Contrast-enhanced MRA of peripheral vessels
Tim Leiner
Department of Radiology, Maastricht University Hospital
Publicationdate
Contrast-enhanced MR angiography (CE-MRA) is more sensitive and specific for diagnosis and preinterventional work-up of Periferal Arterial Disease (PAD) compared to Duplex (1).
CE-MRA detects more patent arteries than IA-DSA in patients with chronic critical ischemia and can modify the choice of therapeutic strategy in these patients (2).
It is important to distinguish between patients with intermittend claudication and patients with chronic critical ischemia because they need a different imaging approach.
In this overview guidelines are given how to tailor the MRA-examination by optimizing the use of surface coils, k-space filling, spatial resolution and contrast delivery.
by Tim Leiner
Department of Radiology, Maastricht University Hospital, the Netherlands
Periferal Arterial Occlusive Disease
 Patient with intermittend claudication on the left and an isolated stenosis in the left iliac artery.
Patient with intermittend claudication on the left and an isolated stenosis in the left iliac artery.
Intermittend claudication
Intermittend claudication is a benign form of periferal arterial occlusive disease.
Typically these patients have 'single level' disease usually an isolated stenosis in the iliac or femoral artery.
Mostly these patients are treated with risk factor management and exercise training.
There is only a relative indication for invasive therapy in order to relief the symptoms ( usually PTA, sometimes surgery).
Only a limited number of these patients will progress to more severe disease i.e. critical ischemia.
When MRA is performed in these patients perfect imaging of lower leg and feet is not the issue since no surgeon will perform a infragenual procedure in patients with these complaints.
A one-step examination from aorta to the lower leg will usually be sufficient and venous filling is usually no issue.
Chronic critical ischemia
In patients with chronic critical ischemia
however, there is rest pain and/or tissue loss.
They typically have 'multi level' disease with bilateral, severe stenoses or occlusions in multiple arteries and segments.
In critical ischemia there is an absolute indication for invasive therapy.
The goal is wound healing and limb saving.
In these patients it is the job of MRA to find patent arteries in the lower leg or feet for bypass surgery with or without PTA.
The utmost attempt must be made to find vessels in the lower legs and feet because if no arteries are found amputation will be unavoidable in most cases.
A two-step examination is necessary. First you have to focus on the lower leg and feet with the best spatial resolution possible. Secondly the iliac and femoral level can be imaged. Venous enhancement from the first serie will usually not be a problem at these levels.
How to optimize the Imaging Protocol
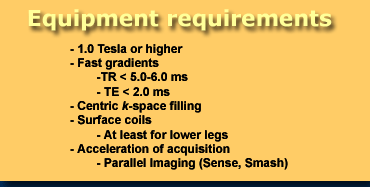
Equipment requirements
Centric k-spacing provides the capability to acquire the optimal part of the central k-space during the arterial-phase of contrast enhancement in a short time-period. The remaining time is used for increasing spatial resolution. Venous enhancement will not be of much of a problem because if the outer k-space is filled with data this does not add much to the contrast in the image.
The arterio-venous (AV) window will be enlarged allowing longer scan time. If centric k-space filling is not available use linear k-space filling (see tips and tricks).
Surface coils
Although some advocate the use of the bodycoil for imaging all three station, surface coils will dramatically improve image quality. Especially t in the lower leg and feet a surface coil is mandatory.
a 3-station coil is optimal for MRA from the aorta to the feet. If not available use as many surface coils as possible. Synergy body and synergy spine coils are very helpfull,
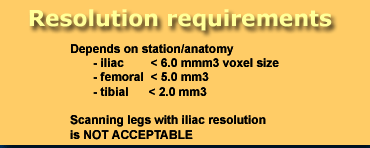
Spatial resolution
As a rule of thumb you need at least 3 pixels per vessel-diameter in order to reliably differentiate between 50% stenosis.
So at different stations a different spatial resolution is needed (figure).
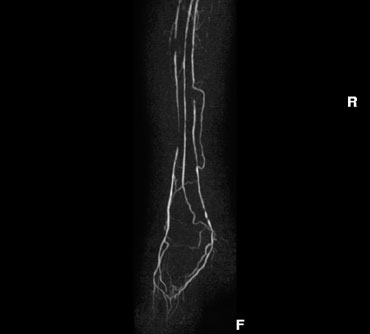
 Sagittal MIP of TOF-series from aorta to the level of the feet. Variation in width and angulation will result in a better coverage at the different levels.
Sagittal MIP of TOF-series from aorta to the level of the feet. Variation in width and angulation will result in a better coverage at the different levels.
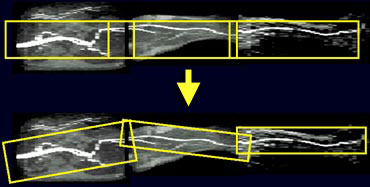
Planning the series
The CE-MRA series can be planned on a rough TOF-serie that gives you a good idea where the vessels of interest are located.
Do not use the same box for every station, but adapt the size and the angulation of the boxes at iliac, femoral and crural level. Especially at the femoral level a small box usually is sufficient. This will save time and allows you to speed up going to the lower leg.
At the crural level especially if the pedal arch has to be included a large box will be needed. The spatial resolution at this level has to be high. This results in more thin slices and a longer scan time. How to beat venous enhancement in the lower leg when there is a longer scantime is explained later.
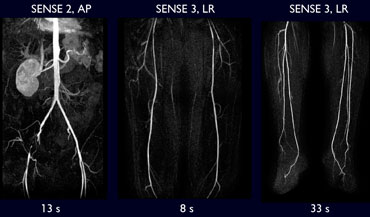 Three station CE-MRA in patient with intermittent claudication. Fast scanning was possible with SENSE.
Three station CE-MRA in patient with intermittent claudication. Fast scanning was possible with SENSE.
Contrast bolus-timing
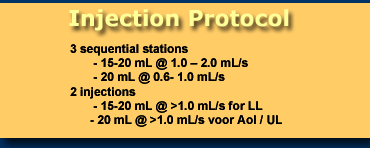
Injection protocol
In patients with intermittent claudication a one-step examination with imaging of 3 sequential stations is optimal.
In patients with critical ischemia first the lower legs with the pedal arch included are examined. Secondly a separate contrast injection is necessary for the examination of the Aorto-Iliac and Femoral station. Depending on the speed of the MR-system contrast can be delivered at a higher rate.
Tips and Tricks in MRA
How to beat venous enhancement in lower legs
1. Prolong the arterio-venous (AV) window by venous compression. Use a midfemoral compression with a pressure cuff at 50-60 mmHg. A normal blood pressure cuff without the metal parts usually works fine.
2. Use centric k-space filling if available. If ontrast appears in the veins, this will not add much to the contrast in the image as at that moment the periferal lines of k-space are scanned, which mostly add to he resolution in the image.
3. In patients with critical ischemia do a biphasic examination to concentrate first on lower leg and feet.
Centric k-spacing not available
At the iliac level centric k-spacing is not necessary. Linear filling of k-space works good at this level and provides the advance that the sequence can be started in front of the arrival of the contrast-bolus.
If centric k-spacing is not available at your MR-machine, use linear filling of k-space at all levels. At the level of the lower leg and feet the arterial contrast in the images will be less optimal and the risk of venous enhancement will be greater.
3-station coil not available
A 3-station coil is optimal for MRA from the aorta to the feet. If not available use as many surface coils as possible. Synergy body and synergy spine coils are very helpfull,
Use the best surface coil that you have for imaging the lower leg and feet and consider to do a biphasic examination.
Problems with breath-hold
The most important issue in MRA of the aorta and iliac arteries is that the patient manages to hold his breath. A lower resolution breath-hold scan is superior to a higher resolution scan with breathing artifacts.
Before the actual series start you need to practise the breath-hold with the patient. If adequate breath-hold is not possible than you have shorten scantime by lowering the matrix-size and increasing the slice thickness at the expense of in-plane resolution.