Cardiac Anatomy
Tineke Willems and Marieke Hazewinkel
Radiology department of the University Medical Centre Groningen and the Medical Centre Alkmaar, the Netherlands
Publicationdate
This review is based on a presentation given by Tineke Willems and was adapted for the Radiology Assistant by Marieke Hazewinkel.
We will discuss:
- The different cardiac axes
- The cardiac anatomy in the order of normal blood flow: from the right to the left.
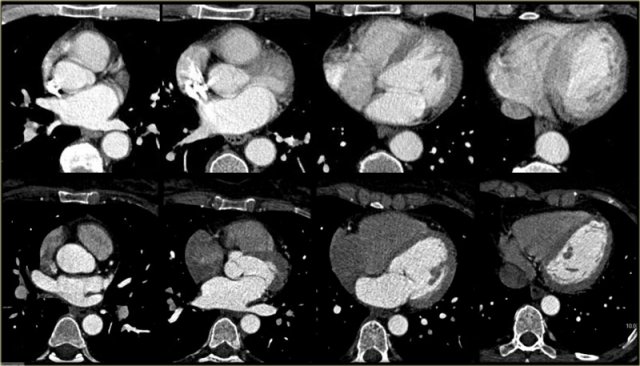
Cardiac Axes
Cardiac CT with ECG triggering offers good image quality of the heart when compared to CT performed for other purposes.
As in any other field of radiology, analysis of the acquired images requires a systematic approach.
First of all, it is important to understand that the orientation of the heart in the human body differs from that of other anatomic structures: the right ventricle, for example, does not lie completely on the right, but more anterior.
The left ventricle does not lie on the left, but more posterior.
Also, the heart does not always maintain the same position within the mediastinum - in young people it tends to have a vertical orientation, whereas in older people it tends to rest on the diaphragm, a more horizontal orientation.
Cardiologists analyze the heart using cardiac axes.
These axes are also used in cardiac CT/MR and must be reconstructed in order to assess the heart properly.
Axial slices, such as those imaged on the left, are useful for a global assessment of the morphology of the heart and its relation to the pericardium.
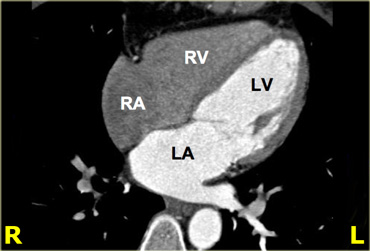
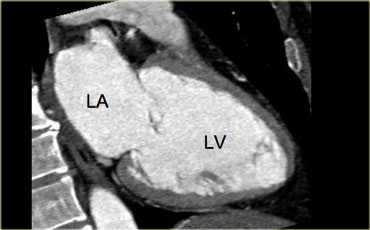
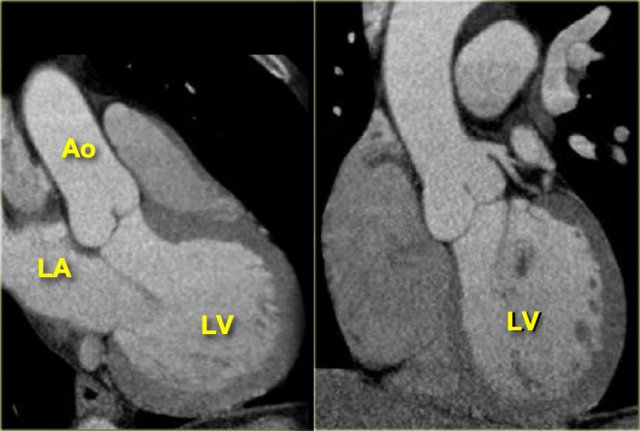
4-chamber view
On the left is a 4-chamber view, achieved by rotating upwards from the apex of the heart on the axial slices.
In this axis, the right ventricle is projected next to the right atrium, and the left ventricle next to the left atrium.
The mitral valve comes into view and - depending on the contrast protocol - the tricuspid valve may also be visible.
Another feature of this cardiac axis is that the apex of the heart is well demarcated.
Note that the apex is formed by the left ventricle.
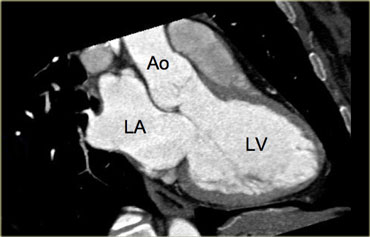
3-chamber view
When the border between the mitral and aortic valves is localized on the axial slices and the images are rotated from this point, a 3-chamber view like the image on the left can be reconstructed.
On this image, the left atrium, left ventricle, mitral-, aortic valve and proximal aorta ascendens are visible.
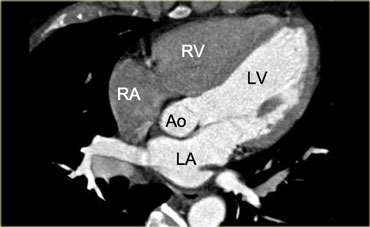
5-chamber view
On the left is an image of a 5-chamber view, which is similar to the 4-chamber view, but additionally displays the aortic valve and left ventricular outflow tract.
This view is achieved by rotating the 4-chamber view a little more cranially.
2-chamber view
The 2-chamber view in the image on the left is achieved by rotating the images perpendicularly to the mitral valve and parallel to the cardiac septum.
This axis gives an overview of the left atrium ventricle and mitral valve.
It is a good view for analyzing ventricular function, especially that of the inferior and anterior walls.
For attaining functional data, consecutive short axes must be reconstructed making use of the 3- and 4-chamber views.
Cardiac anatomy from right to left
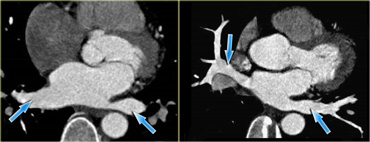
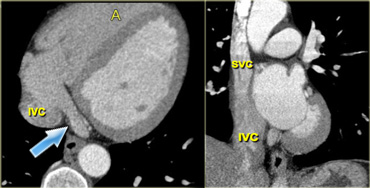 Axial (left) and coronal oblique (right) reconstructions of the heart, depicting the right atrium and its main contributing blood vessels: the coronary sinus (blue arrow) and superior and inferior vena cava. IVC=inferior vena cava, A=anterior, SVC=superior vena cava
Axial (left) and coronal oblique (right) reconstructions of the heart, depicting the right atrium and its main contributing blood vessels: the coronary sinus (blue arrow) and superior and inferior vena cava. IVC=inferior vena cava, A=anterior, SVC=superior vena cava
Right atrium
The cardiac anatomy will be discussed in the order of normal blood flow: from the right to the left.
In the normal situation, contrast will be injected intravenously - usually in the arm - reaching the right atrium via the superior vena cava.
The right atrium has an anterolateral position in the heart, and lies inferior to the left atrium.
The superior vena cava enters through the roof of the right atrium.
The inferior vena cava enters the right atrium from below near the cardiac septum.
Another structure that carries blood towards the right atrium is the coronary sinus, (venous return of the coronaries) which enters anterior to, and just to the left of the inferior vena cava.
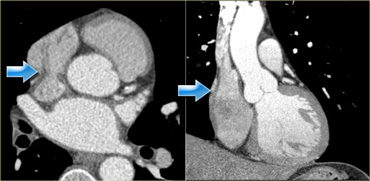 Axial (left) and coronal (right) reconstructions showing the crista terminalis (blue arrows) and its location in the right atrium
Axial (left) and coronal (right) reconstructions showing the crista terminalis (blue arrows) and its location in the right atrium
Crista terminalis
In the right atrium lies the crista terminalis, a muscular ridge that runs from the entrance of the superior- to that of the inferior vena cava.
This structure separates the smooth part of the right atrium - the sinus venosus - from the trabecularized right atrial appendage.
On the images on the left it is visible as a smooth linear structure (blue arrows).
This is not always the case, however, it may simulate a mass.
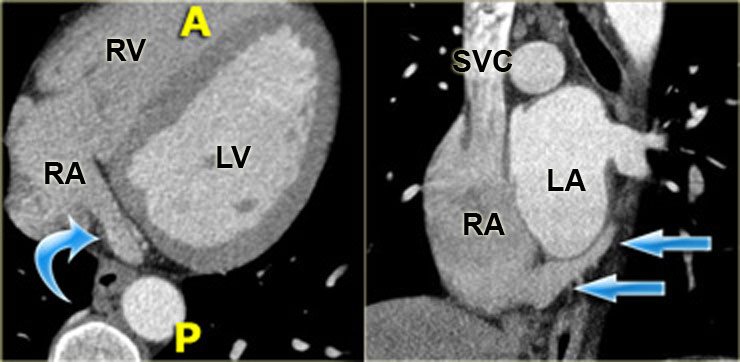 Axial (left) and coronal oblique (right) reconstructions showing the coronary sinus as it enters the right atrium (blue arrows). A=anterior, P=posterior
Axial (left) and coronal oblique (right) reconstructions showing the coronary sinus as it enters the right atrium (blue arrows). A=anterior, P=posterior
Coronary sinus
The coronary sinus is the main draining vein of the myocardium.
It runs in the atrioventricular groove on the posterior surface of the heart and enters the right atrium in the vicinity of the tricuspid valve.
On the left is a reconstruction illustrating the course run by the coronary sinus in the atrioventricular groove on the posterior surface of the heart.
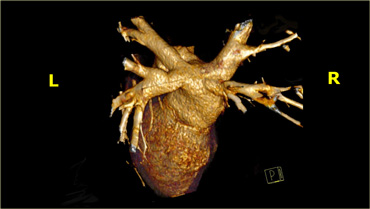
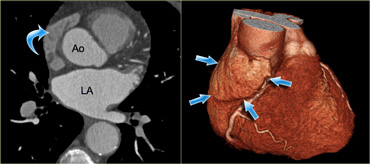 Axial (left) and 3D-reconstructions (right) of the heart demonstrating the right atrial appendage (blue arrows). Ao=aorta, LA=left atrium
Axial (left) and 3D-reconstructions (right) of the heart demonstrating the right atrial appendage (blue arrows). Ao=aorta, LA=left atrium
Right atrial appendage
The right atrial appendage is the trabecularized part of the right atrium.
It partially covers the atrioventricular groove and the right coronary artery that runs in it.
Characteristically, it is flat and triangular in shape and contains small muscular bundles which run parallel to the atrium itself.
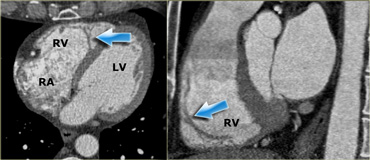 Axial (left) and sagittal oblique (right) reconstructions showing the right ventricle. The blue arrows indicate the moderator band. RA=right atrium, RV=right ventricle, LV=left ventricle
Axial (left) and sagittal oblique (right) reconstructions showing the right ventricle. The blue arrows indicate the moderator band. RA=right atrium, RV=right ventricle, LV=left ventricle
Right ventricle
Blood leaves the right atrium and enters the right ventricle via the tricuspid valve.
This valve has three leaflets and three papillary muscles, which partially insert on the septum (in contrast to the papillary muscles of the mitral valve, which do not).
The right ventricle is shaped differently to the left ventricle: the left ventricle is cylindrical in shape and the cavity of the right ventricle is effectively wrapped around it.
The right ventricle also has a thinner wall which is more trabecularized, especially towards the apex.
The moderator band is another distinguishing feature of the right ventricle.
It runs from the septum to the lateral wall of the right ventricle, and plays a key role in the electrophysiological conduction of the right ventricle's free wall (blue arrows).
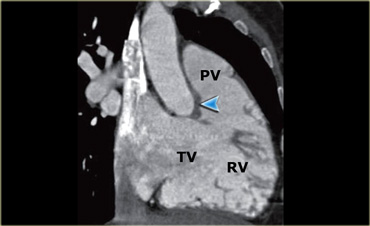 Reconstruction showing the tricuspid (TV) and pulmonary (PV) valves as well as the cavity of the right ventricle (RV). The blue arrow indicates the crista supraventricularis
Reconstruction showing the tricuspid (TV) and pulmonary (PV) valves as well as the cavity of the right ventricle (RV). The blue arrow indicates the crista supraventricularis
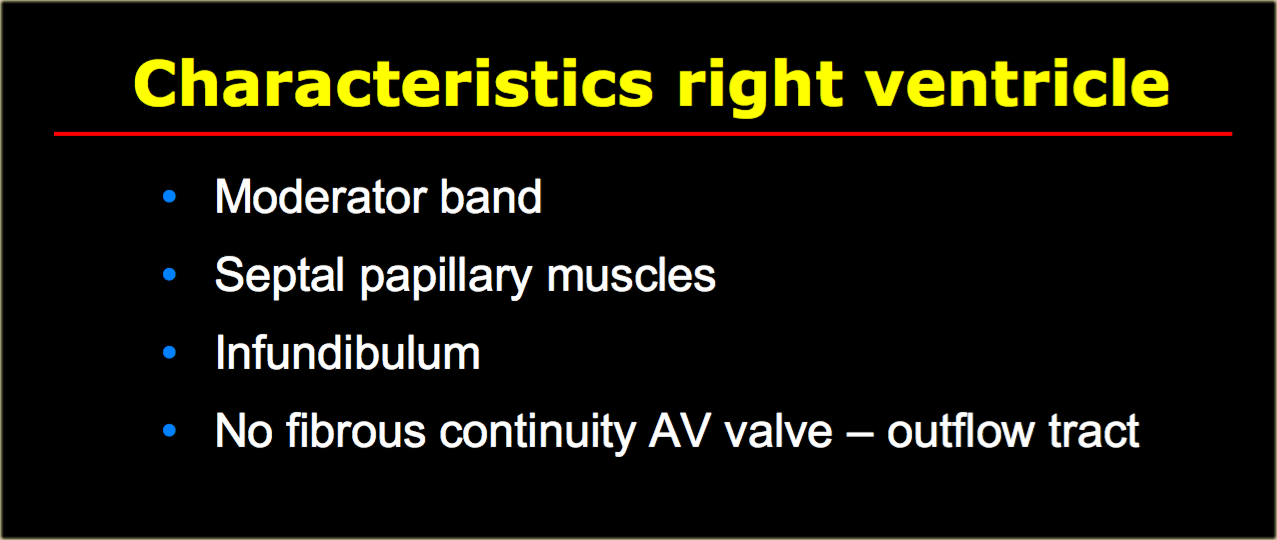
Pulmonary valve
Next, blood runs towards the pulmonary valve - first entering the smooth, muscular infundibulum of the right ventricle.
The pulmonary valve has three cusps, and is separated from the tricuspid valve by a thick muscle known as the crista supraventricularis (blue arrow in the image on the left).
This differs from the left ventricular outflow tract, where the mitral and aortic valves lie side by side.
On the left is a summary of the characteristics which are specific for the right ventricle and are useful in distinguishing the left from the right ventricle in cases with complex congenital cardiac anatomy.
Pulmonary veins
Oxygen-rich blood enters the left atrium via the pulmonary veins.
In most cases, there are two pulmonary veins on the left and two on the right.
The middle pulmonary veins usually drain into the superior pulmonary vein.
There are frequent variations in pulmonary vein anatomy however, especially on the right, where an anomalous insertion is associated with atrial fibrillation.
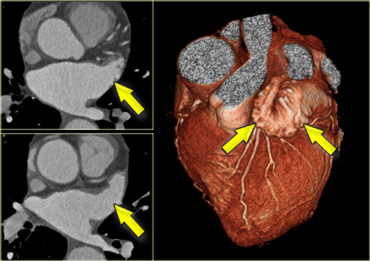 Axial and 3D-reconstructions illustrating the shape and location of the left atrial appendage (yellow arrows).)
Axial and 3D-reconstructions illustrating the shape and location of the left atrial appendage (yellow arrows).)
Left atrial appendage
The left atrial appendage is a finger like, trabecularized structure which originates supralaterally in the left atrium. It lies over the left atrioventricular groove, and partially covers the left coronary artery in it.
Its small, parallel-running muscles should not be mistaken for thrombus.
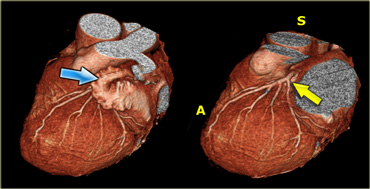 3D-reconstructions showing the left atrial appendage (blue arrow) and the left coronary artery (yellow arrow) after the left atrial appendage has been removed. A=anterior, S=superior).)
3D-reconstructions showing the left atrial appendage (blue arrow) and the left coronary artery (yellow arrow) after the left atrial appendage has been removed. A=anterior, S=superior).)
When assessing the coronary arteries, the left atrial appendage must be removed, so that the LCX and proximal LAD may be visualized.
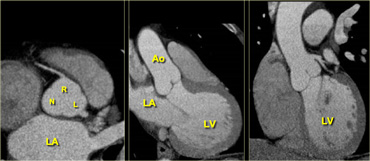 Axial (left) reconstruction, 3-chamber view (middle) and coronal reconstruction (right) of the heart illustrating the relationships between the left atrium, ventricle and aortic root. LA=left atrium, R=right coronary cusp, L=left coronary cusp, N=non-coronary cusp, Ao=aorta, LV=left ventricle
Axial (left) reconstruction, 3-chamber view (middle) and coronal reconstruction (right) of the heart illustrating the relationships between the left atrium, ventricle and aortic root. LA=left atrium, R=right coronary cusp, L=left coronary cusp, N=non-coronary cusp, Ao=aorta, LV=left ventricle
Left ventricle
Blood enters the left ventricle via the mitral valve.
This is a complex valve, consisting of an annulus and posterior and anterior leaflets.
The leaflets are connected to the papillary muscles via cord-like tendons called chordae tendinae.
The papillary muscles insert into the lateral and posterior walls as well as the apex of the left ventricle.
In normal situations the left ventricle has a uniform thickness, varying end-diastolically from 0.6 to 1.0 cm.
Blood enters the aortic valve via the left ventricular outflow tract.
Note that there appears to be a fibrous connection between the mitral and aortic valve.
Aortic valve
Like the pulmonary valve, the aortic valve has three cusps.
Just cranially to it there is a slight dilatation of the aortic root.
This is the sinus of Valsalva.
It fills with blood during diastole, supplying the coronary arteries with oxygen-rich blood.
The image on the right shows that the coronary arteries originate fairly cranially, on the border of the ascending aorta.
 Axial reconstruction depicting the tricuspid aortic valve with its right and left coronary (R and L respectively) and non-coronary cusp (N)
Axial reconstruction depicting the tricuspid aortic valve with its right and left coronary (R and L respectively) and non-coronary cusp (N)
The cusps of the aortic valves are named according to their relationship with the coronary arteries, namely the right coronary, left coronary and non-coronary cusp (R, L and N).