Non-Meniscal pathology
David Rubin and Robin Smithuis
Radiology department of the Washington University School of Medicine, St. Louis, USA and the Rijnland hospital in Leiderdorp, the Netherlands
Publicationdate
This article is based on a presentation given by David Rubin and adapted for the Radiology Assistant by Robin Smithuis.
This review focusses on all the non-meniscal pathology of the knee.
See the article entitled Knee MRI - meniscal pathology for the pathology of the meniscus.
Interactive cases are presented in the menubar.
by David Rubin and Robin Smithuis
Ligaments
Anterior Cruciate Ligament
The ACL has interesting anatomy. It is an intra-articular structure, but it is extra-synovial.
The synovium folds over the ligament. So at arthroscopy they look through the synovium.
Sometimes when there is a tear ,the synovium layer is intact and only a hemorrhagic ACL is seen.
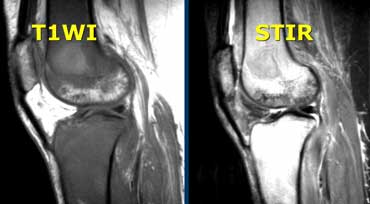
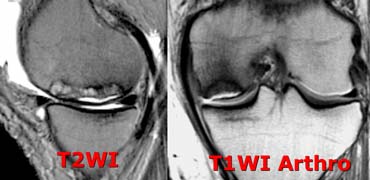
The ACL is composed of 3-5 layers of fibers. Between the fibers there can be fat or synovium or sometimes a little bit of fluid. This explains why the ACL is not black on PD-images.
Do not look at the ACL on PD-images because this may give a false impression of pathology.
Only look at the ACL on T2W-images and even on these images the ACL does not have to be entirely black.
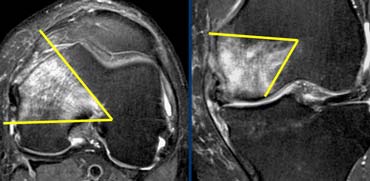
Criteria for the normal ACL are:
- Fiber-orientation as steep or steeper than the intercondylar roof.
- Fibers all the way from the tibia to the femur.
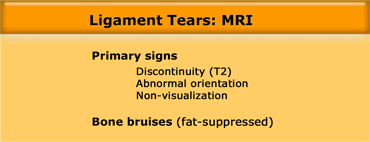
So on MR the primary signs of a tear are: discontinuity on T2, abnormal orientation or non-visualisation.
Many secondary signs of tears have been described, but these are not helpfull, since we have to rely on direct visualisation of the ligament.
Only bone bruises can be a helpfull secondary sign.
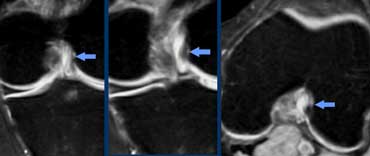
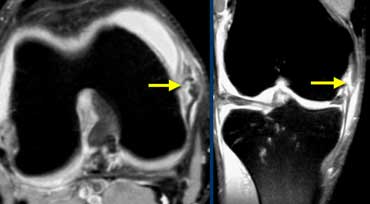
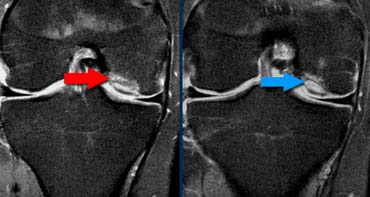
Notice that on coronal and axial images fibers of the ACL are right next to the bone of the intercondylar notch (arrows).
There should never be any fluid between these ACL-fibers and the bone of the lateral condyle ('empty notch sign').
Also notice that the PCL is also composed of many fibers.
Anterior Cruciate Ligament (2).
The case on the left shows a ligament that's too flat and we see disrupted fibers so there is abnormal orientation and discontinuity.
Based on these images we cannot differentiate between complete tear, high grade partial tear or partial tear.
MRI does not accurately differentiate between partial or complete ACL tear.
But yes we can differentiate between high grade or low grade injury.
A high grade injury is 'not able to see 50% of the fibers'.
So if the othopaedic surgeons operate on a high grade injury, they will either find a totally torn ACL or a high grade partial tear, that needs to be repaired.
On the other hand if most of the fibers appear to be intact on MR indicating a low grade ACL tear, they will find an intact or partially torn ACL, that is stable and doesn't need any treatment.
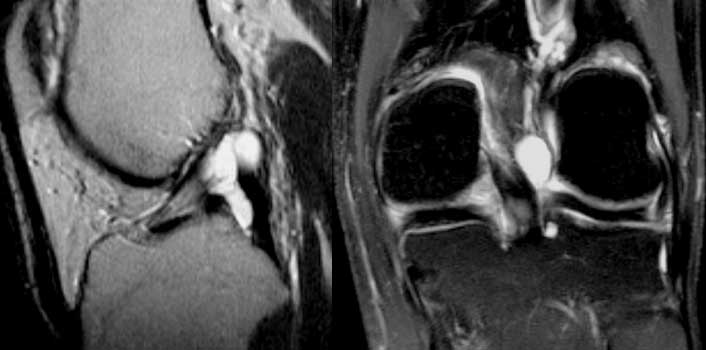
 LEFT: ACL-tear with bone bruises on lateral side. RIGHT: Anterior condyle hits the posterior part of the tibia. ACL torn due to stretching.
LEFT: ACL-tear with bone bruises on lateral side. RIGHT: Anterior condyle hits the posterior part of the tibia. ACL torn due to stretching.
Anterior Cruciate Ligament (3).
Bone bruises appear in a very typical location indicating the dislocation, that was the cause of the ACL-tear.
Anterior Cruciate Ligament (4)
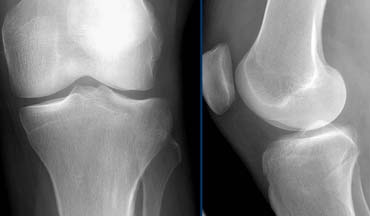
On X-rays an important indirect sign of an ACL-tear is a Segond fracture.
Difficult to see on MR, but much more easy to see on radiographs.
A Segond fracture is an avulsion fracture at the attachment of the lateral collateral band due to internal rotation and varus stress.
In 75-100% there will also be a tear of the ACL.
The unhappy triad or O'Donoghues syndrome is a different combination of injuries.
The unhappy triad injury commonly occurs in contact sports such as football when the knee is hit from the outside.
This causes an injury to three knee structures:
- ACL tear
- MCL tear (medial collateral ligament)
- Medial meniscal tear
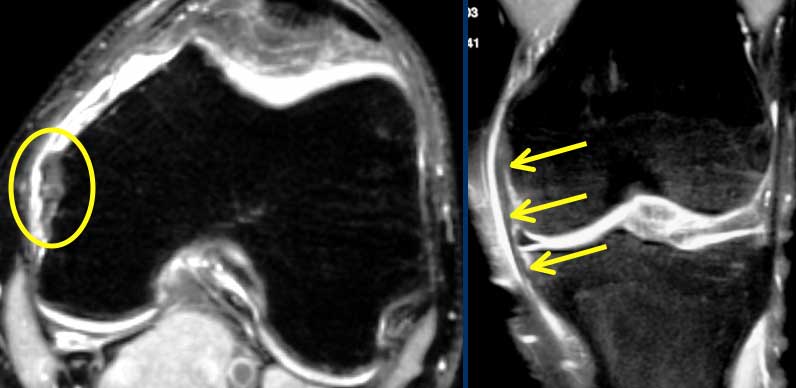
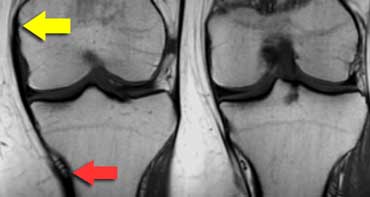
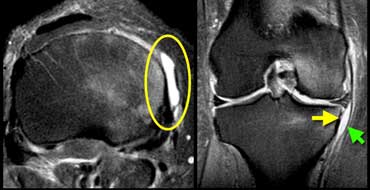
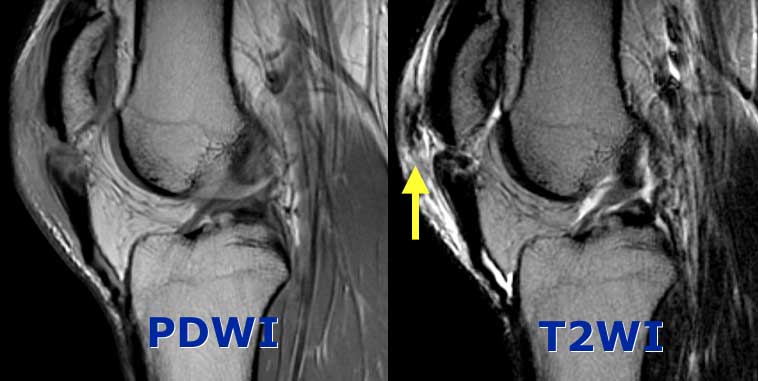
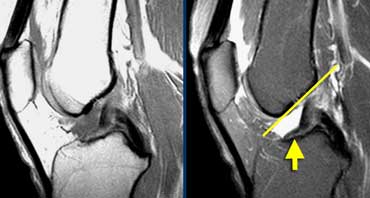 Torn ACL. ACL fibers are too flat (yellow arrow) compared to intercondylar roof (Blumensaat's line).
Torn ACL. ACL fibers are too flat (yellow arrow) compared to intercondylar roof (Blumensaat's line).
Anterior Cruciate Ligament (5)
Case on the left shows a torn ACL.
Fibers have an abnormal orientation (too flat).
Yet it is difficult to see if these are attached to the femur.
The acute angulation in the ligament is due to fact that the ACL and PCL have scarred together (see below).
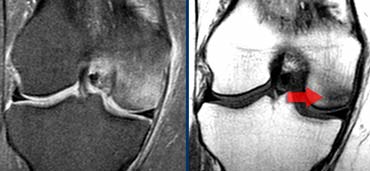
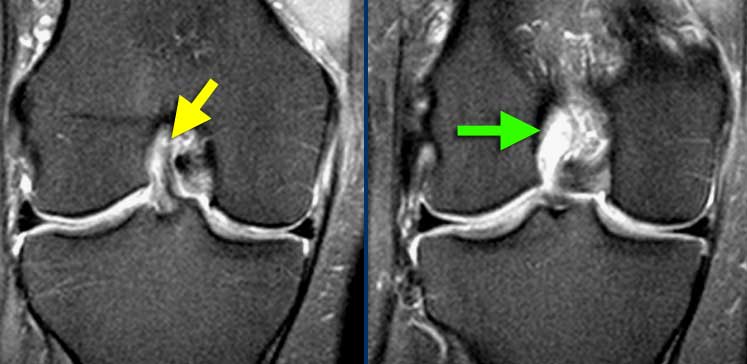 LEFT: ACL-fibers have a normal orientation but do not connect to femurcondyle. RIGHT: Empty notch sign: fluid against the interior part of the lateral condyle
LEFT: ACL-fibers have a normal orientation but do not connect to femurcondyle. RIGHT: Empty notch sign: fluid against the interior part of the lateral condyle
Sometimes it is easier to see whether these fibers are attached in the coronal plane.
Against the interior part of the lateral condyle there never should be fluid.
If this is the case it is called the 'empty notch sign' indicating that the ACL is torn from it's attachment to the femur.
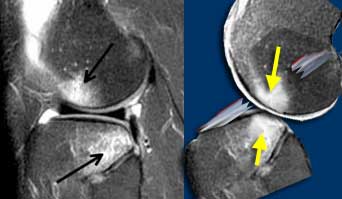
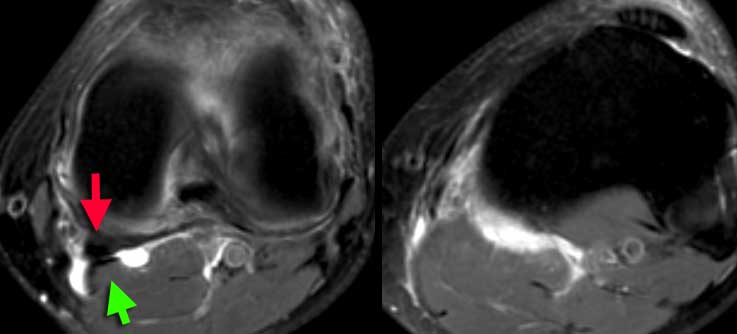
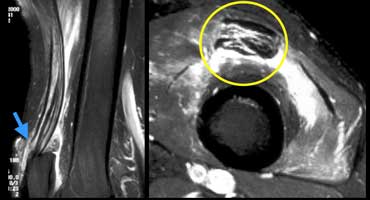
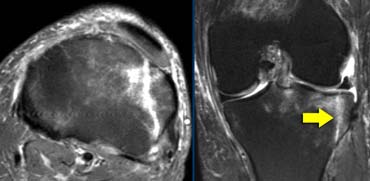
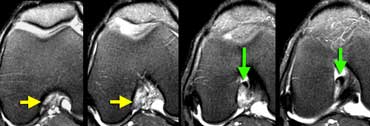 In the axial plane there is an empty notch sign (yellow arrows) where there should be ACL attached to the condyle. At a lower level (going right) the torn ACL is scarred to the PCL (green arrows)
In the axial plane there is an empty notch sign (yellow arrows) where there should be ACL attached to the condyle. At a lower level (going right) the torn ACL is scarred to the PCL (green arrows)
Also in the axial plane there should be ligament next to the condyle.
At a lower level we see the torn ACL attached to the posterior cruciate ligament.
They have scarred together.
This is a very common appearance of a chronic ACL tear.
This scarring leads to the acute angulation of the ligament.
Even though the ACL is connected to the PCL it is not strong enough and still needs reconstruction.
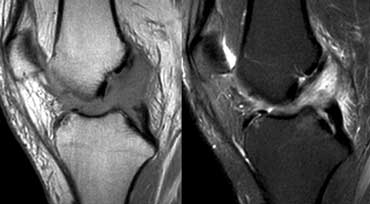 ACL Mucoid degeneration. This patient had an operation for another reason and the surgeons called it normal because it looks normal.
ACL Mucoid degeneration. This patient had an operation for another reason and the surgeons called it normal because it looks normal.
Anterior Cruciate Ligament (6)
Case on the left shows a non-visualisation of the ACL on a PD-image. But the lesson is 'do not look at ligaments on a PD-image'.
If you want to judge the ACL-ligament look at the T2W-images.
The T2W-images show fibers going all the way from the tibia to the femur with a normal orientation. So the ACL is intact.
This is a case of mucoid degeneration. Normally between the ACL-fibers there can be synovium or fat.
In normal aging that can change into gelatinous material.
This has no effect on the strenght of the ACL.
 ACL Mucoid degeneration with cyst-formation (intra-osseus ganglion). Mucoid material is squeezed from between the ACL-fibers into the bone. At arthroscopy ACL and bone looked normal.
ACL Mucoid degeneration with cyst-formation (intra-osseus ganglion). Mucoid material is squeezed from between the ACL-fibers into the bone. At arthroscopy ACL and bone looked normal.
Anterior Cruciate Ligament (7)
Another case of ACL Mucoid degeneration.
Often this is associated with cyst-formation in the bone.
You could call it ganglion cyst, but you could also call it normal because it has no clinical meaning.
This is part of normal aging.
Anterior Cruciate Ligament (8)
Case on the left shows cyst seperate from ACL unlike mucoid degenaration.
This is a ganglion cyst. Probably also a form of degeneration.
The difference with Mucoid degeneration is that these cysts can be symptomatic.
Sometimes these cysts will drained under ultrasound guidance.
Be sure to use a very large needle, because it is very thick material.
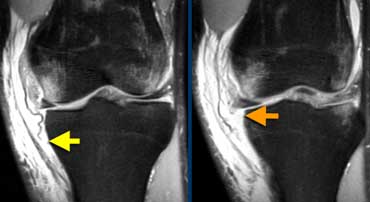
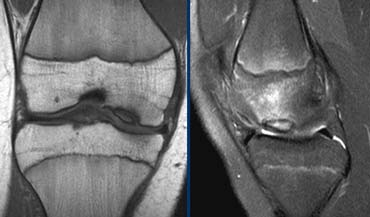
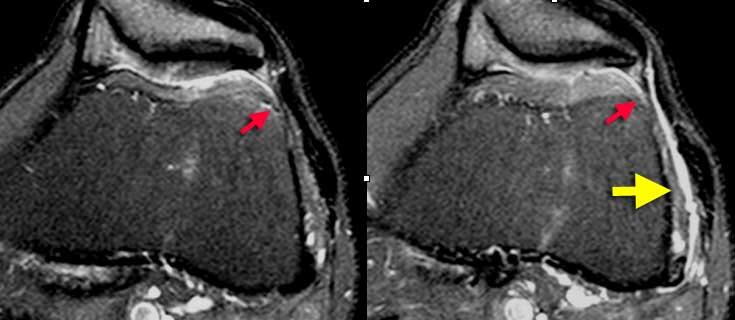
 Acute PCL-tear: In the coronal and axial plane most of the fibers are gone so it's a high grade tear.
Acute PCL-tear: In the coronal and axial plane most of the fibers are gone so it's a high grade tear.
Posterior Cruciate Ligament
We use the same criteria for all the other ligaments in the body.
The case on the left shows a high grade PCL tear.
 MCL from medial epicondyle (yellow arrow) to below the inferomedial geniculate vessels (red arrow) about 7 centimetres below the joint space.
MCL from medial epicondyle (yellow arrow) to below the inferomedial geniculate vessels (red arrow) about 7 centimetres below the joint space.
Medial collateral ligament
The superficial medial collateral ligament (MCL) extends from the medial epicondyle to insert not just near the joint but 7 cm below the joint space.
At that point there are three landmarks: the inferomedial geniculate artery and paired veins (figure).
The deep part of the MCL, even when it is normal, you may not be able to see.
It is closely applied to the medial meniscus and the superficial MCL.
Medial collateral ligament (2)
The case on the left shows a Grade I sprain of the medial collateral ligament.
Medial collateral ligament (3)
The case on the left shows a Grade II sprain of the medial collateral ligament.
Medial collateral ligament (4)
The case on the left shows a superficial MCL that is torn from it's attachment on the tibia.
Remember it should be attached 7 cm below the joint line.
Deep MCL is also torn the ligament is absent.
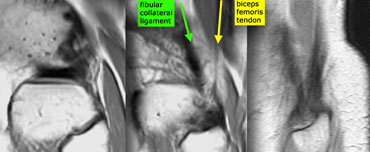 Posterolateral corner anatomy from medial to lateral on sagittal images. Fibular collateral ligament (green) and Biceps femoris tendon (yellow) form a letter V and insert as conjoined tendon on fibular head.
Posterolateral corner anatomy from medial to lateral on sagittal images. Fibular collateral ligament (green) and Biceps femoris tendon (yellow) form a letter V and insert as conjoined tendon on fibular head.
Posterolateral Corner injury
Normal anatomy
Posterolateral corner contains seven or eight structures.
Only three of them are important to us because they are visible on MR and because the surgeon might want to fix them.
These structures are:
1. Fibular collateral ligament
2. Biceps femoris muscle and tendon.
3. Popliteal tendon
The fibular collateral ligament together with the tendon of the biceps femoris form the letter V on sagittal images.
They inserts on the fibulahead as the conjoined tendon.
Posterolateral corner injury (2)
On the left a football player, who was hit in the front part of the knee.
The image on the far left shows a bone bruise anteromedially.
So you suspect ligamentous injury on the contralateral side, which is the posterolateral corner.
The next image shows a normal popliteus tendon but biceps femoris tendon is not attached to the fibula.
 LEFT: distal rupture of fibular collateral ligament.RIGHT: biceps femoris tendon and collateral ligament do not attach.
LEFT: distal rupture of fibular collateral ligament.RIGHT: biceps femoris tendon and collateral ligament do not attach.
On the left more images of the same patient located more anteriorly.
The fibular collateral ligament has a normal proximal attachment but is not attached to the fibula.
On a sagittal plane there is a gap between biceps femoris tendon and collateral ligament on one side and the fibular head on the other.
These findings indicate a conjoined tendon rupture.
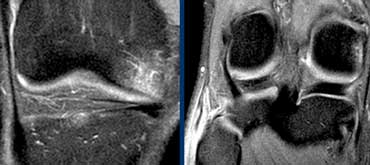
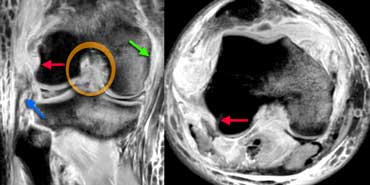 LEFT: cruciate lig.rupture (orange), med coll lig rupture (green), proximal rupture of the fibular collateral ligament (blue).RIGHT: no attachment of popliteus tendon (red arrows)
LEFT: cruciate lig.rupture (orange), med coll lig rupture (green), proximal rupture of the fibular collateral ligament (blue).RIGHT: no attachment of popliteus tendon (red arrows)
Posterolateral corner injury (3)
On the left PD-fatsat images after severe injury.
There are bone bruises and many ligaments are ruptured.
There is a posterolateral corner injury with proximal rupture of the fibular collateral ligament.
There is also a rupture of the popliteus tendon because it is not attached proximally.
Cysts, Bursae and Recesses
 LEFT: popliteal cyst originating between semimembranosus tendon (red arrow) and gastrocnemius muscle and tendon (green arrow).RIGHT: ruptured popliteal cyst with fluid tracking down the muscles.
LEFT: popliteal cyst originating between semimembranosus tendon (red arrow) and gastrocnemius muscle and tendon (green arrow).RIGHT: ruptured popliteal cyst with fluid tracking down the muscles.
There are about 12 named bursae and recesses in the knee.
Some very common and others uncommon.
These are synovial lined structures.
The most common recess is the popliteal or Baker's cyst.
The origin is between the semimembranosus and gastrocnemius tendon.
Prepatellar bursitis
On the left the typical imaging findings of prepatellar bursitis.
Deep infrapatellar bursitis
An uncommon form of bursitis is the deep infrapatellar bursitis.
Sometimes associated with Osgood-Schlatter.
 Medial collateral ligament bursitis located between the deep MCL (yellow arrow) and the superficial MCL (green arrow).
Medial collateral ligament bursitis located between the deep MCL (yellow arrow) and the superficial MCL (green arrow).
These bursae are all named by the structures next to them.
So a bursitis of the bursa between the deep MCL and the superficial MCL is called a medial collateral ligament bursitis.
 Iliotibial Band Friction syndrome: no fat between iliotibial band (yellow arrow) and the lateral condyle.
Iliotibial Band Friction syndrome: no fat between iliotibial band (yellow arrow) and the lateral condyle.
Cysts, Bursae and Recesses (2)
Adventitial bursae are bursae, that are formed in places where normally there is no bursa>
The bursa is formed due to abnormal friction.
Iliotibial Band Friction syndrome
A common place for abnormal friction is between the iliotibial band and the lateral condyle in speedwalkers, bicyclists and sometimes runners.
When a bursa is formed in this location it is called the 'Iliotibial Band Friction syndrome'.
On the left a speedwalker with lateral knee pain.
Between iliotibial band and the lateral condyle there should be fat, but in this case it is missing.
 Iliotibial Band Friction syndrome : Fluid within a bursa is seen between the iliotibial tract and the femur (yellow arrows). Joint fluid stops at the red arrows.
Iliotibial Band Friction syndrome : Fluid within a bursa is seen between the iliotibial tract and the femur (yellow arrows). Joint fluid stops at the red arrows.
Same patient. On axial images fluid within a bursa is seen between the iliotibial tract and the underlying femur.
Sometimes fluid in this location has to be differentiated from joint fluid.
You have to look at all the images.
In this case the joint fluid stops at the red arrows.
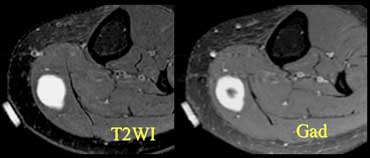
Remember that not everything that's bright on a T2W-image is fluid.
You have to be suspicious, if there is something, that looks like a fluid collection, but it is not in a location, where there normally is a bursa, cyst or recess.
Give Gadolineum to differentiate cystic from solid.
Quadriceps and Patellar tendon
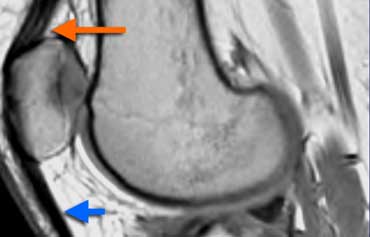 Normal Extensor mechanism: The quadriceps tendon comes in three layers (orange arrow). Patellar tendon (blue arrow) and quadriceps tendon have a sharp posterior demarcation.
Normal Extensor mechanism: The quadriceps tendon comes in three layers (orange arrow). Patellar tendon (blue arrow) and quadriceps tendon have a sharp posterior demarcation.
Normal Extensor mechanism
The extensor mechanism of the knee is composed of the quadriceps muscle and tendon, the patella and the patellar tendon.
The quadriceps tendon is made of four tendons but comes in three layers on sagittal images.
It has a broad attachment all the way from the front of the patella almost to the back.
The tendons of the quadriceps aswell as the patellar tendon are homogeneous in signal but don't have to be black on PD-images.
They have a sharp posterior demarcation.
There should be no focal thickness.
 Partial quadriceps tendon tear: T2W-images.LEFT: Abnormal attachment of tendon.RIGHT: Most of tendon is retracted (red arrow) deep part (vastus intermedius) is still intact.
Partial quadriceps tendon tear: T2W-images.LEFT: Abnormal attachment of tendon.RIGHT: Most of tendon is retracted (red arrow) deep part (vastus intermedius) is still intact.
Quadriceps tendon tear
The case on the left shows an abnormal quadriceps attachment.
There is only one layer and the attachment does not go from the front of the patella to nearly the back.
In such a case extra images higher up have to be made after repositioning of the coil to see what's going on up there.
The missing part of the torn quadriceps tendon is retracted.
The deep part is still intact
 LEFT: Torn tendon with pre-existing tendinopathy (red arrow). RIGHT: Intact vastus intermedius tendon.
LEFT: Torn tendon with pre-existing tendinopathy (red arrow). RIGHT: Intact vastus intermedius tendon.
Same patient, axial images.
The torn quadriceps tendon is very thick indicating tendinopathy.
Normal tendons do not tear, so always look for signs of pre-existing tendinopathy.
Anywhere in the body, if you see a tendon that looks torn, but there is no pre-existing tendinopathy, think hard, if you really have the right diagnosis.
An image below this level shows normal vastus intermedius muscle and tendon.
 LEFT: Partial quadriceps tear. Only rectus femoris tendon is torn (blue arrow). RIGHT: Pre-existing tendinopathy (yellow cirkle) on axial image.
LEFT: Partial quadriceps tear. Only rectus femoris tendon is torn (blue arrow). RIGHT: Pre-existing tendinopathy (yellow cirkle) on axial image.
Another example of a partially torn quadriceps tendon.
If there is no continuity between the patella and the quadriceps tendons it is a complete tear.
Jumper's Knee
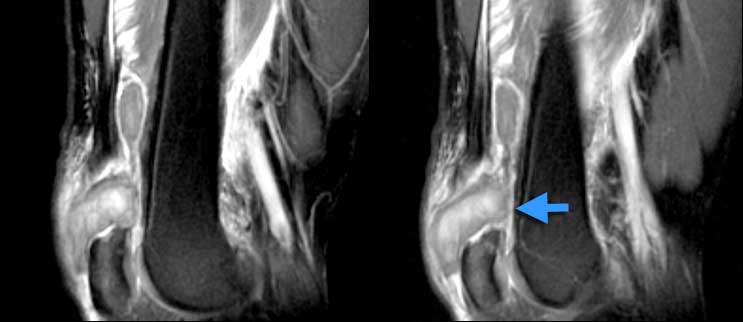
Jumper's knee is a spectrum from tendinopathy to tear.
Just the same as with the quadriceps tendon or any other tendon the MR shows a spectrum from eccentric tendon thickening, indistinct posterior border, increased signal on T2W-images and finally fiber disruption.
Patellar tendinopathy
Patient on the left is a professional ballet dancer with pain underneath the knee cap.
Patellar tendon proximally is too thick. Posterior border is indistinct. In patella a little bit of edema ( or bone bruise). If left untreated could end up like...
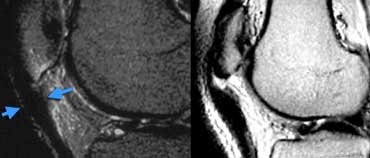
Partial patellar tendon tear. Image on the right of a different patient.
 Complete Patellar tendon tear. Image on the right shows hemorrhagic bursitis ( low signal in bursa).
Complete Patellar tendon tear. Image on the right shows hemorrhagic bursitis ( low signal in bursa).
Complete Patellar tendon tear. Images on the left show no continuity between fibers and patella. The tendon is thickened.
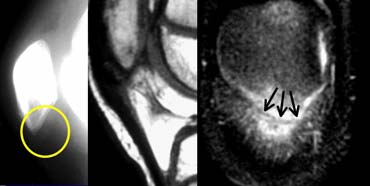
Patellar sleeve avulsion.
In children we have a different situation. They don't develop tendinopathy.
The case on the left shows images of a girl who had pain beneath the patella after doing gymnastics.
Although the X-ray is normal there accually is a fracture through the cartilage part of the lower pole.
On MR it looks just like the jumper's knee above. Only on coronal images the dark fractureline within the bright cartilage is visible.
Usually these fractures are sutured.
When these lesions are unrecognized they heal with ossification just below the patella.
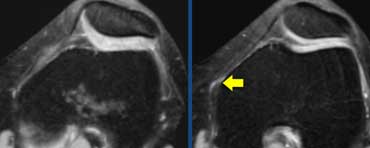
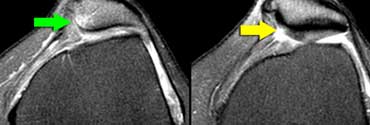
Patellar dislocation
Normal anatomy
The patellar cartilage is the thickest in the body. It should have smooth contours.
The most important part of the medial retinaculum is the medial patellofemoral ligament which inserts all the way posteriorly just in front of the MCL.
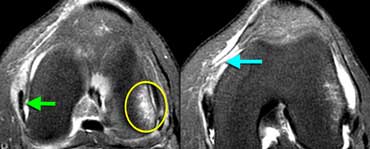 LEFT: Bone bruise lateral condyle (yellow circle). Normal MCL (green arrow) but missing patellar femoral ligament anterior to it.RIGHT: Medial patellar femoral ligament thorn from femoral attachment.
LEFT: Bone bruise lateral condyle (yellow circle). Normal MCL (green arrow) but missing patellar femoral ligament anterior to it.RIGHT: Medial patellar femoral ligament thorn from femoral attachment.
Case on the left is a female soccerplayer who twisted her knee.
Four MR-images from caudal to cranial demonstrate all the imaging features of a patellar dislocation with rupture of the medial patellar femoral ligament .
The patella was dislocated and the medial facet has bumped onto the lateral condyle.
The patella has spontaneously reduced.
Bone bruise may be complicated by cartilage fracture.
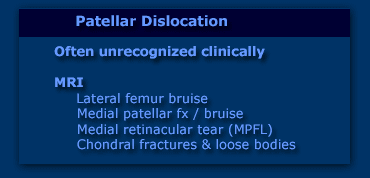
Patellar dislocation (2)
Patellar dislocation is a common condition, but clinically often unrecognized because the patella after the dislocation comes back in it's normal position.
The patient comes with a swollen painfull knee which could be anything from ACL-, MCL- or meniscal tear to a fracture.
So the MRI-findings are important in recognizing this condition.
Patients who have loose bodies or continuing dislocation may undergo operation with retinaculum repair.
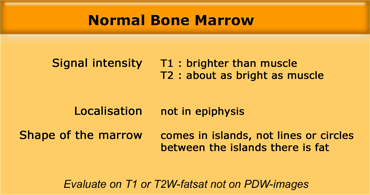
Bone and Cartilage
Normal and abnormal bone marrow
In adults the bone marrow is largely composed of fat.
Normal islands of red marrow may produce confusing images.
Red bone marrow can be pronounced in young women, cigarette smoking, high altitude, hemoglobinopathy or for no reason at all.
As long as the criteria on the left are fullfilled it is normal.
Normal red marrow on the left.
Restricted to the metaphysis and not into the epiphysis.
Comes in islands.
On T1 brighter than muscle.
Abnormal Bone Marrow
Case on the left shows abnormal bone marrow.
On T1W the signal intensity is lower than muscle.
On T2W-images the signal is very bright.
The abnormal signal comes into the epiphysis.
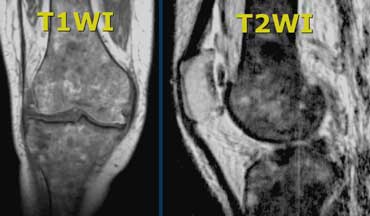 Abnormal bone marrow. There is abnormal signal intensity in the form of circles in metaphysis and epiphysis.
Abnormal bone marrow. There is abnormal signal intensity in the form of circles in metaphysis and epiphysis.
Another case with abnormal marrow.
In this case the marrow is too dark on T1 and T2 due to iron deposition in the marrow after many blood transfusions in a patient with hemosiderosis.
 Avascular Necrosis: fluid underneath the cartilage just like a crescent sign on a X-ray. Cartilage is normal.
Avascular Necrosis: fluid underneath the cartilage just like a crescent sign on a X-ray. Cartilage is normal.
Avascular Necrosis
The most common marrow abnormality is Avascular Necrosis (AVN).
Some people will say 'AVN, Osteochondrosis Dissecans and Stress fracture all look the same'.
There is however a distinct difference.
AVN has the following features:
1. Focal abnormality is subchondral and originates in the bone.
2. Normal cartilage (until it collapses).
3. Wedge shaped marrow edema due to bone infarction.
The wedge-shaped pattern of bone marrow edema is just the same as any other infarction in the body i.e. liver infarction or kidney-infarction.
Insufficiency fracture
On the left a different entity, but the patient had the same symptoms.
Acute onset of medial pain.
There is diffuse marrow edema on T2W-image.
On T1W-image the focal abnormality is not directly subchondral.
The abnormality on the T1 is more inside the edema.
On the T1W-image a dark line is visible indicating a insufficiency fracture.
This patient will get better with no weight bearing.
On the left another patient with knee pain after trauma.
There is some effusion but otherwise the x-rays are normal.
 Tibiaplateau fracture. This also is a osteochondral fracture as the fracture line extends all the way through the cartilage to the joint surface.
Tibiaplateau fracture. This also is a osteochondral fracture as the fracture line extends all the way through the cartilage to the joint surface.
In the same patient the MRI shows an obvious tibiaplateau fracture.
The point is that any patient who is unable to bear weight in the hip, knee or ankle with normal X-rays needs another study.
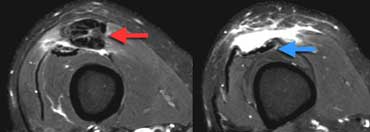
Osteochondritis Dissecans
The diagnosis Osteochondritis Dissecans is usually made on X-rays.
The question for MRI is whether it is stable or unstable.
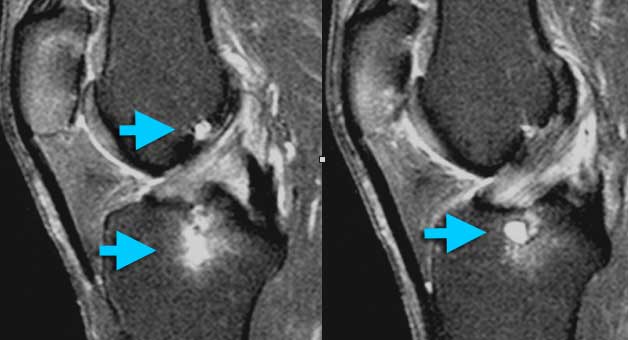
The case on the left is unstable for two reasons:
- small cysts at the base of the lesion (red arrow)
- even more important is fluid at the base of the lesion (blue arrow)
Notice that this layer of fluid is different from AVN where the fluid is between the cartilage and the bone.
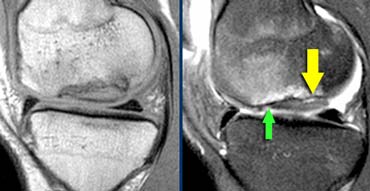 Unstable Osteochondritis Dissecans. The only helpfull sign for the diagnosis unstable OD is the fluid (yellow arrow) not the edema nor the break in the osteochondral surface (green arrow).
Unstable Osteochondritis Dissecans. The only helpfull sign for the diagnosis unstable OD is the fluid (yellow arrow) not the edema nor the break in the osteochondral surface (green arrow).
Not helpfull for the discussion stable versus unstable OD are
- bone marrow edema (could be stable or unstable)
- break in the osteochondral surface.
So the case on the left is unstable because there is fluid at the base of the lesion.
The case on the left shows a OD with bone marrow edema and a break in the osteochondral surface.
But since there is no fluid we cannot tell if this is stable or unstable.
At operation the OD was found to be stable
In those cases where you cannot tell whether the lesion is stable or unstable MR-arthrogram is helpfull.
We look for Gadolineum tracking around the osteochondral lesion.