Fractures
Robin Smithuis
Radiology department of the Rijnland Hospital in Leiderdorp, the Netherlands
Publicationdate
Fractures of the distal radius account for one-sixth of all fractures seen in the emergency department.
The radiologist must possess an understanding of the factors that alter clinical decision making and patient treatment.
In this review we will discuss:
- Importance of standard radiography of the wrist
- Proper description of fractures with knowledge of injury mechanisms, consequent care and complications
- Commonly used fracture eponyms like Colles', Smith's, Barton's etc.
- AO- and Fernandez classification
- Treatment
- Complications
Imaging
 PA view: wrist and elbow at shoulder heightLateral view: shoulder, elbow and wrist in sagittal plane
PA view: wrist and elbow at shoulder heightLateral view: shoulder, elbow and wrist in sagittal plane
Positioning
PA view should be taken with the wrist and elbow at shoulder height.
This means that the wrist, elbow and shoulder are all in the transverse plane, perpendicular to the x-ray beam.
Only in this position, the radius and the ulna are parallel.
Lowering the arm makes the radius cross the ulna and become relatively shorter resulting in improper measurement of the length of the radius.
Lateral view is taken with the elbow adducted to the side.
Shoulder, elbow and wrist are again in one plane, i.e. the sagittal plane.
This positioning will make the lateral view exactly perpendicular to the PA view.
On a correctly positioned PA view the extensor carpi ulnaris tendon groove (arrow) can be seen.
The extensor carpi ulnaris tendon groove should be at the level of or radial to the base of the ulnar styloid.
 True lateral: The palmar cortex of pisiform (red arrow) lies between the palmar cortex of scaphoid and capitate.
True lateral: The palmar cortex of pisiform (red arrow) lies between the palmar cortex of scaphoid and capitate.
A true lateral view is defined by the relationship between the pisiforme, capitate and scaphoid bones.
On a standard lateral view, the palmar cortex of the pisiform bone should overlie the central third of the interval between the palmar cortices of the distal scaphoid pole and the capitate head.
Apparent volar tilt of the surface of the distal radius, as measured on the lateral view, increases with supination and decreases with pronation of the wrist (5).
A change of 10 degrees rotation between two consecutive control lateral radiographs is not uncommon during clinical follow-up and results in 5 degrees change in apparent tilt.
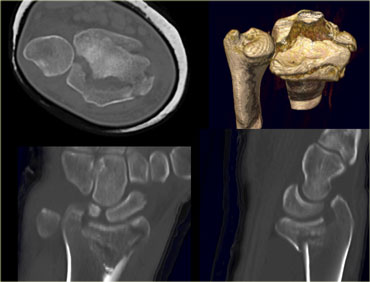
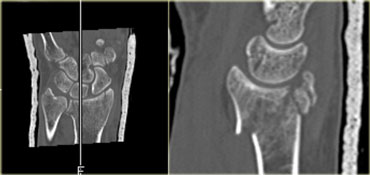
CT should be performed if conventional radiographs provide insufficient detail about radiocarpal articular step-off and gap displacement.
On the left a patient with a communitive intraarticular fracture of the distal radius with displacement of the volar rim of the radius together with the carpus (i.e. a volar Barton's).
There is an axial CT image with 3D-, coronal and sagittal reconstructiosn.

On the left sagittal reconstructions of 1mm axial CT slices.
Scroll through the images and notice how well CT demonstrates the fracture components and the displacement.
Magnetic resonance (MR) imaging is of benefit when concomitant injuries of ligaments and triangular fibrocartilage complex (TFCC) are suspected or if a fracture is suspected but not demonstrated on routine radiographs.
On the left a fracture of the ulnar styloid process not visible on standard radiography, but clearly demonstrated with MR.
Measurements
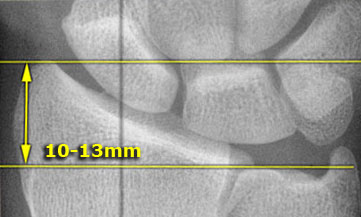
Radial length or height
Radial length is measured on the PA radiograph as the distance between one line perpendicular to the long axis of the radius passing through the distal tip of the radial styloid.
A second line intersects distal articular surface of ulnar head.
This measurement averages 10-13 mm.
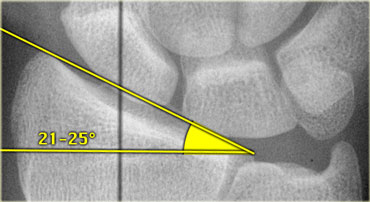
Radial inclination or angle
Radial inclination represents the angle between one line connecting the radial styloid tip and the ulnar aspect of the distal radius and a second line perpendicular to the longitudinal axis of the radius.
The radial inclination ranges between 21 and 25 degrees .
Loss of radial inclination will increase the load across the lunate.
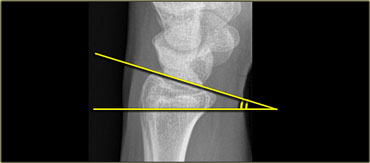
Radial tilt
Radial tilt is measured on a lateral radiograph.
The radial tilt represents the angle between a line along the distal radial articular surface and the line perpendicular to the longitudinal axis of the radius at the joint margin.
The normal volar tilt averages 11 degrees and has a range of 2-20 degrees .
Radiological Interpretation
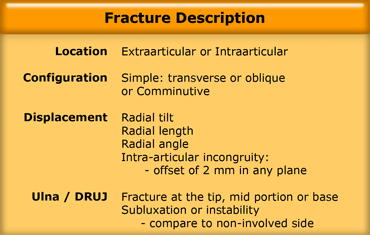
There are many ways to describe distal radial fractures and there are several classification systems.
In clinical practice however frequently eponyms like Colles' and Barton's are used.
When these epomyms are used, an accurate description of the fracture characteristics should always be included in the report(5).
In addition it should also be noted if there is osteoporosis or additional findings such as ligamentous injuries.
We will discuss the following:
- Description of the fracture characteristics (5)
- Desciption of the commonly used fracture eponyms
- Most popular classification systems
Location
One of the most important characteristics is whether a fracture is extraarticular or intraarticular.
Extraarticular fractures are usually less complicated, unless they are comminutive.
Intraarticular fractures either involve the radiocarpal joint, distal radioulnar joint, or both.
Configuration
Always mention whether the fracture is transverse (good prognosis), oblique or comminuted (multifragmented).
When a fracture is oblique or when it is comminuted with crossing of the mid axial line, it can be unstable.
On the left a patient with an extraarticular distal radius fracture.
Notice the oblique course on the lateral view.
Fractures with this configuration frequently show loss of reduction at follow up and need surgical treatment.
On the left a sagittal reconstruction of an oblique intraarticular fracture of the distal radius.
This is a volar Barton's type fracture.
Even in a cast the volar fragment will show progressive displacement at follow-up and a volar buttress plate is needed to hold the volar rim in place.
Displacement
Fractures are either displaced or nondisplaced.
A fracture with an offset of 2 mm or more in any plane or 2 mm offset involving the articular surface is considered displaced.
Displacement can be dorsal, volar, radial or proximal.
Axial shortening, radial inclination and radio-ulnar displacement can be measured on the routine posterior/anterior film.
Dorsal tilt and dorsal or palmar displacement can be measured on the routine lateral X-ray.
Fragment displacement and rotation may be further determined using CT.
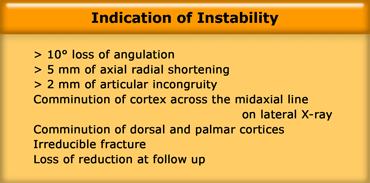
Instability
Instability is defined as a high risk of secondary displacement after initial adequate reduction.
Radiographic signs that favor instability are displacement and an oblique or comminuted configuration (as mentioned above).
These signs are listed in the table on the left.
Although the initial x-ray after reduction may look good, always look for loss of reduction at follow up.
Articular incongruity is the most important factor in the development of posttraumatic osteoarthritis of the wrist.
Ulna and Distal radioulnar joint (DRUJ)
Assessment of a wrist fracture must also include a description of the distal ulna and distal radioulnar joint (9).
The distal ulna articulates with the sigmoid notch of the radius.
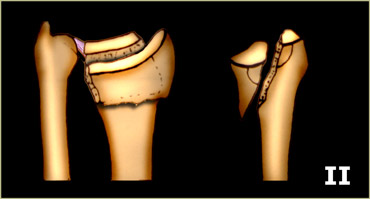
Type I: stable
Avulsion fractures of the tip of the ulnar styloid and stable fractures of the ulnar neck have a good prognosis.
Following reduction of the radius the DRUJ is congruent and stable.
Extraarticular unstable fractures however, require plate fixation.
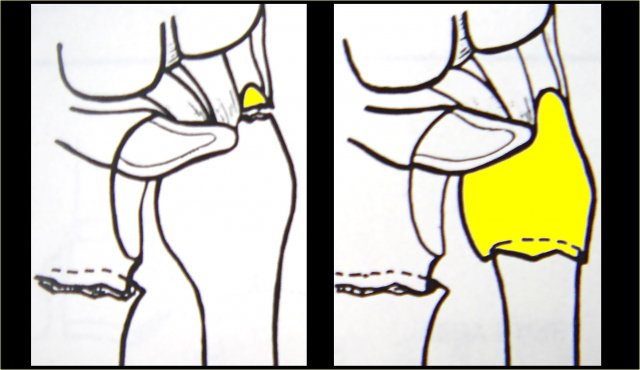
Type II: unstable
There is subluxation or dislocation of the ulnar head as a result of avulsion of the base of the ulnar styloid or tear of the TFCC and/or capsular ligaments.
The subluxation has to be reduced with closed or operative treatment to avoid chronic instability and arthosis.
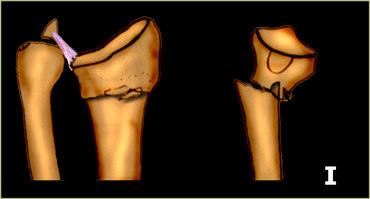
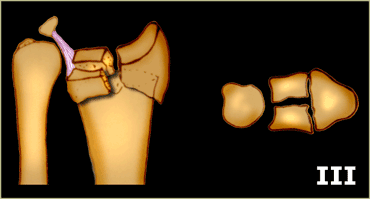
 Intraarticular fracture of sigmoid notch or ulnar headModified and reprinted with permission from reference (9)
Intraarticular fracture of sigmoid notch or ulnar headModified and reprinted with permission from reference (9)
Type III: potentially unstable
Intraarticular fractures of the sigmoid notch and intraarticular fractures of the ulnar head are potentially unstable because the incongruity of the DRUJ.
Subluxation is possible.
Common Fracture Eponyms
Colles' fracture
A Colles' fracture is a fracture of the distal metaphysis of the radius with dorsal angulation and displacement leading to a 'silver fork deformity'.
Colles fractures are seen more frequently with advancing age and in women with osteoporosis.
In many cases a Colles' fracture is an extraarticular, uncomplicated and stable fracture, but it can be intraarticular.
So look for signs of instability in all Colles' fractures, especially:
- Intraarticular radiocarpal or DRUJ extension of the fracture
- Radial shortening
- Loss of radial inclination
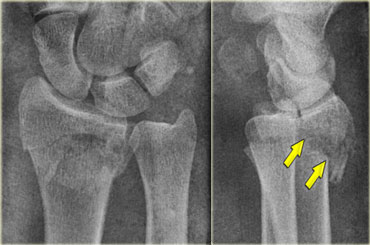
On the left a detailed AP view of the same patient as above.
In addition to the dorsal angulation seen on the lateral view, notice the following:
- Extension into the radiocarpal joint and the distal radioulnar joint
- Displacement of the articular fragments (blue arrow)
- Radial shortening and loss of radial inclination resulting in distal ulna abutting the lunate (yellow arrow)
- Fracture of ulnar styloid
Just calling this fracture a Colles' fracture would be insufficient.
All the characteristics have to be mentioned in the radiology report to convey the full extent of the injury, possible complications and treatment.
Smith's fracture
Smith's fractures occur in younger patients and are the result of high energy trauma on the volar flexed wrist.
Volar comminution and intraarticular extension are more common.
On the left an extraarticular Smith's fracture with palmar and radial angulation and displacement.
There is also an avulsion of the ulnar styloid process.
Barton's fracture
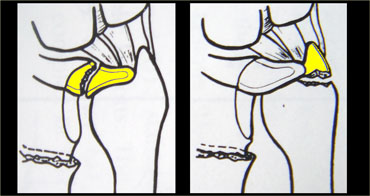
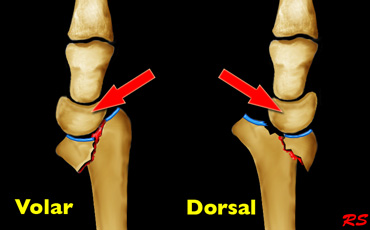
Volar-type Barton's is a fracture-dislocation of the volar rim of the radius.
This type is the most common.
Dorsal-type Barton's is a fracture-dislocation of the dorsal rim of the radius.
Dislocation of the radiocarpal joint is the hallmark of Barton's fractures.
These are shear type fractures of the distal articular surface of the radius with translation of the distal radial fragment and the carpus.
These fractures have a great tendency for redislocation and malunion.
They usually require operative treatment.
On the left a volar-type Barton's fracture.
The radiographic findings are the following:
- Comminuted intraarticular fracture of the distal radius
- Volar rim maintains relationship with the carpus and both are displaced proximally (blue arrow)
- Fracture of radial styloid process with loss of radial inclination (yellow arrow)
On the left a dorsal-type Barton's fracture.
The radiographic findings are the following:
- Comminuted intraarticular fracture of the distal radius
- Dorsal rim and carpus are displaced dorsally and proximally
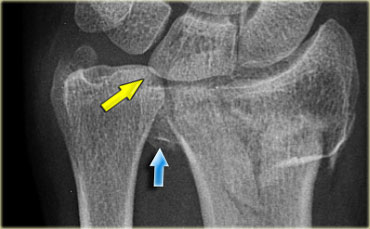
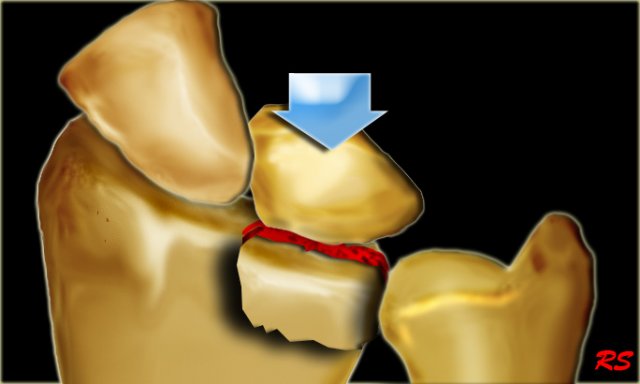
Die-punch fracture
A die-punch fracture is a depression fracture of the lunate fossa of the distal radius.
It is the result of a transverse load through the lunate.
The radiographic findings can be very subtle.
In many cases there is also a subtle proximal displacement of lunate, seen as a break in carpal arc I.
(see the article Wrist - Carpal instability).
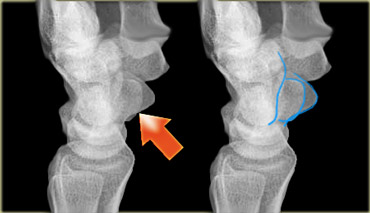
On the left a typical die-punch fracture.
The blue arrow indicates the depressed fragment of the lunate fossa.
Notice the articular step-off.
The yellow arrow indicates a subtle fracture of the radial styloid process.
There is no disruption of carpal arc I.
Notice that you can easily overlook such a fracture.
On the left two 3D-reconstructions of the same fracture as above.
Chauffeur's fracture
An isolated fracture of the radial styloid process is also called a Hutchinson's or chauffeur's fracture.
Displacement of the fragment is uncommon.
There can be associated injury to the scapholunate ligament.
In most cases a fracture of the radial styloid process is part of a comminutive intraarticular fracture.
Ulnar styloid process fracture
An ulnar styloid process fracture is usually associated with radial fractures and rarely isolated.
An isolated fracture of the tip is clinically insignificant.
Displaced fractures of the base are usually associated with TFC tears and can be associated with instability of the distal radioulnar joint (DRUJ).
On the left a subtle fracture of the tip of the ulnar styloid process (blue arrow) in a patient with a volar Barton's fracture.
Notice the depression of the volar rim.
Fractures in Children
Torus fracture
Torus fractures, or buckle fractures, are extremely common injuries in children.
Because children have softer bones, one side of the bone may buckle.
The word torus is derived from the Latin word 'Tori' meaning swelling or protuberance.
These injuries tend to heal much more quickly than the similar greenstick fractures.
Green stick fracture
These are partial fractures, since only one part of the bone is broken and the other side is bent.
The name is derived from an analogy of breaking a young, fresh tree branch.
Most often the greenstick fracture must be bent back into the proper position.
Greenstick fractures can take a long time to heal because they tend to occur in the middle, more slowly growing parts of bone.
Epiphysiolysis fracture
These are usually Salter Harris type II epiphysiolysis fractures.
Restorage of the anatomical situation is necessary to prevent growth disturbances.
Redislocation is common after closed reduction.
In many cases they need percutaneous pinning.
Classification systems
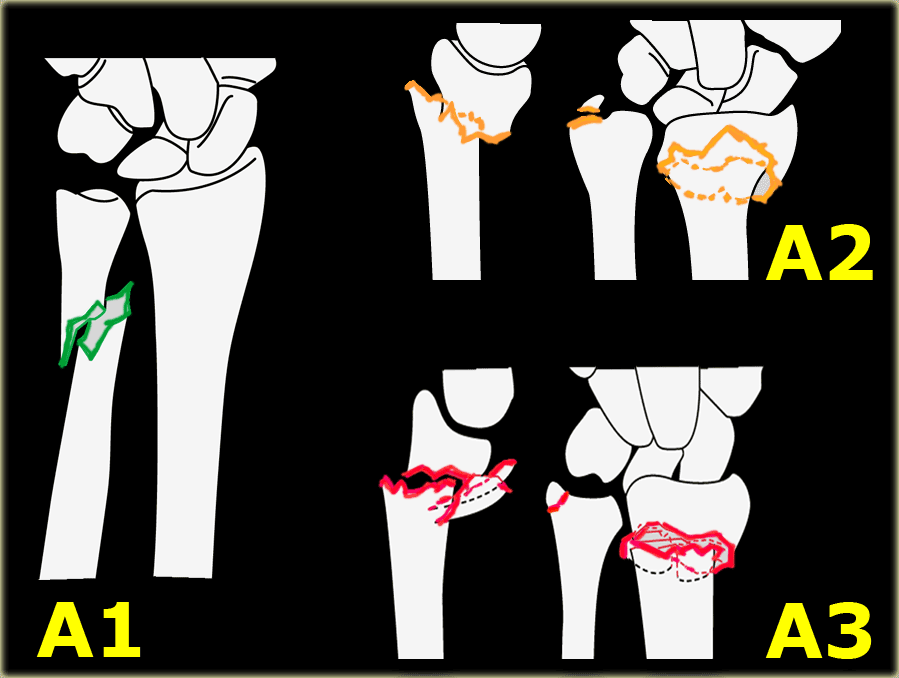
Muller AO-classification
The Muller AO-classification is adapted by the Orthopaedic Trauma Association.
In reference (6) a link is provided to download the illustrations of the Muller AO Classification of Fractures.
A = extra-articular fracture
- A1 = ulna, radius intact
- A2 = radius, simple and impacted
- A3 = radius, multifragmentary
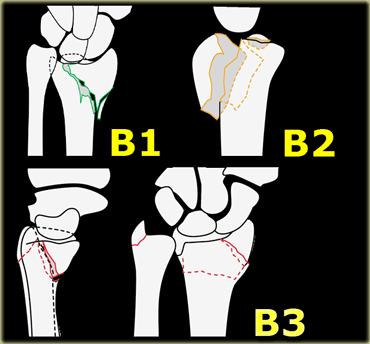
B = partial articular fracture
- B1 = radius, sagittal
- B2 = radius, frontal, dorsal rim
- B3 = radius, frontal, volar rim
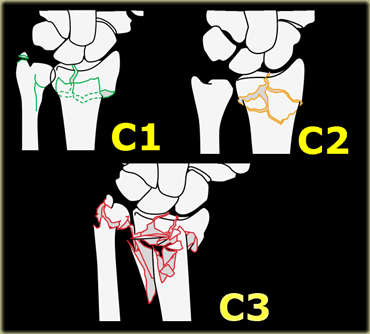
C = complete articular fracture of radius
- C1 = articular simple, metaphyseal simple
- C2 = articular simple, metaphyseal multifragmentary
- C3 = articular multifragmentary
Fernandez Classification
This classification is popular, since it addresses the mechanism of injury and the consequent treatment options.
Instability is defined as a high risk of secondary displacement after initial adequate reduction.
Associated traumatic lesions are ligamentous rupture, nerve compression and compartment syndrome.
Type 1 : Bending fracture
- Mechanism: one cortex of the metaphysis fails due to tensile stress and the opposite undergoes a certain degree of comminution.
- Stability: can be stable or unstable
- Displacement pattern: non-displaced, dorsal (Colles') or volar (Smith's fracture)
- Number of fragments: two main fragments
- Associated lesions: uncommon
- Recommended treatment: usually conservative, when unstable:percutaneous pinning or external fixation
Type 2 : Shearing fracture
- Mechanism: fracture of the joint surface (i.e. volar and dorsal Barton's, radial styloid process fractures, simple articular fracture)
- Stability: unstable
- Displacement pattern: dorsal, volar or radial
- Number of fragments: two-part, three-part or comminuted
- Associated lesions: less common
- Recommended treatment: open reduction with screw- or plate fixation
Type 3 : Compression fracture
- Mechanism: compression fracture of the joint surface with impaction of subchondral and metaphyseal bone (i.e. die-punch fracture or intraarticular comminuted fracture
- Stability: stable or unstable
- Displacement pattern: non-displaced, dorsal, volar or radial
- Number of fragments: 3- or 4-part or comminuted
- Associated lesions: common
- Recommended treatment:
- closed
- limited arthroscopic assisted
- extensile open reduction
- percutaneous pins combined with external and internal fixation
- bone graft
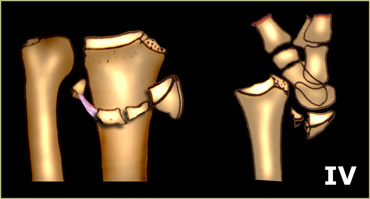
Type 4 : Avulsion fracture
- Mechanism: avulsion fracture usually associated with ligamentous injury
- Stability: unstable
- Displacement pattern: dorsal, volar, radial or proximal
- Number of fragments:
- 2-part: radial styloid, ulnar styloid
- 3-part: volar, dorsal margin
- comminuted
- Associated lesions: frequent ligamentous injury
- Recommended treatment: closed or open reduction with pin or screw fixation or tension wiring
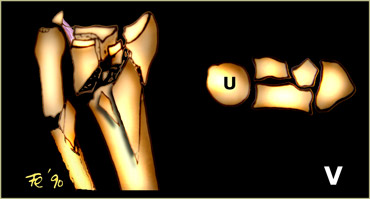
Type 5 : Combined fractures
- Mechanism: combination of forces of type I-IV as a result of high velocity injuries
- Stability: unstable
- Displacement pattern: dorsal, volar, radial or proximal
- Number of fragments: comminuted
- Associated lesions: always present
- Recommended treatment: combined method
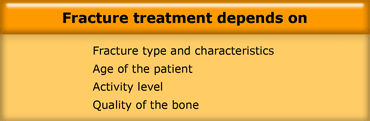
Treatment
The treatment decision of a distal radius fracture is complex and depends on the type of the fracture, the age and activeness of the patient and the quality of the bone.
At one extreme a stable, undisplaced extra-articular fracture has an excellent prognosis.
At the other an unstable, displaced intra-articular fracture is difficult to treat and has a poor prognosis.
If the alignment of the bones is not acceptable, they need to be reduced by closed or open reduction.
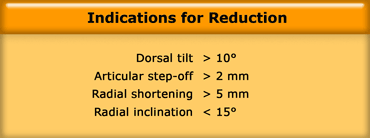
Indications for Reduction in Distal Radius Fractures
Many authors suggest that distal radial fractures be reduced anatomically, but the real question is 'what is acceptable and what is not?'.
Based on basic science and clincal studies some of the recommendations of the International Distal Radius Fracture Study Group are presented in the table on the left, although these recommendations are still the subject of ongoing debate (5).
Closed Reduction
The initial treatment for most radius fractures is closed reduction and plaster immobilization.
A displaced fracture is reduced under regional or general anaesthetic.
First the arm is placed under traction to unlock the fragments.
The deformity is then reduced with appropriate closed reduction, depending on the type of deformity.
A splint or cast is placed in such a way that the risk of re-displacement is minimized.
X-rays are taken to ensure that the reduction was successful.
The cast is usually maintained for about 6 weeks.
Guidelines for non-acceptable reduction are (8):
- Radial shortening > 5 mm
- Radial inclination Tilt on lateral projection > 10 degrees dorsal tilt and > 20 degrees volar tilt
- Intra-articular step-off 2 mm or more
- Articular incongruity 2 mm or more of the sigmoid notch (articular surface of distal radius in DRUJ).
On the left a control radiograph made after reduction.
The reduction was unsuccessful, because there is a dorsal tilt > 10 degrees , loss of inclination and radial shortening.
Surgical treatment
Although in most cases closed reduction is attempted, surgical intervention is required when there is failure to obtain or maintain closed reduction.
40% of distal radial fractures are considered to be unstable and require surgical fixation.
Many techniques of fixation are now available, including percutaneous pinning, intramedullary pinning, external fixation, and internal fixation with customized implants, including the Distal Volar Radius (DVR) system.
Surgical fixation allows almost immediate mobility.
Ultimately less stiffness and greater function is possible.
On the left a post-operative image of a Salter-Harris II fracture, which is held in place with two pins after closed reduction.
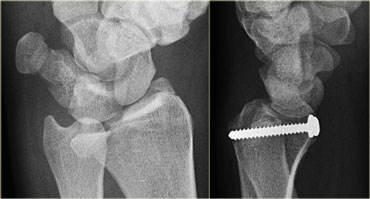
On the left a patient with a die-punch fracture, nicely shown on an oblique radiograph.
The fracture fragment of the lunate fossa was replaced and fixated with a screw.
Volar buttress plate
Barton's fractures are rarely successfully treated with closed reduction due to the shearing nature of the injury.
A volar buttress plate is the treatment of choice.
Comminution or osteoporotic bone make external fixation the preferred surgical treatment option.
On the left an intraarticular fracture of the distal radius with shortening of the radius.
The ulna abutts the lunate.
External fixation was used to lengthen the radius.
On the left a patient with a dorsal Barton's fracture (shown before).
After closed reduction the position of the dorsal rim is better, but this still is an unstable situation.
Volar plates were used with screws to lock the dorsal rim.
The volar approach was chosen, because this is an easier approach.
Final result after one of the plates has been removed.
Complications
Malunion
Non-union is uncommon in distal radial fractures, since there is excellent vascularisation of this region.
Malunion however is a common complication and is related to radial shortening, angulation and incongruity of the articular surface.
This results in malfunction and early osteoarthritis.
More than 2 mm incongruity of articular surface is the most important factor in the development of posttraumatic osteoarthritis of the wrist.
On the left a patient with malunion.
The radial shortening results in the ulna abutting the lunate.
Notice the loss of radiocarpal joint space indicating osteoarthritis.
Closed reduction is frequently unsuccessful when the fracture has an oblique course or when the fracture is comminutive.
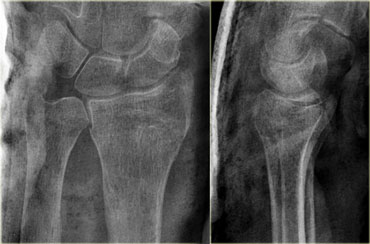
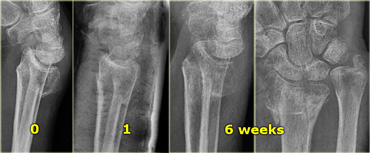
On the left a patient with an intraarticular fracture with dorsal tilt (i.e. intraarticular Colles' fracture).
On the lateral radiograph at presentation there is an extreme dorsal tilt.
After closed reduction and at follow up after one week, there is an acceptable tilt.
Finally at 6 weeks follow-up, there is malunion with extreme dorsal tilt, radial shortening and loss of inclination.
The ulna abutts the lunate.
The final result will be malfunction, radiocarpal and distal radioulnar osteoarthritis.
Risks specific to cast treatment relate to the potential for compression of the swollen arm causing compartment syndrome or carpal tunnel syndrome.
Reflex sympathetic dystrophy and median nerve injury are uncommon complications.
Complications associated with plating include tendon irritation or rupture and the need for plate removal.
On the left another patient with malunion and osteoarthritis.
There is also scapholunate dissociation as a result of associated ligamentous rupture with volar tilt of lunate indicating volar flexion instability (VISI).
On the left another patient after unsuccessful treatment.
There is loss of radial inclination and radial shortening, dorsal tilt and an articular step-off.