MRI of the Paranasal Sinuses
Laurie Loevner and Jennifer Bradshaw
Radiology department of the University of Pennsylvania, USA and the radiology department the Medical Centre Alkmaar, the Netherlands
Publicationdate
This article is based on a presentation given by Laurie Loevner and adapted for the Radiology Assistant by Jennifer Bradshaw.
This review focusses on the complimentary roles that CT and MR play in the assessment of:
- Complicated sino-nasal infections
- Sino-nasal and skull base lesions
- Fibro-osseous lesions
Role of CT and MRI
CT is of value for determining anatomic landmarks and variants.
This information is of vital importance to the ENT-surgeon.
In addition, we need it to identify erosive processes and acquired developmental deficiencies of the bone.
CT is also excellent for determining whether there is intraorbital extension of sino-nasal disease
in the ventral 2/3 of the orbit.
When pathology approaches the orbital apex, an MRI study is necessary to assess spread to the cavernous sinus and intracranial compartment.
CT is performed without contrast medium.
If additional imaging is necessary, orbital MRI is the next step.
The real value of unenhanced CT is the following: if you see an opacified sinus with hyperdense contents, it is usually a sign of benign disease.
Tumor is not hyper-dense.
The hyperdensity is due to one or a combination of the following:
- inspissated secretions
- fungus
- blood
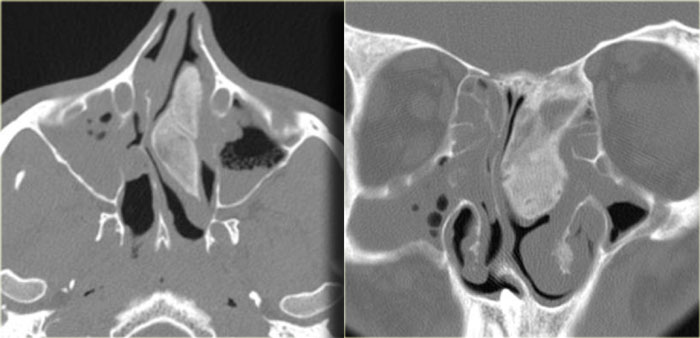
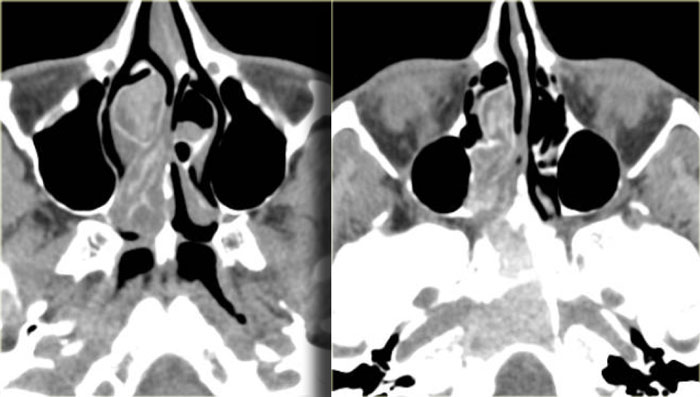
On the left you see a case that was initially interpreted as a tumor.
There is hyperdense material in the posterior right ethmoid, the bilateral spheno-ethmoidal recesses, the sphenoid sinus and there is involvement of the clivus.
The hyperdensity is a good prognostic sign, indicating a benign process.
This is an example of allergic fungal sinusitis.
Usually it is more anteriorly located.
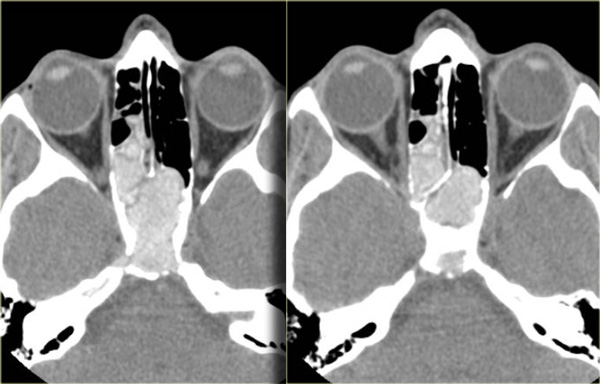
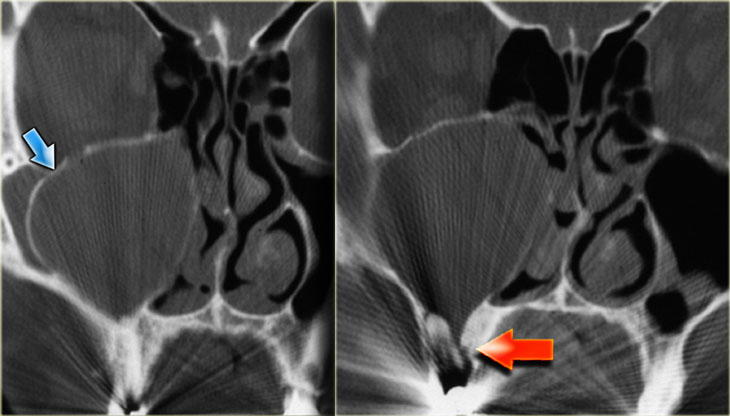
On the left another, more characteristic, example of allergic fungal sinusitis.
There is bilateral opacification of the nasal cavities, usually a sign of an inflammatory process or polyps.
Note the concentric lamellated appearance of alternating hyper- and hypodensity in the maxillary sinusses.
The hyperdensity is due to inspissated secretions and fungal elements.
The hypodensity reflects cysts, mucosal disease, and granulation tissue.
In the ethmoidal region some of the hyper-density reflects periostitis and neo-osteogenesis along the septae.
Signal characteristics of secretions
MRI is extremely helpful in complicated sinonasal disease.
MRI can discern secretions and mucosa from masses.
When you understand the signal characteristics, you are readily able to distinguish soft tissues masses from inspissated secretions.
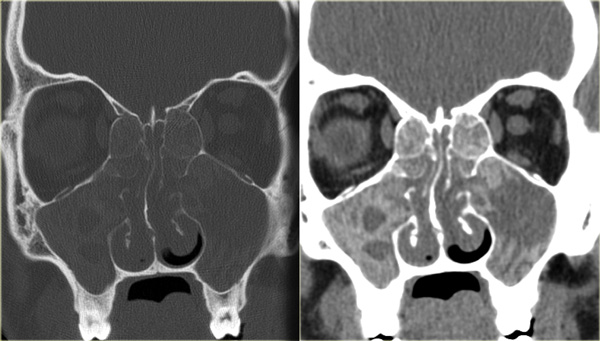
The signal intensity of secretions can vary and mainly depends on the ratio of water to protein and the viscosity.
Different protein contents result in different signal intensities on T1 and T2W-images (figure).
Fungus usually has a high protein content of more than 28% and can mimic an aerated sinus because it is low on T1- and T2WI. You need CT to make the distinction!
MRI is also useful for determining invasion of the skull base.
Involvement of the skull base is seen as replacement of the high signal of the fatty marrow on T1WI by hypointense signal of the tumor.
Also look for foraminal extension, whether by perineural spread or direct invasion of the tumor.
MRI is also the study of choice for detecting intracranial extension of sinonasal disease.
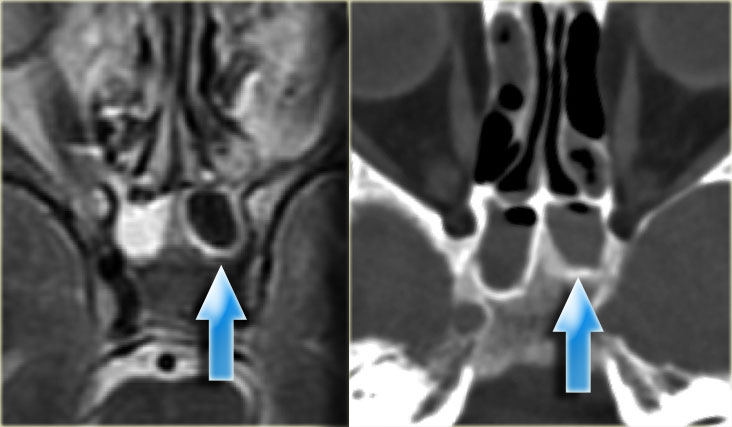
Pseudo-pneumatized sinus
Role of CT and MR (2)
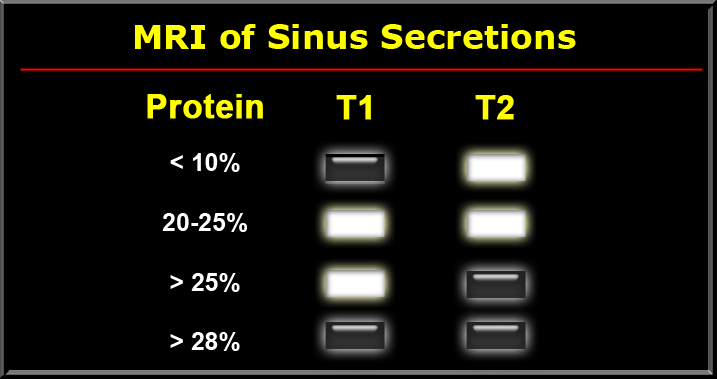
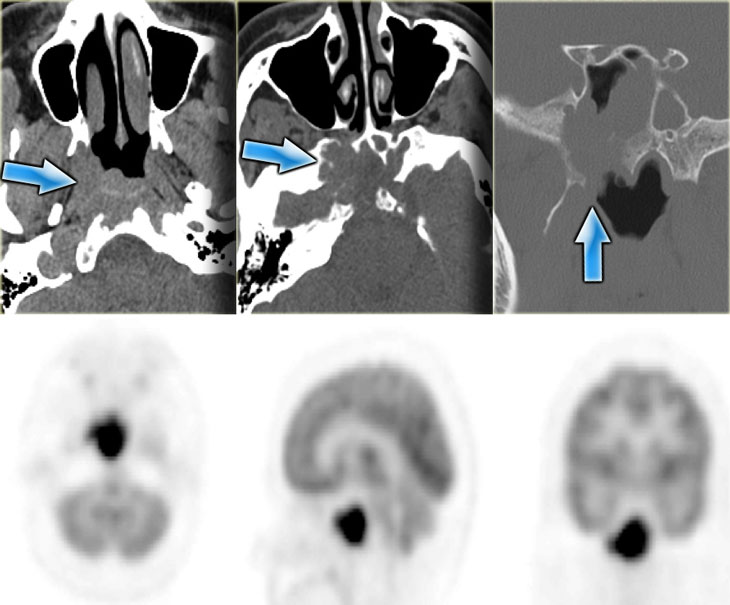
On the left a T2W-image in an immuno-compromised patient with fever.
Initially a MRI was performed to rule out sinusitis.
Notice the low signal intensity of the left sphenoid sinus, which also had a low signal intensity on the T1W-image (not shown).
Continue with the CT.
The CT clearly shows the opacified sinus, which is slightly hyperdense.
The signal characteristics on MRI and the attentuation on CT are a result of the high protein content of fungus.
This is a good example of the pitfall of the 'pseudo-pneumatized sinus' .
This is an example of an Actinomyes infection.
So, when invasive fungal infection is suspected, start with a CT, then move on to MRI to rule out spread to the eye, cavernous sinus and intracranial compartment!
Enhancement
In general bright signal on T2 is a sign of benign disease, since fluid and mucosal disease usually have a high water content.
Secretions do not have solid enhancement.
If you have an enhancing mass, you must rule out tumor.
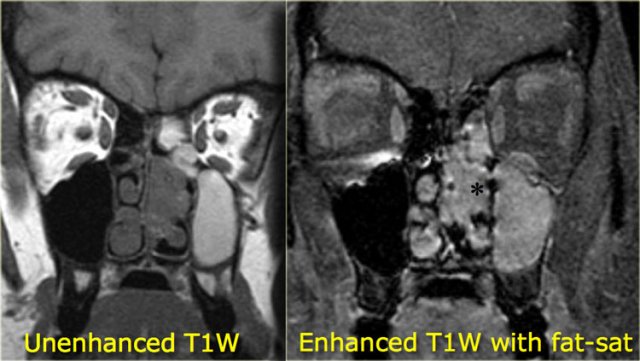
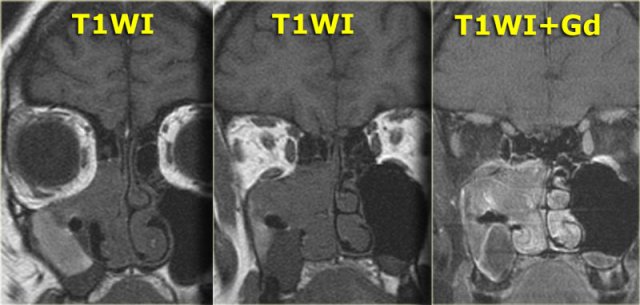
On the left an example of infectious sinonasal disease.
On the pre-contrast scan you see relatively high signal content of the maxillary sinusses due to proteineous material.
After the administration of i.v. contrast there is only enhancement of the circumferential mucosa and no solid enhancement.
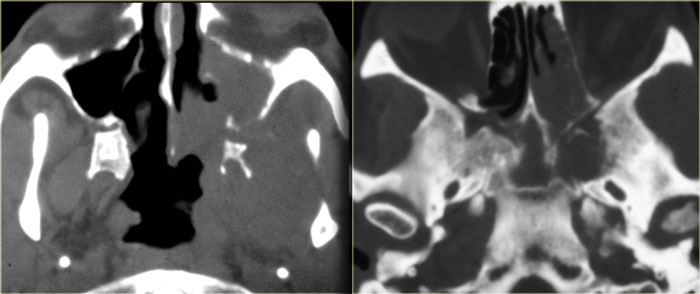
Role of CT and MR (3)
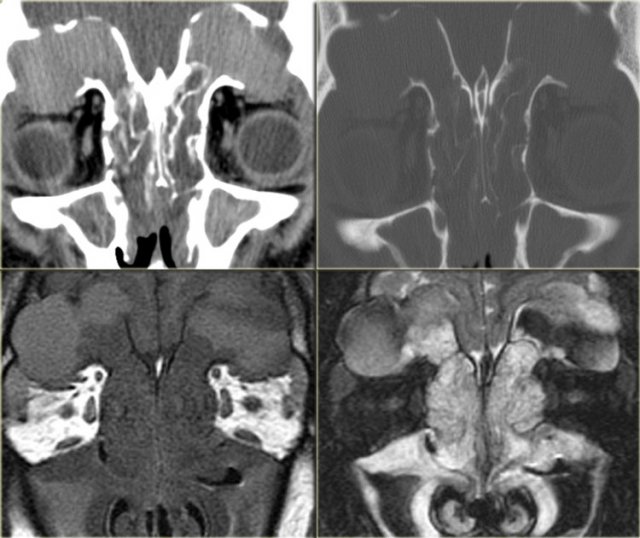
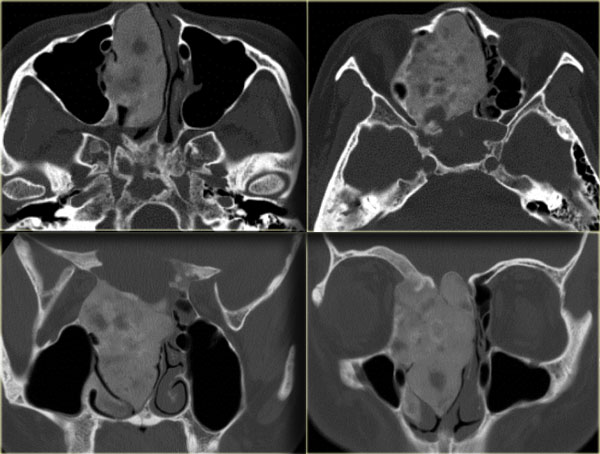
In complicated cases both CT and MR are needed to demonstrate the extention of the disease.
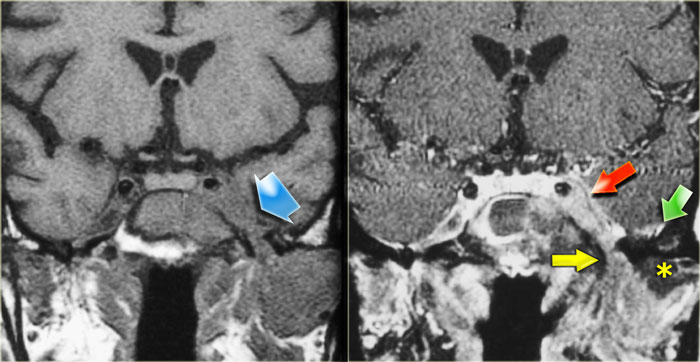
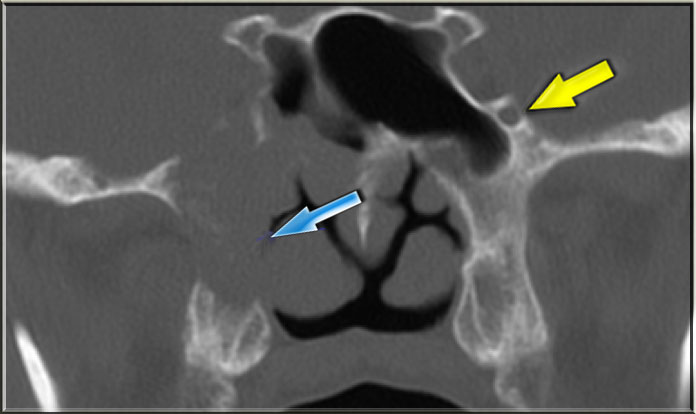
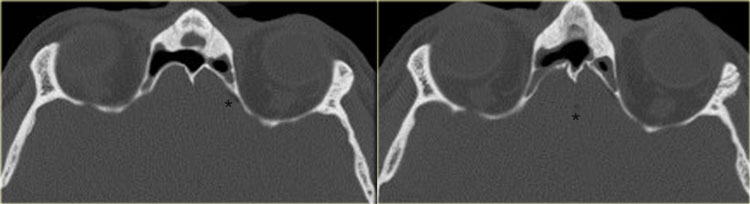
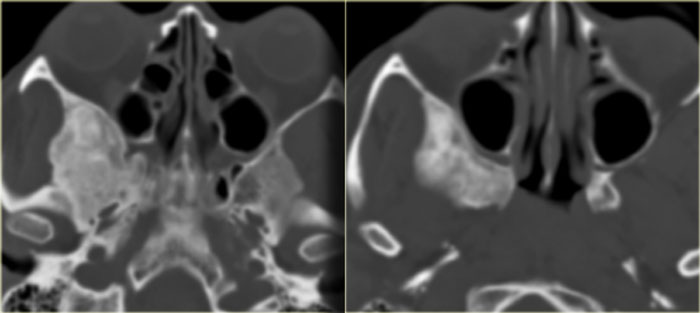
On the left CT-images of a patient post-lung transplant with fever and multiple rapidly progressing cranial nerve palsies.
We will show you CT- and MR-images of this patient. The diagnosis lymphoma was made through biopsy.
First study the images to study the extention od the disease.
Then continue reading.
On the CT-images the findings are:
- Soft tissue mass in the maxillary sinus (red arrow).
- Destruction of the sinus wall (yellow arrow).
- Remodelling and destruction of the pterygoid bone (blue arrow).
- Large soft tissue mass in the masticator space (asterisk).
The image on the right is more cranial.
There is opacification of the sphenoid sinus with destruction of and osteopenia of the sphenoid bone.
CT nicely demonstrates the bone destruction and some of the soft tissue involvement.
Continue with the MR-images.
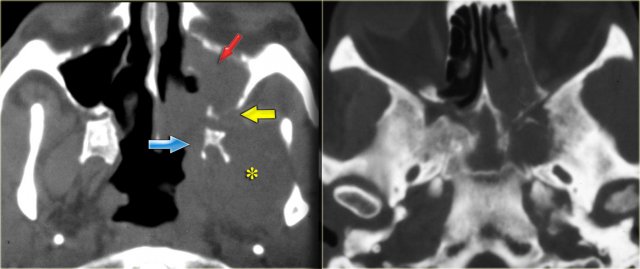
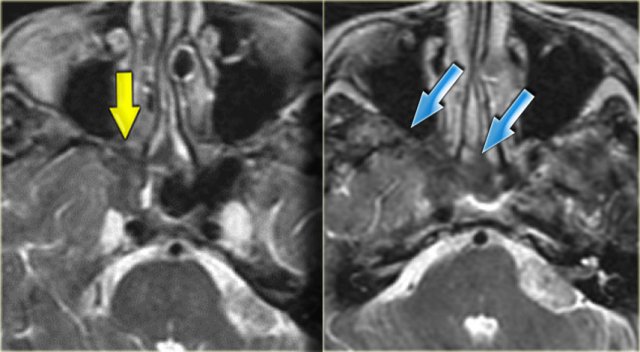
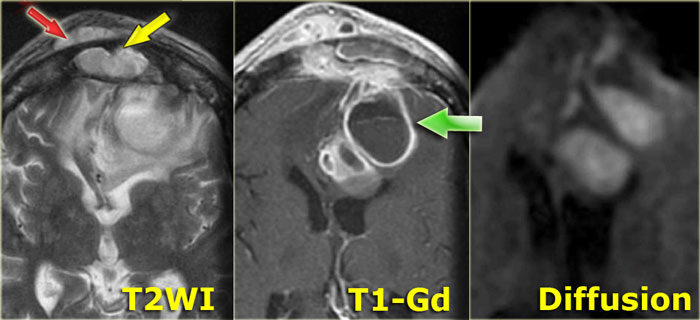
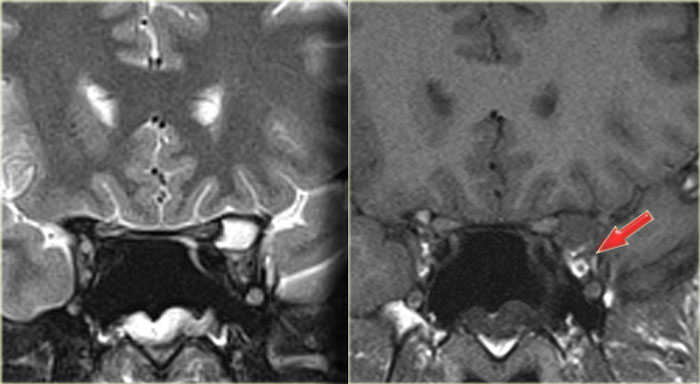
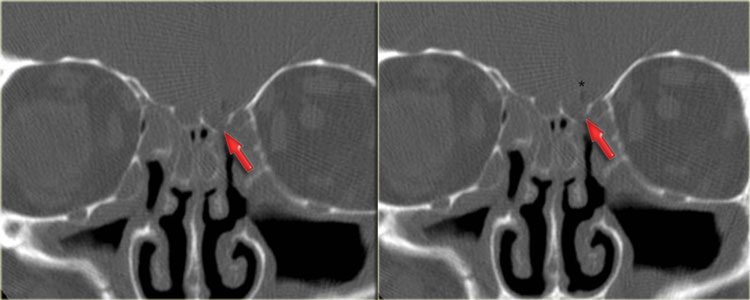
On the left the corresponding MRI.
First study the images, then continue reading.
The findings are:
- Fluid in the right sphenoid sinus (red arrow).
- Hypointense tissue in the left sphenoid sinus (yellow arrows).
- Tracking along the dural margin of the middle cranial fossa (blue arrows).
- Extension into the left zygomatic-masticator space (large yellow arrow).
- Following contrast, there is no solid enhancement of the tissue in the sphenoid space.
Continue with the coronal images.
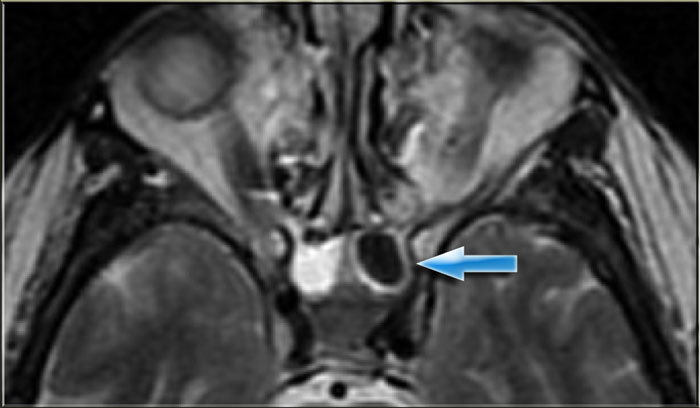
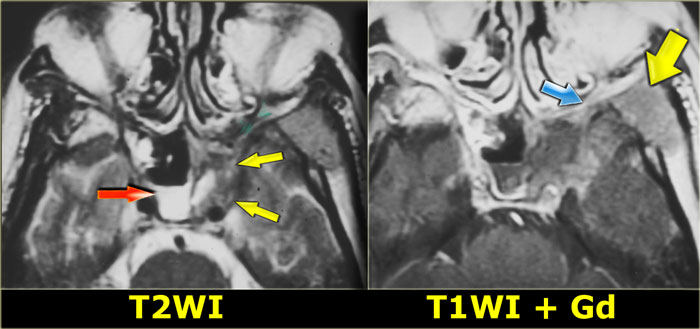
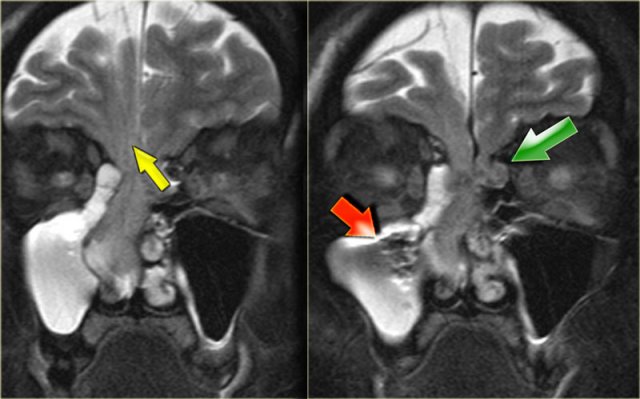
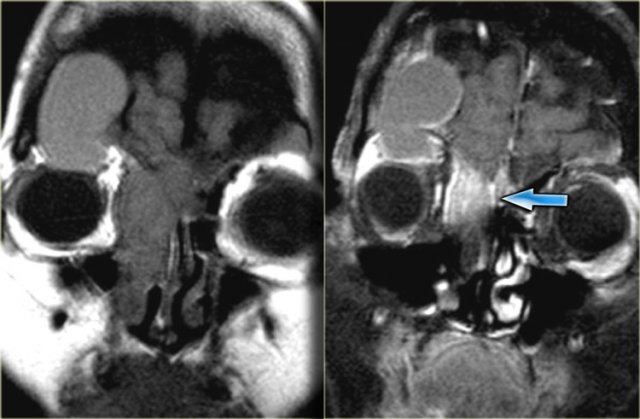
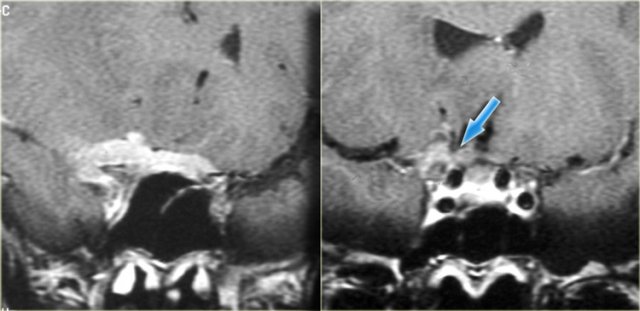
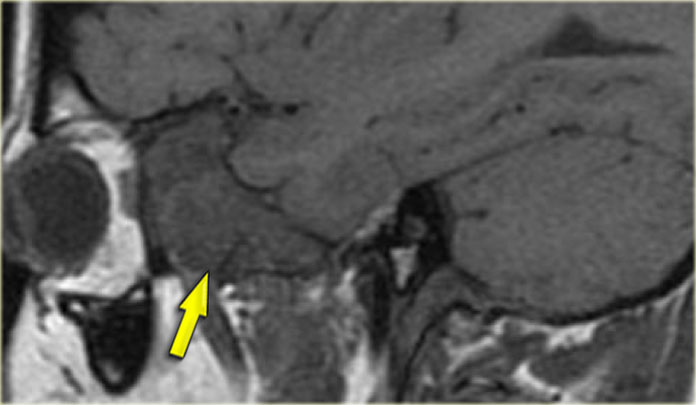
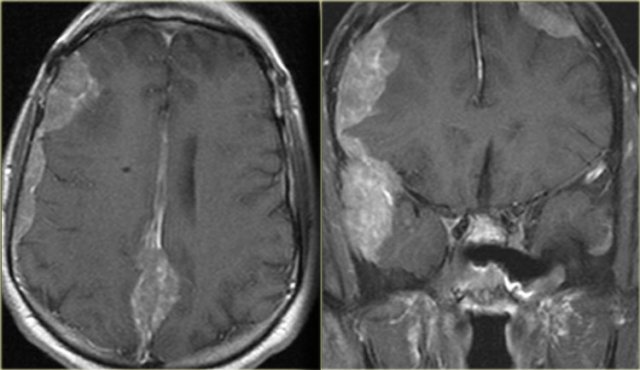
Coronal images of the same patient: T1 pre-and post-contrast.
Normal aspect of the right Meckel's cave, tissue in the left Meckel's cave extending into the cavernous sinus (blue arrow).
The red arrow points to the dural margin of the cavernous sinus: there is enhancement on both sides of the dura.
The disease wraps around the temporal lobe (green arrow) and extents downward in the foramen ovale (yellow arrow) and into the masticator space.
The asterix indicates normal non-enhancing tissue in the masticator space.
This patient had a lymphoma.
Nine out of ten times an immunocompromised patient will have a fungal infection, in one out of ten it will be a lymphoma.
CT and MR have a complimentary role in this case, but finally a biopsy is called for to differentiate between these two diagnoses, because of different treatment.
Role of CT and MR (4)
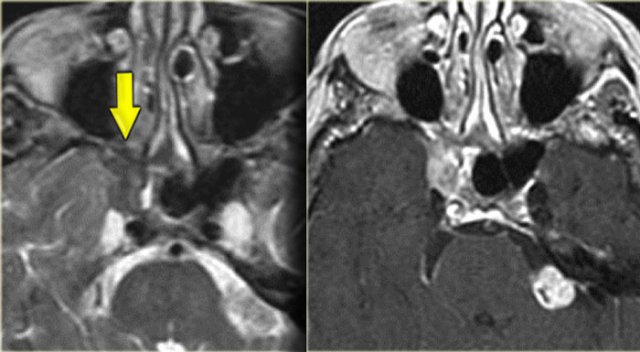
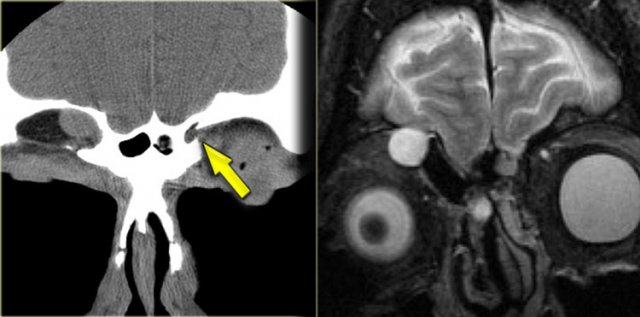
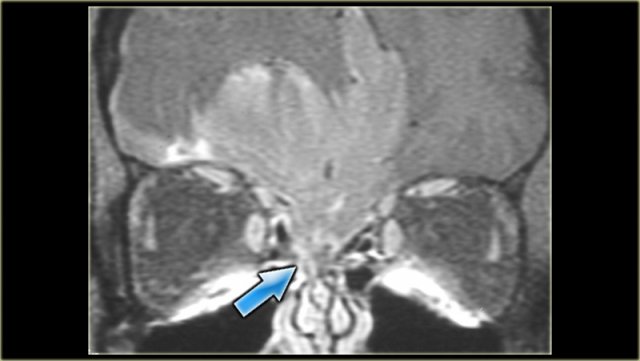
On the left images of a 64-yrs-old, immuno-competent patient, who had a follow-up scan for left-sided vestibular neuroma.
On the image on the left hypointense tissue is seen in the pterygo-palatine fossa and videan canal (yellow arrow).
On the image on the right, which is more cranial, there is hypointense tissue in the pterygo-maxillary fissure and pterygo-palatine fossa.
Continue with the contrast-enhanced T1W-image.
There is solid enhancement of the abnormality.
The differential diagnosis again consists of 2 catagories: neoplasm and chronic invasive fungal infection.
In an immuno-competent patient, a neoplasm is much more likely.
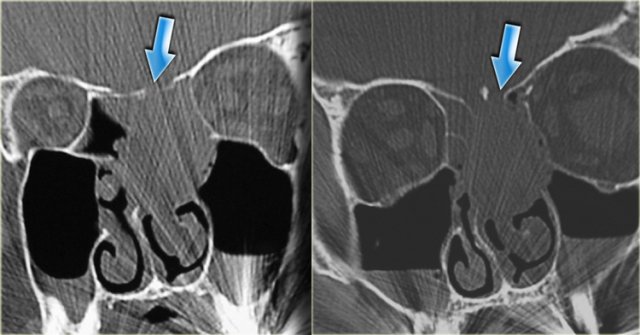
Continue with the CT-images.
This is the corresponding CT, performed not to make the diagnosis, but to assess the condition of the adjacent bony structures, especially the sphenoid sinus.
Also, it serves to guide the endoscopist for intraoperative biospy.
There is extensive destruction of the skull base.
The coronal image illustrates a normal foramen rotundum on the left (yellow arrow), which on the right has been obliterated by soft tissue.
There is extensive bone destruction, and a possible area for biopsy is indicated by the blue arrow.
At biopsy the diagnosis of a spindle cell carcinoma was made.
Complications of Sinusitis
When assessing the complications of sinusitis, CT is excellent for imaging of subperiostial abscesses or orbital extension into the ventral 2/3 of the orbit.
MRI is necessary for assessing intracranial complications, such as brain or epidural abscesses, subdural empyema or sinus thrombosis.
Brain abscess
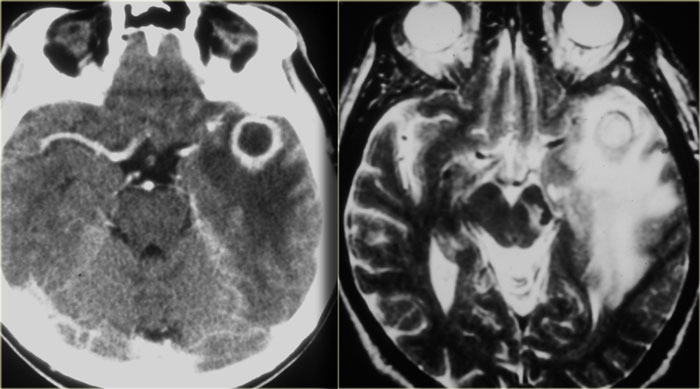
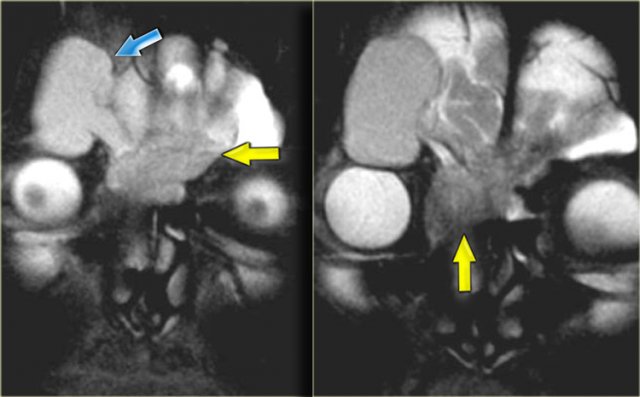
On the left images of a patient was initially diagnosed with a glioblastoma multiforme.
There are abnormalities in both frontal lobes.
Notice however the abnormal tissue in the frontal sinus (yellow arrow), subperiosteal abscess (red arrow) and the fluid-fluid level (green arrow) in the large intracranial lesion which has ring enhancement.
All abnormalities are continuous meaning there is frontal bony destruction.
The restricted diffusion also supports the diagnosis of brain abscess.
This is a subperiosteal abscess and osteomyelitis of the frontal bone, usually with a soft tender swelling of the forehead.
This is also called Pott's puffy tumor after Sir Pott, an English surgeon who first described this entity.
Brain abscess (2)
On the left images of another patient, who had recently been treated for sinusitis and now presented with a seizure.
The CT shows an abnormality in the left temporal lobe with shaggy thick rim enhancement, and a large amount of vasogenic edema.
This is also a brain abscess, most probably due to reflux of bacteria into cranial veins and the venous plexus around the cavernous sinus.
Mucocele
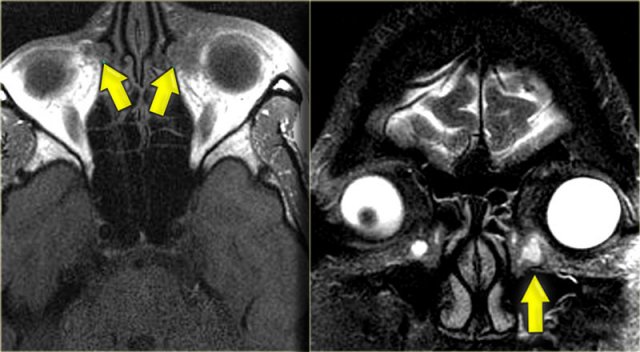
On the left images of a patient with acute sinusitis and ethmoid air cell disease.
He presented with blurred vision.
First study the images, then continue reading.
Notice the fluid in the left anterior clinoid process.
The optic nerve runs medial to it.
Continue with the coronal images.
The coronal T2WI shows expansion of the clinoid process.
The T1WI shows loss of normal fat compared with the right side, and extension into the orbital apex (red arrow).
This is a mucocele of the anterior clinoid with secondary involvement of the optic nerve.
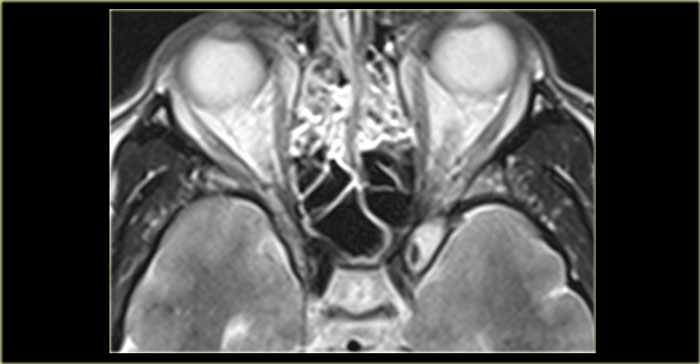
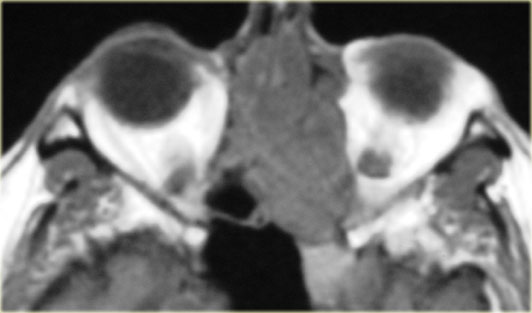
Orbital Cellulitis and Abscess
Left is an axial T1WI, right is a coronal T2WI.
There is an abnormality on the left side, but to a lesser degree also on the right.
Try to determine which structures are involved.
The yellow arrows point to the naso-lacrimal ducts.
The naso-lacrimal sac connects with the duct, which then drains into the inferior meatus.
On the left there is peri-orbital pre-septal soft tissue swelling.
On the coronal image there is bilateral high signal at the junction of the nasolacrimal duct and sac, indicative of a fluid collection.
On the left side there is also edema of the surrounding tissue.
Post-contrast T1WI, axial and coronal.
Lateral to the naso-lacrimal ducts on both sides, there are the fluid collections which now show peripheral enhancement.
The additional images (T2WI) show mucosal disease of the right maxillary sinus and a fluid level in the left maxillary sinus, in addition to extensive ethmoidal and sphenoidal sinus disease.
This patient had acute sinusitis which was complicated by orbital cellulitis and dacrocystitis with abscesses.
Developmental or inflammatory narrowing of the naso-lacrimal duct is a risk factor for developing dacrocystitis.
Complication of FESS
A rare complication of FESS is seen on the images on the left.
The Hounsfields Units of the tiny abnormalities that the asterisk points to were around -120.
First study the axial images.
Then continue with the coronal images.
There is a bone defect at the fovea ethmoidalis (red arrow).
Also there are post-operative changes indicating that the patient had undergone FESS.
The intracranial air is a complication of FESS.
With this complication, usually the patient goes home feeling fine, and then shows up approximately two weeks later with CSF leak and meningitis, due to the defect in the bone and dura.
Tension pneumocephalus occurs when air in the head acts like a mass: there is a bony defect which lets air in but not out (valve-like function).
Every time the patient sneezes, air is forced through the defect into the intra-cranial space, and remains trapped there.
At a certain moment the amount of air is sufficient to cause mass effect on the surrounding intra-cranial structures.
Tumor and tumorlike lesions
Role of CT and MR
When it comes to imaging of neoplasms of the paranasal sinuses, CT and MRI play complementary roles.
It is not about the histology but about answering the question 'is it tumor or not?' and then determining the extent of the disease, for example intracranial or orbital extension.
Use MRI to differentiate inspissated secretions from neoplasms.
Scanning down to the hyoid bone allows for examination of the levels I and II lymph nodes: about
10% of paranasal neoplasms have nodal metastases at presentation.
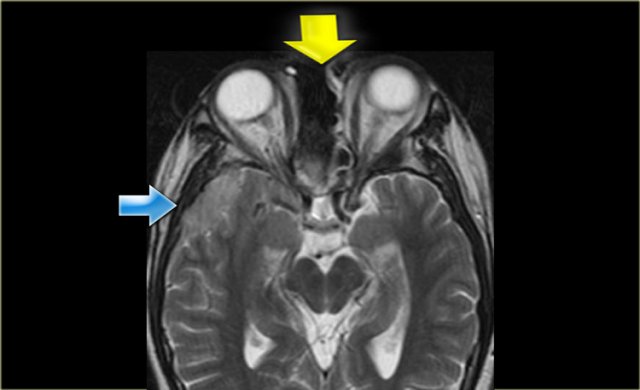
Encephalocele
Coronal T2WI of the patient on the left show an abnormal structure in the right nasal cavity.
When you've decided what it is, then stop to think about whether the abnormality is developmental or acquired.
This patient has an encephalocele.
There are two findings on the images that let you know that this is developmental.
First of all, notice the smaller encephalocele on the left side (green arrow).
Acquired encephaloceles are more often than not unilateral.
The second clue is the cortical dysplasia (yellow arrow) as part of a migrational abnormality.
Acquired encephaloceles (ie after surgery) tend to lead to dead gliotic brain, which would have a high signal intensity on T2WI.
The strange looking structure in the left image (red arrow) is surgical packing, placed there after the involuntary encounter with brain tissue.
The blue arrow points to the sphenoid sinus which is hyperintense, due to mucoid impaction as a result of obstruction by the encephalocele.
Mucocele
Mucoceles are benign, locally expansile paranasal sinus masses most commonly found in the frontal sinus.
Secondary to obstruction of the sinus ostia, there is accumulation of fluid within a mucoperiosteal lined cavity, resulting in erosion and remodelling of the surrounding bone.
The most common causes of mucoceles are chronic infection, allergic sinonasal disease, trauma and previous surgery.
The most common location of a mucocele is the fronto-ethmoidal sinus, followed by the sphenoid sinus.
The least common location is the maxillary sinus.
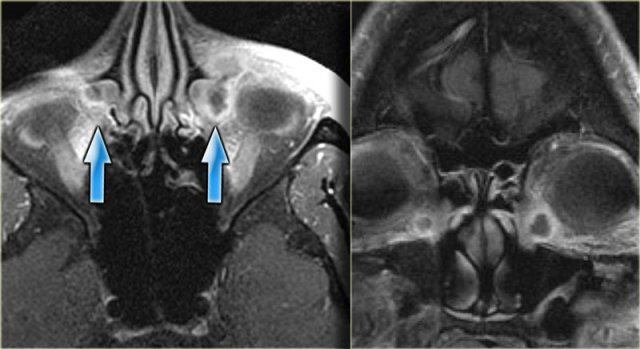
On the left a patient with an uncommon cause of a mucocele.
Notice the obstructing solid mass at the frontal ethmoidal junction (yellow arrows).
Pre- and post-contrast MRI of the same patient.
The mucocele shows high signal intensity on T1W (benign finding).
The mass in the ethmoidal region is hypointense and solidly enhancing.
Mucocele (2)
The case on the left shows two classic complications of frontal facial trauma.
The bilateral nasal fractures are the clue to a traumatic etiology.
Looking at the CT scan on the far left you will notice a convex soft tissue mass in the frontal sinus.
The corresponding MRI shows a round hyperintense structure in the same location.
Study the images on the left and then continue reading.
Now look again carefully at the far left CT.
Did you notice the bony defect on the left side, at the lateral border of the ethmoid air space (yellow arrow)?
The MRI shows that there is brain tissue at the site of the defect.
This patient had both a mucocele and an acquired encephalocele.
The two most common causes of mucoceles are trauma and chronic inflammation due to blockage of the ostia.
Mucocele (3)
This companion case nicely demonstrates bilateral mucoceles.
This patient has chronic sinusitis with sino-nasal opacification, mucoid impaction in the maxillary sinusses and huge bilateral mucoceles.
The CT shows hyperdensity and the MRI shows hyperintensity on T2WI, both of which you will remember are benign signs in sino-nasal disease, indicating a proteinaceous substance.
There is smooth bone remodelling and elevation of the frontal sinusses, and although it looks as if there is bony destruction at the orbital boundary of the frontal sinus, usually the surgeon will still see a fine line of bone in place.
Inverted papilloma
Inverted papilloma is characterized by inversion of the neoplastic epithelium into the underlying stroma.
It presents as a unilateral nasal polyp arising from the lateral nasal wall, usually in the region of the middle meatus and middle turbinate.
Extension into the maxillary and ethmoid sinuses is common.
It causes non-specific symptoms like nasal congestion or epistaxis.
Biopsy is necessary to make the diagnosis and because more than 10% of inverted papillomas harbor a squamous cell carcinoma.
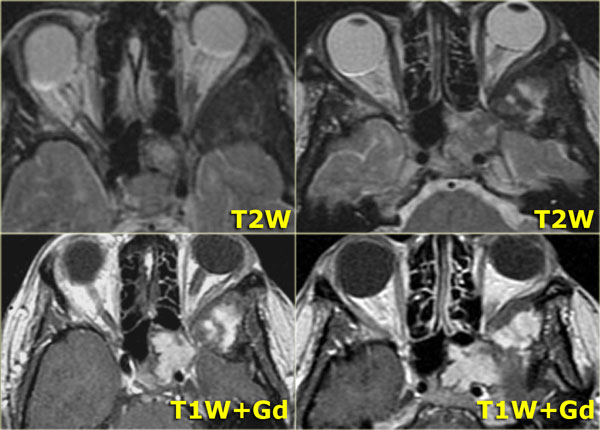
When you want to differentiate inspissated secretions from neoplasms it is important to have pre- and post-contrast images.
If you were to just look at the post-contrast study on the right, you might be tempted to think that there was solid enhancement of the mass in the nasal cavity (asterisk) as well as in the ethmoidal and maxillary sinus on the right.
Looking at the pre-contrast study, however, you will notice that the contents of the ethmoidal and maxillary sinuses are hyperintense as opposed to the mass in the nasal cavity (the middle meatal region), because the sinuses are filled with inspissated secretions.
This solidly enhancing mass is a tumor until proven otherwise.
The imaging findings are non-specific and the differential diagnosis includes a polyp or a carcinoma.
Biopsy revealed an inverted papilloma.
Inverted papilloma (2)
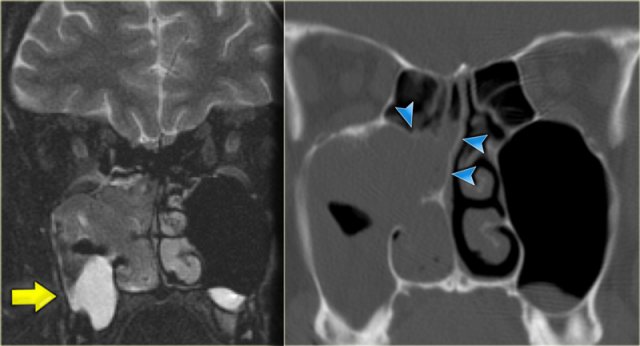
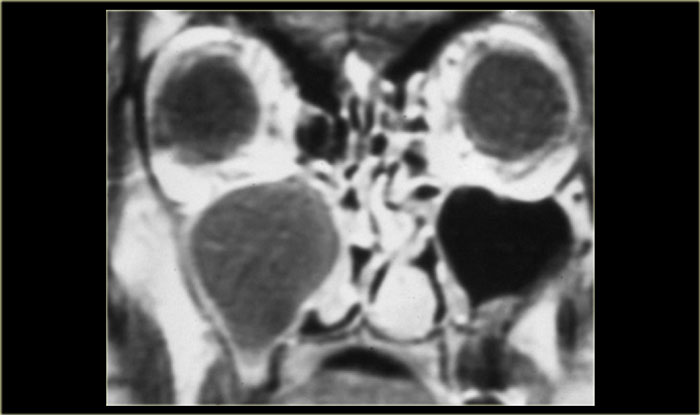
On the left another patient who presented with nasal stuffiness.
Study the images on the left.
Decide for yourself whether you are looking at a solid mass, inspissated secretions, a combination of both or something entirely different.
The pre-contrast T1WI shows a hyperintense area within the maxillary sinus, corresponding to a proteinaceous substance.
Medial to it is an area with hypointense signal similar to the signal in the orbital globes (so probably cystic).
The majority of the soft tissue in the right maxillary sinus is relatively hypointense on the pre-contrast T1WI,
but solidly enhances, meaning tumor.
The T2W-image on the left confirms the cystic element (yellow arrow).
The coronal CT nicely demonstrates remodelling of the bone and expansion (arrowheads).
This proved to be an inverting papilloma.
The localisation is rather typical.
Malignant tumors of the sinonasal tract
Malignant tumors of the sinonasal tract are extremely rare.
The clinical presentation is non-specific and often mimics benign disease.
As a result a delay in diagnosis is common.
75% of all paranasal sinus tumors are Stage T3 or T4 at the time of diagnosis.
Perineural spread is a manifestation of advanced disease and indicates a poor prognosis.
On the left an axial MR-image showing a mass in the ethmoids.
The MRI shows no intracranial extension.
What is the next step?
A CT is necessary to determine the integrity of the adjacent bone.
Notice the bony destruction of the fovea ethmoidalis and planum sphenoidale.
This indicates that this is a malignant lesion and biopsy demonstrated an adenocarcinoma.
If the patient is a surgical candidate, frontal endoscopic sino-nasal surgery won't be enough and a cranio-facial take-down will also be required.
Meningioma
A meningioma can spread transcranially.
On the left is a patient with a meningioma, which spreads along the anterior clinoid (arrow).
Continue with a coronal image more anteriorly.
MRI nicely demonstrates how the meningioma spreads down into the sino-nasal cavity.
Keratocyst
First look at the images on the left.
From where is this lesion arising?
The lesion is expansile with bone remodelling and there is an obvious relation to a tooth.
It is very important to determine whether or not sinus pathology has an odontogentic origin, simply
because the surgical approach is different.
If odontogentic, the surgery will be done preferably by a maxillofacial surgeon.
If approached by a sino-nasal route it won't be removed entirely.
This is a keratocyst
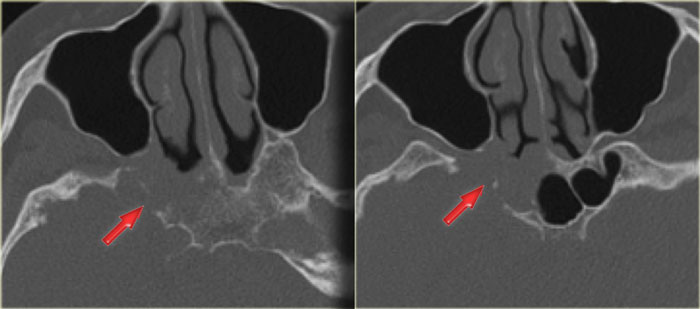
On the left another case.
This patient presented with facial pain.
On this contrast-enhanced MRI we see a non-enhancing expansile lesion in the right maxillary sinus.
As it doesn't enhance, we know we aren't dealing with tumor.
It is tempting to call this a retention cyst and move on to the next case, but a CT is called for to make the correct diagnosis.
The corresponding CT shows elevation of the maxillary bone (blue arrow).
The red arrow in the right image indicates the cyst dissecting around the root of a tooth.
This is also a keratocyst.
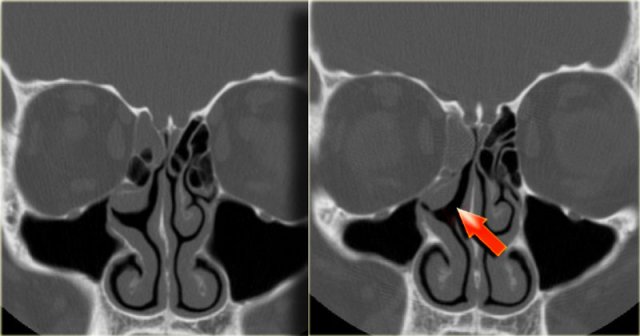
Silent sinus
On the left a patient who presented with asymmetric eyes.
First study the images and try to describe what is going on.
Then continue reading.
This film was originally read as ethmoid sinusitis and post-surgery.
However, this patient had never undergone sino-nasal surgery.
What you in fact see, is adhesion of the middle right turbinate (red arrow) and the uncinate process
to the floor of the orbit.
There is also volume loss of the right maxillary sinus.
This is called the silent sinus syndrome, which consists of painless facial asymmetry and enophthalmos caused by chronic maxillary sinus atelectasis.
The most characteristic imaging feature of the silent sinus syndrome is the inward retraction of the sinus walls into the sinus lumen with associated decrease in sinus volume and enlargement of the middle meatus (2).
In many cases the infundibulum is occluded due to lateral retraction of the uncinate process.
Fibro-osseous Lesions
Fibro-osseous lesions are very common incidental findings and often misinterpreted as tumor.
CT is usually diagnostic, so when you see a bizarre lesion at the skull-base, think of a fibro-osseous lesion and get an unenhanced CT.
The most common skull base lesion is fibrous dysplasia, followed by osteomas.
Osteomas are usually located in the sino-nasal cavities.
Fibromas are less common and can be ossifying or non-ossifying.
Malignancies are rare.
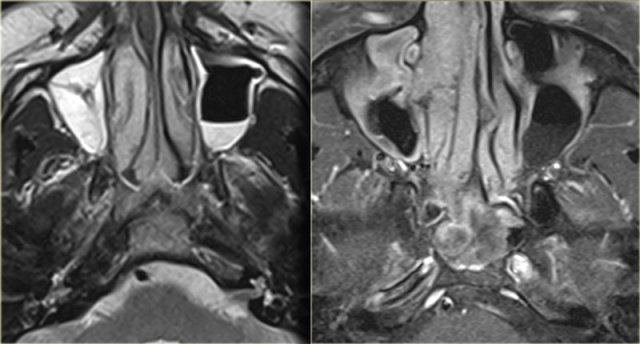
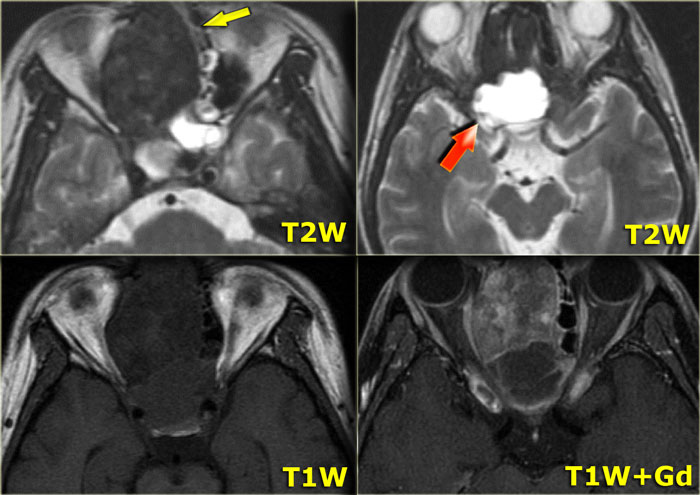
Fibrous dysplasia
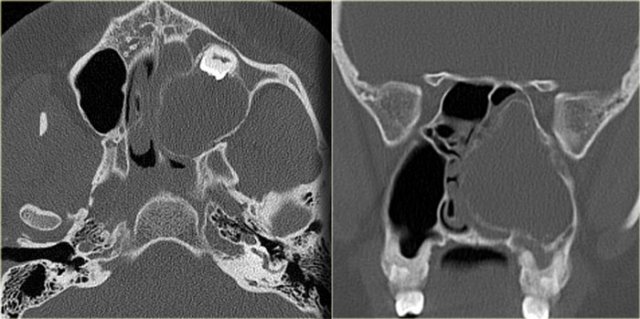
On the left images of a patient who was thought to have a chondrosarcoma.
On the T2W-images there is a hypointense lesion (yellow arrow) with a cystic component (red arrow).
On the pre- and post-contrast T1W-images there is solid enhancement of a mass with peripheral enhancement of the cystic portion.
Question: what should be the next step?
Next step: get a CT!
On CT this is classic fibrous dysplasia (FD) with cortical sparing and ground-glass appearance.
Many of the fibrous dysplasia lesions in the clivus, skull base or sino-nasal cavity and in children may have large cystic components, so don't let that dissuade you from the diagnosis!
Fibrous dysplasia (2)
On the left another example of fibrous dysplasia.
This lesion originates from the middle turbinate.
Fibrous dysplasia (3)
On the left another patient read as having a soft tissue tumor (yellow arrow) anterior to the temporal bone.
These are the corresponding axial CT images showing classic fibrous dysplasia of the sphenoid wing.
The differential diagnosis is a meningioma.
Fibrous dysplasia (4)
On the left images of a different patient with soft tissue in the sphenoid sinus on the left, and an abnormality of the left sphenoid wing, which is about 3 times its normal size whilst maintaining its normal shape.
On the post-contrast images there is solid enhancement.
Again the diagnosis is fibrous dysplasia.
Fibrous dysplasia is a very vascular lesion and can enhance avidly.
Osteitis
In contrast, this is a patient with osteitis of the middle turbinate and ethmoid septae.
Note the laminated high density, due to chronic inflammation and recurrent periostal reaction with neo-osteogenesis around the septae.
Osteoma
This is a patient who had been having brain MRI for the past 1,5 yrs for frontal headaches.
On the MRI (not shown) it looked as if the patient had a little mucosal disease of the frontal sinus.
The sinus CT clearly shows an osteoma with a bony defect (arrow) indicating progressive growth.
This lesion requires surgical excision.
Note: multiple para-nasal osteomas are found in Gardner's syndrome, which also includes cutaneous and soft tissues tumors in addition to colonic polyps with a predilection to malignant degeneration.
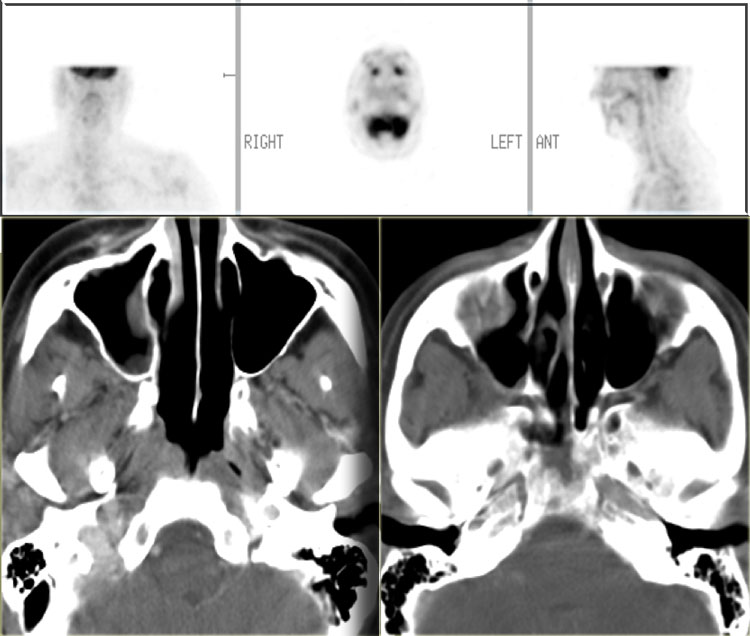
Monitoring response to therapy
Imaging can also be used to monitor treatment response.
This patient had a skull-base B-cell lymphoma.
Pre-treatment we see the extent of the lesion, which is FDG-avid.
Three months into therapy the skull-base mass has resolved.
There is no more pathological FDG uptake, and there is remineralisation of the bone.
The patient on the left had a resection of a carcinoma.
Now there is a recurrence (blue arrow on MR and fusion image).
The green arrow, however points to post-radiation tissue changes.
On the left a patient who had a prior cranio-facial resection (yellow arrows) for an undifferentiated carcinoma.
This patient was treated with chemoradiation.
The T2WI on the left shows tumor recurrence intracranially.
Continue with the contrast enhanced images.
In cases like this a recurrence tend to show bizarre patterns such as these extensive dural implants.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.