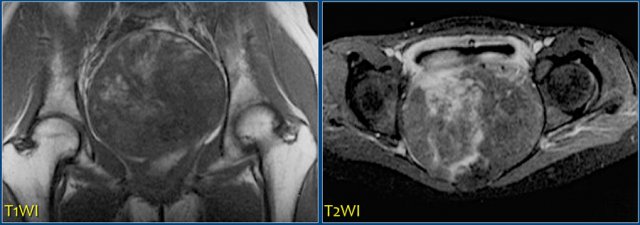
On the left a patient with a chondrosarcoma of the right acetabulum.
On the CT expansion and subtle calcifications are present.
On the coronal T2-weighted image the tumor is seen as a large lobulated mass with very high SI, which is typical for chondroid tumors.
The T1-weighted image after Gd shows typical peripheral nodular enhancement.
In the center there is no enhancement.
This is probably due to a large myxoid component. .
Chondrosarcoma arising from osteochondroma
Chondrosarcoma (8)
On the left a patient with a calcified mass arising from the proximal fibula.
The size of the lesion and the high uptake on the bone scan suggest that this is a chondrosarcoma.
Peripheral chondrosarcomas can arise from osteochondromas.
Measuring the cartilage cap will help in distinguishing benign osteochondromas from chondrosarcomas.
With 2 cm used as a cutoff for distinguishing benign osteochondromas from chondrosarcomas, the sensitivities and specificities were 100% and 98% for MR imaging and 100% and 95% for CT, respectively (3).
Chondrosarcoma (8) continued
On the left the axial T2 WI.
Notice that the tumor arises from an osteochondroma, which is shown in the center part of the image (arrow).
Chondrosarcoma (9)
On the left a patient with a broad-based osteochondroma with extension of the cortical bone into the stalk of the lesion.
Notice the lytic peripheral part with subtle calcifications.
This part corresponds to a zone of high SI on T2-WI with FS on the right.
This represents a thick cartilage cap.
This is an example of progression of an osteochondroma to a peripheral chondrosarcoma.
Chondrosarcoma (10)
On the left a typical broad-based osteochondroma arising from the proximal humerus.
The major part of the bony protrusion consists of fatty bone marrow.
There is a thin peripheral cartilage cap, i.e. no suspicion for malignant degeneration.
Chondrosarcoma (11)
On the radiograph there is only a vague sclerotic lesion.
The sagittal T2-WI FS much better demonstrates the presence and extension of a lesion with lobulated margins and a mixed pattern of high and low SI. Calcificatons contribute to the low SI within the tumor.
Diff. diagnosis: enchondroma or low-grade chondrosarcoma.
Biopsy: low grade chondrosarcoma.
low grade vs high grade
Chondrosarcoma (12)
Here a lesion consisting of rings-and-arcs calcifications in the proximal humerus.
The differential diagnosis is enchondroma or low grade chondrosarcoma.
The CT shows the calcifications with subtle endosteal thinning of the cortical bone (arrows).
Final diagnosis: low grade chondrosarcoma.
Chondrosarcoma (13)
Here a patient with a lesion in the proximal humerus with typical popcorn calcification.
The most likely diagnosis is enchondroma, however progression to a low-grade chondrosarcoma cannot be excluded based on the plain radiograph alone.
There is increased activity on the nuclear bone scan, which is more in favor of the diagnosis of a chondrosarcoma.
This proved to be a low-grade chondrosarcoma.
Chondrosarcoma (14)
Here a calcified lesion in the diaphysis of the tibia.
On the sagittal T1-weighted CE image, the calcifications (low SI) are present in the proximal part.
However, the lesion with septal-nodular enhancement pattern is far more extensive than suspected on the plain radiograph at first sight.
Notice subtle endoteal scallopping of the tumor (arrows).
This is, together with the diameter of the lesion in favor of the diagnosis chondrosarcoma.
Chondrosarcoma (15)
Here a lytic ill-defined lesion in the distal diaphysis of the femur in an old patient.
Notice the cortical thickening, but also endosteal scalloping (blue arrow).
The differential diagnosis should include metastasis and myeloma.
At closer look, there are also faint calcifications present (arrowhead).
The T1WI+Gd with fatsat demonstrates the presence of a solid enhancing part and perilesional edema.
In combination with the ill-defined appearance on the plain radiograph this suggest that this is a high grade chondrosarcoma.
Chondrosarcoma (16)
On the radiograph a lesion in the proximal humerus, which consists of rings-and-arcs calcifications in the proximal humerus.
Diff. diagnosis: enchondroma or low grade chondrosarcoma.
The CT shows the calcifications with endosteal thinning of the cortical bone (arrow).
On the axial T1WI CE FS typical peripheral septal enhancement seen in both benign and low-grade malignant chondroid tumors.
The endosteal scallopping and the size of the lesion are in favor of low-grade chondrosarcoma.
Biopsy: low grade chondrosarcoma.
CT shows expansile lesion of the right acetabulum with soft tissue extension.
Subtle calcifications are present indicating chondroid matrix.
CE-T1WI with fatsat shows typical peripheral nodular enhancement.
The central area without enhancement is probably due to a large myxoid component.
Diagnosis: Chondrosarcoma grade 2
Here a lobulated lytic lesion of the proximal humerus.
The presence of calcifications suggest a chondroid tumor.
The lytic parts with cortical involvement and expansion raise the suspicon of a high grade chondrosarcoma.
Diagnosis: high grade chondrosarcoma
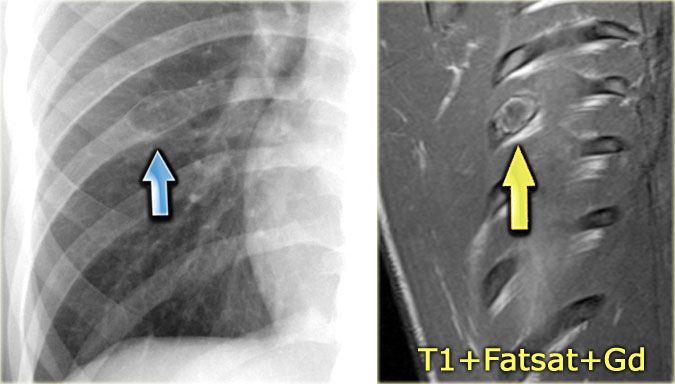
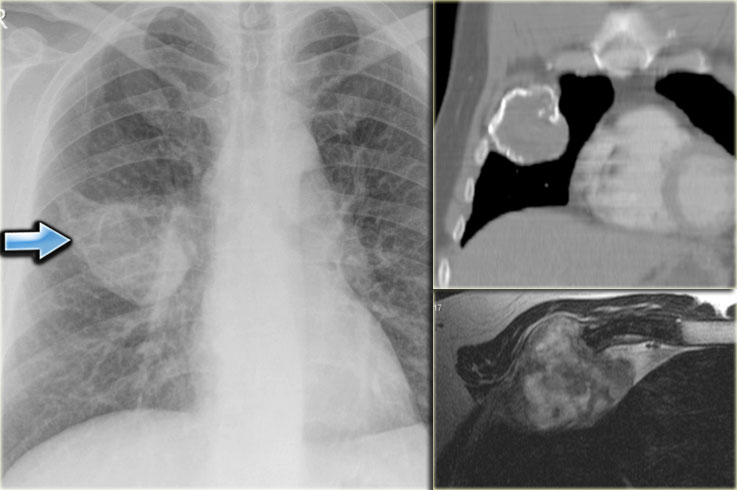
Chest X-ray shows non-specific soft tissue mass in the right lower lobe.
CT shows the mass extending from the posterior chest wall, with irregular calcifications, consistent with chondrosarcoma.
Diagnosis: high grade chondrosarcoma.
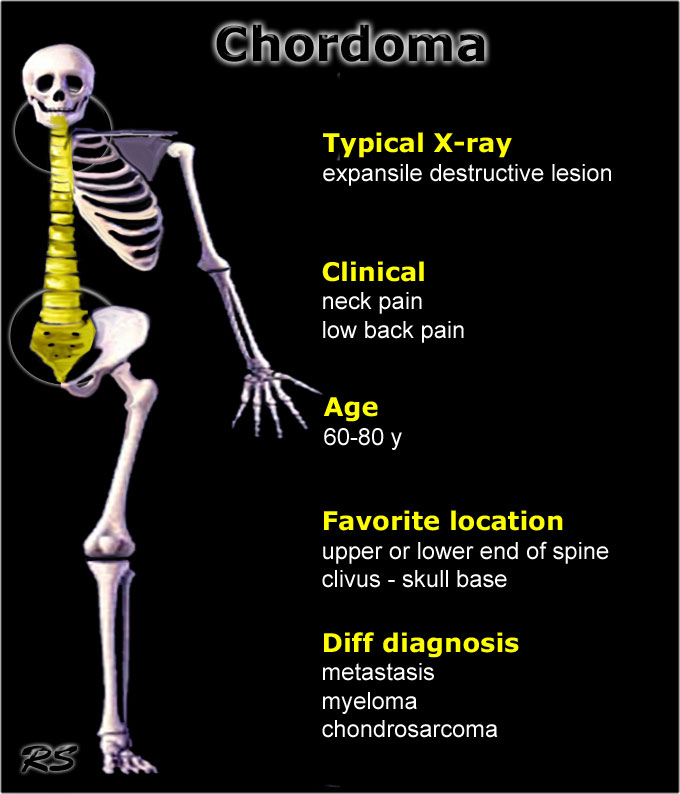
Chordoma
key facts:
- Rare low-grade malignant tumor usually in older patients.
- Typical presentation: expansile, destructive bone lesion that may be associated with a soft-tissue mass.
- On MRI T2-weighted images will show very high SI, more or less lobulated like a chondrosarcoma.
- On CT there may be calcifications also resembling chondrosarcoma.
- Preferential site of origin:
- Sacro-cocygeal
- Skull base / clivus
- May occur anywhere in the spine, most commonly in body and arch.
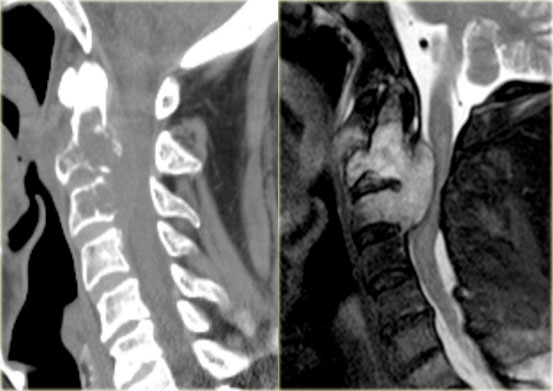
Here images of a patient with lytic lesions of the C2 and C3 vertebrae with cortical destruction posteriorly.
The differential diagnosis based on the CT-findings includes primarily metastases and myeloma.
The sagittal T2-weighted image with fat saturation demonstrates continuity between the abnormalities with soft tissue extension and compression of the myelum.
Now our differential should also include chordoma which has its origin in the neural axis as it arises from notochord remnants.
Chordoma (2)
Here another case of the cervical spine.
T2 weighted images with and without fat suppression.
Notice the involvement of more than one vertebral level, extensive soft tissue mass and very high signal intensity.
Chordoma (3)
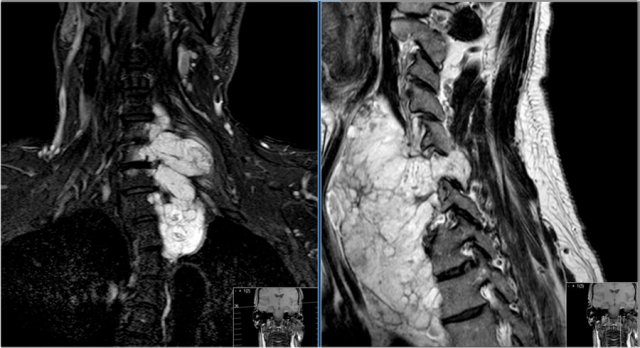
Here a large tumor in the sacral region which proved to be a chordoma.
Chordoma does not metastasize, but local recurrence is commmon.
Chordomas in the sacrococcygeal region may be cured by radical en bloc excision.
Chordomas in the base of the skull are usually inaccessible to surgery but may respond to radiation therapy.
Cortical desmoid
key facts:
- Also known as Tug lesion
- Tendinous insertion may 'tug' its attachment resulting in a surface mass, sometimes with reactive calcification.
- Underlying cortex may resorb ('tendonoperiostitis')
- Best known site: posteromedial corner distal femoral metaphysis
Degenerative cyst or Geode
key facts:
- Also known as geode
- Well-defined lytic lesion with or without visible connection to a joint surface and may extend quite far from the joint.
- Associated with osteoarthritis with degeneration of cartilage.
- MR: homogeneous high signal intensity on T2 WI due to the synovial fluid within the lesion. Usually no or limited edema.
- In later stages the cysts may contain fibrous tissue and have a lower SI.
- Differential diagnosis: intraosseous ganglion and less freqently a chondroid tumor.
Degenerative cyst (2)
Here a patient with arthrosis of the knee and a large well-defined osteolytic lesion in the epiphysis of the tibia.
In young patients the differential diagnosis would include chondroblastoma, intraosseous ganglion and giant cell tumor.
In this elderly patient with arthrosis this lesion is most probably a degenerative cyst.
Click here to compare this case to a chondroblastoma in the knee.
Degenerative cyst (3)
Here a well-deined osteolytic lesion with sclerotic margins in a patient with features of arthrosis.
Most likely diagnosis: degenerative cyst.
No change during follow up.
Degenerative cyst versus intraosseus ganglion
Here a well-defined lucent lesion in the epiphysis of the proximal tibia in young patient.
On the sagittal T2WI with FS, the lesion has high SI, but there is no extensive edema, which makes the diagnosis chondroblastoma less likely.
In an older patient with arthrosis the most likely diagnosis would be a degenerative cyst.
Degenerative cyst versus intraosseus ganglion (2)
Here another intraosseus ganglion.
The radiograph shows a well-defined osteolytic lesion in the proximal tibia epiphysis.
It is well-defined with high SI on T2WI with FS and there is no reactive edema.
Here another case.
Sagittal T2-WI with FS confirms subchondral location of cystic lesion with limited amount of edema.
The differential diagnosis is degenerative cyst, ganglion and chondroblastoma.
In a young patient this could be a chondroblastoma.
This patient was older and there is some arthrosis.
Diagnosis: degenerative cyst.
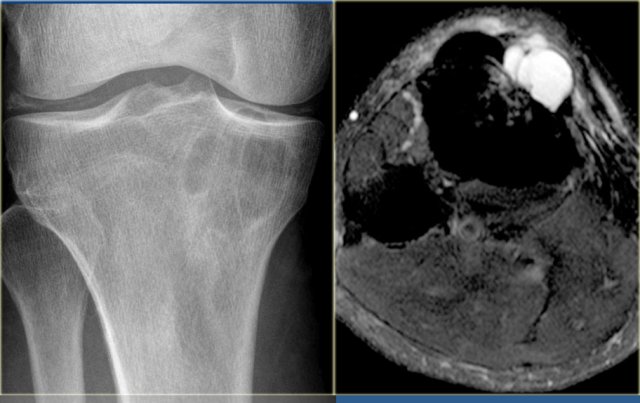
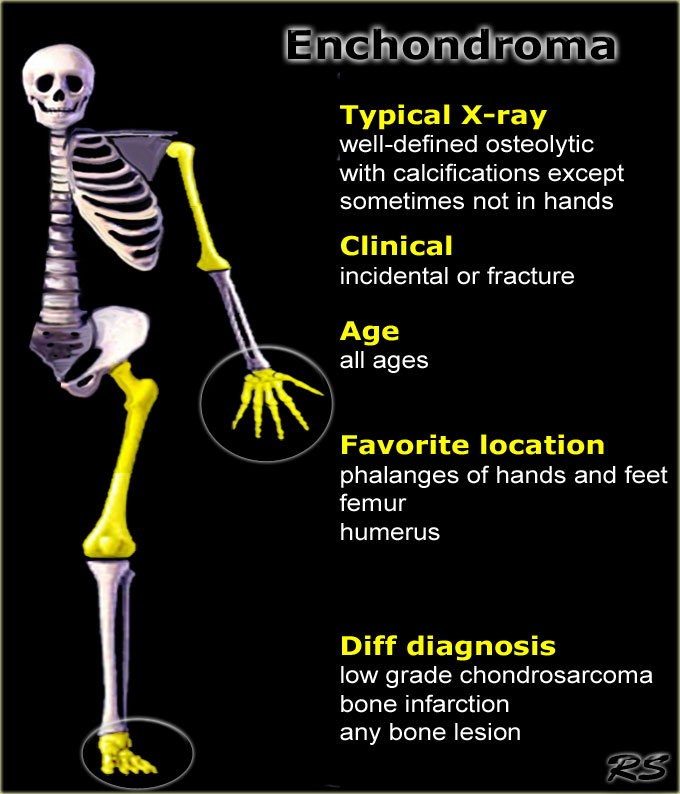
Enchondroma
key facts:
- Well-defined osteolytic cartilage-forming lesion, most commonly encounterered centrally in the phalanges of hands and feet.
- Other common locations: femur, humerus and metacarpals.
- Must have calcifications except in phalanges.
- May show mild expansion, but endosteal scalloping is not allowed for the diagnosis.
- Enchondromas may have an eccentric origin.
- Pain and periostitis is sign of malignancy, i.e.chondrosarcoma.
- On MR enchondromas show lobulated contours, very high signal intensity on T2-weighted images with fat suppression. The enhancement pattern is peripheral or septal-nodular. Dynamic enhancement should not be rapidly progressive unlike in chondrosarcoma.
- Uptake on bone scan usually low or absent
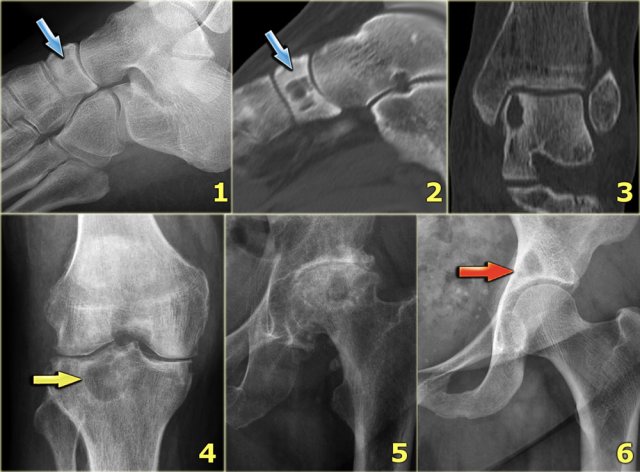
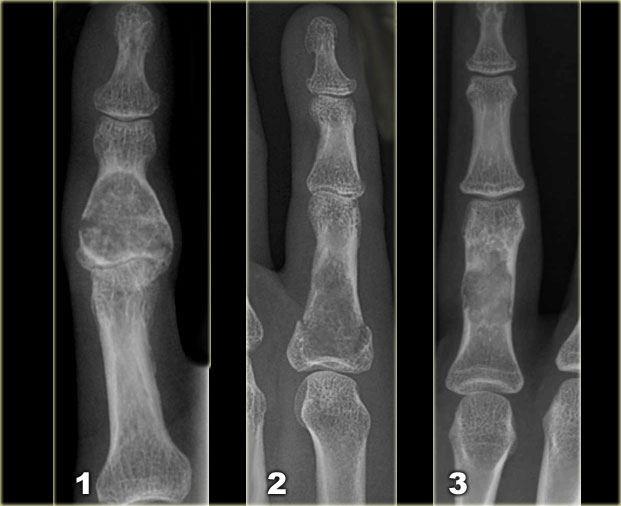
Left:
Well-defined lytic lesion with sclerotic margin and some expansion. There are fine calcifications.
This patient presented with a fracture, which is a common first presentation of an enchondroma.
Middle:
Well-defined lytic lesion without a sclerotic border also with a fracture.
Right:
Lesion with irregular cortical bone destruction.
Low-grade chondrosarcoma has to be included in the differential diagnosis, but is uncommon at this specific location.
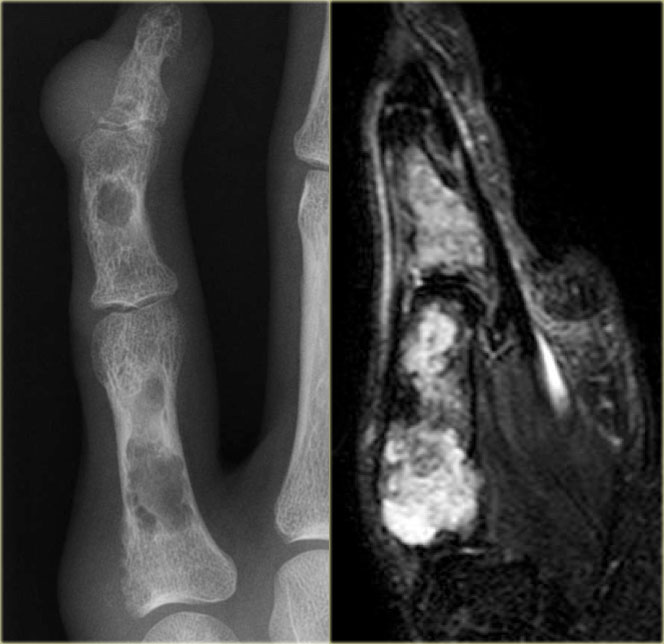
Enchondroma (2)
Lytic lesion within the phalanx with irregular cortical bone destruction and soft tissue extension should raise the suspicion of a chondrosarcoma.
A lytic lesion within a metacarpal bone with expansion with or without calcifications, with or without cortical bone destruction is not infrequently due to chondrosarcoma.
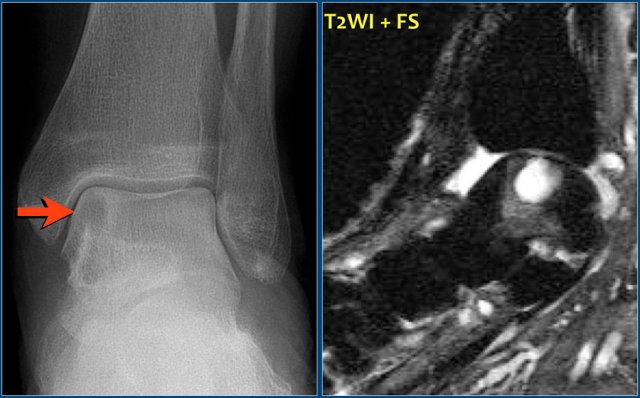
Enchondroma (3)
On the left another enchondroma.
here is a well-defined eccentric osteolytic lesion.
The location is typical for enchondroma.
Notice the lack of calcifications.
Enchondroma (4)
On the left a well-defined lytic lesion with some expansion of the rib.
The differential diagnosis based on the radiograph is: fibrous dysplasia, enchondroma, and less likely eosinophilic granuloma or hemangioma.
The coronal T1-WI after Gd with fatsat shows a lobulated lesion with peripheral enhancement consistent with the diagnosis of an enchondroma.
Multiple enchondromas
Multiple enchondromatosis is known as Ollier's disease.
Multiple enchondromas and hemangiomas of soft tissue are known as Maffucci's syndrome.
In both conditions there is a 30% risk of malignant transformation.
Enchondroma (5)
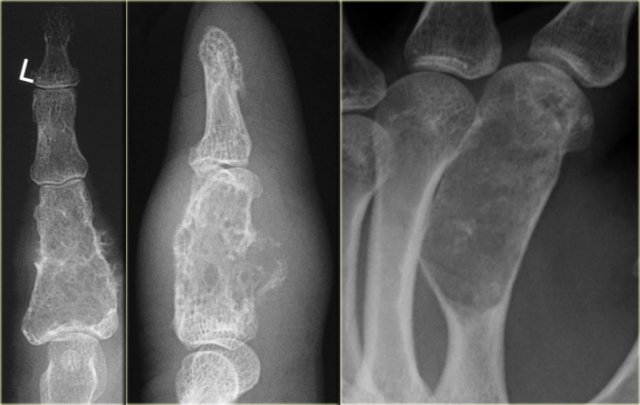
On the left a patient with multiple eccentric lytic lesions in the metacarpal bones and phalanges of the left hand.
On T2-WI with FS there is homogeneous high SI of the lesions.
On the left another patient with multiple well-defined lytic lesions in a central and eccentric localisation in the phalanges.
On the right the MR of a different patient with multiple lobulated chondroid lesions with high SI on T2-WI with fatsat.
Here a well-defined osteolytic lesion in the proximal ulna.
There is no mineralisaton.
Differential diagnosis: ABC, GCT, fibrous dysplasia.
Despite the lack of calcifications the final diagnosis was enchondroma.
Periosteal chondroma
Periosteal or juxtacortical chondroma arises at the surface of the bone.
Scalloping of cortical bone is possible, but there is no marrow involvement.
It may be difficult to differentiate from a periosteal chondrosarcoma.
The size of the lesion is the most important factor.
It may also be difficult to differentiate a periosteal chondroma from a periosteal osteosarcoma, however periosteal chondroma is much more common.
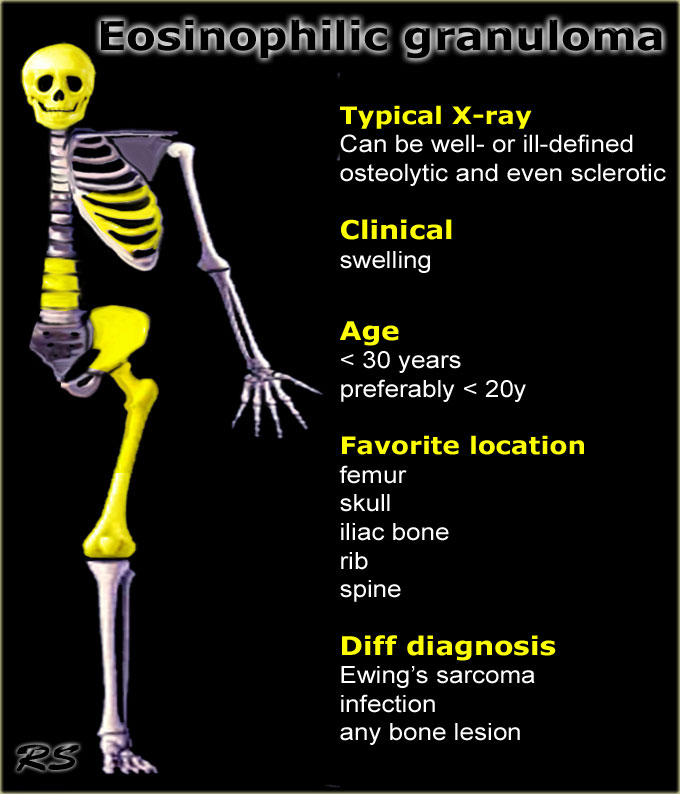
Eosinophilic granuloma
key facts:
- also called Langerhans cell histiocytosis.
- EG may present as a well-defined osteolytic lesion with a benign periosteal reaction or as an aggressive lesion with ill-defined margins and an aggressive type of periostitis mimicking Ewing sarcoma or osteomyelitis.
- MRI usually demonstrates a large amount of edema.
- Favorate location: skull and femur, but may occur anywhere.
- In the spine EG may present as a collapsed vertebra or vertebra plana.
- In the skull usually the outer and inner table are destroyed as seen on CT.
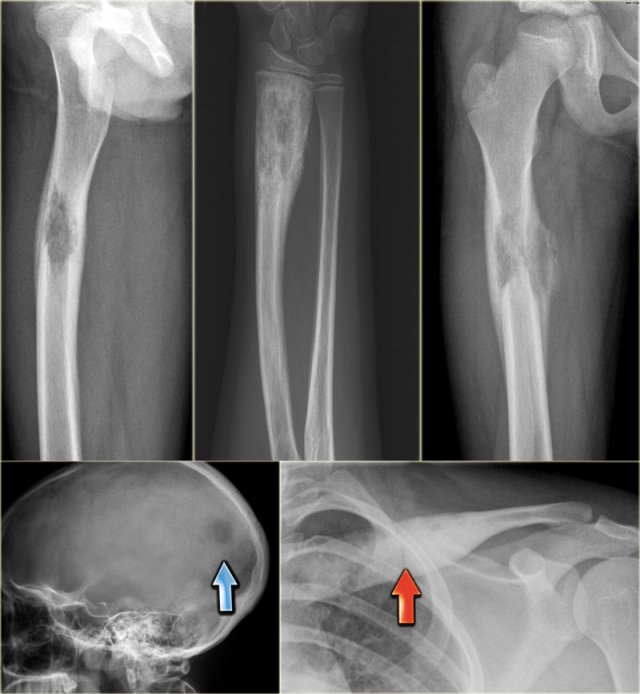
Eosinophilic granuloma (2)
Here some examples of EG demonstrating the various more or less aggressive presentations as ill-defined osteolytic lesions (blue arrow) and even as a less common sclerotic lesion (red arrow).
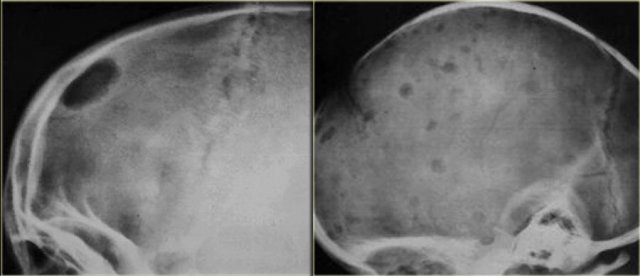
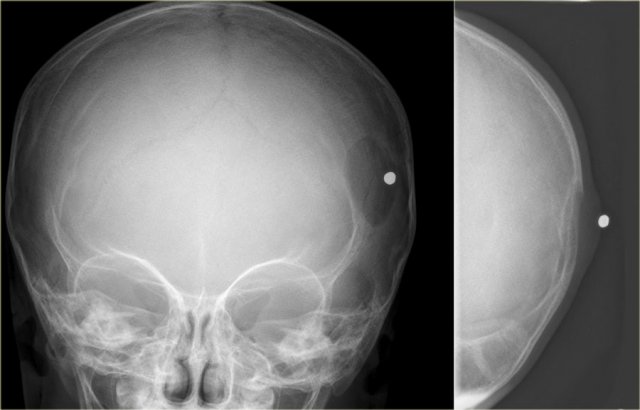
Eosinophilic granuloma (3)
On the left a well-defined osteolytic lesion.
A zone of sclerosis can be seen surrounding the lytic lesion.
Sometimes a so called button-sequestrum is found in the central part.
The case on the right shows multiple ill-defined lesions in the parietal and frontal bone.
Histology revealed eosiniphilic granuloma.
In a young child with multiple lytic lesions of the neurocranium EG is the most likely diagnosis.
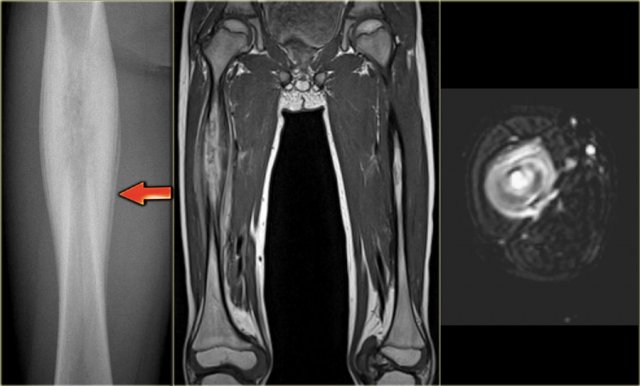
Eosinophilic granuloma (4)
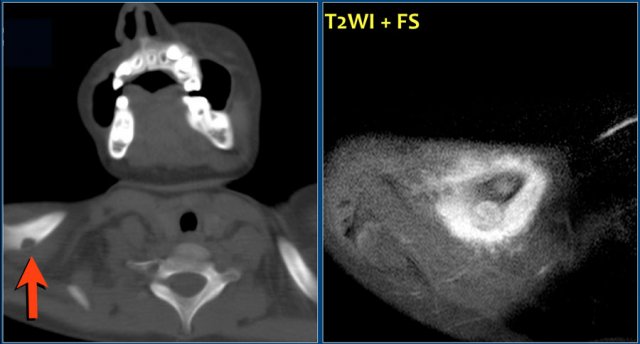
On the left an ill-defined lytic lesion in the shaft of the femur with a solid layered periosteal reaction.
Differential diagnosis: EG, osteomyelitis and Ewing sarcoma.
Ewing sarcoma usually shows an irregular and interrupted periosteal reaction, however cannot be excluded.
Axial T2-WI with FS shows high SI of the bone marrow and a soft tissue mass envelopping the bone.
Eosinophilic granuloma (5)
On the left another case of EG presenting as a well-defined osteolytic lesion in a young child.
Both inner and outer table of the skull are affected.
Eosinophilic granuloma (6)
Here again the sclerotic lesion in the clavicle that was shown earlier.
Notice on the T2-W MR-image the edema surrounding the clavicle.
Based on these imaging findings differentiation from a malignant bone tumor or infection is not possible.
Final diagnosis: eosinophilic granuloma.
Here a well-defined osteolytic lesion of the right clavicle.
Diff. diagnosis: osteomyelitis, eosinophilic granuloma.
T2-WI and T1-WI with Gd and Fs reveal the lesion with extensive osseous and soft tissue edema.
Final diagnosis: eosinophilic granuloma.
Here a more aggressive appearance of eosinophilic granuloma.
The radiograph shows a solid and interrupted periosteal reaction.
Sagittal T1-WI and axial T2-WI with FS also show aggressive appearance with bone marrow and soft tissue edema.
Differential diagnosis: Ewing sarcoma, osteomyelitis.
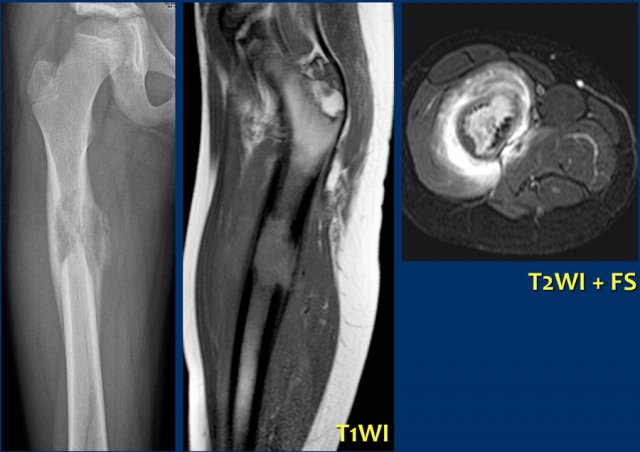
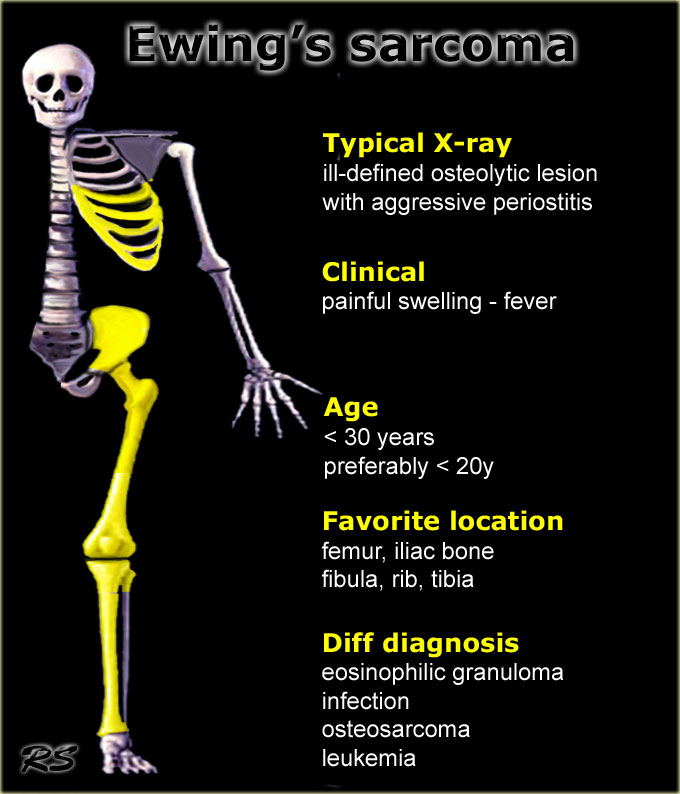
Ewing sarcoma
key facts:
- Typical presentation: ill-defined osteolytic lesion with a moth-eaten or permeative type of bone destruction, irregular cortical destruction and aggressive periostitis in the lower extremity of a child.
- Plain radiographs usually illustrate the malignant nature.
- Based on the age, the location and the radiographic appearance the diagnosis of Ewing sarcoma can be made in over 70% of cases.
- In long bones, the tumor is most commonly located centrally in the meta- or diaphysis
- MR imaging reveals the soft tissue extension.
- Treatment of Ewing sarcoma consists of neoadjuvant chemotherapy, followed by surgical resection and adjuvant chemotherapy.
The tumor also may respond to radiation therapy. - Differential diagnosis:
- Osteosarcoma is frequently included in the differential diagnosis, particularly when reactive sclerosis is present.
- Primary lymphoma of bone also presents with permeative pattern of destruction and often a large soft tissue mass. The mean age of presentation in these patients is usualy higher than in Ewing sarcoma.
- In some cases osteomyelitis or eosinophilic granuloma may mimic Ewing sarcoma.
Ewing sarcoma (2)
On the left some examples of a Ewing sarcoma.
- ill-defined lytic lesion of the femur diaphysis with a permeative pattern of destruction. Notice reactive sclerosis, irregular periosteal reaction and soft tissue mass.DD: ostesarcoma, lymphoma
- Ewing sarcoma of the chest wall presenting with a large soft tissue mass. Many Ewing sarcomas are accompanied with a large soft tissue mass.
- Ewing sarcoma of the proximal femur: almost normal radiographic appearance! See next images.
- ill-defined lytic lesion in the distal humerus. Layered periosteal reaction laterally and irregular periosteal reaction with interruption on the antero-medial side.
- Ewing sarcoma of the iliac bone. Hardly visible on plain radiograph. Continue with the discussion of this case.
Ewing sarcoma (3)
On the left images of a large lytic tumor arising from the right iliac bone.
On the plain film it is very hard to appreciate the lesion because of the permeative destruction pattern.
Scintigraphy shows extensive uptake within the iliac bone.
Sometimes, a cold spot is found in Ewing sarcoma.
MR reveals the intra- and extraosseous tumor extension.
Ewing sarcoma (4)
This case was also shown above.
There is a Ewing sarcoma with permeative growth through the haversian channels accompanied by a large soft tissue mass as seen on the MR.
The radiograph does not show any sign of cortical destruction.
In fact it looks normal, although someone might argue that the cortex is somewhat ill-defined and that there maybe is some periosteal reaction.
Ewing sarcoma (5)
On the left a mixed lytic-sclerotic lesion within the diaphysis of the femur.
There is a permeative pattern of destruction with a spiculated periosteal reaction and soft-tissue extension.
The final diagnosis was a Ewing sarcoma.
Based on these images osteosarcoma should be in the differential.
Ewing sarcoma (5) continued
The fat suppressed T1-weighted enhanced MR image demonstrates the permeative cortical destruction and enhancing soft tissue mass.
Ewing sarcoma (6)
On the left a similar case.
On the radiograph there is a subtle interruped periosteal reaction of the humeral diaphysis with otherwise normal appearing cortical bone.
Axial T2-weighted MR image with FS shows large accompanying soft tissue mass with almost normal appearing cortical bone.
This suggests a malignant small-cell tumor like Ewing sarcoma or lymphoma.
Final diagnosis: Ewing sarcoma
Ewing sarcoma (7)
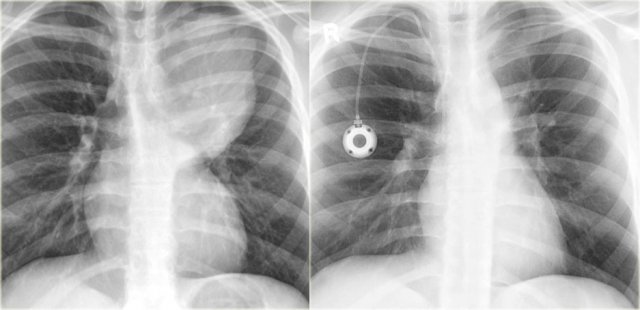
Treatment for Ewing's sarcoma includes surgery, radiation and chemotherapy.
On the left a Ewing sarcoma, presenting as a large pleural soft tissue mass (same case as above).
On the right, the soft tissue mass has completely resolved after neoadjuvant chemotherapy.
Here a young patient with an ill-defined lytic lesion of the distal humerus.
There is irregular cortical destruction and partially interrupted periosteal reaction.
Final diagnosis: Ewing's sarcoma.
Diff. diagnosis: osteosarcoma.
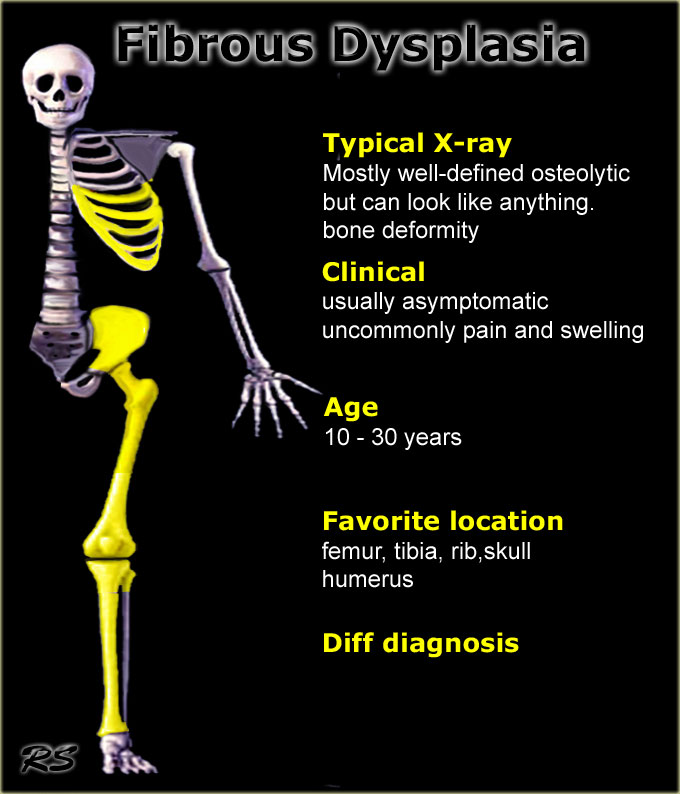
Fibrous dysplasia
key facts:
- In general FD is lytic and well-defined, but can look like almost anything (1).
- Various presentation: bone deformity, discrete lucency, patchy, sclerotic, expansile and polyostotic. The deformity can be very prominent.
- FD may also contain cystic parts, calcifications and ossifications.
- Mostly found in children and young adults, but sometimes as coincidental finding at older ages
- Preferential sites: femur, tibia, rib, neurocranium and humerus. Located in diaphysis or metadiaphysis.
- Usually FD presents as a solitary lesion, but in about 10% it is polyostotic. In polyostotic disease femur and tibia are often simultaneously involved.
-
Differential diagnosis:
- In young patients with location in proximal humerus or femur: solitary bone cyst or aneurysmal bone cyst.
- In eccentric locations: NOF or adamantinoma (tibia).
- When calcifications are present: chondroid lesion (enchondroma).
Fibrous dysplasia (2)
Here a polyostotic manifestation of FD.
There are multiple lesions, which are partially lytic and partially mixed lytic/sclerotic.
The radiographic appearance is determined by the extent of dysplastic bone and the amount of bone produced and the degree of calcifications and ossifications.
Fibrous dysplasia (3)
On the left images of a patient with fibrous dysplasia of the rib with remarkable expansion.
Fibrous dysplasia can cause huge deformaties of bones.
CT shows expansion and a peripheral zone of sclerosis.
No internal matrix formation.
Axial T2-weighted image shows mixed pattern of low and high SI within the expansile lesion.
Fibrous dysplasia (3)
Fibrous dysplasia can be monostotic or polyostotic.
In this patient there are identical lesions within the proximal femur and left acetabulum.
There is a groundglass appearance with focal areas of calcifications.
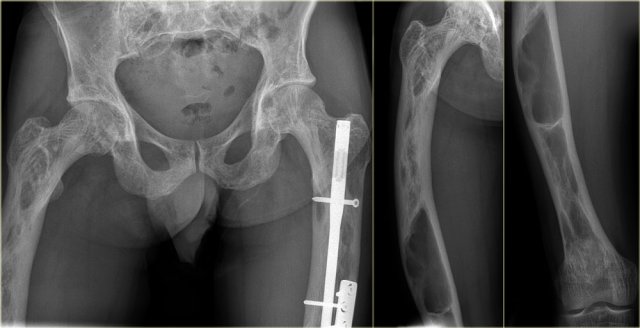
Fibrous dysplasia (4)
The appearance of FD may vary from entirely lytic (probably due to cystic degeneration) to entirely sclerotic.
On the left images of a patient with polyostotic fibrous dysplasia, with lucent lesions in the proximal and mid-diaphyseal femur, and lesion with groundglass density and calcifications in the fibula.
Fibrous dysplasia (5)
Bone scintigram in 40-year old patient in the tibia shaft.
Plain radiograph shows well-defined lesion with ground glass density and sclerotic margin.
Features are not characteristic for adamantinoma, histology revealed fibrous dysplasia.
Fibrous dysplasia (6)
On the left images of a patient with polyostotic FD.
On the far left a well-defined lytic lesion with groundglass appearance in the proximal femur diaphysis, consistent with fibrous dysplasia.
T2-weighted MR image with FS reveals cytic degeneration of the fibrous dysplasia, which is a common finding.
This patient has a second lesion in the shaft of the humerus witha pathologic fracture.
Fibrous dysplasia (7)
The radiograph on the left shows a mixed lytic-sclerotic lesion of the left iliac bone.
Axial CT image on the right shows some broadening of the iliac bone with a ground glass appearance and no cortical destruction.
Here a patient with polyostotic fibrous dysplasia.
Notice multifocal areas of high uptake on bone scintigraphy: acetabulum, femur diaphysis, tibia and ankle.
The radiographs show ground glass abnormalities with or without calcifications.
Ganglion
Here a lucent lesion in the proximal tibia epiphysis.
It is well-defined with high SI on T2 WI with FS without reactive edema.
Diagnosis: intraosseus ganglion.
Diff. diagnosis: degenerative cyst.
Here a well-defined lucent lesion in the epiphysis of the proximal tibia in a young patient.
The sagittal T2-WI with FS demonstrates that the lesion has high SI, but there is no extensive edema, which makes a chondroblastoma less likely.
Diagnosis: intraosseus ganglion.
Diff. diagnosis: degenerative cyst, chondroblastoma.
Giant cell granuloma
The mandible is a predilection site of giant cell granuloma.
Here a well-defined lytic lesion in the left mandible.
Final diagnosis: giant cell granuloma of bone.
Diff diagnosis: ameloblastoma.
Here an expansile lytic lesion with thin peripheral bone shell originating from the left mandibular head.
The axial T2-weighted image with FS shows multiple cavities with fluid levels consistent with secondary ABC.
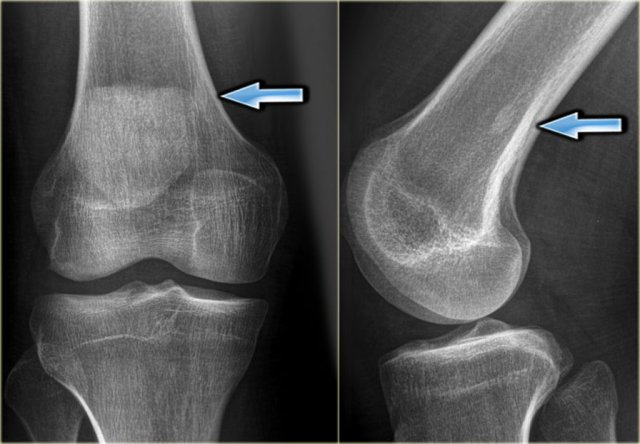
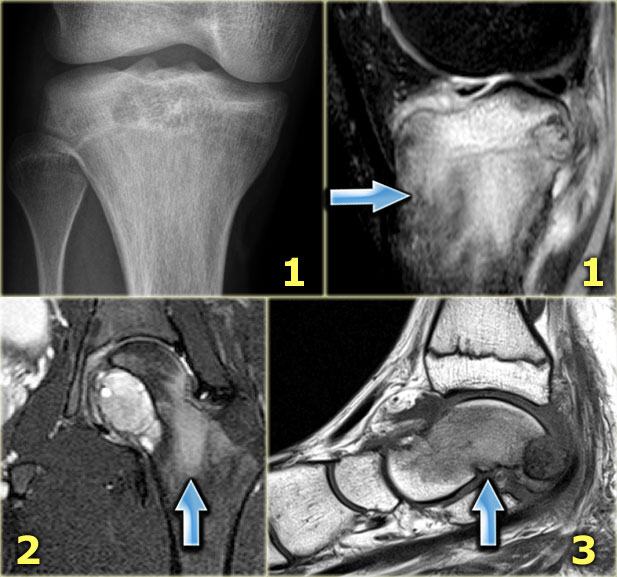
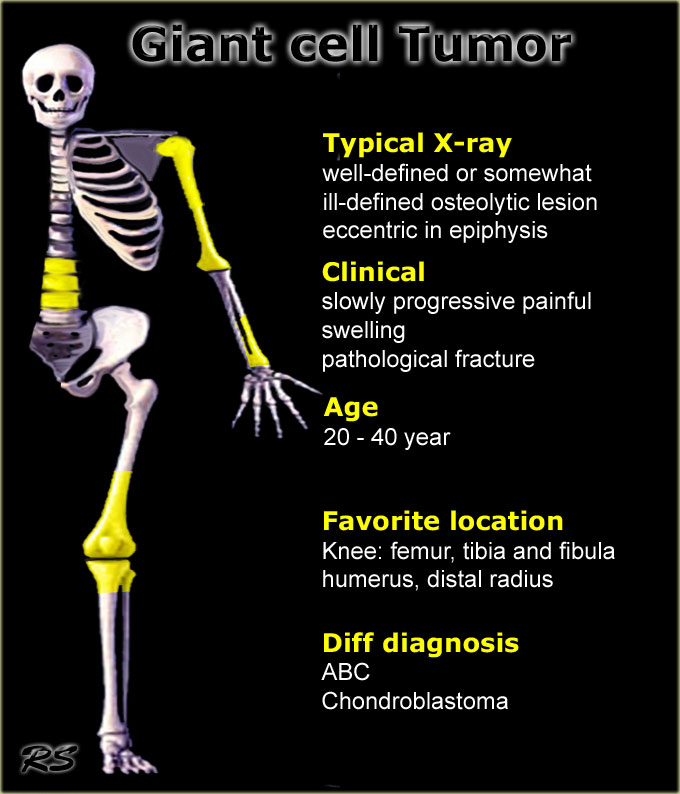
Giant cell tumor
key facts:
- Presents as an eccentric lytic lesion with a geographic pattern of bone destruction, but can also have a more aggressive appearance with ill-defined borders.
- By far most giant cell tumors are seen around the knee. GCT is located in the epiphysis with or without extension to metaphysis and frequently abuts the articular surface.
- Most common bone tumor in adults aged 25 - 40 y.
-
Differential diagnosis:
- ABC may have the same radiographic features but is found in a younger age group.
- Chondroblastoma is also located in the epiphysis, but is seen exclusively in the epiphysis without extention to the metaphysis and is seen in a younger age group.
- Metastases, especially in older patients.
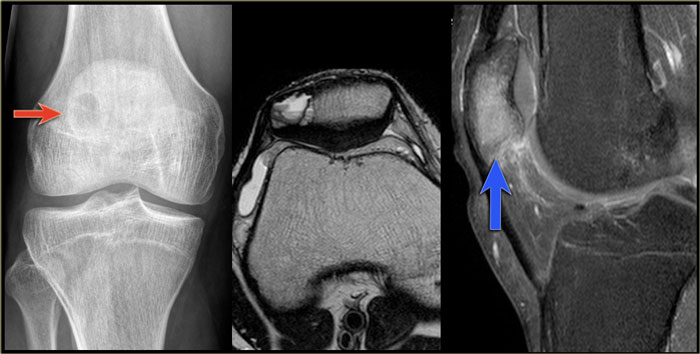
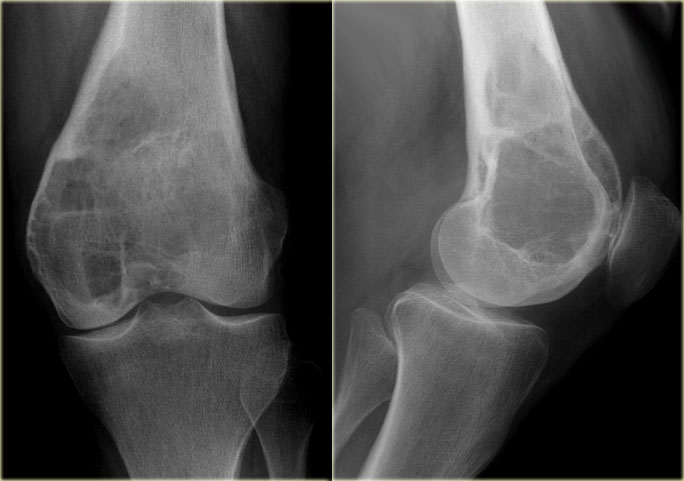
Giant cell tumor (2)
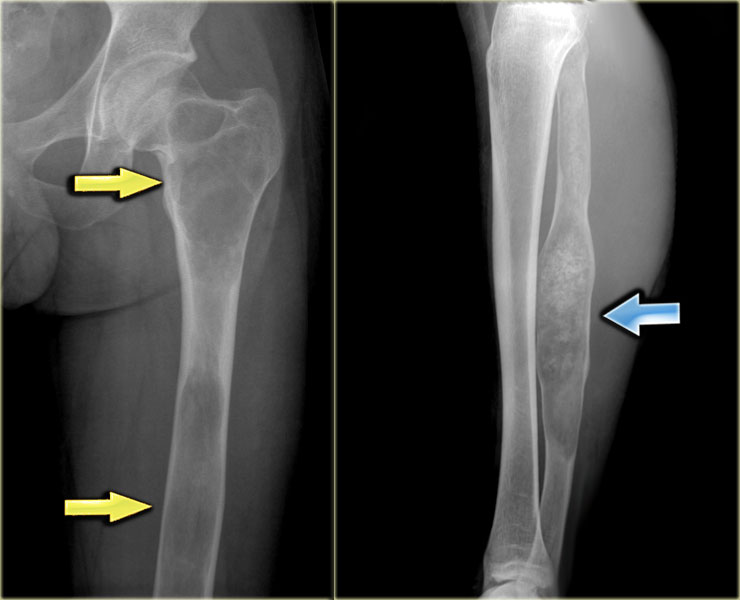
On the left a giant cell tumor presenting as an eccentric lytic lesion in the medial epi- and metaphysis of the distal femur.
There is a small transitional zone resulting in well-defined borders.
Continue with the MR-images.
Giant cell tumor (2) continued
MR-images of the same patient.
Sagittal T1-weighted TSE images before and after Gd.
The tumor extends to the subchondral bone plate with endosteal cortical involvement.
There is inhomogeneous enhancement.
On T2-weighted image, the tumor has a remarkable low SI, which is commonly seen in GCT.
There is surrounding edema with high SI.
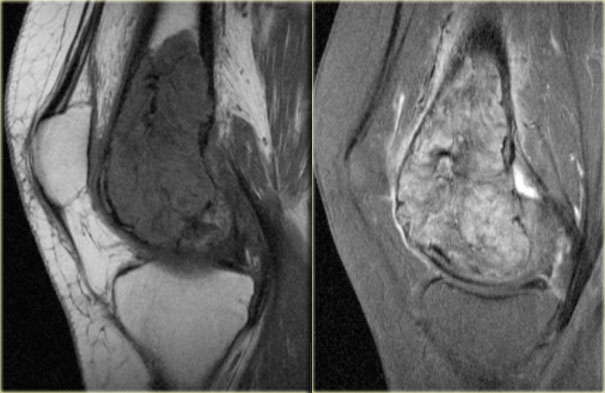
Giant cell tumor (3)
On the left a typical giant cell tumor of the distal radius.
Notice the aggressive appearance with ill-defined borders, extension to the soft tissues and destruction of subchondral bone plate.
The localisation in the epiphysis and metaphysis is in favor of diagnosis of GCT.
On the right a coronal T1-weighted CE image.
There is diffuse heterogeneous enhancement, and extension to the radiocarpal joint and surrounding edema in bone and soft tissues.
Giant cell tumor (3) continued
On the left images of the same patient during follow-up after curettage and cement-placement.
There is soft tissue swelling with osteolysis of the bone adjacent to the cement.
This indicates recurrent or residual disease.
On the left another GCT presenting as an ill-defined expansile lesion with a very subtle peripheral bone shell arising from the spinous processes C5 and C6.
The sagittal T2-weighted MR-image with FS demonstrates multiple small cavities within the tumor, due to secondary ABC.
Giant cell tumor (4)
On the left a large lytic lesion originating from the sacral bone.
CT prior to biopsy shows a lesion, that is entirely lytic without minerelization.
Differential diagnosis in a patient of 50 years of age: metastasis, plasmacytoma, chordoma, chondrosarcoma (no calcifications present), giant cell tumor.
Giant cell tumor (4) continued
On the coronal T1WI after Gd , the tumor shows diffuse enhancement of the intra- and extraosseous component, with the exception of multiple cystic cavities, which have a low SI on T1 and high SI on T2.
These cysts are not uncommonly encountered in giant cell tumor.
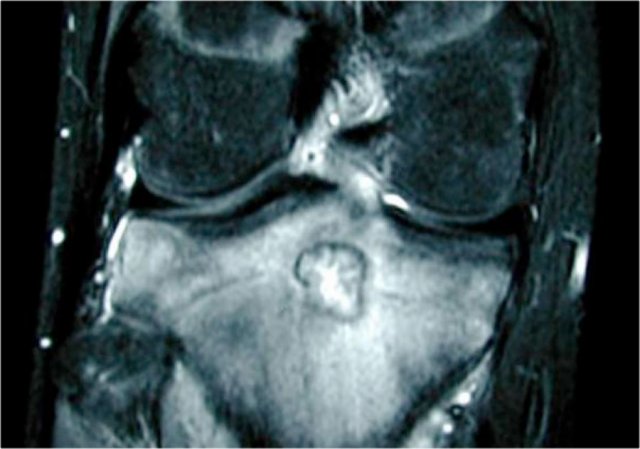
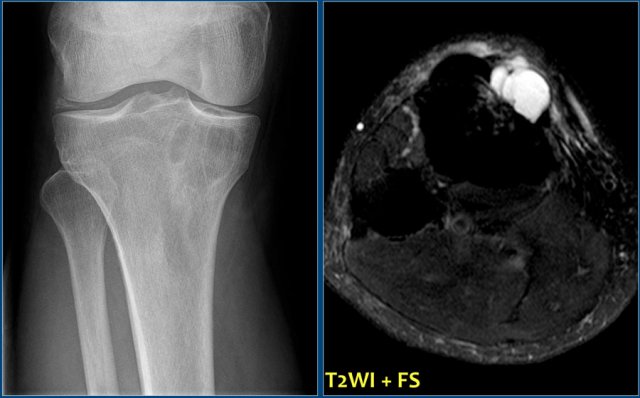
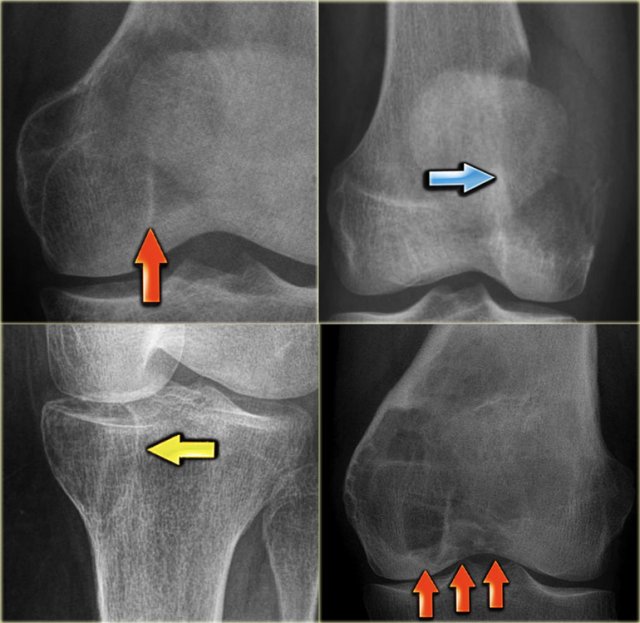
On the left more examples of GCT around the knee.
Notice that most of these lesions are well-defined and located in the epiphysis and extend into the metaphysis.
Some extend onto the articular surface (yellow arrow and small red arrows).
The lesion on the upper right has an ill-defined border with a broad zone of transition (blue arrow).
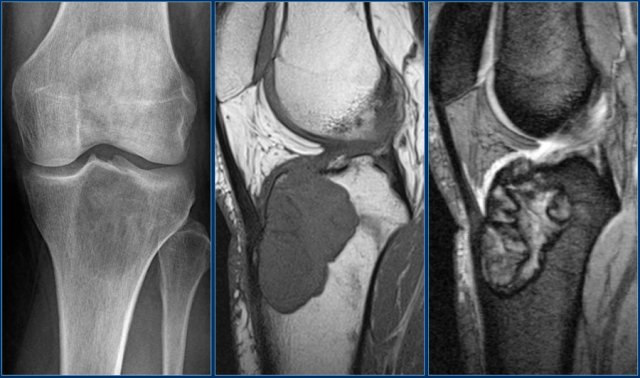
Here another typical giant cell tumor presenting as an osteolytic lesion in the epi- and metaphysis of the proximal tibia.
Non-specific intermediate signal intensity on T1WI and mixed high and low SI on T2WI with FS.
The low signal on T2WI is usually due to hemosiderin within the GCT.
Here a giant cell tumor in the fibula.
There is a partially ill-defined expansile lesion of the proximal epi- and metaphysis of the fibula in an adult.
A thin peripheral bone shell suggests benign lesion, although malignancy (e.g. metastasis) cannot be excluded.
In younger patients ABC should also be considered.
Here an ill-defined expansile lesion with very subtle peripheral bone shell arising from the spinous processes C5 and 6.
On the sagittal T2WI with FS multiple small cavities are seen within the tumor, due to secondary ABC.